1. Introduction
Surgical treatment for obesity began in the 1950s. Sleeve gastrectomy, which was developed in the 2000s, has become popular worldwide with the progress of laparoscopic surgery, and is currently the most performed bariatric surgical procedure [
1]. In this surgery, the weight loss effect and the metabolic improvement effect are remarkably observed. Therefore, this surgery has been re-recognized as a metabolic surgery, and then the number of surgical cases is increasing [
2,
3]. The low invasiveness, weight loss effect, and metabolic improvement effect of this procedure have been highly evaluated, and research on the factors that influence the effect has progressed [
4,
5,
6]. On the other hand, with the spread of this technique, it is important to perform it safely for short-term and long-term results. A management system is in place for this purpose. In the U.S., ACS (American College of Surgeons) and ASMBS (American Society for Metabolic and Bariatric Surgery) have their own education and certification systems to ensure safety [
7,
8]. In Japan, bariatric surgical treatment was started in 1982. The first case was done by open method. After that, the Japanese Society for Treatment of Obesity (JSTO) was established in 2007 in the background of an increase in diabetes and an increase in the trend toward obesity among adult men, and then JSTO started national registry of bariatric surgery cases and multidisciplinary educational program in order to facilitate surgical treatment of obesity in Japan (
Table 1).
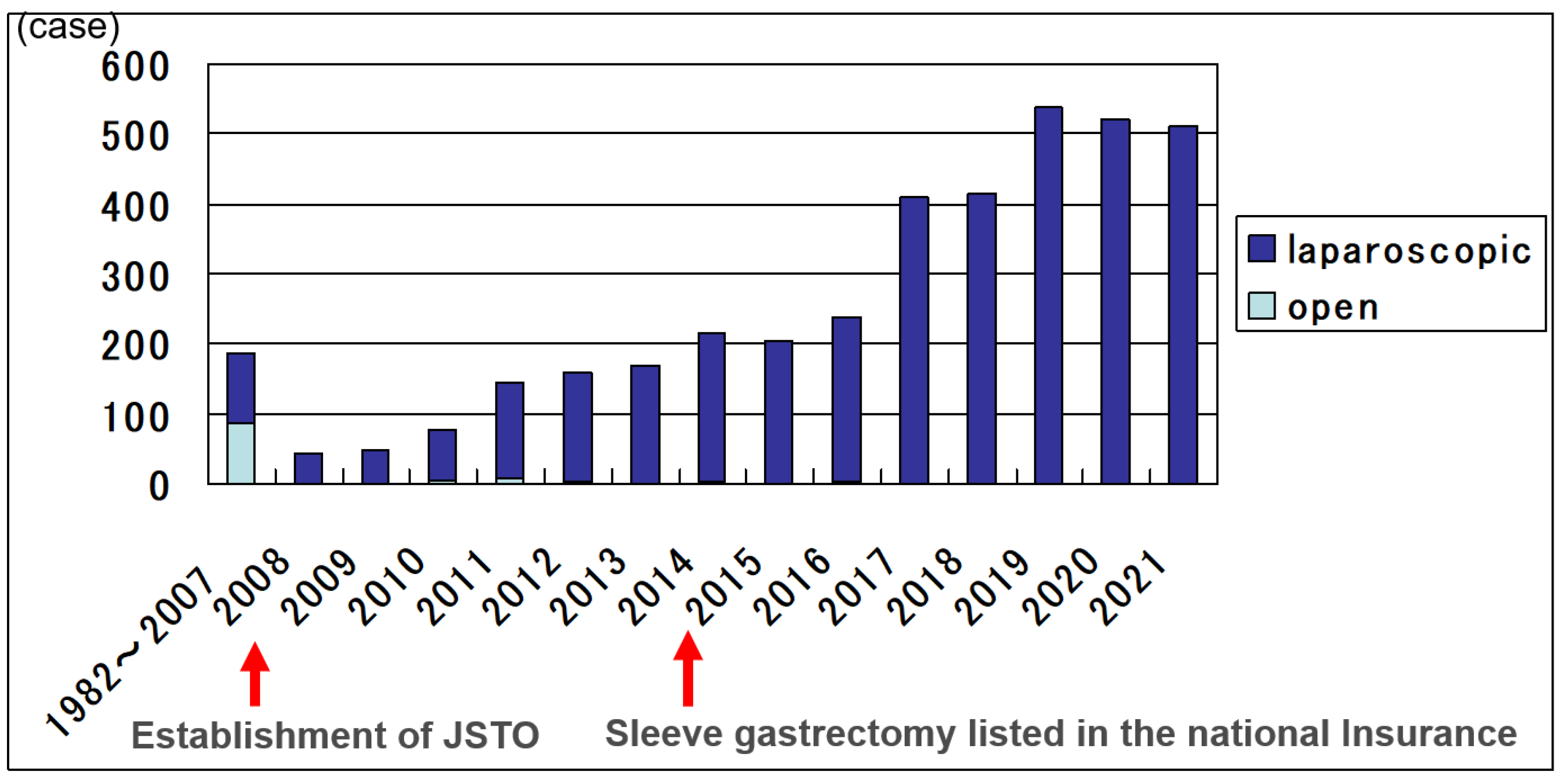
The national registry database by JSTO aims to ensure safety and efficacy in order to facilitate increased utilization of bariatric surgery. The database committee decided input items at the time of its start, and the analyzed results were shared with the board of directors and the society members through annual reports published at each academic society. Before the establishment of JSTO, total cases were 186, and half of them were done by open method. After the establishment of JSTO, the numbers were increasing and reached 4055 in 2021 totally (
