Introduction
According to Eurostat, the EU experienced excess all-cause mortality in the first nine months of 2022, i.e., the mortality was higher than the average of the same months between 2016 and 2019, before COVID-19 (1). In this study, our primary aim is to investigate if the pattern—2022 nation-level monthly all-cause mortality relative to pre-pandemic numbers—can be linked to nation-level COVID-19 vaccination uptake by the end of the previous year, 2021.
Although research has indicated that COVID-19 vaccination has prevented SARS-CoV-2-related hospital admission and deaths (2-4), its preventive effect has waned (5). Also, COVID-19 vaccination has side effects (6-9), such as myocarditis and pericarditis (10, 11), and along with this knowledge, it is worth noting that a recent study falsified a suspected association between the two diagnoses and COVID-19 virus infection (12). Coining this information with research showing that vaccine side effects generally tend to be underreported (13), we ask if COVID-19 vaccination may be associated with long-term mortality. To study this potential link, we regress all-cause mortality in the first nine months of 2022 (relative to pre-pandemic levels) on vaccination uptake in 31 European countries by the end of 2021. The 31 countries are the EU member states, plus Norway, Iceland, Liechtenstein, and Switzerland. The estimates are weighted by each country’s population size by January 1, 2020. Also, we include an interaction term between vaccination uptake and the time that has passed since the beginning of 2022. Our motive is to assess if a potential link between vaccination uptake and all-cause mortality has changed over time. (To further illuminate the study’s topic, the Appendix illustrates the association between 2021 vaccination uptake and all-cause mortality the same year relative to pre-pandemic levels.)
In the following, we present the materials and methods in detail and report the empirical results. Then, we discuss the findings, address the study’s limitations, and suggest avenues for future research. When discussing the results and addressing study limitations, we particularly emphasize the issues of causal inference and ecological fallacy.
Materials and Methods
As a dependent variable, we applied data from Eurostat, which models the countries’ all-cause mortality each month divided by the average of the same month between 2016 and 2019 multiplied by 100 (1). Finally, the expression is subtracted by 100, which implies that positive values indicate excess mortality and negative values indicate sub-mortality. Vaccination uptake is the percentage of the total population in each country that has received a “primary course” by week 52, 2021. We gathered the data from the COVID-19 vaccine tracker by the European Centre for Disease Prevention and Control (14), except for Switzerland, where we used Our World in Data as a source (15) (for details on countries’ vaccination uptake and size in population, please see
Table 1). Each month in 2022 is modeled straightforwardly, where January takes the value of one, February two, etc.
We control for pre-COVID life expectancy in 2019 using Eurostat data (16) as it is a proxy for health status in each country (17). Lastly, we control for average all-cause mortality in 2020 and 2021 divided by the average between 2016 and 2019 (18). Our motive for the control variable is that relatively high mortality in 2020 and 2021 may induce relatively low mortality in 2022 and vice versa. On the other hand, relatively high mortality in 2020 and 2021 may indicate a deteriorating health status not captured by pre-COVID life expectancy. For consistency, we multiply the measure by 100.
Below, we first present descriptive statistics and correlations. Next, in our statistical models, we apply linear multilevel mixed-effects random intercept regression analyses where monthly observations are nested at the country level (for details, please see, e.g., 19, 20). As noted, observations are weighted according to the population size by January 1, 2020, and we carry out all analyses in Stata 17.0 (21).
Results
Table 2 reports minimum values, maximum values, descriptive statistics, and correlations. We observe strong correlations between vaccination uptake and the control variables average 2020-2021 mortality and life expectancy, which may cause problems with multicollinearity (for an informative discussion, please see e.g., 22). Later, we explain how we deal with the issue.
Model 1,
Table 3, shows that vaccination uptake has a non-significant direct association with the dependent variable, but the significant monthly association indicates that the overall mortality tends to increase over time. The interaction between vaccination uptake and time passed in months since the beginning of 2022 (V*M) is strongly significant and implies that the mortality increases the higher the vaccination uptake. Specifically, it shows that a one percentage point increase in 2021 vaccination uptake is associated with an increase in 2022 monthly mortality by 0.105 percent (95% CI, 0.075-0.134).
