1. Introduction
The American Physical Therapy Association, published a vision statement, titled: “Vision 2020”, which served as a “call to arms” for the maturation of the physiotherapeutic profession, specifically citing evidence-based medicine as a priority. This was fundamentally centered on reinforcing the objectivity of the examination and intervention processes by implementing modern technologies in the interest of justifying reimbursement in the wake of changing healthcare policies. It has created an initiative to provide physical medicine professionals, such as physiotherapists, with tools that are user-friendly, help synthesize and interpret data, yet are also cost-effective choices. This “call to arms” and integration of strain gauge technology in the isometric training of the knee in everyday physiotherapeutic practice, provides the focus of this paper.
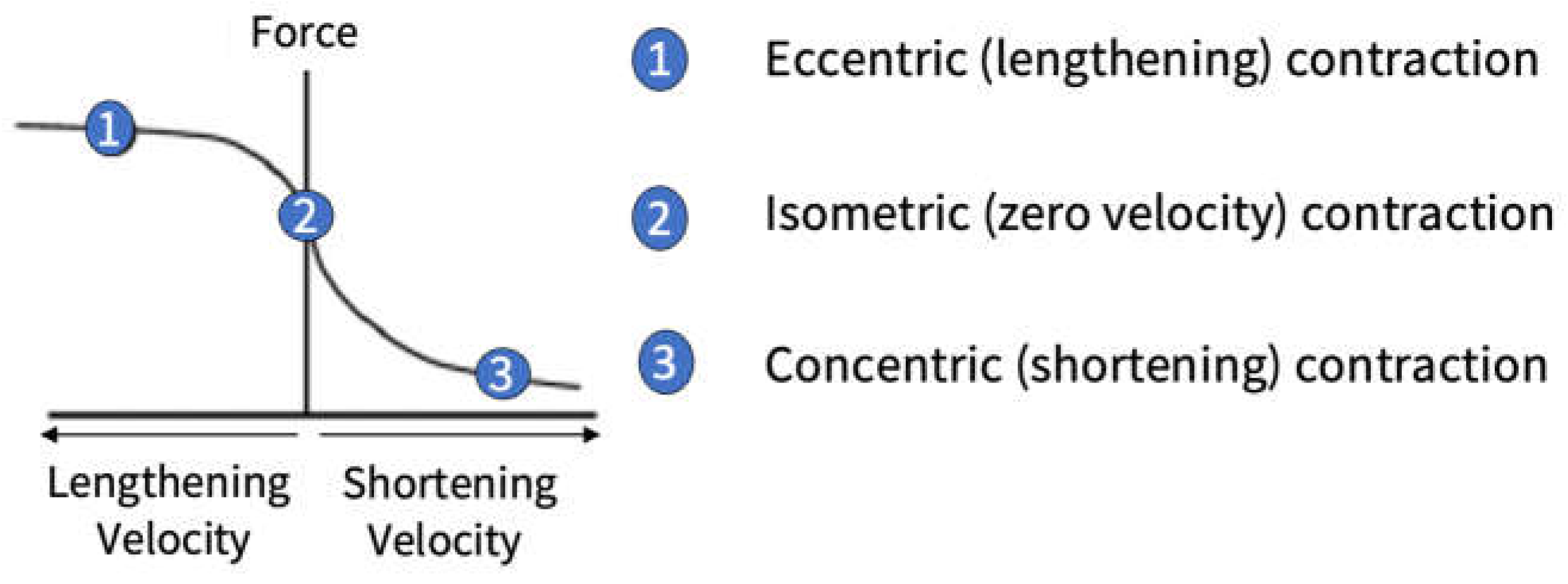
Isometric translates to ‘the same length’, so an isometric contraction, also known as a static contraction, is performed by increasing tension in a muscle while keeping its length constant [
1]. The definition of isometric contraction at a musculotendinous level is not technically correct as what happens in an isometric contraction against an immovable object, is that the muscle contracts and the tendon lengthens the magnitude of both these changes depending on the stiffness-compliance of the tissues involved. For example, there will be very little tendon lengthening if it is naturally stiff. Irrespective of the stiffness-compliance of the tissues, there is length change within the muscle and so defining isometrics as a zero-velocity contraction, or no change in range of motion, is strictly more correct. Isometrics as a zero-velocity contraction sits between the eccentric and concentric force-velocity curves as denoted in
Figure 1. Isometric contractions allow individuals to produce a greater force (maximal voluntary isometric contraction – MVIC) than a maximal concentric action otherwise known as a one-repetition maximum (1RM).
Isometrics have enjoyed a resurgence in popularity in recent times, this being attributed to many reasons: 1) isometric assessments are typically easy to administer, safe and a more time-efficient method to measure maximal strength than traditional 1RM testing [
2]; 2) it’s a reliable way to test maximal strength and peak force in youth and adult athletes [
3]; 3) some of the performance variables from isometric assessments have been shown to significantly correlate to athletic movements such as the vertical jump and sprint speed [
4]; 4) isometrics can be performed at multiple angles and can be used to train ‘weak points/sticking regions’ [
5]; 5) isometrics can provide variability to your programming; 6) in some activities or sports, isometric strength is key to performance e.g. isometric core strength of sprinters to combat angular momentum of the limbs; 7) isometric contractions results in less fatigue compared with high intensity concentric contractions; 8) produces less stress on the body, due to lower impact forces, reducing injury risk [
6]; (9) isometrics as a training method can be used in training programs to develop strength, power, muscle size and tendon stiffness; 10) one of the greatest benefits is its accessibility, being that it can take place anywhere at any time, whether sitting in a plane or working out in a gym and, 11) effectively improves one’s strength after injury whilst minimizing pain and risk of reinjury [
7].
Isometric exercise plays an important role in physiotherapeutic practice as part of rehabilitation from many different injuries. This is exemplified none more so with the knee, with isometrics being prescribed for the rehabilitation of osteoarthritis of the knee [
7,
8,
9,
10,
11,
12,
13,
14,
15]. Interest in isometric training spiked after Rio et al. [
7] reported significantly greater pain relief following a single session of isometric exercise as compared with isotonic exercise. Researchers subsequently have compared isometric and isotonic exercises for patellar tendinopathy-related rehabilitation, with many noticing greater pain relief from isometric contractions [
12,
13,
14]. The effect isometric exercise has on the reduction in pain has been attributed to how it affects cortical changes with antinociceptive effects, including a release of intracortical inhibition [
7]. The isometric rehabilitation of the knee provides the focus of this article.
One of the limitations noted when reading research using isometric exercise for rehabilitation in physiotherapy is the lack of load quantification. In terms of monitoring progress and prescribing load, the majority of the studies participant’s exercise intensity is quantified as an RPE or a % of max effort. In general, however, there is very little objective quantification of load intensity. Quantification of the mechanical load that tissue is exposed to is important in terms of cellular signaling and tissue remodeling i.e., mechanotransduction [
16]. So, metrics such as force (mean and peak), the force applied over a certain time (impulse), the force associated with a change in muscle length (work), and/or the rate at which the force is applied (rate of force development – RFD) are important in terms of optimizing mechanical overload and therefore tissue remodeling.
Given the limitations of load quantification with isometric training in physiotherapeutic practice, and the importance of understanding this in terms of mechanotransduction, this article aims to provide a framework and practical examples of how the physiotherapist may take a more quantitative evidence-based approach for isometric assessment, monitoring, and exercise prescription by integrating a strain gauge into their practice. Furthermore, the knee will provide the focus for this implementation.
