1. Introduction
The accelerated pace with which new diagnostic possibilities are produced and the need for efficient use of resources in health systems lead to the urgent need to provide systematic and effective solutions to reduce these inefficiencies and improve the rational use of health technology [
1]. The fundamental role of technology assessment is recognized as multidisciplinary policy research in the generation of evidence to inform the prioritization, selection, introduction, distribution, and management of health technologies.
Different guidelines have been developed to conduct the Health Technologies Assessment (HTA). The literature refers to two pioneering models: the mini-HTA developed by the Danish Agency in 2005 [
2], and the Core model developed by the EUnetHTA in 2006 [
3]. Another recently released model is the mini-HTA model developed under the AdHopHTA project in 2015 [
4]. However, the learning curves (LC) within the assessment domains are not systematically considered.
The MedtecHTA project [
5], 2013-2016, aimed at analyzing existing methodologies for the assessment of medical devices, recommended incorporating LC in decision analysis models. Other publications by Fuchs et al., 2016 [
6] and 2017 [
7], and Tarricone et al., 2017 [
8] propose these same challenges based on the unique characteristics of medical devices that have not yet been addressed and the impact on organizational changes with the acquisition of new technology.
Dengue is one of the most rapidly spreading viral diseases in the world, and the prevalence of the disease has increased approximately 30 times over the past half century, despite efforts to prevent it [
9]. One model estimated indicators of 390 million dengue virus infections per year (with a 95% confidence interval of 284–528 million), of which 96 million (67-136 million) manifested clinically (for any severeness of the disease). Another dengue prevalence study estimated that 3.9 billion people are at risk of dengue virus infection [
10].
WHO guidelines recommend classifying the disease into dengue without warning signs, dengue with warning signs, or severe dengue for timely and appropriate clinical management. It also indicates abdominal ultrasound to detect plasma leakage, a symptom associated with severe dengue. Studies refer to POCUS as a predictor or prognostic sign of severe dengue, even in children. [
11,
12,
13,
14,
15] Nevertheless, the use of POCUS for endemic infectious diseases in tropical regions has been limited. According to S. Bélard et al. (2015), focused assessment with sonography for HIV-associated TB (FASH) and echinococcosis (FASE) are the only two POCUS protocols for tropical infectious diseases that have been formally investigated and routinely implemented in patient care [
13].
The usefulness of point-of-care ultrasound (POCUS) in terms of accessibility to diagnostic methods in low-resource settings is clear and is considered an extension of the physical examination. Nonetheless, it is important to formalize the scanning and training protocols for infectious diseases [
12,
16]. The tasks of identifying the training hours required to achieve competency in image acquisition, interpretation, and cognitive foundations and assessing the maintenance of these competences are still an unexamined area of research [
17]. Acquiring valid POCUS images and interpreting them correctly are operator-dependent skills. Selecting a reliable and valid statistical tool to evaluate the LC of these clinical proficiencies is an essential element in ensuring patient safety. The Cumulative Summation Control Chart (CUSUM) and Learning Curve CUSUM (LC-CUSUM) control charts are statistical tools that can help assess the LC, indicate when the required proficiency level has been reached, and monitor performance [
18,
19].
Modeling healthcare systems is complex; conventional simulation strategies do not fully address the multiplicity of medical care and the process of care for diseases and pathologies. System dynamics (SD) has been successfully used to model the early management of COVID-19 and its implications for the Indonesian health system [
20]. SD has been evaluating the economic effects of healthcare in low- and middle income settings [
21]. SD has also been used to assess control strategies for diseases transmitted by the Aedes albopictus mosquito (the "Asian tiger") spread by human travel [
22] and to conceptualize the environmental causes of the chronic kidney disease epidemic in Sri Lanka. [
23]
SD is a methodology that is applied to examine complex and dynamic problems with a focus on the interrelationships between various elements of the system [
24]. SD is known to facilitate the analysis of the mutual effects of different variables, the impact of interventions over time when it is not immediately identifiable, and the analysis of non-linear internal and external factors [
25]. Models built with SD have structure and behavioral validation. [
26,
27,
28]. Hence, SD was selected to build the simulation model presented in this work. SD served to analyze the relationship between the variables associated with the assessment domains and the behavior of LC over time. The balance and reinforcement loops resulting from the relationships between the variables allowed us to consider the use of the POCUS for other types of diagnoses in the emergency service.
Considering that the literature [
5,
6,
7,
8] recognizes the differentiating characteristics of medical devices and that it proposes a challenge to incorporate LC within the assessment domains for operator-dependent technologies, this work evaluates the POCUS technology from a hospital level [
29], incorporating LC to contribute to the classification of a tropical disease endemic to Africa and Central and South America.
The objectives of this work are (1) to present a conceptual model that integrates the four assessment domains suggested by the AdHopHTA project in 2015 [
4] with the LC, and (2) to verify and calibrate said conceptual model using the SD method in the classification of a tropical disease such as dengue, characterized by a high spread rate.
2. Materials and Methods
2.1. Conceptual SD model
To identify the theoretical elements of the model such as domains and assessment criteria, the models currently used at the hospital level were studied. The mini-HTA model of AdHopHTA [
4] and different assessments carried out under the AdHopHTA mini-HTA model were analyzed, including the assessment of Focused Assessment Sonography for Trauma (ECO-FAST). Interviews were conducted with physicians who use POCUS equipment in the emergency area in Colombian and Spanish hospitals.
