1. Introduction
Early-onset scoliosis (EOS) is a progressive disorder that includes complex curvatures of the pediatric spine related to different etiologies (idiopathic, congenital, syndromic, and neuromuscular) in children younger than 10 years. If left untreated, EOS in these patients may lead to poor respiratory and cardiac development and progressive deformities and cause complex and difficult-to-treat spinal problems [1-3]. Currently, surgical treatments with growth-preserving instrumentation (GPI) techniques without growth arrest are preferred in cases of high-angle and progressive EOS. Several surgical methods have been reported in the literature; these include traditional growing rods (TGR), vertically expandable titanium ribs (VEPTR), and magnetically controlled growing rods (MCGR) are applied for their spinal distraction effects and the Shilla technique (Shilla) and Luque Trolley technique (Luque Trolley) are applied owing to their growth-guidance effects and appications in vertebral body tethering (VBT), which are fairly new modalities applied to the convex side of the curvature and whose compressive effect is utilized during growth[4-9]. The Shilla technique involves the use of different distraction and compression systems when compared with other GPI techniques. This is attributable to the passive growth guidance effect of the Shilla technique when correcting the deformity and the absence of the need for planned surgery [6,8-10]. Although screw heads attached proximal and distal to the instrumentation ensure that the apical vertebral segments remain fixed, the segments can be followed without the need for lengthening with deformity correction and orientation effect without distraction [
11,
12].
In EOS cases treated using GPI, problems related to wound healing., infection, implant failure, metallosis, early fusion, neurologic deterioration, and unplanned surgeries may occur regardless of the technique used. The purpose of EOS surgery is to avoid postoperative complications when selecting the appropriate GPI for the patient. Many multicenter studies have compared the advantages and disadvantages of different growth-friendly techniques [1,13-15]. Similar to other techniques, various problems may occur as a result of Shilla application. The Shilla technique aims to avoid these problems and the problems caused by active lengthening procedures.
Studies on the effects of implant-related complications associated with Shilla growth guidance on the correction of the patient's deformity and growth are insufficient. The impact of complications on treatment requires further investigation. For this purpose, the complications encountered with Shilla growth guidance in EOS cases with different etiologies and the adverse effects resulting from these complications were analyzed. Furthermore, whether implant-related complications have a negative effect on deformity correction and growth in patients treated with the Shilla technique was investigated.
2. Materials and Methods
A total of 26 patients underwent Shilla treatment for EOS with different etiologies between January 2013 and December 2021. Of these 26, 16 patients were examined for a follow-up period of at least 1 year (30.8 ± 29.2) met the inclusion criteria and were evaluated in this case-control series. The improvement in deformity and growth effect as well as implant-related complications and unplanned surgeries were retrospectively analyzed. Interpatient comparisons were performed between those with and without implant-related complications during the treatment period. Although 3 patients (18.8%) were graduated, treatment was continued for 13 patients. Ethics committee approval was obtained from our hospital (KAEK/2021.12.296). Clinical and radiological Cobb angles, spine length between T1–T12 and T1–S1, kyphosis and lordosis angles in the sagittal plane, apical vertebral levels, coronal and sagittal balances, pelvis and shoulder balances, EOSQ-24 (Early Onset Scoliosis 24-Item Questionnaire) results were measured preoperatively, in the early postoperative period, and at the final follow-up. Inclusion criteria were as follows: (1) age of 5–10 years or bone age development of <10 years, (2) Cobb angle of >45°, (3) increase in Cobb angle of >10° within 1 year, (4) open triradiate cartilage, (5) Sanders stage Sanders stage of less than 3, (6) unsuccessful conservative treatment, (7) no deformity surgery, and (8) regular follow-up > 1 year by the responsible author. Exclusion criteria were as follows (1) age of <5 years and >10 years, (2) Cobb angle of <45°, (3) closed triradiate cartilage, (4) Sanders stage of Sanders stage of greater than or equal to 3, (5) improvement in curvature with conservative treatment, (6) previous surgery for spinal curvature, and (7) no regular follow-up. In the present study, whether implant-related problems had a negative effect on deformity correction and spinal growth was investigated, and unplanned surgeries and complications were retrospectively evaluated.
