Introduction
Rectal prolapse is a relatively rare pelvic floor surgical disorder, which mainly manifests as downward displacement of the anal canal, rectal mucosa, full rectum or part of the sigmoid colon, and prolapse out of the anus. Among them, the prolapse of the whole rectum or even part of the sigmoid colon out of the anus is called complete rectal prolapse (CRP) [
1] (
Figure 1). Although CRP is a benign disease, long-term recurrent CRP may damage the nerves in the pubic area and cause symptoms such as fecal incontinence and urinary incontinence, which can seriously affect the quality of life of patients [
2]. In general, the occurrence of CRP is closely related to several anatomical abnormalities around the pelvic floor, including deep pelvic floor peritoneal reflexion, redundant sigmoid colon, sacro-rectal separation, pelvic floor descent, and anal sphincter function. Therefore, how to correct the above anatomical defects becomes the key to treat CRP. The choice of the way to correct the anatomical defects also becomes the top priority in the treatment of CRP.
The clinical treatment of CRP mainly includes conservative and surgical treatment. The conservative treatment method is based on the application of cathartic agents and bowel control. However, this method does not correct the anatomical defects of CRP at the root. Long-term application of conservative therapy not only reduces anal function, but also increase the postoperative recurrence rate [
3]. Surgery is the primary and effective treatment for CRP; however, due to the low incidence of CRP (2%-4%) and patient heterogeneity, conventional CRP surgery has failed to achieve the desired therapeutic effect [
4,
5]. The complication rate after traditional Altemeier is as high as 60%, and some patients may also suffer serious complications such as anastomotic leakage, fecal incontinence, and even death after surgery [
6]. Therefore, individualized and precise treatment of CRP patients should be based on anatomical defects, patient health status and operator experience to effectively reduce recurrence, complications and mortality of CRP.
The Altemeier procedure, as one of the representative transperineal approaches, has been widely used since the 1970's. Altemeier et al. [
7] concluded that the Altemeier procedure has the advantages of being less invasive, applicable to a wider population, and requiring less anesthesia; The Altemeier procedure is less risky, but the postoperative recurrence rate varies widely in the literature, with historical reports of a 58% recurrence rate after the Altemeier procedure, so the procedure is now mostly indicated for older patients or those with multiple comorbidities[
8] .
In their long-term clinical practice, the authors found that patients with CRP may have a drastic change in diameter at the site of intestinal lumen ligature, an anatomical abnormality that has not yet been reported. The weakness of the distal bowel wall at the site of ligature results in poor resistance to high abdominal pressure during defecation, and conventional Altemeier surgery that does not completely correct the difference in bowel lumen diameter may lead to re-ligature and recurrence of CRP. To improve the above anatomical abnormalities, a modified Altemeier procedure is described in the present study. In this study, we performed either conventional Altemeier or modified Altemeier surgery in the 60 patients with CRP included, and summarized and analyzed the clinical outcomes. We hypothesized that the surgical efficacy of modified Altemeier surgery for CRP was superior to that of conventional Altemeier surgery. Through this retrospective analysis, we compared the clinical indicators of recurrence rate, complication rate, postoperative anal function and quality of life between conventional and modified Altemeier surgery to verify our hypothesis and provide a reference for the selection of surgical modality for CRP patients.
1. Materials and Methods
1.1. Subjects
Retrospective analysis of 60 patients with CRP admitted to our department from August 2019 to August 2022. These patients were all first-time participants in rectal prolapse surgery. Patients were randomly assigned to the Altemeier group (traditional group) and the modified Altemeier group (modified group). A total of 30 patients were included in the conventional group, of whom 19 were male and 11 were female. The age of the patients ranged from 16-87 years, with a mean of (42.47±20.505) years. The length of rectal prolapse in traditional group was 5-20 cm, with a mean of (8.27±4.034) cm; the duration of the disease was 1-60 years, with a mean of (16.8±18.643) years. In the modified group, there were 30 patients, including 21 males and 9 females; all patients were 17-82 years old, with a mean of (44.60±18.205) years; the length of rectal prolapse was 5-20 cm, with a mean of (10.6±3.607) cm. The duration of the disease was 1-60 years, with a mean of (27.13±18.643) years. The general data (gender, age, duration of disease, and length of prolapse,
Table 1) were statistically compared between the two groups of patients. The differences in gender and age under different groups were not statistically significant (P > 0.05), i.e., there were no significant differences in gender and age between the traditional and modified groups, but the differences in the time of anal mass prolapse and the maximum prolapse length in squatting position between the two groups were statistically significant.
1.2. Inclusion and exclusion criteria:
Inclusion criteria: (1) All patients had total rectal prolapse, with prolapse visible when pulling on the anus or during stool, and all had CRP grading criteria at the level of Oxford prolapse grade 5 [
9] (
Figure 2). All cases were diagnosed in accordance with the American Association of Colorectal Surgeons guidelines for the treatment of rectal prolapse; (2) The included patients were suitable for both surgical procedures. All cases had completed preoperative e-colonoscopy, blood biochemistry, cardiopulmonary and other ancillary tests, and there were no obvious contraindications to surgery; (3) Patients and their families were informed of the study content and signed an informed consent form; (4) Patients cooperated with the follow-up.
Exclusion criteria: (1) Patients with combined proctitis, ulcerative colitis, Crohn's disease, oncological diseases or autoimmune diseases; (2) Patients with combined severe cardiovascular and cerebrovascular diseases; (3) Patients who are pregnant or lactating; (4) Patients with incomplete recording or completion of medical history data; (5) Patients who cannot understand or fully cooperate with the questionnaire; (6) Patients with psychiatric abnormalities or concomitant psychiatric diseases.
