Introduction
Obesity has reached an alarming proportion around the world. This has been described as a "global epidemic" and a "major public health issue" by the World Health Organization. (1) The expansion may be related to the evolving cultural, social, and economic forces affecting numerous nations. Obesity has been more common in the general population since the 1990s, affecting both the general public and women of reproductive age, particularly pregnant women. (2) Obesity during pregnancy increases the risks to both the mother and the newborn (4). Furthermore, it place pregnant women and their infants at risk for a range of unfavorable pregnancy outcomes, including postpartum weight retention, which increases the potential for long-term obesity. (5) Obesity is also an issue for healthcare workers. It has become one of the most serious healthcare complications for pregnant women in the last decade, putting an additional strain on healthcare systems and there is a strong relationship between Body mass index (BMI) and healthcare spending. (6) The obesity pandemic has also been common in the state of Qatar, a country with a population of 2,6 million people, where only 12.0 percent of whom are natives. This country is rapidly modernizing, quickly becoming one of the world's largest liquid gas exporters, ranking in the top ten countries in terms of per capita GDP. (7-9) Women constitute around 25% of the country's population. (10, 11) Rapid modernization, a diverse population, increased availability of various varieties of food and fast food, a high intake of processed foods, and a lack of physical activity, among other things, have all been linked to an increase in the number of obese persons. (7) According to the Qatar National Health Strategy, 70.1% of adults (including ex-pats and indigenous) residing in Qatar are either overweight (28.7%) or obese (41.4%). (9) The purpose of this research is to find out how BMI is distributed and changing among pregnant women in Qatar, as well as how it affects pregnancy outcome and other health consequences.
Methods
This study used data from the Qatar Pearl-Peristat Registry funded by The Qatar National Research Fund is funding the registry (QNRF). The registry is a retrospective study that focuses on maternal and newborn medical records from four government-run hospitals in the country, with information spanning the perinatal and postpartum periods. The private sector has been omitted from the registry because it accounts for less than 15% of all births in Qatar and does not use the same electronic health record system. Most of the registry data came from Cerner™ shared electronic medical records (EMR), which connects all four government hospitals. In addition, a post-delivery social data questionnaire was used to collect socioeconomic and demographic health information about the parturient women's social status. Under the guidance of a full-time, qualified research associate, the registry research team comprises 12 research assistants who collect patient data directly from the family (social data) or through the EMR (electronic clinical data, Cerner™). The collected data was assessed and saved in software developed specifically for the Dendrite® database system, and it was analyzed with both Dendrite® and SPSS® version 21. The Medical Research Center of Hamad Medical Corporation granted ethical approval from the Pearl-Peristat Registry. For participants, no written consent was required. Before getting social data, participants provided verbal agreement and were handed patient information pamphlets. The current study looked at the BMI of singleton babies at the four main state-run hospitals where women were delivered. The BMI was measured Before pregnancy (or early in the first trimester), during the antenatal clinic visits, and at the time of birth.
Body Mass Index Calculation and Classification
Using hospital weight and height data, the pre-pregnancy, booking, and delivery BMIs were calculated. The BMI of everyone was computed by dividing their weight (kilogram) by their height (centimeter). For the analysis, the pre-pregnancy BMI variable was determined. The pre-pregnancy BMI is the BMI before pregnancy or the BMI during the first trimester of pregnancy. Moribund obesity has been combined with the "obesity" category to allow for more meaningful comparisons; it is referred to as obesity in this study. The following BMI categories were statistically compared: (1) "underweight," (2) "normal weight," (3) "overweight," and (4) "obesity."
Outcome metrics
Maternal variables include maternal age, gravidity, parity, mode of delivery, gestational diabetes mellitus, hypertension, cholestasis, and post-partum hemorrhage (PPH). Neonatal variables included low birth weight (less than 2500 grams), gestational age less than 37 weeks, live births or stillbirths, and admission to the postnatal ward or NICU.
Statistics for analysis:
To understand the distribution of the variables, descriptive statistics were generated using IBM SPSS 21 statistical software. A two-sided P value of 0.05 was used to assess statistical significance. Both univariate and multivariate analyses were used in the modeling technique. To evaluate the association between BMI and research findings, we used univariate and multivariate logistic regression. The univariate method was used to investigate the basic (unadjusted) association. A multivariable analysis was performed to investigate the relationship between BMI and pregnancy outcomes, considering the influence of other relevant confounding variables.
