Submitted:
07 May 2023
Posted:
09 May 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. COVID-19 pandemic in Peru
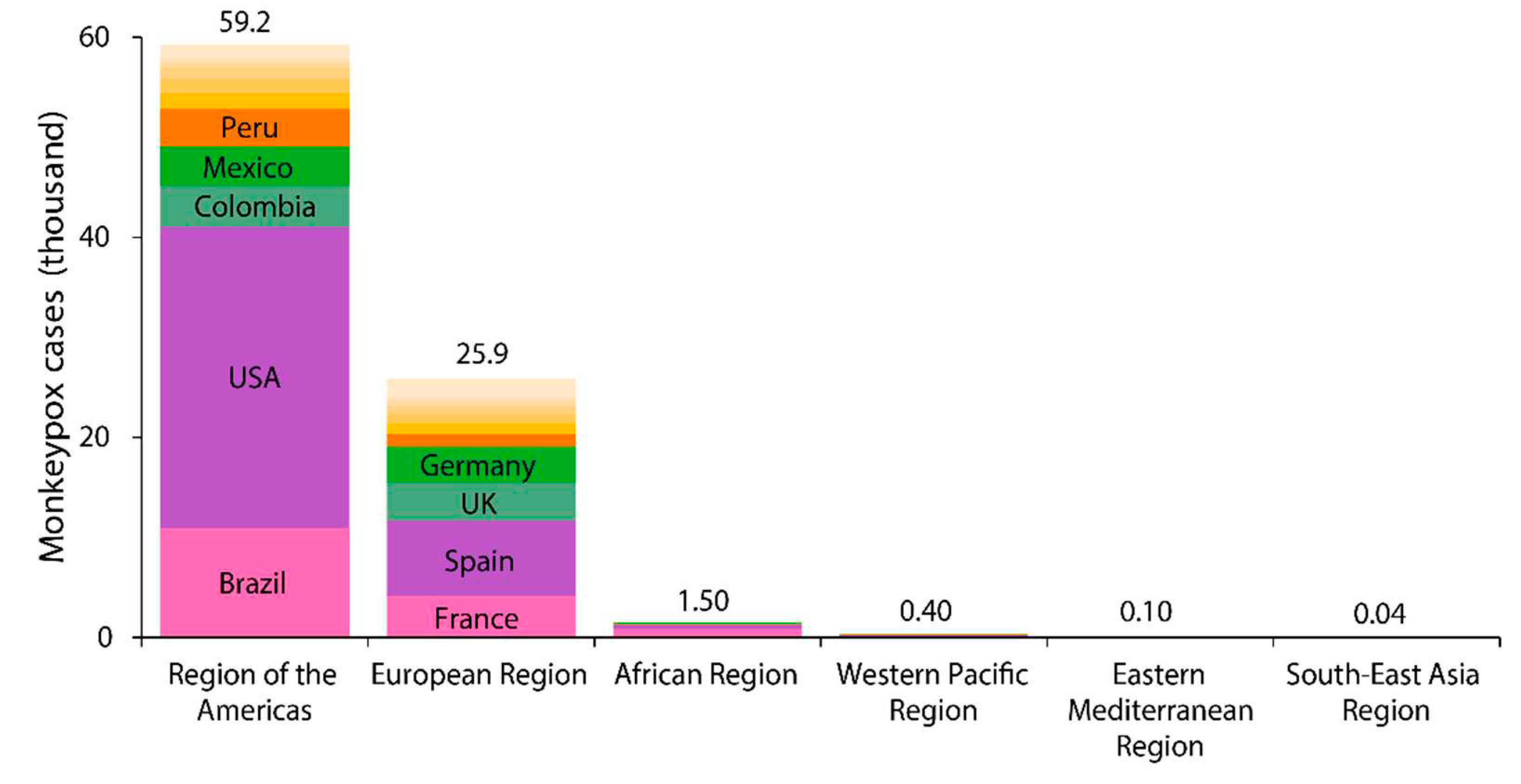
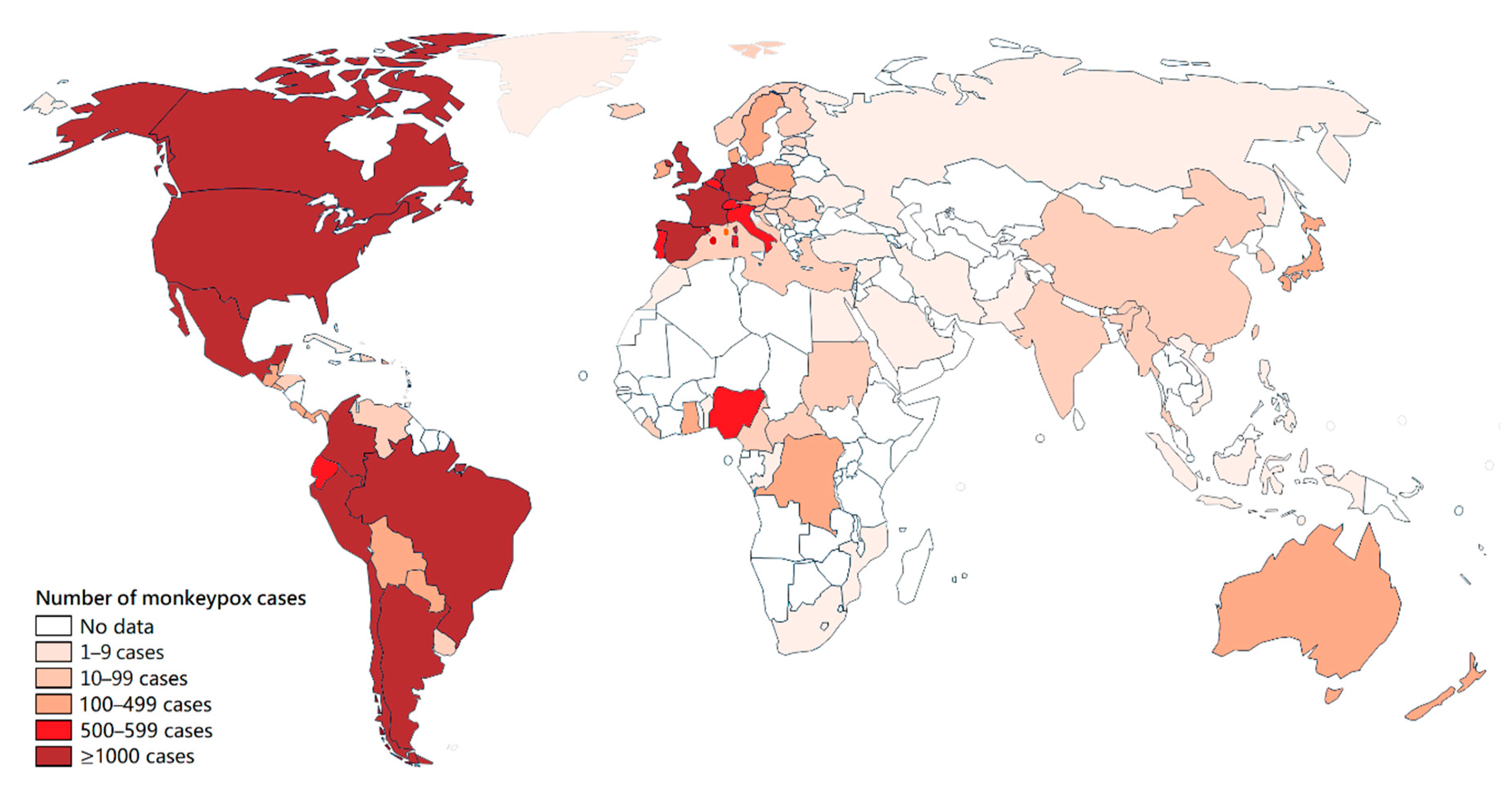
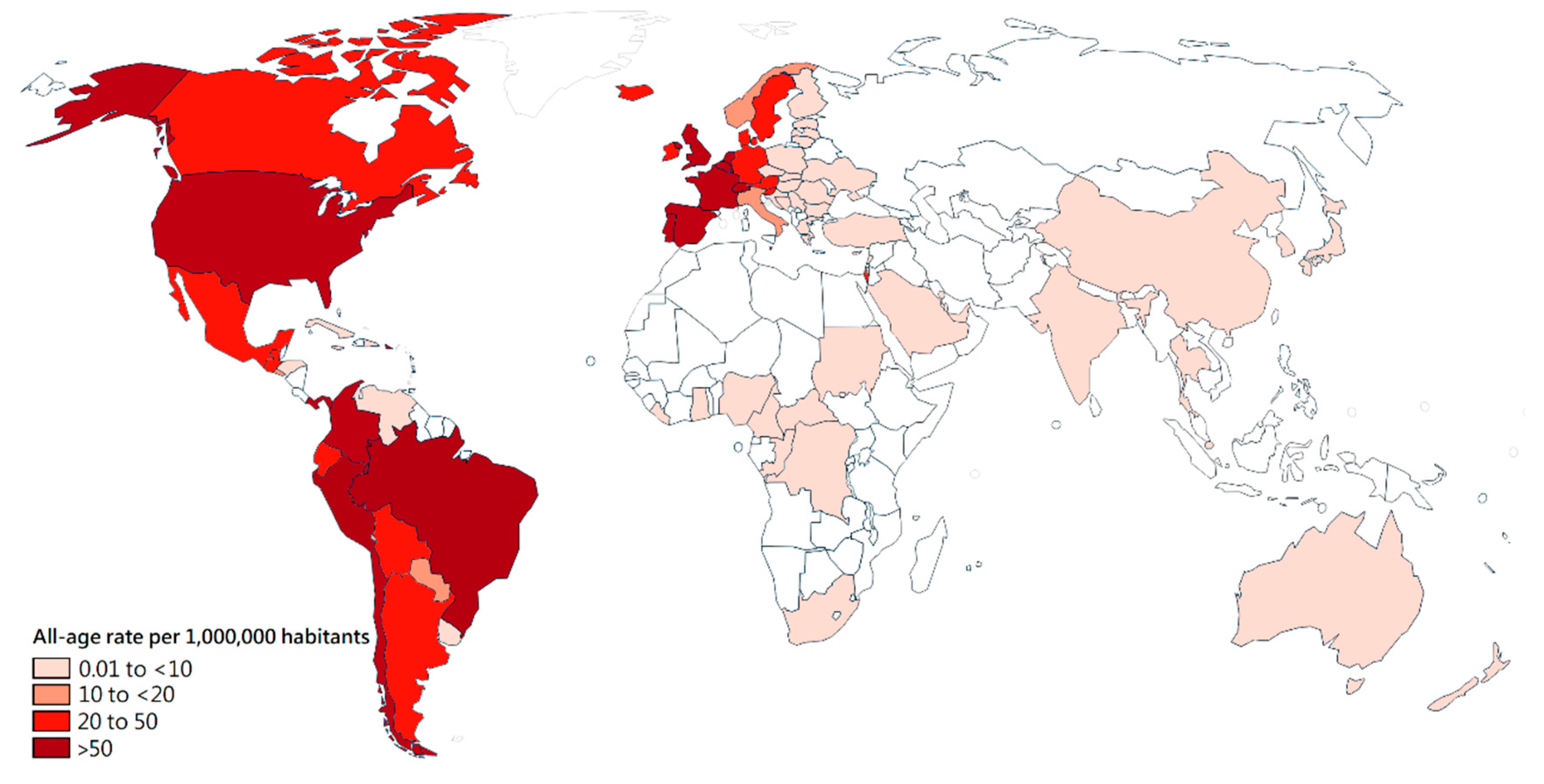
3. Epidemiology
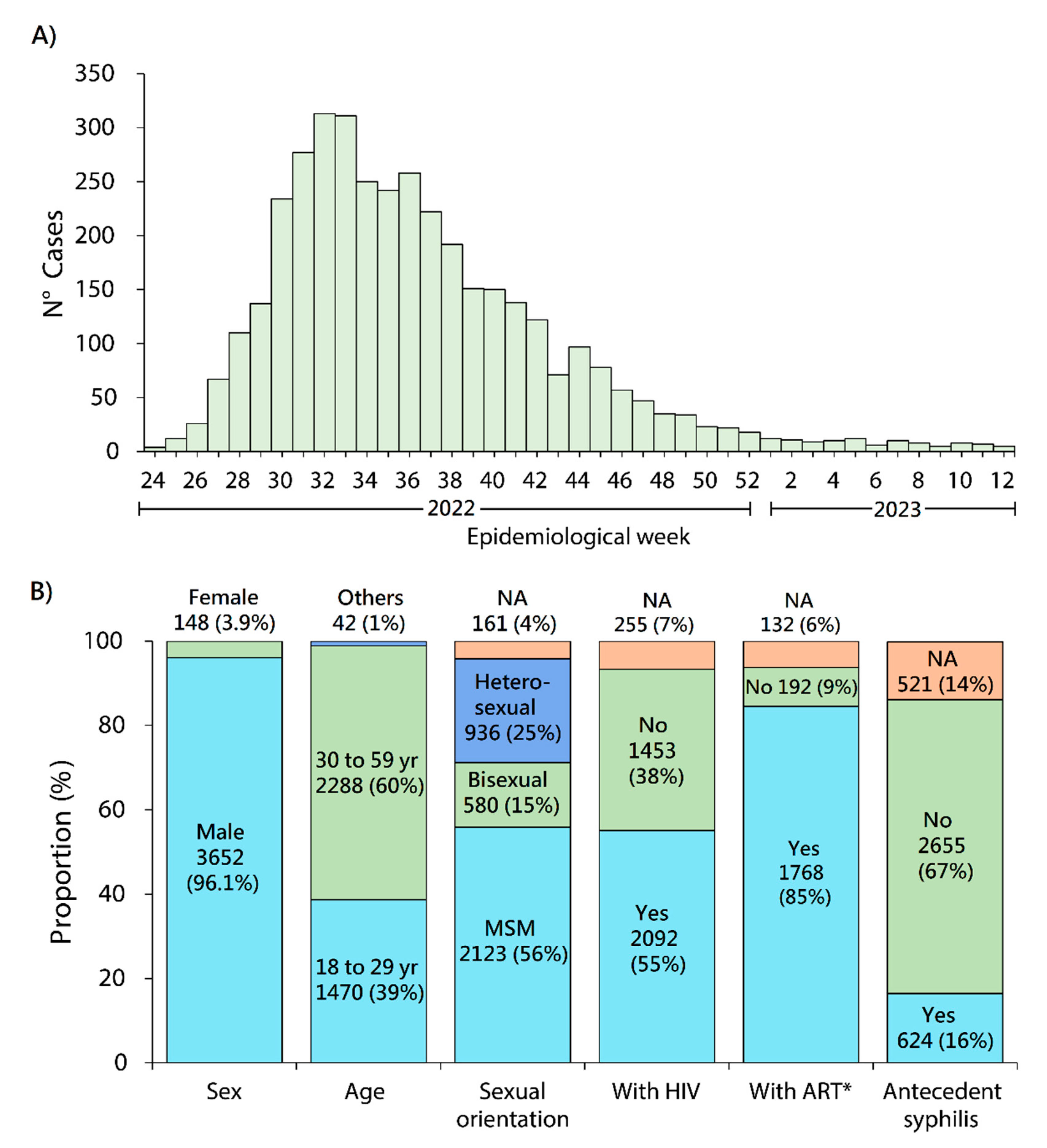
4. Transmission and population at risk
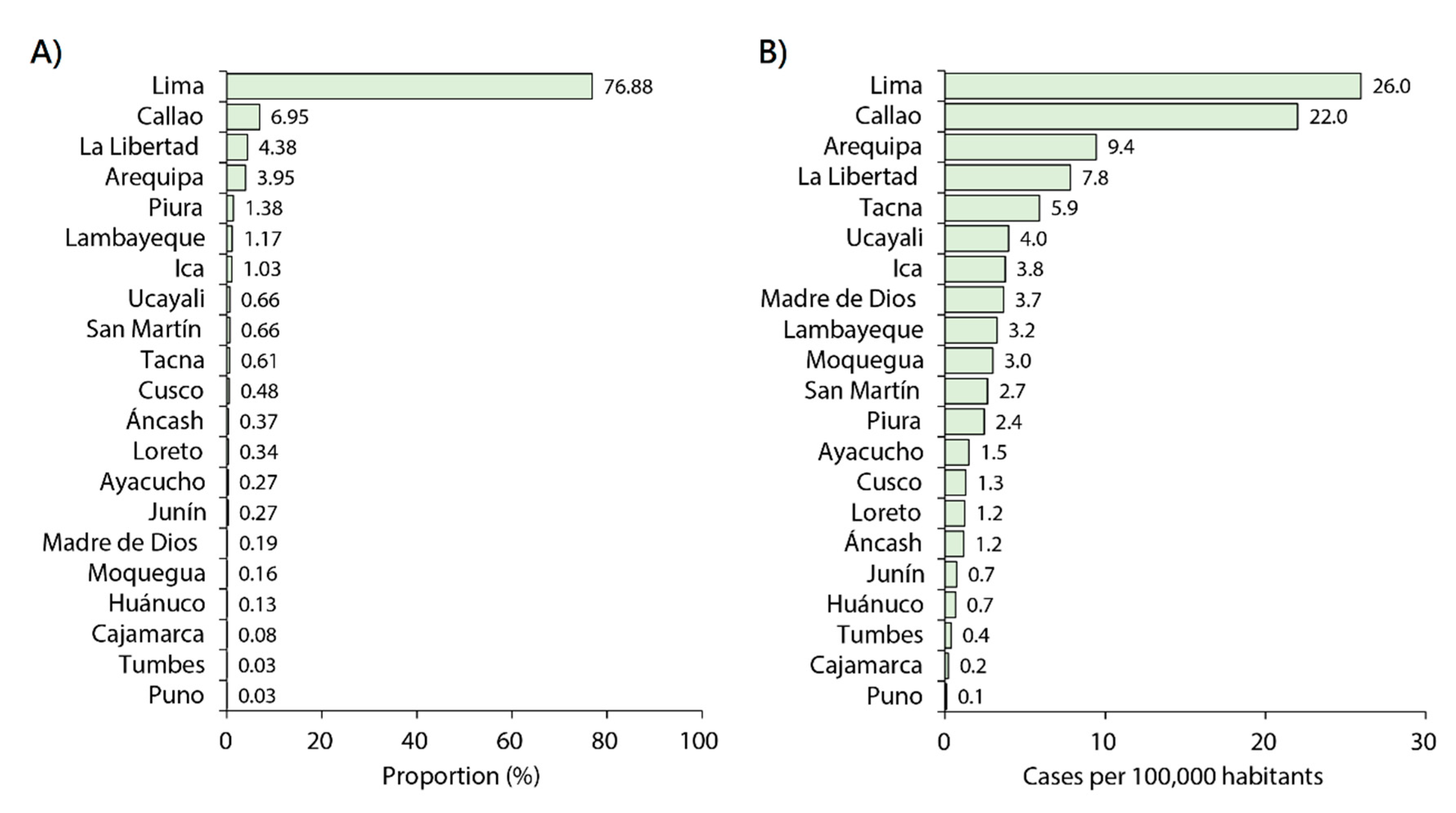
5. MPXV outbreak in Peru
6. MPXV vaccination in Peru
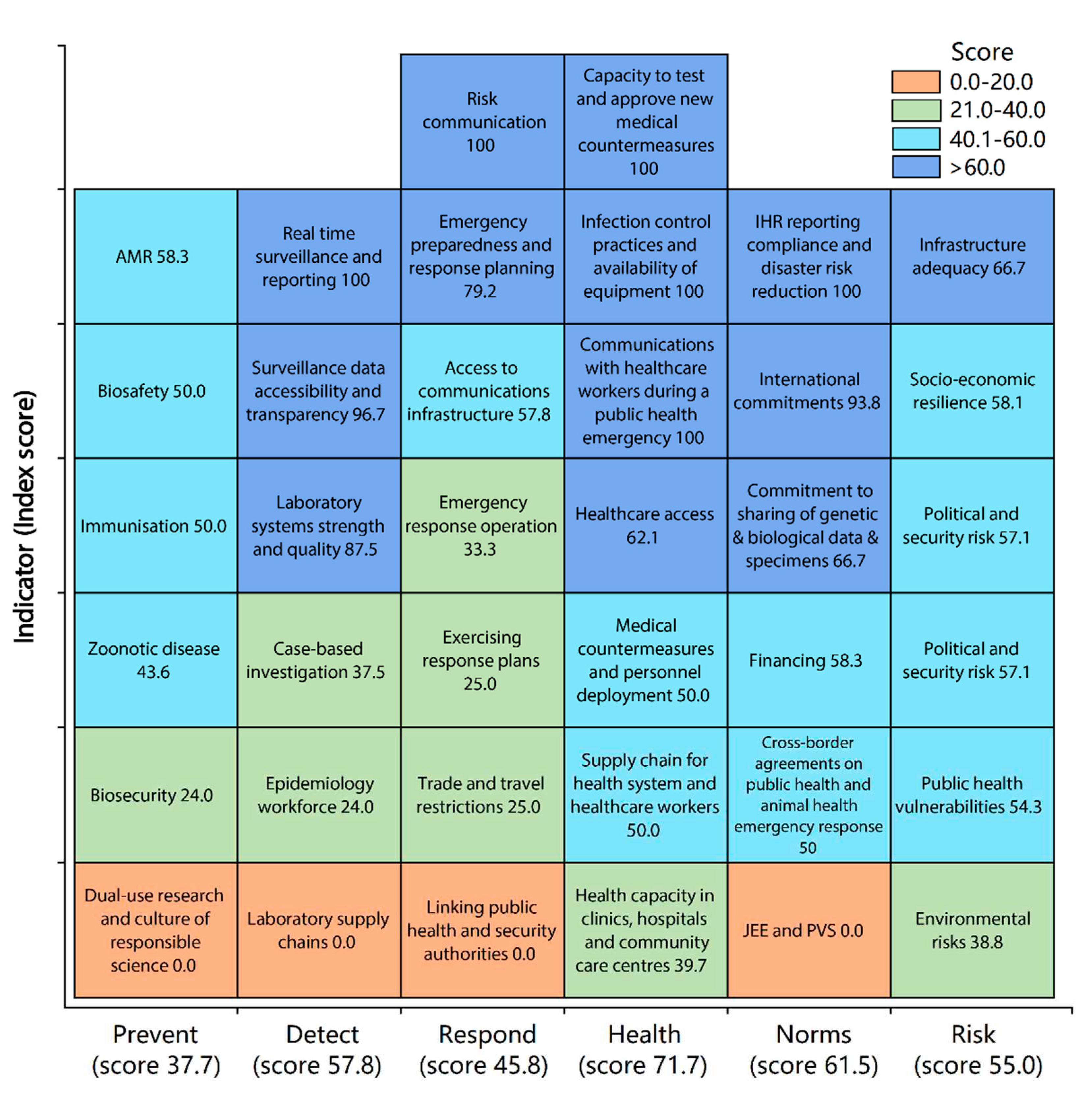
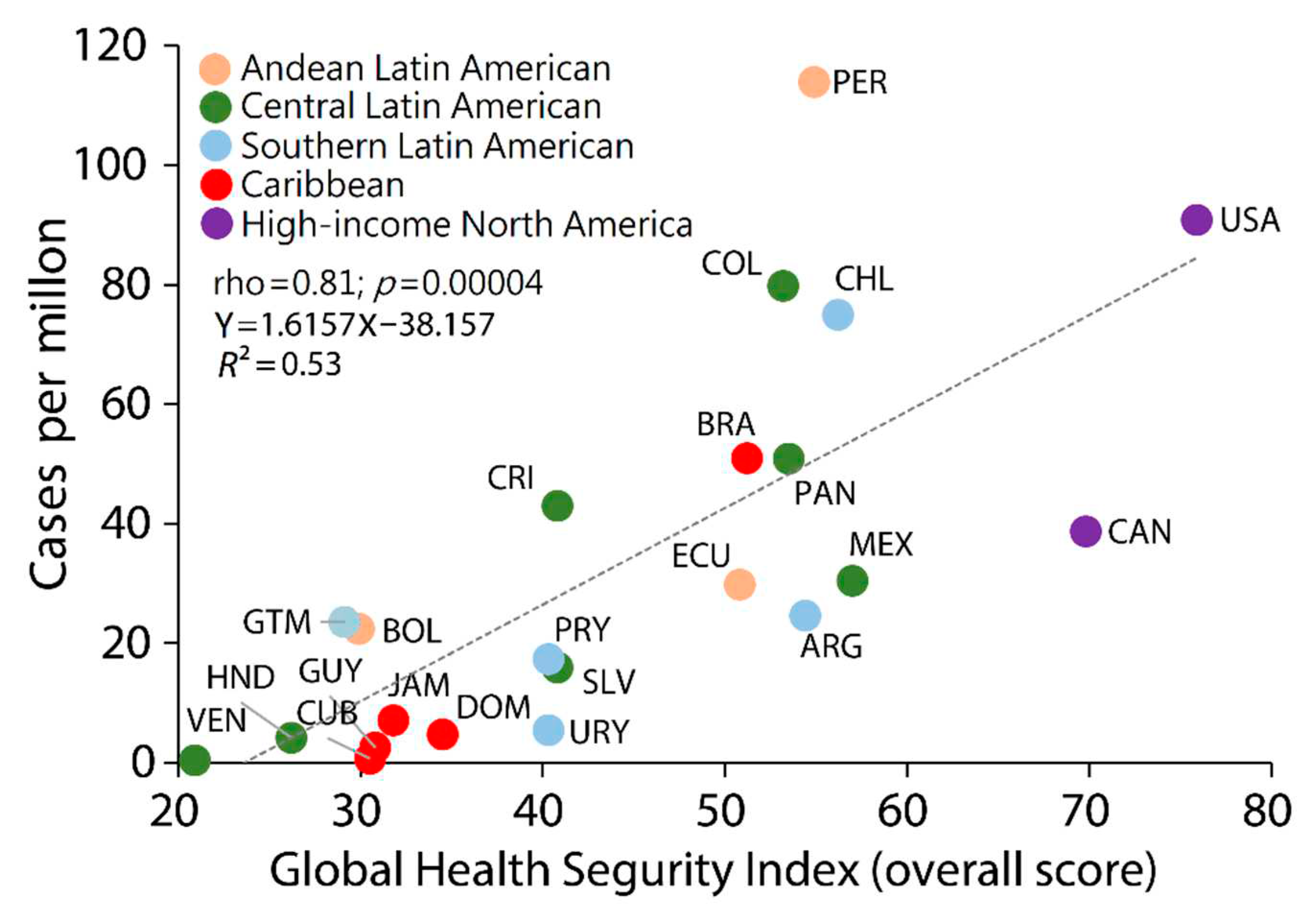
7. Reflections and recommendations
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Conflicts of Interest