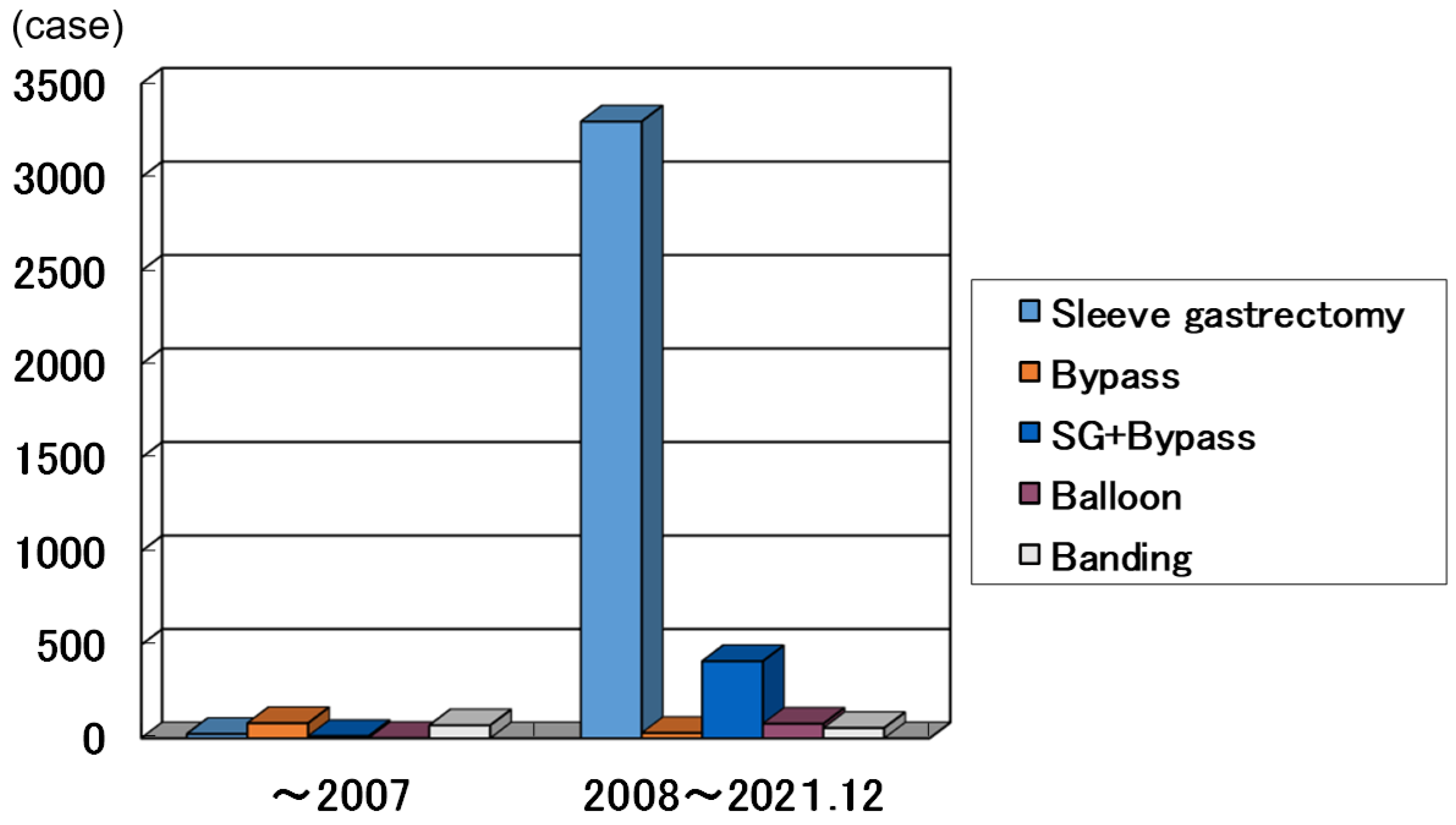
Figure 1). Most operation methods were performed laparoscopically. And recently sleeve gastrectomy was indicated on many cases according to the prevalence of laparoscopic method. In Japan, for obesity surgery, only sleeve gastrectomy was allowed for insurance medical treatment. If the main purpose was to treat diabetes, bypass surgery was often recommended to the patient, but in this case, it would be self-financed. In Japan, before 2008, the half were gastric bypass and the other half were banding method and sleeve gastrectomy. After 2008, sleeve gastrectomy was mostly done in 3240 cases (83.7%), and the next was sleeve bypass method [
9] (
Figure 2). Under such background, in this study, we verified the safety and efficacy of sleeve gastrectomy in Japan based on national registration by JSTO.
After 2008, sleeve gastrectomy was mostly done (
Figure 2) in 3240 cases (83.7%).
2. Subjects and Methods
2.1. JSTO database and subjects
The study was based on the database registered by JSTO. Each member facility of JSTO was issued an ID and password. The database includes gender, age, weight, BMI, comorbidities (including diabetes, hypertension, dyslipidemia, sleep apnea, and other complications), treatment efficacy rate, Includes date, surgical technique, laparoscopy, change to open surgery, reoperation, surgical complications, , postoperative complications , postoperative hospital stay period, postoperative follow-up period, weight loss (kg), diabetes improvement, hypertension improvement, dyslipidemia improvement for each registered patient. For the benefit to avoid complication at registration of each facility, it