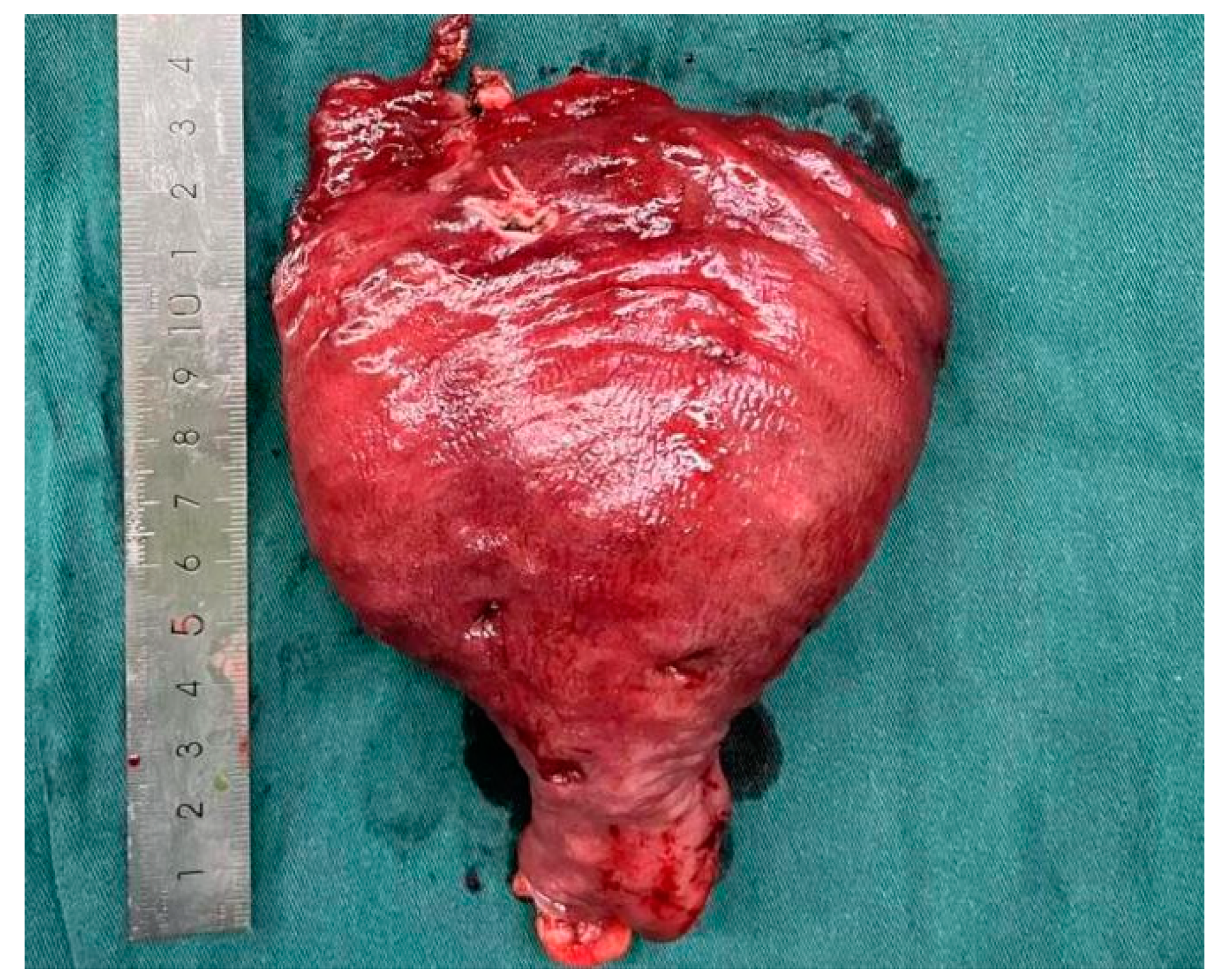
1.3. Detection of novel abnormal anatomical structures
After intraoperative resection of the specimen, the distal and proximal diameters were measured using a specimen measuring tape to determine the distal and proximal diameters. (
Figure 5)
1.4. Preoperative preparation and surgical procedure
Routine bowel preparation was performed preoperatively, and the surgery was performed under general anesthesia and in the lithotomy position. Both procedures are performed by the same surgeon. The specific surgical operations in each group were as follows:
The traditional Altemeier procedure is performed as described previously [
10]. In brief,the patient is placed in a lithotomy position and the dentate line is fully exposed. One traction suture is placed at each of the perianal positions 3, 6, 9 and 12 to retract the anus. The prolapsed bowel is retracted with forceps. The rectum is circumferentially incised with an ultrasonic knife 2-3 cm proximal to the dentate line, and the rectal mesentery and prolapsed intestinal canal are freed along the rectal wall. The descending pelvic floor peritoneum is opened in front of the rectum to free the prolapsed inner rectum and part of the sigmoid colon; then, the excess pelvic floor peritoneum is released and removed upward, and the upper pelvic floor peritoneum is sutured to the anterior wall of the rectum or colon for the purpose of pelvic floor reconstruction; finally, a traction line is sutured at the proximal end of the colon to prevent retraction, and the free intestine is pulled outward to the anus to the maximum extent. In a tension-free state, the proximal intestinal canal was selected to be severed at a distance of about 3 cm from the outside of the anus, and then a full end-to-end anastomosis between the colon and the anal canal was performed.