References
- McCollum, A.M.; Damon, I.K. Human monkeypox. Clin Infect Dis. 2014 Jan;58(2):260-7. doi: 10.1093/cid/cit703. Epub 2013 Oct 24. Erratum in: Clin Infect Dis. 2014 Jun;58(12):1792. PMID: 24158414. [CrossRef]
- Lum, F.-M.; Torres-Ruesta, A.; Tay, M.Z.; Lin, R.T.P.; Lye, D.C.; Rénia, L.; Ng, L.F.P. Monkeypox: disease epidemiology, host immunity and clinical interventions. Nat. Rev. Immunol. 2022, 22, 597–613. [Google Scholar] [CrossRef] [PubMed]
- Beer, E.M.; Rao, V.B. A systematic review of the epidemiology of human monkeypox outbreaks and implications for outbreak strategy. PLOS Neglected Trop. Dis. 2019, 13, e0007791. [Google Scholar] [CrossRef] [PubMed]
- Ejaz, H.; Junaid, K.; Younas, S.; Abdalla, A.E.; Bukhari, S.N.A.; Abosalif, K.O.; Ahmad, N.; Ahmed, Z.; Hamza, M.A.; Anwar, N. Emergence and dissemination of monkeypox, an intimidating global public health problem. J. Infect. Public Heal. 2022, 15, 1156–1165. [Google Scholar] [CrossRef] [PubMed]
- Velavan, T.P.; Meyer, C.G. Monkeypox 2022 outbreak: An update. Trop. Med. Int. Heal. 2022, 27, 604–605. [Google Scholar] [CrossRef] [PubMed]
- Damaso, CR. The 2022 monkeypox outbreak alert: Who is carrying the burden of emerging infectious disease outbreaks? The Lancet Regional Health – Americas; 2022, 13;100315.
