1. Introduction
Complete knowledge of the clinical pathways (CPs) related to non-union fractures is imperative to guide healthcare practitioners in planning treatment and improving the quality of life of patients. Holistic patient care requires that quality of life should be managed and included in diverse CPs [
1]. The multidisciplinary team of healthcare professionals should follow CPs that provide and manage all possible consequences for these patients to secure the best potential outcomes [
2]. This aligns with the complex treatment and costs associated with managing non-union fractures [
3,
4]; as well as, the recurring follow-up required by patients to achieve positive outcomes.
Non-union of fractures occur in about 2% of all fractures, but the prevalence of these fractures in diaphyseal fractures can be as high as 20% in certain situations [
5]. Long bones are more prone to developing non-union fractures [
5]. Non-union is defined as a permanent failure of the healing process necessitating further treatment [
6]. Non-union fractures may remain non-united for a period of six to nine months without healing or showing any signs of healing following injury [
7]. The healing process of non-union fractures varies depending on anatomical region, pre-existing co-morbidities, and fracture type. In general, lower-energy closed fractures are expected to heal significantly faster than high-energy open long bone fractures due to the presence of soft tissue injuries [
8]. Rather than relying on a certain time limit to describe non-union, it has been advocated that a more practical definition of non-union may be a fracture that will not heal without additional intervention [
9].
A clinical route, or CP, is a multidisciplinary tool that standardises treatment for a specific group of patients based on evidence-based practice [
10]. CPs have been connected to more efficient systems by lowering in-hospital problems and errors, enhancing documentation, and encouraging favorable patient outcomes and safety [
11,
12]. Developing optimal CPs requires collaboration from all healthcare workers [
13,
14]. Developing CPs begins with selecting an appropriate clinical condition that has certain needs in terms of patient and clinical care [
15]. CPs are evidence-based road navigators to enhance overall patient outcomes [
15]. CPs can also be improved and adapted to facilitate the monitoring of acute clinical care. Despite advancements in clinical care, the CPs for patients with non-union fractures of the lower limb remain unknown.
Non-union is a difficult outcome to predict at the time of injury and during the healing process [
16]. Non-union fracture, like any other complication, is seen as an unsatisfactory outcome in clinical practice by doctors and patients [
16]. These unfavorable outcomes may hamper patients' quality of life. Many studies have reported a negative relationship between fracture healing and age, with non-union associated with older age [
17,
4]. Non-union fractures also appear to be more common in patients with diabetes [
18], HIV-related disorders [
19], and present or past smokers [
20,
21].
In South Africa, several patients present with fractures and comorbidities that may impact fracture healing. Patients' perspectives on their quality of life due to lower limb non-unions have yet to be adequately recorded. With the reported prevalence of lower limb non-union fractures [
5]; as well as, the critical importance of lower limb weight-bearing bones that carry the body, it is essential to determine the CPs of lower limb non-union fractures. Poor clinical pathways may lead to poor quality of life. This study aimed to determine CPs and assess the quality of life of patients with lower limb non-union fractures in five Gauteng state hospitals in South Africa.
2. Materials and Methods
2.1. Study Design
A cross-sectional study design was used to collect baseline data while patients were still in the hospital. A prospective study design was used to collect data on their CPs, and we surveyed them to establish their quality of life.
2.2. Sample
Our sample included 22 patients diagnosed with lower limb non-union fractures admitted and treated in the orthopedic departments of five state hospitals in Gauteng, South Africa. Patients were recruited while still in the hospital and followed for a period of six months. Patients diagnosed with non-union lower limb fractures were recruited consecutively to participate in the study, and those who did not reside in the Gauteng province were excluded for follow-up reasons. We also excluded patients with pathological fractures and patients with multiple fractures. The present study was approved by the Ethics Committee at the University of the Witwatersrand (M 150236) and the University of Pretoria (349/2017).
