1. Introduction
The first case of COVID-19 in Spain was confirmed in a male German tourist on the island of La Gomera on January 31 2020, one day after the World Health Organization (WHO) declaration of COVID-19 as a Public Health Emergency of International Concern. The first cases of autochthonous SARS-CoV-2 transmission were confirmed on February 26, at the start of a pandemic that became the worst health crisis in our country and globally since the influenza pandemic of 1918 [
1]. By the end of March 2022, more than 470 million cases were confirmed worldwide, according to official data, with around 40% being detected in Europe, while around 11.5 million cases were recorded in Spain [
2].
Healthcare workers were at the forefront of the crisis from the beginning, being the professional category most exposed to SARS-CoV-2 and having the highest probability of infection in comparison to the general population [3-5]. The WHO estimated that between 80,000 and 180,000 healthcare workers worldwide may have died from COVID-19 between January 2020 and May 2021 [
6]. Other studies report a mortality rate from COVID-19 of around 1.5% among healthcare workers [
7]. In Spain, healthcare centers were considered high-risk settings in the document Coordinated response actions to control the transmission of COVID-19 [
8] approved by the Inter-territorial Council of the National Healthcare System, which established alert levels and recommended actions as a function of risk level. Various factors were involved, including working exclusively in-person in medical care activities, long shifts due to personnel shortages, lack of information on the disease caused by a new virus, close and prolonged contact with infected patients, aerosol-generating healthcare procedures, insufficient or inappropriate use of personal protective equipment at the beginning of the pandemic, closed and crowded spaces, and scarce or deficient ventilation [9-11].
Up to May 11 2020, the National Epidemiological Surveillance Network (Red Nacional de Vigilancia Epidemiológica, RENAVE) had reported 40,961 cases of COVID-19 in healthcare personnel, representing 24.1% of the total number of cases during the first wave of the pandemic and 52 deaths were recorded (0.1% of the 40,961 cases). Up to the last week of March 2022, 2.8% of cases with information available on occupation were healthcare or social-healthcare personnel, and this percentage was significantly higher among females than males (4.2 vs. 1.3%) [
12].
According to the Spanish business directory (DIRCE, INE), the national code of economic activities (NACE) Q-86 (heading Human Health activities) was assigned to 55,943 companies in 2019. According to the National Active Population Survey (Encuesta de Población Activa - EPA) these companies employed 1,138,136 people in January 2020 and 72% were women. Only 0.7% of these healthcare companies were hospital centers, but these employed 60% of the workers.
The objective of this study was to describe the impact of the pandemic on healthcare workers (NACE Q86) in terms of temporary disability (TD) associated with COVID-19 between February 15 2020 and May 1 2021 as a function of type of healthcare activity, occupation, sex, and age, identifying the most affected occupational groups and supporting the design of preventive measures.
2. Materials and Methods
The study included episodes of TD in Human Health activities (economic activity Q86) for infection with COVID-19 disease (ICD-10 codes: B34.2, B97.21, and U07.1) or for quarantine due to close contact with patients with COVID-19 (ICD-10 code: Z20.828):
Q86. HUMAN HEALTH ACTIVITIES
861. Hospital activities.
862. Medical and dental practice activities.
8621. General medical practice activities.
8622. Specialist medical practice activities.
8623. Dental practice activities.
869. Other human health activities.
We performed an analysis by economic activity division (2-digit NACE) using sectorial and territorial data on TD due to COVID-19 over the study period, available from the Spanish Ministry of Inclusion, Social Security, and Migrations [
13]. A more detailed analysis by activity group (3-digit NACE) was based on data from the National Institute of Social Security for the period between February 15 and September 17, 2020, including information on occupation, age, sex, and autonomous community.
The number of TDs for confirmed infection and quarantine was analyzed by economic activity, considering the daily reports in the previous 7 days. The ratio between TDs for quarantine and infection (TD quarantine/infection ratio) was calculated for the previous 7 days. The calculation of rates by economic activity was based on the monthly Social Security affiliation figures disaggregated to 2-digit NACE [
14]. Analysis by 3-digit NACE was performed with data provided by the EPA, available on the webpage of the National Statistics Institute (Instituto Nacional de Estadística, INE) [
15]. Rates by occupation were based on the 3-digit numbers for employed persons in the National Occupations Classification (Clasificación Nacional de Ocupaciones, CNO), available from the EPA.
The following TD rates were obtained for COVID-19:
TD rate by economic activity (accumulated over the whole study period and over 14 days): number of TDs in a given NACE code per 100,000 active workers affiliated to the Social Security with the same NACE code.
TD rate by occupation (accumulated over the whole study period and over 14 days): number of TDs in worker with a given CNO code per 100,000 occupied workers in that CNO code.
We also calculated the cumulative incidence over 14 days (14-day rate) of COVID-19 cases in 16- to 65-year-olds notified to the National Epidemiological Surveillance Network (Red Nacional de Vigilancia Epidemiológica, RENAVE) from February 15 2020 to May 1 2021. The TDs evolution was described in the context of the COVID-19 cases obtained from epidemiological surveillance data provided by the Carlos III Health Institute, using the population aged between 16 and 65 years (available on the INE webpage) as denominator [
16].
