Key Message
What Is Already Known on This Topic
Hospital bed saturation is a serious concern in surgical departments. Senior multidisciplinary board rounds instead of ward rounds can improve inpatient care and flow.
What This Study Adds
We describe the introduction of a flow-enhancing framework (SAFER surgery R2G) designed for any inpatient surgical specialty, with the potential to significantly and safely shorten hospital stays, reduce cancellations, and more efficiently use ICU/HDU beds.
How This Study Might Affect Research, Practice or Policy
The model is designed in principle to deliver benefits across multiple services and hospitals. Our experience might represent a basis for comparison and new projects, as further applications are required to validate our results.
Local Problem
The Royal London hospital is an 845-bed major trauma centre where the Helicopter Emergency Medical Service is based. The increasing demand for emergency beds in acute wards has contributed to capacity saturation and this, along with a slower patient flow, delays step-downs from the high dependency (HDU) and intensive care units (ICU). The consequent unavailability of postoperative surgical beds occasionally results in ‘on the day’ hospital-initiated cancellation of elective surgery, for both benign and cancer cases, peaking in 2016 at over 50% at times. In our digestive surgery service, ward rounds were run on a consultant firm basis on the 25-bed ward admitting approximately 1000 cases yearly, including general/digestive surgical cases and up to 25% short-stay emergency “outlier” patients, i.e., temporarily occupying a general/digestive surgery bed from different specialties such as vascular surgery, trauma, and neurosurgery, and to a lesser extent patients from medical specialities.
Patient flow was perceived as an issue and tackled at the Trust level (Barts Health NHS Trust) in a large-scale improvement project, by choosing the ”SAFER patient flow bundle” [
1] and the ”Red to Green days” [
2] models.
Available Knowledge and Rationale
Bed shortage has long been a concern for Healthcare Systems [
3]; at times it has contributed to serious consequences for patients due to saturation of hospital capacity [
4] and raised general public concern [
5,
6]. Awareness of these limited resources in surgery has triggered the development of initiatives (including by some of the authors) to streamline elective surgery patient flow as well as procedure prioritisation [
7,
8], and selection [
9], in order to increase the efficiency of theatre scheduling [
10,
11] and utilization [
12], and to enhance postoperative clinical recovery [
13]. However, evidence from projects introducing early discharge from acute admissions shows uncertain improvement in health and resources, suggesting that these interventions must be tailored to the specific environment and individual patient [
14].
Surgical ward rounds (i.e., clinicians visiting each patient on their list, reviewing their history, examination, investigations and treatment on the ward) are the setting where the inpatient care plan is usually defined, making good use of hospital resources and anticipating clinical readiness for discharge [
15]. In recent decades research interest has also grown around ward round methodology. Structured ward rounds have proven to enhance the quality of surgical care [
15,
16], showing benefits in patient safety by using a ward-round template [
17,
18] and involving senior medical and nursing staff in setting their care plan [
19].
While senior assessment during daily ward rounds has proven clinically beneficial and cost effective [
20,
21], multidisciplinary (MDT) bedside ward rounds in surgery have been reported [
22] to enhance team work with reductions in length of stay (LOS) and costs [
23]. However, given that senior staff tend to have busy, independent schedules, having them regularly attend full MDT bedside rounds might be difficult, or require amendments in their job plan. Short (30’) board rounds (i.e., gatherings in an office, discussing a list of patients) instead of bedside ward rounds can facilitate this daily senior MDT assessment [
24].
In the context of centralised, super-specialised patient care, patient flow has become a critical issue in hospital management [
25], and delayed discharges have been shown to worsen hospital bed occupancy and quality of care [
26], especially in emergency departments [
27,
28]. Along with MDT board rounds, the “SAFER patient flow bundle” [
1] model has been introduced in the English National Health Service (NHS England), along with the “Red to Green days” [
2] approach. The “SAFER patient flow bundle” is based on enhancing patient flow by a systematic daily senior review of all patients on the ward, focusing on achieving an early discharge; “Red to Green days” focuses on tackling causes of delayed progress towards discharge in real time. Since their introduction [
29], these models have found an expanding application in the NHS [
30], however they were not designed for adoption in all settings. To our knowledge, use of these models has never before been reported in a general surgery environment.
Aim
Our aim was to set up, introduce and conduct a 12-month study on an MDT board round framework (called “SAFER Surgery R2G”) specifically adapting the “SAFER patient flow bundle” and the “Red to Green days” approaches in the Royal London Hospital general/digestive surgery ward. The goal was to improve patient flow (i.e., 10% LOS reduction in general/digestive surgery patients) safely (i.e., keeping hospital re-admissions below 5%), sustainably (with >60% staff compliance) and without additional resources.