We mean-center the variables to minimize potential multicollinearity problems [cf. 23], and the variance inflation factor (VIF) taking a value of one concerning the month variable and the interaction term shows that multicollinearity is not a problem. However, the VIF concerning the vaccination uptake taking a value of 5.17, may be problematic. To amend the issue, we omit the control variables in Model 2 and observe that all the VIFs are now low. Also, the remaining estimates and their error terms are not much altered.
As robustness checks, in Models 3 and 4, we add an interaction term between each control variable and the month variable at a time. We observe that statistical conclusions concerning the independent variables and their interaction term are unaltered. The only exception is vaccination uptake showing a borderline significant association with the dependent variable in Model 3. Model 5 replicates the first model except that it excluded July when a heat wave occurred. The overall increasing monthly association is now borderline significant, but the interaction term association remains robust. Finally, we carried out unreported analyses controlling for 2018 nation-level median age and 2019 per-capita GDP adjusted for purchasing power, respectively, as done in Models 3 and 4, but without altering any statistical conclusion (analyses are available upon request).
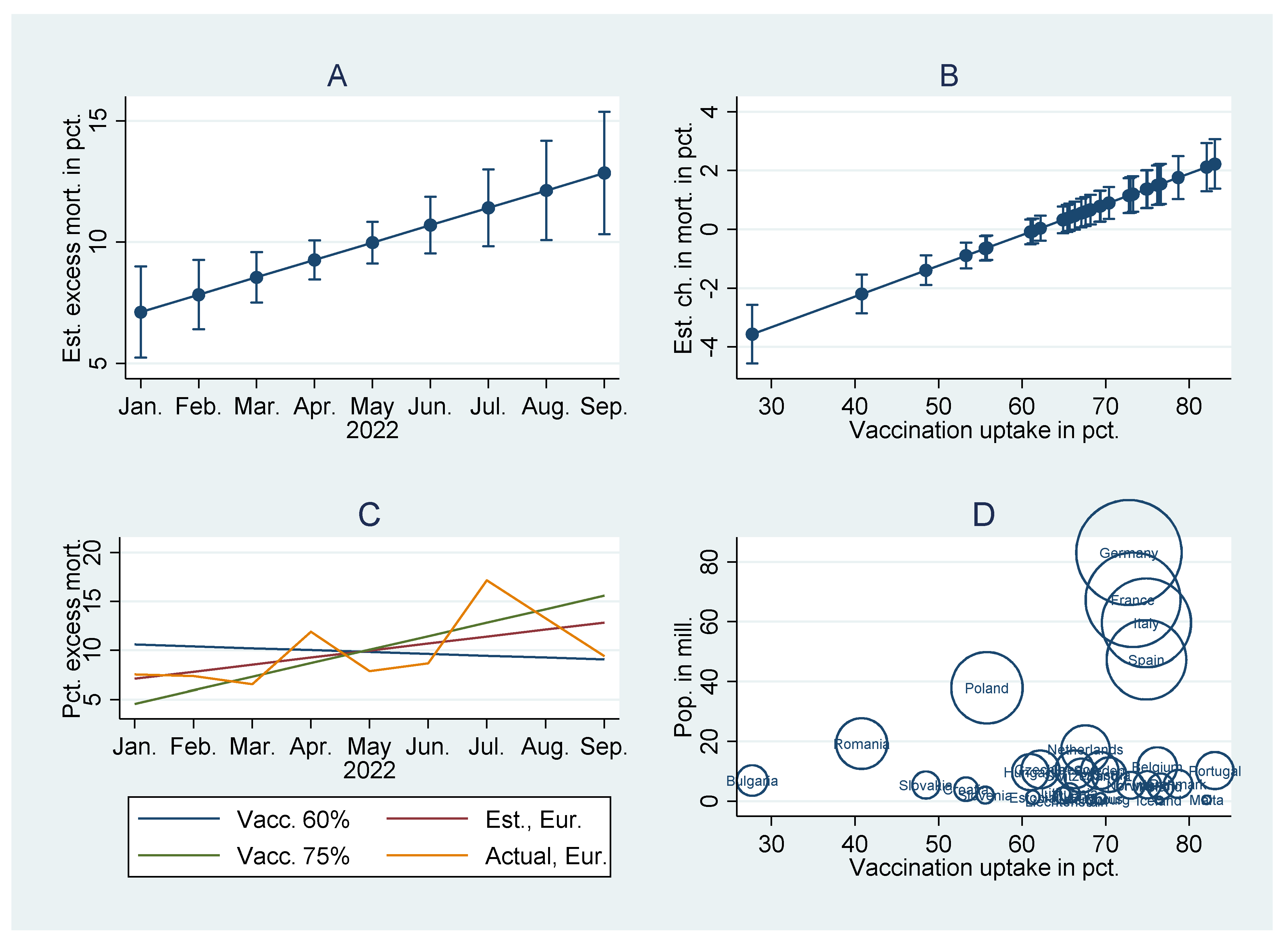
Figure 1A–C, based on Model 1,
Table 3, concludes the findings. It indicates increasing all-cause excess mortality (
Figure 1A), and more strikingly, the increase is higher the higher the national vaccination uptake (
Figure 1B). As noted, a one percentage point increase in 2021 vaccination uptake is associated with an increase in 2022 monthly mortality by 0.105 percent (95% CI, 0.075-0.134). In countries with relatively high vaccination uptakes, which include numerous of Europe’s states and the most populous (
Figure 1D, based on
Table 1), the result estimates a mortality increase (
Figure 1C). In countries with relatively low vaccination uptakes, the result estimates a low or even negative mortality increase (
Figure 1C).
Discussion
This study shows that the all-cause mortality during the first nine months of 2022 in 31 European countries increased more the higher the 2021 vaccination uptake. The association is strongly significant (
Table 3), but to make causal inferences, it is further necessary to (1) rule out reverse causality and (2) account for alternative explanations (cf. John Stuart Mill cited in Cook and Campbell, 23, pp. 18-20). Below we discuss both issues. Also, we discuss our study in light of potential (3) ecological fallacy, which is a “failure in reasoning that arises when an inference is made about an individual based on aggregate data for a group” (24).