- Thornhill JP, Barkati S, Walmsley S, et al. Monkeypox Virus Infection in Humans across 16 Countries - April-June 2022. N Engl J Med. 2022, 387, 679–691.
- Mitjà, O.; Alemany, A.; Marks, M.; Mora, J.I.L.; Rodríguez-Aldama, J.C.; Silva, M.S.T.; Herrera, E.A.C.; Crabtree-Ramirez, B.; Blanco, J.L.; Girometti, N.; et al. Mpox in people with advanced HIV infection: a global case series. Lancet 2023, 401, 939–949. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. WHO Coronavirus (COVID-19) Dashboard. Peru. WHO: Geneva; 2022. Available in: https://covid19.who.int/region/amro/country/pe.
- COVID-19 Excess Mortality Collaborators. Estimating excess mortality due to the COVID-19 pandemic: a systematic analysis of COVID-19-related mortality, 2020-21. Lancet. 2022, 399, 1513–1536.
- Ramírez-Soto, M.C.; Ortega-Cáceres, G.; Arroyo-Hernández, H. Excess all-cause deaths stratified by sex and age in Peru: a time series analysis during the COVID-19 pandemic. BMJ Open 2022, 12, e057056. [Google Scholar] [CrossRef]
- Herrera-Añazco, P.; Uyen-Cateriano, A.; Mezones-Holguin, E.; Taype-Rondan, A.; Mayta-Tristan, P.; Malaga, G.; Hernandez, A.V. Some lessons that Peru did not learn before the second wave of COVID-19. Int. J. Heal. Plan. Manag. 2021, 36, 995–998. [Google Scholar] [CrossRef]
- Schwalb A, Seas C. The COVID-19 Pandemic in Peru: What Went Wrong? Am J Trop Med Hyg. 2021, 104, 1176–1178.
- Ministry of Health, Peru (MINSA). Situation of COVID-19 Peru. Lima: MINSA; 2022 [2022/08/21]. Available in: https://covid19.minsa.gob.pe/sala_situacional.asp.
- US Centers for Disease Control and Prevention. Human monkeypox—Kasai Oriental, Democratic Republic of Congo, February 1996–October 1997. MMWR Morb Mortal Wkly Rep. 1997, 46, 1168–1171.