Methods
Context
The 25-bed general/digestive surgery in-patient ward at our hospital provides care for patients belonging to upper gastrointestinal, colorectal and hepato-pancreatobiliary specialities. The service has 11 consultants and 18 junior doctors, its own resident nursing team and a ward manager. The digestive specialist consultant firms are responsible for the care of their respective patients. The general/digestive surgery department runs a 24-hour consultant emergency on-call rota from mid-day to mid-day (e.g., Consultant A – starts at 12, 00 on Monday and finishes on 12, 00 on Tuesday). Patients for planned major complex surgery are admitted to a separate ward but are postoperatively stepped down from the HDU to the ward.
During our project, the division of surgery ran several initiatives to improve patient flow. These initiatives focused on different steps of the flow process, potentially interfering with our work:
a “complex discharge” (i.e., delay caused by aftercare issues external to the hospital) facilitation project by a dedicated team liaising with referring GPs and aftercare units;
a “theatre-go” policy, which aimed to start the first operation in every list even when the postoperative bed had not been identified, assuming this would become available later in the morning;
a pre-discharge step-down policy towards a lower intensity area and increased usage of the discharge lounge.
Patient Involvement
Previous reports have shown benefits of inpatients' realistic expectations and motivation to participate in enhancing the pre- and post-discharge setting [
31]. For this reason, even though we did not involve patients structurally, they and their families were actively involved in setting the discharge goals.
Intervention
Study Design
This is an 18-month quality improvement study, led by four of the authors named (three consultant surgeons AA, RV, MAT and a specialist nurse LS), monitoring the impact of introducing in the Royal London Hospital general/digestive Surgery Service the “SAFER patient flow bundle” and “Red to Green” models, adapted into a combined framework suitable for the surgical ward (SAFER Surgery R2G), and comparing the outcomes at three PDSA cycles (0, 1, 2). The study is registered ISRCTN13976096 and is reported here according to the SQUIRE 2.0 standard [
32].
SAFER Patient Flow Bundle
The SAFER patient flow bundle [
1] is a model designed to increase patient flow and safety in acute medical wards by consistently adopting five elements of good practice:
Senior clinical review, provided every morning to every patient, ensuring management and discharge decisions, including any necessary rehabilitation.
All patients to be assigned clinical criteria for discharge and an expected date, assuming no unnecessary delay.
Flow of patients (assessment, admission, discharge) ensured as early as possible, every weekday morning.
Early discharge of at least 33% of patients by midday.
Review provided systematically by the MDT, aiming at reducing unnecessarily prolonged stays, encouraging daily board rounds.
Red-to-Green Days
The Red-to-Green days [
2] model is an approach to optimise patient flow by assessing whether the day spent in hospital was useful or not, colour-labelling each day accordingly and aiming at improving service performance to avoid unnecessary bed-occupancy days.
In a green bed day, necessary acute inpatient care is provided and at least one diagnostic/therapeutic procedure in the plan towards discharge is performed.
In a red bed day, no diagnostic/therapeutic procedure towards discharge is performed, or care is unnecessarily provided in an acute hospital setting.
PDSA-0 – Baseline & Feasibility
In a baseline three-month Plan-Do-Study-Act cycle (PDSA-0) in October-December 2016 the protocol for the study was designed, based on available evidence and experiences, Barts Health Trust policies and projects. In December 2016 the general/digestive surgery service audit meeting attended by all grades of medical staff approved the preliminary protocol, designed according to the following key principles:
all admissions to the general/digestive surgery ward as of January 1st 2017 are included in the project, irrespective of the base specialty;
each surgical firm informs the nurse in charge of the key care plan set during the afternoon ward rounds;
-
a daily senior multi-disciplinary team (MDT) morning board round is attended by all relevant clinical staff representatives, addressing:
- o
updated key care plan aimed at safe, early discharges;
- o
appropriateness evaluation of each bed day;
hospital managers and site managers attend the board round at least once weekly;
the improvement is designed to achieve long term sustainability;
safety and effects of the improvement are monitored by recording adverse events, basic patient flow parameters, staff member compliance and feedback.
