1. Introduction
With high burdens of morbidity and premature mortality, many Southern African countries are failing to meet their health targets [
1]. Contributing to this, are the marked human resources for health (HRH) shortages and maldistribution [
1,
2]. Botswana, Eswatini (formerly Swaziland) and Lesotho are three landlocked middle-income Southern African countries (
Table 1), which are mostly rural and have pronounced health worker shortages, especially in rural areas [
3,
4,
5,
6,
7,
8,
9]. With Lesotho completely surrounded by South Africa, all three countries share borders with South Africa [
7,
8,
9]. In 2019, these three countries had the highest reproductive-age (15-49 years) HIV prevalence in the world, with Eswatini ranking first and Botswana third [
10]. Lesotho has the highest tuberculosis (TB) incidence in the world, which stood at 650/100,000 people in 2020 [
11]. All three countries have a physician to population ratio of below 5 per 10,000 population and a nurse and midwife population ratio of below 42 per 10,000 population [
12]. The ratio of doctors, nurses and midwives for each of the three countries is therefore below the United Nation’s Sustainable Development Goal target of 44.5 per 10,000 population [
1,
13,
14].
These shortages are associated with the limited training capacity in these countries, emigration of health professionals to other countries, the dual health systems, and growing population sizes [
1,
3,
4,
5,
17]. Unique to Botswana, is the fact that only 16% of the country is inhabitable as 84% is dominated by the Kalahari Desert, 60% of the population is concentrated in the Eastern part of the country, 40% live in rural areas, most of which are sparsely populated, further complicating the provision of health services [
18]. These countries use return-of-service (RoS) scheme training strategies to increase the production of new entry health professionals, nursing specialists and medical specialists [
4,
18,
19,
20,
21]. Through RoS schemes, governments fund aspiring health professionals or health professionals in employment to respectively study towards a health profession or specialise in return for service [
14,
21,
22]. Of the three countries, Botswana is the only one which has had a medical school since 2009, creating some internal training capacity for medical students and specialists [
17,
18,
21,
23]. Notwithstanding, all these countries send beneficiaries to neighbouring countries and abroad for their studies [
18,
19,
20]. There is no literature outlining the policy intentions, planning process and recruitment into service of the beneficiaries casting doubt on the effectiveness and value for money of these schemes. These aspects can only be understood once the histories, evolution and architecture of these policies are understood. This study, therefore, aimed to describe the design and implementation of RoS schemes in Botswana, Eswatini and Lesotho, and further understand how they adhere to principles of the World Health Organisation (WHO) framework for human resources for health (HRH) development in Africa [
24,
25].
2. Materials and Methods
Design
Data were derived through a multimethod research design including: a) literature review, b) policy review, and c) semi-structured interviews of policymakers and implementors. The Consolidated criteria for Reporting Qualitative research (COREQ) and the Checklist for the use and Reporting of Document Analysis (CARDA) were used for the article [
26,
27].
Recruitment and Data collection
The aim of the literature review was to review information on the history of bursary or scholarship schemes with an expectation of a government return-of-service. First, a literature search was undertaken through searching databases (Pubmed, CENTRAL and EBSCO Host (including CINAHL)) between 01 October 2020 and 31 August 2022. Next, the archives of the National Libraries in Gaborone, Mbabane and Maseru were searched. Databases were searched using the search terms: (‘bursar*’ OR ‘scholarship*’ OR ‘return of service’ OR ‘return for service’ OR ‘in-service’ OR ‘grant*’ OR ‘financial aid’) AND (‘health’) AND (‘Eswatini OR Swaziland’ OR ‘Botswana’ OR ‘Lesotho’) to identify relevant literature examining the history of RoS schemes, studies of their implementation or operation and their evolution over time. Data were extracted using a designed and piloted tool to extract relevant information on the RoS policy context, content, process, and actors (Appendix 1). Second, we contacted individuals with ultimate responsibility for the operation of the schemes in the three countries, specifically: the Director of Tertiary Education Financing (Ministry of Education), and the Director of Human Resource Development (Ministry of Health) in Botswana; the Permanent Secretaries in the Ministries of Labour and Public Service in Eswatini; the Director of the National Manpower Development Secretariat (NMDS) and the Deputy Director of Human Resource Development (Ministry of Health) in Lesotho. These senior officers were requested for access to officials who were the most relevant to be interviewed on RoS schemes for health professionals. A total of 9 policymakers were identified, with two in Eswatini, three in Lesotho and four in Botswana. Participants were excluded if they had less than 2-years’ experience in the role or refused to consent. Microsoft Teams virtual platform was used for interviews to gain a deeper understanding of how RoS policies were designed and implemented, and how they have evolved over time (Appendix 2). Participants were interviewed as individuals (4) or in the presence of other colleagues (5). As part of the interview process, they were allowed to refer to policy documents to confirm certain aspects. The interviewer took field notes along with audio recordings of the interviews using Microsoft Teams. Interviews took an average of 64 minutes. Transcripts were obtained from Microsoft Teams, transferred to Microsoft Word and cleaned by the first author who also translated the non-English language phrases (siSwati, seSotho and seTswana) used in the interviews. Lastly, between the 01st of November 2020 and 15th of February 2022, policymakers were requested to provide all existing versions of policy documents that are on record since inception of the schemes for the policy review. We requested for all RoS scheme related documents including unsigned contract copies, RoS scheme beneficiary selection criteria, correspondents templates with stakeholders and beneficiaries, audit reports, etc. Similar to the literature review, this policy review extracted information on the piloted data extraction tool (Appendix 1).
Reflexivity
The first author (SAM) is a South African Public Health Medicine Specialist who held several leadership positions as an undergraduate medical student at the University of Cape Town in the early 2000s. This exposed him to agreements that the university had with other governments. In those years, he also studied with and befriended RoS beneficiaries from a number of Southern African countries including the three countries of interest in this study.
Data analysis
The Walt and Gilson policy analysis framework [
28] was used to analyse both the policy document review and literature review and were summarised using a narrative approach to reporting. An approach of familiarisation, coding, theme development, review of themes, theme definition and reporting was followed for the qualitative interview analysis. The qualitative interview results are presented based on four main themes and nine sub-themes that were derived using inductive thematic analysis in NVIVO 12. There was member checking of transcripts by participants to verify accuracy of the information. Peer checking of half of the transcripts by BA and RJ helped devise the themes and all authors reached consensus on the final themes.
Ethics approval
Ethics approvals were obtained from the University of New South Wales (HC200519), the Botswana Health Research and Development Division (HPDME 13/18/1), the Botswana Ministry of Tertiary Education, Research, Science and Technology (DRST 7/2/13 XXVII (27)), the Eswatini Health and Human Research Review Board (FWA 00026661/IRB 000 11253), and the Lesotho Ministry of Health Review Board (ID 24-2021). Participants have been de-identified. Direct quotes are labelled using random labels known only by the 1st author (SAM) and senior authors (BA and RJ).