Concerning potential reverse causality (1), the timing of the independent and dependent variables is crucial. Relating the timing condition to our study, we find it unreasonable, actually logically impossible, that increasing monthly all-cause mortality in 2022 could have occurred before and hence caused vaccination uptake in the previous year, 2021. Accordingly, ceteris paribus it is more likely to assume that 2021 vaccination uptake will have caused monthly increases in 2022 mortality than the other way around.
Concerning alternative explanations (2), we controlled for average all-cause mortality in 2020 and 2021 divided by the average between 2016 and 2019. The all-cause mortality during 2020 and 2021 was relatively low in countries with relatively high vaccination uptakes (
Table 2), and had we not controlled for this issue, one could alternatively have argued for a so-called “bounce-back effect,” i.e., relatively low mortality at one period is followed by relatively high mortality later, and vice versa. E.g., the relatively high mortality in the first months of 2022 could have been due to relatively low mortality in the previous two years, but, as mentioned, we controlled for this issue. Moreover, we not only controlled for average 2020 and 2021 mortality relative to the average between 2016 and 2019, but we additionally included an interaction term between this variable and the month variable simultaneously with the interaction term between vaccination uptake and the month variable (
Table 3, Model 3). Despite this—in our opinion, conservative test—we still observed a significant association between 2021 vaccination uptake and the 2022 monthly increase in all-cause mortality. Nonetheless, future research should extend the time frame beyond 2022’s first nine months to assess whether the relatively high all-cause mortality persists in countries with high vaccination uptakes. If so, there is even more reason to assume that there is a genuine association between 2021 COVID-19 vaccination uptake and 2022 excess mortality. Secondly, we controlled for 2019 pre-COVID life expectancy. The variable correlated positively with vaccination uptake and negatively with the other control variable—average 2020 and 2021 mortality relative to the 2016-2019 average mortality (
Table 2). Accordingly, the inclusion of pre-COVID life expectancy as a control variable partakes to rule out other potential alternative explanations of our findings. Also, we included an interaction term between this variable and the month variable simultaneously with the interaction term between vaccination uptake and the month variable, but without altering any statistical conclusion (
Table 3, Model 4). Finally, we carried out unreported analyses controlling for 2018 nation-level median age and 2019 per-capita GDP adjusted for purchasing power, respectively, as done in Models 3 and 4 (
Table 3), but without altering any statistical conclusion (analyses are available upon request).
