Introduction
Up to 90% of patients undergoing surgery will present hypothermia in the perioperative period.1 The Standards and Practice Parameters Committee of the ASA established in October 1986 the recommendation to monitor body temperature in any patient undergoing anesthesia.2 Postoperative hypothermia is defined as a decrease in body temperature below 35°C in the first 24 hours after surgery.3
Anesthesia and the surgical procedure affect the thermoregulatory center, thereby contributing to adverse events during the perioperative period.4 The decrease in temperature affects processes going from drug metabolism to the healing process and immunoprotection during perioperative hypothermia, which increases morbidity and complications that may result in cardiovascular events, altered platelet activity, or postoperative infections.5
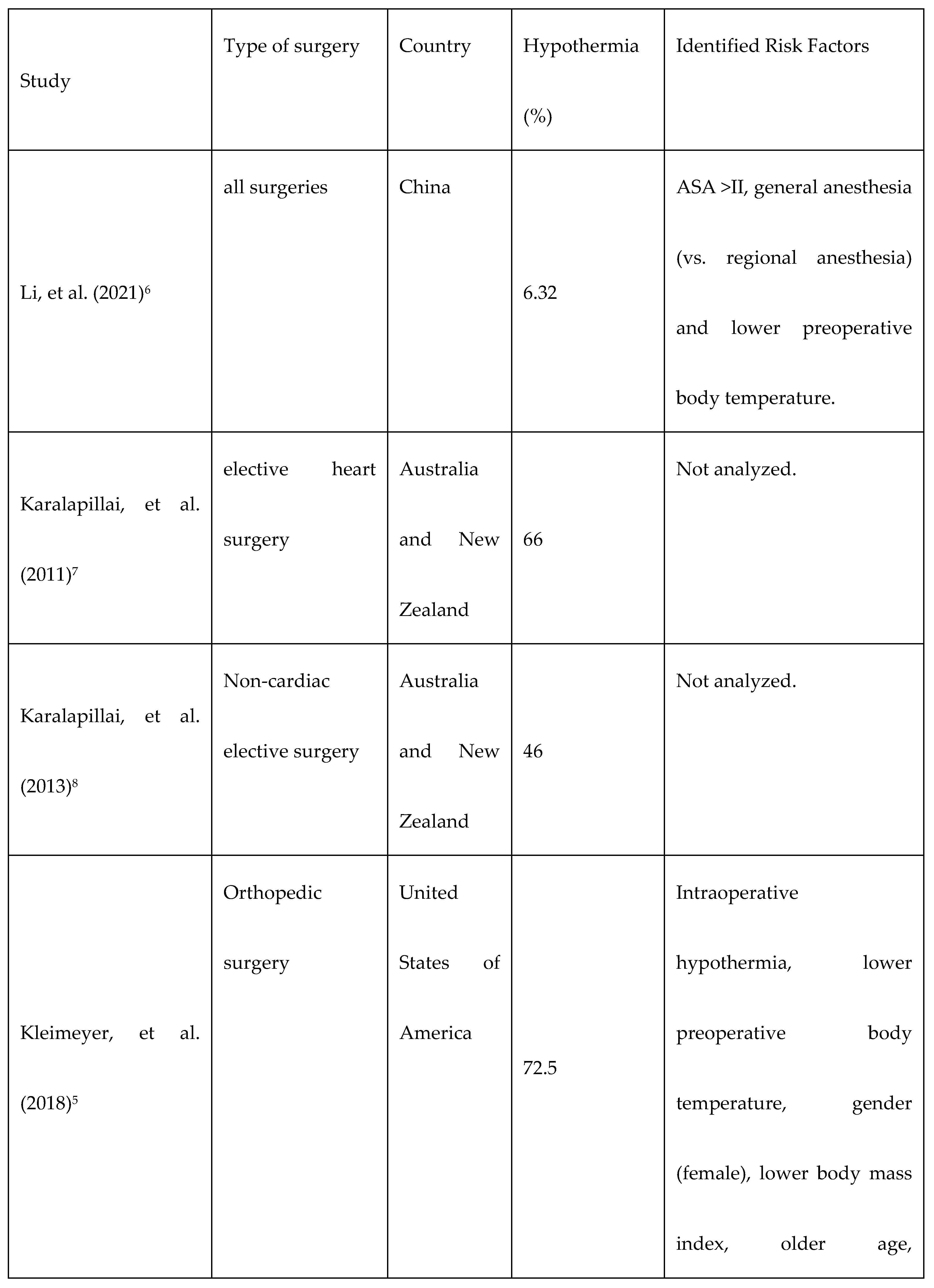
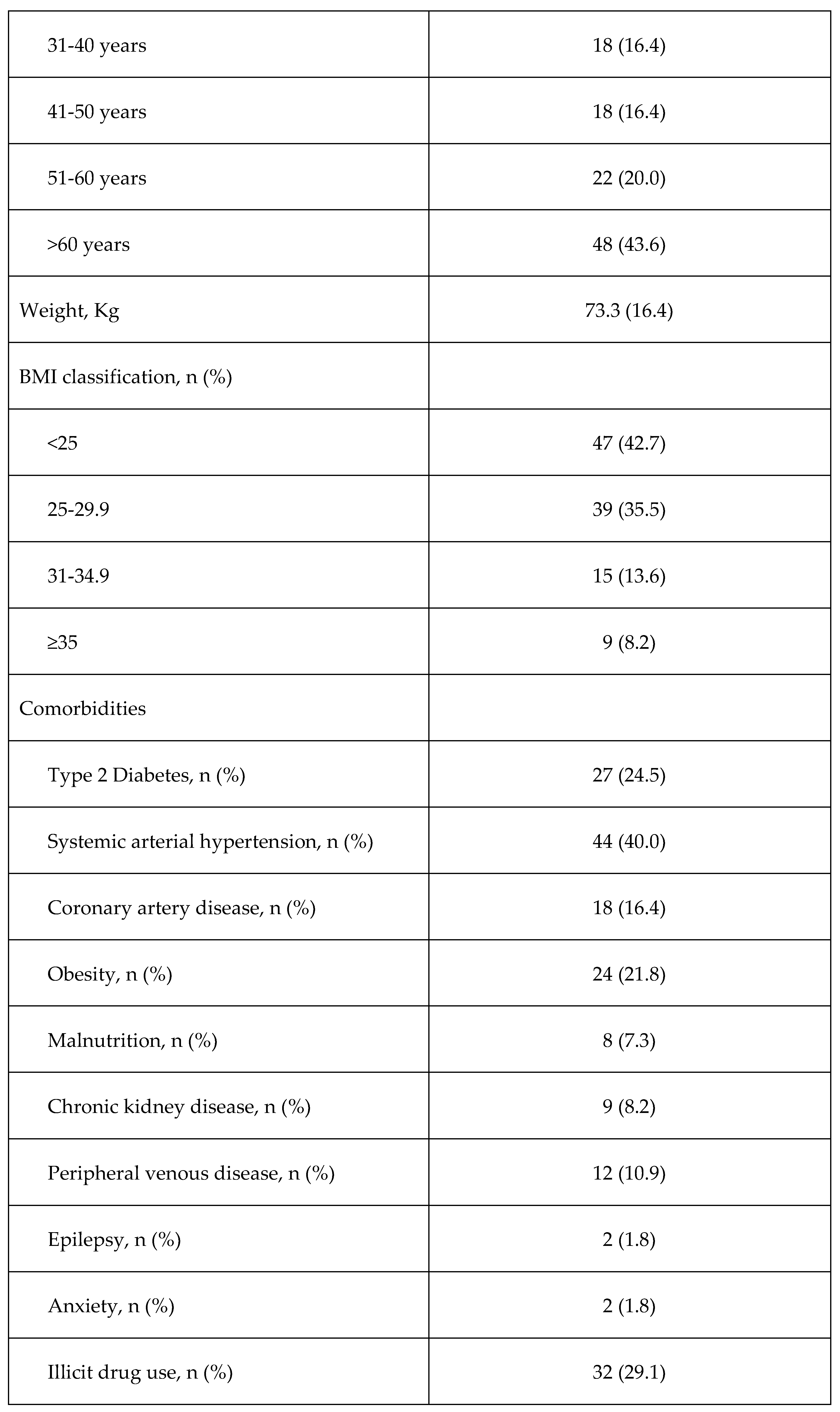
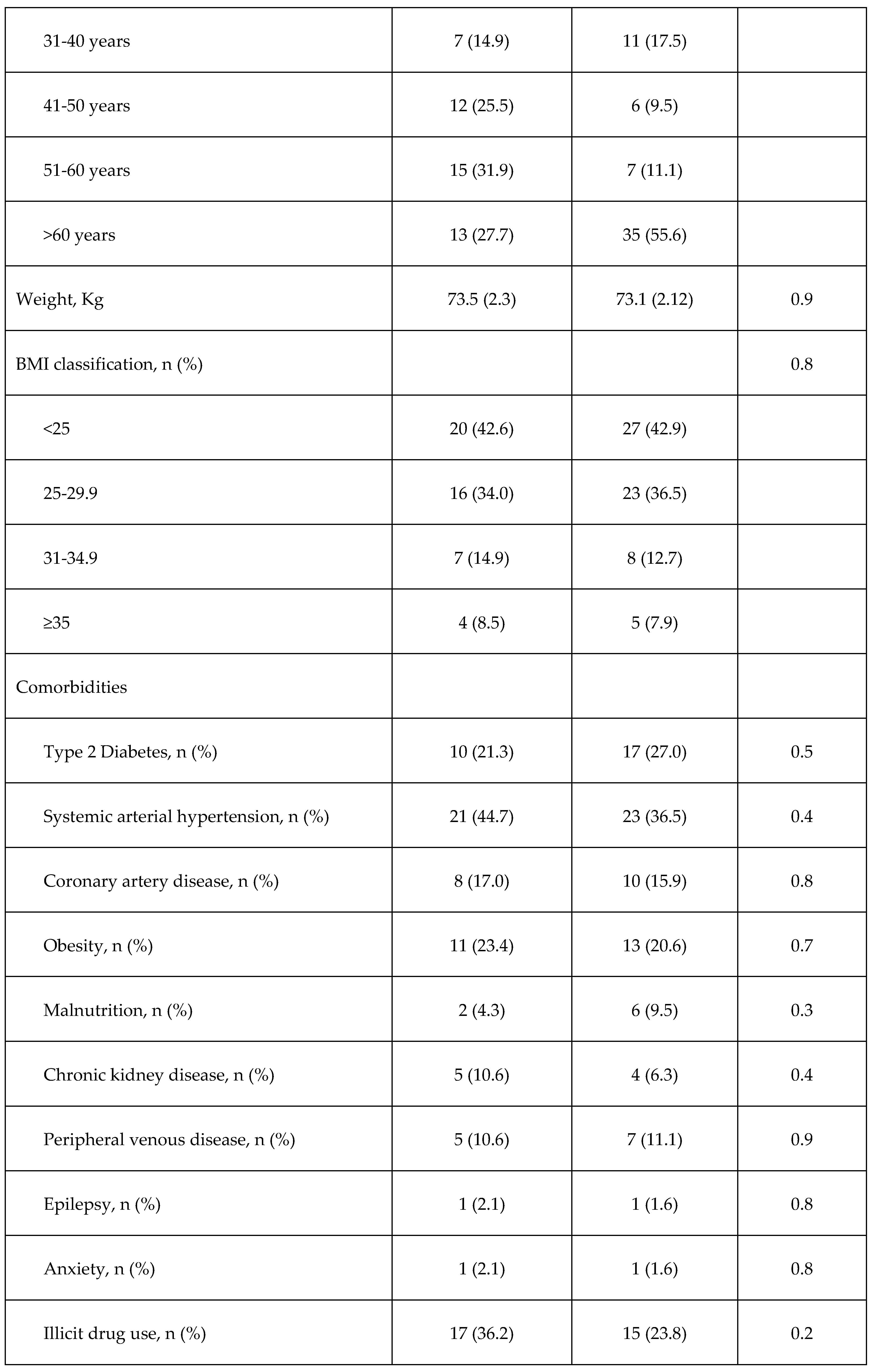
As shown in
Table 1, the occurrence of hypothermia can vary widely depending on the type of patients included in the study.
