Submitted:
05 May 2023
Posted:
06 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Materials and Methods
2.1. Study design and setting
2.2. Participants
2.3. Risk-screening tool
2.4. Data analysis
3. Results
3.1. Characteristics of return visits by elders
3.2. Return visit reason and time
3.3. Factors associated with return visits by elders
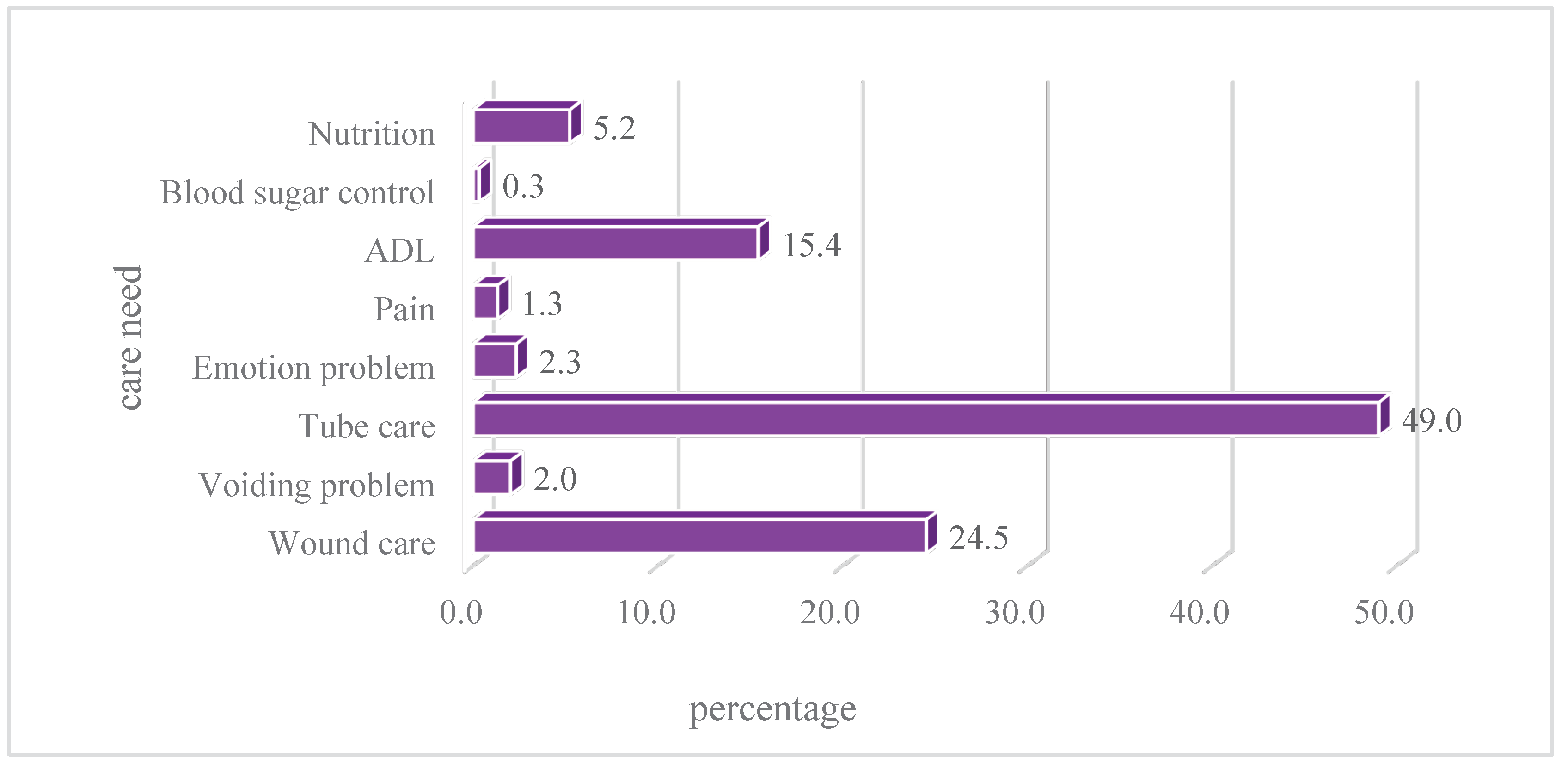
3.4. Distribution of risk factors for return visits by elders
4. Discussion
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Kolk, D.; Kruiswijk, A.F.; MacNeil-Vroomen, J.L.; Ridderikhof, M.L.; Buurman, B.M. Older patients’ perspectives on factors contributing to frequent visits to the emergency department: a qualitative interview study. BMC Public Health 2021, 21, 1709. [Google Scholar] [CrossRef] [PubMed]
- de Gelder, J.; Lucke, J.A.; de Groot, B.; Fogteloo, A.J.; Anten, S.; Heringhaus, C.; et al. Predictors and outcomes of revisits in older adults discharged from the emergency Department. J of Am Geriatr Soc 2018, 66, 735–741. [Google Scholar] [CrossRef] [PubMed]
- Naseer, M.; Agerholm, J.; Fastbom, J.; Schon, P.; Ehrenberg, A.; Dahlberg, L. Factors associated with emergency department revisits among older adults in two Swedish regions: A prospective cohort study. Arch Gerontol Geriatr 2020, 86, 103960. [Google Scholar] [CrossRef] [PubMed]
- Duseja, R.; Bardach, N.S.; Lin, G.A.; Yazdany, J.; Dean, M.L.; Clay, T.H.; et al. Revisit rates and associated costs after an emergency department encounter: A multistate analysis. Ann of Intern Med 2015, 162, 750–756. [Google Scholar] [CrossRef] [PubMed]
- Aminzadeh, F.; Dalziel, W.B. Older adults in the emergency department: A systematic review of patterns of use, adverse outcomes, and effectiveness of interventions. Ann Emerg Med 2002, 39, 238–247. [Google Scholar] [CrossRef] [PubMed]
- Tsai, C.L.; Ling, D.A.; Lu, T.C.; Lin, J.C.; Huang, C.H.; Fang, C.C. Inpatient outcomes following a return visit to the emergency department: A nationwide cohort study. West J Emerg Med 2021, 22, 1124–1130. [Google Scholar] [CrossRef] [PubMed]