3. Results
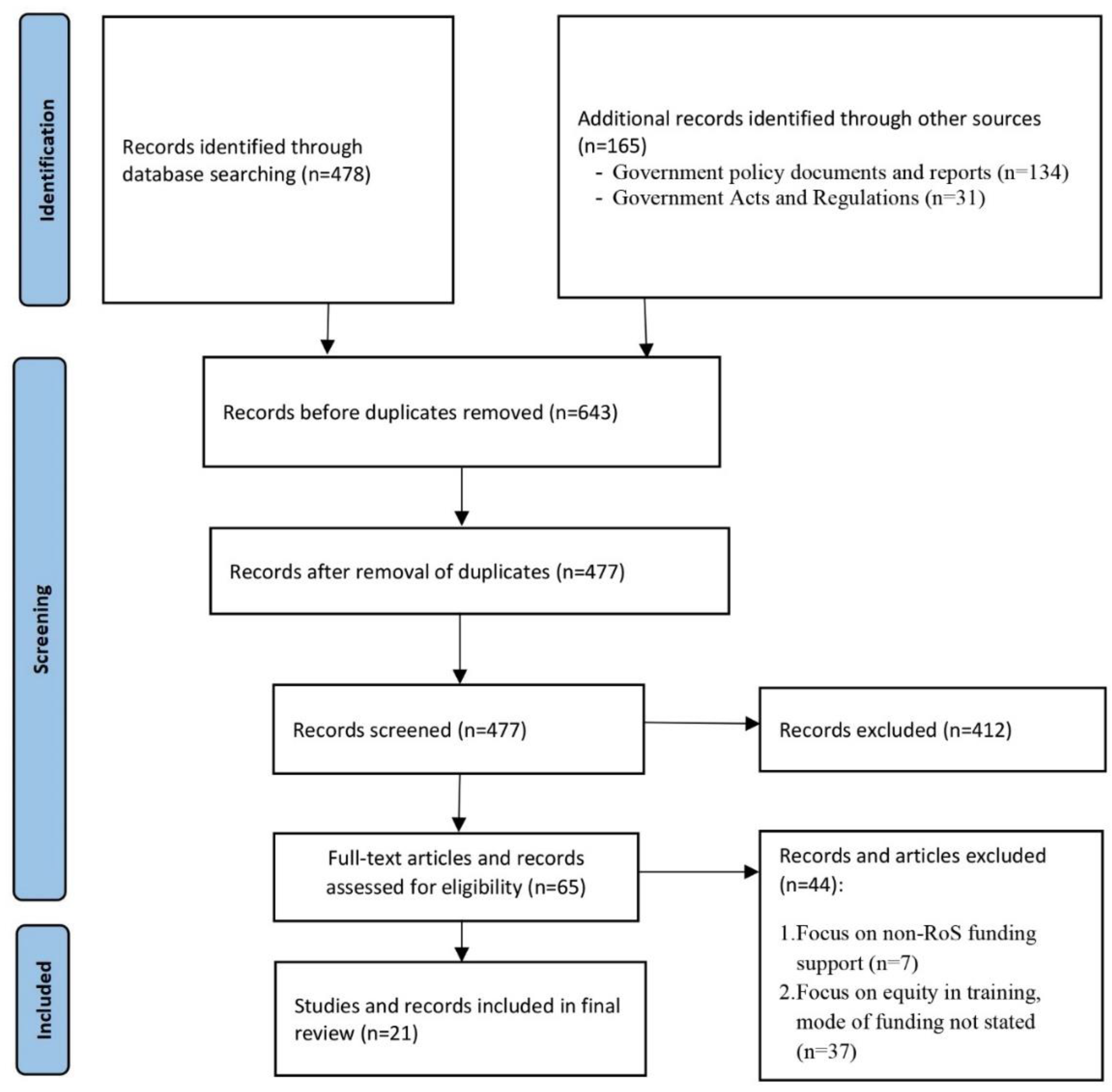
The literature review identified a total of 668 records of which 45 were deemed as potentially suitable for our review. Following full-text appraisal of these texts, 21 were included in the final review (
Figure 1). All approached policymakers agreed to interview. Interview respondents were four officials from Botswana (three from the Ministry of Health and one from the Ministry of Education), two from Eswatini (one from the Ministry of Labour and one from the Ministry of Public Service) and three from Lesotho (two from NMDS and one from the Ministry of Health). Of these participants, four were female and five were male, and had experiences that ranged from 5 to 22 years administering the schemes.
Understanding RoS schemes in three Southern African countries (Context and Content)
Types of schemes
Broadly, the governments have two programmes that benefit health workers, namely, the in-service programme for government employees, and the pre-service programme for future employees, mostly youth with high academic grades at school [
29,
30,
31,
32,
33,
34] (
Table 2).
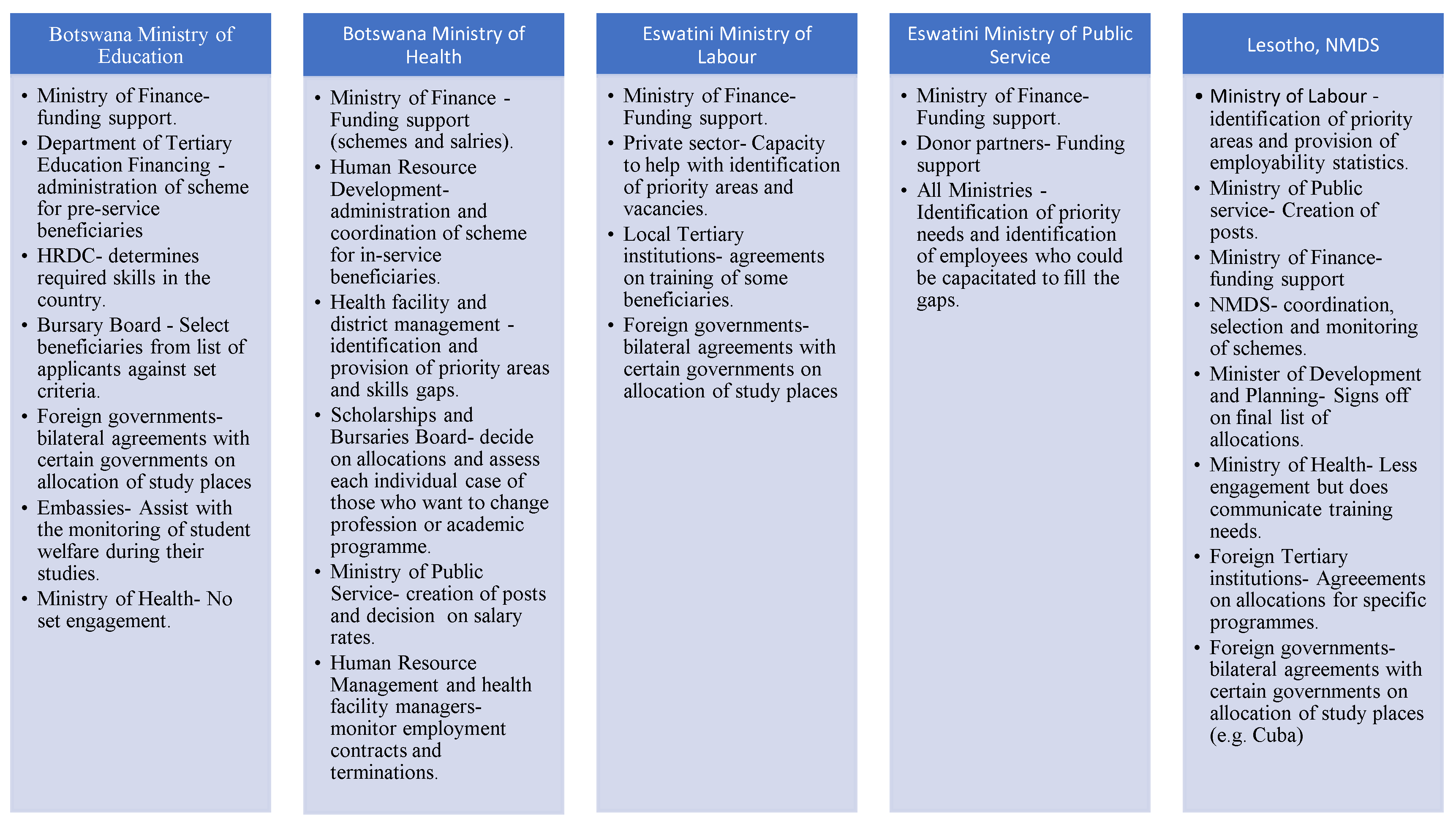
Stewardship for the in-service programmes is the Ministry of Health in Botswana, Ministry of Public Service in Eswatini and the NMDS in Lesotho [
30,
31,
32,
33,
34]. Whilst the NMDS is also responsible for the pre-service programme in Lesotho, the Ministry of Education and Ministry of Labour are responsible for the pre-service programme in Botswana and Eswatini respectively [
4,
17,
18,
19,
20,
32,
33,
35,
36,
37,
38,
39].