5-12 Its occurrence has been associated with factors such as sex, type of surgery, duration and age.
13 Likewise, no study has reported the occurrence of postoperative hypothermia and variables associated with its occurrence only in patients undergoing major abdominal surgery who may have different risk factors and frequency of occurrence of postoperative hypothermia than patients undergoing other types of surgery.
Considering the complications that can derive from hypothermia, determining the factors that can contribute to its development may lead to prevention strategies that ultimately increase patient safety. Therefore, the aim of this study was to describe the proportion of patients undergoing major abdominal surgery who develop postoperative hypothermia, as well as the variables associated with its occurrence in a tertiary care hospital.
Material and methods
Study design
A prospective cohort study was conducted in patients undergoing major abdominal surgery between November 2021 and March 2022 in a tertiary care referral center in Mexico City. The inclusion criteria were patients with an age over 18 years who underwent scheduled or emergency major abdominal surgery lasting more than 2 hours. Patients with neuromuscular diseases, pregnant women, patients with prolonged advanced life support, as well as those who did not give their consent to participate in the study were not included. Patients who withdrew their consent at any time during the study were eliminated. The study was approved by the ethics and research committee of Centro Médico Nacional 20 de Noviembre, ISSSTE (approval number 459.2021) and all patients signed a written informed consent form to participate in the study.
Data Collection
During the pre-anesthetic evaluation, patients who met the inclusion criteria were invited to participate in the study. After consenting to participate in the study, their baseline characteristics, surgical procedure data, and post-procedural data were collected. Clinical variables collected were sex, age, weight (in kilograms), body mass index (BMI), body temperature (°C), the American Society of Anesthesiologists physical status (ASA-PS) classification (see below), and comorbidities (type 2 diabetes, hypertension, obesity, malnutrition, coronary artery disease, chronic kidney disease, peripheral venous disease, epilepsy, anxiety, illicit drug use, and current smoking). Data related to the surgical procedure were: type of surgery (urgent or elective), organ involved (kidney or urinary tract, liver and bile ducts or gallbladder, esophagus or stomach, small bowel, large bowel, exploratory laparotomy, or gynecological), duration of surgery (minutes from primary incision to wound closure), anesthetic technique (balanced general or combined [balanced general + neuraxial]), duration of anesthesia (minutes from drug induction until the patient woke up), and room temperature during surgery.
Body temperature was measured using an electronic axillary skin thermometer and was reported in degrees Celsius (°C) during the pre-anesthetic evaluation (preoperative), during surgery (intraoperative) and after surgery (postoperative). Patients were classified as hypothermic when they presented a body temperature lower than or equal to 35°C.14 Postoperative pain and postoperative hypoxemia were also recorded. Hypoxemia was classified according to room-air peripheral arterial oxygen saturation (SpO2), as mild (SpO2 = 86-90%), moderate (SpO2 = 81-85%), severe (SpO2 = 76-80%), or extreme (SpO2 <70%) hypoxemia. The presence of pain was determined with the visual analog pain scale.
Patients were classified in stages 1 to 5 according to the 2020 ASA-PS classification15 during the pre-anesthetic evaluation, considering ASA-PS 1 as normal healthy patient; ASA-PS 2, mild systemic disease; ASA-PS 3, severe systemic disease that is not life-threatening; ASA-PS 4, severe systemic disease that is a constant threat to life; and ASA-PS 5, moribund patient who is not expected to survive without the surgery.
The clinical evaluation of the patient was based on the diagnosis of malnutrition, detection of postoperative hypoxemia and pain during the stay in the post-anesthesia care unit (PACU). Patients with a BMI less than 18.5 were classified as having severe malnutrition according to the GLIM criteria for the diagnosis of malnutrition.10
Outcome
The main outcome was the presence of postoperative hypothermia, defined as a body temperature below 35°C during PACU stay after surgery.14
Sample size
Considering that the presence of variables under study could double the risk of hypothermia, the calculation was done considering a 0.5 probability of the presence of each variable in the study sample, with statistical power of 80% (1-β = 0.80) and a type 1 error probability of 5% (α=0.05). The sample size obtained was 136 subjects. The following formula for estimating an odds ratio was applied:
where Zα=1.96, Zβ=1.28, P1=0.5 (proportion of patients with the risk factor), P: weighted mean of P1 and P2. P2 was calculated according to the following formula:
Considering P1=0.5 and OR=2.0 (expected odds ratio due to any study factor).
Statistical analysis
Descriptive data are presented as mean with standard deviation for quantitative variables, and as frequency and percentage for qualitative variables. Comparisons between patients who presented hypothermia and normal temperature during PACU stay were made using the Student’s t-test for quantitative data and the Chi-square test or Fisher's exact test for qualitative data.
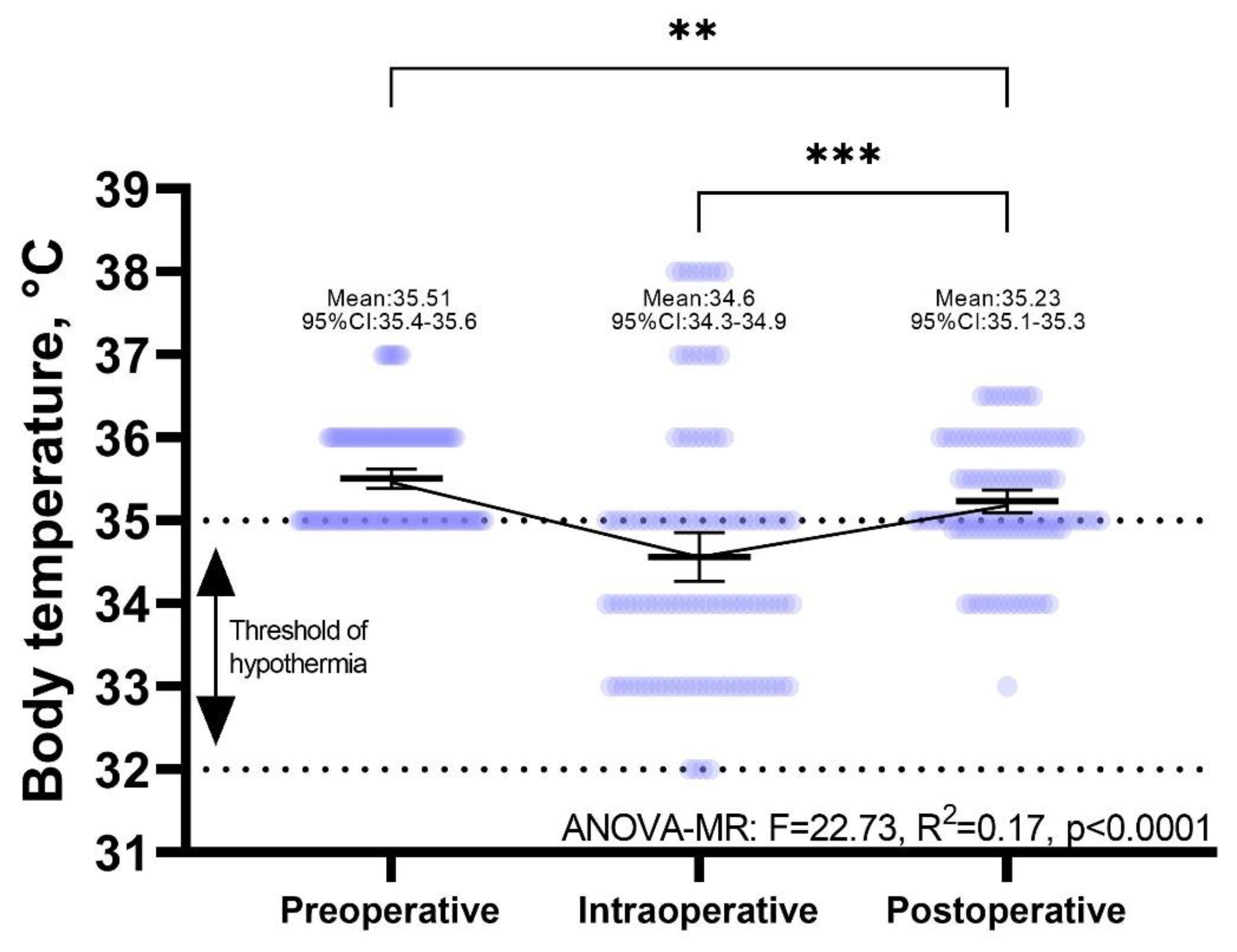
A repeated measures ANOVA (RM-ANOVA) model was performed to compare preoperative, intraoperative, and postoperative temperatures. The model is summarized in a scatter plot showing the mean and 95% confidence intervals (95% CI). Pairwise comparisons were performed using the Bonferroni post-hoc test.