emphasizes the ease of entering input terms. The registrations were uploaded after surgery at arbitrary timing. Therefore, follow-up period was up to 1 year at most registered institutions. Determination of treatment response was based on weight loss and improvement in comorbidities at enrollment, and specific criteria were entrusted to each site to simplify the process. Physician standards and facility standards were conducted as ethical guidelines in accordance with health insurance medical fees or clinical research. The data were anonymized by each facility. Authors were members of the database committee of JSTO and directly parsed the database. In this study, the aim is to clarify the indication, the safety and the effectiveness of the sleeve gastrectomy using national registry data base compiled by JSTO. The number of the subjects were 3240. The period of the surgery was from 2008 to 2021.
2.2. Methods
Indications of surgery, the safety of the surgery, and the outcome of bariatric and metabolic effects were evaluated. The evaluated factors were preoperative BMI, age, gender proportion and coexisting comorbidities as indications of surgery. BMI and age were estimated by mean±SD. Preoperative comorbidities input was either of the presence or absence, so that they were evaluated by the positive rate(%). As the safety of the surgery, laparoscopic procedure, change to open surgery, reoperation, surgical complications, postoperative complications were estimated by positive rate (%). And postoperative hospital stay period were evaluated by median value. As the outcome of bariatric effects, body weight loss (kg) and the postoperative follow up period were evaluated by mean±SD. As the outcome of metabolic effect, diabetes, hypertension, and dyslipidemia were evaluated. Postoperative improvements were input of presence or absence and they evaluated by the positive rate (%).
