Submitted:
28 May 2023
Posted:
31 May 2023
You are already at the latest version
Abstract
Keywords:
BACKGROUND
OBJECTIVES
- (1)
- To assess practitioners’ knowledge, attitudes and practices (KAP) in the diagnosis and management of drug resistant TB patients in both the government and private sectors.
- (2)
- To assess practitioners' perspectives on strengthening the National TB Elimination Programme (NTEP) with respect to knowledge and awareness regarding drug resistant TB.
METHODOLOGY:
- Drug resistant TB: its transmission and extent of problem
- Case definition/ diagnosis of drug resistant TB
- Treatment of drug resistant TB
- Infection control practices & XDR-TB
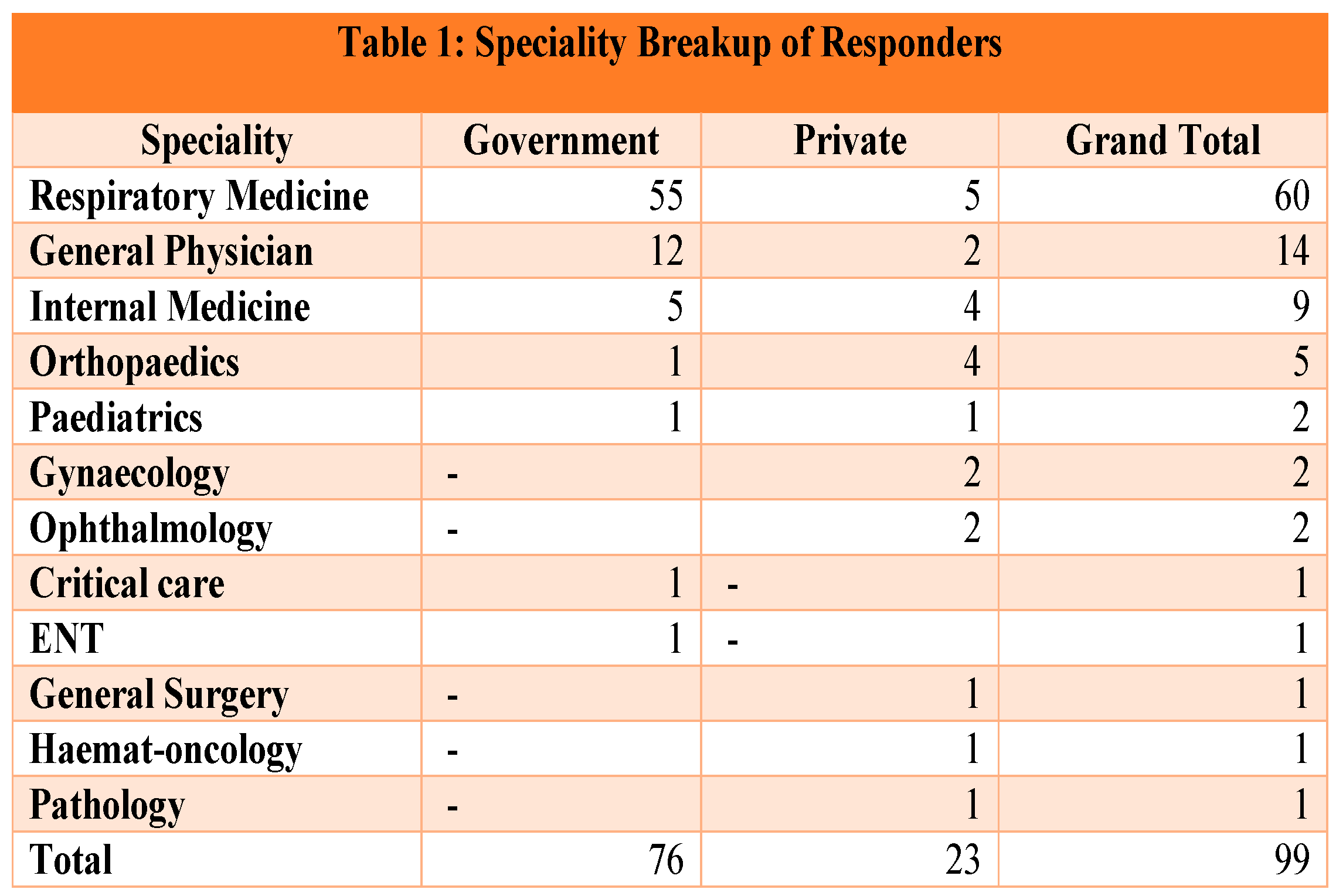
- 76.7% (76) and 23.3% (23) doctors were from the Government and private sector respectively.