3. Results
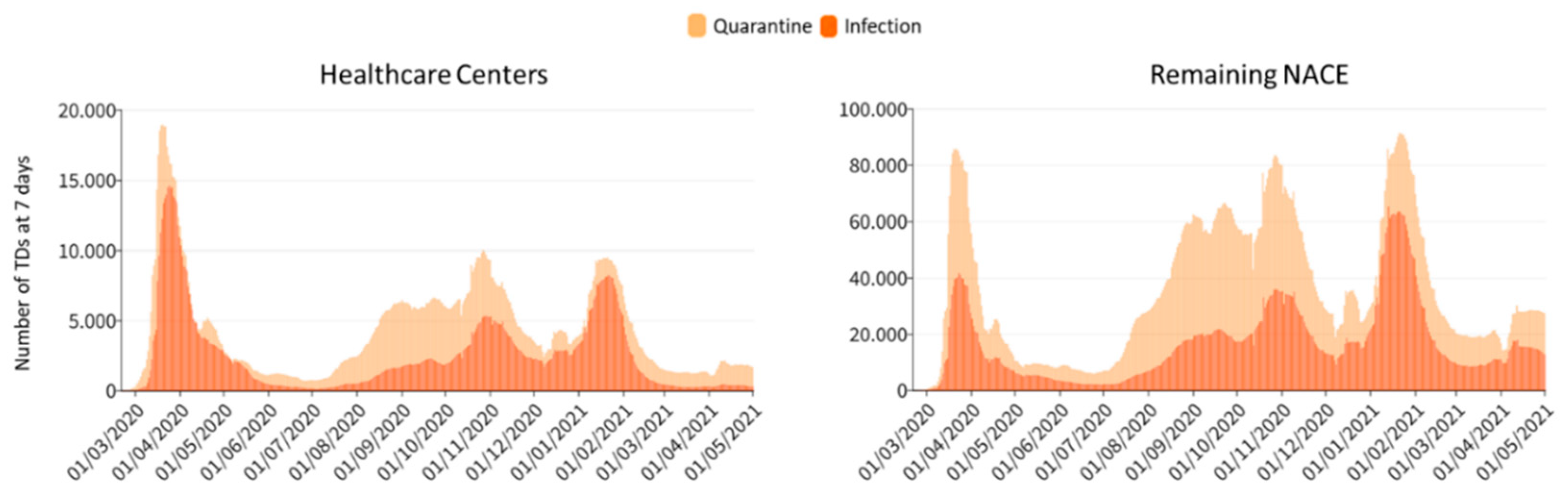
Between February 15 2020 and May 1 2021, 4,180,373 TD episodes related to COVID-19 were recorded for all economic activities, of which 1,400,274 for infection with COVID-19 and 2,780,099 for quarantine. No information on economic activity was available for 11.6% of these, being excluded from the analysis, which finally considered 3,697,491 TDs (1,198,524 for infection and 2,498,967 for quarantine). Among workers in Human Health activities (NACE Q86), there were 429,127 TDs (157,085 for infection and 273,042 for quarantine), representing 11.6% of the total number of TDs during this period (
Figure 1). TDs for infection in Human Health activities corresponded to 13.1% of the total TDs for infection.
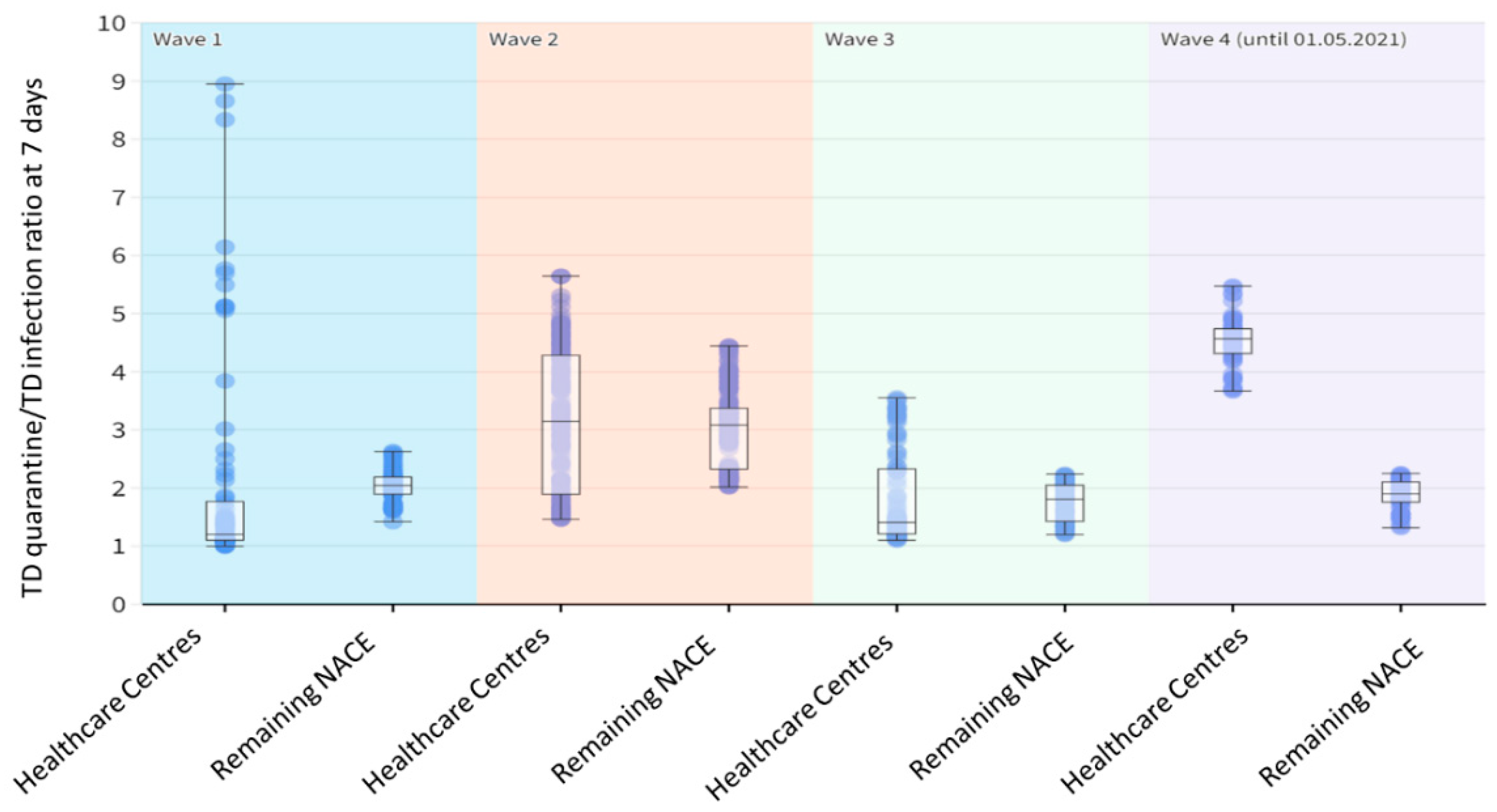
In all economic activities except for Human Health activities (remaining NACE codes), the median ratio between TDs for quarantine (close contacts) and those for infection (cases) was 2.15 (Interquartile range, IQR: 1.9-2.8) for the study period. This ratio was >3 (IQR: 2.3-3.4) during the second wave of the pandemic and was never < 1 during the whole study period (