1.1. Strain Gauge Integration
The strain gauge is a device that can be used to quantify the strength/force output of various muscles, during a myriad of exercises. Force applied from muscles distorts an S-Beam load cell and this deformation produces a voltage change within the device, which is then converted to a digital reading of load/weight/force. The strain gauge shown in
Figure 2 can detect both tensile (pulling) and compressive (pushing) forces depending on the attachments being used as shown in
Figure 3 and
Figure 4. The strain gauge shown (TruStrength, Auckland, NZ) can measure forces up to 1000 kg or 10,000 N, which is needed if you are measuring movements like isometric mid-thigh pulls and squats. However, smaller strain gauges could be used depending on the needs of the user. This model also collects information (sampling rate) at 1000 Hz, which is thought important for accuracy when measuring time series data such as rate of force development (RFD) or impulse at 200ms. The strain gauge is a highly portable and reliable device, that has high utility as shown in
Figure 3 and 4 where it can be attached to a rack to measure a multitude of isometric movements depending on the attachments.
1.2. Strain Gauge Integration for Assessment and Monitoring
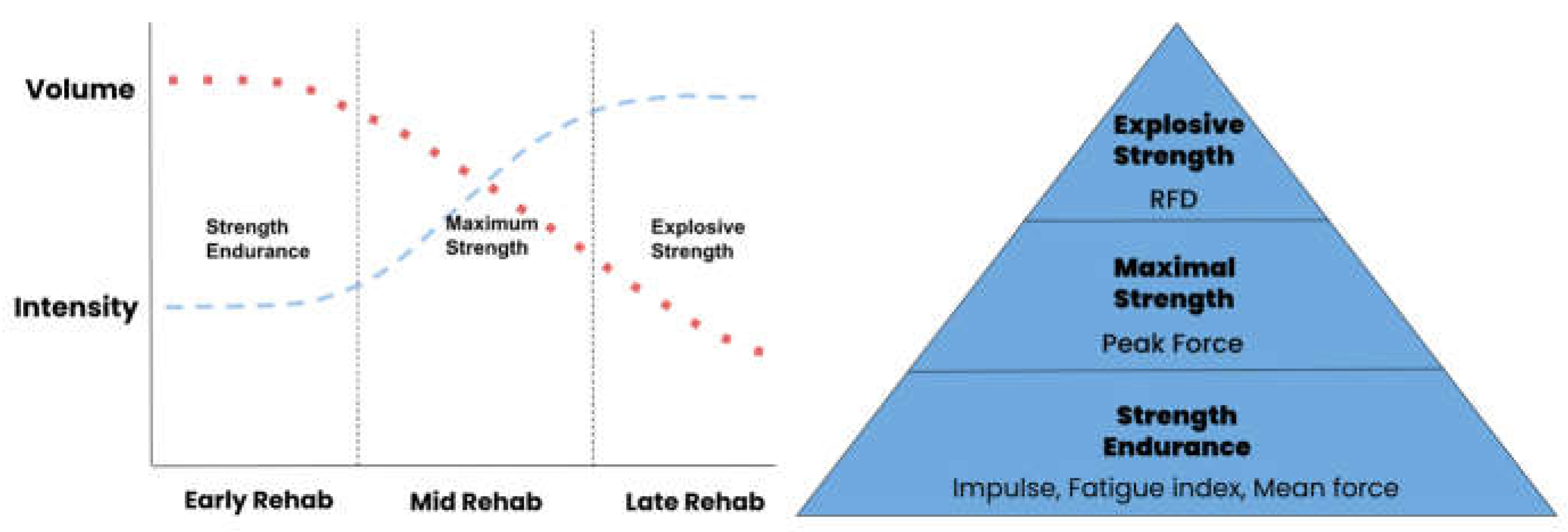
In terms of assessment and monitoring of strength or force capability, a simple model is provided that gives insight into three strength qualities that could be monitored and developed in the rehabilitation process (see
Figure 5) i.e., strength-force endurance/impulse or mean force, maximum strength/peak force, and explosive strength/rate of force development (RFD).
Strength endurance is the ability to sustain muscular force without fatiguing. This applies to both dynamic and static/isometric contractions. It provides the base of the training pyramid, and exercise prescription is typically high-volume and low-intensity muscular contractions. Max strength is defined as the ability of the neuromuscular system to produce a maximal voluntary force, which in isometric terms is referred to as an MVIC. With this type of training, there is an increase in intensity and a decrease in volume. Finally, explosive strength describes one’s ability to produce force in very short time periods, otherwise known as rate of force development (RFD) and sits at the top of the pyramid as the contractions are high intensity in nature. The progression of these strength qualities is diagrammatized in
Figure 5, where rehabilitation begins with low-intensity muscular work incorporating higher volumes. At the other end of the progression is the training of RFD which is typified by high intensity (explosive) – low volume type of muscular contractions i.e., late-stage rehab.
Implicit in the systematic progression of these strength qualities is the ability to assess and monitor changes in their status. Strain gauge technology can not only provide a means of quantifying isometric overload, but also provide the practitioner with data about changes in these strength qualities (enhanced diagnostics).
1.2.1. Strain Gauge Assessment of Strength Endurance (Impulse)
The various strength qualities have an equivalent force measure that can be determined from the force-time data provided by the SG software. Working with injured clients/athletes, it is also possible to calculate the degree of asymmetry or strength deficits between the injured and non-injured limbs.
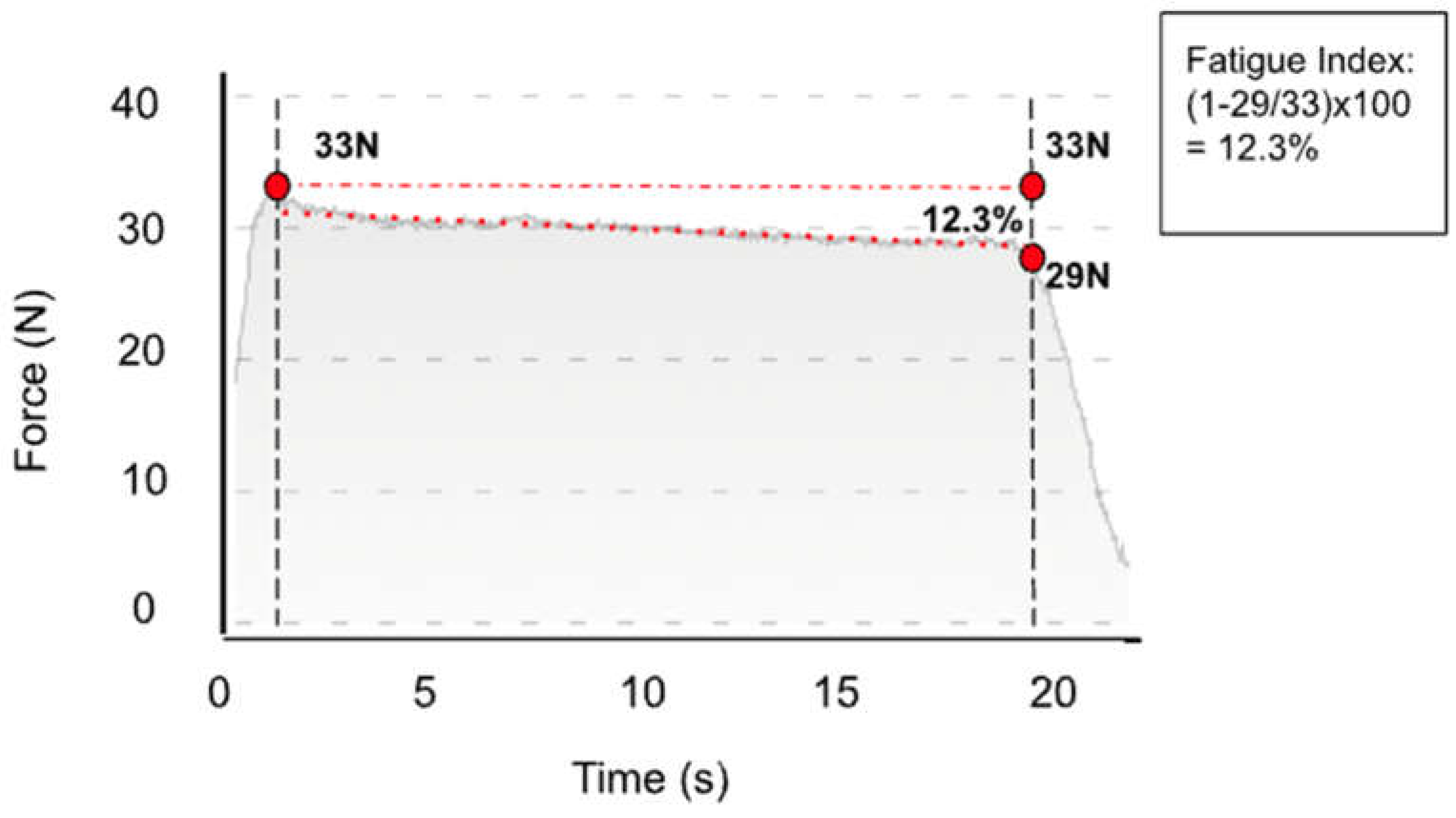
The strain gauge can be used in three ways to monitor changes in the strength endurance of clients. First, the change in initial force production can be measured and compared to the final force output via a fatigue index (FI = Final/Initial x 100) for isometric contractions, an example of which is shown in
Figure 6. The intention is to reduce the level of fatigue over time by increasing strength endurance. Strength endurance is measured over multiple repetitions (e.g., > 20) or over longer time periods (e.g. 20-30 s) with moderate resistance while maintaining a consistent force.