Demographic characteristics, etiology, follow-up periods, complications, and magnetic resonance imaging (MRI) results were recorded. For radiological evaluation, standard whole spinal orthoroentgenography was obtained preoperatively, in the early postoperative period, and at the last follow-up examination in standing position and in seated position for neuromuscular and syndromic patients who could not stand). The entire spinal region was evaluated with MRI for preoperative intraspinal pathology control. MRI evaluation was performed by a radiologist experienced in spinal radiology
(Table 1).
Statistical Analysis
Mean, standard deviation, median, minimum, maximum, frequency, and ratio values were used to present descriptive statistics. Kolmogorov–Smirnov test was used to check the conformity of variables to normal distribution. Independent samples t test and Mann–Whitney U test were used to analyze independent quantitative data. Paired Samples t test and Wilcoxon test were used to analyze dependent quantitative data. Spearman correlation analysis was used for correlation analysis. SPSS 28.0 program was used in the analysis. The results were measured and compared by two spine surgeons. Intra- and inter-correlations were high (intraclass correlation coefficient >0.80, p<0.05).
3. Results
In measurements recorded during the early postoperative period and final follow-up, improvements in Cobb angle and shoulder balance angle, and increase in T1-T12 and T1-S1 length were significant compared with preoperative measurements (p<0.05). No significant change was observed in terms of kyphosis (T2-T12), lordosis (L1-S1), coronal balance, sagittal balance, and pelvic balance (p>0.05)
(Table 2).
Kyphosis (T2-T12) values during the preoperative period, early postoperative period, and final follow-up showed no significant intergroup differences (p>0.05). The group with complications showed significantly lower lordosis (L1-S1) values in the postoperative and final follow-up measurements than the group without complications (p<0.05). The decrease in lordosis (L1-S1) between preoperative and early postoperative measurements was significantly higher in the group with complications than that in the group without complications (p<0.05). In the early postoperative period and final follow-up measurements, no significant intergroup difference was observed in terms of the lordosis (L1-S1) values (p>0.05). In the preoperative, early postoperative period, and final follow-up measurements of coronal, sagittal, shoulder, and pelvic balance, no significant intergroup differences were noted (p>0.05). In the group with complications, final follow-up measurement of shoulder balance showed a significant decrease compared with the preoperative period (p<0.05). The change in preoperative and early postoperative period shoulder balance measurements showed no significant