Submitted:
15 May 2023
Posted:
16 May 2023
You are already at the latest version
Abstract
Keywords:
1. Schizophrenia – an overview
2. NMDA receptor hypothesis of schizophrenia
3. Glutamatergic neurotransmission in the CNS
4. NMDA receptor structure and function
4.1. GluN2D receptor subunit expression and distribution
4.2. GluN2D receptor subunit function
5. Alterations to GluN2D in schizophrenia
6. How might alterations to the GluN2D subunit contribute to schizophrenia?
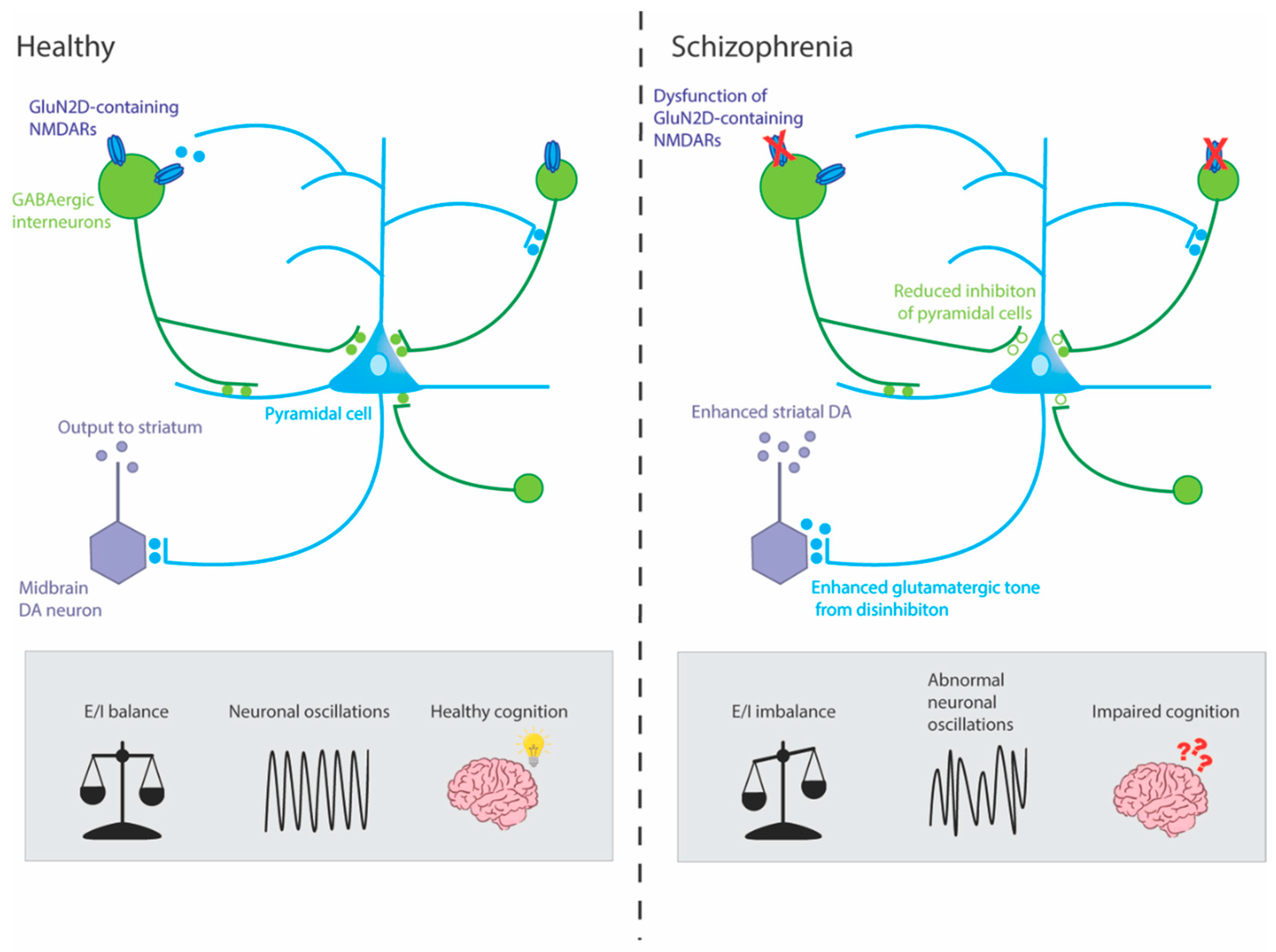
6.1. NMDAR hypofunction on GABAergic interneurons
6.2. GluN2D subunit and Parvalbumin-positive GABAergic interneurons
7. Consequences of loss of GluN2D function
7.1. Genetic models
7.2. Pharmacological manipulations
8. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- Saha, S.; Chant, D.; Welham, J.; McGrath, J. , A systematic review of the prevalence of schizophrenia. PLoS Med 2005, 2, e141. [Google Scholar] [CrossRef] [PubMed]
- McCutcheon, R.A.; Reis Marques, T.; Howes, O.D. , Schizophrenia-An Overview. JAMA Psychiatry 2020, 77, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Kahn, R.; Sommer, I.; Murray, R.; Meyer-Lindenberg, A.; Weinberger, D.; Cannon, T.; O’Donovan, M.; Correl, C.; Kane, J.; van Os, J. , Schizophrenia. Nature Reviews Disease Primers. Nov 2015, 12, 15067. [Google Scholar]
- Keefe, R.S.; Eesley, C.E.; Poe, M.P. , Defining a cognitive function decrement in schizophrenia. Biological psychiatry 2005, 57, 688–691. [Google Scholar] [CrossRef] [PubMed]
- Awad, A.G.; Voruganti, L.N. , The burden of schizophrenia on caregivers: a review. Pharmacoeconomics 2008, 26, 149–162. [Google Scholar] [CrossRef] [PubMed]
- Cloutier, M.; Aigbogun, M.S.; Guerin, A.; Nitulescu, R.; Ramanakumar, A.V.; Kamat, S.A.; DeLucia, M.; Duffy, R.; Legacy, S.N.; Henderson, C.; Francois, C.; Wu, E. , The Economic Burden of Schizophrenia in the United States in 2013. J Clin Psychiatry 2016, 77, 764–71. [Google Scholar] [CrossRef] [PubMed]
- Neil, A.L.; Carr, V.J.; Mihalopoulos, C.; Mackinnon, A.; Morgan, V.A. , Costs of psychosis in 2010: Findings from the second Australian National Survey of Psychosis. Australian & New Zealand Journal of Psychiatry 2014, 48, 169–182. [Google Scholar]
- Ripke, S.; Neale, B.M.; Corvin, A.; Walters, J.T.; Farh, K.-H.; Holmans, P.A.; Lee, P.; Bulik-Sullivan, B.; Collier, D.A.; Huang, H. , Biological insights from 108 schizophrenia-associated genetic loci. Nature 2014, 511, 421–427. [Google Scholar]
- Gottesman, I.I.; Shields, J. , A polygenic theory of schizophrenia. International Journal of Mental Health 1972, 1, 107–115. [Google Scholar] [CrossRef]
- Trubetskoy, V.; Pardiñas, A.F.; Qi, T.; Panagiotaropoulou, G.; Awasthi, S.; Bigdeli, T.B.; Bryois, J.; Chen, C.-Y.; Dennison, C.A.; Hall, L.S. , Mapping genomic loci implicates genes and synaptic biology in schizophrenia. Nature 2022, 604, 502–508. [Google Scholar] [CrossRef]
- Walsh, T.; McClellan, J.M.; McCarthy, S.E.; Addington, A.M.; Pierce, S.B.; Cooper, G.M.; Nord, A.S.; Kusenda, M.; Malhotra, D.; Bhandari, A.; Stray, S.M.; Rippey, C.F.; Roccanova, P.; Makarov, V.; Lakshmi, B.; Findling, R.L.; Sikich, L.; Stromberg, T.; Merriman, B.; Gogtay, N.; Butler, P.; Eckstrand, K.; Noory, L.; Gochman, P.; Long, R.; Chen, Z.; Davis, S.; Baker, C.; Eichler, E.E.; Meltzer, P.S.; Nelson, S.F.; Singleton, A.B.; Lee, M.K.; Rapoport, J.L.; King, M.C.; Sebat, J. , Rare structural variants disrupt multiple genes in neurodevelopmental pathways in schizophrenia. Science 2008, 320, 539–43. [Google Scholar] [CrossRef] [PubMed]