- Friedmann, P.D.; Jin, L.; Karrison, T.G.; Hayley, D.C.; Mulliken, R.; Walter, J.; et al. Early revisit, hospitalization, or death among older persons discharged from the ED. Am J Emerg Med 2001, 19, 125–129. [Google Scholar] [CrossRef] [PubMed]
- Imsuwan, I. Characteristics of unscheduled emergency department return visit patients within 48 hours in Thammasat University Hospital. J Med Assoc Thai 2011, 94, S73–S80. [Google Scholar]
- Lerman, B.; Kobernick, M.S. Return visits to the emergency department. J Emerg Med 1987, 5, 359–362. [Google Scholar] [CrossRef]
- Han, C.Y.; Chen, L.C.; Barnard, A.; Lin, C.C.; Hsiao, Y.C.; Liu, H.R.; et al. Early revisit to the Emergency department: An integrative review. J Emerg Nurs 2015, 41, 285–295. [Google Scholar] [CrossRef]
- Montoy, J.C.C.; Tamayo-Sarver, J.; Miller, G.A.; Baer, A.E.; Peabody, C.R. Predicting emergency department "bouncebacks": A retrospective cohort analysis. West J Emerg Med 2019, 20, 865–874. [Google Scholar] [CrossRef] [PubMed]
- Hogervorst, V.M.; Buurman, B.M.; De Jonghe, A.; van Oppen, J.D.; Nickel, C.H.; Lucke, J.; et al. Emergency department management of older people living with frailty: A guide for emergency practitioners. Emerg Med J 2021, 38, 724–9. [Google Scholar] [CrossRef] [PubMed]
- Department of Household Registration Taiwan. Important indicators of population age structure. Retrieved from: https://www.ris.gov.tw/app/portal/346 (accessed on 19 April 2023).
- Lin, S.C.; Ko, M.C.; Tang, S.C.; Chen, C.Y.; Chen, C.C. Prevalence of and predictors for frequent utilization of emergency department of older adult. Hospital Administration & Medical Affair Management 2018, 3, 43–62. [Google Scholar] [CrossRef]
- Wu, S.C. Evaluation of the impact of aging population on emergency medicine and suggestions for avoidable emergency department visits. J Gerontol Service Manag 2015, 3, 35–40. [Google Scholar] [CrossRef]
- Factors associated with unscheduled return visits: a study of the patient’s perspective. J Emerg Med 2004, 6, 306–314.
