INTRODUCTION:
The introduction of 3D radiographic examinations into dentistry has allowed, through computerized image processing, an increasingly simplified and precise organization of surgical procedures. (1,2) In implantology it’s a priority to establish where to place the implants and what angle to give them. The 3D exam allows the clinician to evaluate sections of the upper jaw or mandible to decide with extreme precision where to insert the fixtures. The volumetric RX investigation, also, allows the use of computer data in order to develop three-dimensional objects, thanks to the 3D printers widely used today. (3,4,5) The computerized management of clinical procedures can be carried out by surgical guides which give the dentist the possibility of inserting the implants with extreme precision guaranteeing predictable results ( 6,7,8). On the other hand, the creation of those guides, in some cases, could be an excessively complex and onerous solution when compared with the size of the edentulous site and the number of implants to be inserted. (9,10,11)
In the case of surgical interventions based on the freehand insertion technique, it is essential to interface and correlate the 3D radiographic investigations with the patient's clinical conditions in order to identify with certainty where to insert the fixtures; in the absence of adequate clinical reference points, such as the remaining teeth in the arch, this identification could turn out to be incorrect and therefore nullify the precision with which the implant sites were instead located on the 3D exam.
This risk of error is minimal in the case of monoedentulous sites thanks to the presence of the mesial and distal teeth close to the implant area and becomes increasingly greater as these dental references become distant. (12,13,14,15)
This study evaluated the precision with which the implant sites, on the patient's mucosa, are identified in different clinical conditions using a thermo-printed device that is easy and cheap to make and can also be used as a guide in identifying these areas.
MATERIALS AND METHODS.
This study is based on an experimental protocol, based on surgical templates to be built on diagnostic dental cast, to be worn by the patient during the 3D exam, in order to verify the accuracy of the clinical identification of the implant site on the mucosa in procedures without surgical guides.
Twenty-two patients with partial edentulism were selected for which prosthetic rehabilitations with single or multiple implants were planned. Alginate impressions were taken on all patients, in order to obtain cast models, as well as preliminary orthopantomographic x-ray examinations.
By interfacing clinical and orthopantomographic data, a preliminary decision was made where the implants could potentially be located. This preliminary decision made it possible to mark on the cast model, using a felt-tip pen, the site where to locate any single fixture.
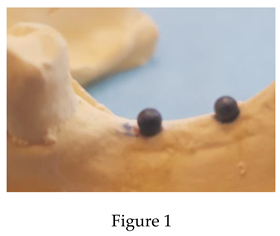
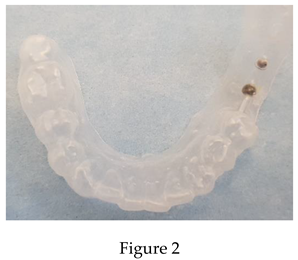
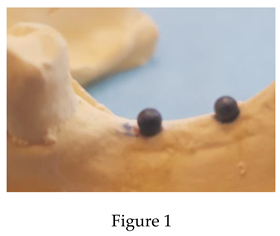
For each patient, on the cast models, exactly in the points marked by the marker, steel spheres with a diameter of 2 millimeters were glued using cyanoacrylate. On those cast models thus modified, thermo-printed templates were made with 0.5 mm thick sheets of soft consistency. These templates, during the hot thermoforming, detached and incorporated the tiny spheres previously placed, so as to represent precise radio-opaque landmarks integral with the devices themselves.
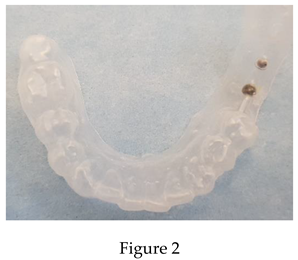
All templates have been finished and regularized at the edges so that they can be comfortably worn by the patient during the 3D RX exam without causing obstacles to correct execution.
On the RX images, the metal spheres appear clearly visible in the hypothetical points where the fixtures could be inserted and given their very small size, the unwanted scatter effects in the RX images, normally caused by metal objects, were completely negligible and not have reduced the minimum quality and legibility of the exams.
By scrolling through the various sections of the 3D exam, the hypothetical positions where to place the implants were verified.