Botswana has two main schemes under the pre-service programme, namely the top achievers’ programme (TAP) and the grant-loan scheme [
39]. Whereas the grant-loan scheme only funds beneficiaries for undergraduate studies, the TAP starts funding a beneficiary from undergraduate pre-entry studies (e.g., A-levels, O-levels, pre-medical studies, etc.) to doctoral studies. The grant-loan scheme uses a sliding scale of four categories that prioritises beneficiary groups per academic programme of study with health sciences, engineering and all skills deemed to be scarce being ranked top, and the last category is performing arts which is regarded as an optional course.
Aim of the programmes
RoS schemes were suggested to serve six main aims whose purpose is to build the health workforce capacity, strengthen the economy and improve educational opportunities for citizens.
- (a)
Address critical skills shortages and strengthen government capacity
Countries often reflect on health workforce shortages, especially nursing and medical specialists. This is due to recognition that training of employees in specialist fields helps reduce specialist referrals to neighbouring countries (e.g., South Africa) and the private sector.
GBL1:For example, we refer to South Africa, we refer to private hospitals, we refer to medical laboratories… So, for us it's an issue of not having the right skilled manpower. …you don't have to refer for cancer or something like that, …we can do on our own home ground. So, that within four or five years, uh, let me say ten years at least, we are able to be sustainable. We don't have to refer people for cardiology…
One of the principal purposes of Eswatini’s Ministry of Labour is to manage issues of supply and demand of human resources into the labour market.
PP2: So, I study the …dynamics in the labour market, and then say for the labour market to be efficient and effective, what does it require? Obviously, one of the major… inputs into it, it's human resources. … that's where then we have to then have very clear human resource planning and development strategies, …skills, uh, requirements in the short term…, in the medium term, in the long-term…
- (b)
Professionals who are relevant and up-to date
It is important for the public service to have employees who have kept up with the latest knowledge trends in their profession.
PP1:I guess the objectives would be for government to gain because we live in an ever-changing world, so, we need to constantly have skills that are…, on par with the rest of the world (sic).
- (c)
Human resource development and career pathing
These schemes are used for development and career progression of existing health employees. This allows employees to benefit from global academic opportunities and thus further benefit their countries. For instance, midlevel health workers e.g., pharmacy assistants and dental therapists might be offered opportunities to be pharmacists and dentists respectively. Medical doctors may specialise in fields like psychiatry, obstetrics and gynaecology, internal medicine, emergency medicine, pathology, etc. Nurses, dentists and allied health workers can also specialise further, thus increasing their individual earning potential whilst contributing to the health system.
- (d)
Improve employability prospects for citizens
At least one of each of the countries’ policies places emphasis on the need to ensure that citizens are prioritised to take up job opportunities in all sectors, especially the public sector [
18,
29,
30,
31,
32,
33,
39,
40,
41,
42]. Foreigners are only employed when there is no citizen who can perform the same job. In that event, the foreigner and/or employer needs to have plans in place to ensure that there is skill transfer to citizens for when the foreigners leave. As supported by a participant:
PP2: So, at independence you know the country had a desire to fill, uh, strategic positions of the economy with, uh, qualified emaSwati [Swati nationals]. So, uhm, there was then a targeted, uhm programme to train emaSwati [Swati nationals] so that when they come back, they will take up their positions, and the policy then was called local, it was called a localisation policy.
- (e)
Strengthen management and population health skills
In-service programmes also help to enhance identified management gaps in all the ministries in Eswatini and Lesotho, and in only the Ministry of Health in Botswana. Population health skills are also strengthened through these programmes.
- (f)
Fulfill national political mandates
The three countries get guidance for training health professionals from the governments’ macro policy instruments such as the Poverty Reduction Strategy and the National Development Strategy (NDS) in Eswatini [
37,
43], Vision 2016 [
44] in Botswana and Lesotho’s National Strategic Development Plan (NSDP) [
35]. The NDS, Vision 2016 and NSDP place access to health in the highest level of priority [
35,
37,
43,
44]. These documents are often written by consultants. As narrated by a participant:
PP2: So, this was like the start..., the span of this study was like 5 years. So, uh, that priority, identification came to an end this past year, 2020. So, we have since appointed a consultant now to undertake a new study, you know, to project… the training needs for the next five years again.
Who are the beneficiaries?
Table 3 summarises the characteristics of beneficiaries and it shows that being a citizen is common for all the policies and countries. Pre-service schemes place lots of weight on academic merit. Individuals applying for in-service schemes should apply for a programme that is in line with their current job. Whilst the criteria used to select beneficiaries are generally transparent, this is not the case in Lesotho. These are set standard criteria and do not vary from year to year.
DS1:…we don't want students knowing our criteria because sometimes, we try to share the criteria with them… But you know how students are, if you didn't succeed, now… they go back to criteria. Now I passed more than whoever blah blah blah.
Even though Botswana’s in-service programme used to exclude pregnant employees for academic sponsorship, that has since changed as narrated by a participant.
GBL1:We are trying to cater for everybody. You know? So, pregnancy is not no longer an issue.
What are the beneficiary obligations?
Beneficiaries are contracted/bonded to return for service after completion of their studies as per
Table 3.
Further shown in
Table 3 is that undergraduate health sciences beneficiaries in Botswana are required to serve a one-year service period for each year of funding support at the end of their studies. Botswana’s grant-loan scheme beneficiaries, Eswatini’s Ministry of labour beneficiaries and Lesotho’s NMDS beneficiaries are also not compelled to serve in government if they are within the country. However, whilst those who serve in the public sector in Lesotho must repay 50% of the funding support within five years of completion of their studies, those who work in the public sector have to repay 65%.
Lesotho’s NMDS beneficiaries serve for a minimum of three years if funded for a year. Beyond a year, it’s twice the service period for each year of funding. The latter condition is similar for Eswatini’s Minister of Labour’s. Eswatini’s Minister of Labour’s beneficiaries must repay 50% of the funding support if in the country and 100% if outside the country. In-service beneficiaries from Eswatini’s Ministry of Public Service scholarships are mandated to serve a year more than the funded period, something similar for Botswana’s Ministry of health in-service beneficiaries funded for more than a year. The maximum period of service is 5-years for the latter, regardless of the funding duration.
PP1: Officers who are sent on training are expected back in the positions they were prior to leaving. We do not allow for officers to change professions under this facility.
Are there possibilities for contract deviations?
If a Ministry of Labour funded beneficiary in Eswatini fails an academic year, then the funding is suspended for the following year and completely cancelled after two consecutive years of non-progression. If the beneficiary is the one who voluntarily opts out of the academic programme, then they are obliged to repay 100% of the funding support received. Botswana’s Ministry of Education applies a similar principle but also offers beneficiaries an opportunity to complete their studies at the University of Botswana “where it is much cheaper”.
If an in-service beneficiary in Botswana wants to change profession (e.g., nurse to medical doctor) then they must address a motivational letter to the responsible Board who will then deliberate and decide on the matter. A similar process is also followed for medical specialist who could decide to sub-specialise (2-years) after completion of their initial 4-to-5-year specialist training (e.g., internal medicine specialty to nephrology, etc.).