- Fromer, M.; Roussos, P.; Sieberts, S.K.; Johnson, J.S.; Kavanagh, D.H.; Perumal, T.M.; Ruderfer, D.M.; Oh, E.C.; Topol, A.; Shah, H.R.; Klei, L.L.; Kramer, R.; Pinto, D.; Gumus, Z.H.; Cicek, A.E.; Dang, K.K.; Browne, A.; Lu, C.; Xie, L.; Readhead, B.; Stahl, E.A.; Xiao, J.; Parvizi, M.; Hamamsy, T.; Fullard, J.F.; Wang, Y.C.; Mahajan, M.C.; Derry, J.M.; Dudley, J.T.; Hemby, S.E.; Logsdon, B.A.; Talbot, K.; Raj, T.; Bennett, D.A.; De Jager, P.L.; Zhu, J.; Zhang, B.; Sullivan, P.F.; Chess, A.; Purcell, S.M.; Shinobu, L.A.; Mangravite, L.M.; Toyoshiba, H.; Gur, R.E.; Hahn, C.G.; Lewis, D.A.; Haroutunian, V.; Peters, M.A.; Lipska, B.K.; Buxbaum, J.D.; Schadt, E.E.; Hirai, K.; Roeder, K.; Brennand, K.J.; Katsanis, N.; Domenici, E.; Devlin, B.; Sklar, P. , Gene expression elucidates functional impact of polygenic risk for schizophrenia. Nat Neurosci 2016, 19, 1442–1453. [Google Scholar] [CrossRef] [PubMed]
- Ursini, G.; Punzi, G.; Chen, Q.; Marenco, S.; Robinson, J.F.; Porcelli, A.; Hamilton, E.G.; Mitjans, M.; Maddalena, G.; Begemann, M.; Seidel, J.; Yanamori, H.; Jaffe, A.E.; Berman, K.F.; Egan, M.F.; Straub, R.E.; Colantuoni, C.; Blasi, G.; Hashimoto, R.; Rujescu, D.; Ehrenreich, H.; Bertolino, A.; Weinberger, D.R. , Convergence of placenta biology and genetic risk for schizophrenia. Nat Med 2018, 24, 792–801. [Google Scholar] [CrossRef] [PubMed]
- Malaspina, D.; Harlap, S.; Fennig, S.; Heiman, D.; Nahon, D.; Feldman, D.; Susser, E.S. , Advancing paternal age and the risk of schizophrenia. Arch Gen Psychiatry 2001, 58, 361–7. [Google Scholar] [CrossRef] [PubMed]
- Fountoulakis, K.N.; Gonda, X.; Siamouli, M.; Panagiotidis, P.; Moutou, K.; Nimatoudis, I.; Kasper, S. , Paternal and maternal age as risk factors for schizophrenia: a case–control study. International journal of psychiatry in clinical practice 2018, 22, 170–176. [Google Scholar] [CrossRef] [PubMed]
- Radua, J.; Ramella-Cravaro, V.; Ioannidis, J.P.; Reichenberg, A.; Phiphopthatsanee, N.; Amir, T.; Yenn Thoo, H.; Oliver, D.; Davies, C.; Morgan, C. , What causes psychosis? An umbrella review of risk and protective factors. World Psychiatry 2018, 17, 49–66. [Google Scholar] [CrossRef] [PubMed]
- Stilo, S.A.; Murray, R.M. , Non-Genetic Factors in Schizophrenia. Curr Psychiatry Rep 2019, 21, 100. [Google Scholar] [CrossRef] [PubMed]
- Cantor-Graae, E.; Selten, J.-P. , Schizophrenia and migration: a meta-analysis and review. American Journal of Psychiatry 2005, 162, 12–24. [Google Scholar] [CrossRef]
- Varese, F.; Smeets, F.; Drukker, M.; Lieverse, R.; Lataster, T.; Viechtbauer, W.; Read, J.; Van Os, J.; Bentall, R.P. , Childhood adversities increase the risk of psychosis: a meta-analysis of patient-control, prospective-and cross-sectional cohort studies. Schizophrenia bulletin 2012, 38, 661–671. [Google Scholar] [CrossRef]
- Kane, J.M.; Correll, C.U. , Pharmacologic treatment of schizophrenia. Dialogues in clinical neuroscience 2022. [Google Scholar]
- Leucht, S.; Corves, C.; Arbter, D.; Engel, R.R.; Li, C.; Davis, J.M. , Second-generation versus first-generation antipsychotic drugs for schizophrenia: a meta-analysis. Lancet 2009, 373, 31–41. [Google Scholar] [CrossRef] [PubMed]
- Stępnicki, P.; Kondej, M.; Kaczor, A.A. , Current concepts and treatments of schizophrenia. Molecules 2018, 23, 2087. [Google Scholar] [CrossRef]
- Keefe, R.S.; Bilder, R.M.; Davis, S.M.; Harvey, P.D.; Palmer, B.W.; Gold, J.M.; Meltzer, H.Y.; Green, M.F.; Capuano, G.; Stroup, T.S. , Neurocognitive effects of antipsychotic medications in patients with chronic schizophrenia in the CATIE Trial. Archives of general psychiatry 2007, 64, 633–647. [Google Scholar] [CrossRef] [PubMed]
- Hietala, J.; Syvälahti, E. , Dopamine in schizophrenia. Annals of medicine 1996, 28, 557–561. [Google Scholar] [CrossRef] [PubMed]
- Gründer, G.; Cumming, P. , The dopamine hypothesis of schizophrenia: Current status. In The neurobiology of schizophrenia, Elsevier: 2016; pp 109-124.