Figure 1 and
Figure 2).
In Human Health activities, the median ratio for the study period was 2.5 (IQR: 1.5-3.9). After a peak of up to 9 TDs for quarantine per TD for infection during the first days of the pandemic, there was an abrupt drop to values close to one TD for quarantine per TD for infection for the rest of the first wave (IQR=1.1-1.8). The same can be observed during the second wave until the middle of the third, with values ranging from 5.7 to 1 TDs for quarantine per TD for infection. From the middle of the third wave, this ratio increased, reaching values above 5 in the fourth wave (IQR=4.3-4.7) (
Figure 1 and
Figure 2).
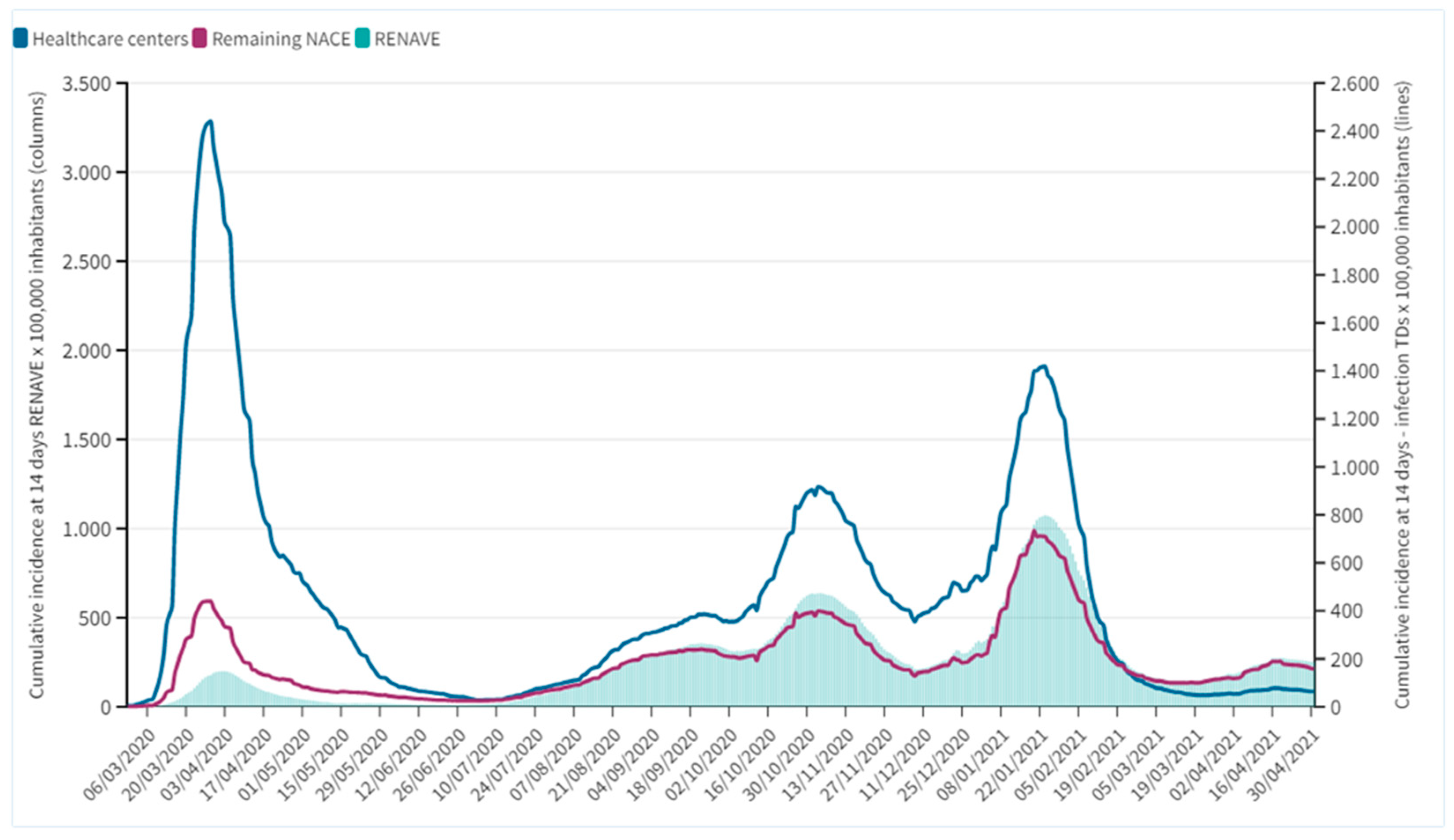
In Human Health activities, the maximum 14-day rate of TD for infection was reached on March 29 2020, with 2,440 TDs/100,000 affiliates. In all other economic activities, the maximum rate was recorded on January 20 2021 in the third wave, with 734 TDs /100,000 affiliates. The 14-day rates in Human Health activities were always above the cumulative incidence over 14 days notified to RENAVE and were above the rates in other economic activities, except for the last two months (
Figure 3).