- Huang, J.A.; Weng, R.H.; Tsai, W.C.; Hu, W.H.; Yang, D.Y. Analysis of emergency department utilization by elderly patients under National Health Insurance. Kaohsiung J Med Sci 2003, 19, 113–120. [Google Scholar] [CrossRef] [PubMed]
- Han, C.Y.; Lin, C.C.; Goopy, S.; Hsiao, Y.C.; Barnard, A. Elders' experiences during return visits to the emergency department: A phenomenographic study in Taiwan. Nurs Res 2017, 66, 304–310. [Google Scholar] [CrossRef]
- Benbassat, J.; Taragin, M. Hospital readmissions as a measure of quality of health care: Advantages and limitations. Arch Intern Med 2000, 160, 1074–1081. [Google Scholar] [CrossRef]
- Driesen, B.; Merten, H.; Wagner, C.; Bonjer, H.J.; Nanayakkara, P.W.B. Unplanned return presentations of older patients to the emergency department: A root cause analysis. BMC Geriatr 2020, 20, 365. [Google Scholar] [CrossRef]
- Rising, K.L.; Padrez, K.A.; O'Brien, M.; Hollander, J.E.; Carr, B.G.; Shea, J.A. Return visits to the emergency department: The patient perspective. Ann Emerg Med 2015, 65, 377–386. [Google Scholar] [CrossRef]
- Morin, C.; Choukroun, J.; Callahan, J.C. Safety and efficiency of a redirection procedure toward an out of hours general practice before admission to an emergency department, an observational study. BMC Emerg Med 2018, 18, 26. [Google Scholar] [CrossRef] [PubMed]
- Meldon, S.W.; Mion, L.C.; Palmer, R.M.; Drew, B.L.; Connor, J.T.; Lewicki, L.J.; et al. A brief risk-stratification tool to predict repeat emergency department visits and hospitalizations in older patients discharged from the emergency department. Acad Emerg Med 2008, 10, 224–232. [Google Scholar] [CrossRef]
- Cox, D.D.; Subramony, R.; Supat, B.; Brennan, J.J.; Hsia, R.Y.; Castillo, E.M. Geriatric falls: Patient characteristics associated with emergency department revisits. West J Emerg Med 2022, 23, 734–738. [Google Scholar] [CrossRef] [PubMed]
- Afilalo, M.; Xue, X.; Colacone, A.; Jourdenais, E.; Boivin, J.F.; Grad, R. Association between access to primary care and unplanned emergency department return visits among patients 75 years and older. Can Fam Physician 2022, 68, 599–606. [Google Scholar] [CrossRef] [PubMed]
- Han, C.Y.; Redley, B.; Lin, C.C.; Chen, L.C.; Ng, C.J.; Wang, L.H. Standard risk assessment forms help reduce preventable harm in older adult inpatients: A retrospective chart review study. J Adv Nurs 2021, 77, 4439–4450. [Google Scholar] [CrossRef] [PubMed]
- Lim, J.; Lee, J. Factors associated with mortality of elderly adults hospitalized via emergency departments in Korea. Korean J Adult Nurs 2020, 32, 273–282. [Google Scholar] [CrossRef]
- Salvi, F.; Mattioli, A.; Giannini, E.; et al. Pattern of use and presenting complaints of elderly patients visiting an Emergency Department in Italy. Aging Clin Exp Res 2013, 25, 583–590. [Google Scholar] [CrossRef] [PubMed]
- Guo, D.Y.; Chen, K.H.; Chen, I.C.; et al. The association between emergency department return visit and elderly patients. J Acute Med 2020, 10, 20–26. [Google Scholar] [CrossRef]