Results
The study comprised 2960 single pregnant women who had their pre-pregnancy or early pregnancy BMI calculated. Underweight women accounted for 83, normal-weight women for 1053, overweight women accounted for 937, and obese women accounted for 887. (
Table 1)
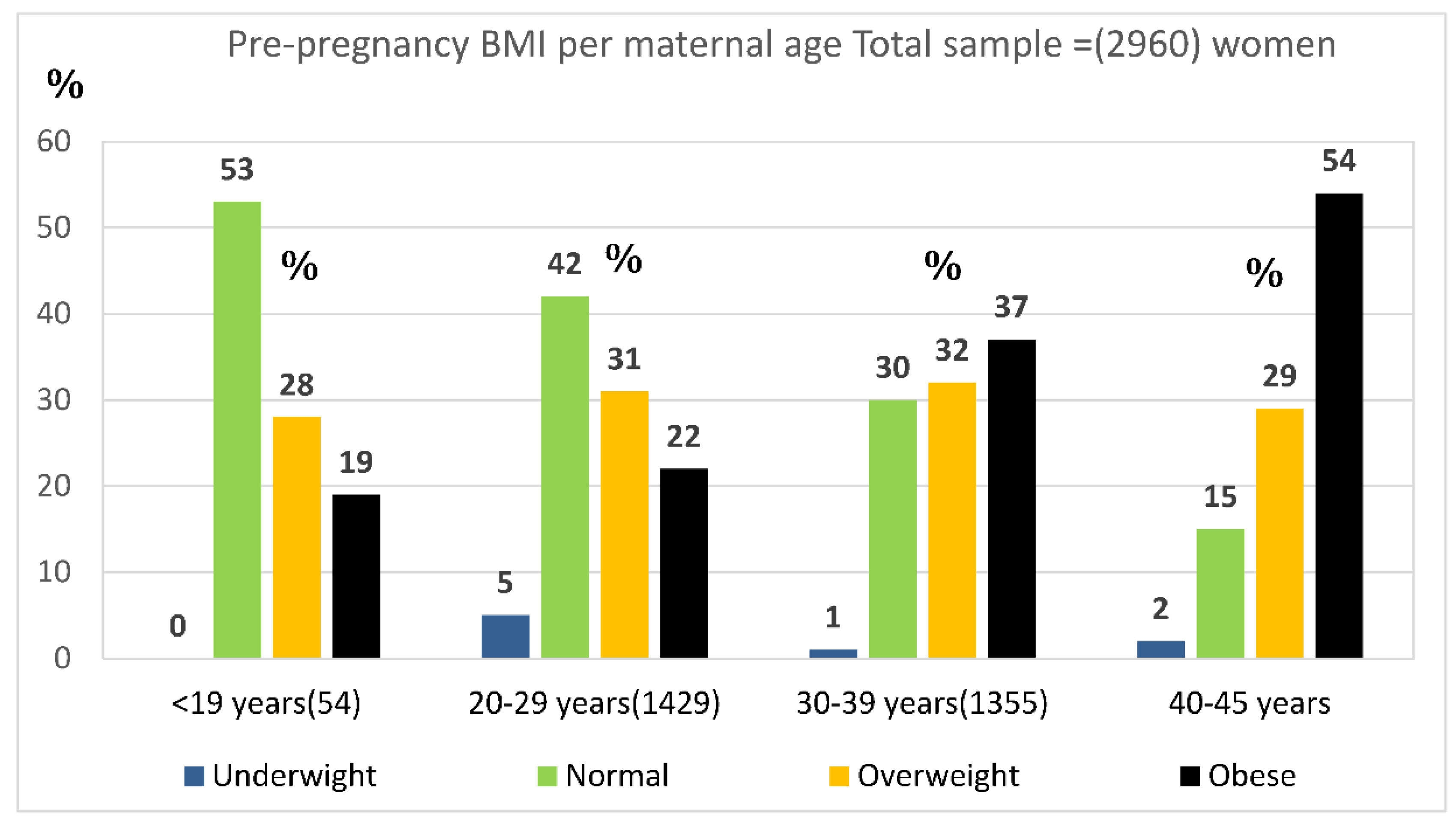
Obesity risk increased linearly as maternal age increased. Obesity was found in 19% of women younger than 20-year-old, 22% of 20- to 29-year-old women, 37% of 30- to 39-year-old women, and 54% of women over 40 years old. (See
Figure 1) The pre-pregnancy BMI was calculated to be 2,960. 2.8% (83) of women were underweight, 35.6% (1105) were normal weight, 31.6% (937) were overweight, and 30% (887) were obese, according to their pre-pregnancy BMI. (Table,
Figure 1)
Increased BMI increases the risk of cesarean section, gestational diabetes (GDM), and hypertension. The incidence of CS was 15.7% in the underweight group, 24.9% in the normal weight group, 31.3% in the overweight group, and 41% in the obese group. GDM was diagnosed in 37.5 percent of obese women, 31.8 percent of overweight women, 23 percent of normal-weight women, and 16.7 percent of underweight women. Hypertensive conditions were three times as common in obese women than in normal-weight women. Women who were overweight or obese did not have an increased risk of postpartum hemorrhage; 5.3% of obese women versus 5.6% of normal-weight women experienced PPH. (
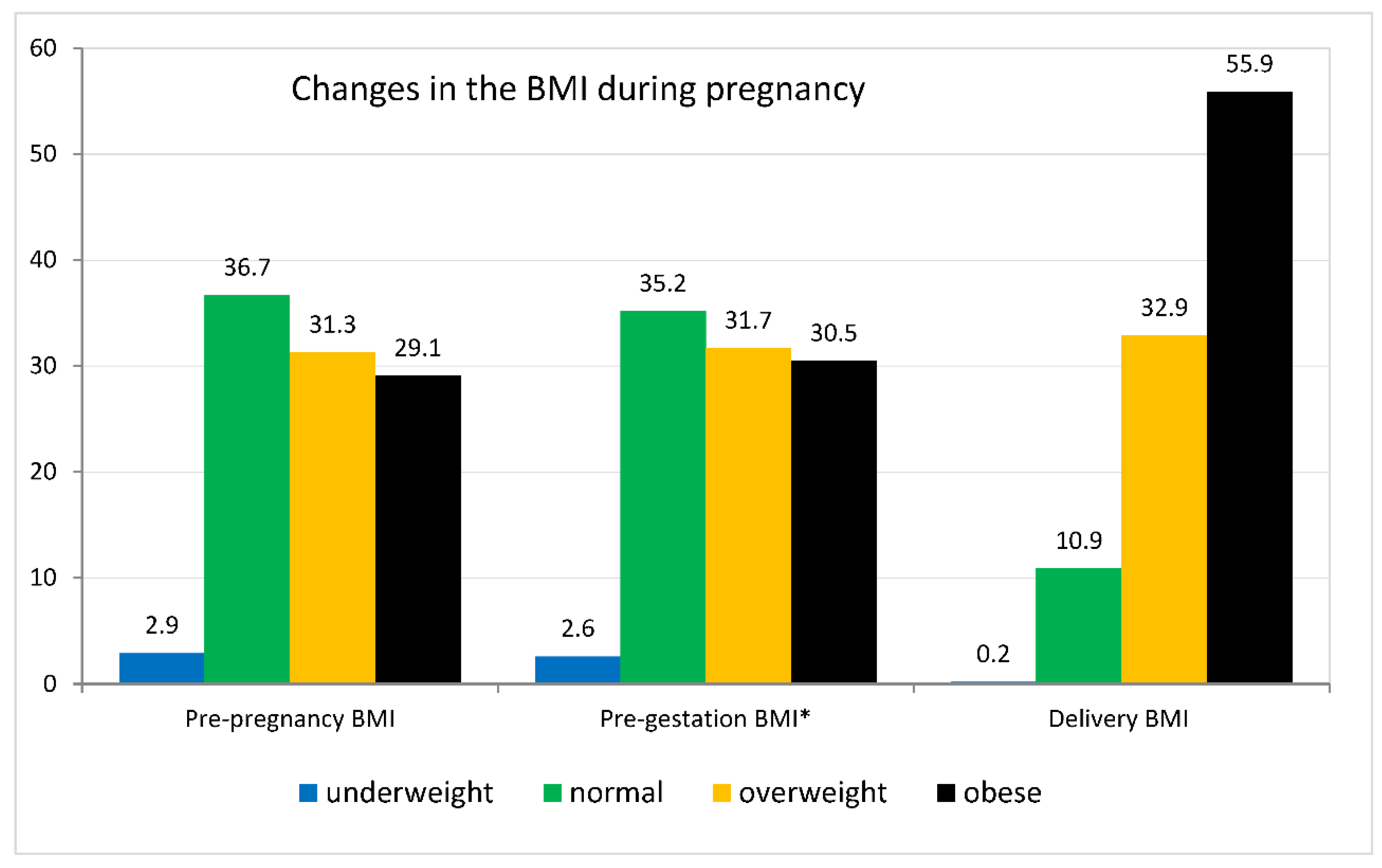
Table 2) The proportion of overweight and obesity among Qatari women were 32% and 37%, compared to 31% and 28% in non-Qatari women, respectively. Throughout pregnancy, rate of obesity and overweight was significantly snowballing where only 29% of the sample size labeled as obese in the pre-pregnancy period, while the rate increased to be 56% at delivery. In other words, the underweight group gained the most weight during pregnancy, whereas the obese group gained the least. The mean weight gain in underweight was 13 (±9 kg), 11(±6) in normal weight, kg 9 (kg ±6) in overweight and 6.8 (±7 kg.) in obese women with total weight gain of 9 (±7 kg) in all age groups. (
Figure 2)