The evaluation of potential variables associated with hypothermia was carried out by means of logistic regression analysis to determine the effect of each variable on the development of postoperative hypothermia. The variables were included in each univariate model by the Enter method. Variables associated with postoperative hypothermia were included in a multivariable model adjusted by sex, age, and duration of surgery. The results are summarized by means of the regression coefficient, Odds Ratio (OR) and 95% CI.
The quantitative variables (weight, age, preoperative temperature, intraoperative temperature, room temperature, surgery time, and anesthetic time) were included in linear regression models to determine the decrease or increase for every °C for every increase of one unit in the independent variable. The results of the models are summarized in regression coefficients, standard error, and 95%CI.
The assumptions of each statistical model were verified by residual analysis. A value of p<0.05 was considered as statistically significant. All analyses were performed using SPSS v.21 Software. The RM-ANOVA graph was built with GraphPad Prism v. 9.0.3.
Results
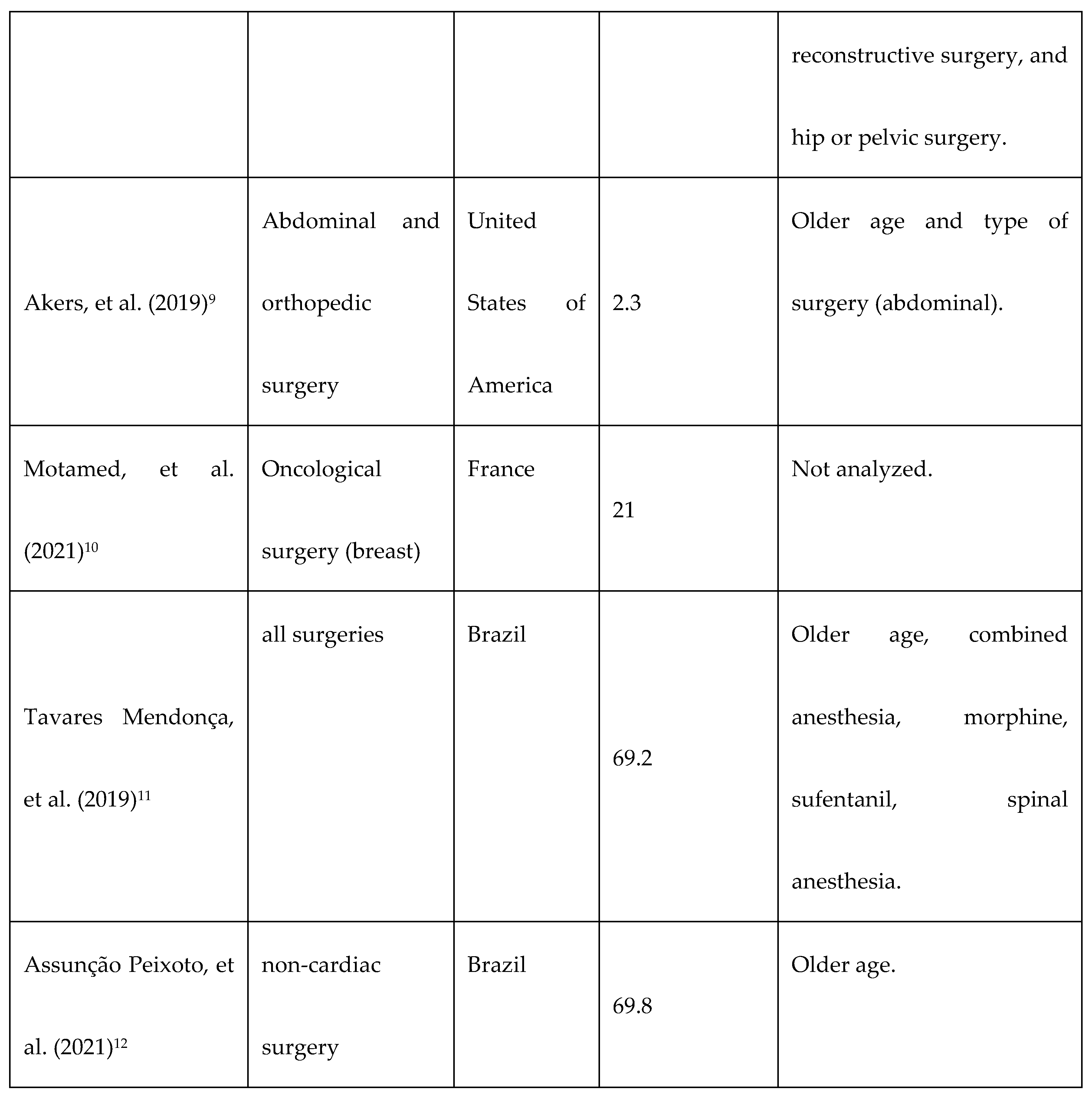
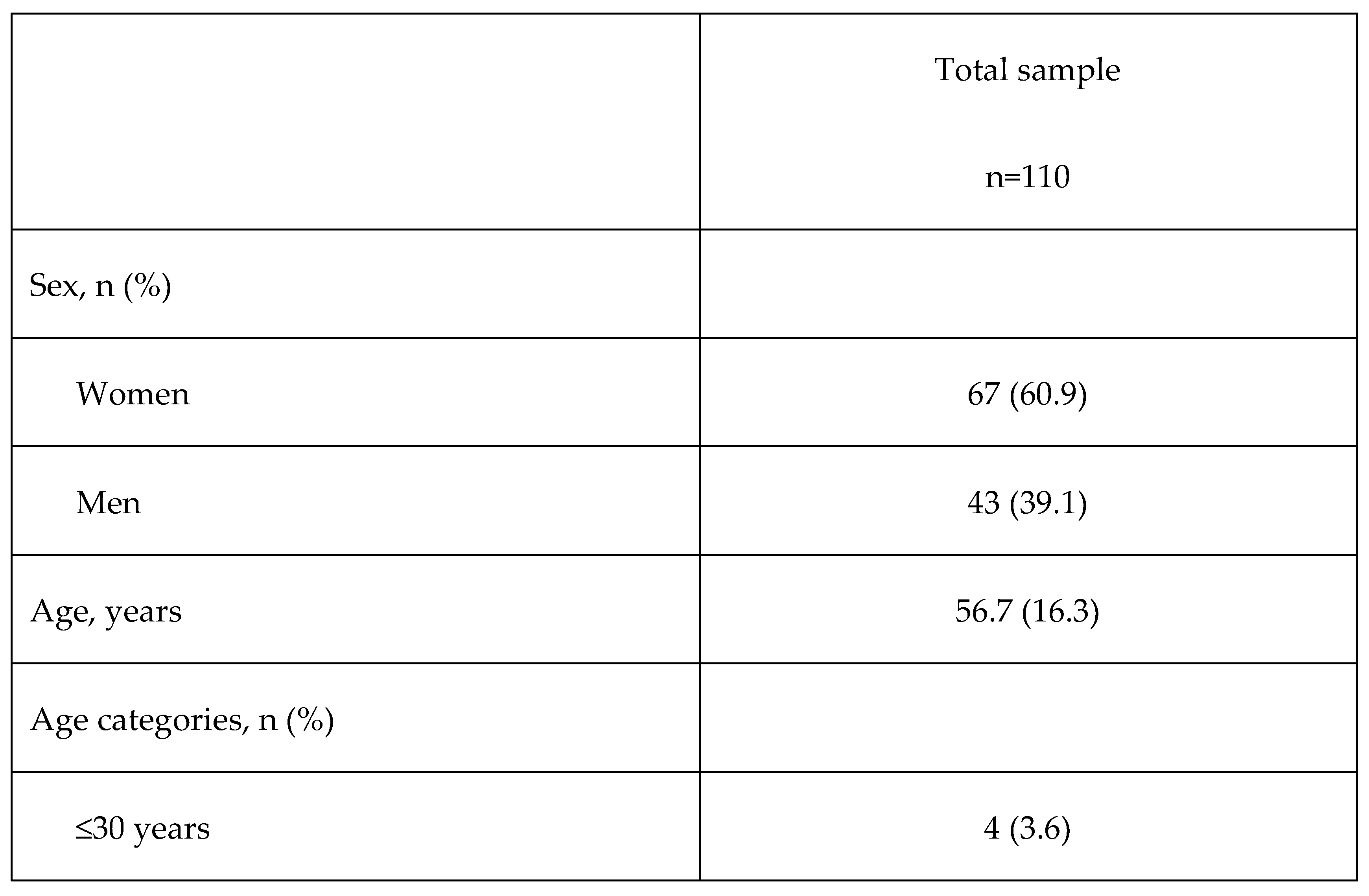
A total of 110 patients were included in the analysis. Of them, 61% (n=67) were women. The mean age was 56.7 years (SD: 16.3, range: 75), with the most frequent age range being adults over 60 years (43.6%). The most frequent comorbidities were smoking (59.1%), arterial hypertension (40.0%), and type 2 diabetes (24.5%).