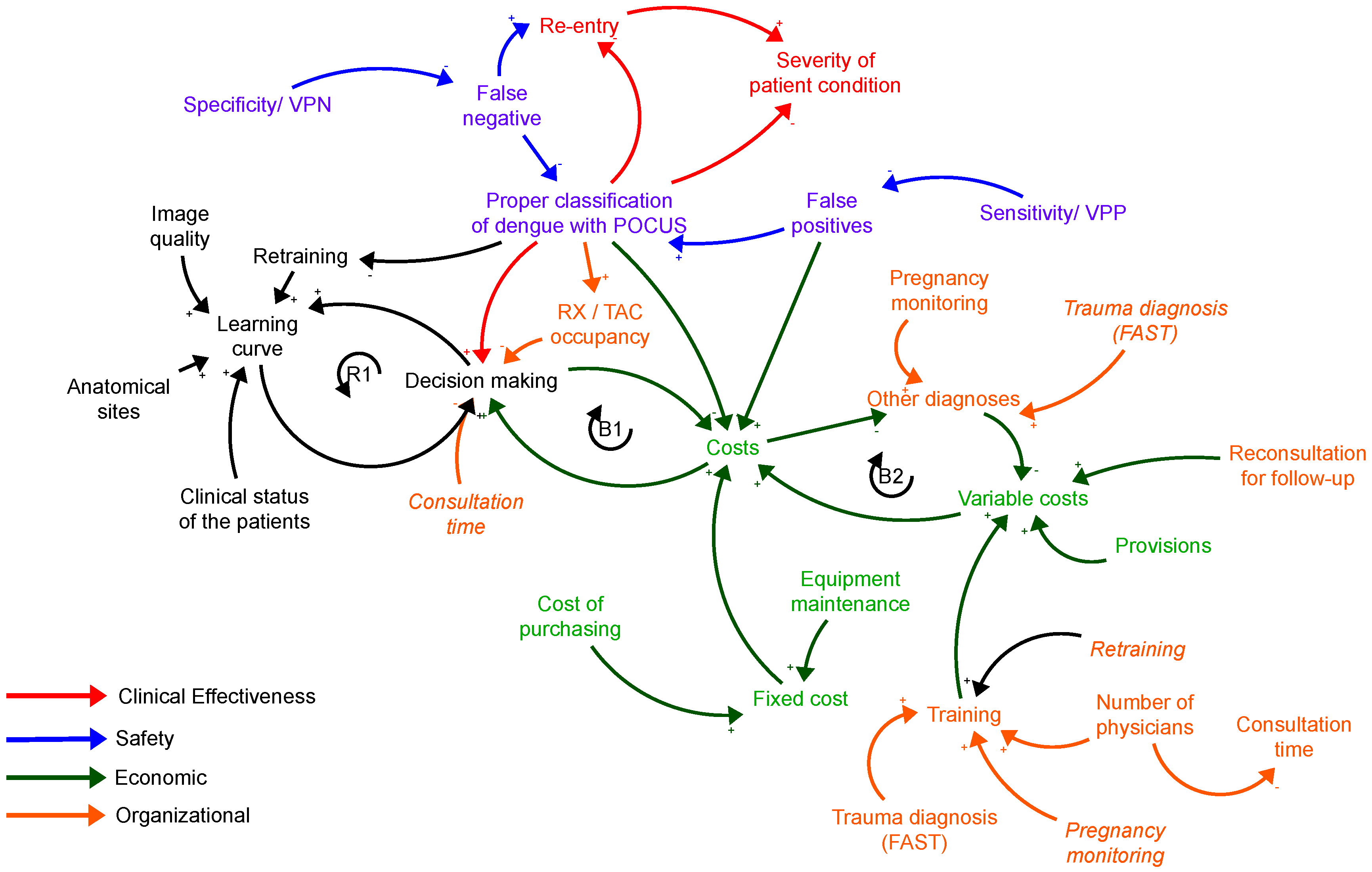
The general process of emergency care for patients with suspected dengue was studied, specifically the classification of dengue. Once the process was understood, the causal relationships represented in
Figure 1 were identified and grouped into four evaluation domains: clinical effectiveness, patient safety, organizational aspects, and economic aspects. [
30,
31,
32,
33,
34,
35] The LC factor was incorporated into this representation.
The LC criterion was modeled using the LC-CUSUM and CUSUM control charts, considering its applicability in medical processes, such as cardiac surgery or disease outbreaks. The LC-CUSUM has the ability to signal when a process reaches a state of control, that is when a student reaches an adequate level of performance, and CUSUM detects when the process changes to an out-of-control state. [
36]
The LC-CUSUM and CUSUM control charts are tools that allow: Quantitative evaluation of discrete variables. Immediate retrospective or prospective feedback. Individualized evaluation of the LC. [
36], and the ability to define and achieve specific learning objectives and proficiencies. [
37]
Recent studies [
19] carry out a critical analysis of CUSUM and support its use in this sense, mainly if you want to quickly detect changes in performance in real time with binary data with predefined acceptable and unacceptable levels of proficiency. For the design of the LC-CUSUM and CUSUM graphs, it is required to set some parameters that determine the performance of these diagnostic tools. Among these parameters are the unacceptable failure rate P
0, the tolerable failure rate P
1 and the numerical value H that determines the control limit location on the CUSUM and LC-CUSUM charts. The corresponding acceptable and unacceptable failure rates were used to set a control limit (H) that, when crossed, indicates that proficiency has been achieved (LC-CUSUM) or lost (CUSUM). From these rates, we estimated the average number of procedures to detect a signal under H
0 and H
1 denoted as Average run length (ARL), given ARL
0 and ARL
1, respectively. Based on the literature and the concept of an expert radiologist, we established P
0 = 0.3 and P
1 = 0.1 for LC CUSUM and P
0 = 0.1 and P
1 = 0.2 for CUSUM. [
38,
39] A Monte Carlo simulation routine was carried-out to establish H and ARLs.
2.2. Case study
The case study was based on a prospective cohort study carried out in a Public Health Institution for first level care in Cali, Colombia. The included participants correspond to patients who attended the emergency department between April 2019 and March 2020 and who were considered by the treating physician to match the diagnosis of dengue virus disease. The data used is part of the research on the usefulness of POCUS to detect plasma leakage in subjects with dengue fever (PO-CUS-DENGUE). The POCUS-DENGUE project was approved by the Institutional Review Board of Universidad del Valle (Number: 022-018) and the University of Minnesota (STUDY00004437). Other data on patient demand was approved by the Institutional Review Board of the case study institution under the project "Point-of-care ultrasound bio-medical equipment evaluation model (POCUS) considering the learning curve: case application of dengue screening.