Concerning ecological fallacy (3), we are cautious about making individual-level inferences from our nation-level findings. In other words, we emphasize that our study shows a positive association between 2021 nation-level vaccination uptake and 2022 nation-level monthly increase in excess mortality while ruling out reverse causality and accounting for alternative explanations. Having said that, it may be worth discussing ecological fallacy in general and the plausibility of making individual-level inferences from our nation-level findings, which we do in the following paragraphs.
Firstly, we address the classical Robinson’s paradox (25). At a US state level, Robinson found that the illiteracy rate was lower the higher the foreign-born population rate, but at an individual level, foreign-borns had a higher probability of being illiterate than national-borns. An explanation of the paradox is that foreign-borns had a high proclivity to settle in states with high literacy rates, which illustrates a reverse causality. Returning to our study, we have argued that reverse causality is not a potential challenge to the results’ interpretation as the timing of the independent variable precedes the dependent variable.
Secondly, we address the Simpson’s paradox (26, 27), which could imply that individual-level vaccination was associated with a monthly decrease in the individual-level mortality probability despite a positive association between the nation-level vaccination uptake and increased monthly mortality. However, Simpson’s paradox hinges on the omitted variable bias (28), or cross-level bias, which is the “difference between the expectation of an estimator from an ecological [group-level] study and the individual-level parameter of interest” (29, p. 2). E.g., the mortality may have increased in a high-vaccinated country, not because vaccination is detrimental to health, but because relatively few people died there in the previous two years. Similarly, the mortality may have decreased in a low-vaccinated country, not because of a lower health risk than in high-vaccinated countries, but because relatively many people died there in the two previous years. Related to this argument, it is relevant to address that there, for some countries, in concert with relatively low mortality in the pandemic’s two years, was a mortality increase early in 2022, arguably due to the COVID-19 omicron variant (e.g., 30). However, again, we emphasize having accounted for this issue by controlling for the 2020-2021 mortality (plus including other control variables, as discussed above). Also, we have shown that the mortality particularly increased during the first nine months of 2022 in high-vaccination countries, while the mortality due to omicron abated early the same year (31).
Finally, we emphasize that individual-level studies, too, can be subject to fallacy (29, 32). E.g., collective vaccination status can be genuinely associated with reduced disease transmission. Accordingly, individual-level studies can be limited in capturing the association between collective vaccination status and health outcomes. In light of this argument, Loney and Nagelkerke (29, p. 2) assert that “even when the emphasis is clearly on the individual, with the ultimate objective of understanding the aetiology of disease, ecological [group-level] analyses can be more ‘truthful’ than individualistic analyses and may avoid a large portion of confounding on the individual level.” Subramanian, Jones (32, p. 342) similarly state that “meaningful analysis of individual-level relationships requires attention to substantial heterogeneity in state [or group-level] characteristics. The implication is that perils are posed by not only ecological fallacy but also individualistic fallacy.” To illustrate their point, they showed that the individual-level association between race and illiteracy in the US was biased in the absence of controlling for state-level heterogeneity. Hence, not only group-level studies but also individual-level ones can be subject to fallacy. Returning to our data, we accordingly acknowledge as a limitation that the association between nation-level vaccination uptake and excess mortality may not have fully captured an individual-level association, but at the same time an individual-level association could also have been biased in the absence of controlling for higher-level heterogeneity (cf. 32). Therefore, we encourage future studies to address both levels simultaneously.
Other explanations of excess mortality than those studied in this paper can be delayed diagnosis or medical treatment during COVID-19, although we cannot see that the issues have been more prevalent in high-vaccination vs. low-vaccination countries. I.e., we do not expect delayed diagnosis or medical treatment during COVID-19 to substantially have induced omitted variable bias. Nonetheless, we encourage future studies to address the constructs as potential carrier of excess mortality, or eventually study them in concert with vaccination uptake.