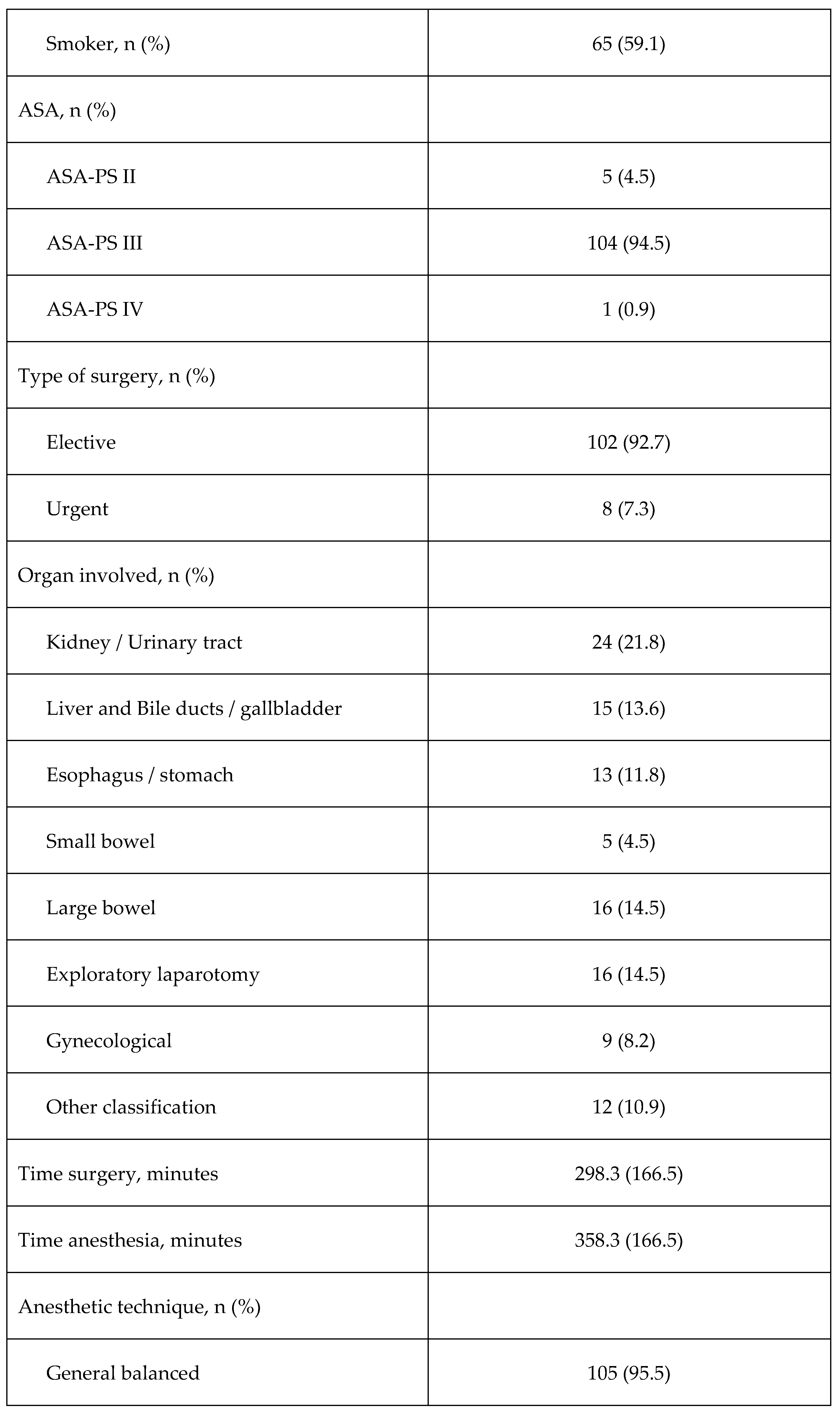
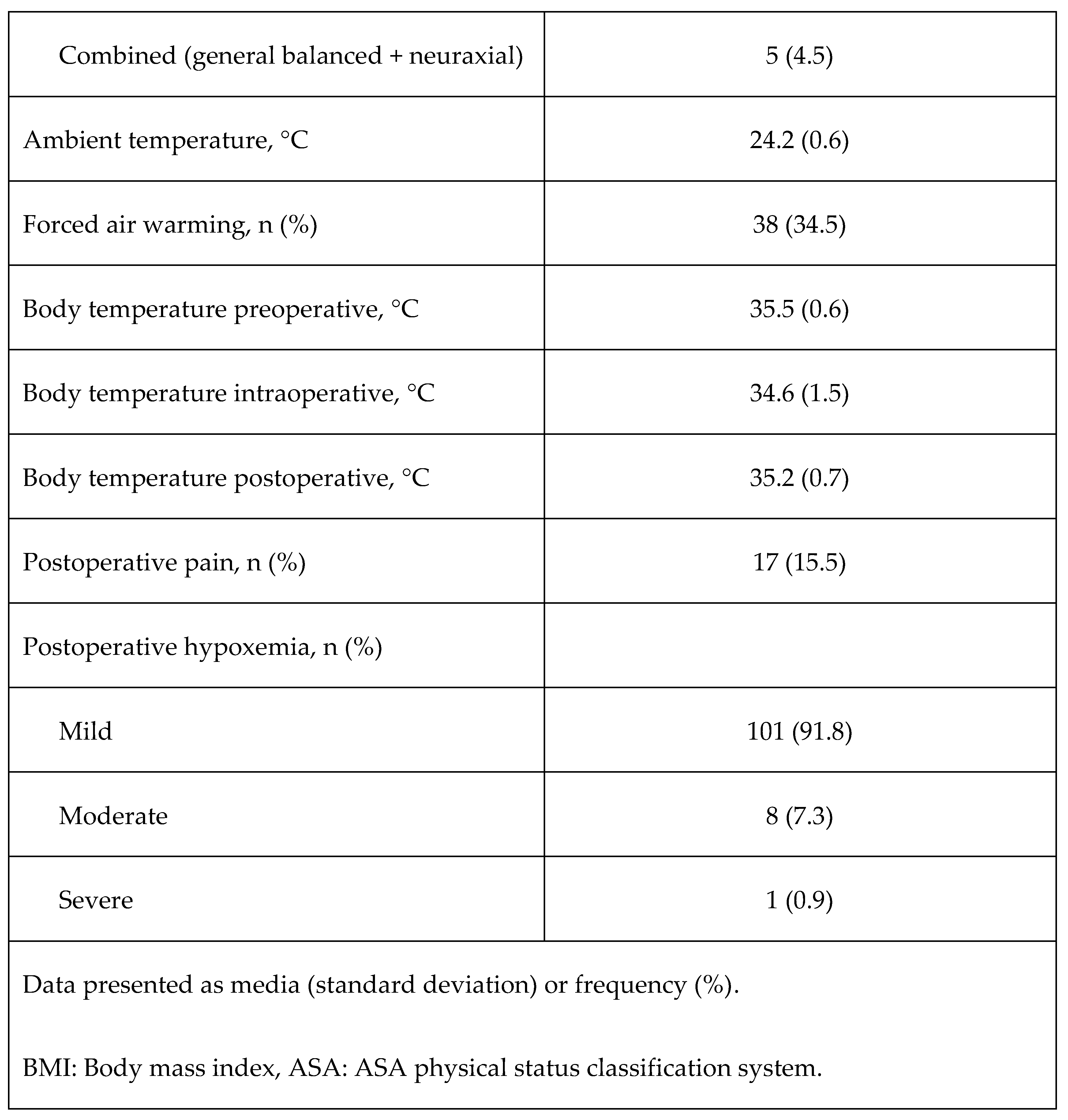
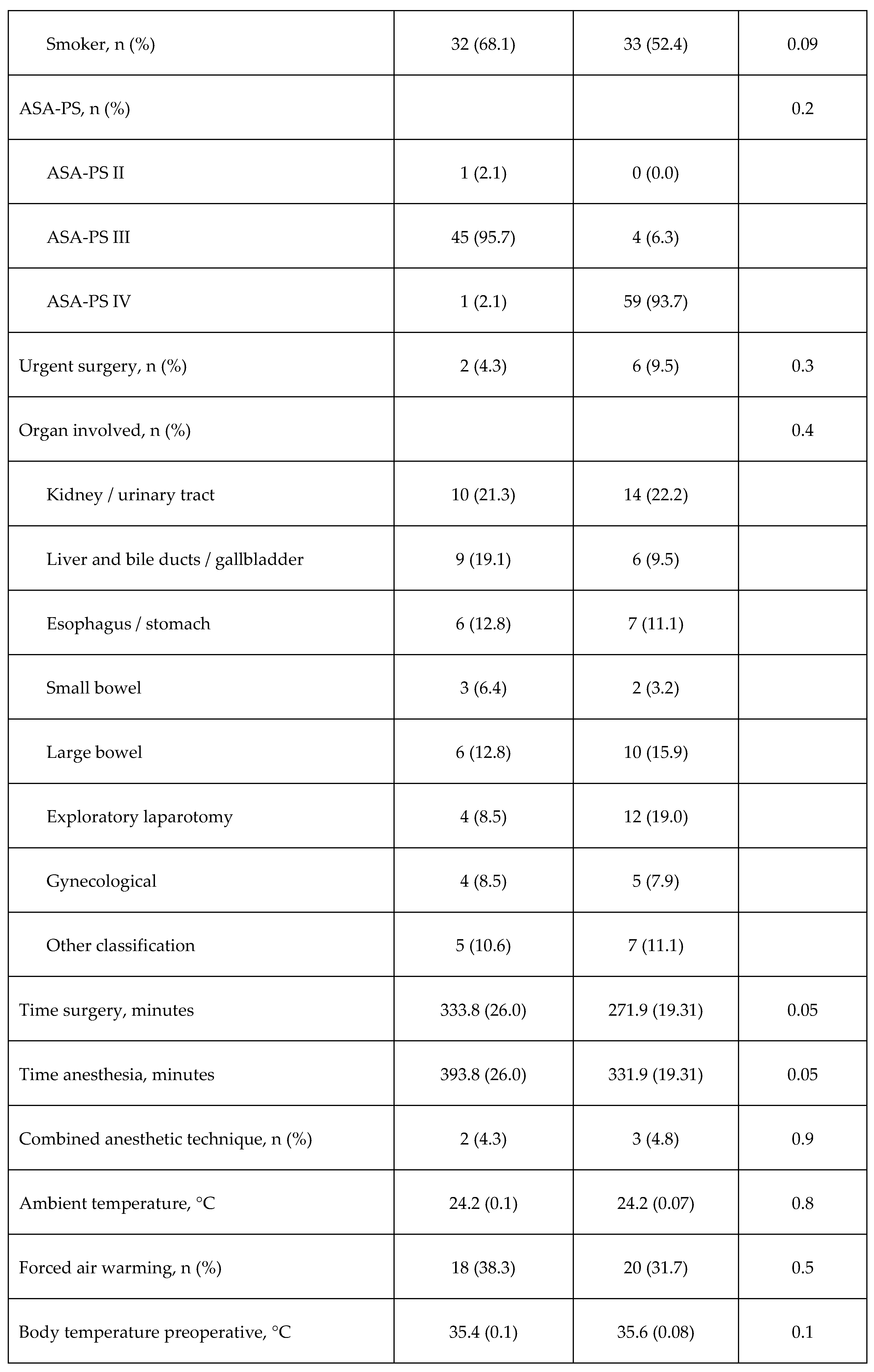
Table 2 shows the characteristics of patients. The most frequently involved organ on which surgery was performed was Kidney or urinary tract (21.8%), followed by large bowel (14.5%) and exploratory laparotomy (14.5%). The average duration of the surgeries was longer than 4 hours (mean: 298 minutes, SD: 166.5, range: 480). Most surgeries were elective (92.75%) with general balanced anesthetic techniques (95.5%) and most patients were in the ASA-PS III category (94.5%). Of the total number of patients in this category (n=104), 