GBL1:I think that one is discretion, the Board will decide whether you sign another bond, because this one would have been five years and then you sign another one which is for a different programme that becomes additional two years. …it's normally, uh, a special dispensation because we don't always allow for somebody to continue, uh, immediately after completing. You must come back, serve a certain period of time then continue with another qualification.
Whilst Lesotho NMDS beneficiaries are generally not allowed to change academic programmes, exceptions can be made if the new programme is a priority programme for the country in that year. There are also situations when beneficiaries cannot serve their obligatory service period due to lack of jobs. The important thing is for such beneficiaries to inform the funding Ministry (or NMDS if in Lesotho).
Origins of the schemes
Anticipating independence (which eventually came in 1968), the Eswatini government launched the localisation and training policy in 1965 where nationals would be trained to take up these strategic positions upon their return [
31,
40,
41]. Building on the localisation policy, in 1977, there was then a formal government scholarship programme which targeted to train nationals for public and private sector positions. Until the year 2000, when Eswatini’s in-service training policy was introduced, it was not structured as it was guided by the Government’s General orders and training Register [
31,
34].
Lesotho’s policy (for both in-service and pre-service beneficiaries) was introduced as the National Manpower Development Council Act in 1978 [
32]. This Act is operationalised through the Loan-Bursary Fund Regulations of 1978 [
32,
33]. The Act legislates the establishment of NMDS, governance and administration of bursaries and the need to establish regulations governing the loan bursary scheme and determining the rates of allowances payable to existing public sector employees who get awarded bursaries [
32,
33].
Botswana’s pre-service and in-service policies were launched in 1995 and 1996 respectively [
18,
29,
30,
39]. The in-service programme is governed by the 1999 Training Management handbook which operationalises the relative legislation defining public sector conditions, including conditions for RoS beneficiaries who are offered opportunities as government employees [
29,
30]. Even though Botswana published guidelines for the award of pre-service schemes in 2011 [
39], all the five policies quoted in this study have never been reviewed as expressed by a participant:
DS1:…they were introduced in 1978 and they have never been reviewed. We are also, we are only now in the process of reviewing them…
Policy Development Framework
All three countries’ policy documents are supported by Acts of parliament [
29,
30,
32,
33,
41,
42] and they predate the WHO guidelines for human resource for health in Africa [
24,
25]. Furthermore, the policies were generic for the whole of government and not limited to health.
Countries of study
Whilst all three countries have internal capacity for training generalist nurses, midwives, nutritionists and environmental health practitioners, the National University of Lesotho and University of Botswana began training pharmacists in 2001 and 2018 respectively. Botswana is the only country among the three training medical doctors since 2009. Eswatini and Lesotho solely rely on other countries for the training of medical doctors and most other key health professions. Notwithstanding, due to limited internal training capacity, Botswana still sends medical students and other health sciences beneficiaries to other countries e.g., United Kingdom, Australia, United States of America, Canada and Cuba being the most common destination countries. South Africa is a popular destination for Botswana’s beneficiaries for all programmes except for undergraduate medical beneficiaries who could not be accepted after 2009 when the medical school opened.
GBL2:…we send…, these employees, around the world to get the gist of these different…, academic fields…, within the different countries that we may have, or we would like them sent to…
Botswana sends two students to Cuba each year, as a participant elaborates:
FZ1: So, we have got medical students in Cuba right now. Right now, we have thirteen. We don't have a lot of students there as much as South Africa has. …Cuba is strictly medicine. But then we also have students who do medicine under the top achievers’ program. This… programme is specifically for high excelling students. …who are at the local institutions doing BSc, Bachelor of Science year one…
Countries of study are either identified through national government bilateral agreements, donor funding or from select choice of countries and/or universities made by the beneficiary.
DS1:So, Lesotho went to the extent of arranging with the government of South Africa for certain institutions to give slots to a maximum of five students per institution for medicine.
PP2: …we have bilateral, uhm, skills development programmes with those countries. Like Cuba…, Russia…, Taiwan. So, we select students, you know, yeah, to benefit from this, uh, bilateral, uh, skills development programmes but, uh, there are those like for example in Ukraine, you know most of those students in Ukraine, they just go there, yeah, and then when, they are there, yeah, of course we do ascertain if the quality of education they are getting is up to standard… If like they are best of our minds (sic) and they want to go and pursue their training, in those countries, and we think they qualify and the universities they are training at are good enough, then we support them wherever they are.
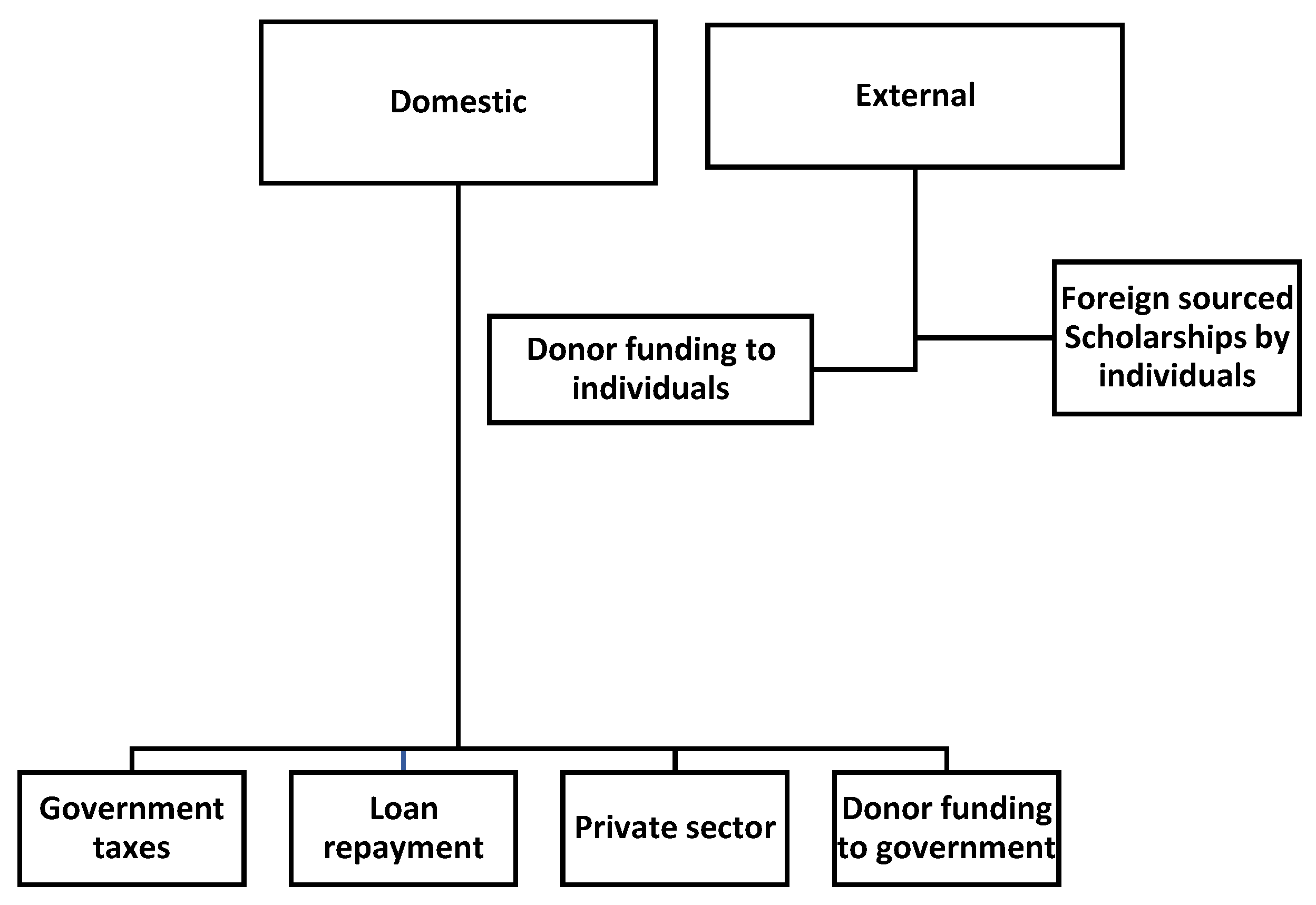
How are the schemes funded and what do they pay for?