A more detailed analysis of the period between February 15 and September 17 2020 was performed using INSS data, with information on activity group (3-digit NACE), occupation, age, sex, and autonomous community.
Table 1 lists the characteristics of the population employed in Human Health activities, the distribution of TDs for COVID-19, and COVID-19 infection rates per 100,000 individuals by economic activity group, sex, age, occupation, and autonomous community.
Hospital Activities (NACE 861) accounted for 84% of TDs and showed the highest accumulated TD rate for COVID-19 infection (8,279 cases per 100,000 employees). Employees older than 24 years accounted for 95% of recorded TDs, although the highest rate (8,828/100,000) was observed in those aged < 25 years: (
Table 1).
Among the total number of TDs, 76% were for women. The rate of TD for infection for the whole study period was higher for women (6,476/100,000) than for men 5,426/100,000), observing the greatest difference among under 24-year-olds (9,589/100,000 for women and 6,795/100,000 for men).
Regarding differences among autonomous communities, the largest number of TDs was in the Community of Madrid and Cataluña (55% of all TDs). The highest TD rate over the whole period was in the Community of Madrid (9,933/100,000), followed by Castilla y León (9,672/100,000) and Cataluña (9,274/100,000), and the lowest rates were in Ceuta, Islas Canarias, and Asturias (1,021, 1,761, and 2,045/100,000, respectively) (
