1. Introduction
Central venous pressure (CVP) is a hemodynamic parameter that has widely been monitored in the intensive care units (ICU) for assessing the cardiac function, the right atrium preload, the volume status and the fluid responsiveness in critically ill patients [
1,
2,
3]. Over the course of time the usefulness and the accuracy of CVP as a strong hemodynamic and endovascular volume index has been debated and the currently available published research reveals no absolute correlation between CVP values and the total blood volume present in human circulation [
4]. In line with these data, the European Society of Intensive Care Medicine does not recommend the CVP as a measure to guide the fluids’ administration and to predict the patient responsiveness to fluid therapy [
4]. It seems that many inherent weaknesses of the CVP affect negatively its reliability, given that CVP values are altered by many of parameters outside the circulating blood volume, such as venous compliance, systematic vascular resistances, pulmonary hypertension, tricuspid valve insufficiency, heart failure, cardiac dysrhythmias and conditions associated with increased intrathoracic pressure, including cardiac tamponade, tension pneumothorax, positive pressure mechanical ventilation and positive end-expiratory pressure [
5].
Despite the inherent limitations of the CVP, that generate its sensitivity in a variety of parameters and clinical disorders, and the presence of other methods for volume status estimation and guidance to fluid administration in the clinical setting, such as trans-esophageal echocardiography and ultrasound-guide techniques, CVP remains the most frequent estimated hemodynamic parameter in the critically ill setting by intensivists and critical care nurses [
6]. In Greece, recently the CVP measurement and estimation are among the legal professional duties of the critical care nurses [
7].
Although many studies have been carried out in order to determine the accuracy and the reliability of CVP value for the estimation of critically ill volume and hemodynamic status [
8,
9,
10], nothing we know regarding the extent in which critical care nurses, use CVP measurements in their decision-making process for the optimal volume, hemodynamic and cardiovascular management of the critically ill patients, given that CVP measurements are both a frequent intervention and a legally recognized critical care nurses’ professional responsibility. Attempting to add new research data on this lacked body of knowledge the aim of the present study was the development of a new questionnaire for accessing how critical care nurses use CVP measurements to address patients’ hemodynamics and volume status. Additionally, the investigation of the validity and reliability of this new-developed questionnaire.
2. Materials and Methods
2.1. Study design and participants
A cross-sectional, validation study was conducted among critical care nurses from four ICUs of two general tertiary hospitals of Greece. Nurses who were unwilling to give their consent to participate in our study and those with uncompleted filled out questionnaires were excluded. Based on these exclusion criteria the final study sample was 120 critical care nurses. Data collection took place during a three-month period (from August to October 2018). This sample size meets the minimum requirement for the instrument validation process for at least 10 participants per each questionnaire item [
11].
2.2. Content Validity
Aiming to create the new questionnaire, named “CVP-Score”, a comprehensive literature review was conducted. In the currently available published research, we did not find any instrument which measure how nurses use CVP values in order to manage the critically ill patients and to determine their nursing care plans. At the first phase of the development of the CVP-Score 10 items have been selected for the entire questionnaire. Each item was a full sentence of specific interventions related to how nurses use CVP values in order to determine their care planning and to make clinical decisions for the critically ill patient management. Each item of the questionnaire could be answered using a 4-point Likert scale from “Never” (1 point) to “Always” (4 points).
Assessing the content validity of the new-developed questionnaire, this tool was evaluated by a five-expert panel, consisting by 2 ICU nurses, 1 intensivist, and 2 researchers with significant scientific work on intensive and critical care nursing. Each item of the questionnaire was graded by the experts as “essential”, “useful but inadequate” or “unnecessary”. All experts’ evaluations were taken into account and finally 2 items were excluded from the questionnaire, given that their content validity ratio was lower than 0.99. Specifically, the content validity ratio of the first and second excluded items were 0.66 and – 0.2, respectively. Subsequently, 10 persons from the general population and out of our study sample, provide feedback on the 8-item questionnaire, evaluating the linguistic clarity of the tool.
2.3. Data collection
Structured face to face interviews were conducted for data collection purposes, among 120 critical care nurses from two ICUs of two general tertiary hospitals of Greece, using the “CVP Score” and a second short questionnaire on basic participants’ demographics. CVP score ranged from 8 to 32. High values of the CVP Score indicate high use of CVP for the nursing assessment of patients’ hemodynamic and volume status, while low values are indicative that nurses considered CVP as a poor clinical tool in order to estimate patients’ hemodynamics and to plan their provided care based on its values. At second stage (second assessment) the participants re-answer the questionnaire through phone interviews, after one month from the first assessment.