- Heymann, D.L.; Szczeniowski, M.; Esteves, K. Re-emergence of monkeypox in Africa: a review of the past six years. Br. Med Bull. 1998, 54, 693–702. [Google Scholar] [CrossRef] [PubMed]
- Jezek, Z.; Szczeniowski, M.; Paluku, K.M.; Mutombo, M. Human Monkeypox: Clinical Features of 282 Patients. J. Infect. Dis. 1987, 156, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Rimoin, A.W.; Mulembakani, P.M.; Johnston, S.C.; Smith, J.O.L.; Kisalu, N.K.; Kinkela, T.L.; Blumberg, S.; Thomassen, H.A.; Pike, B.L.; Fair, J.N.; et al. Major increase in human monkeypox incidence 30 years after smallpox vaccination campaigns cease in the Democratic Republic of Congo. Proc. Natl. Acad. Sci. 2010, 107, 16262–16267. [Google Scholar] [CrossRef] [PubMed]
- et al. Temporal and spatial dynamics of monkeypox in Democratic Republic of Congo, 2000-2015. EcoHealth. 2019, 16, 476–487. [Google Scholar] [CrossRef] [PubMed]
- et al. Outbreak of human monkeypox in Nigeria in 2017-18: a clinical and epidemiological report. Lancet Infect Dis. 2019, 19, 872–879. [Google Scholar] [CrossRef]
- Mitjà O, Ogoina D, Titanji BK, Galvan C, Muyembe JJ, Marks M, et al. Monkeypox. Lancet 2023, 401, 60–74.
- World Health Organization (WHO). WHO Health Emergency Dashboard. Monkeypox. Geneva: WHO; 2022 [2022/09/22]. Available in: https://worldhealthorg.shinyapps.io/mpx_global/.
- Fuller, T.; Thomassen, H.A.; Mulembakani, P.M.; Johnston, S.C.; Lloyd-Smith, J.O.; Kisalu, N.K.; Lutete, T.K.; Blumberg, S.; Fair, J.N.; Wolfe, N.D.; et al. Using Remote Sensing to Map the Risk of Human Monkeypox Virus in the Congo Basin. Ecohealth 2010, 8, 14–25. [Google Scholar] [CrossRef]
- Ogoina, D.; Iroezindu, M.; James, H.I.; Oladokun, R.; Yinka-Ogunleye, A.; Wakama, P.; Otike-Odibi, B.; Usman, L.M.; Obazee, E.; Aruna, O.; et al. Clinical Course and Outcome of Human Monkeypox in Nigeria. Clin. Infect. Dis. 2020, 71, e210–e214. [Google Scholar] [CrossRef]
- Ogoina, D.; Yinka-Ogunleye, A. Sexual history of human monkeypox patients seen at a tertiary hospital in Bayelsa, Nigeria. Int. J. STD AIDS 2022, 33, 928–932. [Google Scholar] [CrossRef] [PubMed]
- Curran KG, Eberly K, Russell OO, Snyder RE, Phillips EK, Tang EC, et al. HIV and Sexually Transmitted Infections Among Persons with Monkeypox - Eight U.S. Jurisdictions, May 17-July 22, 2022. MMWR Morb Mortal Wkly Rep. 2022, 71, 1141–1147.
- Maldonado-Barrueco, A.; Sanz-González, C.; Gutiérrez-Arroyo, A.; Grandioso-Vas, D.; Roces-Álvarez, P.; Sendagorta-Cudos, E.; Falces-Romero, I.; Mingorance, J.; García-Rodríguez, J.; Quiles-Melero, I. Sexually transmitted infections and clinical features in monkeypox (mpox) patients in Madrid, Spain. Travel Med. Infect. Dis. 2023, 52, 102544. [Google Scholar] [CrossRef] [PubMed]
- Rizzo, A.; Pozza, G.; Salari, F.; Giacomelli, A.; Mileto, D.; Cossu, M.V.; Mancon, A.; Gagliardi, G.; Micol, B.; Micheli, V.; et al. Concomitant diagnosis of sexually transmitted infections and human monkeypox in patients attending a sexual health clinic in Milan, Italy. J. Med Virol. 2022, 95, e28328. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann C, Jessen H, Boesecke C. Monkeypox in Germany. Dtsch Arztebl Int. 2022, 119, 551–557.
- Núñez, I.; García-Grimshaw, M.; Ceballos-Liceaga, S.E.; Toledo-Salinas, C.; Carbajal-Sandoval, G.; Sosa-Laso, L.; García-Rodríguez, G.; Cortés-Alcalá, R.; de la Torre, A.; Fragoso-Saavedra, S.; et al. Epidemiological and clinical characteristics of patients with human monkeypox infection in Mexico: a nationwide observational study. Lancet Reg. Heal. - Am. 2022, 17, 100392. [Google Scholar] [CrossRef] [PubMed]
- Pascom ARP, Souza IN, Krummenauer A, Duarte MMS, Sallas J, Rohlfs DB, Pereira GM, Medeiros AC, Miranda AE. Epidemiological and clinical characteristics of monkeypox cases in Brazil in 2022: a cross-sectional study. Epidemiol Serv Saude. 2022, 31, e2022851.
- Sihuincha Maldonado M, Lucchetti AJ, Paredes Pacheco RA, Martínez Cevallos LC, Zumaeta Saavedra EU, Ponce Zapata LR, Lizarbe Huayta FA, Matos Prado ED. Epidemiologic characteristics and clinical features of patients with monkeypox virus infection from a hospital in Peru between July and September 2022. Int J Infect Dis. 2023, 129, 175–180.