- Davis, K.L.; Kahn, R.S.; Ko, G.; Davidson, M. , Dopamine in schizophrenia: a review and reconceptualization. The American journal of psychiatry 1991. [Google Scholar]
- Seeman, P.; Lee, T.; Chau-Wong, M.; Wong, K. , Antipsychotic drug doses and neuroleptic/dopamine receptors. Nature 1976, 261, 717–719. [Google Scholar] [CrossRef] [PubMed]
- Van Rossum, J. , The significance of dopamine-receptor blockade for the mechanism of action of neuroleptic drugs. Arch. Int Pharmacodyn Ther 1996, 160, 492–494. [Google Scholar]
- Seeman, M.V. , History of the dopamine hypothesis of antipsychotic action. World Journal of Psychiatry 2021, 11, 355. [Google Scholar] [CrossRef]
- Seeman, P. , Dopamine receptors and the dopamine hypothesis of schizophrenia. Synapse 1987, 1, 133–152. [Google Scholar] [CrossRef]
- Snyder, S.H. , Dopamine receptors, neuroleptics, and schizophrenia. The American journal of psychiatry 1981. [Google Scholar]
- Lisman, J.E.; Coyle, J.T.; Green, R.W.; Javitt, D.C.; Benes, F.M.; Heckers, S.; Grace, A.A. , Circuit-based framework for understanding neurotransmitter and risk gene interactions in schizophrenia. Trends in neurosciences 2008, 31, 234–242. [Google Scholar] [CrossRef] [PubMed]
- Kantrowitz, J.T.; Javitt, D.C. , N-methyl-d-aspartate (NMDA) receptor dysfunction or dysregulation: the final common pathway on the road to schizophrenia? Brain Res Bull 2010, 83, 108–21. [Google Scholar] [CrossRef] [PubMed]
- Coyle, J.T.; Tsai, G.; Goff, D. , Converging evidence of NMDA receptor hypofunction in the pathophysiology of schizophrenia. Annals of the New York Academy of Sciences 2003, 1003, 318–327. [Google Scholar] [CrossRef] [PubMed]
- Krystal, J.H.; Karper, L.P.; Seibyl, J.P.; Freeman, G.K.; Delaney, R.; Bremner, J.D.; Heninger, G.R.; Bowers, M.B., Jr.; Charney, D.S. , Subanesthetic effects of the noncompetitive NMDA antagonist, ketamine, in humans. Psychotomimetic, perceptual, cognitive, and neuroendocrine responses. Arch Gen Psychiatry 1994, 51, 199–214. [Google Scholar] [CrossRef] [PubMed]
- Javitt, D. , Negative schizophrenic symptomatology and the PCP (phencyclidine) model of schizophrenia. The Hillside journal of clinical psychiatry 1987, 9, 12–35. [Google Scholar] [PubMed]
- Luby, E.D.; Cohen, B.D.; Rosenbaum, G.; Gottlieb, J.S.; Kelley, R. , Study of a new schizophrenomimetic drug—Sernyl. AMA Archives of Neurology & Psychiatry 1959, 81, 363–369. [Google Scholar]
- Luby, E.D.; Gottlieb, J.S.; Cohen, B.D.; Rosenbaum, G.; Domino, E.F. , Model psychoses and schizophrenia. American Journal of Psychiatry 1962, 119, 61–67. [Google Scholar] [CrossRef] [PubMed]
- Rosenbaum, G.; Cohen, B.D.; Luby, E.D.; Gottlieb, J.S.; Yelen, D. , Comparison of sernyl with other drugs: simulation of schizophrenic performance with sernyl, LSD-25, and amobarbital (amytal) sodium; I. Attention, motor function, and proprioception. AMA archives of general psychiatry 1959, 1, 651–656. [Google Scholar] [CrossRef]
- Cohen, B.D.; Luby, E.D.; Rosenbaum, G.; Gottlieb, J.S. , Combined sernyl and sensory deprivation. Comprehensive Psychiatry 1960, 1, 345–348. [Google Scholar] [CrossRef]
- Itil, T.; Keskiner, A.; Kiremitci, N.; Holden, J. , Effect of phencyclidine in chronic schizophrenics. Canadian Psychiatric Association Journal 1967, 12, 209–212. [Google Scholar] [CrossRef]
- Lahti, A.C.; Koffel, B.; LaPorte, D.; Tamminga, C.A. , Subanesthetic doses of ketamine stimulate psychosis in schizophrenia. Neuropsychopharmacology 1995, 13, 9–19. [Google Scholar] [CrossRef] [PubMed]
- Anis, N.A.; Berry, S.C.; Burton, N.R.; Lodge, D. , The dissociative anaesthetics, ketamine and phencyclidine, selectively reduce excitation of central mammalian neurones by N-methyl-aspartate. Br J Pharmacol 1983, 79, 565–75. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Kornhuber, H.; Schmid-Burgk, W.; Holzmüller, B. , Low cerebrospinal fluid glutamate in schizophrenic patients and a new hypothesis on schizophrenia. Neuroscience letters 1980, 20, 379–382. [Google Scholar] [CrossRef] [PubMed]
- Javitt, D.C.; Zukin, S.R. , Recent advances in the phencyclidine model of schizophrenia. The American journal of psychiatry 1991. [Google Scholar]
- Javitt, D.C. , Glutamatergic theories of schizophrenia. Isr J Psychiatry Relat Sci 2010, 47, 4–16. [Google Scholar] [PubMed]
- Kantrowitz, J.; Javitt, D.C. , Glutamatergic transmission in schizophrenia: from basic research to clinical practice. Curr Opin Psychiatry 2012, 25, 96–102. [Google Scholar] [CrossRef] [PubMed]
- Snyder, S.H. , The dopamine hypothesis of schizophrenia: focus on the dopamine receptor. The American journal of psychiatry 1976. [Google Scholar]
- Nakazawa, K.; Zsiros, V.; Jiang, Z.; Nakao, K.; Kolata, S.; Zhang, S.; Belforte, J.E. , GABAergic interneuron origin of schizophrenia pathophysiology. Neuropharmacology 2012, 62, 1574–83. [Google Scholar] [CrossRef]
- Javitt, D.C.; Hashim, A.; Sershen, H. , Modulation of striatal dopamine release by glycine transport inhibitors. Neuropsychopharmacology 2005, 30, 649–656. [Google Scholar] [CrossRef]
- Nair, V.D.; Savelli, J.E.; Mishra, R.K. , Modulation of dopamine D 2 receptor expression by an NMDA receptor antagonist in rat brain. Journal of Molecular Neuroscience 1998, 11, 121–126. [Google Scholar] [CrossRef]
- Micheletti, G.; Lannes, B.; Haby, C.; Borrelli, E.; Kempf, E.; Warter, J.-M.; Zwiller, J. , Chronic administration of NMDA antagonists induces D2 receptor synthesis in rat striatum. Molecular brain research 1992, 14, 363–368. [Google Scholar] [CrossRef] [PubMed]
- Kegeles, L.S.; Abi-Dargham, A.; Zea-Ponce, Y.; Rodenhiser-Hill, J.; Mann, J.J.; Van Heertum, R.L.; Cooper, T.B.; Carlsson, A.; Laruelle, M. , Modulation of amphetamine-induced striatal dopamine release by ketamine in humans: implications for schizophrenia. Biological psychiatry 2000, 48, 627–640. [Google Scholar] [CrossRef] [PubMed]
- Smith, G.S.; Schloesser, R.; Brodie, J.D.; Dewey, S.L.; Logan, J.; Vitkun, S.A.; Simkowitz, P.; Hurley, A.; Cooper, T.; Volkow, N.D. , Glutamate modulation of dopamine measured in vivo with positron emission tomography (PET) and 11C-raclopride in normal human subjects. Neuropsychopharmacology 1998, 18, 18–25. [Google Scholar] [CrossRef] [PubMed]
- Homayoun, H.; Moghaddam, B. , NMDA receptor hypofunction produces opposite effects on prefrontal cortex interneurons and pyramidal neurons. Journal of Neuroscience 2007, 27, 11496–11500. [Google Scholar] [CrossRef] [PubMed]
- Li, Q.; Clark, S.; Lewis, D.V.; Wilson, W.A. , NMDA receptor antagonists disinhibit rat posterior cingulate and retrosplenial cortices: a potential mechanism of neurotoxicity. Journal of Neuroscience 2002, 22, 3070–3080. [Google Scholar] [CrossRef] [PubMed]
- Olney, J.W.; Farber, N.B. , Glutamate receptor dysfunction and schizophrenia. Archives of general psychiatry 1995, 52, 998–1007. [Google Scholar] [CrossRef] [PubMed]
- Olney, J.; Labruyere, J.; Wang, G.; Wozniak, D.; Price, M.; Sesma, M. , NMDA antagonist neurotoxicity: mechanism and prevention. Science 1991, 254, 1515–1518. [Google Scholar] [CrossRef]
- Sun, J.; Jia, P.; Fanous, A.H.; Van Den Oord, E.; Chen, X.; Riley, B.P.; Amdur, R.L.; Kendler, K.S.; Zhao, Z. , Schizophrenia gene networks and pathways and their applications for novel candidate gene selection. PloS one 2010, 5, e11351. [Google Scholar] [CrossRef]
- Greenwood, T.A.; Light, G.A.; Swerdlow, N.R.; Radant, A.D.; Braff, D.L. , Association analysis of 94 candidate genes and schizophrenia-related endophenotypes. PLoS One 2012, 7, e29630. [Google Scholar] [CrossRef]
- Balu, D.T.; Coyle, J.T. , Neuroplasticity signaling pathways linked to the pathophysiology of schizophrenia. Neurosci Biobehav Rev 2011, 35, 848–70. [Google Scholar] [CrossRef]
- Balu, D.T. , The NMDA receptor and schizophrenia: from pathophysiology to treatment. In Advances in Pharmacology, Elsevier: 2016; Vol. 76, pp 351-382.