2.3. Methods
We reviewed admission registers, and all the patients with non-union lower limb fractures in the various orthopedic wards of the different hospitals were recruited to participate in the study and requested to complete the Short Form – 36 (SF-36) questionnaire. The questionnaire includes questions in eight domains which fall under the physical component score (PCS) and the mental component score (MCS). The PCS included physical functioning, physical role, body pain, and general health; and the MCS evaluated mental health, vitality, emotional role, and social functioning. In addition to the SF-36 questionnaire, the CPs questionnaire was used to collect data from the period of admission up to discharge. Data were collected from medical records and included a structured intervention of the multidisciplinary team. The information required for CPs included admission date, length of stay in the hospital, medication is given in the hospital, postoperative complications, mobility status at discharge, return to work, return to previous home status, readmissions within six months, health-related quality of life at home, and frequency of follow-up appointments.
2.4. Statistical Analysis
Data were collected and analysed using Stata version 14. Data were presented as frequencies and percentages, and the corresponding 95% confidence interval was also provided for categorical measurements. In addition, the Kruskal-Wallis test, the non-parametric equivalent of the one-way analysis of variance (ANOVA), was used to compare two or more independent samples of equal or different sample sizes. In this study, we used the Kruskal-Wallis test to compare patients with different diagnoses within each domain of the SF-36. The data were analysed to assess the quality of life of patients with lower limb non-union fractures. The Kruskal-Wallis test was performed with the hypothesis that several patients were from the same population.
3. Results
Over a period of six months, we prospectively surveyed patients with lower limb non-union fractures in five state hospitals in Gauteng, South Africa. A total of 22 patients (91% male; mean age 40.68 ± 13.74 years) completed the CPs and SF-36 questionnaire. Results are presented in
Table 1.
Most patients were men, single, and younger than 60 years. Other socio-demographic characteristics of this group were; 68% (n = 15) unemployment, 86 % (n = 19) smokers, and 36% (n = 8) HIV positive. The distribution of non-union fractures in lower limbs, and presentation domains, that is, impairment, activity, and participation of patients, are presented in
Table 2.
Most patients with lower limb non-union fractures had fractures in the distal femur and distal tibia at 22.7% (n = 5) each. A total of 54.6% (n = 12) of the patients were readmitted to the hospital within a period of six months due to complications of non-union fractures. The length of hospital stay was the median of four months (IQR = 3 – 5).
3.1. Quality of Life Measure
Data from the SF-36 were analysed using the non-parametric Kruskal-Wallis Chi-square test to assess significant differences between the eight domains of SF-36 and non-union fracture diagnosis. The Kruskal-Wallis Chi-square test was selected because it is non-parametric, and the study had a small sample size.
Table 3 revealed the results of the lower limb non-union fracture diagnosis on SF-36 domains.
The results of the Kruskal-Wallis test demonstrated that role emotional scores (p-value = 0.03) were significantly affected by the location of lower limb non-union fractures. The physical health of patients was significantly (p-value = 0.0001) affected by the location of non-union lower limb fractures.