- Center for Diseases Control (CDC), Ministry of Health, Peru. Monkeypox situational room. Lima: CDC; 2022 [2022/08/21]. Available in: https://www.dge.gob.pe/sala-monkeypox/#an%C3.
- Thornhill, J.P.; Palich, R.; Ghosn, J.; Walmsley, S.; Moschese, D.; Cortes, C.P.; Galliez, R.M.; Garlin, A.B.; Nozza, S.; Mitja, O.; et al. Human monkeypox virus infection in women and non-binary individuals during the 2022 outbreaks: a global case series. Lancet 2022, 400, 1953–1965. [Google Scholar] [CrossRef]
- Center for Diseases Control (CDC), Ministry of Health, Peru. Epidemiological alert. Code: AE 012 -2022. Lima: CDC-Peru; 2022. Available in: https://www.dge.gob.pe/epipublic/uploads/alertas/alertas_202212_26_143419.pdf.
- Ministry of Health, Peru (MINSA). Technical Document: Monkeypox Preparedness and Response Plan. Lima: MINSA; 2022. Available in: https://www.gob.pe/institucion/minsa/normas-legales/3114429-421-2022-minsa. 3114.
- Nuclear Threat Initiative, Johns Hopkins Center for Health Security, The Economist Intelligence Unit. The Global Health Security Index [Internet]. GHS Index. [Access on August 05, 2022]. Available online: https://www.ghsindex.org/#l-section--map (accessed on 16 April 2020).
- Ji, Y.; Shao, J.; Tao, B.; Song, H.; Li, Z.; Wang, J. Are we ready to deal with a global COVID-19 pandemic? Rethinking countries’ capacity based on the Global Health Security Index. Int. J. Infect. Dis. 2021, 106, 289–294. [Google Scholar] [CrossRef]
- Leichtweis, B.G.; Silva, L.d.F.; da Silva, F.L.; Peternelli, L.A. How the global health security index and environment factor influence the spread of COVID-19: A country level analysis. One Heal. 2021, 12, 100235. [Google Scholar] [CrossRef] [PubMed]
- Kupferschmidt, K. Why monkeypox is mostly hitting men who have sex with men. Science 2022, 376, 1364–1365. [Google Scholar] [CrossRef] [PubMed]
- O’shea, J.; Filardo, T.D.; Morris, S.B.; Weiser, J.; Petersen, B.; Brooks, J.T. Interim Guidance for Prevention and Treatment of Monkeypox in Persons with HIV Infection — United States, August 2022. MMWR. Morb. Mortal. Wkly. Rep. 2022, 71, 1023–1028. [Google Scholar] [CrossRef] [PubMed]
- Hoffmann, C.; Jessen, H.; Wyen, C.; Grunwald, S.; Noe, S.; Teichmann, J.; Krauss, A.; Kolarikal, H.; Scholten, S.; Schuler, C.; et al. Clinical characteristics of monkeypox virus infections among men with and without HIV: A large outbreak cohort in Germany. HIV Med. 2022, 24, 389–397. [Google Scholar] [CrossRef] [PubMed]
- Rizk, J.G.; Lippi, G.; Henry, B.M.; Forthal, D.N.; Rizk, Y. Prevention and Treatment of Monkeypox. Drugs 2022, 82, 957–963. [Google Scholar] [CrossRef]
- Wolrd Health Organization (WHO). Vaccines and immunization for monkeypox. Interim guidance. WHO: Geneva; . Available in: https://www.who.int/publications/i/item/WHO-MPX-Immunization. 16 November.
- The Centers for Disease Control and Prevention (CDC). JYNNEOS Vaccine. Atlanta: CDC; 2022 . Available in: https://www.cdc.gov/poxvirus/monkeypox/interim-considerations/jynneos-vaccine.html. (accessed on 26 December 2021).
- et al. Phase 3 efficacy trial of modified vaccinia Ankara as a vaccine against smallpox. N Engl J Med. 2019, 381, 1897–1908. [Google Scholar] [CrossRef]
- US Food & Drug Administration. Monkeypox update: FDA authorizes emergency use of JYNNEOS vaccine to increase vaccine supply. Aug 9, 2022. Available in: https://www.fda.gov/news-events/press-announcements/monkeypox-update-fda-authorizes-emergency-use-jynneos-vaccine-increase-vaccine-supply. (Date accessed: April 30, 2023).
- Ministry of Health, Peru (MINSA). Press release No. 1132. Lima: MINSA; 2022 [2022/10/11]. Available in: https://www.gob.pe/institucion/minsa/noticias/659167-minsa-anuncia-la-llegada-del-primer-lote-de-vacunas-contra-la-viruela-del-mono-comunicado-de-prensa-n-1132.
- Ministry of Health (MINSA), Peru. Vaccination against monkeypox. MINSA: Lima; 2022. Available in: https://www.gob.pe/31021-vacunacion-contra-la-viruela-del-mono.
- Zumla A, Valdoleiros SR, Haider N, Asogun D, Ntoumi F, Petersen E, Kock R. Monkeypox outbreaks outside endemic regions: scientific and social priorities. Lancet Infect Dis. 2022, 22, 929–931.
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