- Hashimoto, K.; Fukushima, T.; Shimizu, E.; Komatsu, N.; Watanabe, H.; Shinoda, N.; Nakazato, M.; Kumakiri, C.; Okada, S.; Hasegawa, H.; Imai, K.; Iyo, M. , Decreased serum levels of D-serine in patients with schizophrenia: evidence in support of the N-methyl-D-aspartate receptor hypofunction hypothesis of schizophrenia. Arch Gen Psychiatry 2003, 60, 572–6. [Google Scholar] [CrossRef] [PubMed]
- Weickert, C.S.; Fung, S.J.; Catts, V.S.; Schofield, P.R.; Allen, K.M.; Moore, L.T.; Newell, K.A.; Pellen, D.; Huang, X.F.; Catts, S.V.; Weickert, T.W. , Molecular evidence of N-methyl-D-aspartate receptor hypofunction in schizophrenia. Mol Psychiatry 2013, 18, 1185–92. [Google Scholar] [CrossRef] [PubMed]
- Labrie, V.; Lipina, T.; Roder, J.C. , Mice with reduced NMDA receptor glycine affinity model some of the negative and cognitive symptoms of schizophrenia. Psychopharmacology 2008, 200, 217–230. [Google Scholar] [CrossRef] [PubMed]
- Mohn, A.R.; Gainetdinov, R.R.; Caron, M.G.; Koller, B.H. , Mice with reduced NMDA receptor expression display behaviors related to schizophrenia. Cell 1999, 98, 427–436. [Google Scholar] [CrossRef] [PubMed]
- Halene, T.B.; Ehrlichman, R.S.; Liang, Y.; Christian, E.P.; Jonak, G.J.; Gur, T.L.; Blendy, J.A.; Dow, H.C.; Brodkin, E.S.; Schneider, F. , Assessment of NMDA receptor NR1 subunit hypofunction in mice as a model for schizophrenia. Genes, Brain and Behavior 2009, 8, 661–675. [Google Scholar] [CrossRef] [PubMed]
- Hakami, T.; Jones, N.C.; Tolmacheva, E.A.; Gaudias, J.; Chaumont, J.; Salzberg, M.; O'Brien, T.J.; Pinault, D. , NMDA receptor hypofunction leads to generalized and persistent aberrant γ oscillations independent of hyperlocomotion and the state of consciousness. PloS one 2009, 4, e6755. [Google Scholar] [CrossRef] [PubMed]
- Anderson, P.M.; Pinault, D.; O'Brien, T.J.; Jones, N.C. , Chronic administration of antipsychotics attenuates ongoing and ketamine-induced increases in cortical γ oscillations. International Journal of Neuropsychopharmacology 2014, 17, 1895–1904. [Google Scholar] [CrossRef] [PubMed]
- Hudson, M.; Rind, G.; O'brien, T.; Jones, N. , Reversal of evoked gamma oscillation deficits is predictive of antipsychotic activity with a unique profile for clozapine. Translational psychiatry 2016, 6, e784–e784. [Google Scholar] [CrossRef]
- Zhou, Y.; Danbolt, N.C. , Glutamate as a neurotransmitter in the healthy brain. Journal of neural transmission 2014, 121, 799–817. [Google Scholar] [CrossRef]
- Hollmann, M.; Heinemann, S. , Cloned glutamate receptors. Annual review of neuroscience 1994, 17, 31–108. [Google Scholar] [CrossRef]
- Nakanishi, S.; Masu, M. , Molecular diversity and functions of glutamate receptors. Annual review of biophysics and biomolecular structure 1994, 23, 319–348. [Google Scholar] [CrossRef] [PubMed]
- Yonezawa, K.; Tani, H.; Nakajima, S.; Nagai, N.; Koizumi, T.; Miyazaki, T.; Mimura, M.; Takahashi, T.; Uchida, H. , AMPA receptors in schizophrenia: A systematic review of postmortem studies on receptor subunit expression and binding. Schizophrenia Research 2022, 243, 98–109. [Google Scholar] [CrossRef] [PubMed]
- Rubio, M.D.; Drummond, J.B.; Meador-Woodruff, J.H. , Glutamate receptor abnormalities in schizophrenia: implications for innovative treatments. Biomolecules & therapeutics 2012, 20, 1. [Google Scholar]
- Maksymetz, J.; Moran, S.P.; Conn, P.J. , Targeting metabotropic glutamate receptors for novel treatments of schizophrenia. Molecular brain 2017, 10, 1–19. [Google Scholar]
- Scatton, B. , The NMDA receptor complex. Fundamental & clinical pharmacology 1993, 7, 389–400. [Google Scholar]
- Traynelis, S.F.; Wollmuth, L.P.; McBain, C.J.; Menniti, F.S.; Vance, K.M.; Ogden, K.K.; Hansen, K.B.; Yuan, H.; Myers, S.J.; Dingledine, R. , Glutamate receptor ion channels: structure, regulation, and function. Pharmacol Rev 2010, 62, 405–96. [Google Scholar] [CrossRef]
- Monyer, H.; Sprengel, R.; Schoepfer, R.; Herb, A.; Higuchi, M.; Lomeli, H.; Burnashev, N.; Sakmann, B.; Seeburg, P.H. , Heteromeric NMDA receptors: molecular and functional distinction of subtypes. Science 1992, 256, 1217–1221. [Google Scholar] [CrossRef]
- Karakas, E.; Furukawa, H. , Crystal structure of a heterotetrameric NMDA receptor ion channel. Science 2014, 344, 992–997. [Google Scholar] [CrossRef]
- Furukawa, H.; Singh, S.K.; Mancusso, R.; Gouaux, E. , Subunit arrangement and function in NMDA receptors. Nature 2005, 438, 185–192. [Google Scholar] [CrossRef]
- Lerma, J.; Zukin, R.S.; Bennett, M. , Glycine decreases desensitization of N-methyl-D-aspartate (NMDA) receptors expressed in Xenopus oocytes and is required for NMDA responses. Proceedings of the National Academy of Sciences 1990, 87, 2354–2358. [Google Scholar] [CrossRef]
- Greer, P.L.; Greenberg, M.E. , From synapse to nucleus: calcium-dependent gene transcription in the control of synapse development and function. Neuron 2008, 59, 846–860. [Google Scholar] [CrossRef] [PubMed]
- Artola, A.; Bröcher, S.; Singer, W. , Different voltage-dependent thresholds for inducing long-term depression and long-term potentiation in slices of rat visual cortex. Nature 1990, 347, 69–72. [Google Scholar] [CrossRef] [PubMed]
- Miyamoto, E. , Molecular mechanism of neuronal plasticity: induction and maintenance of long-term potentiation in the hippocampus. Journal of pharmacological sciences 2006, 100, 433–442. [Google Scholar] [CrossRef] [PubMed]
- Sugihara, H.; Moriyoshi, K.; Ishii, T.; Masu, M.; Nakanishi, S. , Structures and properties of seven isoforms of the NMDA receptor generated by alternative splicing. Biochemical and biophysical research communications 1992, 185, 826–832. [Google Scholar] [CrossRef] [PubMed]
- Paoletti, P.; Bellone, C.; Zhou, Q. , NMDA receptor subunit diversity: impact on receptor properties, synaptic plasticity and disease. Nature Reviews Neuroscience 2013, 14, 383–400. [Google Scholar] [CrossRef] [PubMed]