58.2% were women and 36.4% men. During recovery in the PACU, all patients presented some degree of hypoxemia, the majority (91.8%) being mild cases.
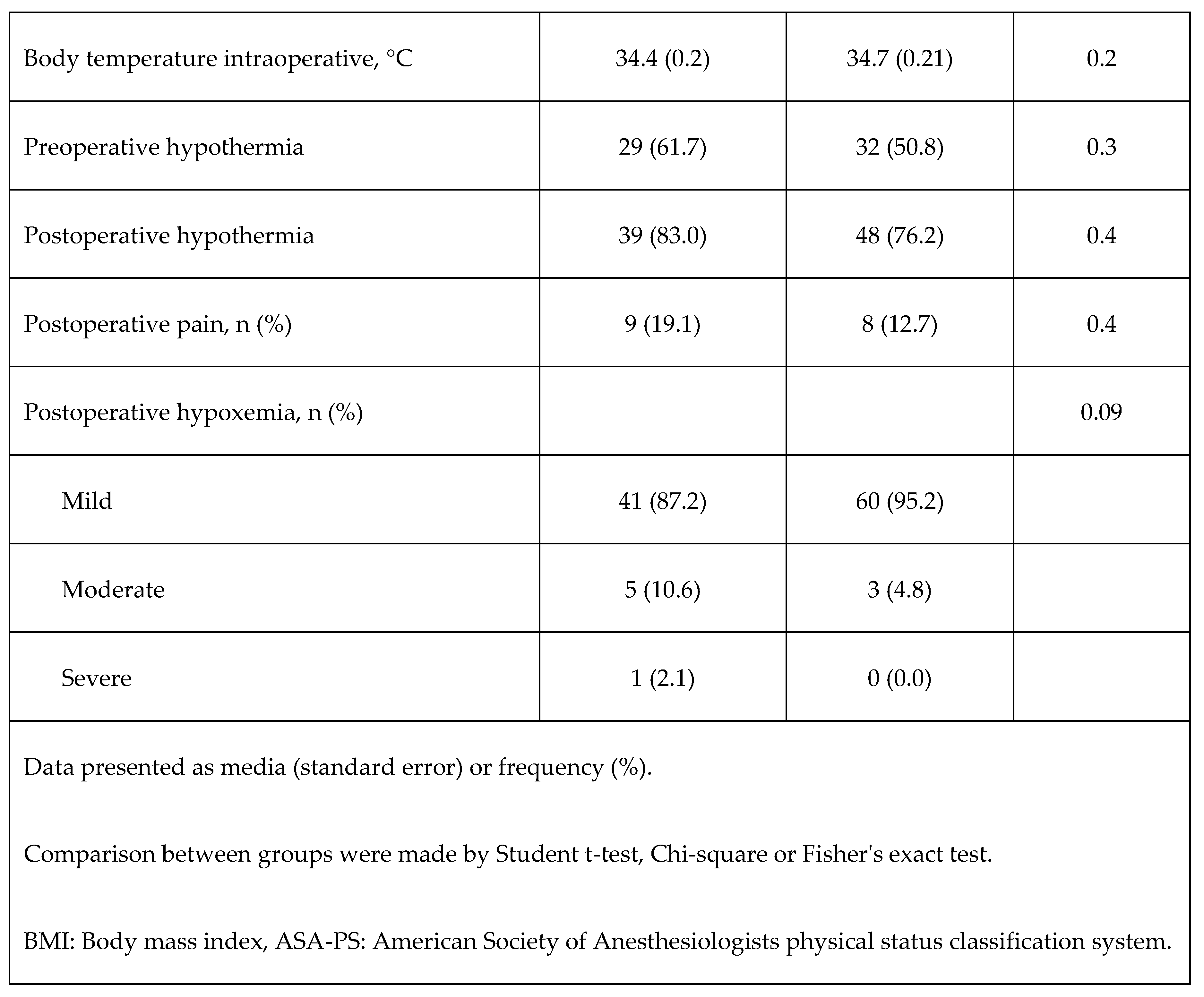
Hypothermia occurred in 61 patients (55.5%) prior to surgery (preoperative), while 87 (79.1%) presented intraoperative hypothermia, and 63 (57.3%) had postoperative hypothermia during PACU stay.
Figure 1 shows the distribution of body temperature before, during and after surgery. Body temperature after surgery was lower than the temperature before surgery (p=0.009), but the temperature during surgery was lower than that observed after surgery (p=0.0002).