differences between the groups with and without complications (p>0.05). The change in early postoperative period and final follow-up shoulder balance measurements was not significantly different between the groups with and without complications (p>0.05). In the group with complications, early pelvic balance showed a significant decrease in terms of the values measured in the postoperative and preoperative periods (p<0.05). All components of the EOSQ-24 score except the daily living domain showed improvements in the postoperative period (p<0.05)
(Table 6).
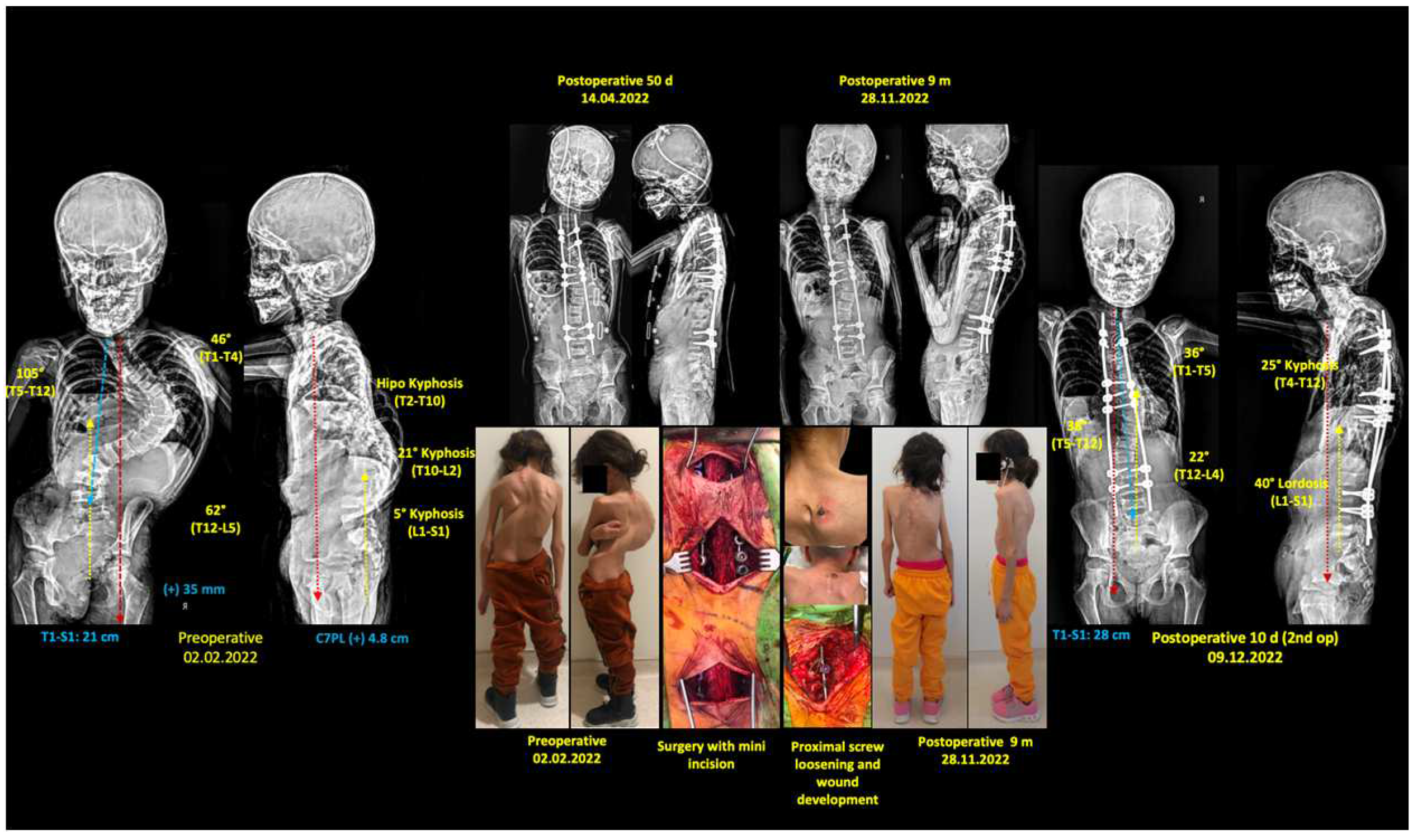
In 8 patients (50%) who underwent Shilla treatment for EOS, no complications developed during the treatment period, spinal growth and curve correction were not adversely affected, and no unplanned surgery was required. Postoperative implant-related complications were observed in 8 patients (50%). Proximal screw loosening, screw malposition, proximal junctional kyphosis (PJK), wound problems, rod breakage, metallosis, and infection occurred. Of the 8 patients with implant-related complications, 6 (37.5%) required unplanned surgery. Unplanned surgery was most commonly performed because of implant failure in the proximal region in 5 cases (31.25%) and deep tissue infection around the implant in 1 case (6.25%). Unplanned surgery was performed 4 times in 1 patient, 2 times in 1 patient, and 1 time in 4 patients. Analysis of the etiologies and index surgical age distribution of the 6 patients who required unplanned surgery revealed that 2 were idiopathic (115 months, 116 months), 3 were syndromic (Marfan 60 months, Deletion 55 months, Doose 72 months), and 1 was NMS (CP 61 months). Loosening of the proximal pedicle screws, PJK and skin irritation were observed in five cases, whereas four cases developed wounds as a result of skin irritation. In all cases requiring unplanned surgery, metallosis caused by movement in the vicinity of the implant in the screw-rod connection area was observed. The highest number of unplanned surgeries was 4 in a patient with deletion syndrome (55 months, male, follow-up 26 months). The accompanying kyphosis deformity (thoracic proximal kyphosis of 62°) and inadequate bone morphology caused early loosening of the proximal screw fixation. Although pedicle screw fixation and rod placement provided initial improvement, early proximal implant failure, rod displacement, skin wound problems, and PJK resulted in repeated unplanned surgical interventions. In the long term, maintenance of growth was planned while concurrently ensuring correction of the proximal kyphosis deformity at the appropriate stage. In a patient with Marfan syndrome with high angle scoliosis and kyphosis deformity (60 months, female, follow-up 12 months), dislocation of the proximal screw required unplanned surgery caused as a result of implant failure
(Figure 1).