- Schorge, S.; Colquhoun, D. , Studies of NMDA receptor function and stoichiometry with truncated and tandem subunits. Journal of Neuroscience 2003, 23, 1151–1158. [Google Scholar] [CrossRef] [PubMed]
- Henson, M.A.; Roberts, A.C.; Salimi, K.; Vadlamudi, S.; Hamer, R.M.; Gilmore, J.H.; Jarskog, L.F.; Philpot, B.D. , Developmental regulation of the NMDA receptor subunits, NR3A and NR1, in human prefrontal cortex. Cerebral Cortex 2008, 18, 2560–2573. [Google Scholar] [CrossRef]
- Tolle, T.; Berthele, A.; Zieglgansberger, W.; Seeburg, P.H.; Wisden, W. , The differential expression of 16 NMDA and non-NMDA receptor subunits in the rat spinal cord and in periaqueductal gray. Journal of Neuroscience 1993, 13, 5009–5028. [Google Scholar] [CrossRef]
- Monyer, H.; Burnashev, N.; Laurie, D.J.; Sakmann, B.; Seeburg, P.H. , Developmental and regional expression in the rat brain and functional properties of four NMDA receptors. Neuron 1994, 12, 529–40. [Google Scholar] [CrossRef]
- Vicini, S.; Wang, J.F.; Li, J.H.; Zhu, W.J.; Wang, Y.H.; Luo, J.H.; Wolfe, B.B.; Grayson, D.R. , Functional and pharmacological differences between recombinant N-methyl-D-aspartate receptors. Journal of neurophysiology 1998, 79, 555–566. [Google Scholar] [CrossRef]
- Huggins, D.J.; Grant, G.H. , The function of the amino terminal domain in NMDA receptor modulation. Journal of Molecular Graphics and Modelling 2005, 23, 381–388. [Google Scholar] [CrossRef] [PubMed]
- Ishii, T.; Moriyoshi, K.; Sugihara, H.; Sakurada, K.; Kadotani, H.; Yokoi, M.; Akazawa, C.; Shigemoto, R.; Mizuno, N.; Masu, M. , Molecular characterization of the family of the N-methyl-D-aspartate receptor subunits. Journal of Biological Chemistry 1993, 268, 2836–2843. [Google Scholar] [CrossRef] [PubMed]
- Akazawa, C.; Shigemoto, R.; Bessho, Y.; Nakanishi, S.; Mizuno, N. , Differential expression of five N-methyl-D-aspartate receptor subunit mRNAs in the cerebellum of developing and adult rats. J Comp Neurol 1994, 347, 150–60. [Google Scholar] [CrossRef] [PubMed]
- Wenzel, A.; Villa, M.; Mohler, H.; Benke, D. , Developmental and regional expression of NMDA receptor subtypes containing the NR2D subunit in rat brain. Journal of neurochemistry 1996, 66, 1240–1248. [Google Scholar] [CrossRef]
- Dunah, A.W.; Yasuda, R.P.; Wang, Y. h.; Luo, J.; Dávila-García, M.I.; Gbadegesin, M.; Vicini, S.; Wolfe, B.B. , Regional and ontogenic expression of the NMDA receptor subunit NR2D protein in rat brain using a subunit-specific antibody. Journal of neurochemistry 1996, 67, 2335–2345. [Google Scholar] [CrossRef]
- Standaert, D.G.; Landwehrmeyer, G.B.; Kerner, J.A.; Penney Jr, J.B.; Young, A.B. , Expression of NMDAR2D glutamate receptor subunit mRNA in neurochemically identified interneurons in the rat neostriatum, neocortex and hippocampus. Molecular brain research 1996, 42, 89–102. [Google Scholar] [CrossRef]
- Cannon, M.; Murray, R.M. , Neonatal origins of schizophrenia. Archives of disease in childhood 1998, 78, 1–3. [Google Scholar] [CrossRef]
- Birnbaum, R.; Weinberger, D.R. , Genetic insights into the neurodevelopmental origins of schizophrenia. Nature Reviews Neuroscience 2017, 18, 727–740. [Google Scholar] [CrossRef]
- Engelhardt, J. v.; Bocklisch, C.; Tönges, L.; Herb, A.; Mishina, M.; Monyer, H. , GluN2D-containing NMDA receptors-mediate synaptic currents in hippocampal interneurons and pyramidal cells in juvenile mice. Frontiers in cellular neuroscience 2015, 9, 95. [Google Scholar] [CrossRef]
- Garst-Orozco, J.; Malik, R.; Lanz, T.A.; Weber, M.L.; Xi, H.; Arion, D.; Enwright III, J.F.; Lewis, D.A.; O’Donnell, P.; Sohal, V.S. , GluN2D-mediated excitatory drive onto medial prefrontal cortical PV+ fast-spiking inhibitory interneurons. Plos one 2020, 15, e0233895. [Google Scholar] [CrossRef]
- Perszyk, R.E.; DiRaddo, J.O.; Strong, K.L.; Low, C.M.; Ogden, K.K.; Khatri, A.; Vargish, G.A.; Pelkey, K.A.; Tricoire, L.; Liotta, D.C.; Smith, Y.; McBain, C.J.; Traynelis, S.F. , GluN2D-Containing N-methyl-d-Aspartate Receptors Mediate Synaptic Transmission in Hippocampal Interneurons and Regulate Interneuron Activity. Mol Pharmacol 2016, 90, 689–702. [Google Scholar] [CrossRef]
- Camp, C.R.; Yuan, H. , GRIN2D/GluN2D NMDA receptor: Unique features and its contribution to pediatric developmental and epileptic encephalopathy. Eur J Paediatr Neurol 2020, 24, 89–99. [Google Scholar] [CrossRef]
- Ritter, L.M.; Unis, A.S.; Meador-Woodruff, J.H. , Ontogeny of ionotropic glutamate receptor expression in human fetal brain. Developmental Brain Research 2001, 127, 123–133. [Google Scholar] [CrossRef]
- Scherzer, C.R.; Landwehrmeyer, G.B.; Kerner, J.A.; Counihan, T.J.; Kosinski, C.M.; Standaert, D.G.; Daggett, L.P.; Velicelebi, G.; Penney, J.B.; Young, A.B. , Expression of N-methyl-D-aspartate receptor subunit mRNAs in the human brain: hippocampus and cortex. J Comp Neurol 1998, 390, 75–90. [Google Scholar] [CrossRef]
- Akbarian, S.; Sucher, N.J.; Bradley, D.; Tafazzoli, A.; Trinh, D.; Hetrick, W.P.; Potkin, S.G.; Sandman, C.A.; Bunney, W.E., Jr.; Jones, E.G. , Selective alterations in gene expression for NMDA receptor subunits in prefrontal cortex of schizophrenics. J Neurosci 1996, 16, 19–30. [Google Scholar] [CrossRef]
- Dunah, A.W.; Luo, J.; Wang, Y.-H.; Yasuda, R.P.; Wolfe, B.B. , Subunit Composition ofN-Methyl-D-aspartate Receptors in the Central Nervous System that Contain the NR2D Subunit. Molecular Pharmacology 1998, 53, 429–437. [Google Scholar] [CrossRef]
- Brickley, S.G.; Misra, C.; Mok, M.S.; Mishina, M.; Cull-Candy, S.G. , NR2B and NR2D subunits coassemble in cerebellar Golgi cells to form a distinct NMDA receptor subtype restricted to extrasynaptic sites. Journal of Neuroscience 2003, 23, 4958–4966. [Google Scholar] [CrossRef]
- Jones, S.; Gibb, A.J. , Functional NR2B-and NR2D-containing NMDA receptor channels in rat substantia nigra dopaminergic neurones. The Journal of physiology 2005, 569, 209–221. [Google Scholar] [CrossRef]