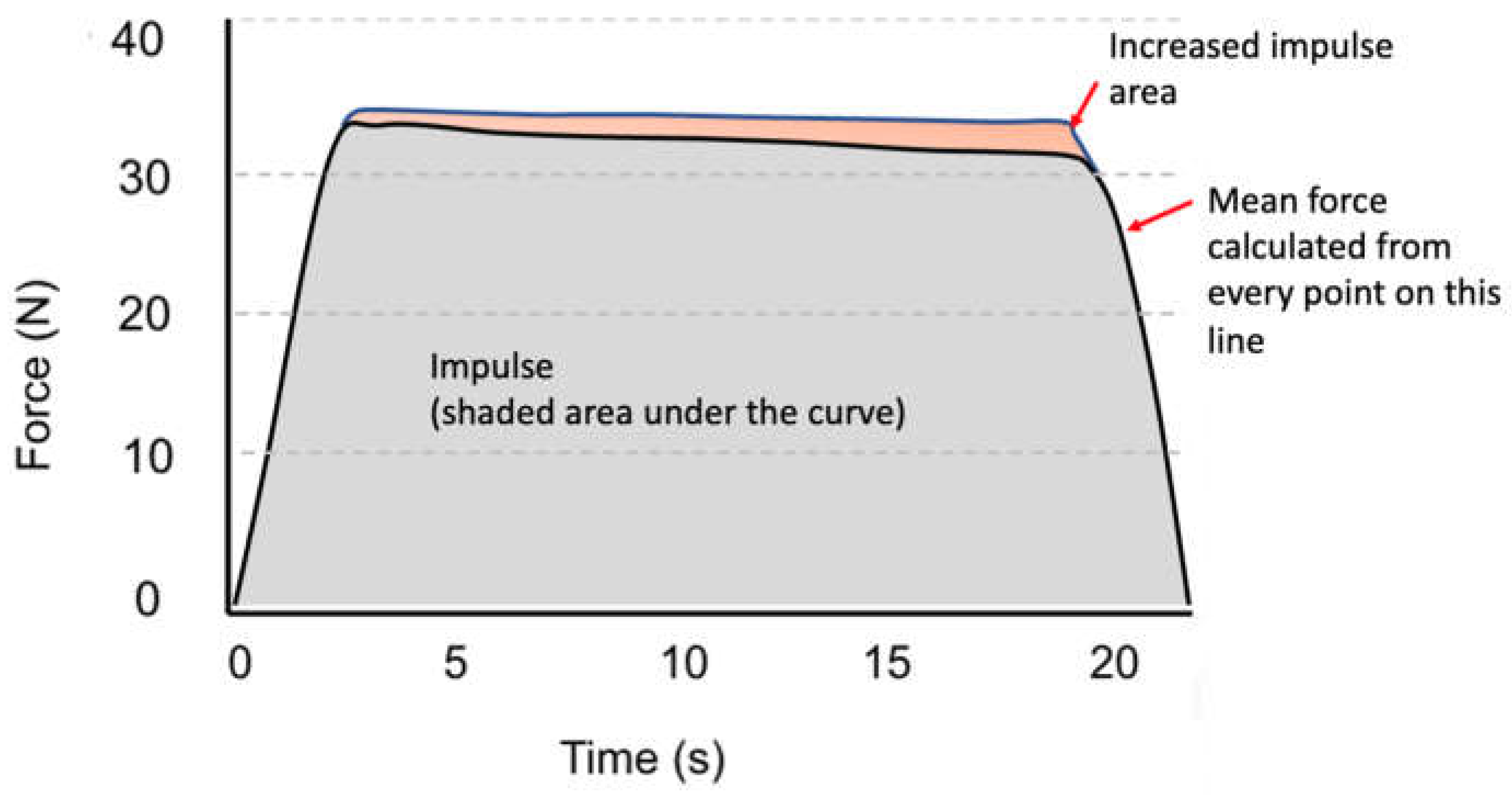
Two other methods to assess and monitor changes in strength endurance involve comparing the mean force and impulse between limbs and testing occasions (see
Figure 7). The mean force is simply the averaged force over the entire signal. Impulse is a measure of the magnitude of the force applied and the time over which it acts and is calculated as the area under the force-time graph. Increases in mean force or impulse over the same time period mean that the client/athlete is applying a greater overall force i.e., force endurance. However, it needs to be ensured that the SG device can quantify such measures to use such diagnostics. The instructions for assessing strength endurance should involve verbal cues such as, “produce as much force as you can for as long as you can.”
1.2.2. Strain Gauge Assessment of Maximal Strength (Peak Force)
The strain gauge can be used to assess and monitor improvements in maximal strength by comparing peak force values between interventions. The peak force can be measured during an isometric or dynamic contraction as shown in
Figure 8. It needs to be ensured that the client/athlete uses a ramped (steadily increasing) contraction over 5-6 seconds to attain this measurement. Also, peak force can be normalized to body mass i.e., Peak force/body mass = N/kg. This allows the comparison of maximal strength between clients/athletes/sexes and accounts for any changes in body mass between testing occasions. Instructions for assessing maximum strength could be, “produce the greatest amount of force possible” or “push or pull as hard as you can.”