2.4. Ethics
Written permission was given from the ethics committee of both the two hospitals. Precautions took place to protect the privacy and anonymity of the participant subjects and the confidentially of their data and information, while participants gave their sign informed consent. The collected data were used only for the purpose of the present study. All the stages of the research were carried out in full accordance with the ethical standards of the Helsinki Declaration of 1975, as revised in 2013.
2.5. Statistical analysis
Quantitative and qualitative variables were expressed as mean [±Standard Deviation (SD)] values and absolute – relative frequencies, respectively. Construct validity was described by calculating the Pearson’s correlation coefficient r of the scores of participants’ responses to an item with their total scores. The Cronbach alpha coefficient was calculated for the internal consistency reliability of the entire questionnaire. Pearson’s rank correlation coefficient was performed to measure the level of agreement between responses at test and re-test, while the Spearman-Brown formula was used for computing the split-half reliability. The IBM SPSS 24.0 for Window software (Armonk, NY: IBM Corp) was used for our statistical analysis purposes.
3. Results
3.1. Demographics
As shown in
Table 1 the mean (±SD) age of our study participants was 42.3±6.1 years, while the majority of our sample was female subjects (71.7%), graduates of technological tertiary education (88.3%) and had no postgraduate education (66.7%). In addition, the half of the study participants’ (51.7%) was working at a specialized ICU, and their mean (±SD) clinical and ICU experience was 17.3 (±6.8) and 13(±7.1) years, respectively.
3.2. Construct Validity
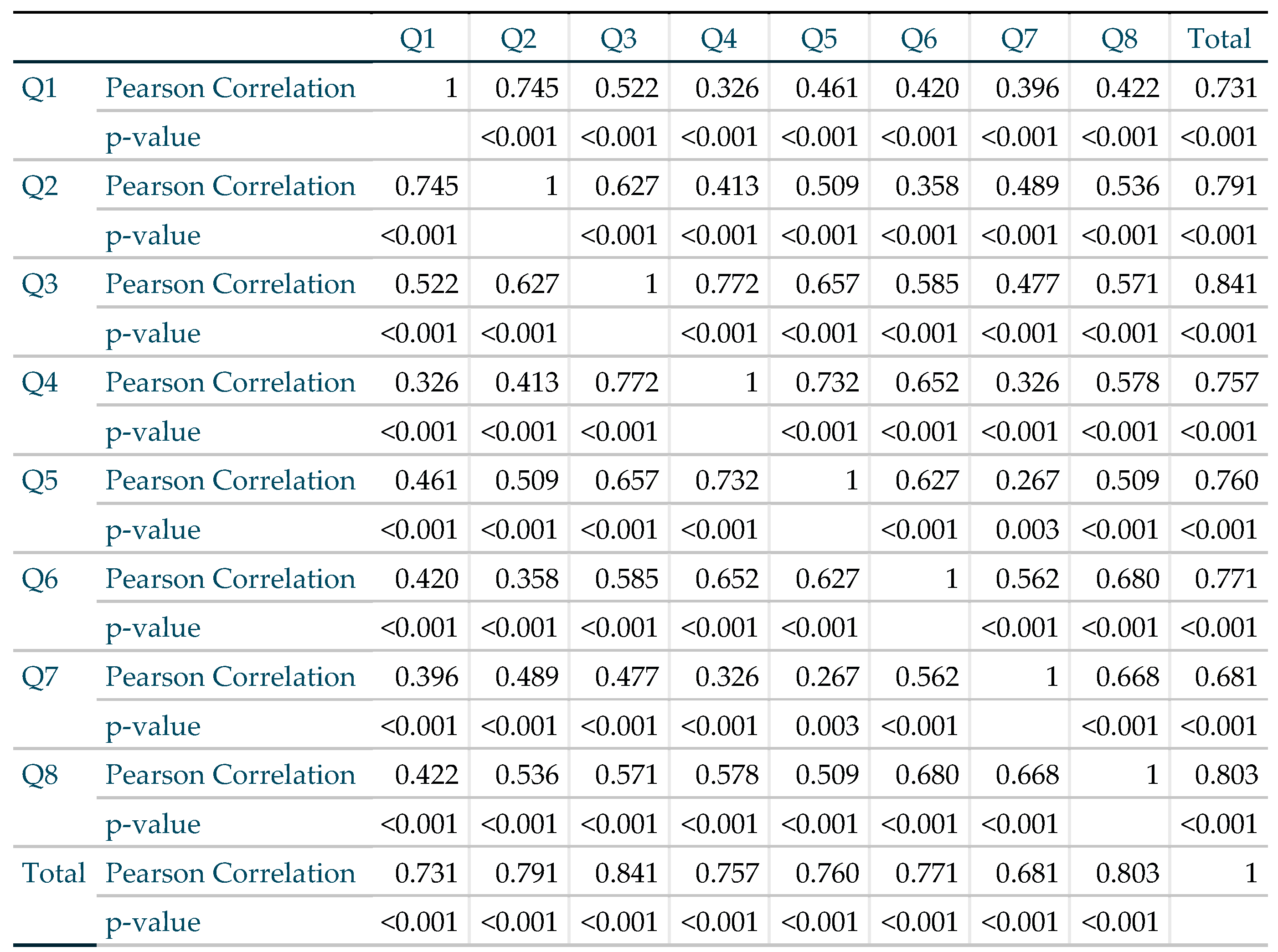
As aforementioned and summarized in
Table 2, construct validity was evaluated with the Pearson’s correlation coefficient r of the scores of participants’ responses to an item with their total scores. All the calculated values were statistically significant and each obtained Person Correlation coefficient value was greater than the critical value from the Pearson’s Correlation Table at 118 (N-2) degrees of freedom.