SD was used to study the behavior of the conceptual model, specifically the Stella Architect software (
www.iseesystems.com) at version 2.1.1. The modules of patient demand, POCUS service, ponderation, training, and POCUS-Dengue costs were designed.
For each assessment domain, the information for the emergency care variables of the institution was gathered. Database literature was reviewed from different sources: Medline and Embase via Ovid, Medline via PubMed, Cochrane Library via Wiley, Global Index Medicus, ClinicalTrials.gov, World Health Organization International, Clinical Trials Registry (WHO ICTRP), WHO Library Database (WHOLIS), Opengrey.eu, and Scopus between 2018 and 2021. Administrative and commercial data were accessed from cross-references.
Lastly, a sensibility analysis was carried out to understand the impact on certain assessment domains and criteria of modifying variables linked to the organizational structure of the service that requires the POCUS equipment, among other types of analysis.
3. Results
3.1. About the Conceptual Model
The resulting conceptual model is presented in
Figure 1. The domain of clinical effectiveness is related to the accurate screening of dengue, the re-consultation rate, and the severity of the patient condition, classified as: recovered at home; recovered after being hospitalized; immediately referred to another hospital with a higher level of complexity; recovered in another hospital.
Figure 1.
Causal diagram of the POCUS assessment model with all four assessment domains and LC.
Figure 1.
Causal diagram of the POCUS assessment model with all four assessment domains and LC.
The security domain is related to the rate of false negatives and false positives associated with dengue screening.
The organizational domain refers to the average time between the performance of the ultrasound and the training course. Infrastructure-related aspects were not considered in this domain since they do not affect the portability of the device.
In terms of the economic domain, an analysis of fixed and variable costs and consequences was carried out to form a value judgment on the use of technology with information on related costs.
The feedback loops (
Figure 1) that represent the dynamics of the subsystems are described below:
- -
Loop B1 (Balance): It represents the relationship between costs and indicators for decision making. When decision-making criteria such as cost-benefit ratio, availability, false negatives and false positives, and adequate screening of extravasation are increased, the associated costs decrease. In cases where the rigor of the mentioned processes decreases, the costs increase. These parameters can be adjusted by the decision-maker through the Stella interface.
- -
Loop B2 (Balance): By using the POCUS equipment for the diagnosis of diseases other than dengue, variable costs decrease due to the reimbursement received by insurers for the provision of these services. As variable costs increase, total costs increase. Finally, when the total costs increase, it means that the reimbursement for the service of other diagnoses decreases.
Loop R1 (Reinforcement): It shows the causal relationship between the LC and the indicators for decision making; the behavior of the curve in terms of a better learning curve will represent a better cost-benefit ratio.
In relation to the LC the Monte Carlo simulation, it was concluded:
For LC-CUSUM the acceptable and unacceptable failure rates were: P1=0,1 y P0= 0,3, with a limit H: 2,5 and for CUSUM the acceptable and unacceptable failure rates were: P0=0,1 and P1= 0,2, with a limit H: 1,5. These values comply with the Average Run Length.
The performance of LC-CUSUM in terms of the Average Run Length (ARL
0) was 98 procedures under the null hypothesis and 17 procedures under the alternative hypothesis (ARL
1), 17 procedures. For CUSUM the ARL
0 was 99 procedures and ARL
1 was 23 procedures on average. The LC design parameters were taken from an article approved for publication in an indexed journal. [
40]
For each sequential image (t), the sequential score is calculated as
and Wt is determined based on the next equation:
In this work, the sequence St was modeled as a Bernoulli distribution (simulated in STELLA® as a binomial distribution with N = 1) with an 80% probability of success. It is possible to adjust this parameter in the simulation.
3.2. About the Case Study
3.2.1. Patient demand module
This module is related to the demand from patients that could have dengue, are confirmed to have dengue, are re-entry patients, are recovering at home, are hospitalized, and are sent to other healthcare institutions.
The demand from patients that could have dengue was simulated through the Poisson distribution of the case study data in days throughout a year. The model determined that confirmed cases of dengue corresponded to patients with positive IgM with a rate of 0.56 (100 / 178).
Furthermore, a possible second evaluation was considered when the person still has dengue symptoms and reenters the model after being labeled as a false negative. Although the case study did not include readmission data, the simulation allows the user to set this parameter. A rate of 0.29 (52/178) was programmed into the model using the consultations taking place during the checkup window as a reference.