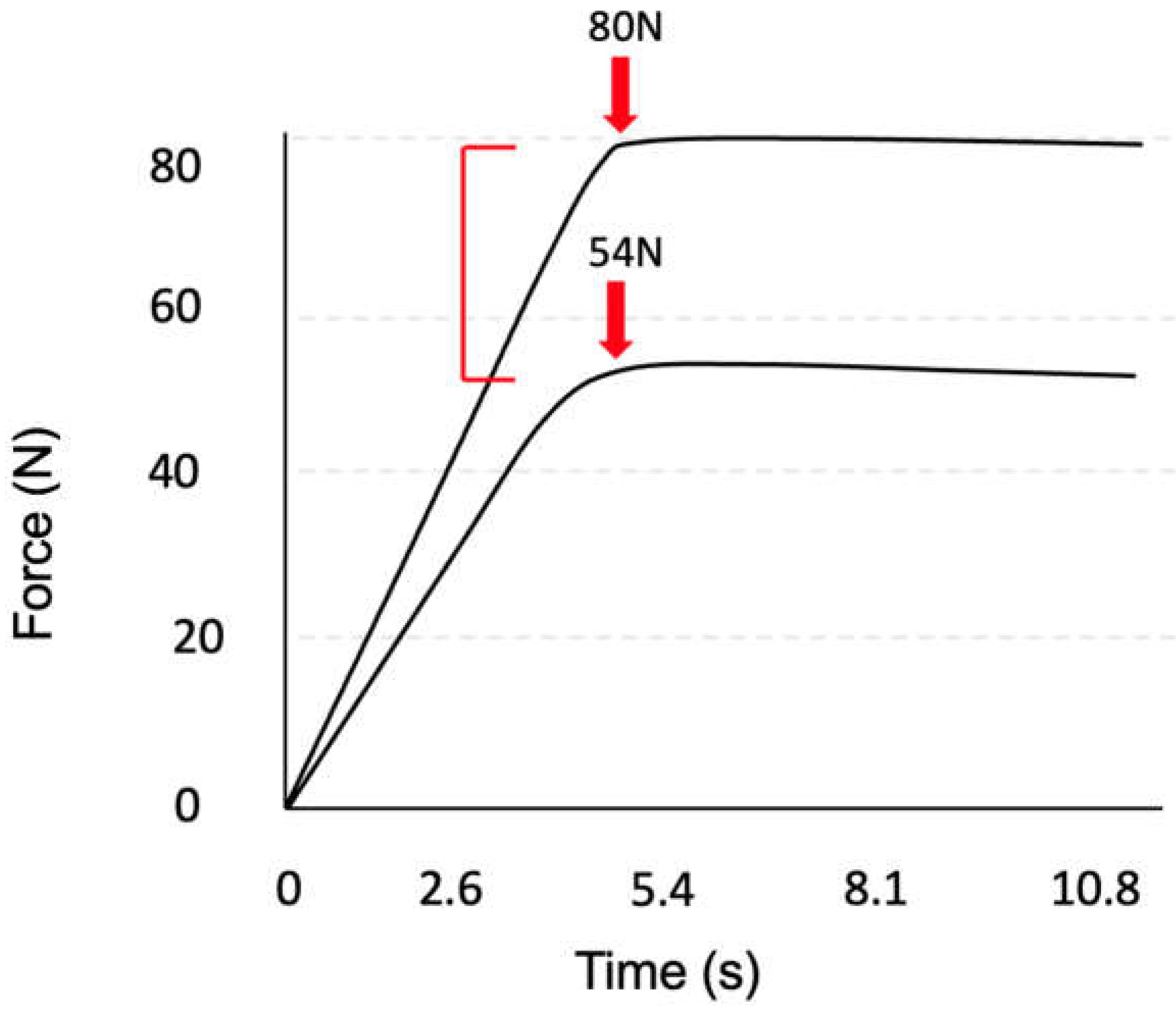
1.2.3. Strain Gauge Assessment of Explosive Strength (RFD)
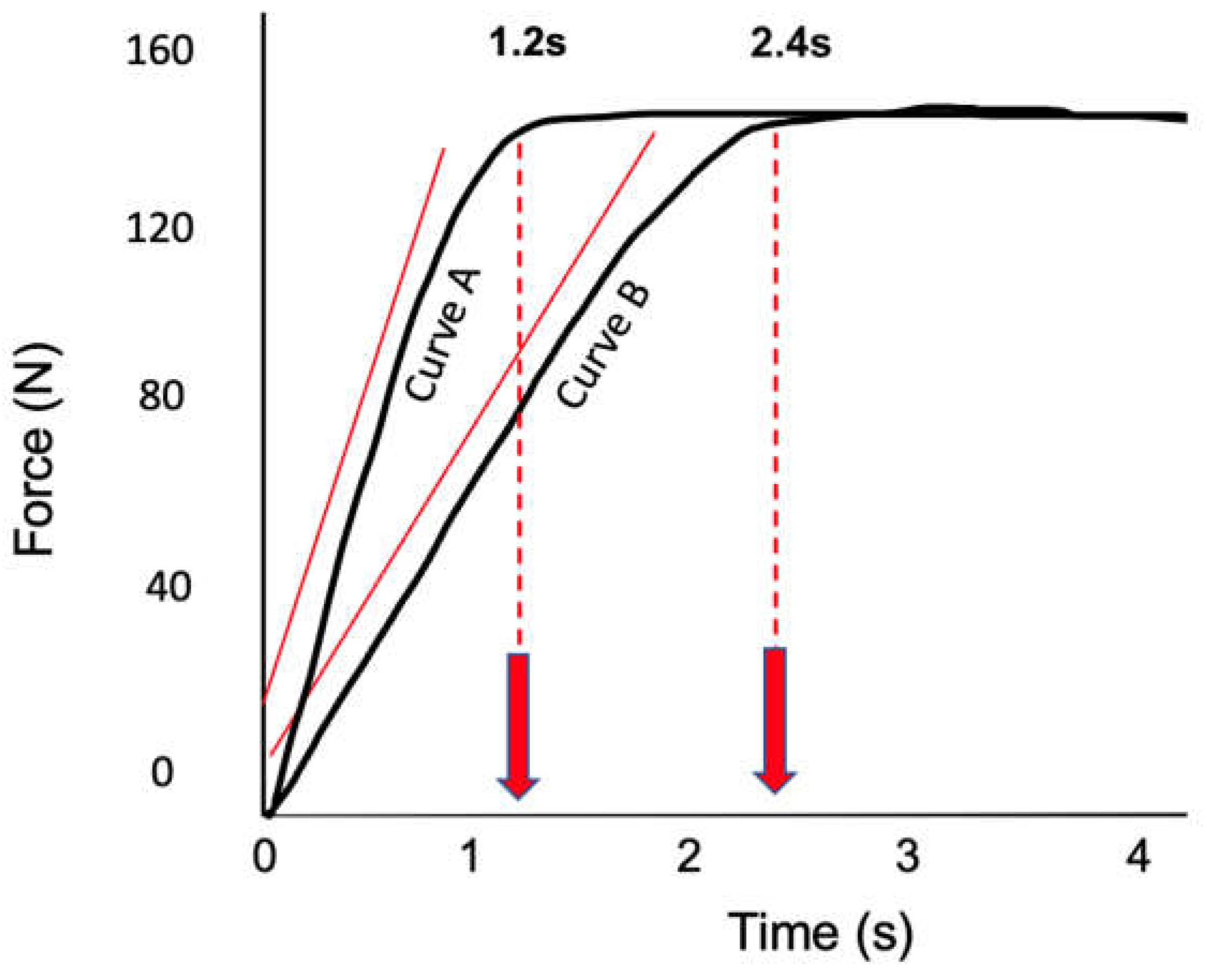
The strain gauge can be used to assess explosive strength via the calculation of RFD. It can be read on the graph where an isometric contraction RFD is calculated from the slope of the force-time curve [
17,
18]. However, there are many ways to calculate RFD, from taking the time from the onset of the contraction to the peak force to finding the peak RFD over the entire force-time signal. In
Figure 9 you can observe two curves that have the same peak forces, however, the maximum force in curve A occurs early and therefore this curve has a higher RFD as denoted by the slope of the red line as compared to curve B.