PDSA-1 - Pilot
A three-month Plan-Do-Study-Act cycle (PDSA-1) was planned to pilot the application from January 1
st to March 31
st 2017. The structured board round was chaired only by the three project leading consultant surgeons with the dedicated specialist nurse. The monthly Service audit meetings were used to report progress to the wider team and receive feedback on any issues raised during the initial PDSA-0. The study team assessed the safety and feasibility of the project at weekly team meetings aside from the board round and discussed interim assessments of the outcome measures. The final study protocol was presented to and approved at a consensus meeting at the monthly departmental audit day (see
Table 1).
During discussions staff described their perception of enhanced patient safety (reducing errors) and quality of care (effective treatments), capacity management (better use of the bed-day), and teamwork, due to the chance of discussing the care plan in the multidisciplinary meeting, where senior decision making was promptly available.
PDSA-2, Full Improvement
The PDSA 2 full improvement study was conducted from 1st April to 31st December 2017. As a main change compared to the previous phase, all rotating consultants on-call the previous night chaired the daily MDT board round every day, immediately following their respective post-emergency take ward rounds. A prospective audit of the board round was run, collating information on project progress, outcome measures, attendance, and feedback. The SAFER Surgery R2G framework was planned to be kept in use beyond the study.
Along with the pilot PDSA-1 progress, we observed some changes that might potentially interact with the project setting. These include the contemporary hospital flow-enhancing initiatives, and the extension of the SAFER Surgery R2G model to other surgical wards, sharing the improvement team and making them less available to our project. The Division of Surgery and the Service of Anaesthesia deemed the flow steadily improved, enough to start a theatre-go policy, established in month 7 (July 2017).
Study Outcome Measures
Patient Flow Measurements
We chose the average length of stay (LOS) of general/digestive surgery patients as the primary outcome measure. Secondary measures: the weekly count of ward discharges (WCWD) of general/digestive surgery patients in the index week; the monthly count of ICU / HDU step-downs to the surgical ward; the count of hospital-initiated on-the-day cancellations of elective surgical cases due to ICU / HDU or ward bed unavailability. As broad measures of process are controlled by patient safety, while introducing changes to expedite hospital stays, we chose the weekly count of readmissions within 30 days from discharge. The above data were gathered and analysed from the hospital admission systems, which contained no gaps.
The above patient flow measures were analysed:
at the end of PDSA-0 as the 12-month baseline from year 2016;
at the end of the first 3-months January-March 2017 PDSA-1;
at the end of the 9-month PDSA-2.
Participants’ Compliance and Satisfaction
As a broad index of sustainability staff compliance with the project was measured monthly, as the percentage of actual versus expected attendants per specialty to the MDT board round (see
Table 1).
A qualitative assessment of the satisfaction rates by MDT board round participants per specialty / grade was collected monthly during the Monday board round. It was administered to the (up to 14) participants, as a measure of project effectiveness and work environment appreciation, providing a 1-5 score on the following question: “How satisfied are you by the MDT board round as an occasion to share and act upon the patients’ issues and expedite their progress safely?”. The score was computed as a ratio divided by five and expressed as a percentage.
Statistical Analysis
The results are expressed as mean ± standard deviations, medians, counts or percentages. The Shapiro-Wilk test was used to assess normal distribution of continuous variables. Since the Shapiro-Wilk test was found to be significant in all continuous variables of our series, the null hypothesis that each continuous variable came from a normally distributed population was rejected and non-parametric tests were used. Categorical variables were analysed with χ2 test or Fisher's exact text when appropriate. Comparisons between continuous variables were carried out by using the Mann-Whitney-Wilcoxon rank sum test or the Kruskal-Wallis test followed by the Dwass-Steel-Critchlow-Fligner test for post-hoc comparisons. The continuous variables measured weekly were displayed over time by control charts, placing weekly numbers on the x-axis. The centre line on the control charts represents the mean, with two additional lines for the upper and lower control limits. Statistical significance was assumed in each two-tailed test with p value <0.05. Statistical analysis was carried out by using the R software/environment (version 4.0.3; R Foundation for Statistical Computing. Vienna, Austria).