3.3. Instrument internal consistency reliability
The Cronbach alpha was 0.901 for the entire questionnaire.
3.4. Test-retest reliability
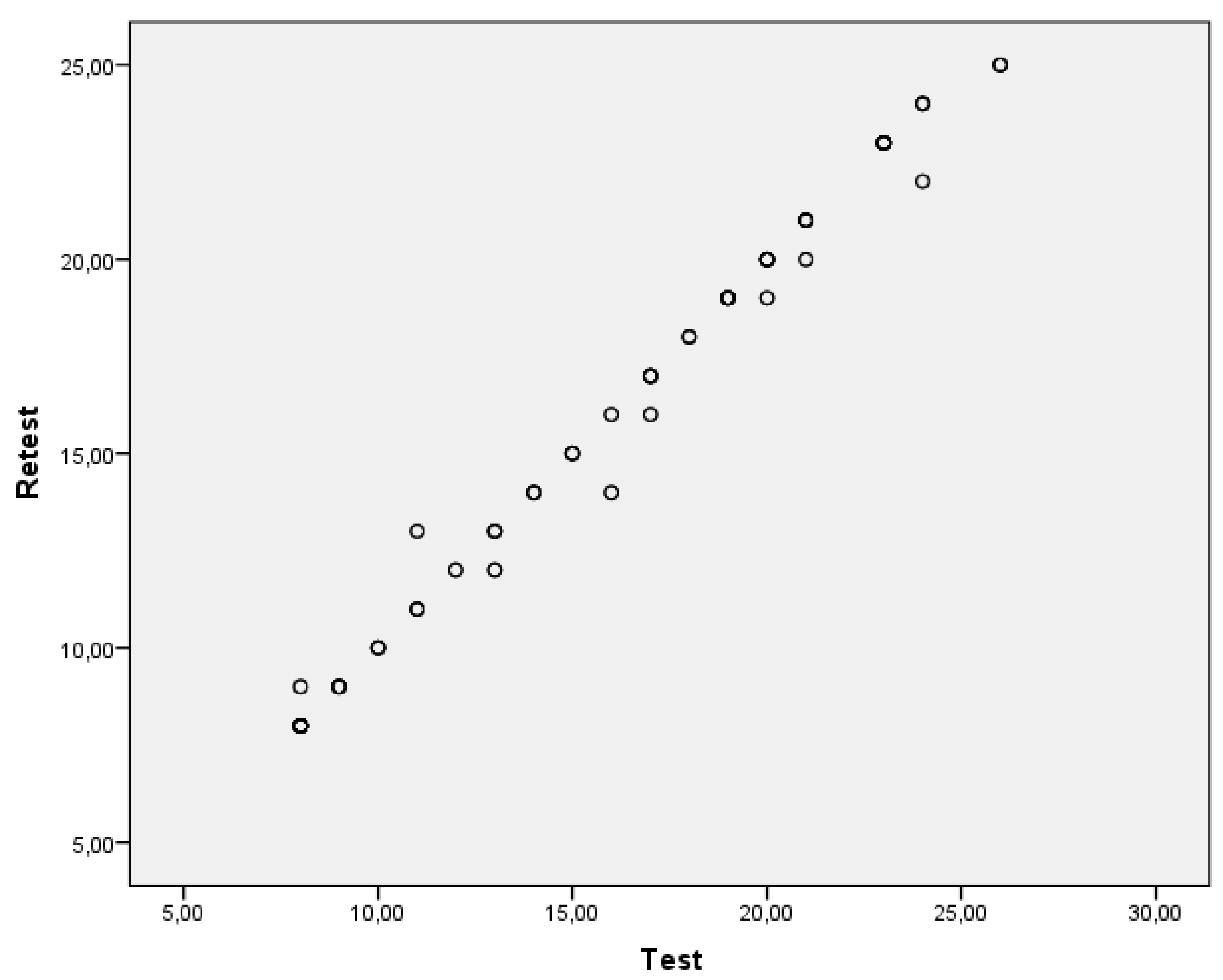
By using test-retest reliability coefficient correlation analysis, a high positive correlation was observed between the total scores of the two applications (r=0.996, p<0.001). The measurements of the CVP-Score are depicted via a scatter plot in
Figure 1.
3.5. Split-half reliability
The split-half reliability was computed to be 0.855 using the Spearman-Brown formula.
4. Discussion
According to the main aim of the present study we developed a new instrument in order to measure how ICU nurses use CVP in order to guide their planning, clinical decisions, interventions and fluid administration titration for the optimal management of the critically ill patient. To the best of our knowledge, this new-developed tool named “CVP Score” was the first one instrument for the above-mentioned purpose. Another important aim of the present study was to test the validity and reliability of this new-developed instrument. According to the findings of our study, “CVP Score” is a valid and reliable instrument that intents to provide researchers a significant and acceptable tool for assessing the extent of CVP values use by critical care clinicians for ICU patients planning of care and decision making.
Validity is defined as the extent to which an instrument measures exactly what it is supposed to measure without mistaking it with another issue, while reliability is the extent to which an instrument gives consistent results in repeated measurements under similar conditions [
11]. Assessing the validity of the “CVP Score” it was followed the appropriate methodology to ensure its content validity, during the development of our instrument. Additionally, the evaluated construct validity of the “CVP Score”, through the correlation of each item score with the total score, emerged as acceptable [