Table 1).
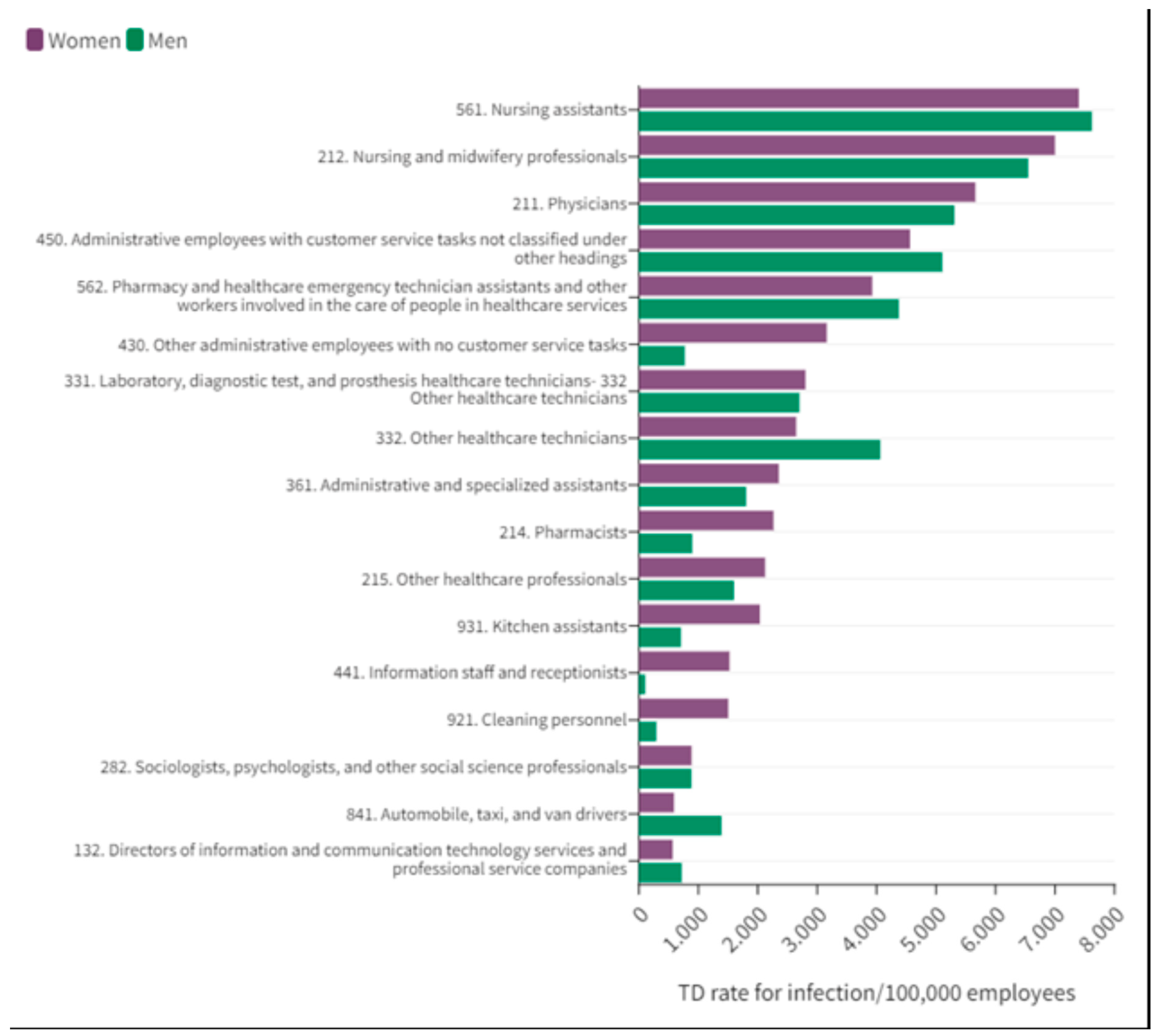
Information on occupation was unavailable for 11,230 TDs for COVID-19 (15.9%), who were excluded from this analysis. Most of the workers in healthcare centers (94%) were engaged in 17 representative occupations. TDs were recorded during the study period for 25.8% of Nursing professionals, 18.1% of Physicians, and 17% of Nursing assistants (17%). The proportion of employees with TD in the other 14 occupations ranged between 0.1 and 5.4% (
Table 1)
In 11 of the 17 occupations, the TD rate/100,000 was higher for women throughout the study period (
Figure 4), observing the greatest between-sex differences in Information staff and receptionists (1,524 in women and 106 in men), Cleaning personnel (1,502 and 294), Other administrative employees (3,160 and 772), Kitchen assistants (2,036 and 707), and Pharmacists (2,265 and 897).
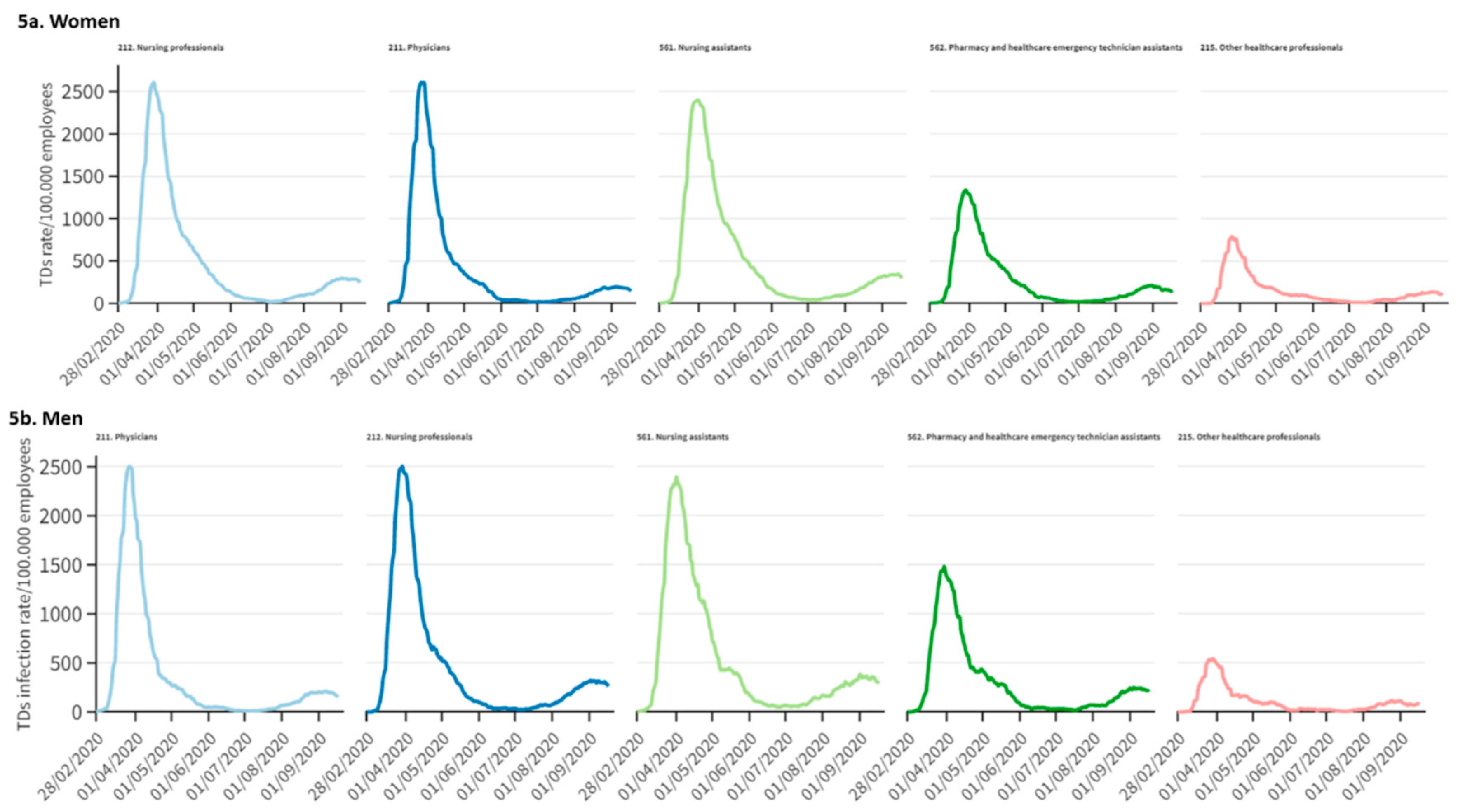
Data on the 14-day TD rate for infection/100,000 show that maximum values were reached during the last week of March in the five occupations with highest rates: observing rates of 2,607 in Physicians, 2,607 in Nursing professionals, 2,402 in Nursing assistants, 1,338 in Pharmacy assistant technicians, and 787 in Other healthcare professionals TD/100.000 employees (
Figure 5a).