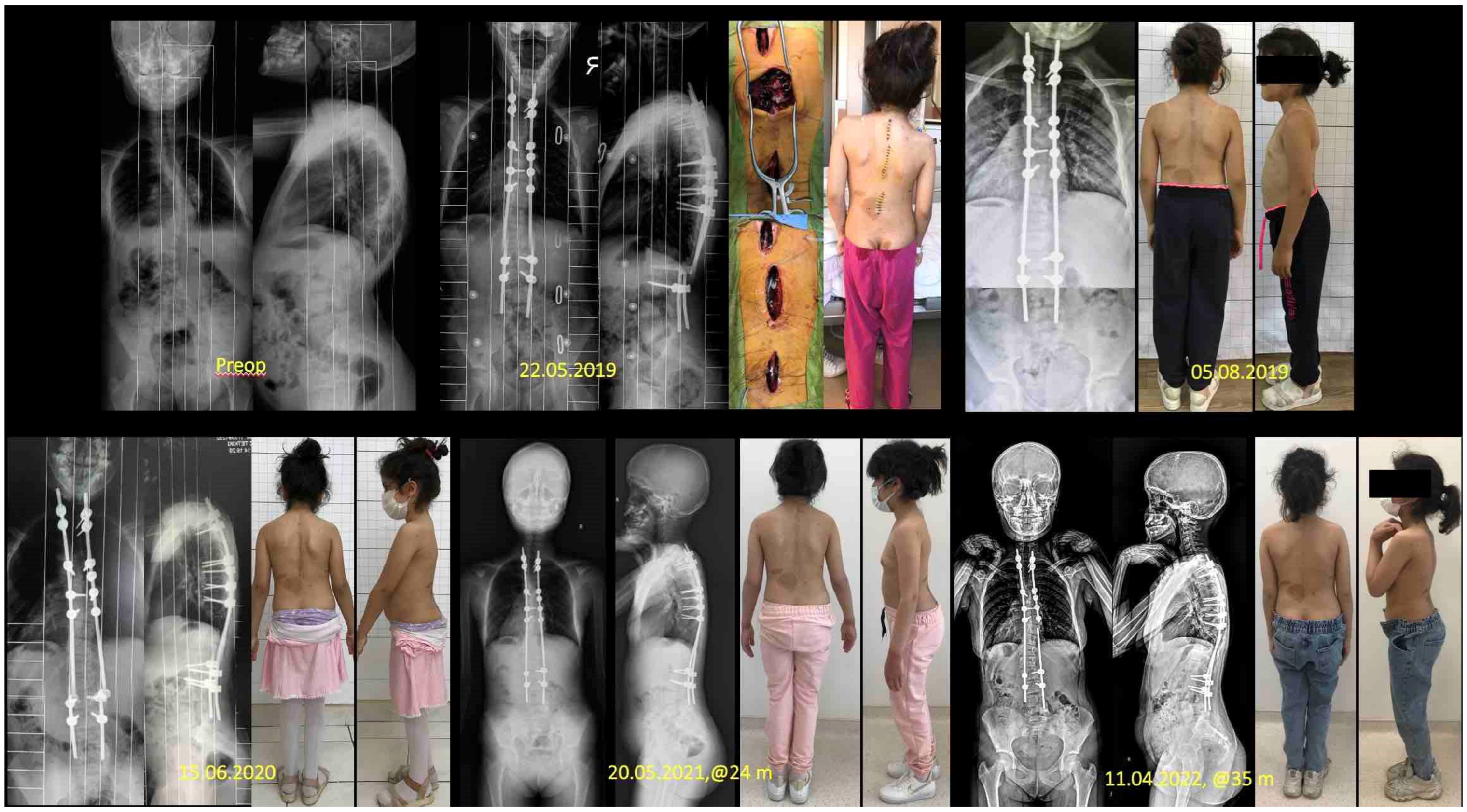
In a patient with NMS-CP (61 months, male, follow-up 16 months), unplanned surgery was performed 3 months after the index surgery due to screw-rod loosening and rod displacement caused by dislocation of screw caps in the concave apical region with proximal failure. Infection developed in one case (6.25%) (72-month-old girl with Doose syndrome, follow-up period over 12 months) following respiratory tract infection in the peri-implant deep tissue after low body resistance five months after surgery. The deep wound resolved after peri-implant debridement and antibiotherapy according to the recommendations of the infectious diseases unit, and no additional problems were encountered in the follow-up. Rod breakage was observed in two cases (12.5%) unilaterally on the concave side of the curve immediately distal to the apical fusion site. No additional unplanned surgery for unilateral rod breakage was required in both cases. An 8-year-old girl with NF-1 continued to be followed-up uneventfully in the 4th year of treatment (
Figure 2). A patient with Down syndrome did not require any intervention during 8 years of follow-up and did not require additional surgery despite unilateral rod breakage. Graduation surgery with fusion was uneventful but the patient died due to sudden cardiac arrest during postoperative CVP catheter removal.