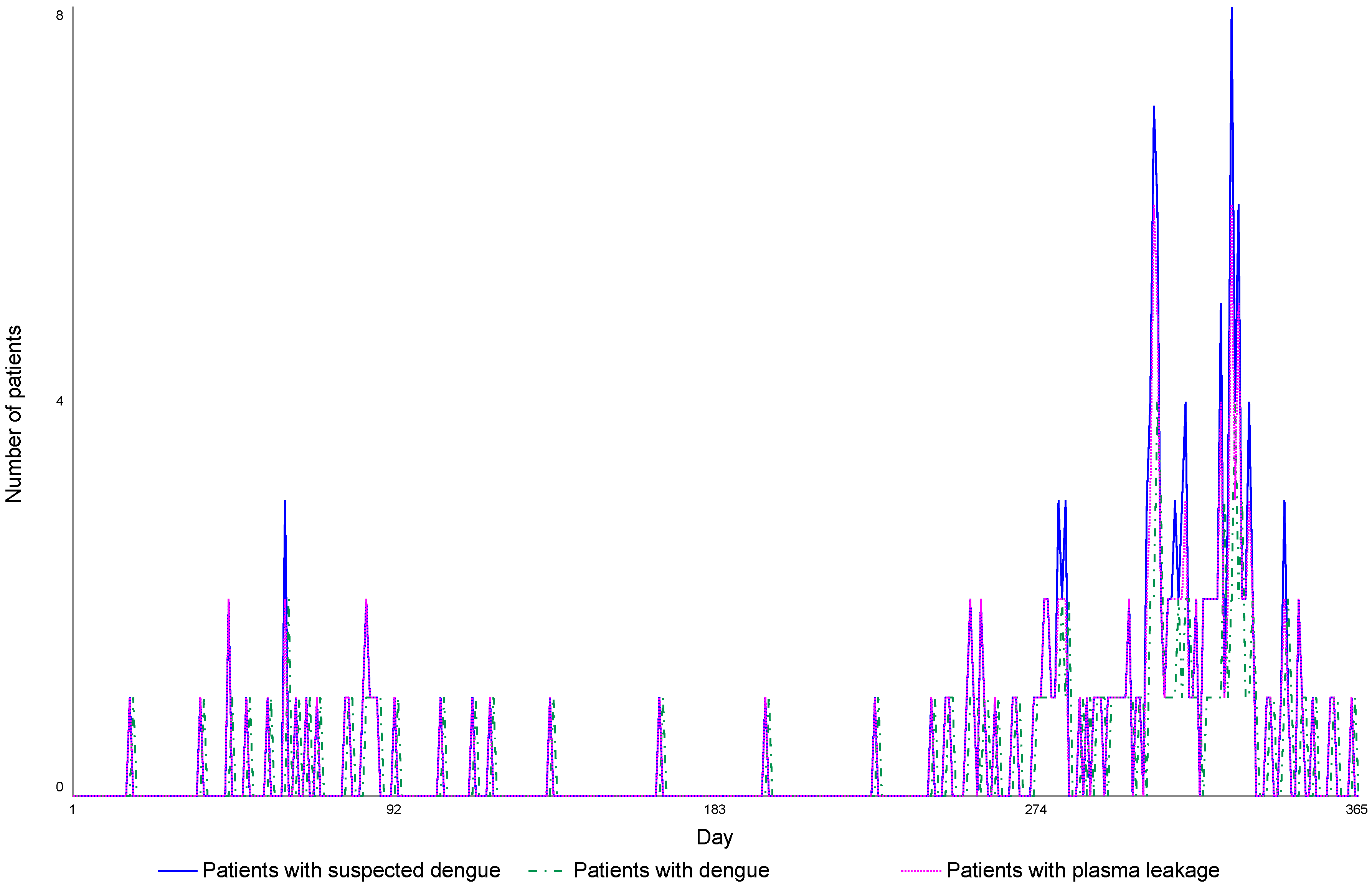
The Wilcoxon signed-rank test was applied, resulting in p = 0.476, which implies that there is no significant difference between simulated and real data (
Figure 2).
Figure 2.
Patient intake behavior. The model follows the behavior of the case study and exhibits an increase in intake for the second semester of the year.
Figure 2.
Patient intake behavior. The model follows the behavior of the case study and exhibits an increase in intake for the second semester of the year.
The following equations represent the behavior of the model: D
c are the patients confirmed to have dengue; O
d are the patients with other diagnoses; P
HyR are the patients that recovered in the hospital and were referred; P
H patients that are hospitalized in the institution; P
R patients that were referred immediately; and P
Rd patients that were referred after a few days. Considering the cohort study and the routine checkup of patients, the hospitalization rate was set at 0.67 (67/100), the immediate referral rate at 0.02 (2/100), and the rate of being referred after a few days at 0.13 (9/67).
3.2.2. POCUS healthcare module
The number of patients with and without plasma leakage is calculated in this module using a rate of 0.83 (149/178) according to the cohort study. It is assumed that all patients suspected of dengue take the POCUS test. However, if the patient has pulmonary compromise and the doctor is not qualified to perform the POCUS test, then the patient is referred to the radiology area for a chest x-ray. The rate for chest x-rays was defined as 0.511 (91/178) which corresponds to patients with positive IgM and leakage confirmed by the expert radiologist.
The true positive and negative values VP and VN and the false positive and negative values FP and FN were calculated according to the equations detailed below. The sensitivity VPN and specificity VPP calculations were based on [
41]. However, the user can modify the parameters of the model.
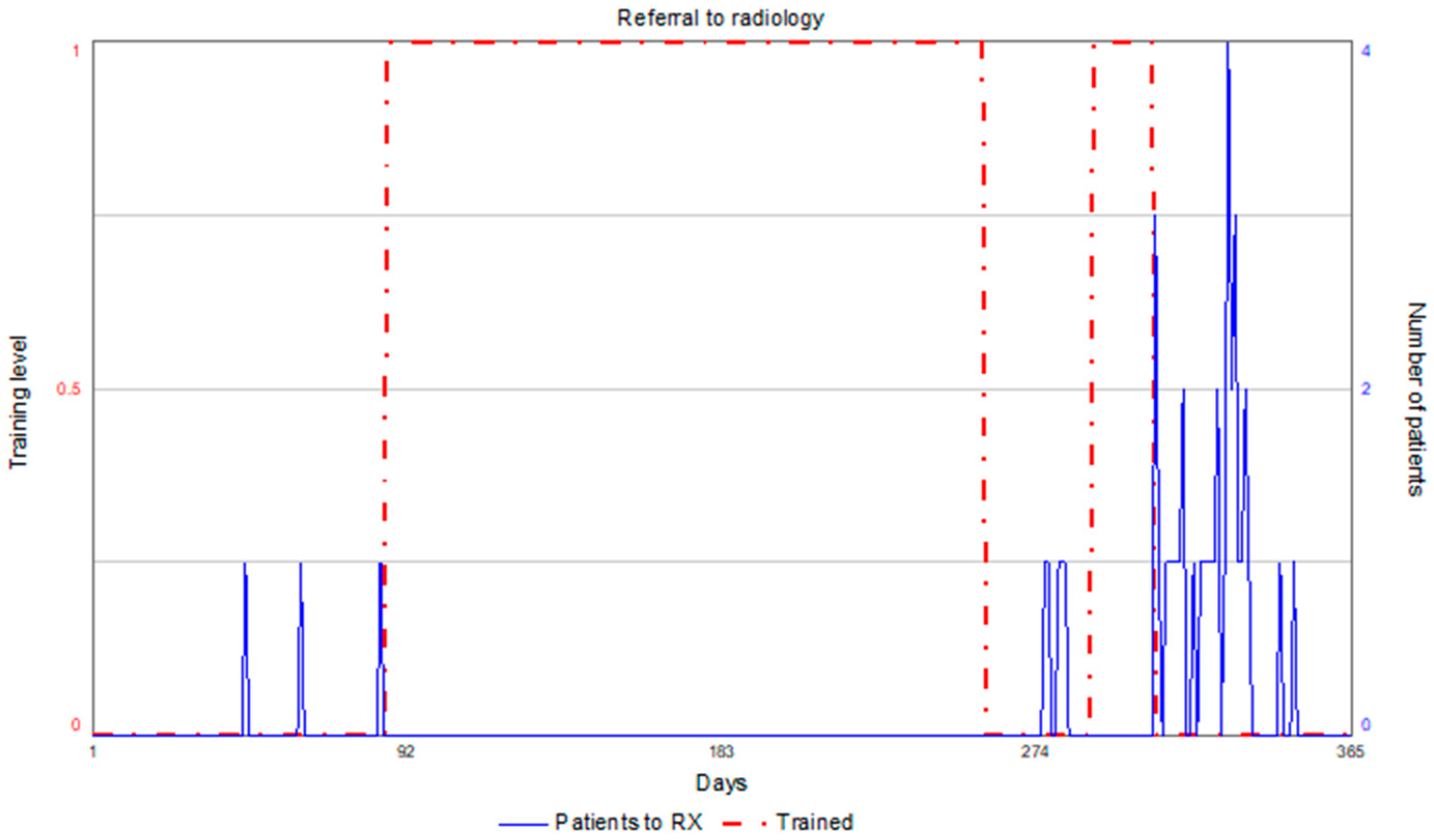
The model delivered a total of 159 patients with plasma leakage, which represents a 6% error compared to real data. According to simulations, if the doctor were trained enough from day 1 and never lost said skillset, the POCUS test would be performed for dengue screening on 177 patients. Given the effect of the learning curve and the base scenario of 20% failure probability, 131 patients entered the emergency room when the doctor was untrained to carry out the POCUS test, and 44 of them would take a chest x-ray. Therefore, the POCUS test is performed on 46 patients (177-131). In
Figure 3, when the red dotted signal
“reached proficiency status” reaches the value of 1, the patients are not sent to the radiology department, and the insurance company is charged for the POCUS test.
Figure 3.
The red dotted signal "reached proficiency status " is at 1, indicating that patients will not be sent to the radiology department.
Figure 3.
The red dotted signal "reached proficiency status " is at 1, indicating that patients will not be sent to the radiology department.
3.2.3. Ponderation and training module
As a result of the Montecarlo simulation and based on the equation presented in section 3.1., this module computed W(t) for LC-CUSUM in success cases, obtaining 0.2513, and in failure cases, obtaining -0.0986. The W(t) for CUSUM was -0.1178 in success cases and 0.6931 in failure cases.