3. Results
3.1. Indications of surgery
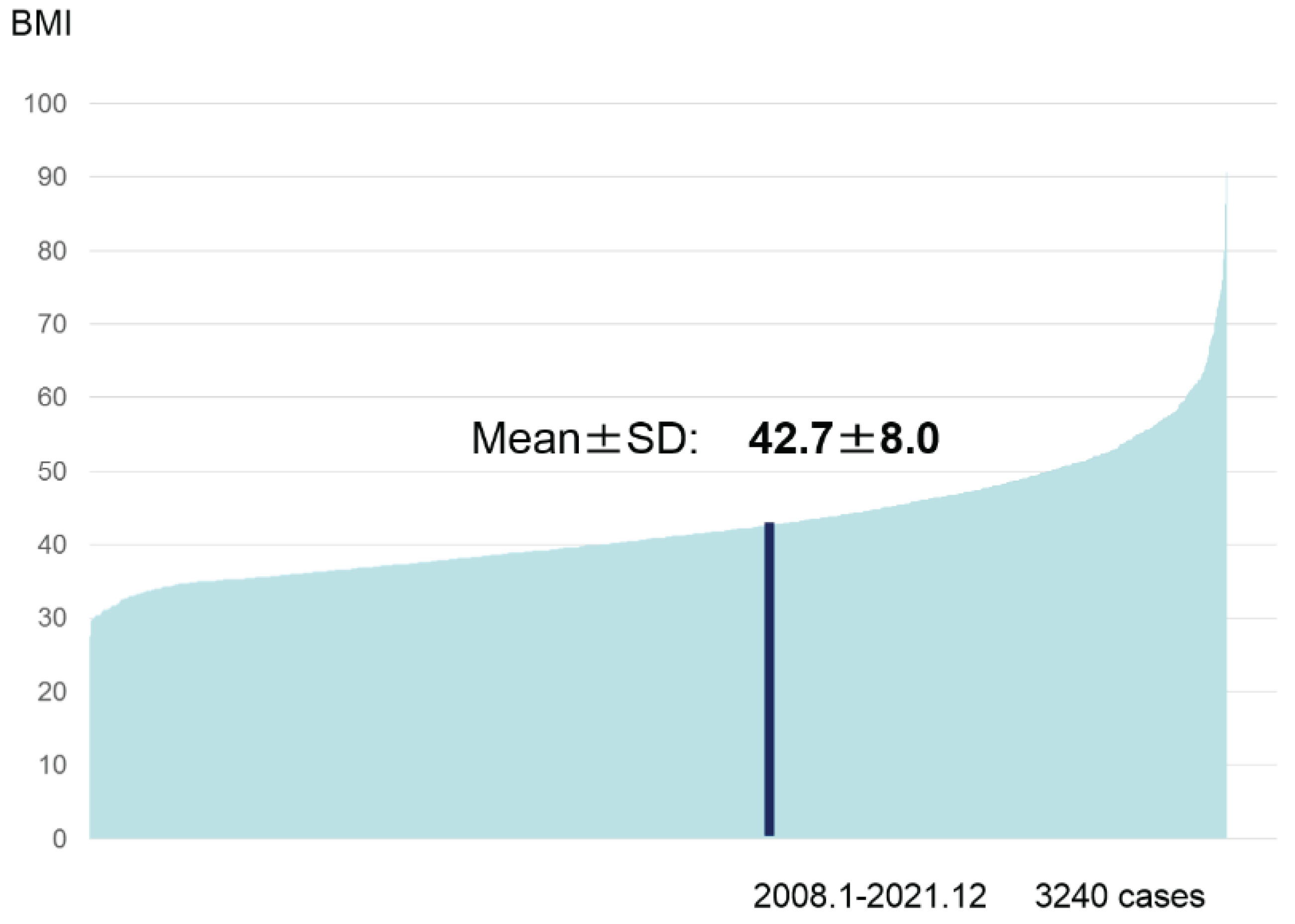
Indications of surgery were determined according to the JSTO statement, IFSO-APC standards, or Japanese insurance medical treatment requirements. The evaluated factors were preoperative BMI, age, gender and the coexisting morbidities. Preoperative BMI was 27.6 to 90.7 kg/m
2(mean±SD 42.7±8.0)(
Figure 3).
The value data ranged from 27.6 to 90.7 kg/m2(mean±SD :42.7±8.0)
As gender, men were 1385(42.7%) and women were 1855(57.3%). Age was 42.2±10.4(mean± SD) (M 42.5±9.5,F 42.5±11.1). As preoperative comorbidities, the combined ratio of DM was 54.4%, hypertension 64.5%, dyslipidemia 65.1%, and sleep apnea syndrome (SAS) 69.8%.