The treatment of the patients who underwent surgery for EOS was accompanied by several additional challenges in terms of anesthesia and reanimation. Video laryngoscope guidance was needed in two of our patients (12.5%) because of difficult intubation. Postoperative respiratory problems were observed in three cases (18.75%). Prolonged treatment in the postoperative intensive care unit and in the ward was required. The early difficulties encountered in the administration of anesthesia and normalization of postoperative respiration were overcome with good care and rehabilitation. In all patients, neuromonitoring was used in index surgeries and when additional surgery was required; no neurological changes were observed during these procedures.
4. Discussion
Increasingly intensive efforts have been undertaken in EOS treatment in the last 15 years owing to improvements in treatment algorithms and GPI techniques [6-8,10,16-19]. One of these methods, the Shilla technique is especially recommended as a method that guides growth by reducing the number of surgical interventions while facilitating the correction of the deformity [
11,
12]. The results and complication rates of EOS treatment have been reported in various studies [15,20-22]. Reportedly, the Shilla procedure is a suitable option to treat EOS with different etiologies; however, this procedure is associated with moderate complication rates [
12,
20]. Wilkinson et al. [
20] reported an overall implant-related complication rate of 29% after the Shilla procedure with a minimum follow-up of 5 years. Screw pull-out and rod breakage occurred in 14% and 14% of the patients, respectively, and deep and superficial infections developed in 9.5% and 4.7% of the patients. In the literature, the Shilla growth guidance technique is an alternative to distraction-based growing rod (GR) systems [
12]. Comparing both applications, Andras et al. showed a greater improvement in Cobb angle and a greater increase in T1-S1 length in patients who underwent GR compared to Shilla [
14]. In their study comparing the radiologic results of TGR and Shilla treatment, Luhmann et al. did not report a significant intergroup difference in clinical parameters during follow-up, and they found that the number of operations was significantly higher in the GBR group [
15]. Loss of correction and the need for osteotomy were reported as disadvantages of Shilla treatment [
23]. Loss of correction via crankshafting or adding-on (e.g. distal migration) was reported in a significant percentage of patients undergoing Shilla growth guidance [
20,
24]. Reportedly, concave side osteotomies may be required and may lead to serious complications [
23]. Agarwal et al. described the modified Shilla approach (active apex correction: APC) as a solution that can help dynamically re-modulate the apex of the deformity and reduce correction loss. Modified Shilla approach was compared with the TGR system and no significant intergroup difference was noted in terms of correction and growth [
23]. Biomechanical complications were more frequent in the GR system (13 of 26 cases) compared to APC (5 of 20 cases). Surgeries related to active extensions with TGR and longer follow-up period were thought to be effective [
23]. In the literature, several comparative studies with other growth-friendly techniques have been conducted to better evaluate the efficacy of treatment in EOS. Haapala et al. [
1] compared MCGR with the Shilla technique and reported similar EOSQ-24 results between the two methods. Furthermore, the lowest postoperative scores were observed in the daily living domain in both treatment groups. In our patients, we observed significant improvement in all domains of EOSQ-24 results after Shilla treatment compared to pre-treatment scores, except for the daily living domain. Children with EOS are prone to develop pulmonary complications after repeated anesthesia procedures. Difficult intubation may be observed more frequently especially in neuromuscular and snydromic cases [
22]. Furthermore, the potentially harmful effects of frequent anesthesia exposure are not yet fully understood.