The learning curve obtained in the base scenario of an 80% success rate for the doctor is presented in
Figure 4 (solid blue line). The training level is reached on day 85, and this level is maintained until day 257; then the training level is recovered on day 290, lost on day 306, and never recovered. The red dotted line represents the number of patients that could have dengue when entering the emergency room.
Figure 4.
learning curve for base scenario of 80% success rate.
Figure 4.
learning curve for base scenario of 80% success rate.
Figure 5 depicts the moments in which the training must be repeated in a black line, which are days 258 and 306.
Figure 5.
Behavior of the learning curve and retraining for base scenario of 80% success rate.
Figure 5.
Behavior of the learning curve and retraining for base scenario of 80% success rate.
3.2.4. POCUS-Dengue cost module
The fixed costs are computed in this module related to purchase value of the training biomedical equipment, usage of the equipment and annual preventive maintenance.
The reference values are taken from the Colombian market. The model assumes an equipment cost of COP $25.000.000, based on the Lumify Phillips device with a curve matrix of 5 to 2 MHz in B mode, and an equipment cost for emergency care of COP $101.000.000, based on the Sonosite Edge 2 device with these transductors: linear from 13 to 6 MHz, curved from 8 to 3 MHz, and endocavitary from 5 to 8 MHZ, in modes B, M, and color. The reference lifecycle of the equipment is 9 years, after which new echographs need to be purchased. The simulation took into consideration a preventive maintenance cost equal to 4% of the purchase price.
The fixed costs included training for POCUS-Dengue, using as a reference the certification in emergency and critical care medicine, with a timeframe of 90 hours, aimed at medical specialists (anesthesiologists, intensivists, surgeons, ER doctors, internists, etc.) in charge of handling critical care patients. The topics encompass the physical principles of ultrasound and instrumentation, basic focused echocardiography (FOCUS), echography of the lungs and pleura, FAST, aortic echography, echography for Deep Vein Thrombosis (DVT), and ultrasound-guided vascular access.
The costs associated with the POCUS-Dengue procedure included the retraining of doctors who lost their skillset. This information is generated by the model in the training module. Another factor is the workforce needed to cover for the clinical staff while they are in training. The model considers that at least three general doctors should be trained, one for each ER shift. This parameter can be adjusted by the user.
The variable costs were related to the supplies needed for echography such as gel and wipes, as well as the retraining process when the doctor needs to repeat the POCUS-dengue certification over time.
In terms of the income received by the healthcare institution from the insurance company due to the POCUS service, the fee corresponds to the one presented in the Fee Manual for Colombia. This income is only factored under the premise that the doctor is trained to perform the test on 46 patients.
The costs and projection of income were determined throughout the equipment lifecycle.
The dengue patient demand involved an analysis of the track record of Colombia. Between 2014 and 2022, it was found that 2019 was an epidemiological year, and there was no increased tendency afterwards. Hence, the model contemplates demand throughout the product lifecycle.