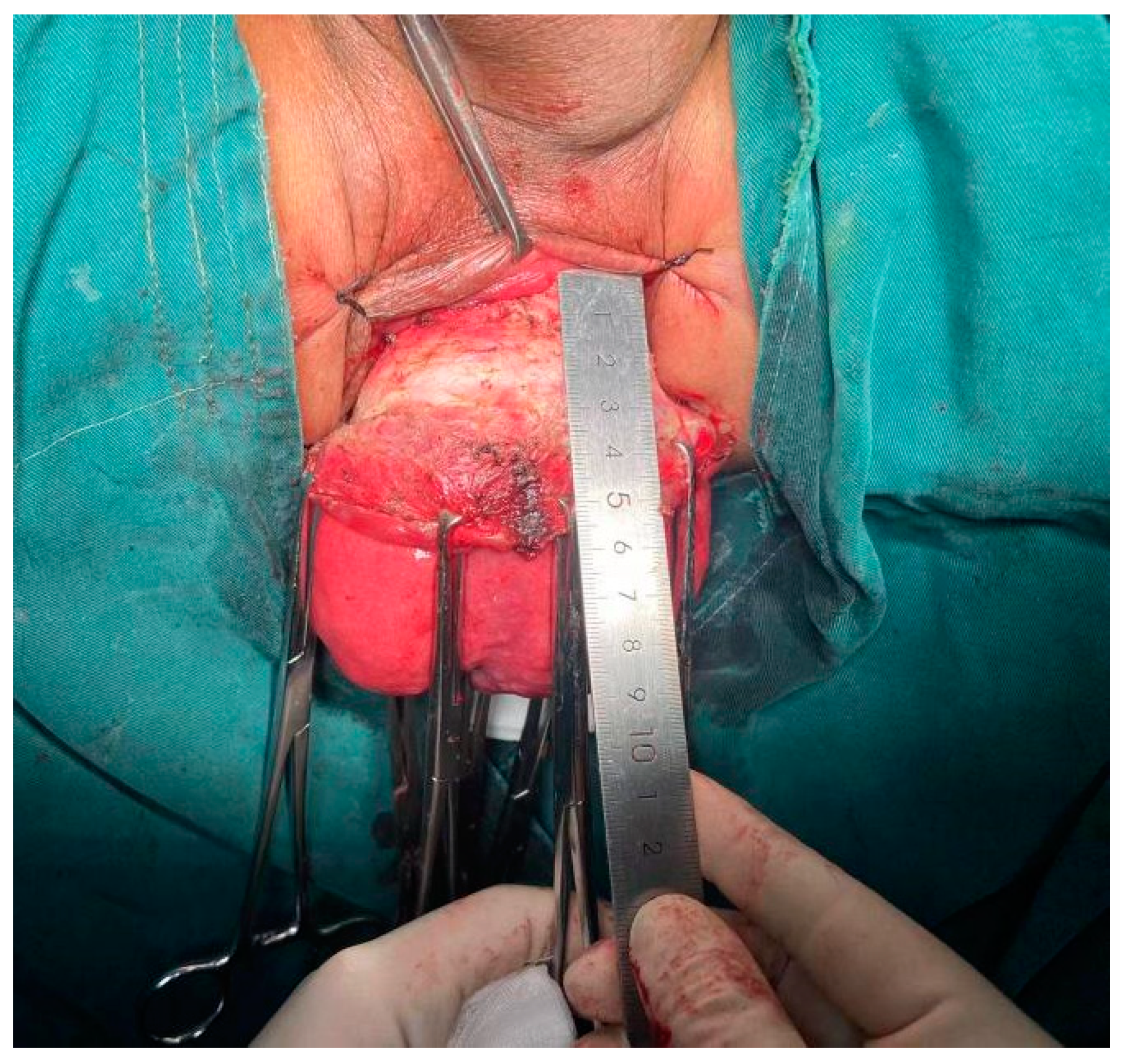
Modified Altemeier operation procedure:
The patient is placed in a lithotomy position and 6 stitches are placed in the perianal area to distract the anus and fully expose the surgical area. The prolapsed intestine was dragged out of the anus to the maximum length that could be dragged out (
Figure 2). The electric knife marks the pre-cut line at 1-1.5 cm proximal to the dentate line, and the ultrasonic knife incises the rectal mucosa along the marked line to the outer circular muscle layer of the intestinal wall. About 2 cm of the submucosal circular muscle layer was tubularly freed along the surface of the submucosa proximally, and this part of the myosheath was preserved (
Figure 3). The anterior rectal wall proximal to the preserved myosheath was dissected along the muscle layer using the ultrasonic knife. The peritoneum is opened and the deepened rectal bladder or recto-uterine trap is expanded on both sides using an ultrasonic knife. Two stitches of traction with a 7 suture are placed in the appropriate position to prevent retraction. The posterior lateral rectal outer layer is opened along the marked line. The prolapsed outer layer is turned downward. The rectosigmoid colon is retracted outward toward the anus to the maximum and the appropriate rectal mesentery is preserved. Adequate freeing along the intestinal wall. Reconstruct and elevate the pelvic floor by adequately elevating and closing the rectal bladder or recto-uterine trap with 3-0 absorbable thread. The posterior pelvic floor muscle and anal raphe were folded and sutured with 2-0 absorbable sutures to narrow