Results
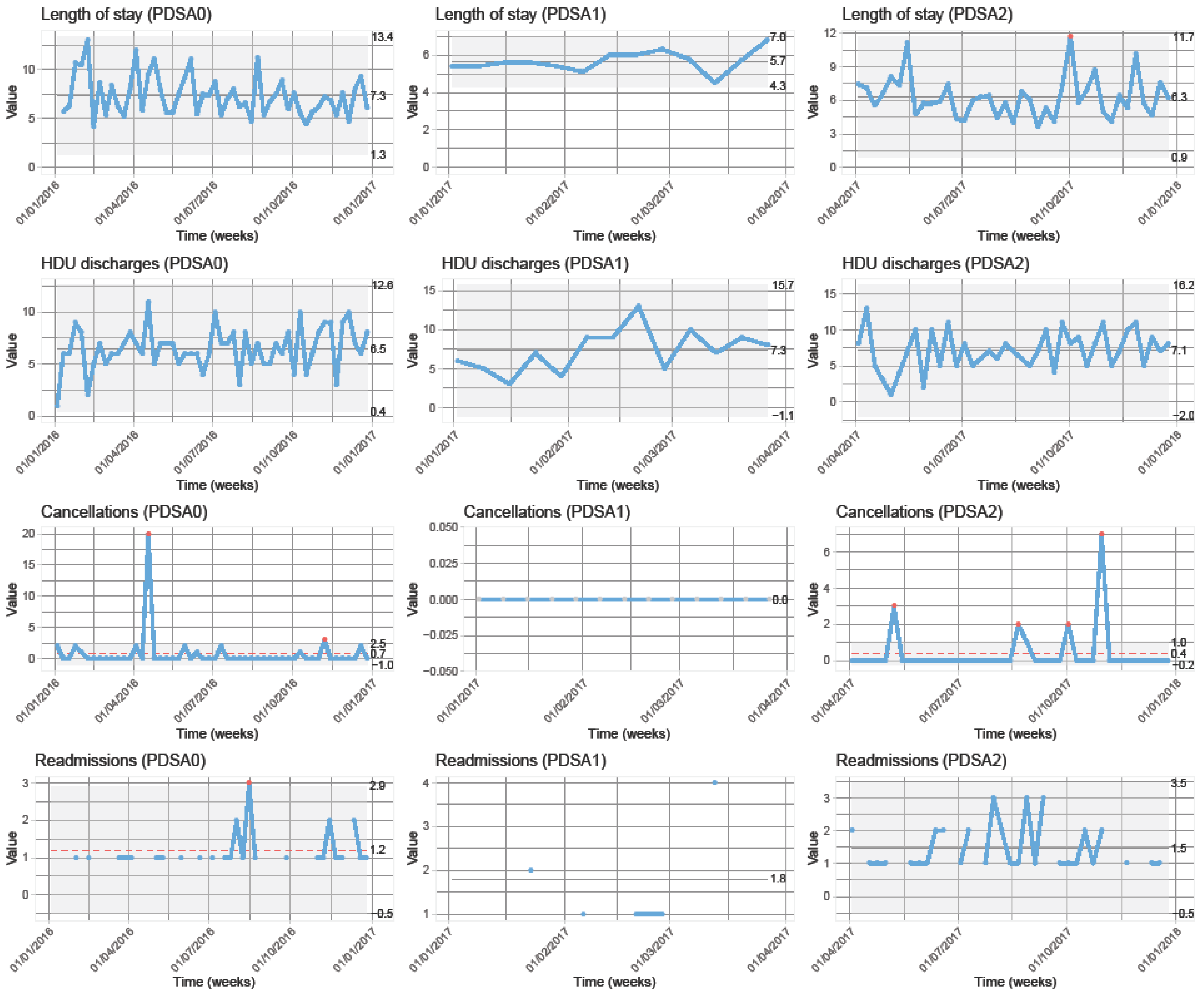
The comparative results of each PDSA are shown in
Table 2, and the relative control charts in
Figure 1.
PDSA-0 - Baseline & Feasibility
The overall control charts are added as supplementary material. Throughout 2016, the 25-bed capacity stayed close to 100%, in the absence of prolonged unavailability. At the end of the PDSA-0 period (31/12/2016) 954 patients had been discharged from the ward, including 401/522 females/males aged 56.6 (±18.4). 17.1% were outlier patients. The baseline mean LOS of general /digestive surgery patients was 7.2(±8.9) days, and the mean weekly ward discharge count (WWDC) was 14.8(±3.5). 30-day monthly re-admissions were 1.2 (±0.5) (N=9). A number of patients perceived by the project team as relevant were subject to complex discharges. However, given that a specific Trust initiative was active, the issue was not measured by our project. Hospital-initiated cancellations counted 6.5(±2.0) cases weekly (N=38), ICU / HDU step-downs 6.5(±2.0) weekly (N=342), and a “Theatre-go” policy was not active.