The percentage of babies admitted to the neonatal intensive care unit (NICU) in the pre-pregnancy BMI-tested sample was higher for obese mothers than for women with a normal BMI. 14.6% of babies born to obese mothers were admitted to the NICU, compared to 11.3% of newborns born to normal-weight mothers. The probability of stillbirth in the obese group was not significantly high in obese group. Preterm births were more common in the underweight (11.8%) and obese (9.9%) groups than in the normal BMI (4.9%) group. It was typical for babies born to overweight or obese mothers to weigh more than 4000 grams. Just 7% of obese women had newborns weighing more than 4000 grams, compared to 3% of women with a normal BMI. (
Table 3)
Results of Logistic Regression
There was no link found between being overweight or obese and stillbirth or low birth weight. An above-normal BMI, on the other hand, was linked to a 1.5-fold greater risk of preterm birth, macrosomia, and NICU hospitalization (see
Table 3). Overweight women were 1.3 times more likely than normal-weight women to have a cesarean section, 1.5 times more likely to develop GDM, and two times more likely to have hypertensive issues. Obese women's traits were enhanced. They were twice as likely to have a cesarean birth, gestational diabetes, and hypertensive issues throughout pregnancy. (
Table 2)
Discussion
The Maternal and Neonatal Registry data were used in this hospital-based study to learn more about the association between BMI and various perinatal outcomes in our population. Pregnant women with a high BMI were more likely to have a cesarean section, develop gestational diabetes, and develop hypertension in our study. For overweight and obese mothers, however, there was no increase in postpartum hemorrhage (PPH). PPH was found in 5.3% of obese women and 5.6% of average-weight women. (table 2) Various research studies have disputed the precise effect of obesity on PPH. Our findings do support that w eight is not a significant risk factor for postpartum hemorrhage, consistent with the previous research findings. (12) However, another study encountered a positive relationship between obesity and postpartum hemorrhage, implying that as obesity levels rise, so will the incidence of atonic postpartum hemorrhage. (13) Inconsistencies in definitions, variations in practices and health care