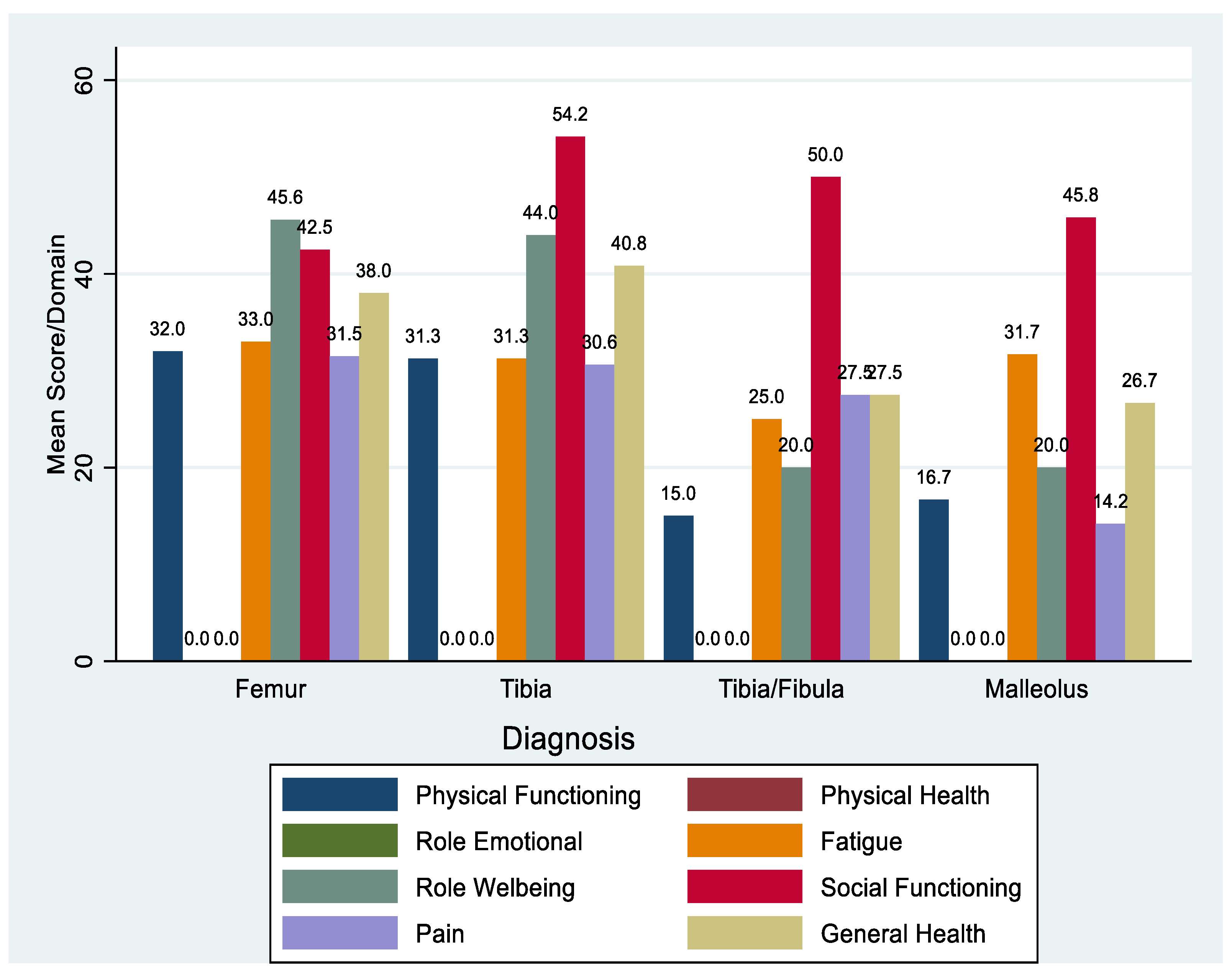
Figure 1 shows that patients diagnosed with the femur, tibia, tibia/fibula and malleolus non-union all score zero for role emotional and physical health. The physical functioning for the femur and tibia non-union reflects mean scores of 32 and 31.3, respectively. These values were reduced to 15 for the tibia/fibula fractures and 16.7 for malleolus non-union fractures. Role well-being shows a similar trend with a higher mean score of 45.6 for femur and 44 for tibia non-union fractures.
Patients with tibia non-union fractures had the highest scores for social functioning (54.2), (
Figure 1); while the pain was least felt in patients with malleolus fractures (14.2). Overall, the MCS domains had the highest scores, and the PCS domains had lower scores, with physical health having the lowest scores.
4. Discussion
In this study, we found that most patients with non-union fractures were younger than 60 years of age. In contrast, previous studies have reported that non-union fracture complications are more prevalent with increasing age due to delayed healing [
16]. Although our results may disqualify the ageing process as a major contributing factor of lower limb non-union fractures, our results suggest that other factors such as smoking (86%), HIV (58%), diabetes (86%) and other social influences may play a role in non-union fracture prevalence.