- Chen, C.C.; Cail, J.Y.; Chen, C.Y.; Ko, M.C.; Tang, S.C. Factors associated with three-day revisit to emergency room among elderly patients. Taiwan Geriatr Gerontol 2018, 13, 205–223. [Google Scholar] [CrossRef]
- Lowthian, J.; Straney, L.D.; Brand, C.A.; Barker, A.L.; Smit Pde, V.; Newnham, H.; et al. Unplanned early return to the emergency department by older patients: The safe elderly emergency department discharge (SEED) project. Age Ageing 2016, 45, 255–261. [Google Scholar] [CrossRef]
| Variable | N | % | M(SD) |
|---|---|---|---|
| Gender | |||
| Male | 598 | 50.4 | |
| Female | 589 | 49.6 | |
| Age (Rang:65-103) | 77.44(7.88) | ||
| 65-74 | 468 | 39.46 | |
| 75-84 | 458 | 38.62 | |
| >85 | 260 | 21.92 | |
| Health problems | |||
| Non-trauma | 960 | 80.9 | |
| Trauma | 227 | 19.1 | |
| Return visit time | |||
| Within 24 hours | 500 | 42.2 | |
| 24-48 hours | 394 | 33.2 | |
| 48-72 hours | 292 | 24.6 | |
| Triage | |||
| Emergency | 230 | 18.39 | |
| Urgent | 956 | 80.61 | |
| Reasons for return visits | |||
| Pertaining to previous disease/treatment | 572 | 48.2 | |
| New medical condition | 615 | 51.8 | |
| Revisit outcome | |||
| Discharge from ED | 785 | 66.3 | |
| Admission | 346 | 29.2 | |
| Transfer to another hospital | 27 | 2.3 | |
| AAD | 19 | 1.6 | |
| Expire | 7 | 0.6 | |
| TRST | |||
| Cognitive impairment | 166 | 14.0 | |
| Difficult walking/transferring | 337 | 28.4 | |
| Falls within one month | 128 | 10.8 | |
| Polypharmacy | 577 | 48.7 | |
| Previous ED visited within 30 days | 592 | 49.9 | |
| Hospitalization within 120 days | 289 | 24.3 | |
| Live alone | 8 | 0.7 | |
| Without a caregiver | 825 | 69.5 | |
| Care needs as assessed by nurses | 291 | 24.5 | |
| History of chronic diseases | 1114 | 93.9 |
| Variable | < 24 hrs | Revisit% | OR(95%CI)/p | 24-48 hrs | Revisit% | OR(95%CI)/p | 48-72 hrs | Revisit% | OR(95%CI)/p | |||
| Yes | No | Yes | No | Yes | No | |||||||
| Age | ||||||||||||
| 65-74 | 208 | 260 | 44.4 | 1 | 154 | 314 | 32.9 | 1 | 106 | 362 | 22.6 | 1 |
| 75-84 | 193 | 265 | 42.1 | 1.10(0.85-1.43) /p=0.479 | 153 | 305 | 33.4 | 0.98(0.74-1.29)/p=0.871 | 112 | 346 | 24.5 | 0.90(0.67-1.23)/p=0.517 |
| >85 | 99 | 162 | 37.9 | 1.31(0.96-1.78)/p=0.088 | 87 | 174 | 33.3 | 0.98(0.71-1.35)/ p=0.906 | 74 | 187 | 28.4 | 0.74(0.52-1.05)/ p,0.087 |
| Gender | ||||||||||||
| Female | 238 | 351 | 40.4 | 0.87(0.69-1.10)/p,0.234 | 193 | 396 | 32.8 | 0.96(0.76-1.23)/p,0.757 | 157 | 432 | 26.7 | 1.25(0.96-1.62)/p,0.103 |
| Male | 262 | 336 | 43.8 | 201 | 397 | 33.6 | 135 | 463 | 22.6 | |||
| Reasons for return visits | ||||||||||||
| Previous problem | 374 | 321 | 53.8 | 2.57(2.06-3.21) p<0.0001 | 205 | 490 | 29.5 | 0.68(0.54-0.85)/p=0.0008 | 115 | 580 | 16.5 | 0.447(0.345-0.58)/p<0.0001 |
| New medical conditions | 206 | 455 | 31.2 | 252 | 409 | 38.1 | 203 | 458 | 30.7 | |||
| Revisit distination | ||||||||||||
| Admission | 165 | 204 | 44.7 | 1.11(0.88-1.42) p=0.76 | 118 | 251 | 32.0 | 0.898(0.7-1.16) p=0.411 | 86 | 283 | 23.3 | 0.99(0.75-1.31) p=0.938 |