As implant-related complications, screw dislocation occurred in 31.25% [
5], skin wound problems occurred in 25% [
4], rod breakage occurred in 12.5% [
2], and deep infection occurred in 6.25% [
1] of the patients. A total of 10 unplanned surgeries were performed: 1 in four patients, 2 in one patient, and 4 in one patient. In patients requiring surgery, signs of metallosis were observed in the rod screw junction. In our series, we observed difficult intubation in 2 (12.5%) (syndromic) cases and prolonged postoperative intensive care unit stay in 3 (18.7%) syndromic cases.
In the present study, preoperative and postoperative data were evaluated retrospectively. Patients were operated and followed up by the responsible author from the indication to the final follow-up. Complications encountered during the follow-up period were closely monitored and managed in the same manner. The long treatment process and patients dropping out of follow-up for various reasons resulted in a decrease in the number of patients and a shortened follow-up period. The lack of comparative studies with other growth-friendly surgical techniques constituted the main limitations of our study. Scoliosis deformity was significantly improved compared to preoperative measurements, spine length was significantly increased, and quality of life scores also improved significantly. The analyses performed to evaluate the effect of complications showed that the lordosis angle and T1-S1 length were significantly lower in the early and final postoperative controls in those who developed complications compared to those who did not develop complications. Although Shilla treatment provided significant improvement in deformity correction and spine height compared to the preoperative period, implant-related complications had a relatively negative effect on spine height and lumbar lordosis.
5. Conclusions
Various implant-related problems were encountered in patients with EOS treated with the Shilla technique. Although implant-related complications were observed after the Shilla procedure, an improvement in the correction of the initial deformity and a significant increase in spinal height were possible. When patients with implant-related complications were compared with uneventful patients, there was no significant difference between the two groups in terms of spinal growth and deformity correction. The T1-S1 length and lumbar lordosis appeared to be affected especially in patients with complications compared to uncomplicated patients. In conclusion, it should be kept in mind that careful planning and long-term follow-up will be required when deciding on treatment with the Shilla method in EOS patients. Avoiding complications and minimizing their negative effects is crucial for successful treatment. Therefore, close follow-up of patients and management of treatment by an experienced team is recommended.
Author Contributions
“Conceptualization, MBB.; methodology, MBB., F.A. and N.S.; software, K.A.; validation, M.B.B., K.A. and A.O.A.; formal analysis, M.B.B., M.Ç.; investigation, M.B.B, A.V.Ö.; resources, M.B.B., A.O.A.; data curation, N.S., F.A.; writing—original draft preparation, M.B.B.; writing—review and editing, M.B.B.; visualization, K.A., A.O.A; supervision, M.B.B.; project administration, M.B.B.; funding acquisition, M.B.B. All authors have read and agreed to the published version of the manuscript.”.
Funding
“This research received no external funding”.
Institutional Review Board Statement
“The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of BAŞAKŞEHİR ÇAM VE SAKURA ŞEHİR HASTANESİ (KAEK/2021.12.296 and 14.01.2022).”.
Informed Consent Statement
“Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper”.
Conflicts of Interest
“The authors declare no conflict of interest.”.