In our study of CPs, we included patients with lower limb non-union fractures who were admitted to the orthopedic wards of various hospitals. We excluded patients not living in the Gauteng province and those with pathological and multiple fractures. A previous prospective study of femoral neck fractures in the elderly also excluded multiple fractures and fractures caused by malignancy [
22]. Another study in Germany also excluded patients with cancer in their description of CPs for fractures of the pelvic ring [
23]. The inclusion and exclusion criteria in developing CPs are important because patients who are not part of the same follow-up process should be excluded when determining patient outcomes. Additionally, patients with multiple fractures may require different simultaneous treatments, which may mask the effect of particular CPs [
24]. Patients with malignancy-associated fractures may require extended treatment, and they may have limited healing rates caused by poor immunity associated with their condition. Patients with cancer may also need to be followed up more frequently, which would change their CP.
In this study, we investigated CPs by reviewing patients’ records to identify their date of lower limb fracture, anatomical area of non-union, the medication used, and other healthcare practitioners involved. Identifying healthcare providers, their working groups, and staff education was emphasised as the core implementation method [
25]. Other studies have retrospectively compared clinical outcomes before and after CPs were implemented [
26,
27]. The patient’s length of stay in our study was a median of four months (IQR = 3-5) in a follow-up period of six months, which is in contrast with a study done in Hong Kong, which only assessed pre-operative length of stay [
28]. The former study did not indicate the length of stay post-operatively. In our study, we assessed impairment, activity limitation, and participation restriction in activities of daily living. Patients’ final outcomes were also observed if they were healed or had returned to work following lower limb fracture non-union. We could not find any studies that reported the international classification of function (ICF) in non-union fractures CPs. The implementation of CPs may vary in lower limb non-union fractures because of different anatomical fracture sites and ICF scores due to different activities of daily living and socio-demographic characteristics. Lower limb non-unions are linked to escalated morbidity resulting in patient physical, mental, and emotional devastation [
29]. Our results show that physical health and the role of emotional domains of patients were significantly affected by the location of non-union fractures of the lower limbs, though we cannot infer the findings as the sample size was too small. Our findings suggest that patients were still functioning physically, but their non-union fracture suppressed their physical health. This also affected their emotions even though their social functioning was not impeded. Another cross-sectional study in South Africa reasoned that declining physical health might also lead to poor psychological health [
30], which was observed in the participants of our study.
Most of the patients in our study were men (n = 20), which precluded any comparisons between the sexes. The high proportion of male patients suggests that men may be more susceptible to non-union fractures in the South African context. This may be due to high smoking rates or highlighting that men have higher levels of physical activity than women [
31]. In the United Kingdom, more men than women were reported to have non-union fractures (57% vs. 43%) [
32].
We found that most patients (86%) diagnosed with lower limb non-union fractures were smokers. Fracture healing is a complex process where biological, social, and systematic aspects interact and influence healing time and the possibility of non-union [
33]. Smoking slows down healing as nicotine inhibits the replication of the different cells necessary for healing [
34]. In a retrospective study in Australia, non-union was the most common fracture healing complication compared to other fracture healing complications [
4]. This study also found that 42% of non-union patients were either current or former smokers [
4].
In our study, the patients were relatively young (40.68 ± 13.74 years) compared to previous studies [
6]. Non-union fractures may be more problematic for younger adults and affect their quality of life to a greater degree since they cannot return to work. A study of patient risk factors in the United Kingdom reported that fracture complications were more prevalent in even younger patients (18–29 years) [
35]. Young people may be more physically active and more prone to non-union and other fracture complications. Previous studies usually reflect a negative correlation between fracture healing and age and also an increase in the incidence of bone fracture with age [
6]. Another study in California noted that advancing age reduces callus vascularisation during fracture healing, likely decreasing oxygen levels at the fracture and limiting the exchange of other nutrients that are needed for healing [
36].
We found that 86% of the patients who had non-union lower limb fractures had diabetes. Studies have shown a strong link between diabetes and fracture healing complications such as non-union [
35]. Additionally, non-union fractures were diagnosed in 91% of the patients who were male and 58% who were HIV positive in this study. HIV has been linked to bone loss in the past [
37]. Whilst HIV-positive people have the same risk of fractures as HIV-negative people, they seem to experience between 30–70% more incidences of fractures due to low bone mineral density [
38]. Another study noted the higher prevalence of fracture healing complications in HIV-positive male patients between the ages of 19 and 60 years [
39].