- Erreger, K.; Geballe, M.T.; Kristensen, A.; Chen, P.E.; Hansen, K.B.; Lee, C.J.; Yuan, H.; Le, P.; Lyuboslavsky, P.N.; Micale, N. , Subunit-specific agonist activity at NR2A-, NR2B-, NR2C-, and NR2D-containing N-methyl-D-aspartate glutamate receptors. Molecular pharmacology 2007, 72, 907–920. [Google Scholar] [CrossRef]
- Chen, P.E.; Geballe, M.T.; Katz, E.; Erreger, K.; Livesey, M.R.; O'toole, K.K.; Le, P.; Lee, C.J.; Snyder, J.P.; Traynelis, S.F. , Modulation of glycine potency in rat recombinant NMDA receptors containing chimeric NR2A/2D subunits expressed in Xenopus laevis oocytes. The Journal of physiology 2008, 586, 227–245. [Google Scholar] [CrossRef]
- Kuner, T.; Schoepfer, R. , Multiple structural elements determine subunit specificity of Mg2+ block in NMDA receptor channels. Journal of Neuroscience 1996, 16, 3549–3558. [Google Scholar] [CrossRef]
- Clarke, R.J.; Johnson, J.W. , NMDA receptor NR2 subunit dependence of the slow component of magnesium unblock. J Neurosci 2006, 26, 5825–34. [Google Scholar] [CrossRef]
- Kotermanski, S.E.; Johnson, J.W. , Mg2+ imparts NMDA receptor subtype selectivity to the Alzheimer's drug memantine. Journal of Neuroscience 2009, 29, 2774–2779. [Google Scholar] [CrossRef]
- Sapkota, K.; Mao, Z.; Synowicki, P.; Lieber, D.; Liu, M.; Ikezu, T.; Gautam, V.; Monaghan, D.T. , GluN2D N-Methyl-d-Aspartate Receptor Subunit Contribution to the Stimulation of Brain Activity and Gamma Oscillations by Ketamine: Implications for Schizophrenia. J Pharmacol Exp Ther 2016, 356, 702–11. [Google Scholar] [CrossRef]
- Wyllie, D.J.; Behe, P.; Colquhoun, D. , Single-channel activations and concentration jumps: comparison of recombinant NR1a/NR2A and NR1a/NR2D NMDA receptors. J Physiol 1998, 510 Pt 1, 1–18. [Google Scholar] [CrossRef]
- Krupp, J.J.; Vissel, B.; Heinemann, S.F.; Westbrook, G.L. , Calcium-dependent inactivation of recombinant N-methyl-D-aspartate receptors is NR2 subunit specific. Molecular pharmacology 1996, 50, 1680–1688. [Google Scholar]
- Cull-Candy, S.; Brickley, S.; Farrant, M. , NMDA receptor subunits: diversity, development and disease. Current opinion in neurobiology 2001, 11, 327–335. [Google Scholar] [CrossRef]
- Hanson, E.; Armbruster, M.; Lau, L.A.; Sommer, M.E.; Klaft, Z.-J.; Swanger, S.A.; Traynelis, S.F.; Moss, S.J.; Noubary, F.; Chadchankar, J. , Tonic activation of GluN2C/GluN2D-containing NMDA receptors by ambient glutamate facilitates cortical interneuron maturation. Journal of Neuroscience 2019, 39, 3611–3626. [Google Scholar] [CrossRef]
- Swanger, S.A.; Vance, K.M.; Pare, J.-F.; Sotty, F.; Fog, K.; Smith, Y.; Traynelis, S.F. , NMDA receptors containing the GluN2D subunit control neuronal function in the subthalamic nucleus. Journal of Neuroscience 2015, 35, 15971–15983. [Google Scholar] [CrossRef]
- Pearlstein, E.; Gouty-Colomer, L.-A.; Michel, F.J.; Cloarec, R.; Hammond, C. , Glutamatergic synaptic currents of nigral dopaminergic neurons follow a postnatal developmental sequence. Frontiers in cellular neuroscience 2015, 9, 210. [Google Scholar] [CrossRef]
- Andrade-Talavera, Y.; Duque-Feria, P.; Paulsen, O.; Rodríguez-Moreno, A. , Presynaptic spike timing-dependent long-term depression in the mouse hippocampus. Cerebral Cortex 2016, 26, 3637–3654. [Google Scholar] [CrossRef]
- Feldman, D.E. , The spike-timing dependence of plasticity. Neuron 2012, 75, 556–571. [Google Scholar] [CrossRef]
- Dubois, C.J.; Lachamp, P.M.; Sun, L.; Mishina, M.; Liu, S.J. , Presynaptic GluN2D receptors detect glutamate spillover and regulate cerebellar GABA release. Journal of Neurophysiology 2016, 115, 271–285. [Google Scholar] [CrossRef]
- Watanabe, T.; Inoue, S.; Hiroi, H.; Orimo, A.; Muramatsu, M. , NMDA receptor type 2D gene as target for estrogen receptor in the brain. Molecular brain research 1999, 63, 375–379. [Google Scholar] [CrossRef]
- Riecher-Rössler, A.; Häfner, H.; Stumbaum, M.; Maurer, K.; Schmidt, R. , Can estradiol modulate schizophrenic symptomatology? Schizophrenia bulletin 1994, 20, 203–214. [Google Scholar] [CrossRef]
- McCarthny, C.R.; Du, X.; Wu, Y.C.; Hill, R.A. , Investigating the interactive effects of sex steroid hormones and brain-derived neurotrophic factor during adolescence on hippocampal NMDA receptor expression. International Journal of Endocrinology 2018, 2018. [Google Scholar] [CrossRef]
- Makino, C.; Shibata, H.; Ninomiya, H.; Tashiro, N.; Fukumaki, Y. , Identification of single-nucleotide polymorphisms in the human N-methyl-D-aspartate receptor subunit NR2D gene, GRIN2D, and association study with schizophrenia. Psychiatr Genet 2005, 15, 215–21. [Google Scholar] [CrossRef]
- Yu, Y.; Lin, Y.; Takasaki, Y.; Wang, C.; Kimura, H.; Xing, J.; Ishizuka, K.; Toyama, M.; Kushima, I.; Mori, D. , Rare loss of function mutations in N-methyl-D-aspartate glutamate receptors and their contributions to schizophrenia susceptibility. Translational psychiatry 2018, 8, 1–9. [Google Scholar] [CrossRef]
- Beneyto, M.; Meador-Woodruff, J.H. , Lamina-specific abnormalities of NMDA receptor-associated postsynaptic protein transcripts in the prefrontal cortex in schizophrenia and bipolar disorder. Neuropsychopharmacology 2008, 33, 2175–2186. [Google Scholar] [CrossRef]
- Sodhi, M.S.; Simmons, M.; McCullumsmith, R.; Haroutunian, V.; Meador-Woodruff, J.H. , Glutamatergic gene expression is specifically reduced in thalamocortical projecting relay neurons in schizophrenia. Biological psychiatry 2011, 70, 646–654. [Google Scholar] [CrossRef]
- Andreasen, N.C. , A unitary model of schizophrenia: Bleuler's fragmented phrene as schizencephaly. Archives of general psychiatry 1999, 56, 781–787. [Google Scholar] [CrossRef]
- Anticevic, A.; Cole, M.W.; Repovs, G.; Murray, J.D.; Brumbaugh, M.S.; Winkler, A.M.; Savic, A.; Krystal, J.H.; Pearlson, G.D.; Glahn, D.C. , Characterizing thalamo-cortical disturbances in schizophrenia and bipolar illness. Cerebral cortex 2014, 24, 3116–3130. [Google Scholar] [CrossRef]
- Chen, P.; Ye, E.; Jin, X.; Zhu, Y.; Wang, L. , Association between thalamocortical functional connectivity abnormalities and cognitive deficits in schizophrenia. Scientific reports 2019, 9, 2952. [Google Scholar] [CrossRef]