Moreover, future research should assess if all-cause mortality in different age cohorts or between genders is a function vaccination uptake or if the type of vaccination has played a role. Similarly, future research should investigate if vaccination uptake or type of vaccination is associated with specific causes of death. Data from England and Wales show excess mortality from April 2022 across gender and age cohorts and several diagnoses (33). However, we do not know if the pattern can be attributed to vaccination uptake, type of vaccination, delayed diagnosis, delayed medical treatment, or if long-COVID (34) has played a role, and future research should investigate these issues.
(The Appendix, carrying out pre-2022 analyses, illuminates a negative association between vaccination uptake and 2021 mortality relative to the 2016-2019 average mortality, which indicates a short-time preventive effect. However, the association becomes non-significant when including relevant controls. 2019 life expectancy, on the other hand, has a significant negative association with 2021 mortality. Finally, the association between 2019 life expectancy and vaccination uptake is strongly positive.)
Copyright and Permission Statement: We confirm that the materials included in this paper do not violate copyright laws. Where relevant, appropriate permissions have been obtained from the original copyright holder(s). All original sources have been appropriately acknowledged and/or referenced.
Funding
This paper has no external funding.
Data Availability Statement
All data used in this research is publicly available. Upon request, the corresponding author can provide raw data and Stata codes.
Conflicts of Interest
The authors decleare no conflict of interest.
Appendix
Table A1 reports pre-2022 descriptive statistics and correlations weighted by countries’ population size. In addition to the pre-2022 country-level variables we already reported on, it includes a variable measuring 2021 all-cause mortality relative to the 2016-2019 average mortality and one measuring 2020 all-cause mortality relative to the 2016-2019 average mortality.
Table A1.
Pre-2022 country-level descriptive statistics and correlations weighted by countries’ population size.
Table A1.
Pre-2022 country-level descriptive statistics and correlations weighted by countries’ population size.
| Min. |
Max. |
Mean |
St. dev. |
|
1 |
2 |
3 |
4 |
| 101.1 |
137.4 |
113.3 |
8.49 |
2021 mort. rel. to 2016-2019 avg. (1) |
|
|
|
|
| 99.6 |
120.7 |
111.8 |
5.20 |
2020 mort. rel. to 2016-2019 avg. (2) |
0.331† |
|
|
|
| 101.4 |
126.1 |
112.5 |
5.59 |
Avg. 2020-2021 mort. rel. to 2016-2019 (3) |
0.901*** |
0.707*** |
|
|
| 75.1 |
84.3 |
81.5 |
2.47 |
Life expectancy in 2019 (4) |
-0.845*** |
0.029 |
-0.620*** |
|
| 27.7 |
83.1 |
68.7 |
10.3 |
Vaccination uptake by the end of 2021 |
-0.862*** |
-0.211 |
-0.742*** |
0.857*** |
We observe a strong negative correlation between vaccination uptake and 2021 mortality, which may indicate a preventive effect that year. Also, we observe a strong positive correlation between pre-COVID life expectancy and 2021 mortality, which may indicate an alternative or complementary explanation to the potential vaccine effect. Finally, we observe a strong positive correlation between pre-COVID life expectancy and vaccination uptake.
Table A2 regresses 2021 mortality on vaccination uptake and pre-COVID life expectancy. Also, it includes 2020 mortality (compared to the 2016-2019 average) as a control variable. The regression aims to assess whether vaccination uptake and pre-COVID life expectancy is genuinely associated with 2021 mortality. The model shows that both independent variables have negative associations with the dependent variable, but only the pre-COVID life expectancy association is significant. The non-significant association between vaccination uptake and 2021 mortality is in line with the largely non-significant direct association between vaccination and 2022 mortality (
Table 3). However, high VIFs concerning the independent variables may indicate multicollinearity problems, particularly since the model has only 31 country observations (22). Altogether, we conclude that vaccination uptake may have temporarily reduced mortality in 2021 (but not in 2022, where the monthly mortality increases the higher the vaccination uptake, as shown earlier in the study).
Table A2.
Pre-2022 country-level linear weighted regressions with robust standard errors and 2021 all-cause mortality compared to the 2016-2019 average as a dependent variable.
Table A2.