systems, racial compositions, and study participant variability are all possible causes of the rise in PPH in various studies. (12,13) One of the study's strengths is that it was carried out at a single institution with very slight changes in some of the confounding variables found in other research. The risk of gestational diabetes (GDM) grows linearly with Obesity. GDM was diagnosed in 37.5 percent of obese women, 31.8 percent of overweight women, 23 percent of normal-weight women, and 16.7 percent of underweight women. This finding is consistent with previous research that shows that the higher the BMI, the higher the incidence of GDM. (14) Obesity prevalence increased linearly with maternal age. Obese women increased from 19% in the 19-to-40 age group to 54% in the >40 age group. Obesity was more prevalent among natives than among foreigners (
Figure 1), and it is an important factor to consider when counseling women of various ages. The importance of basic health care and weight-loss programs should be emphasized more strongly in older age groups considering childbearing. Obesity is linked to aging, which raises the risk of insulin resistance and metabolic syndrome. (15) In our study, mothers with a low BMI at the start of their pregnancy gained more weight than mothers with a higher BMI. (
Figure 2) This observation is worth debating. The allowable weight gain parameters during pregnancy are a source of significant debate. Weight-gain ranges are not provided in the UK recommendations. (16) In comparison, the North American Institute of Medicine (IOM) recommends that underweight women gain up to 18 kg and obese women gain up to 9 kg. (17) Our findings can help with prenatal counseling and tailoring the optimal weight gain during pregnancy conversation. A portion of our study's participants may have gained more weight than necessary, putting them at risk of retaining extra weight after the pregnancy and reaping no legitimate advantage. In one study, 47 percent of pregnant women gained more weight than the Institute of Medicine (IOM) recommends, implying an increased risk of adverse maternal and infant outcomes. (18) Given our findings and the fact that Qatar is a cultural melting pot, fully adhering to IOM norms may not be prudent.