Figure 2 shows a summary of the sources of funding for these schemes. In Lesotho all funding is considered to be from government regardless of the original source [
32,
33]. Both Eswatini’s Ministry of Labour and Lesotho’s NMDS rely on government taxes and loan repayments from beneficiaries for the sustainability of their schemes. Botswana’s schemes largely rely on government taxes. The Ministry of Public Service in Eswatini funds its schemes from government taxes and donor schemes such as the Commonwealth. These schemes fund for tuition (including stationery and instruments (e.g., stethoscope, etc.)), accommodation and living allowances, and transport from the country’s capital city (Gaborone, Mbabane or Maseru) to the destination if outside the country. Medical insurance and VISA costs are also covered for those outside the countries [
4,
29,
31,
32,
33,
34,
44].
What are the benefits for the individuals?
Though not guaranteed of a job after completion of their undergraduate studies, funded individuals have better prospects of being employed than other graduates. Those enrolled through the in-service programmes of the three governments are guaranteed of their jobs upon their return and they also receive a salary during their studies. In Botswana, in-service beneficiaries would be given their full salary in their first year of absence and half salary beyond that, but that has since changed:
GBL1:So,Government decided: ‘ok, fine, uh, anybody who goes on government sponsorship, they will be given full salary irrespective of the number of years that you go for’.
In Eswatini, they still implement a staggered salary where the salary of in-service beneficiaries reduces with each year that the employee is away [
31]. These employee beneficiaries receive a full salary in the first year, 75% in the second year, 50% in the third year and 25% from the fourth year onwards. This then leaves beneficiaries with a 75% shortfall in income from the third year of study. Even though policymakers say this is implemented for fairness, some beneficiaries previously found this to be unfair as it impacted on their pre-enrolment bills which continue through their studies [
31].
PP1:Uh, you can't be getting your full salary whilst you are not doing anything in terms of work. It wouldn't be fair to those who are at work.
Lesotho applies a similar principle where the salary is halved from the first year of absence.
Understanding the implementation and implementers of return-of-service schemes in the three countries (Process and Actors)
How are the service needs determined?
Service needs and numbers of beneficiaries to be funded per programme are determined through a consultative process with Ministries. For instance, prior to 2015 the government of Eswatini identified priority training needs, and training in health was amongst those identified to be high priority. The Human Resource Development Council (HRDC) within Botswana’s Ministry of Education provides a list of programmes that are supposedly scarce on an annual basis. The rationale is that the supported programme must be able to help sustain the students by getting employment in the economy after completion of studies. The processes are similar for Lesotho’s undergraduate beneficiaries as explained by respondents:
FZ1: So, that's why we are guided by… HRDC, they call it top occupants’ fields.
DS1:After finalisation of the priority areas, we publish them for the people to know that these are the programmes that we will be taking out of the country and then when it's time for applications,we issue a notice advert that, applications are now open for these particular programmes and these are the conditions and now you apply…our budget will determine how many students we take because of the issue of affordability. If we can only afford about 200, then we'll take 200 if we can afford up to 400, then we'll take 400.
In Botswana, units and health facilities are asked to provide training needs for the next financial year based on their identified priority service needs. These needs are often informed by the service pressures and employee performance development plans/reviews. These would then be sent to the national Ministry of health’s human resources development unit for consolidation and alignment with available training budget. The final list of priority areas is based on the available budget. Similar processes are undertaken in Eswatini (at inter-ministerial levels for public servants) and Lesotho. As explained by one participant.
DS3: …within that limit, they do not come to us and prescribe how many we can have, but they will say: ‘Ministry of Health I only have this amount of money… so, what are your priorities?’, and then we would stipulate our priorities… then we would say within the one that allows us to recruit new people, our priorities will be doctors, nurses and what…
Application process
The Botswana Ministry of Education releases an advertisement each year around February, when matric results come out. In Lesotho and Eswatini applications start in August/September of the year preceding applications. For in-service training policies, the advertisement for positions follows the identification of priority training areas. These positions are advertised on various platforms including notice boards at workplaces, social media, print and electronic media and word of mouth.
DS1:Our Facebook page is more effective. We also use the state radio…and any other platforms that are available. For example, I just give it to you through WhatsApp, you issue it to the, uh, WhatsApp groups… We also take it to the Ministry website. So, it's actually more or less like word of mouth…and we also put it on our notices.
How are eligible beneficiaries selected from applicants?
In all the countries, a Board or committee will assess the applicants and decide. In Lesotho the final list is signed off by the Minister responsible for NMDS (Minister of Development and planning). These examples from two participants highlights the process:
FZ1: It will be a Board where somebody comes and present to say we have these 300 students looking for sponsorship and then we look at the applications and then we make recommendations as a Board.
DS1:…we first establish a team that's going to work through all the applications from the start to finish. … then the selection is taken. We have a Council that… that oversees, the whole NMDS [National Manpower Development Secretariat] operations. So…, after capturing of the candidates they are then forwarded to, our Council... and the Council will make the… decision on the selected and who is not. From the Council then it will go to our minister, but our ministers is just to show him that ok, these are the students who have been selected, these are those that have not been selected. Then the minister, when he satisfied with what he has gotten then he will approve.
How are beneficiaries monitored during their studies?
Eswatini and Lesotho don’t have formal ways of monitoring beneficiaries during their studies other than the expectation for beneficiaries to submit their results annually.
DS1: We don't have such a system, that is why people are defaulting.
The Botswana Ministry of Education on the other hand relies on their consular staff in the foreign countries. No specific monitoring is done for those studying within the country.
FZ1: We have Education outages who actually are staff members from the Department who are stationed in missions outside the country. So, their job is to monitor the students’ performance and welfare during their course of studies. But once the students have completed and they are back in Botswana, no, we don't really make contact with them at all. Unless they come back to us for another sponsorship.
How are beneficiaries recruited into employment?
Whilst in-service beneficiaries have a straightforward arrangement in that they first return to the job they held before funding support whilst awaiting translation into the new role, this is not as clear for pre-service beneficiaries. In Botswana, the Ministry of Education requires health sciences beneficiaries to complete a certain form in the last month of their final year. In this form, beneficiaries enter their preferred placement hospitals. These forms are then sent to the Ministry of Health by the Ministry of Education so that they are aware of the number of completing students. This is the first and last formal communication between the two Ministries in this process of selection and placement.
In Eswatini and Lesotho undergraduate beneficiaries apply for a vacant position just like everybody else by approaching the Ministry of Health. In all these two countries, health sciences beneficiaries are then expected to inform the Ministry of Labour or NMDS once they have started working so that repayment arrangements can be set-up. As narrated by two respondents:
DS1:So, the Ministry of Health will then place them, I don't really know how that happens, but they register with the Ministry of Health, and the Ministry of Health will place them according to the vacancies, I think.
DS3: …what they normally do, is that they would apply to the Ministry of Health, they introduce themselves like, I am so, and so who is qualified recently, qualified somewhere, I am completing on this date. So, I am applying for a job…
How are beneficiaries monitored after completion of their studies?