the triangular gap behind the anus, inducing anterior displacement of the anus and sharpening of the rectus angle to achieve the effect of anal rapheplasty About 3-5 cm from the closed pelvic floor was selected as the proximal medial bowel resection line under tension-free condition. The proximal mesenteric pulpy muscle layer is interrupted with the preserved rectus muscle sheath ring muscle layer approximately 2 cm proximal to the pre-excision line. The proximal intestinal canal was then dissected along the pre-excision line.A 3-0 absorbable suture was used to perform an end-to-end anastomosis between the whole layer of the dissected intestinal canal and the rectal mucosal cut edge, so that the anastomosis was located in the myosheath (
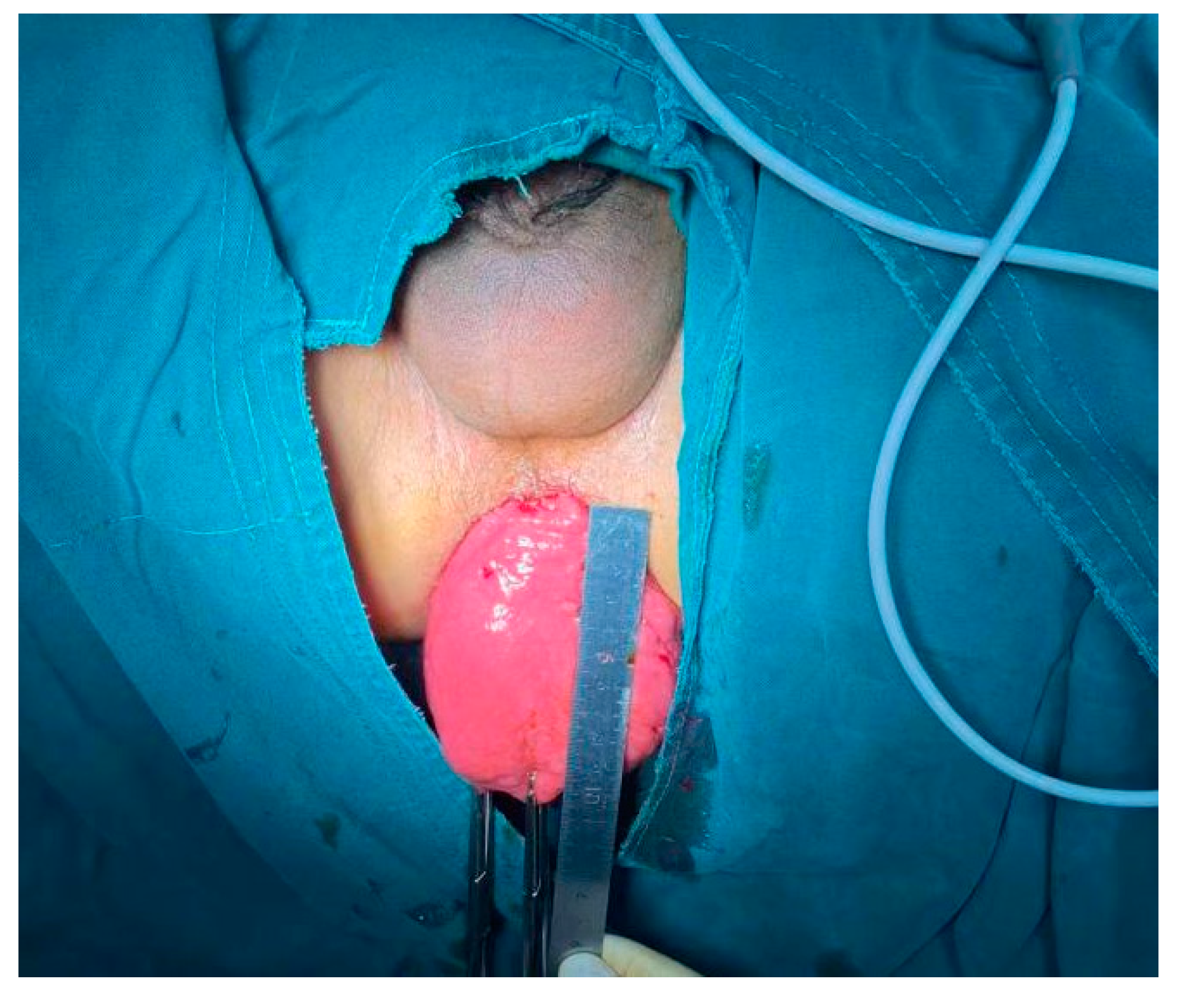
Figure 4). Close the triangular gap behind the anus to promote anterior displacement of the anus and sharpening of the rectus angle to achieve the effect of anal levatorplasty (
Figure 6)
Figure 3.
Separate the rectal mucosa layer by layer to the muscle layer. An ultrasonic knife is used to separate the rectal mucosa to the muscularis layer by layer along the marked line. Unlike the conventional procedure, the modified Altemeier procedure pays more attention to the preservation and protection of the muscular sheath.
Figure 3.
Separate the rectal mucosa layer by layer to the muscle layer. An ultrasonic knife is used to separate the rectal mucosa to the muscularis layer by layer along the marked line. Unlike the conventional procedure, the modified Altemeier procedure pays more attention to the preservation and protection of the muscular sheath.