3.2. Evaluation of the safety of the surgery
As operation method, laparoscopic methods were taken in 99.7% of the cases. The intra operative incidents rate was 0.9% which included difficulties (n=4: 0.12%), organ injury(n=11: 0.34%), bleeding(n=6: 0.19%), staple trouble(n=2: 0.06%), hypercapnia(n=2: 0.06%), and others (n=4: 0.12%). Conversion rate to open from laparoscopic methods was 1.1%. As postoperative complications, bleeding(n=57: 1.76%), SSI(n=19: 0.59%), pneumonia(n=18: 0.56%), stenosis(n=17: 0.52%), anastomotic leakage(n=10: 0.31%), mental disorder(n=7: 0.21%), GERD(n=6: 0.19%), infection(n=6: 0.19%), heart disease(n=5: 0.15%), thrombosis(n=5: 0.15%), liver dysfunction(n=4: 0.12%), rhabdomyolysis(n=3: 0.09%), renal failure(n=3: 0.09%), dehydration(n=3: 0.09%) and others(n=20: 0.62%) were registered. Reoperations were performed in 1.5 % of the cases due to bleeding(n=22: 0.68%), anastomotic leakage(n=5: 0.15%), stenosis(n=3: 0.09%), abscess(n=1: 0.03%) and others (n=17: 0.52%). Postoperative complication rate was 5.6% in total and mortality was 0 %. Postoperative hospital stay was 5 days in the median value.
3.3. Evaluation of the outcome of bariatric and metabolic effects
Body weight loss was 27.6±15.5 (mean±SD)kg in the follow up days of 279±245 after surgery.
As the effect on the preoperative metabolic comorbidities, DM improved in 82.9 % of the cases, hypertension 67.9 % and dyslipidemia 66.6% after 279±245 days after surgery.
4. Discussion
The obese population (BMI>30) in Japan is about 3%, which is one of the lowest in the world [
10]. On the other hand, the diabetic population is on the rise in Japan [
11], and the relationship between obesity and diabetes has also been reported [
12]. In particular, Asians are said to be underweight and prone to diabetes compared to Westerners [
13]. In the 2000s, the metabolic improvement effect of bariatric surgery was recognized, and it came to be called ‘metabolic surgery’ [
14]. In particular, it is highly effective in improving diabetes, and its indications have been determined by academic societies worldwide [
15,
16,
17]. A lower BMI indication has been shown for Asians [
18].
In Japan, JSTO was established in 2008 with the aim of safe increasing of surgery while feeling the need to expand bariatric surgical treatment. Under the leadership of the society, we have promoted the guideline making, the surgical case registration, the multi-professional education program, and the facility certification business. As of 2008, there were less than 200 surgical cases, which rapidly increased thereafter, reaching over 4,000 cases in 2021 after being covered by health insurance in 2014. In JSTO, we have reported safety and efficacy of surgical cases at each annual meeting, and both have shown good results and were improving year by year. In the present analysis, the intraoperative incident rate was 0.9% and the postoperative complication rate was 5.6%. The reoperation rate was 1.5% and there were no deaths, and it was considered that the surgical treatments were performed safely. The operative safety were feasible compared to previous reports which showed 6.5-14% postoperative morbidities [
19,
20]. The median postoperative hospital stay was 5 days. In Japan, in order to confirm safety, there were many facilities where patients were discharged from the hospital in 3 to 5 days even if the surgery went smoothly yet. In the future, it is expected to be shorten.