PDSA-1 - Pilot
At the end of the PDSA-1 pilot phase 275 new patients (116 females / 159 males) aged on average 57 (±18.3) years had been discharged. No major adverse events related to the intervention had been recorded. Average overall attendance of the MDT board rounds was 83% and a satisfaction rate of 91% was recorded overall by the staff speciality representatives attending. In comparison with the previous PDSA-0 the mean general/digestive surgery patients LOS reduced from 7.2(±8.9) to 5.7(±6.6), the mean WWDC increased from 14.8(±3.5) to 17.2 (±4.2), and ICU/HDU weekly step-downs raised from 6.5(±2.0) to 7.3(±2.8). There was no cancellation and monthly 30-day readmissions were 1.8(±1.3).
Additionally, comparing the PDSA-1 with the same three-month (January-March) period in the previous year, the general/digestive surgery mean LOS significantly reduced from 7.7 (±8.4) to 5.7 (±6.9) days (p<0.001), the WWDC increased by 27% from 17.91 (N=215) to 22.9 (N=275) discharges. ICU/HDU monthly step-downs significantly increased to 31.7 (N=95) from 27 (total N=81) (p=0.043).
At the monthly Service Audit Meeting, the issue of lacking communication between surgical teams and the nurse in charge was reported in approximately one third of the afternoons. This issue was not recorded objectively, and not measured throughout the project. However, it was perceived as relevant by the MDT team and triggered a constant reminder to the clinical teams from then on.
PDSA-2 – Full improvement
During the 9-months PDSA-2 the improvements observed during the previous PDSA-1 reduced their immediate magnitude, however stabilising on a positive result. The outlier patient admissions further increased, peaking at 47% of the ward occupation in week 13.
Compared to PDSA-1, the mean LOS increased to 6.3(±7.7) days (p=0.281), a better value than in the baseline PDSA-0 (p=0.478). The mean WWDC reduced to 16.1 (±4.6), still higher figure than the baseline PDSA-0. ICU/HDU weekly step-downs decreased to 7.1(±2.7), again better than in PDSA-0. Cancellations decreased to 0.4(±1.3)(N=15)(p=1), allowing the Division of Surgery and the Service of Anaesthesia to activate a “Theatre-go” policy as of July 2017 and all major elective cases to proceed. Monthly 30-day re-admissions non-significantly increased to 1.5(±0.7)(N=12).
Comparing the whole intervention year 2017 against the previous baseline 2016, overall discharges increased from 954 to 1032 (+8.1%), the mean general/digestive surgery patients’ LOS significantly decreased from 7.2(±8.9) to 6.3(±7.4) days (p=0.003), while the overall LOS decreased from 6.9 (±8.6) to 6.1 (±7.4) almost reaching significance (p=0.062), while WWDC increased from 14.8 (±3.5) to 16.3 (±4.4) (p=0.094). The ICU/HDU step-down increased in total cases from 345 to 375 (p=0.197).
As the PDSA-2 cycle started in April 2017, the MDT board rounds attendance of chairing consultants and senior staff members initially fell to 75% as the lowest average attendance by all actors. During the whole period attendance by surgical teams was the hardest to achieve (consultant 75%, registrar 60%), however the overall average from all specialties was 80% throughout. The monthly review meeting revealed that such a low rate was mostly due to conflicting commitments for the senior staff members, precluding them from attending the board rounds. The SAFER Surgery R2G framework was however applied until the end of the monitored period in December 2017 and still is.
High satisfaction (>75%) rates with the framework were recorded by all MDT staff categories, that commented mainly on enhanced teamwork and faster decisions on clinical plans.
Discussion
Summary
To our knowledge, this is the first report describing a new application of an MDT board round combining the “SAFER patient flow bundle” and the “Red to Green days” approaches adapted for a surgical service in a single framework. In our experience, the adoption of this framework, which we named “SAFER Surgery R2G”, has been associated with objective improvement in patient flow, significantly reducing the general/digestive surgery patients’ LOS by 12.5% (i.e., beyond the 10% threshold we had set initially), without compromising their safety i.e., keeping 30-day readmissions below 5%, the threshold we had chosen at the start of our project. This model has also potentially contributed to solving major capacity issues in the context of saturated bed occupancy, such as reducing cancellations and allowing a stable hospital “theatre-go” policy, making it possible for elective surgical theatre lists to start irrespective of the early actual HDU/ICU bed availability. However, compliance results raised sustainability issues which required effort throughout the intervention year.