Six parameters were used in this study to examine the influence of greater BMI on neonatal outcomes. (table 3) The neonatal intensive care unit (NICU) admission was chosen as the criterion for measuring the physical status at birth and as an indicator of the effect of the mother's BMI on the baby's health. Underweight and obese mothers had a higher percentage of babies admitted to the NICU when compared to women with a normal BMI. Babies delivered to obese mothers were admitted to the NICU at a rate of 14.6%, compared to 11.3% of children born to normal-weight mothers. This finding is consistent with previous research that indicated an increased likelihood of newborn critical care admission for infants born to obese mothers. (19-21) In a study of 3,388 women, there were no differences in NICU admissions between obese and normal mothers. (22) The disparity in findings may be due to differences in identifying and prioritizing infants who can benefit from NICU treatment among institutions.
Using birth weight as a proxy for intrauterine growth, researchers observed that the probability of delivering a baby weighing more than 4000 g rose as maternal BMI before conception increased. Just 7% of obese women had newborns weighing more than 4000 grams, compared to 3% of women with a normal BMI. This discovery adds to previous studies that found a 1.5-2.3% increase in the likelihood of obese mothers giving birth to large-for-gestational-age infants. Obesity in the mother is a well-known risk factor for rapid intrauterine growth, with fetal macrosomia consistently associated with a higher maternal body mass index. (23) Obesity is significantly linked to the delivery of newborns in the 90th percentile (24).
Few researches raised concerns regarding an association between obesity and an increased risk of stillbirth. (25) In our report, the incidence of stillbirth was 1.1% in the obese group versus 0.7% in the normal BMI group with low significance (
Table 3). In contrast, there were no stillbirths in the underweight group, confirming previous studies that found a reduction in stillbirths among mothers with a low BMI. (26) There are several unsolved questions about the specific role of obesity on stillbirth. Obesity and stillbirth are both challenging issues with multiple complicating factors. This study, on the other hand, uses a different study group to validate the same conclusions about an increased risk of stillbirth with increasing BMI. Furthermore, because it is based on a single institution with a diverse population, numerous confounding factors that have been observed in earlier studies may not apply to this study. Based on our findings, we believe that encouraging weight loss programs before pregnancy can help reduce stillbirth rates in subsequent pregnancies in our demographic, in addition to the many benefits of weight loss.
The study's advantages
The study cohort's prospective nature is a major strength of our investigation. Because of the large size of the cohort, a phenotype may be chosen to investigate the effects of high BMI on maternal and infant outcomes. Several confounding variables associated with diverse healthcare systems or practices are avoided by conducting the study in a single institution (Hamad Medical Corporation) that follows the same clinical protocols and shares rotating medical and nursing staff with a reasonably large sample size. Furthermore, because the study population and sample are distinct, our findings can be applied to a broader range of population.
List of Abbreviations:
| BMI |
Body Mass Index |
| EMR |
Electronic Medical Record |
| GDM |
Gestational Diabetes Mellitus |
| HMC |
Hamad Medical Corporation |
| NICU |
Neonatal Intensive Care Unit |
| PPH |
Postpartum Hemorrhage |
References
- Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000;894:i-xii, 1-253. PMID: 11234459.
- Office for National Statistics. NHS. Statistics on Obesity, Physical Activity and Diet: England, January 2008. London, 2008.