- Schmitt, A.; Koschel, J.; Zink, M.; Bauer, M.; Sommer, C.; Frank, J.; Treutlein, J.; Schulze, T.; Schneider-Axmann, T.; Parlapani, E. , Gene expression of NMDA receptor subunits in the cerebellum of elderly patients with schizophrenia. European archives of psychiatry and clinical neuroscience 2010, 260, 101–111. [Google Scholar] [CrossRef]
- Lewis, D.A.; Hashimoto, T.; Volk, D.W. , Cortical inhibitory neurons and schizophrenia. Nat Rev Neurosci 2005, 6, 312–24. [Google Scholar] [CrossRef]
- Gonzalez-Burgos, G.; Lewis, D.A. , NMDA receptor hypofunction, parvalbumin-positive neurons, and cortical gamma oscillations in schizophrenia. Schizophrenia bulletin 2012, 38, 950–957. [Google Scholar] [CrossRef]
- Sohal, V.S.; Zhang, F.; Yizhar, O.; Deisseroth, K. , Parvalbumin neurons and gamma rhythms enhance cortical circuit performance. Nature 2009, 459, 698–702. [Google Scholar] [CrossRef]
- Cobb, S.R.; Buhl, E.H.; Halasy, K.; Paulsen, O.; Somogyi, P. , Synchronization of neuronal activity in hippocampus by individual GABAergic interneurons. Nature 1995, 378, 75–8. [Google Scholar] [CrossRef]
- Uhlhaas, P.J.; Singer, W. , Abnormal neural oscillations and synchrony in schizophrenia. Nat Rev Neurosci 2010, 11, 100–13. [Google Scholar] [CrossRef]
- Cardin, J.A.; Carlén, M.; Meletis, K.; Knoblich, U.; Zhang, F.; Deisseroth, K.; Tsai, L.-H.; Moore, C.I. , Driving fast-spiking cells induces gamma rhythm and controls sensory responses. Nature 2009, 459, 663–667. [Google Scholar] [CrossRef]
- Buzsaki, G.; Wang, X.J. , Mechanisms of gamma oscillations. Annu Rev Neurosci 2012, 35, 203–25. [Google Scholar] [CrossRef] [PubMed]
- Alekseichuk, I.; Turi, Z.; de Lara, G.A.; Antal, A.; Paulus, W. , Spatial working memory in humans depends on theta and high gamma synchronization in the prefrontal cortex. Current Biology 2016, 26, 1513–1521. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-M. A.; Stanford, A.D.; Mao, X.; Abi-Dargham, A.; Shungu, D.C.; Lisanby, S.H.; Schroeder, C.E.; Kegeles, L.S. , GABA level, gamma oscillation, and working memory performance in schizophrenia. NeuroImage: Clinical 2014, 4, 531–539. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K.M.; Niznikiewicz, M.A.; Nestor, P.G.; Shenton, M.E.; McCarley, R.W. , Left auditory cortex gamma synchronization and auditory hallucination symptoms in schizophrenia. BMC neuroscience 2009, 10, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Spencer, K.M. , Baseline gamma power during auditory steady-state stimulation in schizophrenia. Frontiers in human neuroscience 2012, 5, 190. [Google Scholar] [CrossRef] [PubMed]
- Hunt, M.J.; Kasicki, S. , A systematic review of the effects of NMDA receptor antagonists on oscillatory activity recorded in vivo. Journal of Psychopharmacology 2013, 27, 972–986. [Google Scholar] [CrossRef]
- Kocsis, B.; Brown, R.E.; McCarley, R.W.; Hajos, M. , Impact of ketamine on neuronal network dynamics: Translational modeling of schizophrenia-relevant deficits. CNS neuroscience & therapeutics 2013, 19, 437–447. [Google Scholar]
- Hamm, J.P.; Gilmore, C.S.; Clementz, B.A. , Augmented gamma band auditory steady-state responses: support for NMDA hypofunction in schizophrenia. Schizophrenia research 2012, 138, 1–7. [Google Scholar] [CrossRef]
- Plourde, G.; Baribeau, J.; Bonhomme, V. , Ketamine increases the amplitude of the 40-Hz auditory steady-state response in humans. British journal of anaesthesia 1997, 78, 524–529. [Google Scholar] [CrossRef]
- Curley, A.A.; Lewis, D.A. , Cortical basket cell dysfunction in schizophrenia. The Journal of physiology 2012, 590, 715–724. [Google Scholar] [CrossRef]
- Lewis, D.A.; Curley, A.A.; Glausier, J.R.; Volk, D.W. , Cortical parvalbumin interneurons and cognitive dysfunction in schizophrenia. Trends Neurosci 2012, 35, 57–67. [Google Scholar] [CrossRef]
- Suzuki, Y.; Jodo, E.; Takeuchi, S.; Niwa, S.; Kayama, Y. , Acute administration of phencyclidine induces tonic activation of medial prefrontal cortex neurons in freely moving rats. Neuroscience 2002, 114, 769–779. [Google Scholar] [CrossRef]
- Jackson, M.E.; Homayoun, H.; Moghaddam, B. , NMDA receptor hypofunction produces concomitant firing rate potentiation and burst activity reduction in the prefrontal cortex. Proceedings of the National Academy of Sciences 2004, 101, 8467–8472. [Google Scholar] [CrossRef]
- Moghaddam, B.; Adams, B.; Verma, A.; Daly, D. , Activation of glutamatergic neurotransmission by ketamine: a novel step in the pathway from NMDA receptor blockade to dopaminergic and cognitive disruptions associated with the prefrontal cortex. Journal of Neuroscience 1997, 17, 2921–2927. [Google Scholar] [CrossRef]
- Lorrain, D.; Baccei, C.; Bristow, L.; Anderson, J.; Varney, M. , Effects of ketamine and N-methyl-D-aspartate on glutamate and dopamine release in the rat prefrontal cortex: modulation by a group II selective metabotropic glutamate receptor agonist LY379268. Neuroscience 2003, 117, 697–706. [Google Scholar] [CrossRef]
- Vollenweider, F.; Leenders, K.; Scharfetter, C.; Antonini, A.; Maguire, P.; Missimer, J.; Angst, J. , Metabolic hyperfrontality and psychopathology in the ketamine model of psychosis using positron emission tomography (PET) and [18F] fluorodeoxyglucose (FDG). European neuropsychopharmacology 1997, 7, 9–24. [Google Scholar] [CrossRef]
- Breier, A.; Malhotra, A.K.; Pinals, D.A.; Weisenfeld, N.I.; Pickar, D. , Association of ketamine-induced psychosis with focal activation of the prefrontal cortex in healthy volunteers. The American journal of psychiatry 1997. [Google Scholar]
- Miyamoto, S.; Leipzig, J.N.; Lieberman, J.A.; Duncan, G.E. , Effects of ketamine, MK-801, and amphetamine on regional brain 2-deoxyglucose uptake in freely moving mice. Neuropsychopharmacology 2000, 22, 400–412. [Google Scholar] [CrossRef]