A 5% projection of costs and income was estimated, using as a reference the salary increase in Colombia between 2017 and 2021. The return on investment (ROI) was determined, as were the net present value and the cost-benefit ratio. A social discount of 9% was applied, as established by the National Department of Planning for the assessment of investment projects in the public sector.
In the base scenario, the cost-benefit ratio is 0.15, meaning that costs exceed benefits, and the ROI is negative for every year of the simulation, marking the lifecycle of the POCUS equipment.
The validation of the model was based on the coherence of units and extreme condition analysis. When a model is exposed to extreme conditions, the researchers can verify whether the model offers reasonable results and, thus, is error-free in its structure. The model showed consistent behavior in every module. One example of this is the demand behavior and Wilcoxon signed-rank test, with no significant difference between simulated and real data linked to the case study.
4. Discussion
The problem discussed in this work focused on the study of the influence of the learning curve in HTA on the acquisition of POCUS equipment. The HTA encompasses different assessment domains. Some articles in the organizational or legal domain contemplate training programs [
35,
42,
43]. However, these do not explicitly mention the LC. Some studies highlight this addition as a challenge in the field of medical device assessment. [
5,
6,
7,
8]
A conceptual model was developed and validated with a case study for an operator-dependent technology that applied the LC. The first result is an understanding of the LC and an identification of a valid statistical tool for its representation within a systemic model. In regards to this matter, it was found that certain factors have an impact on the training process and are considered for skill assessment in various ultrasound-related medical specialties: familiarity with the medical equipment, selection of an adequate transducer, image quality, image pattern recognition, and insight interpretation. [
44] The development of skills by any individual depends on many factors that vary according to the trainee, the procedure, the instructor, the setting, and the required performance level. [
18]
There are different guidelines for POCUS training, yet there are few tools to assess the reference points recommended to establish the level of competency. Establishing the moment in which competency is achieved or lost for operator-dependent technologies is a challenge. These technologies require methods to define individual reference points and monitor the learning process. The control graphs CUSUM and LC-CUSUM showcase the characteristics needed to assess LC by delivering feedback to the apprentice to improve until they recover competency. [
45] These intuitive control graphs helped analyze the behavior over time and thus understand the influence on other system variables.
The conceptual model built based on the assessment domains established in the AdHopHTA project in 2015 [
4] led to the identification of the influence of LC in the decision-making indicator: cost-benefit. The variable costs are influenced by the reimbursement that insurance companies earn from hospitals due to echography billing. This indicator is influenced by the income that is not earned when the doctor loses the required skillset, leading the patient to take other diagnostic tests such as x-ray or CT scans. This indicator is also marked by the costs linked to the retraining process.
The analysis of the proposed model extracted the need to use the POCUS equipment for other uses to improve the cost-benefit ratio. The model evidenced that patient demand, along with LC behavior, has a significant impact on this variable. This is supported by the recommendations of the Royal College of Radiologists that the doctor should not remain for more than three months without using these echography-related exploration skills. [
46] In this sense, it could be used in the ECO-FAST service and gynecological emergency situations. This would increase the income earned by the hospital due to the reimbursement of services. Nonetheless, the training of doctors in these new skills must also be considered in the variable costs.
Another relevant aspect is the availability of medical equipment. Although the POCUS-dengue test takes 20 minutes, the demand and alternative uses of the equipment could lead to excessive occupation, which could translate into increasing maintenance costs and cutting the lifecycle set by the manufacturer.
Regarding the assessment of clinical effectiveness and safety, the model calculates the VP, VN, FN, and FP based on the sensitivity and specificity referenced in the literature and rates for patients with plasma leakage. Therefore, patient demand also affects this indicator.
The model presents a degree of adaptability to different hospital environments, the model parameters can be customized by the user according to the hospital specifications, installed capacity, available human resources, epidemiological context, and even new bibliographic references related to the behavior of the disease. Patient demand, checkup consultation rates, readmission rates, the number of doctors to be trained, and diagnosis sensitivity and specificity can be customized.
5. Conclusions
This work established the influence of LC on economic and organizational indicators, mainly in the assessment of operator-dependent technologies such as POCUS. Variables such as patient demand and LC behavior had a significant impact on the income and costs of the healthcare system in dengue screening and ultimately the cost-benefit indicator.
In terms of the LC study, the results show that the control charts LC-CUSUM and CUSUM are a proper graphic tool to intuitively assess the learning curves and can be used to monitor in real time once the apprentice reaches a certain level of competency.
This work highlights the development of HTA models under a systemic approach and the importance of research on the impact of LC in decision-making for medical equipment acquisition. It is expected to keep exploring real-world scenarios of operator-dependent technologies and the barriers that limit the routine use of POCUS for dengue screening.
Author Contributions
Conceptualization, S.U-P. and J.I.G-M; methodology, S.U-P. and J.I.G-M; formal analysis, S.U-P., L.V.B-V and J.I.G-M.; investigation, S.U-P., L.V.B-V and J.I.G-M.; data curation, S.U-P., L.V.B-V.; writing—original draft preparation, S.U-P., L.V.B-V.; writing—review and editing, S.U-P., L.V.B-V and J.I.G-M.; funding acquisition, S.U-P. and J.I.G-M. All authors have read and agreed to the published version of the manuscript.
Funding
Funding support was provided by the Universidad Del Valle, Project CI 21140.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Institutional Review Board of Universidad del Valle (Number: 022-018), the University of Minnesota (STUDY00004437) and the Red de salud del Norte E.S.E (Number: ASI-019-2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
The data presented in this study are available upon request from the corresponding author.
Acknowledgments
The authors are deeply thankful to Dr. Lyda Osorio and Dr. Jonathan D Kirsch and Dr. Daniela Zuluaga for their clinical, methodological, and analytical contribution to the case study data. Equally, the authors thank Dr. Jaime Mosquera for his contributions in the construction of the control charts for the case study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- World Health Organization. Health Intervention and Technology Assessment in Support of Universal Health Coverage.; 2014.