Pre-2022 country-level linear weighted regressions with robust standard errors and 2021 all-cause mortality compared to the 2016-2019 average as a dependent variable.
| |
Coeff. |
Beta |
| Intercept |
248.5*** |
|
| |
(29.6) |
|
| 2020 mort. comp. to the 2016-2019 avg. |
0.481** |
0.295 |
| |
(0.152) |
|
| |
[ 1.27] |
|
| Life expectancy in 2019 |
-2.14** |
-0.633 |
| |
(0.552) |
|
| |
[4.55] |
|
| Vaccination uptake by the end of 2021 |
-0.209 |
-0.257 |
| |
(0.149) |
|
| |
[4.76] |
|
| R-square/R-square adj. |
0.854/0.837 |
|
| F-value |
39.5*** |
|
References
- Eurostat. Excess mortality by month. Available online: https://ec.europa.eu/eurostat/databrowser/view/demo_mexrt/default/table?lang=en.
- Haas EJ, Angulo FJ, McLaughlin JM, Anis E, Singer SR, Khan F, et al. Impact and effectiveness of mRNA BNT162b2 vaccine against SARS-CoV-2 infections and COVID-19 cases, hospitalisations, and deaths following a nationwide vaccination campaign in Israel: an observational study using national surveillance data. Lancet. 2021, 397, 1819–1829. [CrossRef]
- Bernal JL, Andrews N, Gower C, Robertson C, Stowe J, Tessier E, et al. Effectiveness of the Pfizer-BioNTech and Oxford-AstraZeneca vaccines on covid-19 related symptoms, hospital admissions, and mortality in older adults in England: test negative case-control study. Bmj-British Medical Journal. 2021, 373. [CrossRef]
- Watson OJ, Barnsley G, Toor J, Hogan AB, Winskill P, Ghani AC. Global impact of the first year of COVID-19 vaccination: a mathematical modelling study. The Lancet Infectious Diseases. 2022. [CrossRef]
- Nordstrom P, Ballin M, Nordstrom A. Risk of infection, hospitalisation, and death up to 9 months after a second dose of COVID-19 vaccine: a retrospective, total population cohort study in Sweden. Lancet. 2022, 399, 814–823. [CrossRef]
- Kadali RAK, Janagama R, Peruru S, Malayala SV. Side effects of BNT162b2 mRNA COVID-19 vaccine: A randomized, cross-sectional study with detailed self-reported symptoms from healthcare workers. International Journal of Infectious Diseases. 2021, 106, 376–381. [CrossRef]
- Klugar M, Riad A, Mekhemar M, Conrad J, Buchbender M, Howaldt HP, et al. Side Effects of mRNA-Based and Viral Vector-Based COVID-19 Vaccines among German Healthcare Workers. Biology-Basel. 2021, 10. [CrossRef]
- Finsterer, J. Neurological side effects of SARS-CoV-2 vaccinations. Acta Neurologica Scandinavica 2022, 145, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Patone M, Mei XW, Handunnetthi L, Dixon S, Zaccardi F, Shankar-Hari M, et al. Risk of Myocarditis After Sequential Doses of COVID-19 Vaccine and SARS-CoV-2 I nfection by Age and Sex. Circulation. 2022, 146, 743–754. [CrossRef]
- Karlstad Ø, Hovi P, Husby A, Härkänen T, Selmer RM, Pihlström N, et al. SARS-CoV-2 Vaccination and Myocarditis in a Nordic Cohort Study of 23 Million Residents. JAMA Cardiology. 2022, 7, 600–612. [CrossRef]
- Oster ME, Shay DK, Su JR, Gee J, Creech CB, Broder KR, et al. Myocarditis Cases Reported After mRNA-Based COVID-19 Vaccination in the US From December 2020 to August 2021. JAMA. 2022, 327, 331–340. [CrossRef]
- Tuvali O, Tshori S, Derazne E, Hannuna RR, Afek A, Haberman D, et al. The Incidence of Myocarditis and Pericarditis in Post COVID-19 Unvaccinated Patients—A Large Population-Based Study. Journal of Clinical Medicine. 2022, 11, 2219. [CrossRef]
- Lazarus R, Klompas M, Bernstein S. Electronic Support for Public Health–Vaccine Adverse Event Reporting System (ESP: VAERS). Grant Final Report, Grant ID: R18 HS. 2010, 17045.