- Duncan, G.E.; Moy, S.S.; Knapp, D.J.; Mueller, R.A.; Breese, G.R. , Metabolic mapping of the rat brain after subanesthetic doses of ketamine: potential relevance to schizophrenia. Brain research 1998, 787, 181–190. [Google Scholar] [CrossRef]
- Grunze, H.C.; Rainnie, D.G.; Hasselmo, M.E.; Barkai, E.; Hearn, E.F.; McCarley, R.W.; Greene, R.W. , NMDA-dependent modulation of CA1 local circuit inhibition. Journal of Neuroscience 1996, 16, 2034–2043. [Google Scholar] [CrossRef] [PubMed]
- Kinney, J.W.; Davis, C.N.; Tabarean, I.; Conti, B.; Bartfai, T.; Behrens, M.M. , A specific role for NR2A-containing NMDA receptors in the maintenance of parvalbumin and GAD67 immunoreactivity in cultured interneurons. Journal of Neuroscience 2006, 26, 1604–1615. [Google Scholar] [CrossRef]
- Behrens, M.M.; Ali, S.S.; Dao, D.N.; Lucero, J.; Shekhtman, G.; Quick, K.L.; Dugan, L.L. , Ketamine-induced loss of phenotype of fast-spiking interneurons is mediated by NADPH-oxidase. Science 2007, 318, 1645–1647. [Google Scholar] [CrossRef]
- Keilhoff, G.; Becker, A.; Grecksch, G.; Wolf, G.; Bernstein, H.-G. , Repeated application of ketamine to rats induces changes in the hippocampal expression of parvalbumin, neuronal nitric oxide synthase and cFOS similar to those found in human schizophrenia. Neuroscience 2004, 126, 591–598. [Google Scholar] [CrossRef]
- Morrow, B.A.; Elsworth, J.D.; Roth, R.H. , Repeated phencyclidine in monkeys results in loss of parvalbumin-containing axo-axonic projections in the prefrontal cortex. Psychopharmacology 2007, 192, 283–290. [Google Scholar] [CrossRef]
- Belforte, J.E.; Zsiros, V.; Sklar, E.R.; Jiang, Z.; Yu, G.; Li, Y.; Quinlan, E.M.; Nakazawa, K. , Postnatal NMDA receptor ablation in corticolimbic interneurons confers schizophrenia-like phenotypes. Nature neuroscience 2010, 13, 76–83. [Google Scholar] [CrossRef]
- Cho, K.K.; Hoch, R.; Lee, A.T.; Patel, T.; Rubenstein, J.L.; Sohal, V.S. , Gamma rhythms link prefrontal interneuron dysfunction with cognitive inflexibility in Dlx5/6+/− mice. Neuron 2015, 85, 1332–1343. [Google Scholar] [CrossRef]
- Ikeda, K.; Araki, K.; Takayama, C.; Inoue, Y.; Yagi, T.; Aizawa, S.; Mishina, M. , Reduced spontaneous activity of mice defective in the ε4 subunit of the NMDA receptor channel. Molecular brain research 1995, 33, 61–71. [Google Scholar] [CrossRef]
- Miyamoto, Y.; Yamada, K.; Noda, Y.; Mori, H.; Mishina, M.; Nabeshima, T. , Lower sensitivity to stress and altered monoaminergic neuronal function in mice lacking the NMDA receptor ε4 subunit. Journal of Neuroscience 2002, 22, 2335–2342. [Google Scholar] [CrossRef]
- Obiang, P.; Macrez, R.; Jullienne, A.; Bertrand, T.; Lesept, F.; Ali, C.; Maubert, E.; Vivien, D.; Agin, V. , GluN2D subunit-containing NMDA receptors control tissue plasminogen activator-mediated spatial memory. Journal of Neuroscience 2012, 32, 12726–12734. [Google Scholar] [CrossRef] [PubMed]
- Ide, S.; Ikekubo, Y.; Mishina, M.; Hashimoto, K.; Ikeda, K. , Cognitive impairment that is induced by (R)-ketamine is abolished in NMDA GluN2D receptor subunit knockout mice. International Journal of Neuropsychopharmacology 2019, 22, 449–452. [Google Scholar] [CrossRef] [PubMed]
- Hagino, Y.; Kasai, S.; Han, W.; Yamamoto, H.; Nabeshima, T.; Mishina, M.; Ikeda, K. , Essential role of NMDA receptor channel ε4 subunit (GluN2D) in the effects of phencyclidine, but not methamphetamine. PloS one 2010, 5, e13722. [Google Scholar] [CrossRef]
- Takeuchi, T.; Kiyama, Y.; Nakamura, K.; Tsujita, M.; Matsuda, I.; Mori, H.; Munemoto, Y.; Kuriyama, H.; Natsume, R.; Sakimura, K. , Roles of the glutamate receptor ε2 and δ2 subunits in the potentiation and prepulse inhibition of the acoustic startle reflex. European Journal of Neuroscience 2001, 14, 153–160. [Google Scholar] [CrossRef]
- Yamamoto, H.; Kamegaya, E.; Sawada, W.; Hasegawa, R.; Yamamoto, T.; Hagino, Y.; Takamatsu, Y.; Imai, K.; Koga, H.; Mishina, M. , Involvement of the N-methyl-D-aspartate receptor GluN2D subunit in phencyclidine-induced motor impairment, gene expression, and increased Fos immunoreactivity. Molecular brain 2013, 6, 1–16. [Google Scholar] [CrossRef]
- Yamamoto, T.; Nakayama, T.; Yamaguchi, J.; Matsuzawa, M.; Mishina, M.; Ikeda, K.; Yamamoto, H. , Role of the NMDA receptor GluN2D subunit in the expression of ketamine-induced behavioral sensitization and region-specific activation of neuronal nitric oxide synthase. Neurosci Lett 2016, 610, 48–53. [Google Scholar] [CrossRef]
- Duncan, G.E.; Miyamoto, S.; Leipzig, J.N.; Lieberman, J.A. , Comparison of brain metabolic activity patterns induced by ketamine, MK-801 and amphetamine in rats: support for NMDA receptor involvement in responses to subanesthetic dose of ketamine. Brain research 1999, 843, 171–183. [Google Scholar] [CrossRef]
- Hrabetova, S.; Serrano, P.; Blace, N.; Heong, W.T.; Skifter, D.A.; Jane, D.E.; Monaghan, D.T.; Sacktor, T.C. , Distinct NMDA receptor subpopulations contribute to long-term potentiation and long-term depression induction. The Journal of Neuroscience 2000, 20, RC81. [Google Scholar] [CrossRef]
- Lozovaya, N.A.; Grebenyuk, S.E.; Tsintsadze, T.S.; Feng, B.; Monaghan, D.T.; Krishtal, O.A. , Extrasynaptic NR2B and NR2D subunits of NMDA receptors shape ‘superslow’afterburst EPSC in rat hippocampus. The Journal of physiology 2004, 558, 451–463. [Google Scholar] [CrossRef] [PubMed]
- Eapen, A.V.; Fernández-Fernández, D.; Georgiou, J.; Bortolotto, Z.A.; Lightman, S.; Jane, D.E.; Volianskis, A.; Collingridge, G.L. , Multiple roles of GluN2D-containing NMDA receptors in short-term potentiation and long-term potentiation in mouse hippocampal slices. Neuropharmacology 2021, 201, 108833. [Google Scholar] [CrossRef] [PubMed]
- Ingram, R.; Kang, H.; Lightman, S.; Jane, D.E.; Bortolotto, Z.A.; Collingridge, G.L.; Lodge, D.; Volianskis, A. , Some distorted thoughts about ketamine as a psychedelic and a novel hypothesis based on NMDA receptor-mediated synaptic plasticity. Neuropharmacology 2018, 142, 30–40. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