5. Conclusions
In the current study, non-union fracture healing impacted the emotional and physical functioning of patients, particularly because it reduces mobility. Lower limb non-union fractures significantly reduced the quality of life of patients due to a slew of emotional issues and impaired physical health. In our study, most patients were smokers, had diabetes and were infected with HIV. South African clinicians should consider these factors when planning the treatment of patients’ fractures and use this information to avoid fracture non-union. Though our sample size was small, there may be a link between smoking, diabetes, HIV-positive and non-union. However, we could not test the assumption as this was not the study aim, and the limited sample size of patients with non-union fractures.
Author Contributions
Conceptualisation, N.M. and H.M.; methodology, N.M. and HM.; formal analysis, G.C.; investigation, N.M.; resources, N.M.; data curation, N.M.; writing—original draft preparation, N.M.; writing—review and editing, H.M. and W.M.; supervision, H.M. and W.M.; project administration, N.M. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the University of the Witwatersrand (M150236) and the University of Pretoria (349/2017) Ethics and Research Committee.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study, and they were informed of the right to withdraw anytime if they were no longer comfortable with the study.
Data Availability Statement
Data for this study is available on request.
Acknowledgments
We acknowledge Dr Glory Chidumwa for his assistance with the statistical analysis and Dr Cheryl Tosh for editing.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kruk, M.E.; Gage, A.D.; Arsenault, C.; Jordan, K.; Leslie, H.H.; Roder-Dewan, S.; Adeyi, O.; Barker, P.; Daelmans, B.; Doubova, S.V. High-quality health systems in the Sustainable Development Goals era: time for a revolution. Lancet Glob 2018, 6, e1196–e1252. [Google Scholar] [CrossRef] [PubMed]
- Taberna, M.; Gil Moncayo, F.; Jané-Salas, E.; Antonio, M.; Arribas, L.; Vilajosana, E.; Peralvez Torres, E.; Mesía, R. The multidisciplinary team (MDT) approach and quality of care. Front Oncol 2020, 10, 85. [Google Scholar] [CrossRef] [PubMed]
- Emara, K.M.; Diab, R.A.; Emara, A.K. Recent biological trends in management of fracture non-union. World J Orthop 2015, 6, 623. [Google Scholar] [CrossRef] [PubMed]
- Ekegren, C.L.; Edwards, E.R.; De Steiger, R.; Gabbe, B.J. Incidence, costs and predictors of non-union, delayed union and mal-union following long bone fracture. IJERPH 2018, 15, 2845. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, J.; Makaram, N.; Simpson, A.; Keating, J. Fracture nonunion in long bones: A literature review of risk factors and surgical management. Injury 2021, 52, S3–S11. [Google Scholar] [CrossRef] [PubMed]
- Giannotti, S.; Bottai, V.; Dell’osso, G.; Pini, E.; De Paola, G.; Bugelli, G.; Guido, G. Current medical treatment strategies concerning fracture healing. Clin Cases Miner Bone Metab 2013, 10, 116. [Google Scholar]
- Stewart, S. Fracture non-union: a review of clinical challenges and future research needs. MOJ 2019, 13, 1. [Google Scholar]
- Kim, P.H.; Leopold, S.S. Gustilo-Anderson classification. Springer. 2012. [Google Scholar] [CrossRef]
- Calori, G.M.; Mazza, E.L.; Mazzola, S.; Colombo, A.; Giardina, F.; Romanò, F.; Colombo, M. Non-unions. Clin Cases Miner Bone Metab 2017, 14, 186. [Google Scholar] [CrossRef]
- WHO. Improving Healthcare Quality in Europe Characteristics, Effectiveness and Implementation of Different Strategies: Characteristics, Effectiveness and Implementation of Different Strategies 2019.