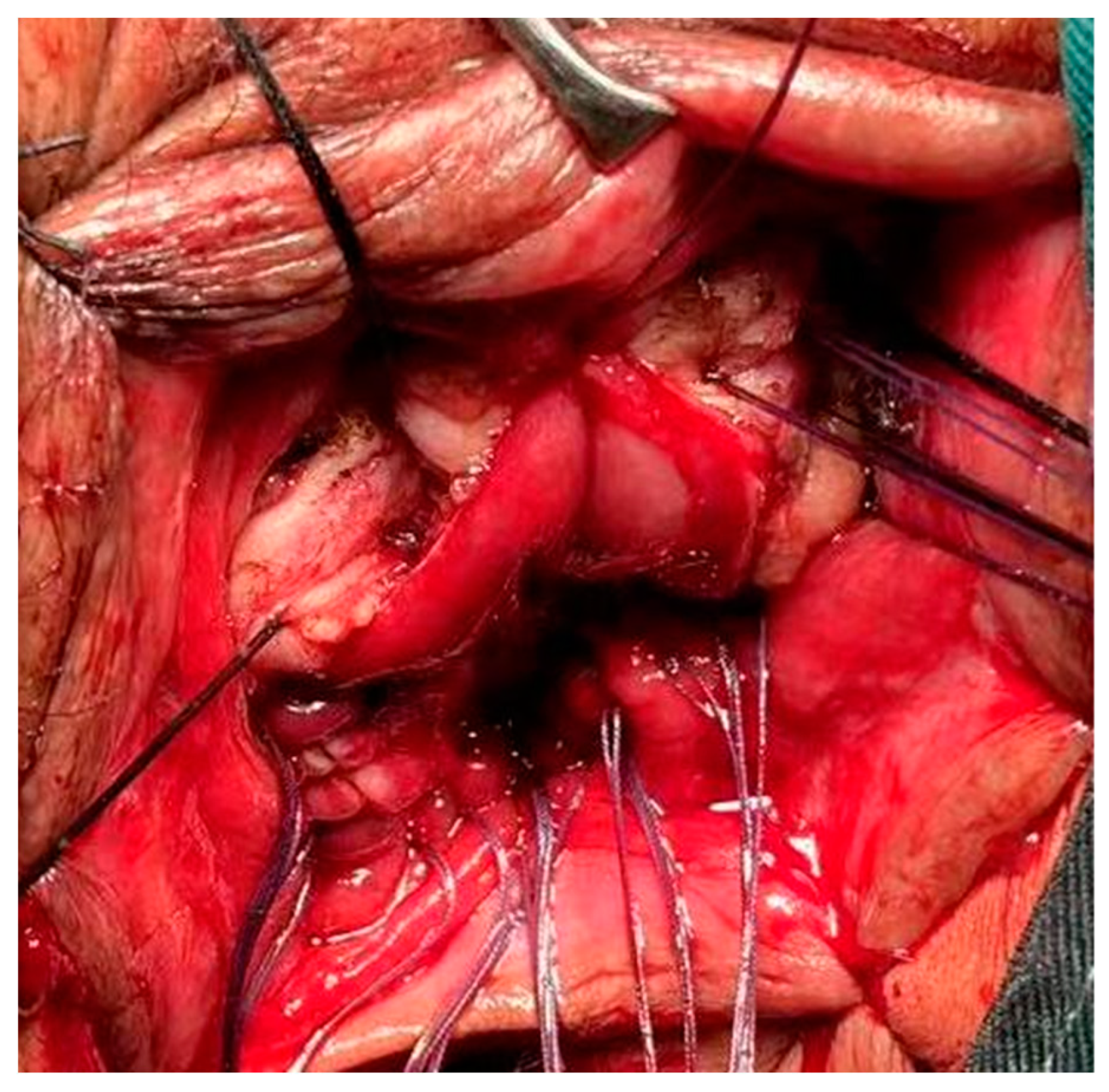
Figure 4.
Diagram of the anastomosis before and after the end of surgery. The modified Altemeier procedure requires interrupted sutures in the proximal intestinal plasma muscle layer and in the sphincter site within the rectal stump to allow the anastomosis to lie within the muscle sheath.
Figure 4.
Diagram of the anastomosis before and after the end of surgery. The modified Altemeier procedure requires interrupted sutures in the proximal intestinal plasma muscle layer and in the sphincter site within the rectal stump to allow the anastomosis to lie within the muscle sheath.
Figure 5.
Surgically resected rectal prolapse specimen. The anatomical defect of pathological dilatation of the distal rectum was presented in the surgical specimen.
Figure 5.
Surgically resected rectal prolapse specimen. The anatomical defect of pathological dilatation of the distal rectum was presented in the surgical specimen.
Figure 6.
Postoperative anal.
Figure 6.
Postoperative anal.
In both groups, an intra-anal drainage tube was left in place. Antibiotics were administered for 5-7 d after surgery, and a dregs-free liquid diet was started for 2 d. The semi-liquid diet was changed to a regular diet after 3 d. The drainage tube was removed after no drainage. Postoperatively, tylenol suppositories and tylenol cream were routinely given to protect the rectal mucosa. After discharge, follow-up and review were performed according to the prescribed schedule. No special postoperative rehabilitation, such as pelvic floor physiotherapy and bowel toning, was performed in either group.