- Danish National Board of Health. Introduction to Mini-HTA- a Management and Decision Support Tool for the Hospital Service. (Danish Centre for Evaluation and Health Technology Assessment (DACEHTA), ed.).; 2005. doi:10.1049/sm.1982.0029. [CrossRef]
- Kristensen FB, Lampe K, Wild C, Cerbo M, Goettsch W, Becla L. The HTA Core Model s — 10 Years of Developing an International Framework to Share Multidimensional Value Assessment. Value Heal. 2017;20(2):244-250. doi:10.1016/j.jval.2016.12.010. [CrossRef]
- Sampietro-Colom L LK, Cicchetti A KK, Pasternack I FB, Rosenmöller M WC, Kahveci R WJ, Kiivet RA et al. The AdHopHTA Handbook: A Handbook of Hospital-based Health Technology Assessment (HB-HTA).; 2015. http://www.adhophta.eu/sites/files/adhophta/media/adhophta_handbook_website.pdf.
- Tarricone R, Torbica A, Drummond M. Key Recommendations from the MedtecHTA Project. Heal Econ (United Kingdom). 2017;26:145-152. doi:10.1002/hec.3468. [CrossRef]
- Fuchs S, Olberg B, Panteli D, Busse R. Health Technology Assessment of Medical Devices in Europe: Processes, Practices, and Methods. Int J Technol Assess Health Care. 2016;32(04):246-255. doi:10.1017/S0266462316000349. [CrossRef]
- Fuchs S, Olberg B, Panteli D, Perleth M, Busse R. HTA of medical devices: Challenges and ideas for the future from a European perspective. Health Policy (New York). 2017;121(3):215-229. doi:10.1016/j.healthpol.2016.08.010. [CrossRef]
- Tarricone R, Torbica A, Drummond M. Challenges in the Assessment of Medical Devices: The MedtecHTA Project. Heal Econ (United Kingdom). 2017;26:5-12. doi:10.1002/hec.3469. [CrossRef]
- Soneja S, Tsarouchi G, Lumbroso D, Tung DK. A Review of Dengue’s Historical and Future Health Risk from a Changing Climate. Curr Environ Heal Reports. 2021;8(3):245-265. doi:10.1007/s40572-021-00322-8. [CrossRef]
- World Health Organisation. Dengue and Severe Dengue. Vol 117.; 2014. www.who.int/mediacentre/factsheets/fs117/en/index.html.
- Pothapregada S, Kullu P, Kamalakannan B, Thulasingam M. Is Ultrasound a Useful Tool to Predict Severe Dengue Infection? Indian J Pediatr. 2016;83(6):500-504. doi:10.1007/s12098-015-2013-y. [CrossRef]
- Bharath Kumar Reddy KR, Laksmana RR, Veerappa BG, Shivananda. Ultrasonography as a tool in predicting the severity of dengue fever in children - A useful aid in a developing country. Pediatr Radiol. 2013;43(8):971-977. doi:10.1007/s00247-013-2642-0. [CrossRef]
- Bélard S, Joekes E, Tamarozzi F, et al. Point-of-Care Ultrasound Assessment of Tropical Infectious Diseases—A Review of Applications and Perspectives. Am J Trop Med Hyg. 2015;94(1):8-21. doi:10.4269/ajtmh.15-0421. [CrossRef]
- Khurram M, Qayyum W, Umar M, Jawad M, Mumtaz S, Khaar HTB. Ultrasonographic pattern of plasma leak in dengue haemorrhagic fever. J Pak Med Assoc. 2016;66(3):260-264.
- Vedaraju KS, Kumar KR V, Vijayaraghavachari T V. Role of Ultrasound in the Assessment of Dengue Fever. Int J Sci Study. 2016;3(10):59-62. doi:10.17354/ijss/2016/12. [CrossRef]
- Brunetti E, Heller T, Richter J, et al. Application of Ultrasonography in the Diagnosis of Infectious Diseases in Resource-Limited Settings. Curr Infect Dis Rep. 2016;18(2):1-11. doi:10.1007/s11908-015-0512-7. [CrossRef]
- Díaz-Gómez JL, Mayo PH, Koenig SJ. Point-of-Care Ultrasonography. N Engl J Med. 2021;385(17):1593-1602. doi:10.1056/NEJMra1916062. [CrossRef]
- Biau DJ, Williams SM, Schlup MM, Nizard RS, Porcher R. Quantitative and individualized assessment of the learning curve using LC-CUSUM. Br J Surg. 2008;95(7):925-929. doi:10.1002/bjs.6056. [CrossRef]
- Woodall WH, Rakovich G, Steiner SH. An overview and critique of the use of cumulative sum methods with surgical learning curve data. Stat Med. 2020;(November):1-14. doi:10.1002/sim.8847. [CrossRef]
- Aminullah E, Erman E. Policy innovation and emergence of innovative health technology: The system dynamics modelling of early COVID-19 handling in Indonesia. Technol Soc. 2021;66. doi:10.1016/j.techsoc.2021.101682. [CrossRef]
- Cassidy R, Tomoaia-Cotisel A, Semwanga AR, et al. Understanding the maternal and child health system response to payment for performance in Tanzania using a causal loop diagram approach. Soc Sci Med. 2021;285(July). doi:10.1016/j.socscimed.2021.114277. [CrossRef]
- Mecoli M, De Angelis V, Brailsford SC. Using system dynamics to evaluate control strategies for mosquito-borne diseases spread by human travel. Comput Oper Res. 2013;40(9):2219-2228. doi:10.1016/j.cor.2012.03.007. [CrossRef]
- Jayasinghe S, Zhu YG. Response to the commentary by M.W.C. Dharma-wardana on ‘Chronic kidney disease of unknown etiology (CKDu): Using a system dynamics model to conceptualize the multiple environmental causative pathways of the epidemic.’ Sci Total Environ. 2020;721:2019-2021. doi:10.1016/j.scitotenv.2020.137591. [CrossRef]
- Sterman J. Business Dynamics : Systems Thinking and Modeling for a Complex World. Irwin/McGraw-Hill; 2000.