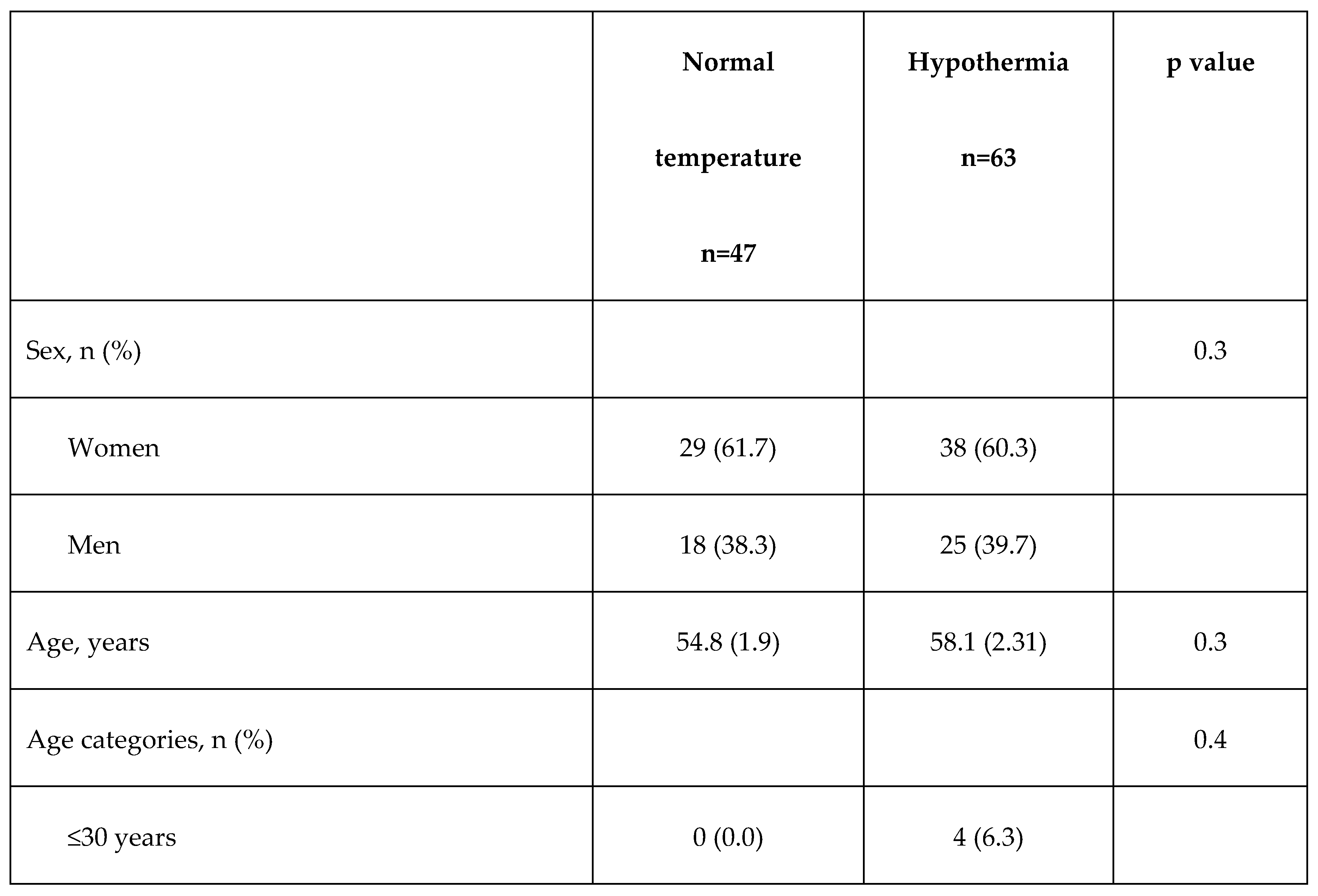
Table 3 shows the comparisons of the main clinical and surgical characteristics and comorbidities according to the occurrence of postoperative hypothermia or not during PACU stay. No significant differences were observed between the various characteristics, except for age categories where there was a higher frequency of subjects older than 60 years.
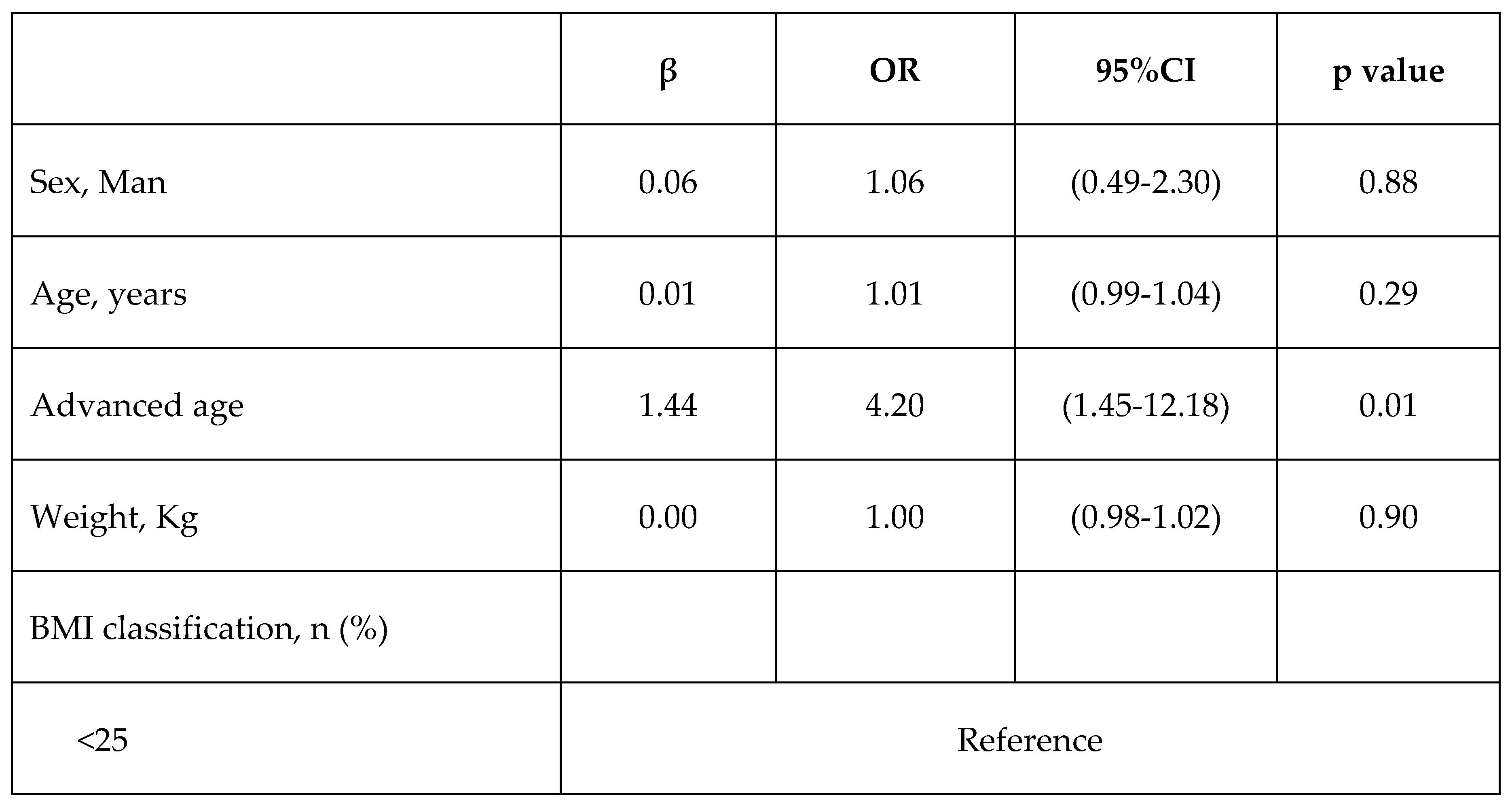
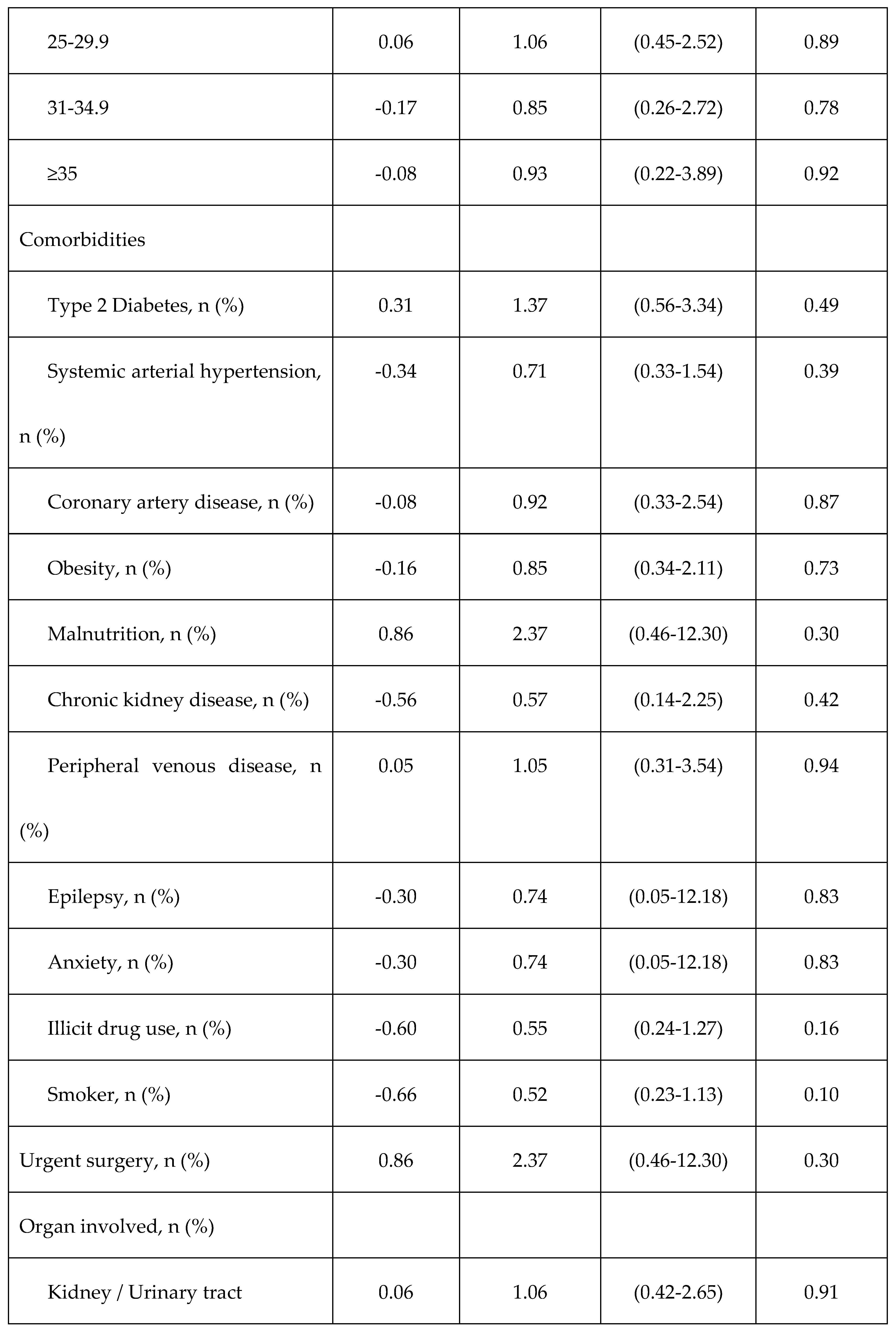
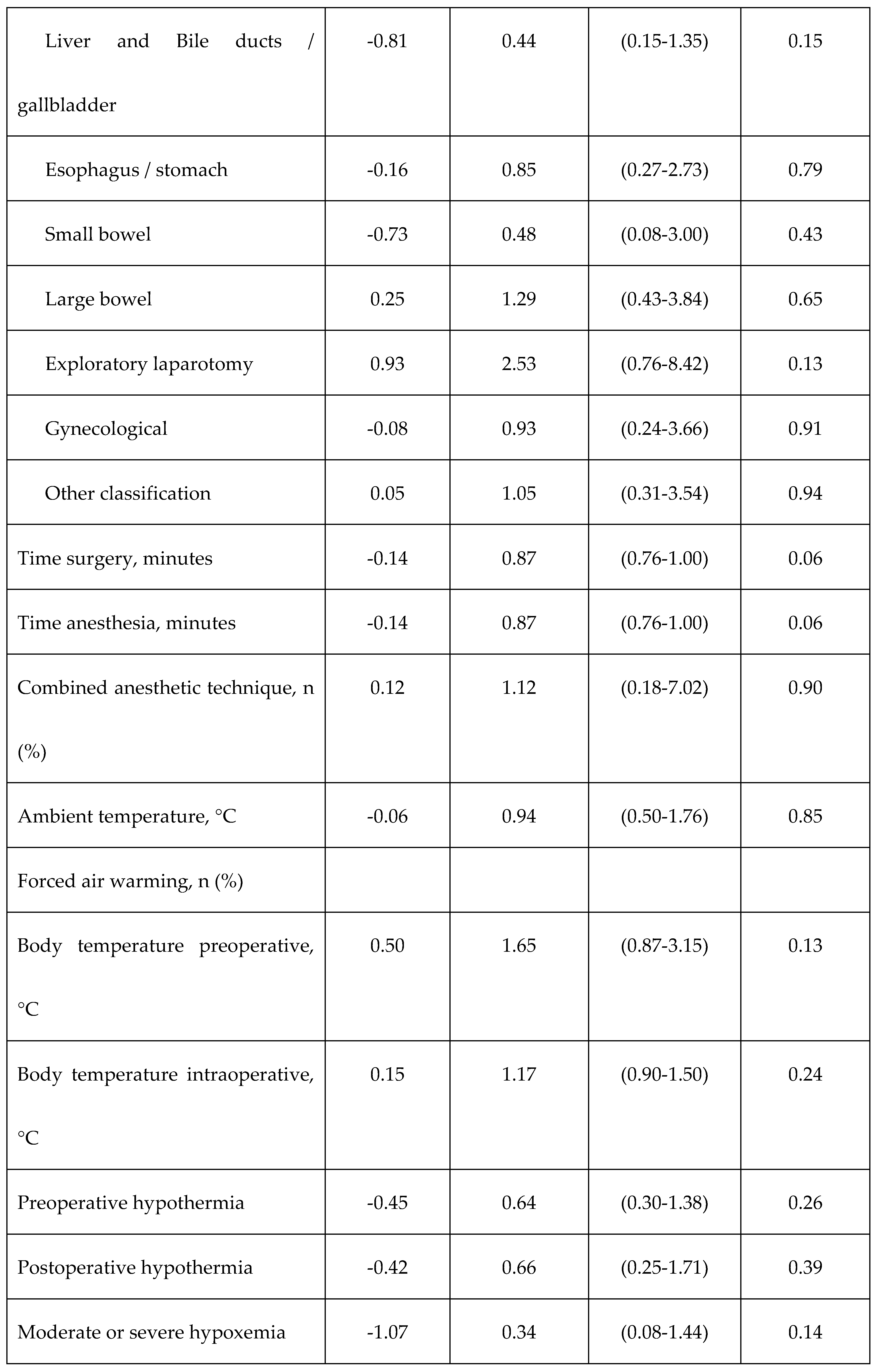
Table 4 shows the results of the univariate logistic regression analyses to identify the factors associated with postoperative hypothermia. Only advanced age (age over 60 years) was associated