RESULTS:
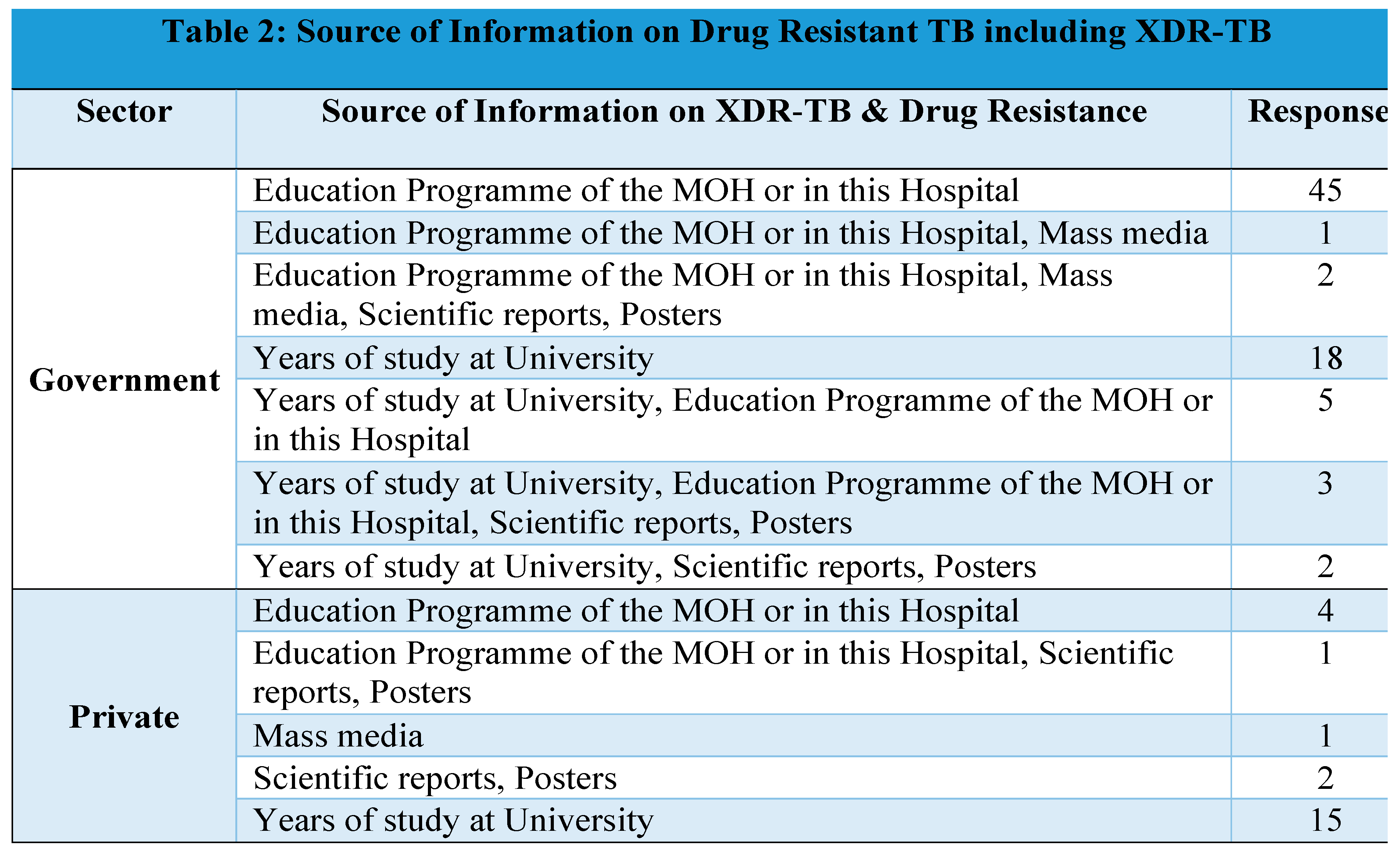
- Government doctors: Educational Program of MOH/ their hospitals
- Private doctors: Learnings at the University
- Drug resistant TB: its transmission and extent of problem
- Case definition/ diagnosis of drug resistant TB
- Treatment of drug resistant TB
- Infection control practices & XDR-TB
- A.