In the three countries, all the funding entities do not have mechanisms to monitor beneficiaries’ fulfilment of the service obligation. Where there are funds expected to be repaid, then debt collectors are often contracted to follow-up on beneficiaries who are behind on their payments. Eswatini’s in-service training policy is the only one that makes mention of a detailed monitoring and evaluation plan [
31]. The monitoring and evaluation plan includes monitoring of beneficiaries during their studies, feedback from beneficiaries on relevance of training and performance of beneficiaries post-completion of studies [
31].
Who are the Actors involved in the success of these schemes?
Figure 3 summarises the stakeholders that are directly or indirectly involved with the schemes. Lesotho’s policy mandates the NMDS Director to keep a record of each student to whom a bursary has been granted [
32,
33]. The Ministry of health is a passive stakeholder for all pre-service schemes, as they are not involved with selection or monitoring of beneficiaries during and after their studies.
4. Discussion
This study of three Southern African countries found similarities in the design of their RoS schemes. Policies governing RoS schemes were all generic and not specific for the health sector. RoS schemes in these countries were introduced to address critical skills shortages, improve employability prospects for citizens, to have competent public sector employees by global standards, and to aid career pathing of government employees. All pre-service programmes were administered outside of the Ministry of Health. Whilst both Eswatini and Lesotho’s in-service schemes are administered outside the Ministry of Health, Botswana’s is administered within the Ministry of Health. Pre-service beneficiaries have both partial repayments and service obligations in Eswatini and Lesotho. Botswana’s undergraduate health sciences beneficiaries generally have no repayment obligations as they mostly benefit from the top achievers’ programme which only has a service obligation. The policies are all older than 20-years and have never been reviewed since inception. However, there are some prescripts that have been operationally amended over time due to changing practices, lessons from other countries and needs to ensure fairness. Pre-service beneficiaries are mostly selected based on academic merits with little weight being put on the origins of the individual and their socio-economic status.
Intersectoral collaboration is one of the main strategies that was advocated for in the 1978 Alma-Ata declaration [
45,
46]. At the time, recognition was already made that health for all would only be attained if there were multisectoral actions [
47]. The governance of RoS schemes in these three Southern African countries therefore presence a perfect opportunity for multiple Ministries to work together to improve the lives and livelihoods of their citizens. This research therefore provides valuable lessons on the dos and don’ts of collaborative governance as it shows that multisectoral collaboration is a non-negotiable necessity in ensuring health systems’ efficiency and good health outcomes but is not sufficient by itself [
47,
48,
49]. As Adeleye et al. [
47] advised, success requires intentional, strategic and coordinated efforts of sectors.
As articulated by Eswatini’s Human Resources for Health strategic plan for 2012-2017, the coordination of RoS beneficiaries between the Ministry of Health and Ministry of Labour, and the Ministry of Health and Ministry of Public Service (create posts) is weak [
20]. Botswana’s 2007-2016 HRH planning strategy also noted that there were fewer health sciences beneficiaries than the target for each of the 7 years of assessment (2000-2006) [
18]. Conclusions reached was that this could have been poor knowledge of the schemes by potential beneficiaries [
18]. Only acknowledged by Eswatini but not unique to them, there are no obligatory mechanisms instituted to commit graduates to serve the public health sector and/or underserved areas [
18,
19,
20]. Furthermore, all the three countries have dedicated HRH planners but it’s not clear how their processes feed into the country agreements that guide RoS scheme implementation [
18,
19,
20]. Eswatini acknowledged the lack of HRH planning capacity in the country [
20]. It is therefore important for a policy to be explicit about its intentions and the outcomes that will be minimally acceptable for its success, and how it will be evaluated [
50].
It is commendable that the policymakers have a fairly good idea on the origins of the schemes. The fact that the policies have not changed over many years makes it easier to preserve institutional memory and transfer from one generation of administrators to the next. However, it is important to recognise that policies are only as relevant as the existing laws, trends, practices and technologies of the day, if any of those change then they need to be reviewed [
2,
48]. As evidenced by the recent equalisation in the treatment of men and women in-service beneficiaries in Botswana, where the policy discriminated against pregnant women [
29]. On recognising this, stakeholders were to then get together and formally review the policy document following their pre-defined procedures. Consistent with principles of a good policy that suggest review timelines in a policy, [
50] a policy document has to therefore have pre-determined review standard operating procedures and timelines, e.g., every 3 or 5 years.
Rural origin health sciences students are said to also be three times more likely to return to their places of origin than their urban counterparts [
51,
52,
53,
54,
55,
56]. The fact that academic merit is the mainstay of these schemes therefore ignores this overwhelming evidence [
51,
52,
53,
54,
55,
56]. Furthermore, the Ministries of Health are passive role players in the implementation of RoS schemes. Governments have to also make effort to increase internal training capacity, which in itself requires an investment in training of a crop of internal educators.
This study notes six major challenges and provides some suggestions for improvement. First, the results of this study suggest it is unlikely that the RoS planning process follows the evidence guidance provided by Mabunda et al. [
22] and Sousa et al. [
2] These authors [
2,
22] propose for HRH planning to be informed by a scientifically determined need (e.g. burden of diseases) and determine the skills-mix that will best meet the needs, match a beneficiary against a pre-identified service area, improve efficiency to minimise waste and attrition, and consider future salaries that will be used to pay beneficiaries. Second, the policies all do not have an evaluation plan. Third, the policies do not have room for incorporating principles of the WHO guidelines on HRH policy development since they are dated [
24,
25]. Frameworks help with the standardisation and simplification of complex processes. Fourth, the fact that employment of these beneficiaries is not guaranteed and is left to the beneficiary to find employment leaves room for frustration and/or exploration of other employment options and thus inefficiency of the programme through leakage of trained health professionals. Fifth, coordination between the Ministry of Health, specifically the Human Resource Management arm, and the implementing unit and/or Ministry has to be strong to improve monitoring of the schemes throughout the implementation cycle. Sixth and last, the fact that governments have opted for an approach where RoS policies apply transversally between Ministries, they need to have clearly defined and specific roles for each of the Ministries receiving the beneficiaries.
This study is limited by poor archiving in all the countries as all implementing organs felt that there could at least be one more policy document that could provide clarity on the origins of the schemes but that could not be located. However, this was supplemented by rich information acquired from the participants and documents. Even though the Eswatini Ministry of Health did not have a participant, inputs acquired from the Ministry of Labour and Ministry of Public Service provide a good description on the origins and implementation of RoS schemes, therefore fulfilling the study aims.
5. Conclusions
Bursaries, Scholarships and Grant-loan schemes play an important role in upskilling health professionals, creation of employability prospects for the youth in the health sector, benchmarking of skills and improvement of networking potential for beneficiaries as they study in neighbouring countries and abroad. Even though the precise origins of the schemes are not known, there are fairly good estimates on when the schemes began and how they have evolved over time. The efficiency of these schemes is further impeded by poor coordination between the implementing/or administering agency, e.g., Ministry of Education and the Ministry of Health. This therefore requires a strategy for the creation of cooperation and coordination plans between the Ministry of Health (specifically human resource management) and the administering agency to ensure that the potential for RoS schemes to provide a solution to the human resources for health gaps is optimised.
Author Contributions
SAM, RJ, AD and BA conceptualised and designed the work. RJ, SAM, OM sought ethics approvals. SAM, WWC and OM collected data. SAM, RJ, and BA analysed, interpreted data and drafted the article. All authors contributed to multiple versions of the article and approved the final version of the manuscript. The corresponding author attests that all listed authors meet authorship criteria and that no others meeting the criteria have been omitted.