References
- Haapala, H.; Saarinen, A. J.; Salonen, A.; Helenius, I. Shilla Growth Guidance Compared with Magnetically Controlled Growing Rods in the Treatment of Neuromuscular and Syndromic Early-Onset Scoliosis. Spine (Phila Pa 1976) 2020, 45, E1604–E1614. https://doi.org/10.1097/BRS.0000000000003654. [CrossRef]
- Williams, B. A.; Matsumoto, H.; McCalla, D. J.; Akbarnia, B. A.; Blakemore, L. C.; Betz, R. R.; Flynn, J. M.; Johnston, C. E.; McCarthy, R. E.; Roye, D. P.; Skaggs, D. L.; Smith, J. T.; Snyder, B. D.; Sponseller, P. D.; Sturm, P. F.; Thompson, G. H.; Yazici, M.; Vitale, M. G. Development and Initial Validation of the Classification of Early-Onset Scoliosis (C-EOS). J. Bone Joint Surg. Am. 2014, 96, 1359–1367. https://doi.org/10.2106/JBJS.M.00253. [CrossRef]
- Pehrsson, K.; Larsson, S.; Oden, A.; Nachemson, A. Long-Term Follow-Up of Patients with Untreated Scoliosis. A Study of Mortality, Causes of Death, and Symptoms. Spine (Phila Pa 1976) 1992, 17, 1091–1096. https://doi.org/10.1097/00007632-199209000-00014. [CrossRef]
- Clement, R.C., Yaszay, B., McClung, A., Bartley, C.E., Nabizadeh, N., Skaggs, D.L., Thompson, G.H., Boachie-Adjei, O., Sponseller, P.D., Shah, S.A. and Sanders, J.O. Growth-Preserving Instrumentation in Early-Onset Scoliosis Patients with Multi-level Congenital Anomalies. Spine Deform. 2020, 1, 1117–1130. https://doi.org/10.1007/s43390-020-00124-2. [CrossRef]
- McCarthy, R. E.; Sucato, D.; Turner, J. L.; Zhang, H.; Henson, M. A.; McCarthy, K. Shilla Growing Rods in a Caprine Animal Model: A Pilot Study. Clin. Orthop. Relat. Res. 2010, 468, 705–710. https://doi.org/10.1007/s11999-009-1028-y. [CrossRef]
- Hardesty, C. K.; Huang, R. P.; El-Hawary, R.; Samdani, A.; Hermida, P. B.; Bas, T.; Balioğlu, M. B.; Gurd, D.; Pawelek, J.; McCarthy, R.; Zhu, F.; Luhmann, S.; Growing Spine Committee of the Scoliosis Research Society. Early-Onset Scoliosis: Updated Treatment Techniques and Results. Spine Deform. 2018, 6, 467–472. https://doi.org/10.1016/j.jspd.2017.12.012. [CrossRef]
- Ruiz, G.; Torres-Lugo, N. J.; Marrero-Ortiz, P.; Guzmán, H.; Olivella, G.; Ramírez, N. Early-Onset Scoliosis: A Narrative Review. E.F.O.R.T. Open Rev. 2022, 7, 599–610. https://doi.org/10.1530/EOR-22-0040. [CrossRef]
- Gomez, J. A.; Lee, J. K.; Kim, P. D.; Roye, D. P.; Vitale, M. G. ‘Growth friendly’ Spine Surgery: Management Options for the Young Child with Scoliosis. J. Am. Acad. Orthop. Surg. 2011, 19, 722–727. https://doi.org/10.5435/00124635-201112000-00002. [CrossRef]
- Alkhalife, Y. I.; Padhye, K. P.; El-Hawary, R. New Technologies in Pediatric Spine Surgery. Orthop. Clin. North Am. 2019, 50, 57–76. https://doi.org/10.1016/j.ocl.2018.08.014. [CrossRef]
- Senkoylu, A.; Riise, R. B.; Acaroglu, E.; Helenius, I. Diverse Approaches to Scoliosis in Young Children. E.F.O.R.T. Open Rev. 2020, 5, 753–762. https://doi.org/10.1302/2058-5241.5.190087. [CrossRef]
- McCarthy, R. E.; Luhmann, S.; Lenke, L.; McCullough, F. L. The Shilla Growth Guidance Technique for Early-Onset Spinal Deformities at 2-Year Follow-Up: A Preliminary Report. J. Pediatr. Orthop. 2014, 34, 1–7. https://doi.org/10.1097/BPO.0b013e31829f92dc. [CrossRef]
- McCarthy, R. E.; McCullough, F. L. Shilla Growth Guidance for Early-Onset Scoliosis: Results After a Minimum of Five Years of Follow-Up. J. Bone Joint Surg. Am. 2015, 97, 1578–1584. https://doi.org/10.2106/JBJS.N.01083. [CrossRef]