- DRUG RESISTANT TB: ITS TRANSMISSION AND EXTENT OF PROBLEM:
- Role of environment: The doctors uniformly agreed that there is a major role of environmental cleanliness and overcrowding in spreading XDR TB
-
Mode of Transmission: 56% believe XDR-TB spreads through droplet spread. 37% were of the opinion that XRD TB is an airborne infection.
- ○
- Government Doctors mainly said it is spread by droplet infection, whereas private sector doctor’s opinion was divided among the available options.
- ○
- Surprisingly 1/7th (14%) of the respondents also belive that it is spread through indirect contact or water borne.
- ○
- The variety of responses suggest lack of clarity regarding the mode of transmission espeically when it comes to multidrug resistant TB.
-
Role of improper medication:
- ○
-
Almost all the respondents correctly identified that improper intake of TB medication increases the risk of XDR-TB.

- 60% of the public sector and 83% of the private doctors believe that XDR-TB is not common in India.
-
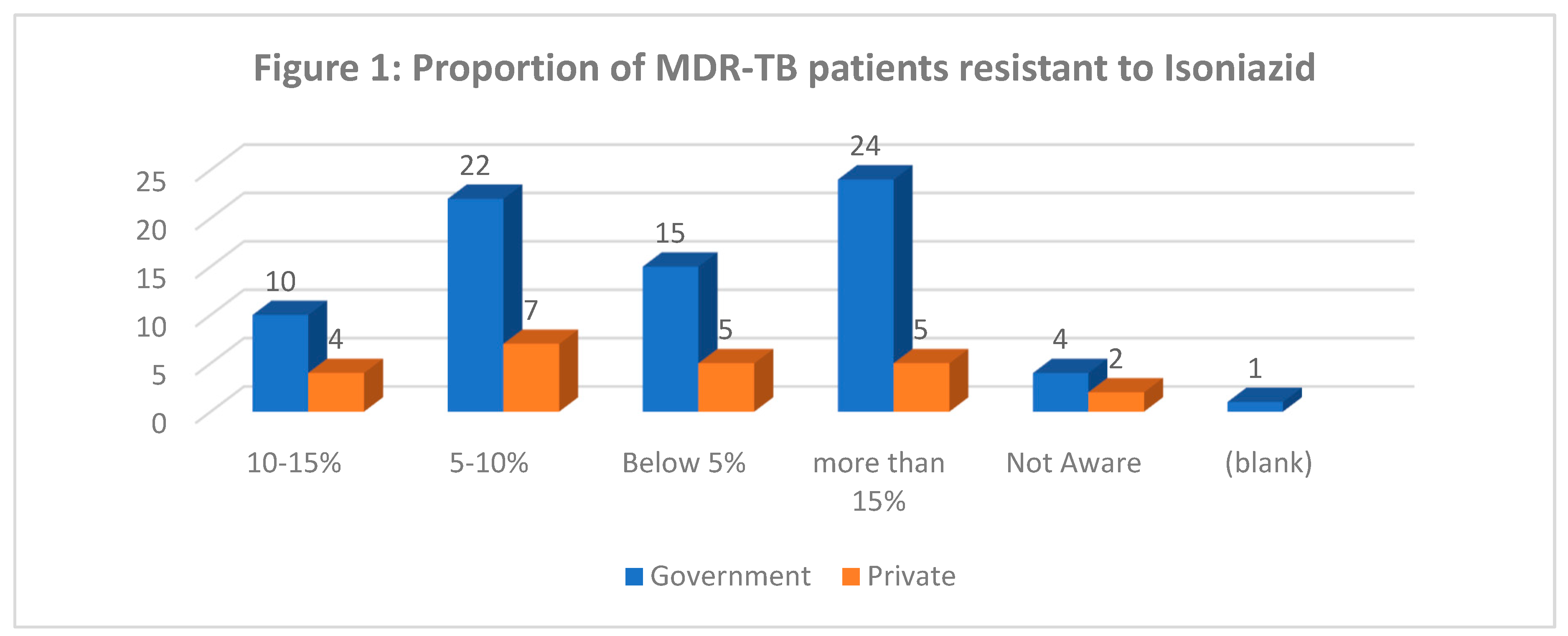
31 % Government doctors think that more than 15 % patients of MDR-TB patients are resistant to isoniazid, whereas 29% private doctors think only 5-10% MDR-TB patients are resistant to isoniazid (Figure 1)
- Nature of XDR-TB infections (Figure 3): 70% government doctors and 64% private doctors strongly agree that XDR-TB can cause serious infections disease that is fatal
-
Felt Need for Raising Awareness:
- ○
- Almost all the doctors (98% - 97/99) feel the need for increased awareness among the community regarding XDR-TB.