- European Centre for Disease Prevention and Control. COVID-19 Vaccine Tracker. Available online: https://vaccinetracker.ecdc.europa.eu/public/extensions/COVID-19/vaccine-tracker.html#uptake-tab.
- Our World in Data. Coronavirus (COVID-19) Vaccinations. Available online: https://ourworldindata.org/covid-vaccinations.
- Eurostat. Life expectancy by age and sex. Available online: https://ec.europa.eu/eurostat/databrowser/view/demo_mlexpec/default/table?lang=en.
- Roser M, Ortiz-Ospina E, Ritchie H. Our world in data. Life expectancy: University of Oxford; 2013. Revidert oktober 2019. Available online: https://ourworldindata.org/life-expectancy.
- Eurostat. Deaths and crude death rate. Available online: https://ec.europa.eu/eurostat/databrowser/view/tps00029/default/table?lang=en.
- Raudenbush SW, Bryk AS. Hierarchical Linear Models: Applications and Data Analysis Methods. 2nd ed. Thousand Oaks, CA: Sage; 2002.
- Snijders TAB. Multilevel Analysis. In: Lovric M, editor. International Encyclopedia of Statistical Science. Berlin, Heidelberg: Springer Berlin Heidelberg; 2011. p. 879-82.
- StataCorp. Version 17. College Station, TX StataCorp LP; 2021.
- O’Brien RM. A caution regarding rules of thumb for variance inflation factors. Qual Quant. 2007, 41, 673–690. [CrossRef]
- Cook TD, McCleary R, McCain LJ, Reichardt CS, Fankhauser G, Campbell DT. Quasi-experimentation: design & analysis issues for field settings. Boston: Houghton Mifflin Co.; 1979.
- Hsieh JJ. Encyclopedia Britannica. Ecological fallacy 2017, September 4. Available online: https://www.britannica.com/science/ecological-fallacy.
- Robinson WS. Ecological Correlations and the Behavior of Individuals. Am Sociol Rev. 1950, 15, 351–357. [CrossRef]
- Simpson EH. The Interpretation of Interaction in Contingency Tables. Journal of the Royal Statistical Society: Series B (Methodological). 1951, 13, 238–241. [CrossRef]
- Blyth CR. On Simpson’s Paradox and the Sure-Thing Principle. J Am Stat Assoc. 1972, 67, 364–366. [CrossRef]
- Rothman KJ. A pictorial representation of confounding in epidemiolog1c studies. Journal of Chronic Diseases. 1975, 28, 101–108. [CrossRef]
- Loney T, Nagelkerke NJ. The individualistic fallacy, ecological studies and instrumental variables: a causal interpretation. Emerging Themes in Epidemiology. 2014, 11, 18. [CrossRef]
- Folkehelseinstituttet. Dødelighet i Norge under koronapandemien 2020 til høsten 2022 In: https://www.fhi.no/contentassets/a5c83528acc94ddfbe815a5934faadf5/dodelighet-under-koronapandemien-2020-til-hosten-2022.pdf, editor. Olslo, Norge2022.
- Statista. Number of new coronavirus (COVID-19) deaths in Europe since February 2020 2023. Available online: https://www.statista.com/statistics/1102288/coronavirus-deaths-development-europe/.
- Subramanian SV, Jones K, Kaddour A, Krieger N. Revisiting Robinson: The perils of individualistic and ecologic fallacy. International Journal of Epidemiology. 2009, 38, 342–360. [CrossRef]
- Office for Health Improvements and Disparities. Excess Mortality in England. Available online: https://app.powerbi.com/view?r=eyJrIjoiYmUwNmFhMjYtNGZhYS00NDk2LWFlMTAtOTg0OGNhNmFiNGM0IiwidCI6ImVlNGUxNDk5LTRhMzUtNGIyZS1hZDQ3LTVmM2NmOWRlODY2NiIsImMiOjh9.
- Centers for Disease Control and Prevention. Long COVID or Post-COVID Conditions. Updated Sep. 1, 2022. Available online: https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).