The instructions for assessing explosive strength could be to focus on applying force by, “pulling or pushing as fast and as hard as you can, to generate maximum force in the shortest time possible.”
1.3. Strain Gauge Integration for Exercise Prescription and Recovery
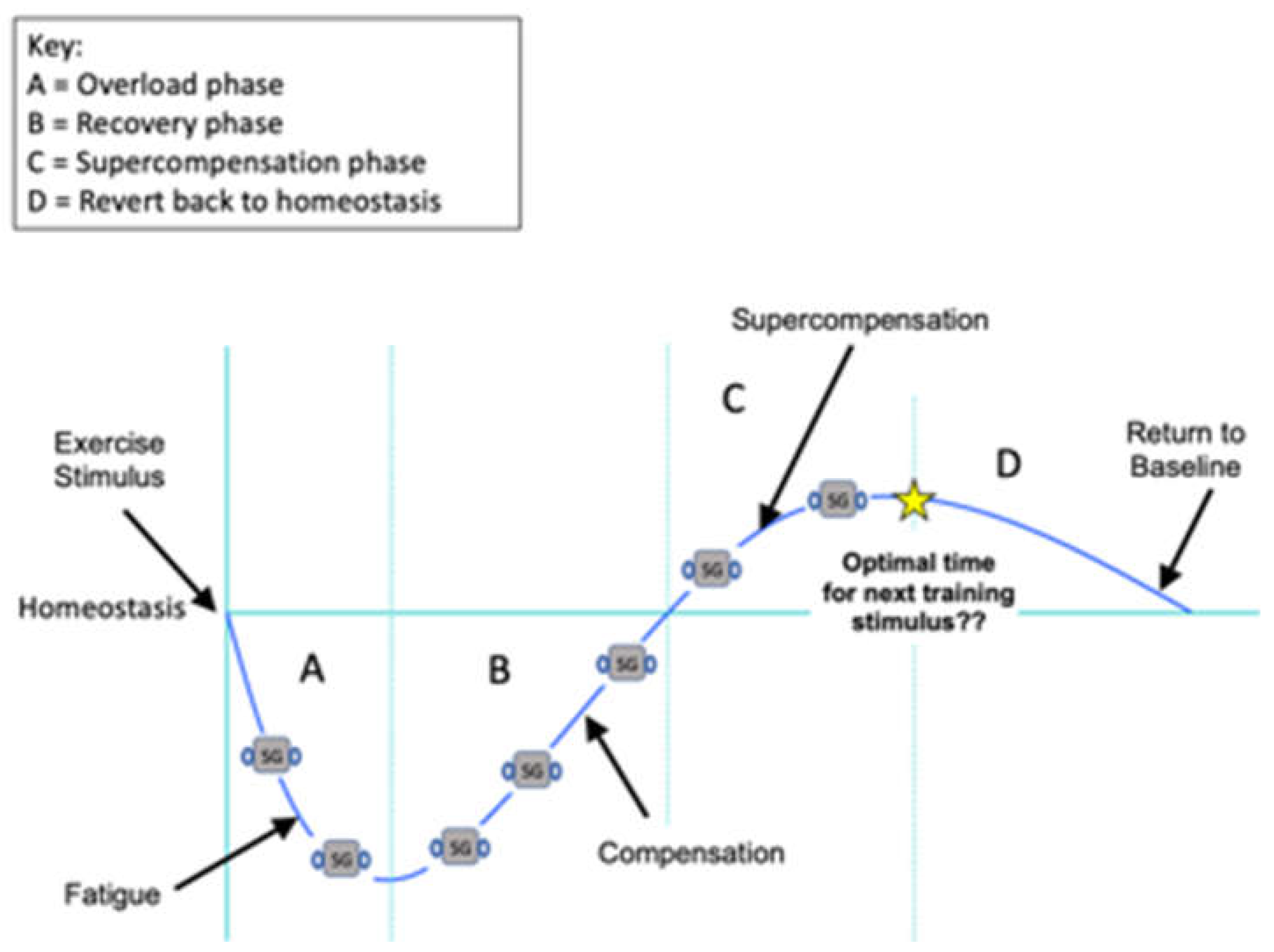
The general adaptation syndrome (GAS) describes how the body requires stress to allow for adaptation [
19]. As can be seen in the diagram (
Figure 10) when the muscles are overloaded such as with isometric training, they experience fatigue and a loss in force capability. When the exercise stimulus ceases, the muscles begin the recovery process and can recover, whereby they become stronger than the previous baseline status i.e., super-compensation. If another isometric exercise bout is not prescribed in a timely fashion, then the strength/force capability will revert to baseline or homeostasis. Alternatively, if isometric training is prescribed during the recovery compensation phase when the client/athlete hasn’t adequately recovered then there is a possibility of cumulative fatigue, compromised adaptation, and potential overtraining and injury.
The general adaptation syndrome highlights the importance of knowing when and how an applied workload has significant effects on adaptation. Integrating load cell technology throughout this process can lead to better analysis and therefore timing of training for better adaptation. For example, understanding the mechanical stress (force-length) that you are prescribing during isometric training will help understand the magnitude of the overload and fatigue and help avoid excessive overloading or underloading. Also, it provides baseline data for you to progress on ensuing occasions. During the compensation and super-compensation phases you can use the load cell to monitor fatigue and recovery status, and possibly distinguish when the client/athlete is ready for another exercise bout i.e., whether or not the individual is still fatigued and underperforming and needs more rest. In short, the strain gauge can be used to identify the optimal time for the next training stimulus and therefore could assist in more effective knee rehabilitation.
2. Exercises and Progressions
In the following section, an exemplar will be given of how the strain gauge can be integrated into the rehab of a specific pathology, in this case, osteoarthritis of the knee. First, a selection of training studies have been reviewed with the intent of identifying the isometric exercises that have been utilized in the rehabilitation of knee osteoarthritis. The exercises and equipment prescribed as well as the number of sessions, duration, repetitions, intensity, and methods of quantification are detailed. Thereafter examples of strain gauge integration are given.