1.5. Evaluation indicators and postoperative follow-up
The evaluation indexes included in this study included anal functional indexes and indexes related to surgical outcomes. Among them, the functional anal indexes mainly monitored the maximum prolapse length in squatting position, and compared the changes of Wexner anal incontinence score (0-20 points) and ED-5Q-5L quality of life autonomy score (total score of 100 points) before and after surgery; the surgical indicators mainly included the surgical method, operation time, intraoperative bleeding, occurrence of complications, hospitalization time, time and severity of postoperative recurrence. Follow-up records were established after patients were discharged from the hospital. Follow-up visits were conducted by telephone or outpatient follow-up at 6 and 12 months postoperatively, respectively. The follow-up included fecal excretion, the presence or absence of prolapse symptoms, and the length of prolapse, etc.
1.6. Statistical
SPSS 22.0 software was used for statistical analysis. Measurement data were described as x± s. Paired data T test was used to compare the means of two samples. Count data were statistically analyzed with chi-square test. P < 0. 05 was considered statistically significant.
2. Results
2.1. Comparison of perioperative index results between two groups of patients
The operation time of the traditional group was lower than that of the modified group, while the intraoperative blood loss was significantly higher than that of the modified group (
P < 0.05). There was no significant difference in the length of hospital stay between the two groups (
P>0.05). The differences in operation time (min) and intraoperative blood loss (ml) between the two groups were statistically significant (
P< 0.05,
Table 2).
2.2. Comparison of the incidence of postoperative complications between the two groups of patients
All patients enrolled in this study were followed up for a mean of 20 months. During the follow-up period, non-life-threatening complications occurred in both groups. During the perioperative period, three patients in the traditional group had anastomotic bleeding, three patients had anastomotic leakage, two patients had anal stenosis, and two patients had blood in the stool; one patient in the modified group had anastomotic hemorrhage and one patient had blood in the stool. The patients with anastomotic hemorrhage and anastomotic leak were treated with emergency surgery. One patient with anastomotic leak underwent prophylactic fistula. One case of anastomotic bleeding was found in the modified group, and the overall efficiency of treatment in the modified group was significantly better than that in the control group (
P < 0.05,
Table 2).
2.3. Changes in anal function and quality of life after surgery in two groups
No significant differences in the preoperative Wexner anal incontinence scores and ED-5Q-5L quality of life autonomy scores between the two groups (
P>0.05). However, postoperative Wexner anal incontinence scores and ED-5Q-5L quality of life autonomy scores were significantly lower in the modified group than in the traditional group (
P<0.001,
Table 3).
2.4. Comparison of postoperative recurrence rate between two groups of patients
The postoperative recurrence rate was 26.67% (8/30) in the traditional group and 7% (1/30) in the modified group (
P<0.05). The postoperative recurrence rate in the traditional group was significantly higher than that in the modified group, and the difference was statistically significant (
P<0.05). 2 patients (6.67%) in the traditional group recurred at 6 months postoperatively without improvement of prolapse symptoms or aggravation; 6 patients (20%) recurred after 2, 4 and 7 months postoperatively, respectively. The prolapse symptoms in the above patients were improved compared with the previous. The patients with recurrence in the modified group recurred 8 months after surgery, and the length of prolapse was reduced from 8 cm before surgery to 0.5 cm (
Table 4). The difference in recurrence under different groups was statistically significant (P<0.05), i.e., there was a significant difference in recurrence between the traditional and modified groups.
3. Discussion
CRP is a relatively rare pelvic floor disorder in colorectal surgery, and currently the main surgical approach is to reduce symptoms while correcting the primary factors of CRP. Traditional surgery is subdivided into transabdominal and transperineal approaches. The perineal Altemeier procedure is more common, but the traditional Altemeier procedure can only correct some of the anatomical defects of CRP, and the rectum is still prone to "sliding" after surgery [
11]. The present study points out that the reasons for the poor efficacy of conventional Altemeier procedure may be (1) the operator's irregular operation and incomplete correction of the anatomical defects of CRP; (2) the possible existence of new anatomical defects and pathogenesis of CRP have not been discovered. We found that in addition to the long sigmoid colon, deep Douglas concavity, insufficient fixation of the rectum to the sacrum (vertical rectum), and loose perirectal tissue support (cavernous anus and detached anal levator muscle), CRP may also have another anatomical abnormality – pathological dilated of distal rectal (
Figure 2). Prolonged passive dilatation of the distal segment of the prolapsed bowel can lead to damage and degeneration of the muscle fibers of the intestinal wall and thinning of the intestinal wall, which may eventually lead to postoperative complications and recurrence. We improved the traditional procedure by not repairing the pelvic floor defect, unstable rectal fixation and uneven tension of the sutured pelvic floor peritoneal anastomosis, and proposed for the first time to lower the resection plane, "sleeve" anastomosed and combined anal levator plication. The results of the study showed that the modified Altemeier procedure significantly improved the clinical outcome of CRP.
The Alemeier procedure, although less risky and safer, has been controversial because of its high postoperative recurrence rate [
12,
13]. Chun et al. [
14] found a postoperative recurrence rate of 20.6% in a retrospective analysis of 109 patients who underwent the Altemeier procedure for rectal prolapse; similarly, in this study, the recurrence rate of the traditional group was 26.67%, of which 13.3% did not show any improvement in prolapse symptoms. The traditional view is that recurrence may be related to the experience of the operator, the length of the resected bowel segment and the type of anastomosis [
15]. This study further suggests that the weakness of the rectal or sigmoid bowel wall in CRP patients to resist abdominal pressure and the failure to correct the distal dilated bowel in the traditional procedure may also be another important cause of recurrence. To effectively prevent the recurrence rate after surgery, the focus should be on completely correcting the anatomical defects of CRP, reinforcing the pelvic floor peritoneum and selecting the appropriate anastomosis. In the present study, no recurrence of the modified Altemeier procedure was observed during a mean follow-up of 20 months, although one patient developed rectal mucosal prolapse at 8 months after surgery, and the length of prolapse was only 0.5 cm. we believe that rectal mucosal prolapse is a postoperative complication of Altemeier and should not be considered as a recurrence of CRP. And the postoperative recurrence rate of patients in the modified Altemeier group was significantly lower than that of the conventional group (26.67%), confirming the advantage of modified Altemeier in reducing the postoperative recurrence rate. However, the present study was only a single-center, small sample, short-term follow-up, and there was a lack of long-term follow-up results over 10 years, so it is difficult to accurately confirm whether the modified Altemeier procedure can completely avoid postoperative recurrence, and the true recurrence rate needs to be further verified by multi-center, large sample and long-term follow-up.