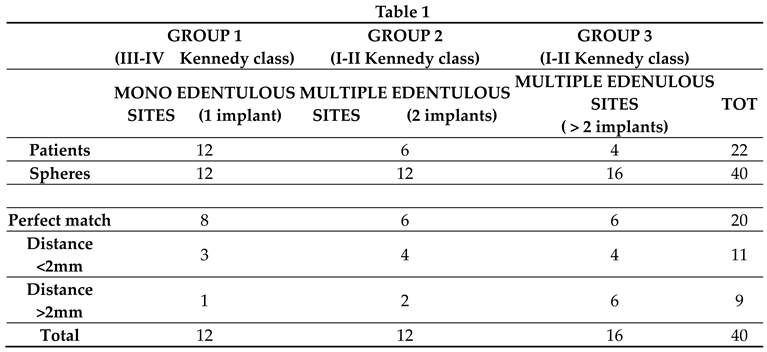
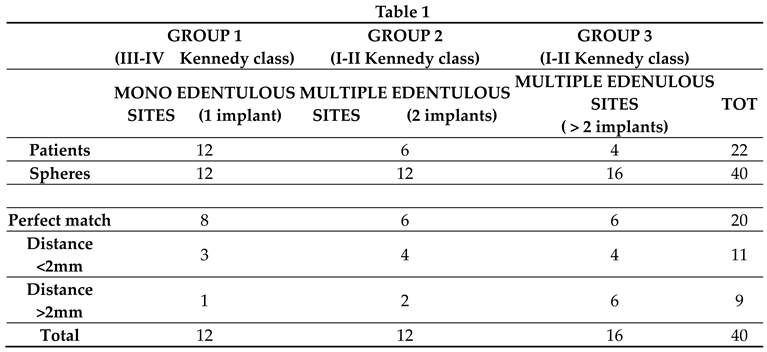
All 22 patients were further divided into 3 groups: 1) patients with monoedentulous intercalated sites (type III or IV Kennedy class); 2) patients with distal edentulism of 3 teeth and planning of 2 implant fixtures (type I or II class Kennedy). 3) patients with distal edentulism where more than 3 teeth were missing and planning of 3 or more implant fixtures (type I or II Kennedy class).
A total of 22 templates were thermoformed as follows: n. 12 templates relating to group 1 (with a single sphere), n. 6 templates for group 2 (with 2 spheres per template) and n. 4 templates for group 3 (with 3 or more spheres).
For each individual clinical case, the implantologist was asked to examine the 3D exam, identify the sections with the radiopaque spheres and then visit the patient to mark on the mucosa with an indelible marker (2 mm tip) where the sites had been selected for implant placement. Subsequently, the mask with the spheres was inserted on the single patient to compare its position with the points marked with the marker.
In case of mismatch, the distance between the metal ball and the dot on the mucosa was measured to quantify the error made by the implantologist.
In total, distributed among the various patients, the correspondences between the positions of 40 metal spheres and as many hypothetical implant sites identified with the marker on the mucosa were analysed.
The result of the measurements was coded in three possibilities: 0 error (precise correspondence between metal sphere and dot on the mucosa), minimum error (distance between metal sphere and dot <2mm), maximum error (distance between metal sphere and dot >2mm) .
RISULTS
In group 1 (monoedentulism) in 8 locations there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the sign on the mucosa indicated by the implantologist as the area of the future implant. A minimum error (<2mm) was found in 3 sites and a maximum error (>2mm) was recorded only in one case.
In group 2 (poliedentulism/2 implants) in 6 locations there was perfect correspondence between the sphere and the sign on the mucosa indicated by the implantologist as the area of the future implant. In 4 sites there was a minimum error (<2mm) and in 2 cases there was a maximum error (>2mm).
In group 3 (poliedentulism/>2 implants) in 6 locations there was perfect correspondence between the sphere and the sign on the mucosa. In 4 sites there was a minimum error (<2mm) and in 6 sites there was a maximum error (>2mm).