- ○
-
All the doctors felt the need for continuing medical education of practitioners on recent advances in the field of XDR-TB control.

- B.
- CASE DEFINITION/ DIAGNOSIS OF DUG RESISTANT TB:
-
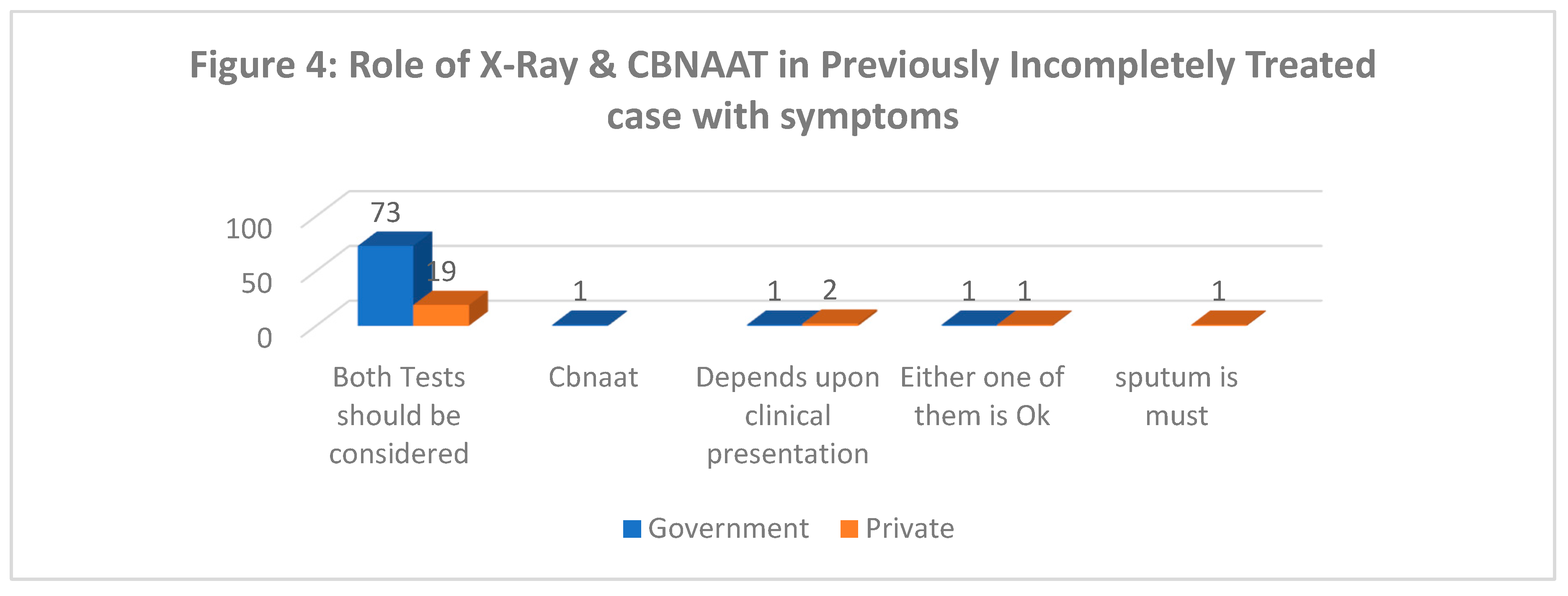
Role of X-Ray and CBNAAT in diagnosis of TB in a symptomatic patient of incompletely treated TB (Figure 4): 96% government and 79% private doctors think that X-ray has a supportive role in diagnosis of TB and that both X-Ray and CBNAAT should considered.