10].
On the other hand, assessing the reliability of our new-developed questionnaire we observed that “CVP Score” had an excellent Cronbach alpha coefficient, given that this parameter should have values higher than 0.59 and lower than 0.95 [
10]. In addition, test-retest reliability was computed as acceptable and finally aiming to estimate the split-half reliability of our tool we found a strong positive correlation, which highlights our questionnaire acceptability[
12].
Despite the significance of the present study, the main limitation was the full absence of a valid and reliable instrument which investigate the same issue. Thereafter, it was inapplicable the examination of parameters such as the criterion, concurrent, and predictive validity of the “CVP Score” [
12,
13].
5. Conclusions
According to the validity and reliability analysis of our new-developed questionnaire, this tool is a valid and reliable instrument that could be used to the critical care setting aiming to measure the extent in which critical care nurses use CVP measurements in their decision-making process for the optimal volume, hemodynamic and cardiovascular management of the critically ill patients. It seems that ICU clinician and researchers could be used “CVP Score” to add new data to the above-mentioned limited body of knowledge. Our study significance could be underlying by the originality of the evaluated tool, taking into account that it is the first one to serve the above-mentioned research purpose. Although, based on the current literature, the value of CVP measurement as a reliable index of cardiovascular and intravascular blood volume status, which can guide the fluid administration therapy and predict fluid responsiveness is controversial, the measurement of CVP remains a standard professional skill and responsibility of ICU clinicians, including critical care nurses. Our study limitations show that further research is needed with using the “CVP Score” on greater samples and in different countries and healthcare systems.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org.