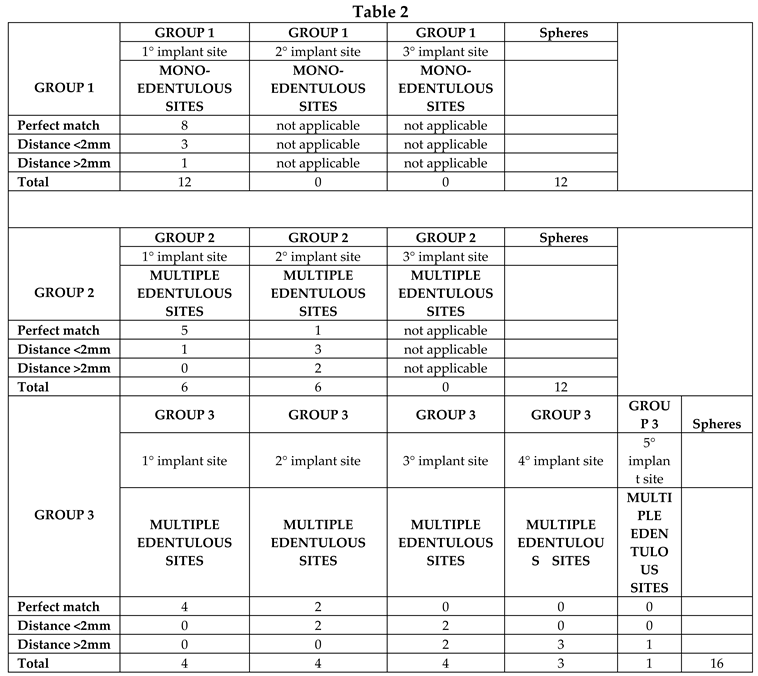
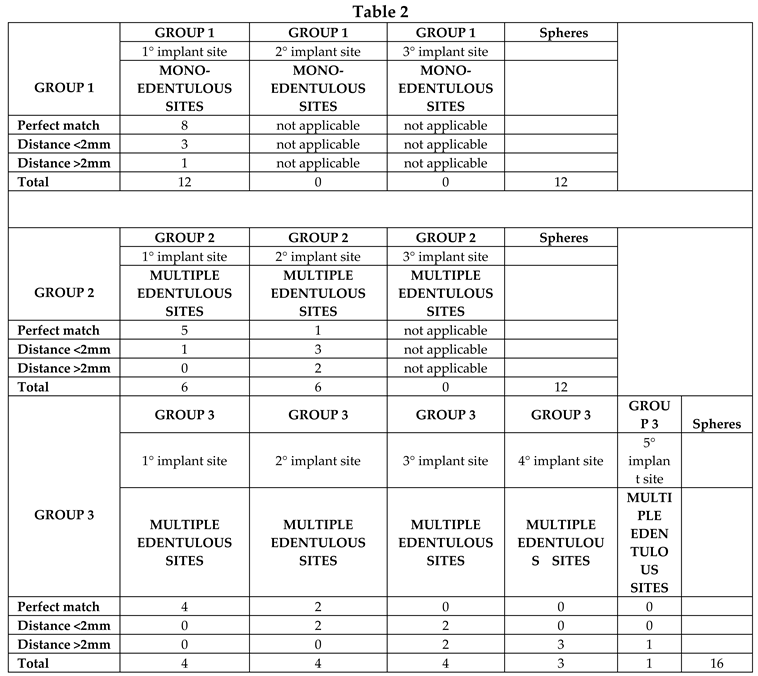
Within the single group, it was also assessed how much the distance between the presumed implant site and the neighboring teeth (which serve as the anatomical reference point for the clinical calculation of the correct position of the fixture) influenced the choices of the implantologist in marking the point on the mucosa. In groups 2 and 3 the mesial implant site (closest to the remaining natural tooth) was defined as the 1st implant site. The subsequent implant site (distal to the first) was defined as the 2nd implant site and so on for the 3rd and 4th implant site studied in this research.
In group 1, given that these are single fixture sites, the data are those already reported above.
In group 2, for the first implant site, in 5 cases there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the mark on the mucosa indicated by the implantologist as the site of the future implant. In one case there was a minimum error (<2mm) and in no case was there a maximum error (>2mm). For the second implant site, in one case there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the mark on the mucosa indicated by the implantologist as the site of the future implant. In 3 cases there was a minimum error (<2mm) and in 2 cases there was a maximum error (>2mm).
In group 3, for the first implant site, in 4 cases there was a perfect correspondence between the metal ball incorporated in the mask made to be worn by the patient and the mark on the mucosa. In no case was there a minimum error (<2mm) and in no case was there a maximum error (>2mm). For the second implant site, in 2 cases there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the mark on the mucosa indicated by the implantologist as the site of the future implant. In 2 cases there was a minimum error (<2mm) and in no case was there a maximum error (>2mm). For the third implant site, in 0 cases there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the mark on the mucosa indicated by the implantologist as the site of the future implant. In 2 cases there was a minimum error (<2mm) and in 2 cases there was a maximum error (>2mm). For the fourth implant site, in 0 cases there was a perfect correspondence between the metal sphere incorporated in the mask made to be worn by the patient and the mark on the mucosa indicated by the implantologist as the site of the future implant. In 0 cases there was a minimum error (<2mm) and in 3 cases there was a maximum error (>2mm). All data were subjected to statistical analysis.