Interpretation
The application of the “SAFER Surgery R2G” framework has shown clearly positive results in LOS reduction. Evidence from other studies supports the advantages of structured board rounds, and senior assessment during daily ward rounds has proven to be clinically beneficial and cost effective [
20,
21]. Board rounds instead of ward rounds can facilitate such daily senior MDT assessment [
24]. However, only little experience has been published about the application of frameworks similar to the one we have introduced in surgical environments [
33], which have potentially relevant implications.
The improvements we have measured in LOS were more evident during the initial 3-month PDSA-1 than during the subsequent 9-months PDSA-2. We attribute this effect primarily to the observation of beds freed at discharge frequently occupied by ‘outlier’ patients who were emergency-admitted on our surgical ward overnight as a bed was unavailable on their respective specialty wards. Outlier patients occupancy peaked at over 18.5% in PDSA1, slowly decreasing to 17.3% % in PDSA-2. Of note, our MDT board round had no effect on their clinical plan or LOS. During PDSA-2, the steady patient flow enhancement allowed for the start of the “theatre-go” policy mentioned above. This policy is still in place.
We experienced difficulty in discharging clinically-ready patients due to an insufficient capacity by the community-based environment to repatriations, community care, rehabilitation, etc. During the second part of the PDSA-2, a pre-discharge step-down lower intensity area and a discharge lounge were increasingly utilised. Additionally, the above-mentioned “complex discharge” dedicated team kept liaising with GPs and aftercare units. Such contemporary initiatives have supported enhancing patient flow, probably allowing for more frequent discharges from the ward.
We recorded the difficulty to reach full attendance by the senior staff busy in conflicting commitments, hence causing some delay in prompt non-urgent decisions on our inpatients and causing some frustration on the part of the less-senior staff.
We assessed the impact of our project on the people involved with a one-question survey in a semi-quantitative fashion, by a grade of appreciation, scoring approximately 75%. On a wider range, participant comments and notes have shown that the SAFER Surgery R2G framework has positively impacted their everyday work, contributing to enhancing the perception of teamwork and clinical leadership on the ward, particularly the nurse in charge leading the meeting. Additionally, ward staff reported that access to care plan information provided by the structured handover and attending the board is easier and faster than looking for colleagues and asking for such information.
Limitations
To measure the effects of our service improvement we have chosen generic and non-specialty specific indicators, independent from diagnoses or procedure groups. This helps to maximise external reproducibility in other hospitals; however, it lacks a more in-depth view of patients’ different subgroups. Additionally, the internal validity of our study is certainly affected by the change over time in the complex hospital organisation where our project was run. To reduce this impact, we have followed PDSA cycles and observed the results over time, completing a 12-month comparative study. More research is, however, needed beyond our work to further investigate its findings.
We identified several confounding factors. Firstly, outlier patients are admitted on the same ward but outside the care-lead of the SAFER Surgery R2G MDT board round. To address this limitation in the study, we have monitored outlier and non-outlier patients, as both categories of patients compete for the same bed capacity.
Additionally, we have not measured the impact on patient flow of the frequent complexity of discharge which, as mentioned above, might have influenced our results, as found from other hospital specialties [
34]. The wider use of regional electronic data systems may be the step forward to refine such measurements [
35]. We could not reliably measure more precise, tool-specific parameters (i.e., time from clinical fitness to actual discharge, morning discharges, totals of Red to Green days, cause of delays etc.), as these outcome measures during our pilot PDSA-1 proved difficult to collect reliably. This appeared to be due to insufficient resources to run the data collection, given some project staff were also enrolled in different contemporary projects.
Participants’ compliance attendance at our MDT board round has been an issue throughout the project. Surgeons are often busy in theatre or are required to manage emergency cases, even though these have not been the reported reasons for lack of attendance in the board round (consultants), or the afternoon handover to the nurse in charge (registrars). Additionally, the senior administrative team at the Royal London Hospital have been busy with several other programs contemporary to ours, and had difficulty in attending the meetings too. Hence, we think that the needs for leadership commitment might represent another limitation to the application of the SAFER Surgery R2G framework. However, even in the context of changes in the hospital organisation, the model is still in use now, showing a sufficient degree of sustainability.
Conclusions
The SAFER Surgery R2G framework is designed for use in any inpatient surgical specialty. It has shown potential to deliver improvements in patient flow in a surgical service, by significantly faster hospital stays, more efficient use of ICU/HDU beds, and reduced cancellations. Our experience might represent a basis for comparison for new projects, as further applications are required to validate our results.