Author Contributions
Conceptualization, K.G.; methodology, K.G. and A.P.; software, K.G. and M.Z.S.; validation, K.G. and A.A.C; formal analysis, K.G.; investigation, K.G., A.P., N.V.F and M.Z.S; data curation, E.P, A.P and N.V.F..; writing—original draft preparation, K.G.; writing—review and editing, K.G. and A.A.C.; supervision, K.G. and E.P.; project administration, K.G. All authors have read and agreed to the published version of the manuscript
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of General Hospital of Athens ¨Evaggelismos¨ (234/18-07-2018) and University Hospital of Larisa (36382/31-07-2018).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patients to publish this paper.
Conflicts of Interest
The authors declare no conflict of interest.
References
- De Backer, D., & Vincent, J.L. Should we measure the central venous pressure to guide fluid management? Ten answers to 10 questions. Critical Care 2018, 22, 43. [CrossRef]
- Guarnieri, M., Belleti, A., Saglietti, F., & Bignami, E. Central venous pressure as a predictor of fluid responsiveness. Is this all you need? General Medicine (Los Angeles) 2016, 4, 1000228. [CrossRef]
- Sondergaard, S., Parkin, G., & Aneman, A. Central venous pressure: soon an outcome-associated matter. Current Opinion in Anaesthesiology 2016, 29, 179–185.
- Cecconi, M., & Aya, H.D. Central venous pressure cannot predict fluid-responsiveness. Evidence Based Medicine 2014, 19, 63. [CrossRef]
- Cecconi, M., De Backer, D., Antonelli, M., Beale, R., Bakker, J., Hofer, C., Jaeschke, R., Mebazaa, A., Pinsky, M.R., Teboul, J.L., Vincent, J.L., & Rhodes, A. Consensus on circulatory shock and hemodynamic monitoring. Task force of the European Society of Intensive Care Medicine. Intensive Care Medicine 2014, 1795–1815. [CrossRef]
- Roger, C., Muller, L., Riou, B., Molinari, N., Louart, B., Kerbrat, H., Teboul, J.L., & Lefrant, J.Y. (2017). Comparison of different techniques of central venous pressure measurement in mechanically ventilated critically ill patients. British Journal of Anaesthesia 2017, 118(2), 223–231. [CrossRef]
- Official Government Gazette of the Hellenic Republic, Second Issue. (2022). Responsibilities and duties of the National Healthcare System and the public primary healthcare system Registered Nurses.
- Dellinger, R.P., Levy, M.M., Rhodes, A., Annane, D., Gerlach, H., Opal, S.M., Sevransky, J.E., Sprung, C.L., Douglas, I.S., Jaeschke, R., Osborn, T.M., Nunnally, M.E., Townsend, S.R., Reinhart, K., Kleinpell, R.M., Angus, D.C., Deutschman, C.S., Machado, F.R., Rubenfeld, G.D., Webb, S., Beale, R.J., Vincent, J.L., & Moreno, R.; Surviving Sepsis Campaign Guidelines Committee including The Pediatric Subgroup. Surviving Sepsis Campaign: international guidelines for management of severe sepsis and septic shock. Intensive Care Medicine 2013, 39, 165–228. [CrossRef]
- Osman, D., Ridel, C., Ray, P., Monnet, X., Anguel, N., Richard, C., & Teboul, J.L. Cardiac filling pressures are not appropriate to predict hemodynamic response to volume challenge. Critical Care Medicine 2007, 35, 64–68. [CrossRef]
- Marik, P.E., Baram, M., Vahid, B. Does central venous pressure predict fluid responsiveness? A systematic review of the literature and the tale of seven mares. Chest 2008, 134, 172–178. [CrossRef] [PubMed]
- Kimberlin, C.L., & Winterstein, A.G. Validity and reliability of measurement instruments used in research. American Journal of Health-System Pharmacy, 2008, 65, 2276–2284. [CrossRef]
- Galanis, P. [Ed.]. (2017). Research methodology in health sciences. Kritiki editions.
- Chobanian, A.V., Bakris, G.L., Black, H.R., Cushman, W.C., Green, L.A., Jr Izzo, J.L., Jones, D.W., Materson, B.J., Oparil, S., Jr Wright, J.T., & Rocella, E.J. Seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure. Hypertension 2003, 42, 1206–1252.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).