DISCUSSION
From the data examined in this study, it’s clear that in certain clinical conditions, such as monoedentulism, it’s extremely easy to identify on the mucosa and then on the cortical bone where to position the implant. In these cases, the presence of the two contiguous teeth (mesial and distal) adjacent to the edentulous site offers the implantologist certain landmarks. When the presumed implant site is far from a natural teeth and when the latter are only on one side, as I or II Kennedy classes, precisely identifying the exact point where to start milling the bone could be a problem.
Our results show that it’s significant that in the 2nd, 3rd and 4th implant site respectively, as the distance from the last natural tooth in the arch increases, the error progressively increases.
In this study, for example, in group 3 (poliedentulism with more than 3 implants) at the level of the 4th implant site, the most distal to the natural tooth remaining in the arch, in 0% of cases there was a precise correspondence between the metal sphere and the point marked on the mucosa; similarly, always in group 3, at the level of the 4th implant site, in 100% of cases there was a maximum error (>2mm).
The same conclusion is reached if the data relating to group 2 are analysed, where more specifically the first implant site (the mesial one) presents data which can be superimposed on those relating to the single implant site of group 1; the second implant site (the most distal) instead has a greater margin of error but not as large as that of the third and fourth implant site of group 3.
This imprecision, due to the reduced ability of the human eye to evaluate distances as the reference anatomical landmark becomes more distant, often pushes the implantologist to use surgical templates which also give important indications on the angle to be given to the axis of the fixture. In clinically simple situations, such as monoimplant sites, surgical guides are not normally used because the precision in inserting the implant is easily controllable.
On the other hand, in extreme situations, such as those of group 3 and with the planning of 3 or more implants and in the presence of important anatomical areas, such as the mandibular canal, it seems appropriate to resort to the classic implant templates. (16) In intermediate situations such as those of group 3, which require the identification of two implant sites, the execution of templates with radiopaque references could represent an economic and easy-to-perform solution. Naturally, the type of information given by these thermo-printed guides is reduced only to identifying the point on the mucosa and on the bone where to insert the fixture without the aid of additional information regarding the angle. (17.18)
With regard to these parameters, the clinician must refer to the data acquired through a 3D RX examination as normally occurs in the execution of freehand techniques.
It seems clear that every time the positioning of the implant suggested by the sphere incorporated in the template has to be modified thanks to the information coming from the 3D sections, the same spheres visible both in the volumetric RX and on the mucosa (when the device is worn), can be considered as the residual teeth that are normally used as landmarks; therefore their extreme proximity to the new point where to place the implant greatly reduces the margin of error.
CONCLUSIONS
This research is part of a study that examines a whole series of preliminary assessments that the implantologist carries out during the setting of the surgical intervention. The planning of such a delicate treatment, which has a high biological cost for the patient, requires attention and is aimed at obtaining predictable results. This study shows that sometimes, in particular situations, our visual assessment, especially on distances, may not be accurate with the consequence of making mistakes that could invalidate the entire implant protocol. (19,20,21,22) In some clinical conditions, the packaging of thermo-printed masks with radiopaque references, which can also be done in the studio without the aid of a dental technician and with the help of a few simple equipment, could allow the implantologist to significantly increase the level of accuracy in identifying the implant site. (23)
References
- Orentlicher G, Horowitz A, Abboud M. Computer-guided implant surgery: Indications and guidelines for use. Compend Contin Educ Dent. 2012, 33, 720–732; quiz 33.
- D’Haese, J.; Ackhurst, J.; Wismeijer, D.; De Bruyn, H.; Tahmaseb, A. Current state of the art of computer-guided implant surgery. Periodontology 2017, 73, 121–133. [Google Scholar] [CrossRef] [PubMed]
- Graham R N J, Perriss R W, Scarsbrook A F. DICOM demystified: a review of digital file formats and their use in radiological practice. Clin. Radiol. 2005, 60, 1133–1140. [CrossRef] [PubMed]
- Kalra M, Aparna IN, Dhanasekar B. Evolution of surgical guidance in implant dentistry. Dent Update 2013;40, 577– 578, 581–582.