Ethics Approval Statements
The “SAFER patient flow bundle” and the “Red to Green days” approaches had already been in use in the NHS hospitals in other specialties for approximately two years and were considered at the time by our Division to be introduced as a service improvement that did not change any clinical practice. The chosen site of improvement was the general/digestive ward at the Royal London Hospital. The study had been approved at the time by the Service with the design of a quality improvement study. The Division of Surgery is aware that the study has been registered publicly and its results submitted for publication. Given that no change in clinical care was made to inpatients, neither ethics approval nor patient consent was deemed necessary.
Author Contributions
R.V. and M.A.T. conceived the study, edited the manuscript, provided, and interpreted the available data. L.S. contributed to managing the study and gathering the data and also provided intellectual content. A.A. co-conceived the study, contributed to interpreting the data and provided relevant intellectual content. G.S. contributed to data interpretation and performed statistical analysis. All authors revised the manuscript.
Funding
The project was run within NHS staff working hours, with no additional external or ad-hoc fund.
Conflicts of Interest
None.
References
- SAFER Patient Flow Bundle: Ward Rounds | NHS Improvement. Available online: https://improvement.nhs.uk/resources/safer-patient-flow-bundle-ward-rounds/ (accessed on 5 October 2020).
- The SAFER Patient Flow Bundle and Red to Green Days Approach | NHS Improvement. Available online: https://improvement.nhs.uk/resources/safer-patient-flow-bundle-and-Red to Green-days-approach/ (accessed on 21 June 2018).
- Agnew, GH. The Shortage of Hospital Beds. Can. Med. Assoc. J. 1942, 46, 373–374. [Google Scholar] [PubMed]
- Simmons, FM. CEU: Hospital overcrowding: An opportunity for case managers. Case Manag. 2005, 16, 52–54. [Google Scholar] [CrossRef] [PubMed]
- Campbell D, Morris S, Marsh S. NHS faces ‘humanitarian crisis’ as demand rises, British Red Cross warns. The Guardian. Available online: http://www.theguardian.com/society/2017/jan/06/nhs-faces-humanitarian-crisis-rising-demand-british-red-cross (accessed on 24 May 2018).
- O’Dowd, A. Doctors condemn need for Red Cross to step in to aid NHS in “humanitarian crisis”. BMJ 2017, 356, j127. [Google Scholar] [CrossRef] [PubMed]
- Déry J, Ruiz A, Routhier F, Gagnon MP, Côté A, Ait-Kadi D; et al. Patient prioritization tools and their effectiveness in non-emergency healthcare services: A systematic review protocol. Syst. Rev. Syst. Rev. 2019, 8, 78. [CrossRef] [PubMed]
- Valente R, Di Domenico S, Mascherini M, Santori G, Papadia F, Orengo G; et al. A new model to prioritize waiting lists for elective surgery under the COVID-19 pandemic pressure. Br. J. Surg. 2021, 108, e12–4.
- Malik HT, Marti J, Darzi A, Mossialos E. Savings from reducing low-value general surgical interventions. 2018, 105, 13–25.
- Cardoen B, Demeulemeester E, Beliën J. Operating room planning and scheduling: A literature review. Eur. J. Oper. Res. 2010, 201, 921–932. [CrossRef]
- Levine WC, Dunn PF. Optimizing Operating Room Scheduling. Anesthesiol. Clin. 2015, 33, 697–711. [CrossRef]
- Lee DJ, Ding J, Guzzo TJ. Improving Operating Room Efficiency. Curr. Urol. Rep. 2019, 20, 28. [CrossRef]
- Neville A, Lee L, Antonescu I; et al. Systematic review of outcomes used to evaluate enhanced recovery after surgery. Br. J. Surg. 2014, 101, 159–170. [CrossRef]
- Gonçalves-Bradley DC, Lannin NA, Clemson L, Cameron ID, Shepperd S. Discharge planning from hospital. Cochrane Database Syst. Rev. 2022, 2, CD000313.