Looking at the improvement in the follow up days of 279±245 after surgery, weight loss effect 27.6±15.5 kg and the improvement of comorbidities was observed in the majority of patients, with diabetes mellitus 82.9 %, hypertension 67.9 %, and dyslipidemia 66.6%. The effect was prominent in diabetes. These efficacy in long-term outcomes has also been reported by multiple institutions [
21,
22,
23]. As described above, the indication and outcome of sleeve gastrectomy has been shown and verified that it is safely administered in Japan, which is located in East Asia and is prone to be suffering diabetes. The laparoscopy rate was 99.7%, and the conversion to open rate was 1.1%. Minimally invasive procedures are thought to contribute to safety. On the other hand, the registry by JSTO were uploaded after surgery at arbitrary timing. Therefore, follow-up period was up to 1 year at most registered institutions. Therefore, there was some range in the registered bariatric and metabolic effects of cases according to the timing of registration. In addition, preoperative comorbidity input was either of the presence or absence, and postoperative improvement was also input of presence or absence. Improvement indicators were based on the criteria of each facility, therefore, there were limitation in detailed analysis in this study. In the registry, the characteristic postoperative complications of sleeve gastrectomy, such as a stump of suture failure, twisting, stenosis, and reflux esophagitis, have also been registered. It is considered necessary to devise ways to avoid these problems and to further consider treatments to be taken at the time of onset. In addition, multi-disciplinary education [
24], facility certification, surgical case registration, and verification of safety effectiveness are considered important, and we would like to continue them in the future. And in this study, there were so limitations that it was considered impossible to construct a specific predictive index. As a future task, we considered the direction of building a follow-up registry system.
5. Conclusions
In conclusion, using JSTO database, we evaluated the indication, postoperative complications and weight loss effect of sleeve gastrectomy in Japan. Regarding the evaluation or prediction of the effect on preoperative comorbidities, future follow-up analysis based on more detailed criteria was considered to be necessary.
Funding
This research received no external funding.
Review Board Statement by Japanese Society of Treatment of Obesity (JSTO)
Statements regarding ethics and consent were obtained from the Ethics Committee of JSTO (IRB #2022-03). All procedures involving human participants were performed in accordance with the ethical standards of the ethical committee of JSTO and the 1964 Helsinki Declaration and its later amendments of comparable ethical standards.
Informed Consent Statement
Informed consent was obtained from all participants included in the study.
Data Availability Statement
Our data used in this study is available on request form the corresponding author.
Acknowledgments
We would like to thank the office of JSTO for several managements.
Conflicts of Interest
The authors declare that there are no conflicts of interest.
References
- Angrisani L, Santonicola A, Iovino P, Formisano G, Buchwald H, Scopinaro N. Bariatric Surgery Worldwide 2013. Obes Surg. 2015, 25, 1822–1832. [Google Scholar] [CrossRef] [PubMed]
- Rubino F, Shukla A, Pomp A, Moreira M, Ahn SM, Dakin G. Bariatric, metabolic, and diabetes surgery: what's in a name? Ann Surg. 2014, 59, 17–22. [Google Scholar]
- Brown WA, Kow L, Shikora S, Liem R, Welbourn R, Dixon J. 6th IFSO global registry report 2021.
- Chambers AP, Kirchner H, Wilson-Perez HE, Willency JA, Hale JE, Gaylinn BD. The effects of vertical sleeve gastrectomy in rodents are ghrelin independent. Gastroenterology 2013, 144, 50–52. [Google Scholar] [CrossRef] [PubMed]
- Myronovych A, Kirby M, Ryan KK, Zhang W, Jha P, Setchell KD, Dexheimer PJ, Aronow B, Seeley RJ, Kohli R. Vertical sleeve gastrectomy reduces hepatic steatosis while increasing serum bile acids in a weight-loss-independent manner. Obesity 2014, 22, 390–400. [Google Scholar] [CrossRef] [PubMed]