- Luhmann, S. J.; McCarthy, R. E. A Comparison of Shilla Growth Guidance System and Growing Rods in the Treatment of Spinal Deformity in Children Less Than 10 Years of Age. J. Pediatr. Orthop. 2017, 37, e567–e574. https://doi.org/10.1097/BPO.0000000000000751. [CrossRef]
- Andras, L. M.; Joiner, E. R.; McCarthy, R. E.; McCullough, L.; Luhmann, S. J.; Sponseller, P. D.; Emans, J. B.; Barrett, K. K.; Skaggs, D. L.; Growing Spine Study Group. Growing Rods Versus Shilla Growth Guidance: Better Cobb Angle Correction and T1-S1 Length Increase but More Surgeries. Spine Deform. 2015, 3, 246–252. https://doi.org/10.1016/j.jspd.2014.11.005. [CrossRef]
- Luhmann, S. J.; Smith, J. C.; McClung, A.; McCullough, F. L.; McCarthy, R. E.; Thompson, G. H.; Growing Spine Study Group. Radiographic Outcomes of Shilla Growth Guidance System and Traditional Growing Rods Through Definitive Treatment. Spine Deform. 2017, 5, 277–282. https://doi.org/10.1016/j.jspd.2017.01.011. [CrossRef]
- Skaggs, D. L.; Akbarnia, B. A.; Flynn, J. M.; Myung, K. S.; Sponseller, P. D.; Vitale, M. G.; Chest Wall and Spine Deformity Study Group; Growing Spine Study Group; Pediatric Orthopaedic Society of North America; Scoliosis Research Society Growing Spine Study Committee. A Classification of Growth Friendly Spine Implants. J. Pediatr. Orthop. 2014, 34, 260–274. https://doi.org/10.1097/BPO.0000000000000073. [CrossRef]
- Tis, J. E.; Karlin, L. I.; Akbarnia, B. A.; Blakemore, L. C.; Thompson, G. H.; McCarthy, R. E.; Tello, C. A.; Mendelow, M. J.; Southern, E. P.; Growing Spine Committee of the Scoliosis Research Society. Early Onset Scoliosis: Modern Treatment and Results. J. Pediatr. Orthop. 2012, 32, 647–657. https://doi.org/10.1097/BPO.0b013e3182694f18. [CrossRef]
- Helenius, I. J. Treatment Strategies for Early-Onset Scoliosis. E.F.O.R.T. Open Rev. 2018, 3, 287–293. https://doi.org/10.1302/2058-5241.3.170051. [CrossRef]
- Zhang, Y. B.; Zhang, J. G. Treatment of Early-Onset Scoliosis: Techniques, Indications, and Complications. Chin. Med. J. (Engl.) 2020, 133, 351–357. https://doi.org/10.1097/CM9.0000000000000614. [CrossRef]
- Wilkinson, J. T.; Songy, C. E.; Bumpass, D. B.; McCullough, F. L.; McCarthy, R. E. Curve Modulation and Apex Migration Using Shilla Growth Guidance Rods for Early-Onset Scoliosis at 5-Year Follow-Up. J. Pediatr. Orthop. 2019, 39, 400–405. https://doi.org/10.1097/BPO.0000000000000983. [CrossRef]
- Ahmad, A. A.; Agarwal, A. Active Apex Correction: An Overview of the Modified Shilla Technique and Its Clinical Efficacy. J. Clin. Orthop. Trauma 2020, 11, 848–852. https://doi.org/10.1016/j.jcot.2020.07.013. [CrossRef]
- Latalski, M.; Fatyga, M.; Sowa, I.; Wojciak, M.; Starobrat, G.; Danielewicz, A. Complications in Growth-Friendly Spinal Surgeries for Early-Onset Scoliosis: Literature Review. World J. Orthop. 2021, 12, 584–603. https://doi.org/10.5312/wjo.v12.i8.584. [CrossRef]
- Agarwal, A.; Aker, L.; Ahmad, A. A. Active Apex Correction (Modified SHILLA Technique) Versus Distraction-Based Growth Rod Fixation: What Do the Correction Parameters Say? Spine Surg. Relat. Res. 2020, 4, 31–36. https://doi.org/10.22603/ssrr.2019-0045. [CrossRef]
- Murphy, R. F.; Mooney III, J. F. The Crankshaft Phenomenon. J. Am. Acad. Orthop. Surg. 2017, 25, e185–e193. https://doi.org/10.5435/JAAOS-D-16-00584. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).