- Kola MZ, Shah AH, Khalil HS, et al. Surgical templates for dental implant positioning; current knowledge and clinical perspectives. ; 21:1–5. Niger J Surg. 2015, 21, 1–5. [CrossRef] [PubMed]
- Scherer U, Stoetzer M, Ruecker M, Gellrich N C. See Template-guided vs. non-guided drilling in site preparation of dental implants. Clin. Oral Investig. 2015, 19, 1339–1346. [CrossRef] [PubMed]
- Schnutenhaus S, Edelmann C, Rudolph H, Dreyhaupt J, Luthardt R G. 3D accuracy of implant positions in template-guided implant placement as a function of the remaining teeth and the surgical procedure. A retrospective study. Clin. Oral Investig. 2018, 22, 2363–2372. [CrossRef]
- Younes F, Cosyn J, De Bruyckere T, Cleymaet R, Bouckaert E, Eghbali A. A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J. Clin. Periodontol. 2018, 45, 721–732. [CrossRef]
- Behneke, M. Burwinkel, N. Behneke Factors influencing transfer accuracy of cone beam CT-derived template-based implant placement. Clin. Oral Implants Res. 2012, 23, 416–423. [CrossRef]
- Gargallo-Albiol, J., Barootchi, S., Salomó-Coll, O., Wang, H.-L., 2019. Advantages anddisadvantages of implant navigation surgery. A systematic review. Ann. Anat. 2019, 225, 1–10.
- Sancho-Puchades, M.; Alfaro, F.H.; Naenni, N.; Jung, R.; Hammerle, C.; Schneider, D. A Randomized Controlled Clinical Trial Comparing Conventional and Computer-Assisted Implant Planning and Placement in Partially Edentulous Patients. Part 2: Patient Related Outcome Measures. Int. J. Periodontics Restor. Dent. 2019, 39, e99–e110. [Google Scholar] [CrossRef] [PubMed]
- Choi W, Nguyen B-C, Doan A, Girod S, Gaudilliere B, Gaudilliere D. Freehand versus guided surgery. Factors influencing accuracy of dental implant placement. Implant Dent. 2017, 26, 500–509.
- Kramer FJ, Baethge C, Swennen G, et al. Navigated vs. conventional implant insertion for maxillary single tooth replacement. Clin Oral Implants Res. 2005, 16, 60–68. [CrossRef] [PubMed]
- Chen, S.; Ou, Q.; Lin, X.; Wang, Y. Comparison Between a Computer-Aided Surgical Template and the Free-Hand Method: A Systematic Review and Meta-Analysis. Implant Dent. 2019, 28, 578–589. [Google Scholar] [CrossRef] [PubMed]
- Schnitman, P.A.; Hayashi, C.; Han, R.K. Why guided when freehand is easier, quicker, and less costly? J. Oral Implantol. 2014, 40, 670–678. [Google Scholar] [CrossRef]
- S. Hillerup Iatrogenic injury to oral branches of the trigeminal nerve: records of 449 cases. Clin. Oral Investig. 2007, 11, 133–142. [CrossRef]
- Payer M, Kirmeier R, Jakse N, et al. Surgical factors influencing mesiodistal implant angulation. Clin Oral Implants Res. 2008, 19, 265–270. [CrossRef]
- Schulz, M.C., Hofmann, F., Range, U., Lauer, G., Haim, D. Pilot-drill guided vs.full-guided implant insertion in artificial mandibles-a prospective laboratorystudy in fifth-year dental students. Int. J. Implant Dent. 2019, 5, 23. [CrossRef]
- Dimitrijevic T, Kahler B, Evans G, Collins M, Moule A. Depth and distance perception of dentists and dental students. Oper. Dent. 2011, 36, 467–477. [CrossRef]
- Nickenig H J, Wichmann M, Hamel J, Schlegel K A, Eitner S. Evaluation of the difference in accuracy between implant placement by virtual planning data and surgical guide templates versus the conventional free-hand method - a combined in vivo – in vitro technique using cone-beam CT (Part II). J. Cranio Maxillofac. Surg. 2010, 38, 488–493.
- Schulz M C, Rittmann L, Range U, Lauer G, Haim D. The use of orientation templates and free-hand implant insertion in artificial mandibles-an experimental laboratory examination in fifth-year dental students. Dent. J. 2018, 6.
- Vermeulen, J. The accuracy of implant placement by experienced surgeons. Guided vs freehand approach in a simulated plastic model. Int. J. Oral Maxillofac. Implants 2017, 32, 617–624. [Google Scholar] [CrossRef] [PubMed]
- Park, J.Y.; Song, Y.W.; Park, S.H.; Kim, J.H.; Park, J.M.; Lee, J.S. Clinical factors influencing implant positioning by guided surgery using a nonmetal sleeve template in the partially edentulous ridge: Multiple regression analysis of a prospective cohort. Clin. Oral Implants Res. 2020, 31, 1187–1198. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).