Funding
SAM is supported by a UNSW Scientia Scholarship. RJ is supported by a Level 2 Future Leader Fellowship by the National Heart Foundation (Grant 102059) and a Scientia Fellowship from UNSW. BA is supported by an NHMRC Emerging Leadership Grant (GNT2010055). The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Institutional Review Board Statement
Ethics approvals were obtained from the University of New South Wales (HC200519), the Botswana Health Research and Development Division (HPDME 13/18/1), the Botswana Ministry of Tertiary Education, Research, Science and Technology (DRST 7/2/13 XXVII (27)), the Eswatini Health and Human Research Review Board (FWA 00026661/IRB 000 11253), and the Lesotho Ministry of Health Review Board (ID 24-2021).
Informed Consent Statement
Written informed consent has been obtained from the participants to publish this article.
Data Availability Statement
Data used in this study are available from this article.
Acknowledgments
The authors would like to acknowledge support received from the National Manpower Development Secretariat (NMDS) in Lesotho, SVNet in Eswatini and officials from all the countries’ Ministries mentioned in this study. We would also like to extend our gratitude to Patience Kovane, Siabulela Makhehla, Ezra Leteane, Nomakheswa Mjanyelwa from NMDS in Lesotho, Lutfo Dlamini a member of parliament in Eswatini, Gugu Mahlalela from SVNet in Eswatini, Gcebile Dlamini from the Ministry of Labour in Eswatini and Dintle Molosiwa from the University of Botswana for all their assistance with information and resources.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
Appendix A. Data Extraction tool
The appendix is an optional section that can contain details and data supplemental to the main text—for example, explanations of experimental details that would disrupt the flow of the main text but nonetheless remain crucial to understanding and reproducing the research shown; figures of replicates for experiments of which representative data is shown in the main text can be added here if brief, or as Supplementary data. Mathematical proofs of results not central to the paper can be added as an appendix.
Appendix B. Interview guide
References
- Boniol, M.; Kunjumen, T.; Nair, T.S.; Siyam, A.; Campbell, J.; Diallo, K. The global health workforce stock and distribution in 2020 and 2030: a threat to equity and ‘universal’ health coverage? BMJ Glob. Health 2022, 7, e009316. [Google Scholar] [CrossRef] [PubMed]
- Sousa, A.; Scheffler, R.M.; Nyoni, J.; Boerma, T. A comprehensive health labour market framework for universal health coverage. Bull World Health Organ. 2013, 91, 892–894. [Google Scholar] [CrossRef] [PubMed]
- Dlamini, C.P.; Khumalo, T.; Nkwanyana, N.; Mathunjwa-Dlamini, T.R.; Macera, L.; Nsibandze, B.S.; Kaplan, L.; Stuart-Shor, E.M. Developing and Implementing the Family Nurse Practitioner Role in Eswatini: Implications for Education, Practice, and Policy. Ann. Glob. Health 2020, 86, 50. [Google Scholar] [CrossRef] [PubMed]
- Asamani, J.A.; Zurn, P.; Pitso, P.; Mothebe, M.; Moalosi, N.; Malieane, T.; Izquierdo, J.P.B.; Zbelo, M.G.; Hlabana, A.M.; Humuza, J.; et al. Health workforce supply, needs and financial feasibility in Lesotho: a labour market analysis. BMJ Glob. Health 2022, 7, e008420. [Google Scholar] [CrossRef] [PubMed]
- Willcox, M.L.; Peersman, W.; Daou, P.; Diakité, C.; Bajunirwe, F.; Mubangizi, V.; Mahmoud, E.H.; Moosa, S.; Phaladze, N.; Nkomazana, O.; et al. Human resources for primary health care in sub-Saharan Africa: progress or stagnation? Hum. Resour. Health 2015, 13, 76. [Google Scholar] [CrossRef] [PubMed]
- The World Bank. World Bank Country and Lending Groups. 2021 [10 December 2022]. Available online: https://datahelpdesk.worldbank.org/knowledgebase/articles/906519-world-bank-country-and-lending-groups.
- Britannica E. Map of Lesotho and geographical facts. 2008 [10 December 2022]. Available online: https://east-usa.com/world/lesotho-map.html.
- Mappr. Swaziland political map with major cities. [10 December 2022]. Available online: https://www.mappr.co/political-maps/swaziland-map/.
- One World-Nations online. Political Map of Botswana. 2020 [10 December 2022]. Available online: https://www.nationsonline.org/oneworld/map/botswana-map.htm.
- Roser M, Ritchie H. Our World in Data: HIV/AIDS. 2019 [10 December 2022]. Available online: https://ourworldindata.org/hiv-aids#prevalence-in-the-total-population.
- The World Bank. Incidence of tuberculosis (per 100,000 people)-Lesotho, World 2022 [10 December 2022]. Available online: https://data.worldbank.org/indicator/SH.TBS.INCD?locations=LS-1W.
- The World Bank. World Data. Washington DC, USA: World Bank, 2020 [cited 2020]. Available online: https://data.worldbank.org/indicator/NY.GDP.PCAP.CD?end=2017&locations=ZA-IN-PE&start=1991.
- World Health Organization. Global strategy on human resources for health: Workforce 2030. Geneva, Switzerland: WHO, 2016. Available online: https://www.who.int/hrh/resources/global_strategy_workforce2030_14_print.pdf?ua=1.
- Mabunda, S.A.; Durbach, A.; Chitha, W.W.; Angell, B.; Joshi, R. Are return-of-service bursaries an effective investment to build health workforce capacity? A qualitative study of key South African policymakers. PLOS Glob. Public Health 2022, 2, e0000309. [Google Scholar] [CrossRef]
- United Nations. Human Development Index (HDI) by Country 2022. 2022 [10 December 2022]. Available online: https://worldpopulationreview.com/country-rankings/hdi-by-country.
- Worldometers. life-expectancy. 2022 [10 December 2022]. Available online: https://www.worldometers.info/demographics/life-expectancy/.
- Nkomazana, O.; Peersman, W.; Willcox, M.; Mash, R.; Phaladze, N. Human resources for health in Botswana: The results of in-country database and reports analysis. Afr. J. Prim. Heal. Care Fam. Med. 2014, 6, 8. [Google Scholar] [CrossRef] [PubMed]
- Republic of Botswana Ministry of Health. Botswana Human Resources Strategic Plan: 2007-2016. 2006 [10 December 2022]. 10 December.
- Kingdom of Lesotho Ministry of Health and Social Welfare. Human Resources Development & Strategic Plan: 2005-2025. 2004 [10 December 2022]. Available online: https://www.socialserviceworkforce.org/system/files/resource/files/Kingdom%20of%20Lesotho%20HR%20Development%20and%20Strategic%20Plan.pdf.
- Kingdom of Swaziland Ministry of Health. Human Resources for Health Strategic Plan: 2012-2017. 2012 [10 December 2022]. Available online: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/swaziland/human_resources_for_health_strategic_plan.pdf.