| Discharge | 415 | 572 | 42.0 | 339 | 648 | 34.3 | 232 | 755 | 23.5 | |||
| TRST | ||||||||||||
| Cognitive impairment | ||||||||||||
| Yes | 77 | 89 | 46.4 | 1.22(0.88-1.7)/ p=0.234 | 41 | 125 | 24.7 | 0.62(0.43-0.91)/p,0.013 | 48 | 118 | 28.9 | 1.29(0.9-1.86)/p,0.167 |
| No | 423 | 597 | 41.5 | 352 | 668 | 34.5 | 244 | 776 | 23.9 | |||
| Difficult walking/transferring | ||||||||||||
| Yes | 129 | 208 | 38.3 | 0.8(0.62-1.03)/ p=0.088 | 106 | 231 | 31.5 | 0.9(0.69-1.18)/ p,0.44 | 102 | 235 | 30.3 | 1.51(1.13-1.99)/p=0.0046 |
| No | 371 | 478 | 43.7 | 287 | 562 | 33.8 | 190 | 659 | 22.4 | |||
| Falls within one month | ||||||||||||
| Yes | 48 | 80 | 37.5 | 0.81(0.55-1.18)/ p=0.262 | 47 | 81 | 36.7 | 1.19(0.81-1.74)/ p=0.37 | 32 | 96 | 25.0 | 1.02(0.67-1.57)/p=0.911 |
| No | 452 | 607 | 42.7 | 347 | 712 | 32.8 | 260 | 799 | 24.6 | |||
| Polypharmacy | ||||||||||||
| Yes | 252 | 325 | 43.7 | 1.13(0.896-1.42)/ p=0.303 | 176 | 401 | 30.5 | 0.79(0.62-1.01)/ p=0.06 | 149 | 428 | 25.8 | 1.13(0.87-1.48)/ p=0.35 |
| No | 248 | 361 | 40.7 | 217 | 392 | 35.6 | 143 | 466 | 23.5 | |||
| Previous ED visited within 30 days | ||||||||||||
| Yes | 244 | 348 | 41.2 | 0.93(0.74-1.17)/ p=0.511 | 198 | 394 | 33.4 | 1.03(0.81-1.31)/ p=0.821 | 149 | 443 | 25.2 | 1.06(0.81-1.38) p=0.661 |
| No | 256 | 338 | 43.1 | 195 | 399 | 32.8 | 143 | 451 | 24.1 | |||
| Hospitalization within 120 days | ||||||||||||
| Yes | 122 | 167 | 42.2 | 1.005(0.77-1.31) p=0.971 | 105 | 184 | 36.3 | 1.2(0.81-1.31)/ p=0.821 | 61 | 228 | 21.1 | 1.06(0.81-1.38) p=0.661 |
| No | 378 | 520 | 42.1 | 289 | 609 | 32.2 | 231 | 667 | 25.7 | |||
| Without a caregiver | ||||||||||||
| Yes | 346 | 479 | 41.9 | 0.98(0.76-1.25)/ p=0.846 | 272 | 553 | 33.1 | 0.97(0.74-1.26)/ p=0.805 | 206 | 619 | 25.0 | 1.07(0.8-1.43) p=0.655 |
| No | 154 | 208 | 42.5 | 122 | 240 | 33.7 | 86 | 276 | 23.8 | |||
| Care needs as assessed by nurses | ||||||||||||
| Yes | 138 | 153 | 40.4 | 1.33(1.02-1.74)P=0.0354 | 88 | 203 | 30.2 | 0.84(0.63-1.11)p=0.218 | 65 | 226 | 22.3 | 0.85(0.62-1.16)p=0.302 |
| No | 362 | 534 | 40.4 | 306 | 590 | 34.2 | 227 | 669 | 25.3 | |||
| Variable | Revisited within 24 hours | ||||||
| β | SEM | Wald | p | Exp B | 95% CI | ||
| Constant | -.67 | .44 | 2.26 | .13 | .51 | ||
| Age | |||||||
| 65-74 | .27 | .16 | 2.70 | .100 | 1.31 | .95-1.81 | |
| 75-84 | .18 | .16 | 1.26 | .262 | 1.20 | .87-1.66 | |
| >85 | * | ||||||
| Gender | |||||||
| Female | .11 | .12 | .88 | .347 | 1.12 | 0.88-1.42 | |
| Male | * | ||||||
| Health problems | |||||||
| Non-trauma | .08 | .16 | .23 | .632 | 1.08 | 0.79-1.47 | |
| Trauma | * | ||||||
| Triage | |||||||
| Emergency | .10 | .15 | .40 | .528 | 1.10 | 0.82-1.49 | |
| Urgency | * | ||||||
| TRST | |||||||
| Cognitive impairment | -.42 | .22 | 3.64 | .056 | 0.65 | 0.42-1.01 | |
| Difficult walking/transferring | .56 | .18 | 9.79 | .002 | 1.76 | 1.23-2.50 | |
| Falls within recent one month | .15 | .20 | .53 | .466 | 1.16 | 0.78-1.72 | |