- Shetty K, Poo SXW, Sriskandarajah K, Sideris M, Malietzis G, Darzi A; et al. ‘The Longest Way Round Is The Shortest Way Home’: An Overhaul of Surgical Ward Rounds. World J. Surg. 2018, 42, 937–949. [CrossRef] [PubMed]
- Pucher PH, Aggarwal R, Darzi A. Surgical ward round quality and impact on variable patient outcomes. Ann. Surg. 2014, 259, 222–226. [CrossRef]
- Gilliland N, Catherwood N, Chen S, Browne P, Wilson J, Burden H. Ward round template: Enhancing patient safety on ward rounds. BMJ Open Qual. 2018, 7, e000170. [CrossRef] [PubMed]
- Tranter-Entwistle I, Best K, Ianev R, Beresford T, McCombie A, Laws P. Introduction and validation of a surgical ward round checklist to improve surgical ward round performance in a tertiary vascular service. ANZ J. Surg. 2020, 90, 1358–1363. [CrossRef] [PubMed]
- Massey D, Aitken LM, Chaboyer W. What factors influence suboptimal ward care in the acutely ill ward patient? Intensive Crit. Care Nurs. 2009, 25, 169–180.
- Geary S, Cale DD, Quinn B, Winchell J. Daily Rapid Rounds: Decreasing Length of Stay and Improving Professional Practice. JONA J. Nurs. Adm. 2009, 39, 293–298. [CrossRef] [PubMed]
- Ahmad A, Weston PJ, Ahmad M, Sharma D, Purewal T. A cost-benefit analysis of twice-daily consultant ward rounds and clinical input on investigation and pharmacy costs in a major teaching hospital in the UK. BMJ Open 2015, 5, e007367. [CrossRef] [PubMed]
- Felten S, Cady N, Metzler MH, Burton S. Implementation of collaborative practice through interdisciplinary rounds on a general surgery service. Nurs. Case Manag. Manag. Process Patient Care 1997, 2, 122–126.
- May;13, 311-317 JHM 2018. Improving teamwork and patient outcomes with daily structured interdisciplinary bedside rounds: A multimethod evaluation. J Hosp Med 2018, 13, 311–317. [CrossRef]
- Shabbir A, Wali G, Steuer A. Four Simple Ward Based Initiatives to Reduce Unnecessary In-Hospital Patient Stay: A Quality Improvement Project. BMJ Open Qual. 2015, 4, u208974–w3661.
- Catalyst, N. What Is Patient Flow? NEJM Catal [Internet]. 2018 Jan 1 [cited 2020 Oct 4]. Available online: https://catalyst.nejm.org/doi/abs/10.1056/CAT.18.0289.
- Majeed MU, Williams DT, Pollock R, Amir F, Liam M, Foong KS; et al. Delay in discharge and its impact on unnecessary hospital bed occupancy. BMC Health Serv. Res. 2012, 12, 410.
- Boden DG, Agarwal A, Hussain T, Martin SJ, Radford N, Riyat MS; et al. Lowering levels of bed occupancy is associated with decreased inhospital mortality and improved performance on the 4-hour target in a UK District General Hospital. Emerg. Med. J. 2016, 33, 85–90. [CrossRef] [PubMed]
- Khanna S, Sier D, Boyle J, Zeitz K. Discharge timeliness and its impact on hospital crowding and emergency department flow performance. Emerg. Med. Australas. 2016, 28, 164–170. [CrossRef] [PubMed]
- Safer, faster, better: Transforming urgent and emergency | NHS Improvement [Internet]. [cited 2018 Jun 21]. Available online: https://improvement.nhs.uk/resources/safer-faster-better-transforming-urgent-and-emergency/.
- Safer Red to Green | Evidence search | NICE [Internet]. [cited 2020 Oct 5]. Available online: https://www.evidence.nhs.uk/search?q=safer+Red to Green&Route=search&ps=100.
- Ohta B, Mola A, Rosenfeld P, Ford S. Early discharge planning and improved care transitions: Pre-admission assessment for readmission risk in an elective orthopedic and cardiovascular surgical population. Int. J. Integr. Care 2016, 16, 10. [CrossRef] [PubMed]
- Ogrinc G, Davies L, Goodman D, Batalden P, Davidoff F, Stevens D. SQUIRE 2.0 (Standards for QUality Improvement Reporting Excellence): Revised publication guidelines from a detailed consensus process. Can. J. Diabetes 2015, 39, 434–439. [CrossRef] [PubMed]
- Irvine S, Awan M, Chharawala F, Bhagawati D, Lawrance N, Peck G; et al. Factors affecting patient flow in a neurosurgery department. Ann. R. Coll. Surg. Engl. 2019, 1–7.
- Candeias, J. RED TO GREEN DAYS [Internet]. 2018. Available online: https://www.academy.solent.nhs.uk/media/38069/jo-candeias-red2green-poster.pdf.
- Emes M, Smith S, Ward S; et al. Improving the patient discharge process: Implementing actions derived from a soft systems methodology study. Health Syst 2018, 8, 117–133. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).