Among men, the five occupations with highest rates also showed maximum values in the last week of March in the five occupations with highest rates, observing 14-day TD rates for infection/100,000 of 2,505 for Physicians, 2,505 for Nursing professionals, 2,398 for Nursing assistants, 1,484 for Pharmacy technicians, and 541 for other healthcare professionals (
Figure 5b).
4. Discussion
These findings demonstrate the high impact of COVID-19 on the number of TD episodes among professionals involved in healthcare activities in Spain during the first year of the pandemic. This impact was also found to have unequal effects between males and females, between healthcare activities, and between occupations. During the first wave of the pandemic, the 14-day TD rate was six-fold higher in healthcare activities than in other economic activities, and 38% of healthcare workers had a COVID-19-related TD, which was for the presence of confirmed infection in more than half of cases. Around 60% of employees in this sector are involved in hospital activities. These represented 84% of the total number of TDs and had the highest COVID-19 rate, three- to four-fold higher than recorded in other healthcare and dental activities.
The distribution of TD episodes varied in the different waves of the pandemic. The quarantine/infection TD ratio, was around one during the first wave and periods in the second wave up to the middle of the third, when the ratio increased until it reached more than five in the fourth wave, i.e., more than five TDs due to quarantine per one TD due to infection. In fact, the number of TDs due to infection never exceeded the TDs for quarantine, as opposite to what was observed in nursing homes during the same period [
9]. The lower quarantine/infection TD ratio in early stages can have various explanations. For instance, the overwhelmed health system was reluctant to grant TDs in order to maximize attending staff, especially for quarantine, with calls made to retired professionals to return to duties. Additionally, diagnosis tests were scarce and only applied to severe cases and health professionals, as in the UK and in the USA [
3], with the aim of avoiding further transmission to patients and colleagues. In the fourth wave, however, when the situation was better controlled, the ratio between TDs for quarantine and those for infection was considerably higher than in non-healthcare activities. This may have been caused by an increase in the number of TDs for quarantine in healthcare workers to minimize contacts with vulnerable people. An important finding was that the number and rate of TDs for COVID-19 infection increased earlier and were higher than the number and rate of cases recorded in the national RENAVE system from the beginning of the pandemic to February 2021. This may be attributable to the granting of TDs to individuals with suspicion of infection (pending confirmation), whereas the RENAVE only recorded confirmed cases. The earlier increase in the TD versus RENAVE system, mainly in the first wave but also in subsequent waves, supports the proposition that TDs are a good source of complementary information for the surveillance of COVID-19 [
9].
The 14-day TD rates for infection were higher in healthcare employees than in the rest of economic activities and in the general population during the first three pandemic waves, and the largest difference was in the first wave. In the healthcare sector in general and in the hospital setting in particular, workers were exposed to higher viral loads for longer time periods and were affected by staff shortages, lack of personal protective equipment; deficient ventilation, and the initial lack of knowledge about the disease. Furthermore, diagnostic tests were prioritized at the beginning of the pandemic for healthcare personnel, who were therefore more likely to be tested and diagnosed in comparison to other workers and the general population [
18]. Improvements in knowledge about the disease and its treatment, together with a higher availability of diagnostic tests and personal protective equipment, led to a reduction in rates beginning with the end of the third pandemic wave, when they were lower than of workers in other sectors and the general population. A definitive reduction in rates followed the high vaccination coverage of healthcare personnel [18, 19].
Given that 72% of workers in the healthcare sector are female, it is not surprising that 75% of TDs in this sector were for women. However, the rate was higher among women and in younger workers (aged < 24 years), and it is known that COVID-19 tends to be less severe in women than in men and in younger than older people [
1,
20]. This is in line with previous results for residential care and social work settings10, where higher TD rates were also observed in women with a greater patient care load and an inadequate supply of protective equipment. Further studies are required to explore these findings to support the design of preventive measures.
TD rates were higher in autonomous communities in which the pandemic was more intense, again finding an association of TDs in healthcare with the circulation of the virus in the general population [
21].