| Polypharmacy | -.23 | .13 | 3.04 | .081 | 0.80 | 0.62-1.03 | |
| Previous ED visited within 30 days | .12 | .14 | .84 | .361 | 1.13 | 0.87-1.47 | |
| A hospitalization within 120 days | -.03 | .15 | .03 | .859 | 0.97 | 0.72-1.31 | |
| Without a caregiver | -.03 | .14 | .03 | .860 | 0.98 | 0.74-1.29 | |
| Care needs as assessed by nurses | -.42 | .17 | 6.38 | .012 | 0.66 | 0.48-0.91 | |
| History of chronic diseases | .51 | .26 | 3.77 | .052 | 1.67 | 0.99-2.79 | |
| Revisited in 24-48 hours | |||||||
| Constant | 1.31 | .47 | 7.56 | .006 | 3.69 | ||
| Age | |||||||
| 65-74 | -.10 | .17 | .37 | .545 | .90 | .64-1.26 | |
| 75-84 | -.05 | .17 | .10 | .750 | .95 | .68-1.32 | |
| >85 | * | ||||||
| Gender | |||||||
| Female | .06 | .13 | .21 | .644 | 1.06 | .83-1.36 | |
| Male | * | ||||||
| Health problems | |||||||
| Non-trauma | -.11 | .17 | .45 | .503 | .89 | .64-1.24 | |
| Trauma | * | ||||||
| Triage | |||||||
| Emergency | -.14 | .16 | .68 | .410 | .87 | .63-1.21 | |
| Urgency | * | ||||||
| TRST | |||||||
| Cognitive impairment | .53 | .24 | 4.90 | .027 | 1.70 | 1.06-2.72 | |
| Movement disability | -.11 | .18 | .35 | .555 | .90 | .63-1.28 | |
| Falls within recent one month | -.23 | .20 | 1.32 | .250 | .79 | .53-1.18 | |
| Polypharmacy | .33 | .14 | 5.95 | .015 | 1.40 | 1.07-1.83 | |
| Previous ED visited within 30 days | -.01 | .14 | .00 | .968 | .99 | .75-1.31 | |
| A hospitalization within 120 days | -.30 | .16 | 3.66 | .056 | .74 | .54-1.01 | |
| Without a caregiver | .01 | .15 | .01 | .930 | 1.01 | .76-1.36 | |
| Care needs as assessed by nurses | .05 | .17 | .09 | .765 | 1.05 | .75-1.48 | |
| History of chronic diseases | -.33 | .29 | 1.36 | .243 | .72 | .41-1.25 | |
| Revisited in 48-72 hour | |||||||
| Constant | 1.69 | .52 | 10.62 | .001 | 5.44 | ||
| Age | |||||||
| 65-74 | -.20 | .18 | 1.20 | .273 | .82 | .57-1.17 | |
| 75-84 | -.14 | .18 | .60 | .439 | .87 | .61-1.24 | |
| >85 | * | ||||||
| Gender | |||||||
| Female | -.21 | .14 | 2.27 | .132 | .81 | .62-1.07 | |
| Male | * | ||||||
| Health problems | |||||||
| Non-trauma | .03 | .18 | .02 | .880 | 1.03 | .72-1.47 | |
| Trauma | * | ||||||
| Triage | |||||||
| Emergency | .03 | .17 | .04 | .843 | 1.04 | .74-1.46 | |
| Urgency | * | ||||||
| TRST | |||||||
| Cognitive impairment | -.08 | .24 | .12 | .731 | .92 | .57-1.48 | |
| Difficult walking/transferring | -.57 | .19 | 9.01 | .003 | .57 | .39-.82 | |
| Falls within the recent one month | .14 | .23 | .41 | .521 | 1.16 | .74-1.80 | |
| Polypharmacy | -.12 | .15 | .62 | .432 | .89 | .67-1.19 | |
| Previous ED visited within 30 days | -.14 | .15 | .83 | .364 | .87 | .64-1.18 | |
| A hospitalization within 120 days | .42 | .18 | 5.48 | .019 | 1.52 | 1.07-2.16 | |
| Without a caregiver | .04 | .17 | .06 | .809 | 1.04 | .75-1.44 | |
| Care needs as assessed by nurses | .48 | .20 | 6.04 | .014 | 1.62 | 1.10-2.37 | |
| History of chronic diseases | -.30 | .33 | .85 | .356 | .74 | .39-1.41 | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