with a higher risk of postoperative hypothermia (OR=4.20, 95%CI: 1.45-12.18, p=0.01). After multivariable adjustment for sex, age, and time surgery, advanced age remained as a risk factor for postoperative hypothermia (OR=18.4, 95% CI:3.79-89.6, p<0.0001).
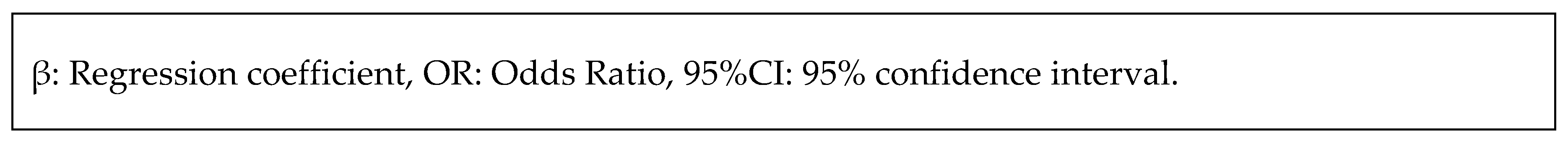
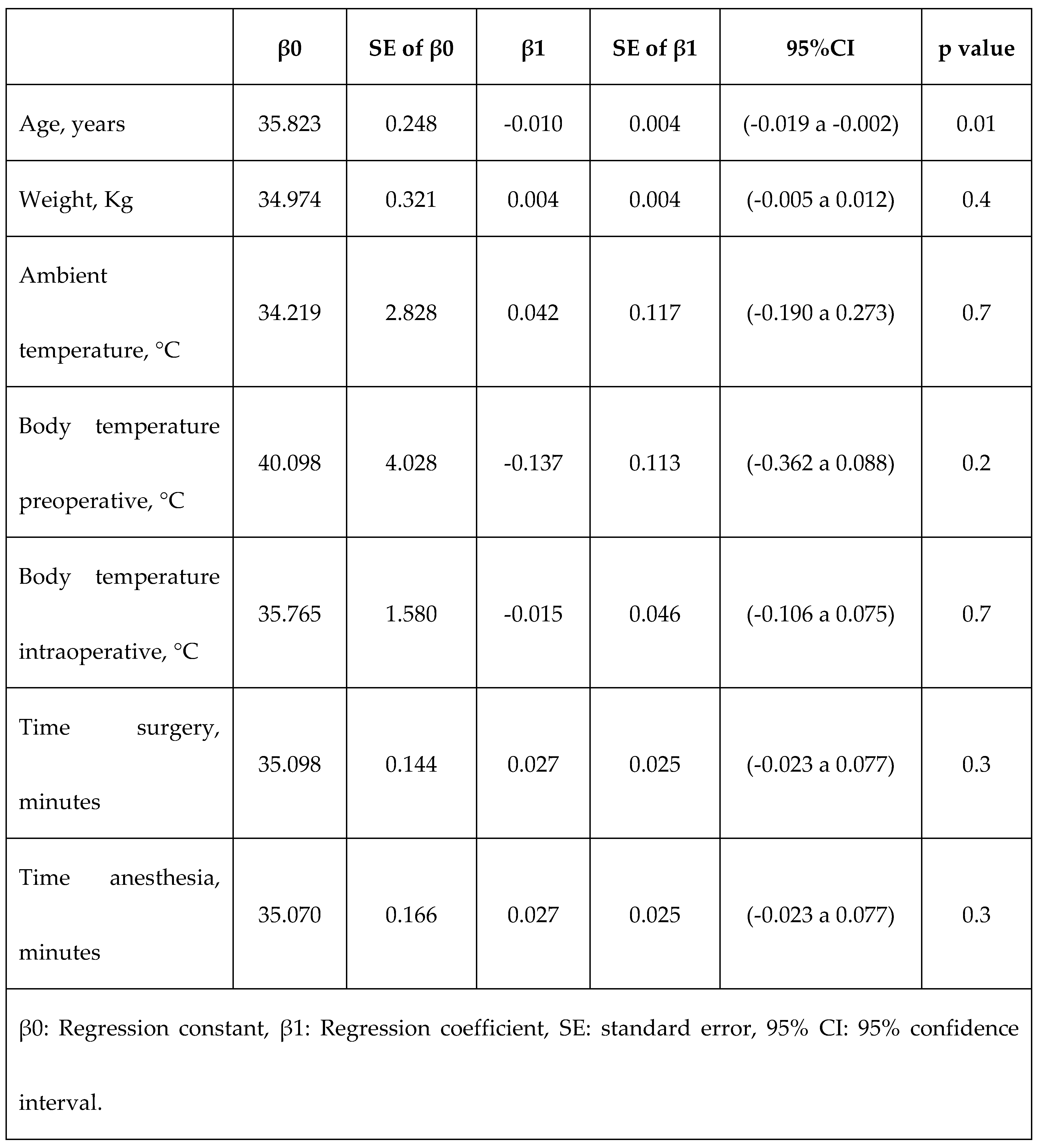
Table 5 shows the results of the linear regression analyses to determine the linear relationship of each of the quantitative variables with the change in body temperature after surgery. Only age was related to a decrease in temperature, considering that every one-year increase over 35.8 years lead to a decrease of 0.01 °C in the postoperative body temperature.