Among occupations, the highest TD rates were among Nursing assistants, followed by Nursing professionals and Physicians, consistent with the different amounts of time they spend with patients. Care activities that require close and prolonged contact with patients involve greater exposure and risk of infection. However, it has also been suggested that infection among coworkers in common areas may be even more important than SARS-CoV-2 transmission from patients [
22], especially at the beginning of the pandemic, and that personal protection equipment may be less rigorously used in areas where professionals rest, eat, and drink. Occupations with the lowest rates of TD for infection include Service managers, Social science professionals, Drivers, Information employees/receptionists, and Cleaning personnel. Prevention measures may have been more effective for cleaning staff, who would also be less at risk of disease transmission through contaminated fomites [
23].
One study limitation is the lack of personal identifiers, given that the same person may have a TD for quarantine and a later TD for infection or may suffer reinfections, and we were unable to distinguish these possibilities, which may have produced an overestimation of the TD rate. Nevertheless, the aim of the study was to determine the overall impact of the pandemic on the work setting in terms of TDs rather than to evaluate their incidence. It is also not possible to differentiate whether infections occurred at work or outside the working environment. Nonetheless, the nature of the work in health activities and the overlapping of the study period with the state of alarm, when mobility and non-work activities were severely limited [
18], suggests that infection is more likely to result from exposure at work, especially during the first wave, although infection in domestic and/or other settings cannot be ruled out. A study in UK hospitals estimated that 73% of infections in healthcare personnel between March and July 2020 were of nosocomial origin [
24]. To our knowledge, this study is the first one of this type in our country, thus comparison of the results with findings from other similar studies couldn´t be performed.
5. Conclusions
This study demonstrated that COVID-19 had a major impact on healthcare centers in Spain and that the effect was unequal between the sexes and occupations. The findings confirm that TDs represent a source of complementary information for epidemiological and public health surveillance. Given the high vaccination coverage of the population and the focus of COVID-19 surveillance on vulnerable individuals and settings, current priorities for healthcare professionals should be to reinforce the utilization of preventive measures and to ensure the follow-up of their mental and physical status to counteract long-term negative effects of COVID-19. Finally, the epidemiological follow-up of healthcare personnel using TDs can also be considered a relevant public health activity, given that utilization of this consolidated and well-primed system can produce an early warning of new emerging infections.
Author Contributions
The author’s contribution to this work is stated as follows: Conceptualization, M.G.G, A.M.G. and J.M.R.R.; methodology, M.G.G, A.M.G. and J.M.R.R.; software, A.M.G. and J.M.R.R.; validation, M.G.G., A.M.G. and J.M.R.R.; formal analysis, A.M.G. and J.M.R.R.; investigation, M.G.G, A.M.G. and J.M.R.R; data curation, A.M.G. and J.M.R.R.; writing—original draft preparation, M.G.G, A.M.G., J.M.R.R, L.M.M., J.O.D., S.E.L. ; writing—review and editing, M.G.G, A.M.G., J.M.R.R, L.M.M., J.O.D., S.E.L. visualization, M.G.G, A.M.G., J.M.R.R, L.M.M., J.O.D., S.E.L.
Funding
This research received no external funding
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Acknowledgments
The authors are grateful to the National Institute of Social Security (Instituto Nacional de la Seguridad Social) for providing TD-related data. We also acknowledge the National Epidemiology Centre (Centro Nacional de Epidemiología) and the Health Alert and Emergency Coordination Centre (Centro Coordinator de Alertas y Emergencias Sanitarias - CCAES) for data on COVID-19 cases notified to the in the National Epidemiological Surveillance Network (Red Nacional de Vigilancia Epidemiológica - RENAVE).
Conflicts of Interest
The authors declare no conflict of interest.
References
- Working group for the surveillance and control of COVID-19 in Spain. The first wave of the COVID-19 pandemic in Spain: characterisation of cases and risk factors for severe outcomes, as at 27 April 2020. Euro Surveill. 2020, 25.
- Spanish Ministry of Health. COVID-19 cases update. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/situacionActual.htm.
- Nguyen, L.H.; Drew, D.A.; Graham, M.S.; Joshi, A.D.; Guo, C.-G.; Ma, W.; et al. Risk of COVID-19 among front-line health-care workers and the general community: a prospective cohort study. Lancet Public Health. 2020, 5, e475–83. [Google Scholar] [CrossRef]
- Mutambudzi, M.; Niedwiedz, C.; Macdonald, E.B.; Leyland, A.; Mair, F.; Anderson, J.; et al. Occupation and risk of severe COVID-19: prospective cohort study of 120 075 UK Biobank participants. Occup Environ Med. 2020, 78, 307–14, Epub ahead of print. Erratum in: Occup Environ Med. 2022 Feb;79(2):e3. PMID: 33298533; PMCID: PMC7611715. [Google Scholar] [CrossRef]
- Wei, J.T.; Liu, Z.D.; Fan, Z.W.; Zhao, L.; Cao, W.C. Epidemiology of and Risk Factors for COVID-19 Infection among Health Care Workers: A Multi-Centre Comparative Study Int J Environ Res Public Health 2020, 17.
- Work Health Organization. Health Workforce Department. Working Paper 1. September 2021. [Citado 28 de marzo de 2022]. Available online: https://apps.who.int/iris/handle/10665/345300.
- Gholami, M.; Fawad, I.; Shadan, S.; Rowaiee, R.; Ghanem, H.; Hassan Khamis, A.; et al. COVID-19 and healthcare workers: A systematic review and meta-analysis. Int J Infect Dis. 2021, 104, 335–46. [Google Scholar] [CrossRef] [PubMed]
- Coordinated response actions to control the transmission of COVID-19. Committee for Alerts, Preparedness and Response Plans. Public Health Commission. Interterritorial Council of the National Health System. 2021. Technical documents for profesional. [Cited 26.03.2021]. Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actuaciones_respuesta_COVID_26.03.2021.pdf.