- Martin, G.P.; Kocman, D.; Stephens, T.; Peden, C.J.; Pearse, R.M. Pathways to professionalism? Quality improvement, care pathways, and the interplay of standardisation and clinical autonomy. Sociolog of Health & Illn 2017, 39, 1314–1329. [Google Scholar]
- Rotter, T.; De Jong, R. B.; Lacko, S. E.; Ronellenfitsch, U.; Kinsman, L. Clinical pathways as a quality strategy. In Improving healthcare quality in Europe; Busse, R., Klazinga, N., Panteli, D., Eds.; Copenhagen (Denmark): European Observatory on Health Systems and Policies, 2019; Volume 309, p. 53. [Google Scholar]
- Fernández-Peña, R.; Ortego-Maté, C.; Amo-Setién, F.J.; Silió-García, T.; Casasempere-Satorres, A.; Sarabia-Cobo, C. Implementing a Care Pathway for Complex Chronic Patients from a Nursing Perspective: A Qualitative Study. IJERPH 2021, 18, 6324. [Google Scholar] [CrossRef] [PubMed]
- Wind, A.; Van Der Linden, C.; Hartman, E.; Siesling, S.; Van Harten, W. Patient involvement in clinical pathway development, implementation and evaluation–A scoping review of international literature. Patient Educ Couns 2022, 105, 1441–1448. [Google Scholar] [CrossRef] [PubMed]
- Hipp, R.; Abel, E.; Weber, R.J. A primer on clinical pathways. Pharmacy 2016, 51, 416–421. [Google Scholar] [CrossRef] [PubMed]
- Nandra, R.; Grover, L.; Porter, K. Fracture non-union epidemiology and treatment. Trauma 2016, 18, 3–11. [Google Scholar] [CrossRef]
- Clark, D.; Nakamura, M.; Miclau, T.; Marcucio, R. Effects of ageing on fracture healing. Curr. Osteoporos. Rep. 2017, 15, 601–608. [Google Scholar] [CrossRef] [PubMed]
- Jiao, H.; Xiao, E.; Graves, D.T. Diabetes and its effect on bone and fracture healing. Curr. Osteoporos. Rep. 2015, 13, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Graham, S.M.; Maqungo, S.; Laubscher, M.; Ferreira, N.; Held, M.; Harrison, W.J.; Simpson, A.H.; Macpherson, P.; Lalloo, D.G. Fracture healing in patients with HIV in South Africa: a prospective cohort study. JAIDS 2021, 87, 1214. [Google Scholar] [CrossRef] [PubMed]
- Pearson, R.G.; Clement, R.; Edwards, K.; Scammell, B.E. Do smokers have greater risk of delayed and non-union after fracture, osteotomy and arthrodesis? A systematic review with meta-analysis. BMJ Open 2016, 6, e010303. [Google Scholar] [CrossRef]
- Smolle, M.A.; Leitner, L.; Böhler, N.; Seibert, F.J.; Glehr, M.; Leithner, A. Fracture, nonunion and postoperative infection risk in the smoking orthopaedic patient: a systematic review and meta-analysis. EFORT Open Reviews 2021, 6, 1006–1019. [Google Scholar] [CrossRef]
- Roberts, H.C.; Pickering, R.M.; Onslow, E.; Clancy, M.; Powell, J.; Roberts, A.; Hughes, K.; Coulson, D.; Bray, J. The effectiveness of implementing a care pathway for femoral neck fracture in older people: a prospective controlled before and after study. Age and Ageing 2004, 33, 178–184. [Google Scholar] [CrossRef]
- Rommens, P.M.; Ossendorf, C.; Pairon, P.; Dietz, S.O.; Wagner, D.; Hofmann, A. Clinical pathways for fragility fractures of the pelvic ring: personal experience and literature review. J Orthop Sci 2015, 20, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Neugebauer, E.A.; Waydhas, C.; Lendemans, S.; Rixen, D.; Eikermann, M.; Pohlemann, T. The treatment of patients with severe and multiple traumatic injuries. Dtsch Arztebl Int. 2012, 109, 102. [Google Scholar] [CrossRef] [PubMed]