- Ruiz-Tovar J, Zubiaga L, Llavero C, Diez M, Arroyo A, Calpena R. Serum cholesterol by morbidly obese patients after laparoscopic sleeve gastrectomy in additional physical activity. Obes Surg 2014, 24, 385–389. [Google Scholar] [CrossRef]
- Nguyen NT, Root J, Zainabadi K, Sabio A, Chalifoux S, Stevens CM, Mavandadi S, Longoria M, Wilson SE. Accelerated growth of bariatric surgery with the introduction of minimally invasive surgery. Arch Surg. 2005, 140, 1198–1202. [Google Scholar] [CrossRef]
- Demaria EJ, Winegar DA, Pate VW, Hutcher NE, Ponce J, Pories WJ. Ann. Early postoperative outcomes of metabolic surgery to treat diabetes from sites participating in the ASMBS bariatric surgery center of excellence program as reported in the Bariatric Outcomes Longitudinal Database. Surg. 2010, 252, 59–66. [Google Scholar]
- Kasama K, Tagaya N, Kanehira E, Oshiro T, Seki Y, Kinouchi M, Umezawa A, Negishi Y, Kurokawa Y. Laparoscopic sleeve gastrectomy with duodenojejunal bypass: technique and preliminary results. Obes Surg. 2009, 9, 1341–1345. [Google Scholar]
- Yoshiike N, Miyoshi M. Epidemiological aspects of overweight and obesity in Japan-international comparisons. Nihon Rinsho. 2013, 71, 207–216. [Google Scholar]
- Goto A, Goto M, Noda M, Tsugane S. Incidence of type 2 diabetes in Japan: a systematic review and meta-analysis. PLoS One. 2013, 6, e74699. [Google Scholar]
- Malone JI, Hansen BC. Does obesity cause type 2 diabetes mellitus (T2DM)? Or is it the opposite? .Pediatr Diabetes. 2019, 20, 5–9. [Google Scholar] [CrossRef] [PubMed]
- Weber MB, Oza-Frank R, Staimez LR, Ali MK, Narayan KM. Type 2 diabetes in Asians: prevalence, risk factors, and effectiveness of behavioral intervention at individual and population levels. Annu Rev Nutr 2012, 32, 417–439. [CrossRef]
- Rubino F, R'bibo SL, del Genio F, Mazumdar M, McGraw TE. Metabolic surgery: the role of the gastrointestinal tract in diabetes mellitus. Nat Rev Endocrionol. 2010, 6, 102–109. [Google Scholar] [CrossRef] [PubMed]
- Rubino F, Kaplan LM, Schauer PR, Cummings DE. The diabetes Surgery Summit consensus conference recommendations for the evaluation and use of gastrointestinal surgery to treat type 2 diabetes mellitus. Ann Surg. 2010, 251, 399–405. [Google Scholar] [CrossRef] [PubMed]
- Dixon JB, Zimmet P, Alberti KG, Rubino F. Bariatric surgery: an IDF statement for obese Type 2 diabetes. Diabet Med. 2011, 28, 628–642. [Google Scholar] [CrossRef]
- American Diabetes Association. Standards of Medical Care in Diabetes 2015. Diabetes Care. 2015, 38, 46–48. [Google Scholar]
- Kasama K, Mui W, Lee WJ, Lakdawala M, Naitoh T, Seki Y, Sasaki A, Wakabayashi G, Sasaki I, Kawamura I, Kow L, Frydenberg H, Chen A, Narwaria M, Chowbey P. IFSO-APC Consensus Statement 2011. Obes Surg. 2012, 22, 677–684. [Google Scholar] [CrossRef]
- Castro V, Saravia B, Loureiro G, Leturio F, García F, Moro D, Barrenetxea A, Díez DV Sleeve gastrectomy as a surgical technique in bariatric surgery: Results of safety and effectiveness. Cir Esp. 2022, 100, 88–94.
- Creange C, Sethi M, Fielding G, Fielding CR 3The safety of laparoscopic sleeve gastrectomy among diabetic patients. Surg Endosc. 2017, 31, 907–911. [CrossRef] [PubMed]
- Seki Y, Kasama K, Hashimoto K. Long-term outcomes of laparoscopic sleeve gastrectomy in morbidly obese Japanese patients. Obes Surg 2016, 26, 138–145. [Google Scholar] [CrossRef] [PubMed]
- Haruta H, Kasama K, Ohta M, Sasaki A, Yamamoto H, Miyazaki Y, Oshiro T, Naitoh T, Hosoya Y, Togawa T, Seki Y, Lefor AK, Tani T. Long-term outcomes of bariatric and metabolic surgery in Japan:Results of multi-institutional survey. Obes Surg 2017, 27, 754–762. [Google Scholar] [CrossRef] [PubMed]
- Saiki A, Yamaguchi T, Tanaka S, Sasaki A, Naitoh T, Seto Y, Matsubara H, Yokote K, Okazumi S, Background characteristics and postoperative outcomes of insufficient weight loss after laparoscopic sleeve gastrectomy in Japanese patients. Ann Gastroenterol Surg 2019, 26, 638–647.
- Montesi L, El Ghoch M, Brodosi L, Calugi S, Marchesini G, Dalle Grave R. Long-term weight loss maintenance for Obesity : a multidisciplinary approach. Diabetes Metab Syndr Obes. 2016, 26, 37–46. [Google Scholar]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).