Altemeier procedure avoids the risks and complications of transabdominal surgery, but the complication rate is still in the range of 10%-20% [
16]. Major complications include anastomotic tear, pelvic infection, and anastomotic bleeding. In the current study, complications related to the anastomosis were observed in both groups, which is consistent with the results of previous studies. However, the incidence of postoperative complications after conventional Altemeier procedure (33.33%), was significantly higher than the results of historical literature studies (10%-20%)[
16]. However, the previous report was a multicenter, large sample and other population study, but the present study was a simple study, and the total sample size of the two studies was different, so the bias in the results was normal. In this study, we point out that Altemeier procedure involves total resection of the rectum and low colon-anal anastomosis, so the key to preventing complications is the anastomotic approach, intraoperative selection of the pre-excision line and determination of the superior incisional margin. The modified Altemeier procedure requires the operator to use the proximal medial bowel as a preexcision line about 3-5 cm from the closed pelvic floor in a tension-free manner, and to perform a "sleeve" double-layer manual anastomosis at the severed end so that the anastomosis is surrounded by anal sphincter, anal levator, and pelvic floor muscles. The anastomotic scar and aseptic inflammatory reaction can make the rectal mucosa firmly fixed in the muscle layer. While enhancing the protection of the anastomosis, this operation solves the problem of difficulty in dilating the lower rectal loop, thus reducing the complications associated with the anastomosis in the traditional procedure. The results of this study showed a significant reduction in the overall complication rate of patients in the modified group compared to the conventional group. Only one of the patients had bleeding from anastomotic dehiscence due to premature defecation, and there was no recurrence 12 months after hemostasis and suturing again. Thus, the modified Altemeier procedure was relatively safe. To further prevent postoperative complications and ensure patient safety, we suggest that for high-risk patients such as those with high anastomotic tension, the time to the first postoperative bowel movement can be appropriately controlled and a prophylactic ileostomy can be performed to temporarily transfer the stool [
17].
The hallmark of successful CRP treatment is not only a lower recurrence and complication rate, but also the restoration of normal anorectal function and improvement of patients' quality of life. The modified Altemeier procedure reported in this study preserves more of the muscle sheath by choosing to remove more of the mucosa than the length of the intestinal canal, avoiding obstruction to the passage of bowel contents and improving the damage to the anorectal ring and pelvic floor muscles caused by the conventional procedure. In addition, the modified Altemeier procedure is chosen to "sleeve" the anastomosis at the severed end, which not only preserves the normal elasticity and compliance of the rectal wall, but also further reduces the terminal intestinal cavity, making the anal cushion tight and facilitating the recovery of anorectal function. This approach can significantly improve the patient's fecal symptoms such as anal incontinence and constipation. Finally, the modified Altemeier procedure was combined with anal levatorplasty to close the posterior anal triangle gap, correct the anatomical defect of anal levator separation, induce anterior displacement of the anus, sharpen the anorectal angle, and restore the normal structure of the anorectum, which plays a more active role in preventing fecal incontinence caused by prolapse [
18]. In this study, not only the Wexner score was significantly lower in the modified group than in the traditional group, but also the postoperative quality of life score and the incidence of perioperative complications were significantly lower than that in the traditional group, suggesting that the modified Altemeier has significant advantages in terms of both improving the treatment effect and reducing complications. Although the operation time was longer in the modified group, the operation was more delicate and accurate, which not only reduced intraoperative bleeding but also provided a basis for rapid postoperative recovery. Even though the Wexner scores and quality of life scores selected for this study were subjective overall patient scores, which to some extent reduced the influence on the authenticity of the study due to misinformation and shame; however, there was a lack of objective evaluation indexes of anal function such as defecography and anorectal manometry before and after surgery in the patients included in this study. The shortcomings of the above study also point out the direction for our future research on CRP.
In conclusion, pathological distal rectal dilatation may be an important anatomical alteration of CRP. In this study, the traditional Altemeier procedure was modified and improved based on this anatomical abnormality, with the aim of completely repairing the anatomical defects of CRP, compensating for the many technical defects of the traditional procedure, and improving the treatment outcome of CRP. However, this study lacked objective indicators such as defecography and anorectal manometry to assess the effects of different procedures on anal function. Future bulk, multicenter, randomized controlled studies are needed to further confirm the long-term efficacy of the modified Altemeier procedure for CRP.
Conclusion
Altemeier procedure is an effective surgical modality for the treatment of CRP, but suffers from high recurrence and complication rates. The present clinical study confirmed that pathological distal rectal dilatation is another anatomical defect of complete rectal prolapse. The modified Altemeier procedure was able to improve the outcome of CRP by improving this anatomical defect. By comparing the clinical indexes of patients in the traditional and modified groups, the clinical effectiveness and safety of the modified Altemeier procedure were confirmed, which has high clinical application value.