- Mabunda, S.; Angell, B.; Joshi, R.; Durbach, A. Evaluation of the alignment of policies and practices for state-sponsored educational initiatives for sustainable health workforce solutions in selected Southern African countries: a protocol, multimethods study. BMJ Open 2021, 11, e046379. [Google Scholar] [CrossRef]
- Mabunda, S.; Angell, B.; Yakubu, K.; Durbach, A.; Joshi, R. Reformulation and strengthening of return-of-service (ROS) schemes could change the narrative on global health workforce distribution and shortages in sub-Saharan Africa. Fam. Med. Community Health 2020, 8, e000498. [Google Scholar] [CrossRef]
- Seitio-Kgokgwe, O.; Gauld, R.D.; Hill, P.C.; Barnett, P. Analysing the Stewardship Function in Botswana’s Health System: Reflecting on the Past, Looking to the Future. Int. J. Heal. Policy Manag. 2016, 5, 705–713. [Google Scholar] [CrossRef] [PubMed]
- Nyoni, J.; Christmals, C.D.; Asamani, J.A.; Illou, M.M.A.; Okoroafor, S.; Nabyonga-Orem, J.; Ahmat, A. The process of developing health workforce strategic plans in Africa: a document analysis. BMJ Glob. Health 2022, 7, e008418. [Google Scholar] [CrossRef] [PubMed]
- Nyoni J, Gbary A, Awases M, Ndecki P, Chatora R. Policies and Plans for Human Resources for Health: Guidelines for Countries in the WHO African region. Brazaville, Congo: WHO Press, 2006 9290231041XXXX [15 January 2020]. Available online: https://www.who.int/workforcealliance/knowledge/toolkit/15.pdf.
- Cleland, J.; MacLeod, A.; Ellaway, R.H. CARDA: Guiding document analyses in health professions education research. Med Educ. 2022, 57, 406–417. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Sainsbury, P.; Craig, J. Consolidated criteria for reporting qualitative research (COREQ): A 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care 2007, 19, 349–357. [Google Scholar] [CrossRef] [PubMed]
- Walt, G.; Gilson, L. Reforming the health sector in developing countries: the central role of policy analysis. Health Policy Plan. 1994, 9, 353–370. [Google Scholar] [CrossRef] [PubMed]
- Government of Botswana. General Orders Covering the Conditions of Service of the Public Service of the Republic of Botswana. 1996.
- Public Service Act (Act No. 30 of 2008 - Cap. 26:01): S.I. 19, 2010, (2010). Available online: https://uclgafrica-alga.org/wp-content/uploads/2019/05/Public-service-act-Botswana.pdf (accessed on 10 December 2022).
- Khumalo NS. An Evaluation of the “In-service Training Policy” in Swaziland with specific reference to the Ministry of Commerce, Industry and Trade and the Ministry of Health: KwaZulu-Natal; 2015.
- Government of Lesotho. National Manpower Development Council Act (Act No. 8 of 1978). 1978.
- Government of Lesotho. Loan Bursary Fund Regulations: Supplement No. 1 to Gazette No. 29 of 11th August, 1978 (Legal Notice No. 20 of 1978). 1978.
- Government of Swaziland. The in-service training policy of 2000. Mbabane, Swaziland: Ministry of Public Service, 2000.
- Government of Lesotho. National Strategic Development Plan 2012/13-2016/17: Growth and Development Strategic Framework. Maseru, Lesotho: 2012 [10 December 2022]. Available online: https://hivstar.lshtm.ac.uk/files/2017/11/national-strategic-development-plan-201213-201617-LESOTHO.pdf.
- Government of the Kingdom of Eswatini. The Kingdom of Eswatini Strategic Road Map: 2019-2022. [10 December 2022]. Available online: https://www.cabri-sbo.org/uploads/bia/Swaziland_2019_Planning_External_NationalPlan_NatGov_COMESASADC_English.pdf.
- Government of the Kingdom of Swaziland. The Swaziland Poverty Reduction Strategy and Action Plan (PRSAP). 2007 [10 December 2022]. Available online: https://www.tralac.org/files/2012/12/Final-Poverty-Reduction-Strategy-and-Action-Plan-for-Swaziland.pdf.
- Ministry of Health of the Kingdom of Swaziland. Policy for Human Resources for Health. 2012 [10 December 2022]. Available online: https://extranet.who.int/countryplanningcycles/sites/default/files/planning_cycle_repository/swaziland/policy_for_human_resources_for_health.pdf.
- Government of Botswana. Guidelines governing award of sponsorship. Goborone, Botswana: Ministry of Education, Department of Tertiary Education Financing, 2011 [cited 2008 Edition].
- Mthethwa KF. Training and localisation policy: A case study of Swaziland: University of the Western Cape; 2003.
- Swaziland. The Immigration Act, 1964. 1965 [10 December 2022]. Available online: https://www.ilo.org/dyn/natlex/docs/ELECTRONIC/86516/97729/F480334340/SWZ86516.pdf.
- Swaziland Ministry of Education and Training. The Swaziland Education and Training Sector Policy. 2011 [10 December 2022]. Available online: https://planipolis.iiep.unesco.org/sites/default/files/ressources/swazilandeducationsectorpolicy2011.pdf.
- Government of Swaziland. The National Development Strategy (NDS). Mbabane, Swaziland: 2014 [10 March 2023]. Available online: https://www.undp.org/sites/g/files/zskgke326/files/migration/sz/UNDP_SZ_Poverty_National_Development_Strategy.pdf.
- Government of Botswana. Vision 2016: A long term vision for Botswana. Gaborone, Botswana: 1999 [10 March 2023]. Available online: https://faolex.fao.org/docs/pdf/BOT181142.pdf.
- Fee, E.; Brown, T.M. A return to the social justice spirit of Alma-Ata. Am J Public Health 2015, 105, 1096–1097. [Google Scholar] [CrossRef] [PubMed]
- Fee, E.; Brown, T.M. Declaration of ALMA-ATA. Am J Public Health 2015, 105, 1094–1095. [Google Scholar] [CrossRef] [PubMed]
- Adeleye, O.A.; Ofili, A.N. Strengthening Intersectoral Collaboration for Primary Health Care in Developing Countries: Can the Health Sector Play Broader Roles? J. Environ. Public Health 2010, 2010, 272896. [Google Scholar] [CrossRef] [PubMed]
- Kerry, V.B.; Ahaisibwe, B.; Malewezi, B.; Ngoma, D.; Daoust, P.; Stuart-Shor, E.; Mannino, C.A.; Day, D.; Foradori, L.; Sayeed, S.A. Partnering to Build Human Resources for Health Capacity in Africa: A Descriptive Review of the Global Health Service Partnership’s Innovative Model for Health Professional Education and Training From 2013-2018. Int. J. Heal. Policy Manag. 2020, 11, 919–927. [Google Scholar] [CrossRef]
- Emerson, K. Collaborative governance of public health in low- and middle-income countries: lessons from research in public administration. BMJ Glob. Health 2018, 3, e000381. [Google Scholar] [CrossRef] [PubMed]
- Peters BG. Policy Problems and Policy Design. Cheltenham, UNITED KINGDOM: Edward Elgar Publishing Limited; 2018.
- de Vries, E.; Reid, S. Do South African medical students of rural origin return to rural practice? South African Medical Journal 2003, 93, 789–793 Epub 2003/12/05 PubMed PMID: 14652974. [Google Scholar] [PubMed]
- Rabinowitz, H.K. Estimating the percentage of primary care rural physicians produced by regular and special admissions policies. Acad. Med. 1986, 61, 598–600. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, H.K. The effects of a selective medical school admissions policy on increasing the number of family physicians in rural and physician shortage areas. Res Med Educ. 1987, 26, 157–162. [Google Scholar] [PubMed]
- Rabinowitz, H.K. Evaluation of a Selective Medical School Admissions Policy to Increase the Number of Family Physicians in Rural and Underserved Areas. New Engl. J. Med. 1988, 319, 480–486. [Google Scholar] [CrossRef] [PubMed]
- Rabinowitz, H.K. The role of the medical school admission process in the production of generalist physicians. Acad. Med. 1999, 74, S39–S44. [Google Scholar] [CrossRef] [PubMed]
- Grobler, L.; Marais, B.J.; Mabunda, S. Interventions for increasing the proportion of health professionals practising in rural and other underserved areas. Cochrane Database Syst. Rev. 2015, 2015, CD005314. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).