- Bjurling-Sjöberg, P.; Wadensten, B.; Pöder, U.; Jansson, I.; Nordgren, L. Struggling for a feasible tool–the process of implementing a clinical pathway in intensive care: a grounded theory study. BioMed Central 2018, 18, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Collinge, C.A.; Mcwilliam-Ross, K.; Beltran, M.J.; Weaver, T. Measures of clinical outcome before, during, and after implementation of a comprehensive geriatric hip fracture program: is there a learning curve? J Orthop Trauma 2013, 27, 672–676. [Google Scholar] [CrossRef] [PubMed]
- Lion, K.C.; Wright, D.R.; Spencer, S.; Zhou, C.; Del Beccaro, M.; Mangione-Smith, R. Standardized clinical pathways for hospitalized children and outcomes. Pediatrics 2016, 137. [Google Scholar] [CrossRef] [PubMed]
- Lau, T.W.; Fang, C.; Leung, F. The effectiveness of a geriatric hip fracture clinical pathway in reducing hospital and rehabilitation length of stay and improving short-term mortality rates. Geriatr Orthop Surg Rehabil 2013, 4, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Ferreira, N.; Marais, L.; Aldous, C. Challenges and controversies in defining and classifying tibial non-unions. SA Orthop J 2014, 13, 52–56. [Google Scholar]
- Singaram, S.; Naidoo, M. The psychological impact of long bone fractures in KwaZulu-Natal, South Africa: A cross-sectional study. JPHiA 2020, 11. [Google Scholar] [CrossRef]
- DeRuiter, W.K.; Faulkner, G.; Cairney, J.; Veldhuizen, S. Characteristics of physically active smokers and implications for harm reduction. Am J Public Health 2008, 98, 925–931. [Google Scholar] [CrossRef]
- Mills, L.A.; Aitken, S.A.; Simpson, A.H.R. The risk of non-union per fracture: current myths and revised figures from a population of over 4 million adults. Acta Orthop 2017, 88, 434–439. [Google Scholar] [CrossRef]
- Nawfal, A.; Sewell, M.D.; Bhavikatt, M.; Gikas, P.D. The effect of smoking on fracture healing and various orthopaedic procedures. Acta Orthop Belg 2012, 78, 285–290. [Google Scholar]
- Zhang, W.; Lin, H.; Zou, M.; Yuan, Q.; Huang, Z.; Pan, X.; Zhang, W. Nicotine in inflammatory diseases: anti-inflammatory and pro-inflammatory effects. Front Immunol 2022, 376. [Google Scholar] [CrossRef] [PubMed]
- Hernandez, R.K.; Do, T.P.; Critchlow, C.W.; Dent, R.E.; Jick, S.S. Patient-related risk factors for fracture-healing complications in the United Kingdom General Practice Research Database. Acta Orthop 2012, 83, 653–660. [Google Scholar] [CrossRef] [PubMed]
- Lu, C.; Hansen, E.; Sapozhnikova, A.; Hu, D.; Miclau, T.; Marcucio, R.S. Effect of age on vascularization during fracture repair. J. Orthop Res 2008, 26, 1384–1389. [Google Scholar] [CrossRef] [PubMed]
- Hileman, C.O.; Eckard, A.R.; Mccomsey, G.A. Bone loss in HIV: a contemporary review. Curr Opin Endocrinol Diabetes Obes. 2015, 22, 446–451. [Google Scholar] [CrossRef]
- Mccomsey, G.A.; Tebas, P.; Shane, E.; Yin, M.T.; Overton, E.T.; Huang, J.S.; Aldrovandi, G.M.; Cardoso, S.W.; Santana, J.L.; Brown, T.T. Bone disease in HIV infection: a practical review and recommendations for HIV care providers. Clin. Infect. Dis. 2010, 51, 937–946. [Google Scholar] [CrossRef]
- Mcmillan, J.M.; Krentz, H.; Gill, M.J.; Hogan, D.B. Managing HIV infection in patients older than 50 years. CMAJ 2018, 190, E1253–E1258. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).