Author/Study
Exercise/Equipment |
Loading Parameters |
Yadav et al., 2017
Ankle plantarflexion Ankle dorsiflexion Knee flexion Knee extension Hip flexion Hip extension TheraBand equipment
|
3x per week for 4 weeks 30 mins duration 1 set of 8 repetitions in 1st and 2nd week 3 sets of 12 repetitions in 3rd and 4th week. No intensity mentioned No quantification mentioned |
| Abdel-aziem et al., 2018
|
3x per week for 4 weeks Ex 1 - 5sec hold, 20 reps Ex 2 - 6sec hold, 3x 10 reps No intensity mentioned No quantification mentioned |
| Kilinc et al., 2020
|
|
| Onwunzo et al., 2021
|
3x per week for 6 weeks 50 min duration 1st set performed five times a day, with a slow count of one to five in the first three weeks 2nd set performed five times a day, with a slow count of one to five in the fourth to sixth week No intensity mentioned No quantification mentioned |
Naqi et al., 2021
Isometric quadriceps Towel
|
|
Rosa et al., 2012
Standing with the leg extended, the thigh is held in a contraction (1) Isometric quad contraction in full knee extension (2) Standing with the hip in abduction and the knee in flexion, with the contralateral leg in a neutral position (3) Standing exercises were conducted for the toes, inward and then outward for 5 s (4)
|
Every third day for 8 weeks (1) Standing with the leg extended, 10 sets of 10 contractions and relaxations of the thigh with a duration of 5 s each were carried out; there within 45 s of rest was allowed between each set. (2) 5 s hold followed by relaxation, repeated 10 times and then on the opposite leg; between each set there was a time for a rest of 45 s. (3) 10 repetitions with rest between sets; this was repeated with the opposite leg. (4) 5 s and repeated 10 times No intensity mentioned No quantification mentioned |
Anwer et al., 2014
|
5x per week for 5 weeks 10 repetitions 1 set of all exercises was performed twice a day for the 1st week. Progressed to 2 sets twice a day until the 3rd week and 3 sets twice a day until the 5th week. (1) 5 s hold (2) lift the leg up to 10 cm above the plinth, hold for 10 s (3) 5 s hold No intensity mentioned No quantification mentioned |
| Saleki et al., 2013
|
|
Topp et al., 2002
0° of dorsi- and plantarflexion 10° of knee flexion when performing knee flexion and extension 10° of hip flexion and 10° of hip extension Maximum resistance Thera-Band elastic bands
|
3x per week for 16 weeks Weeks 1 and 2, each subject performed 1 set of 8 repetitions while producing mild or sub-maximum muscle tension during the exercise with a 3-5 s hold at each joint angle After 2 weeks, they increased to maximum muscle tension for 3 to 5 s Subjects increased the number of repetitions and/or sets of repetitions every week in a scheduled progression of training outlined in their exercise booklets. Progression of training continued until weeks 9 to 16 each subject performed 3 sets of 12 repetitions of each exercise with a 2 min rest between sets (approximately 50 min). |
Hasan. S (2015)
|
5 days per week for 3 weeks (1) 3 sets x 10 reps each side (2) 3 sets x 10 reps each side Maximal contraction No quantification mentioned |
Rutherford et al., 2011
(1) knee extension at 45° of knee flexion (KE45) in sitting (2) knee extension at 15° of knee flexion (KE15) in supine (3) knee extension–hip flexion at 45° of knee flexion and 90° of hip flexion (KEHF) in sitting (4) knee flexion at 55° of knee flexion (KF55) in sitting (5) knee flexion at 15° of knee flexion (KF15) in supine (6) knee flexion at 55° of knee flexion (prone KF55) in prone (7) sitting plantarflexion with the ankle in neutral (8) standing unilateral plantarflexion.
|
One-off test Two sets of three-second maximal isometric contractions were completed for each exercise Participants were instructed to provide maximal efforts on each trial A minimum 60 s rest period separated each contraction |
Huang et al., 2017
Straight leg raising 10 cm lift (1) Side lying straight leg lift 10 cm (2) Seated isometric hip adduction with a ball (3) Ball
|
2sets of each exercise performed twice per day 3months duration (1) 10 reps of 10 s hold, 2 s rest (2) 10 reps of 10 s hold, 2 rest (3) 20 reps of 10 s hold, 2 s rest No intensity mentioned No quantification mentioned |
| Tok et al., 2011
|
5 days per week for 3 weeks 20 min duration 10 s contraction and 20 s rest in between No intensity mentioned No quantification mentioned |
| Choi et al., 2015
|
|
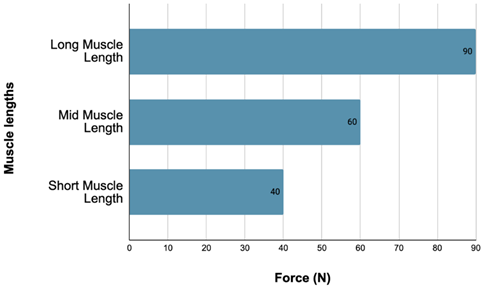
Prone Knee Flexion
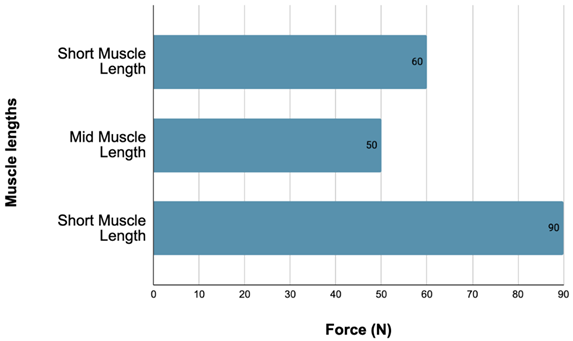
| Muscle length |
Long muscle length
(∼10 degrees) |
Mid muscle length
(45 degrees) |
Short muscle length
(90 degrees) |
| Image |
 |
 |
 |
Force production at long, mid, and short muscle lengths during knee flexion.
|
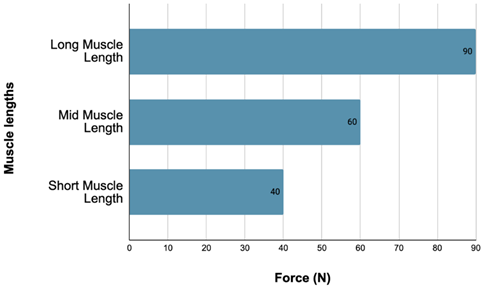 |
| Description/standardisation: |
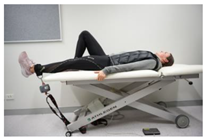
Patients lie on stomach with legs extended. Ankle strap is attached to the ankle which is flexed. The knee is then bent to each muscle length either; long (LML) (90 degrees), mid (MML) (45 degrees) or short (SML) (10 degree approx.). Patient then holds leg at this length for a given time to produce force readings like those shown in the figure. |
The specifics of the studies (n=14) reviewed are described in Table 1. The isometric quadriceps exercise was prescribed in eight studies, followed by knee extension/flexion at different joint angles in six studies, and the straight leg raise was used in four studies. All these exercises focused on quadriceps strengthening, which has been noted to improve knee osteoarthritis pain and function, as well as protecting against knee joint damage and progression of existing osteoarthritis [
20]. For example, Anwer and Alghadir [
12] stated ‘isometric quadriceps’ exercise has been proven effective, ‘in increasing the range of motion, leading to good function and a decrease in pain in patients diagnosed with osteoarthritis of the knee’ (pg. 747). They also acknowledged similarly the use of the isometric ‘straight leg raise’ for the same purpose, which was used in four of the studies above. The use of knee flexion also targets the quadriceps muscles, one study reporting that even isolated knee extension and flexion exercise can induce large improvements in strength, particularly in the more painful knee joint [
21]. Hence why these three exercises are reoccurring within the studies.
The loading parameters for the different exercises were not clearly stated in all the papers. For knee flexion/extension, three studies noted the use of maximal effort contractions, with only one specifying the progression from submaximal contractions in the first two weeks to maximal contractions after week two [
10,
22,
23]. For the isometric quadriceps exercise, two research groups used maximal contractions only [
24,
25]. There were no loading parameters mentioned, however, from studies that included the straight leg raise. In terms of isometric contraction durations, 3 to 6 s holds were prescribed for the knee flexion/extension exercises. The number of repetitions prescribed ranged between 2 to 12 reps. The isometric quadriceps contraction durations ranged between 5 and 10 s and 5 to 20 repetition ranges. Similarly, the isometric leg raise contraction durations ranged between 5 and 10 s and 5 to 10 repetition ranges.
Of the eight studies that used the isometric quadriceps exercise only three reported their rest intervals, which were 10-20 s after each contraction [
25,
26] and 45 s rest after each set [
27]. For the knee flexion/extension exercise only one research group reported rests of at least 60 s between contractions [
23], and another noting 120 s rest periods between sets [
22]. With regards to the straight leg raise only one study reported a rest period of 2 s between repetitions. In summary, the rest periods between repetitions and sets varied a great deal between studies.