- Davahli MR, Karwowski W, Taiar R. A system dynamics simulation applied to healthcare: A systematic review. Int J Environ Res Public Health. 2020;17(16):1-27. doi:10.3390/ijerph17165741. [CrossRef]
- Barlas Y. Formal aspects of model validity and validation in system dynamics. Syst Dyn Rev. 1996;12(3):183-210. doi:10.1002/(SICI)1099-1727(199623)12:3<183::AID-SDR103>3.3.CO;2-W. [CrossRef]
- Šilhánková V, Maštálka M. Urban Dynamics. Vol 27.; 2013. doi:10.4324/9781315438689-23. [CrossRef]
- Lane DC, Sterman JD. Profiles in Operations Research: Jay Wright Forrester. In: International Series in Operations Research and Management Science. Vol 147. Springer New York LLC; 2011:363-386. doi:10.1007/978-1-4419-6281-2_20. [CrossRef]
- Poder TG, Bellemare CA, Bédard SK, Fisette JF, Dagenais P. Impact Of Health Technology Assessment Reports On Hospital Decision Makers - 10-Year Insight From A Hospital Unit In Sherbrooke, Canada: Impact Of Health Technology Assessment On Hospital Decisions. Int J Technol Assess Health Care. 2018;34(4):388-392. doi:10.1017/S0266462318000405. [CrossRef]
- Angelis A, Kanavos P. Value-Based Assessment of New Medical Technologies: Towards a Robust Methodological Framework for the Application of Multiple Criteria Decision Analysis in the Context of Health Technology Assessment. Pharmacoeconomics. 2016;34(5):435-446. doi:10.1007/s40273-015-0370-z. [CrossRef]
- EUNETHA. Process of information retrieval for systematic reviews and health technology assessments on clinical effectiveness. 2016;(December). http://www.eunethta.eu/sites/default/files/Guideline_Information_Retrieval_V1-1.pdf.
- Kidholm K, Ølholm AM, Birk-Olsen M, et al. Hospital managers’ need for information in decision-making - An interview study in nine European countries. Health Policy (New York). 2015;119(11):1424-1432. doi:10.1016/j.healthpol.2015.08.011. [CrossRef]
- Martelli N, Hansen P, van den Brink H, et al. Combining multi-criteria decision analysis and mini-health technology assessment: A funding decision-support tool for medical devices in a university hospital setting. J Biomed Inform. 2016;59:201-208. doi:10.1016/j.jbi.2015.12.002. [CrossRef]
- Ritrovato M, Faggiano FC, Tedesco G, Andellini M, Derrico P. Integrating AHP into EUNETHTA core model: the decision-oriented health technology assessment (doHTA) method. In: ; 2016. doi:10.13033/isahp.y2016.076. [CrossRef]
- Ritrovato M, Faggiano FC, Tedesco G, Derrico P. Decision-oriented health technology assessment: One step forward in supporting the decision-making process in hospitals. Value Heal. 2015;18(4):505-511. doi:10.1016/j.jval.2015.02.002. [CrossRef]
- Biau DJ, Porcher R. A method for monitoring a process from an out of control to an in control state: Application to the learning curve. Stat Med. 2010;29(18):1900-1909. doi:10.1002/sim.3947. [CrossRef]
- Papanna R, Biau DJ, Mann LK, Johnson A, Moise KJ. Use of the Learning CurveCumulative Summation test for quantitative and individualized assessment of competency of a surgical procedure in obstetrics and gynecology: Fetoscopic laser ablation as a model. Am J Obstet Gynecol. 2011;204(3). doi:10.1016/j.ajog.2010.10.910. [CrossRef]
- Arzola C, Carvalho JCA, Cubillos J, Ye XY, Perlas A. Anesthesiologists’ learning curves for bedside qualitative ultrasound assessment of gastric content: A cohort study. Can J Anesth. 2013;60(8):771-779. doi:10.1007/s12630-013-9974-y. [CrossRef]
- Oliveira KF, Arzola C, Ye XY, Clivatti J, Siddiqui N, You-Ten KE. Determining the amount of training needed for competency of anesthesia trainees in ultrasonographic identification of the cricothyroid membrane. BMC Anesthesiol. 2017;17(1):1-7. doi:10.1186/s12871-017-0366-7. [CrossRef]
- Usaquén-Perilla, S.P. Ropero-Rojas, D. Mosquera-Restrepo, J. D-Kirsh, J. P-Kaltenborn Z. García- Melo, J.I. Osorio L. Control charts to establish and monitor proficiency in the detection of pulmonary B- lines with Point of Care Ultrasound. Ing y Univ Eng Dev. 2023;(accepted).
- Balasubramanian S, Janakiraman L, Shiv Kumar S, Muralinath S, Shivbalan S. A reappraisal of the criteria to diagnose plasma leakage in dengue hemorrhagic fever. Indian Pediatr. 2006;43(4):334-339.
- Ramsay CR, Wallace SA, Garthwaite PH, Monk AF, Russell IT, Grant AM. Assessing the learning curve effect in health technologies. Lessons from the nonclinical literature. Int J Technol Assess Health Care. 2002;18(1):1-10. http://www.ncbi.nlm.nih.gov/pubmed/11987432.
- Miniati R, Frosini F, Cecconi G, Dori F, Gentili GB. Development of sustainable models for technology evaluation in hospital. Technol Heal Care. 2014;22(5):729-739. doi:10.3233/THC-140847. [CrossRef]
- Tolsgaard MG, Todsen T, Sorensen JL, et al. International Multispecialty Consensus on How to Evaluate Ultrasound Competence: A Delphi Consensus Survey. PLoS One. 2013;8(2). doi:10.1371/journal.pone.0057687. [CrossRef]
- Schuwirth LWT, Van Der Vleuten CPM. Programmatic assessment: From assessment of learning to assessment for learning. Med Teach. 2011;33(6):478-485. doi:10.3109/0142159X.2011.565828. [CrossRef]
- RCR R college of R. Ultrasound Training Recommendations for Medical and Surgical Specialties Second Edition Board of the Faculty of Clinical Radiology.; 2015.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).