Discussion
In this study, we sought to describe the proportion of patients subjected to major abdominal surgery who experience postoperative hypothermia, and to study potential variables associated to the occurrence of postoperative hypothermia. We found that the incidence of postoperative hypothermia in patients undergoing major abdominal surgery was 57.3%, while preoperative and intraoperative hypothermia occurred in 55.5% and 79.1%, respectively. The occurrence of hypothermia was higher in the intraoperative period, which could be attributable to situations happening during surgery, such as induction of anesthesia or blood loss.
The incidence of postoperative hypothermia varies among studies. With 116 patients, a cross-sectional study performed in Mexico reported a similar proportion to ours (55%).1 Likewise, Zhang et al. reported an incidence of 21.3% in a retrospective cohort study with a larger study population.16 Regarding advanced age as a risk factor, it was hypothesized that modifiable and non-modifiable risk factors are associated with the presentation of hypothermia in the immediate postoperative period in patients undergoing major surgery. However, only age older than 60 years was found to be associated with hypothermia. This coincides with the literature where it has been reported as a risk factor in studies of patients undergoing orthopedic surgery,5,9 abdominal surgery,9 and surgeries in general without distinguishing the anatomical site.6,11,12
Differences in thermoregulatory mechanisms between younger and older adults have been documented.17 Underlying mechanisms include alteration of three of the major protective mechanisms against hypothermia: 1) decreased sympathetic and vasomotor responses that attenuate cutaneous vasoconstriction, 2) decreased heat generation by metabolic activity, and 3) decreased cold perception.17
Other studies have found that the anatomical site is associated with the presence of perioperative hypothermia, especially abdominal procedures when compared to surgeries of other types.9 Therefore, there was special interest in studying whether there was any association between the occurrence of postoperative hypothermia and the specific abdominal site of surgery. However, none of the specific surgical sites or organs were found to be associated with postoperative hypothermia. Therefore, there could be a common pathophysiological trigger for all abdominal surgeries that is not organ specific. In a study that compared the occurrence of perioperative hypothermia in patients undergoing colorectal surgery by open versus laparoscopic surgery, the occurrence of hypothermia was like that reported in our study (67%) and while it was more frequent in the open surgical approach than in the laparoscopic approach (71.23% vs. 63.16%, p<0.001), the type of surgical approach did not behave as a risk factor after adjusting for confounding variables.18
Other variables such as comorbidities, body mass index, ASA-PS and sex were not associated with postoperative hypothermia in this study despite the fact that in other studies there has been an association.5,6 Noteworthy, most patients in our study were ASA-PS III (94.5%), reason why we were unable to capture a bigger picture of what could be expected in patients under different ASA-PS categories. Although there is a possibility that in reality, they are not factors associated with postoperative hypothermia in patients undergoing major abdominal surgery exclusively, it is important to take into account that the sample size calculation for this study was made to detect variables that increased the risk of hypothermia by at least twice, so there is a possibility that larger sample sizes could be required to detect smaller differences. Furthermore, we were unable to reach the final sample size calculated for this study due to administrative constraints, reason why our study could have been underpowered to detect those differences.
Our results of the incidence of hypothermia and age as a significant risk factor contribute to the existing literature by providing insights into a specific population of patients who underwent abdominal surgery. Our findings suggest that age should be considered as a relevant factor in assessing the risk of perioperative hypothermia and the importance of monitoring older patients for hypothermia prevention. Nevertheless, it should be considered that our findings are from a sample of 110 patients undergoing abdominal surgery lasting longer than 2 hours from a single tertiary care referral hospital, which may not be generalizable to populations undergoing surgery at different kind of hospitals. Although our results are consistent with other studies, a further limitation to generalizability of our study is that we did not include pregnant women, patients under 18 years of age, or with neuromuscular problems. Future research could include these and other populations for a comprehensive understanding of the risk factors and mechanisms that lead to hypothermia during surgery.
Adding to the limitations of our study, temperature was measured with an axillar thermometer instead of oral or esophageal measurement devices, which are better approximations of the core body temperature.19 Furthermore, we only assessed forced air maneuvers as a potential intervention done to manage perioperative hypothermia. Other warming devices20 were not assessed due to their empirical low use in this center but could have an important role in prevention and management of perioperative hypothermia. Likewise, variables such as drugs administered in the perioperative period (which could have a pathophysiological role in the triggering of hypothermia) were not collected.21
Conclusions
The incidence of postoperative hypothermia in patients undergoing major abdominal surgery was 57.3%, while preoperative and intraoperative hypothermia occurred in 55.5% and 79.1%, respectively. Age over 60 years was associated with postoperative hypothermia. Prospective studies with a larger number of patients that include other types of surgery at different anatomical sites are required to continue characterizing the potential role of the anatomical site of surgery as a determinant of perioperative hypothermia.
Conflicts of Interest
The authors declare that they have no conflict of interest.
References
- Fernández Soto JR, García Ezquerro C, Labra Nassar A, Martínez Nápoles AR, Escobedo Berumen L, Álvarez Reséndiz GE, et al. Hipotermia postquirúrgica: incidencia en el Hospital Ángeles Lomas. Acta Médica Grup Ángeles. 2020;18(1):111–5.
- American Society of Anesthesiologists. Standards for Basic Anesthetic Monitoring, Committee of Origin: Standards and Practice Parameters. Am Soc Anesthesiol. 2020;1–3.
- National Collaborating Centre for Nursing and Supportive Care. The Management of Inadvertent Perioperative Hypothermia in Adults. London; 2008.
- Kim D. Postoperative Hypothermia. Acute Crit Care. 2019 Feb 28;34(1):79–80.
- Kleimeyer JP, Harris AHS, Sanford J, Maloney WJ, Kadry B, Bishop JA. Incidence and Risk Factors for Postoperative Hypothermia After Orthopaedic Surgery. J Am Acad Orthop Surg. 2018;26(24):e497–503.
- Li C, Zhao B, Li L, Na G, Lin C. Analysis of the Risk Factors for the Onset of Postoperative Hypothermia in the Postanesthesia Care Unit. J Perianesthesia Nurs. 2021;36(3):238–42.
- Karalapillai D, Story D, Hart GK, Bailey M, Pilcher D, Cooper DJ, et al. Postoperative hypothermia and patient outcomes after elective cardiac surgery. Anaesthesia. 2011;66(9):780–4.
- Karalapillai D, Story D, Hart GK, Bailey M, Pilcher D, Schneider A, et al. Postoperative hypothermia and patient outcomes after major elective non-cardiac surgery. Anaesthesia. 2013;68(6):605–11.
- Akers JL, Dupnick AC, Hillman EL, Bauer AG, Kinker LM, Hagedorn Wonder A. Inadvertent Perioperative Hypothermia Risks and Postoperative Complications: A Retrospective Study. AORN J. 2019;109(6):741–7.
- Motamed C, Weil G, Dridi C, Bourgain JL. Incidence of severe hypothermia and its impact on postoperative surgical complications and time delay to adjunct treatments in breast surgery cancer patients: A case-controlled study. J Clin Med. 2021;10(16):4–11.
- Mendonça FT, Lucena MC de, Quirino RS, Govêia CS, Guimarães GMN. Risk factors for postoperative hypothermia in the post-anesthetic care unit: a prospective prognostic pilot study. Brazilian J Anesthesiol. 2019;69(2):122–30.
- Peixoto C de A, Ferreira MBG, dos Santos Felix MM, Pereira CB de M, Cândido JV, Rocha VFR, et al. Factors contributing to intraoperative hypothermia in patients undergoing elective surgery. Perioper Care Oper Room Manag. 2021;22(December 2020).
- Sagiroglu G, Ozturk G, Baysal A, Turan F. Inadvertent Perioperative Hypothermia and Important Risk Factors during Major Abdominal Surgeries. J Coll Physicians Surg Pakistan. 2020 Feb 1;30(2):123–8.
- Duong H, Patel G. Hypothermia [Internet]. StatPearls. 2022 [cited 2023 Mar 13]. Available from: https://www.ncbi.nlm.nih.gov/books/NBK545239/.
- American Society of Anesthesiologists. ASA Physical Status Classification System [Internet]. Committee of Oversight: Economics. 2020. p. 4. Available from: https://www.asahq.org/standards-and-guidelines/asa-physical-status-classification-system.
- Zhang H, Wang J, Zhu S, Li J. The prevalence of and predictors for perioperative hypothermia in postanaesthesia care unit. J Clin Nurs. 2022 Sep 8;31(17–18):2584–92.
- Frank SM, Raja SN, Bulcao C, Goldstein DS. Age-related thermoregulatory differences during core cooling in humans. Am J Physiol - Regul Integr Comp Physiol. 2000;279(1 48-1):349–54.
- Cumin D, Fogarin J, Mitchell SJ, Windsor JA. Perioperative hypothermia in open and laparoscopic colorectal surgery. ANZ J Surg. 2022;92(5):1125–31.
- Lenhardt R. Monitoring and thermal management. Best Pract Res Clin Anaesthesiol. 2003 Dec;17(4):569–81.
- Simegn GD, Bayable SD, Fetene MB. Prevention and management of perioperative hypothermia in adult elective surgical patients: A systematic review. Ann Med Surg. 2021 Dec;72:103059.
- Rauch S, Miller C, Bräuer A, Wallner B, Bock M, Paal P. Perioperative hypothermia—a narrative review. Int J Environ Res Public Health. 2021;18(16).
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).