Authors’ contributions
L.Z. and Y.T. contributed the central idea, analysed most of the data, and wrote the initial draft of the paper. The remaining authors contributed to refining the ideas, carrying out additional analyses and finalizing this paper.Yuze Zhai conceived of the study, designed the study and collected the data. All authors analysed the data and were involved in writing the manuscript.
Funding/Support
None reported.
Acknowledgments
The authors thank all the participants of this study. First of all, we thank Professor Ding Ke for his early efforts in the treatment of rectal prolapse, and we also thank the anorectal doctors and nurses (Xiaoxia Sun, Liwei Yan, Chao Gu, Liyue Han, and Yumei Gao) for their help. All studies conducted in this study involving participants were conducted in accordance with the ethical standards of the Medical Ethics Committee of the Affiliated Hospital of Shandong University of Traditional Chinese Medicine and the 1964 Declaration of Helsinki and its subsequent amendments or similar ethical standards. In this study, we obtained written informed consent from the participants themselves.
Disclaimers
There is no conflict of interest among the authors.
References
- Gleditsch D, Wexels WA, Nesbakken A. Surgical options and trends in treating rectal prolapse: long-term results in a 19-year follow-up study. Langenbecks Arch Surg. 2018;403(8):991-998. [CrossRef]
- Trompetto M, Tutino R, Realis Luc A, Novelli E, Gallo G, Clerico G. Altemeier's procedure for complete rectal prolapse; outcome and function in 43 consecutive female patients. BMC Surg. 2019 Jan 3;19(1):1. PMID: 30606166; PMCID: PMC6318906. [CrossRef]
- Cunin D, Siproudhis L, Desfourneaux V, et al. No surgery for full-thickness rectal prolapse: what happens with continence?. World J Surg. 2013;37(6):1297-1302. [CrossRef]
- Pemberton JH. Anorectal and pelvic floor disorders: putting physiology into practice. J Gastroenterol Hepatol. 1990;5 Suppl 1:127-143. [CrossRef]
- Ng ZQ, Levitt M, Tan P, Makin G, Platell C. Long-term outcomes of surgical management of rectal prolapse. ANZ J Surg. 2019;89(6):E231-E235. [CrossRef]
- Shin EJ. Surgical treatment of rectal prolapse. J Korean Soc Coloproctol. 2011;27(1):5-12. [CrossRef]
- Altemeier WA, Culbertson WR, Schowengerdt C, Hunt J. Nineteen years' experience with the one-stage perineal repair of rectal prolapse. Ann Surg. 1971;173(6):993-1006. [CrossRef]
- Ris F, Colin JF, Chilcott M, Remue C, Jamart J, Kartheuser A. Altemeier's procedure for rectal prolapse: analysis of long-term outcome in 60 patients. Colorectal Dis. 2012 Sep;14(9):1106-11. PMID: 22150996. [CrossRef]
- Collinson R, Cunningham C, D'Costa H, Lindsey I. Rectal intussusception and unexplained faecal incontinence: findings of a proctographic study. Colorectal Dis. 2009;11(1):77-83. [CrossRef]
- Sakata S, McKenna NP, Allawi A, D'Angelo AD, Chua HK, Dozois EJ. How to do an Altemeier perineal rectosigmoidectomy for full-thickness rectal prolapse. ANZ J Surg. 2021 May;91(5):1019-1020. Epub 2021 Jan 18. PMID: 33458932. [CrossRef]
- Trompetto M, Tutino R, Realis Luc A, Novelli E, Gallo G, Clerico G. Altemeier's procedure for complete rectal prolapse; outcome and function in 43 consecutive female patients. BMC Surg. 2019;19(1):1. Published 2019 Jan 3. [CrossRef]
- Cirocco WC. The Altemeier procedure for rectal prolapse: an operation for all ages. Dis Colon Rectum.2010;53(12):1618-1623. [CrossRef]
- Tsunoda A, Yasuda N, Yokoyama N, Kamiyama G, Kusano M. Delorme's procedure for rectal prolapse: clinical and physiological analysis. Dis Colon Rectum. 2003;46(9):1260-1265. [CrossRef]
- Chun SW, Pikarsky AJ, You SY, et al. Perineal rectosigmoidectomy for rectal prolapse: role of levatorplasty. Tech Coloproctol. 2004;8(1):3-9. [CrossRef]
- Kim M, Reibetanz J, Schlegel N, et al. Recurrence after perineal rectosigmoidectomy: when and why?. Colorectal Dis. 2014;16(11):920-924. [CrossRef]
- Rothenhoefer S, Herrle F, Herold A, et al. DeloRes trial: study protocol for a randomized trial comparing two standardized surgical approaches in rectal prolapse - Delorme's procedure versus resection rectopexy. Trials. 2012;13:155. Published 2012 Aug 29. [CrossRef]
- Samalavicius NE, Kavaliauskas P, Simcikas D, Dulskas A. Altemeier procedure for full-thickness rectal prolapse complicated by ischaemic stricture - a video vignette. Colorectal Dis. 2020;22(7):842-843. [CrossRef]
- De la Torre L, Zornoza-Moreno M, Cogley K, et al. Transanal endorectal approach for the treatment of idiopathic rectal prolapse in children: Experience with the modified Delorme's procedure. J Pediatr Surg. 2019;54(4):857-861. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).