- Chen C, Xu X, Yan Y. Estimated global overweight and obesity burden in pregnant women based on panel data model. PLoS One 2018;13(8):e0202183. Published 2018 Aug 9. [CrossRef]
- Fitzsimons KJ, Modder J; Centre for Maternal and Child Enquires. Setting maternity care standards for women with obesity in pregnancy. Semin Fetal Neonatal Med 2010;15(2):100-107. [CrossRef]
- Shaikh H, Robinson S, Teoh TG. Management of maternal obesity prior to and during pregnancy. Semin Fetal Neonatal Med 2010;15(2):77-82. [CrossRef]
- Morgan KL, Rahman MA, Macey S, et al. Obesity in pregnancy: a retrospective prevalence-based study on health service utilisation and costs on the NHS. BMJ Open 2014;4(2):e003983. Published 2014 Feb 27. [CrossRef]
- Taheri S, Al-Thani M. Obesity in Qatar: current and future strategies. Lancet Diabetes Endocrinol 2021;9(9):561-562. [CrossRef]
- World bank, World development indicators. (2022). GDP per capita – Qatar. https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?locations=QA.
- Qatar National Health Strategy (2018-2022). https://www.moph.gov.qa/english/strategies/National-Health-Strategy-2018-2022/Pages/default.aspx.
- World bank, World development indicator. (2022). Population, female (% of total population) – Qatar. https://data.worldbank.org/indicator/SP.POP.TOTL.FE.ZS?locations=QA.
- Woman and Man in the State of Qatar: a Statistical Portrait (2018). https://www.psa.gov.qa/en/statistics/Statistical%20Releases/Social/GenrealSocialStatistics/MenWomenProfile/2018/Woman_Man_2018_EN.pdf.
- Butwick AJ, Abreo A, Bateman BT, et al. Effect of Maternal Body Mass Index on Postpartum Hemorrhage. Anesthesiology 2018;128(4):774-783. [CrossRef]
- Blomberg M. Maternal obesity and risk of postpartum hemorrhage. Obstet Gynecol. 2011;118(3):561-568. [CrossRef]
- Catalano PM. The impact of gestational diabetes and maternal obesity on the mother and her offspring. J Dev Orig Health Dis 2010;1(4):208-215. [CrossRef]
- National Institute for Health and Care Excellence (NICE). Weight management before, during and after pregnancy. Public health guideline [PH27]. London: NICE; 2010.
- Rasmussen KM, Yaktine AL, Institute of Medicine (US) and National Research Council (US) Committee to Reexamine IOM Pregnancy Weight Guidelines, eds. Weight Gain During Pregnancy: Reexamining the Guidelines. Washington (DC): National Academies Press (US); 2009.
- Goldstein RF, Abell SK, Ranasinha S, et al. Association of Gestational Weight Gain With Maternal and Infant Outcomes: A Systematic Review and Meta-analysis. JAMA 2017;317(21):2207-2225. [CrossRef]
- Usha Kiran TS, Hemmadi S, Bethel J, Evans J. Outcome of pregnancy in a woman with an increased body mass index. BJOG 2005;112(6):768-772. [CrossRef]
- Callaway LK, Prins JB, Chang AM, McIntyre HD. The prevalence and impact of overweight and obesity in an Australian obstetric population. Med J Aust 2006;184(2):56-59. [CrossRef]
- Kalk P, Guthmann F, Krause K, et al. Impact of maternal body mass index on neonatal outcome. Eur J Med Res 2009;14(5):216-222. [CrossRef]
- Vinturache AE, McDonald S, Slater D, Tough S. Perinatal outcomes of maternal overweight and obesity in term infants: a population-based cohort study in Canada. Sci Rep 2015;5:9334. Published 2015 Mar 20. [CrossRef]
- Yao R, Ananth CV, Park BY, Pereira L, Plante LA; Perinatal Research Consortium. Obesity and the risk of stillbirth: a population-based cohort study. Am J Obstet Gynecol 2014;210(5):457.e1-457.e4579. [CrossRef]
- Leddy MA, Power ML, Schulkin J. The impact of maternal obesity on maternal and fetal health. Rev Obstet Gynecol 2008;1(4):170-178.
- Sebire NJ, Jolly M, Harris JP, et al. Maternal obesity and pregnancy outcome: a study of 287,213 pregnancies in London. Int J Obes Relat Metab Disord 2001;25(8):1175-1182. [CrossRef]
- Jura M, Kozak LP. Obesity and related consequences to ageing. Age (Dordr) 2016;38(1):23. [CrossRef]
- Gardosi J, Madurasinghe V, Williams M, Malik A, Francis A. Maternal and fetal risk factors for stillbirth: population based study. BMJ 2013;346:f108. Published 2013 Jan 24. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).