The following table outlines how strain gauge technology may be integrated into the isometric exercises to provide quantitative feedback on the loading of a patient. It needs to be noted that this process could be implemented with any pathology, however, in this case knee osteoarthritis is used as an example.
Seated knee extension
| Muscle length |
Long muscle length |
Mid muscle length |
Short muscle length |
Picture
Image |
 |
 |
 |
| Description |
Patients sit upright with knee on edge of plinth/seat. A towel is rolled up and positioned under the knee and a strap is attached around the ankle which remains in a flexed position. The strap is adjusted for each muscle length and the patient contracts the quadriceps for a given time with foot flexed and knee pressing down into towel. |
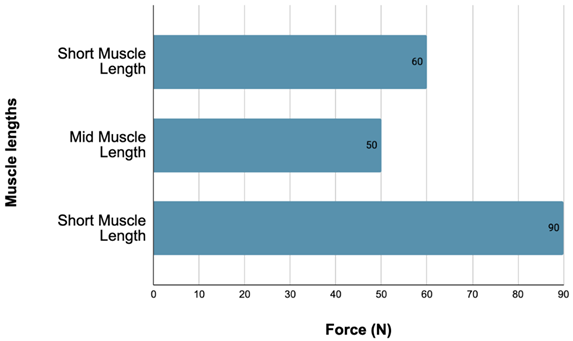
Supine straight leg raise
Picture
Image |
 |
 |
 |
| Force production at long, mid, and short muscle lengths during a lying straight leg raise. |
 |
| Description |
Patients lay in a supine position on back. They bend both knees with feet flat on bench. The leg that the ankle strap is attached to is then lifted into the air to each strap height according to the different muscle lengths/range of motions. They then hold the contraction during the lifting phase for the given period of time. |
3. Conclusion
Isometric training is commonly prescribed in rehabilitation settings, or early in physical preparation plans as a means to increase neuromuscular, musculoskeletal, and proprioceptive function. It is thought that the aforementioned improvements will later transfer to dynamic performance once specific movement patterns are integrated into the physical preparation plan. However, isometric training in physiotherapeutic practice can be very qualitative in terms of monitoring, assessing, and exercise prescription. This article addressed the concerns of the American Physical Therapy Association, requesting a “call to arms” for the maturation of the physiotherapeutic profession, specifically citing evidence-based medicine as a priority. The integration of strain gauge technology in everyday practice is one such solution and provided the focus of this paper.
The integration of strain gauge technology allows the practitioner a better understanding of mechanotransduction, a process that is important in understanding the effects that certain mechanical variables have on cellular signaling and tissue remodeling. Ultimately it is mechanical variables like force, length, and velocity (zero velocity in the case of isometrics), that drive adaptation and optimize the repair and remodeling of injured tissue [
16]. Khan and Scott reported that mechanotransduction was not being taught as an important biological principle in physical therapy and medical programs, which they thought was a major failing of medical education. With the integration of strain gauge in practice, and consequently constant mapping of loading and monitoring of tissue and movement recovery, the fundamentals of mechanotransduction can be implemented, and as such a mechanotherapy approach can be taken to the healing of tendon, muscle, cartilage, and bone.
Finally, the strain gauge is a portable, affordable, and flexible device that can be used for assessment, monitoring, and exercise prescription across a multitude of pathologies. Knee osteoarthritis was used as an example in this article; however, the device and the many attachments allows the user to quantify the force output of many different movements and resistance types. With continued use by the physiotherapist, from objective examination to a rehab by-numbers approach to patient care, it is envisaged that the rehabilitation and return to activity pathway of the client will be better optimized.
4. Patents
The device listed in this article has been patented and is covered under application number 16/520,089
Author Contributions
For research articles with several authors, a short paragraph specifying their individual contributions must be provided. The following statements should be used “Conceptualization, John Cronin; software, Mark Pryer.; validation, Jessica Lane and Mark Pryer; formal analysis, Jessica Lane and John Cronin; investigation, Jessica Lane and John Cronin; writing—original draft preparation, Jessica Lane and John Cronin; writing and editing—Michael Rumpf; supervision, John Cronin and Michael Rump; project administration, Mark Pryer. All authors have read and agreed to the published version of the manuscript.
Funding
No funding was received for the writing of this narrative review.
Institutional Review Board Statement
Not applicable as it was a narrative review.
Informed Consent Statement
Not applicable as it was a narrative review.
Data Availability Statement
Not applicable as it was a narrative review.
Conflicts of Interest
The development of the technology was funded by TexKiwi. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; or in the writing of the manuscript. John Cronin received a share allocation in TexKiwi.
References
- Cameron, M., Monroe, L. (2007). Physical rehabilitation: Evidence-based examination, evaluation, and intervention. Elsevier Science Health Science Division. [CrossRef]
- Oranchuk, D. J., Storey, A. G., Nelson, A. R., & Cronin, J. B. (2019). Isometric training and long-term adaptations: Effects of muscle length, intensity, and intent: A systematic review. Scandinavian Journal of Medicine and Science in Sports, 29(4), 484–503. [CrossRef]
- Moeskops, S., Oliver, J. L., Read, P. J., Cronin, J. B., Myer, G. D., Haff, G. G., & Lloyd, R. S. (2018). Within- and between-session reliability of the isometric midthigh pull in young female athletes. Journal of Strength and Conditioning Research, 32(7), 1892–1901. [CrossRef]
- Wang, R., Hoffman, J. R., Tanigawa, S., Miramonti, A. A., La Monica, M. B., Beyer, K. S., Church, D. D., Fukuda, D. H., and Stout, J. R. (2016). Isometric mid-thigh pull correlates with strength, sprint, and agility performance in collegiate rugby union players. Journal of Strength and Conditioning Research 30(11): 3051-3056. https://www.ncbi.nlm.nih.gov/pubmed/26982977.
- Tsoukos, A., Bogdanis, G. C., Terzis, G., & Veligekas, P. (2016). Acute improvement of vertical jump performance after isometric squats depends on knee angle and vertical jumping ability. Journal of Strength and Conditioning Research, 30(8), 2250-2257. [CrossRef]
- Altan, E., Seide, S., Bayram, I., Gizzi, L., Ertan, H., & Röhrle, O. (2020). A systematic review and meta-analysis on the longitudinal effects of unilateral knee extension exercise on muscle strength. Frontiers in Sports and Active Living, 2, 1-22, 518148. [CrossRef]
- Rio, E., Kidgell, D., Purdam, C., Gaida, J., Moseley, G. L., Pearce, A. J., & Cook, J. (2015). Isometric exercise induces analgesia and reduces inhibition in patellar tendinopathy. British Journal of Sports Medicine, 49(19), 1277-1283. [CrossRef]
- Yadav, M., & Attrey, P. (2017). Effect of dynamic versus isometric resistance exercise on pain and functional ability in elderly patients with osteoarthritis of knee. Indian Journal of Physiotherapy & Occupational Therapy, 11(2): 30-34.