- García Gómez, M.; Gherasim, A.M.; Roldán Romero, J.M.; Zimmermann Verdejo, M.; Monge Corella, S.; Sierra Moros, M.J.; Montoya Martínez, L.M. El impacto de la COVID-19 en la incapacidad temporal de las personas que trabajan en centros socio-sanitarios en España. Utilidad de la incapacidad temporal para el seguimiento de la evolución de la pandemia. Rev Esp Salud Pública. 2022, 96, 4 de abril e202204038. [Google Scholar]
- Kaye, A.D.; Okeagu Chikezie, N.; Pham, A.D.; Silva, R.A.; Hurley, J.J.; Brett, L.A.; et al. Economic impact of COVID-19 pandemic on healthcare facilities and systems: International perspectives. Best Practice & Research Clinical Anesthesiology, Volume 35, Issue 3, 2021, Pages 293-306, ISSN 1521-6896. 2021; 35. [Google Scholar] [CrossRef]
- Danet Danet, A. Psychological impact of COVID-19 pandemic in Western frontline healthcare professionals. A systematic review, Medicina Clínica (English Edition), Volume 156, Issue 9,2021, Pages 449-458, ISSN 2387-0206. [CrossRef]
- Carlos III Public Health Institute, The National Epidemiology Centre. COVID-29 update in Spain -Report nº 124. Available online: https://www.isciii.es/QueHacemos/Servicios/VigilanciaSaludPublicaRENAVE/EnfermedadesTransmisibles/Documents/INFORMES/Informes%20COVID-19/INFORMES%20COVID-19%202022/Informe%20n%c2%ba%20124%20Situaci%c3%b3n%20de%20COVID-19%20en%20Espa%c3%b1a%20a%2030%20de%20marzo%20de%202022.pdf.
- Ministry of Inclusion, Social Security and Migrations. Sectorial and territorial evolution of the temporal disability due to COVID-19. 2021. Available online: https://www.seg-social.es/wps/portal/wss/internet/EstadisticasPresupuestosEstudios/Estadisticas/EST45/EST46.
- Ministry of Inclusion, Social Security and Migrations. Afiliación Media mensual. 2021. Available online: https://sede.seg-social.gob.es/wps/portal/sede/sede/Ciudadanos/2022Estadisticas/090316_C_AI.
- National Statistics Institute. Active Population Survey. [cited 27.04.2021]. 1254. Available online: https://www.ine.es/dyngs/INEbase/es/operacion.htm?c=Estadistica_C&cid=1254736176918&menu=ultiDatos&idp=1254735976595.
- National Statistics Institute. Population census. [cited 27.04.2021]. 3130. Available online: https://www.ine.es/jaxiT3/Tabla.htm?t=31304.
- The Spanish Government. The Council of Ministers. La Moncloa. Government decrees state of emergency to stop spread of coronavirus COVID-19 (14/03/2020). [cited 2021 Sep 6]. Available online: https://www.lamoncloa.gob.es/lang/en/gobierno/councilministers/Paginas/2020/20200314council-extr.aspx.
- Ministry of Health. Interterritorial Council of the National Health System. COVID-19 vaccination working group of the Vaccines Programme and registry Committee. Vaccine strategy against COVID-19 in Spain and updates. Available online: https://www.mscbs.gob.es/profesionales/saludPublica/prevPromocion/vacunaciones/covid19/Actualizaciones_EstrategiaVacunacionCOVID-19.htm.
- Olmedo Lucerón, C.; Limia Sánchez, A.; García Gómez, M. La vacunación frente a la COVID-19 en colectivos laborales. Rev Esp Salud Pública 2021, 95, 22 de octubre e202110121. [Google Scholar]
- The European Commission. Eurostat. Majority of health jobs held by women [Internet]. [cited 2021 Jul 14]. Available online: https://ec.europa.eu/eurostat/web/products-eurostat-news/-/edn-20210308-1.
- Spanish Ministry of Health. Health Alert and Emergency Coordination Centre (CCAES). COVID-19 update nº 150 (28.06.2020). Available online: https://www.sanidad.gob.es/profesionales/saludPublica/ccayes/alertasActual/nCov/documentos/Actualizacion_150_COVID-19.pdf.
- Lindsey, B.B.; Villabona-Arenas, C.J.; Campbell, F.; et al. Characterizing within-hospital SARS-CoV-2 transmission events using epidemiological and viral genomic data across two pandemic waves. Nat Commun 13, 671 (2022). [CrossRef]
- Dyani, L. COVID-19 rarely infects through surfaces. So why are we still deep cleaning? Nature Vol. 590 Pag. 26-28, 4 February 2021. Available from: d41586-021-00251-4.pdf (nature.com).
- Evans, S.; Emily Agnew, E.; Vynnycky, E.; Stimson, J.; Bhattacharya, A.; Rooney, C.; Warne, B.; Robotham, J. The impact of testing and infection prevention and control strategies on within-hospital transmission dynamics of COVID-19 in English hospitals. Philos Trans R Soc Lond B Biol Sci. 2021, 376, 20200268. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).