- Abdel-Aziem, A. A., Soliman, E. S., Mosaad, D. M., & Draz, A. H. (2018). Effect of a physiotherapy rehabilitation program on knee osteoarthritis in patients with different pain intensities. Journal of Physical Therapy Science, 30(2), 307-312. [CrossRef]
- Kilinc, S., Kabayel, Derya D., & Ozdemir, F. (2020). Comparison of the effectiveness of isokinetic exercise vs isometric exercise performed at different angles in patients with knee osteoarthritis. Isokinetics & Exercise Science, 28(1), 35-47. [CrossRef]
- Kangeswari, P., Murali, K., & Arulappan, J. (2021). Effectiveness of isometric exercise and counselling on level of pain among patients with knee osteoarthritis. SAGE Open Nursing, 7, 2377-9608. [CrossRef]
- Anwer, S., & Alghadir, A. (2014). Effect of isometric quadriceps exercise on muscle strength, pain, and function in patients with knee osteoarthritis: a randomized controlled study. Journal of Physical Therapy Science, 26(5), 745-748. [CrossRef]
- Van Ark, M., Cook, J. L., Docking, S. I., Zwerver, J., Gaida, J. E., van den Akker-Scheek, I., & Rio, E. (2016). Do isometric and isotonic exercise programs reduce pain in athletes with patellar tendinopathy in-season? A randomised clinical trial. Journal of Science and Medicine in Sport, 19(9), 702–706. [CrossRef]
- Rio, E., Van Ark, M., Docking, S., Moseley, G. L., Kidgell, D., Gaida, J. E., Van Den Akker-Scheek, I., Zwerver, J., & Cook, J. (2017). Isometric contractions are more analgesic than isotonic contractions for patellar tendon pain: an in-season randomized clinical trial. Clinical Journal of Sport Medicine, 27(3), 253-259. [CrossRef]
- Pearson, S. J., Stadler, S., Menz, H., Morrissey, D., Scott, I., Munteanu, S., & Malliaras, P. (2020). Immediate and short-term effects of short-and long-duration isometric contractions in patellar tendinopathy. Clinical Journal of Sport Medicine, 30(4), 335-340. [CrossRef]
- Khan, K. M., & Scott, A. (2009). Mechanotherapy: how physical therapists’ prescription of exercise promotes tissue repair. British Journal of Sports Medicine, 43(4), 247-252. [CrossRef]
- Kawamori, N., Rossi, S. J., Justice, B. D., Haff, E. E., Pistilli, E. E., O’Bryant, H. S., Stone, M. H., & Haff, G. G. (2006). Peak force and rate of force development during isometric and dynamic mid-thigh clean pulls performed at various intensities. Journal of Strength and Conditioning Research, 20(3), 483-491. [CrossRef]
- Tillin, N. A., Pain, M. T. G., & Folland, J. (2013). Explosive force production during isometric squats correlates with athletic performance in rugby union players. Journal of Sports Sciences, 31(1), 66–76. [CrossRef]
- Selye, H. (1950). Stress and the general adaptation syndrome. British Medical Journal, 1(4667), 1383–1392. [CrossRef]
- Slemenda, C., Brandt, K. D., Heilman, D. K., Mazzuca, S., Braunstein, E. M., Katz, B. P., et al. (1997). Quadriceps weakness and osteoarthritis of the knee. Annals of Internal Medicine. 1997; 127:97–104. [CrossRef]
- Vincent, K. R., & Vincent, H. K. (2012). Resistance Exercise for Knee Osteoarthritis. Physical Medicine & Rehabilitation, 4, S45–S52. [CrossRef]
- Topp, R., Woolley, S., Hornyak III, J., Khuder, S., & Kahaleh, B. (2002). The effect of dynamic versus isometric resistance training on pain and functioning among adults with osteoarthritis of the knee. Archives of Physical Medicine and Rehabilitation, 83(9), 1187-1195. [CrossRef]
- Rutherford, D. J., Hubley-Kozey, C. L., & Stanish, W. D. (2011). Maximal voluntary isometric contraction exercises: A methodological investigation in moderate knee osteoarthritis. Journal of Electromyography and Kinesiology, 21(1), 154–160. [CrossRef]
- Hasan, S. (2015). Quadriceps femoris strength training: effect of neuromuscular electrical stimulation vs isometric exercise in osteoarthritis of the knee. Indian Journal of Physiotherapy & Occupational Therapy, 9(3), 129-134. [CrossRef]
- Choi, Y. L., Kim, B. K., Hwang, Y. P., Moon, O. K., & Choi, W. S. (2015). Effects of isometric exercise using biofeedback on maximum voluntary isometric contraction, pain, and muscle thickness in patients with knee osteoarthritis. Journal of Physical Therapy Science, 27(1), 149-153. [CrossRef]
- Tok, F., Aydemir, K., Peker, F., Safaz, İ., Taşkaynatan, M. A., & Özgül, A. (2011). The effects of electrical stimulation combined with continuous passive motion versus isometric exercise on symptoms, functional capacity, quality of life and balance in knee osteoarthritis: a randomized clinical trial. Rheumatology international, 31(2), 177-181. [CrossRef]
- Rosa, U. H., Tlapanco, J. V., Maya, C. L., Ríos, E. V., González, L. M., Daza, E. R. V., & Rodríguez, L. G. (2012). Comparison of the effectiveness of isokinetic vs isometric therapeutic exercise in patients with osteoarthritis of the knee. Reumatología Clínica (English Edition), 8(1), 10-14. [CrossRef]
- Duchateau, J., & Baudry, S. (2014). Maximal discharge rate of motor units determines the maximal rate of force development during ballistic contractions in humans. Frontiers in Human Neuroscience, 8, 234, 1662-5161. [CrossRef]
- FUTEK. (2022). Advanced Sensor Technology. Futek.com.
- Huang, L., Guo, B., Xu, F., & Zhao, J. (2018). Effects of quadriceps functional exercise with isometric contraction in the treatment of knee osteoarthritis. International Journal of Rheumatic Diseases, 21(5), 952-959. [CrossRef]
- Järvinen, T. A., Järvinen, T. L., Kääriäinen, M., Äärimaa, V., Vaittinen, S., Kalimo, H., & Järvinen, M. (2007, April). Muscle injuries: optimising recovery. Best Practice & Research Clinical Rheumatology, 21(2), 317–331. [CrossRef]
- Kojima, Y., Fukusaki, C., & Ishii, N. (2020). Effects of hyperoxia on dynamic muscular endurance are associated with individual whole-body endurance capacity. PLoS One, 15(4), e0231643. [CrossRef]
- Mujika, I. (2017). Quantification of training and competition loads in endurance sports: Methods and applications. International Journal of Sports Physiology and Performance, 12(s2), S2-9S2-17. [CrossRef]
- Naqi, S., Ali, A. A., Bugti, M., Sheikh, N., Bugti, M. K., Chandio, S., Hussain, A., MR, M. I., & Ahmad, T. (2021). Comparison of the effectiveness of proprioceptive and isometric exercises in patients of knee osteoarthtitis: A randomized control trial. Journal of Novel Physiotherapy and Physical Rehabilitation, 8(1), 014-019.
- Onwunzo, C. N., Igwe, S. E., Umunnah, J. O., Uchenwoke, C. I., & Ezugwu, U. A. (2021). Effects of isometric strengthening exercises on pain and disability among patients with knee osteoarthritis. Cureus, 13(10), pp. e18972. [CrossRef]
- Saleki, M., Ahadi, T., Razi, M., Raeisi, G. R., Forough, B., & Ali, M. K. (2013). Comparison of the effects of acupuncture and isometric exercises on symptoms of knee osteoarthritis. International Journal of Preventive Medicine, 4, Issue 13, Pp 73-77.
- Veugelers, K. R., Young, W. B., Fahrner, B., & Harvey, J. T. (2016). Different methods of training load quantification and their relationship to injury and illness in elite Australian football. Journal of Science and Medicine in Sport, 19(1), 24–28. [CrossRef]
- APT. (1999). Guide to Physical Therapist Practice. American Physical Therapy Association. Vol: 77.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).