-
Case definition of XDR-TB:
- ○
- 84% of government and 96% private doctors were correctly able to identify the case definition of XDR-TB.
- ○
- Overall, 13% of doctors were unable to give correct case definition which could lead to missing of possible XDR suspect.
- ○
- Operational case definition used: Resistance to Rifampicin and Isoniazid, plus any Fluoroquinolone and at least one of three injectable second-line drugs i.e., Amikacin, Kanamycin, or Capreomycin
-
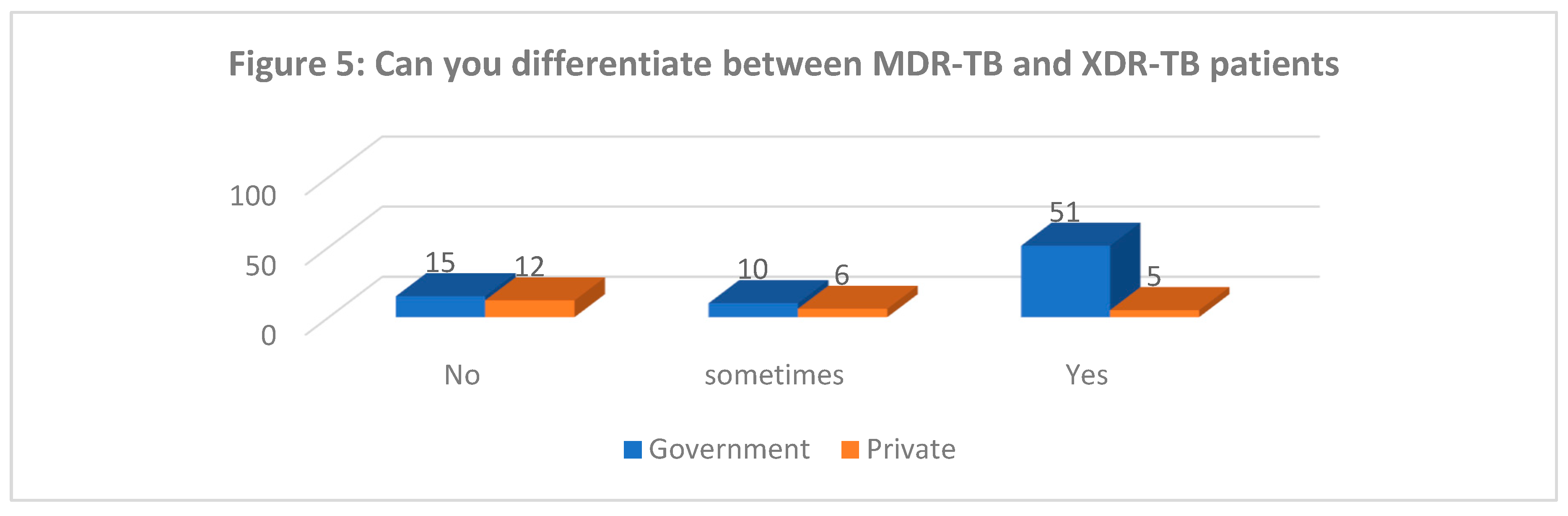
Differentiating between MDR and XDR TB (Figure 5): Majority of private doctors and almost 1/6th of government doctors felt they are unable to differentiate between MDR and XDR TB.
- Getting Cultures done for XDR Suspects: While all Government doctors were sending cultures for XDR suspects a small proportion (13%) of private practitioners even when suspecting XDR-TB do not send for cultures prior to treatment.
-
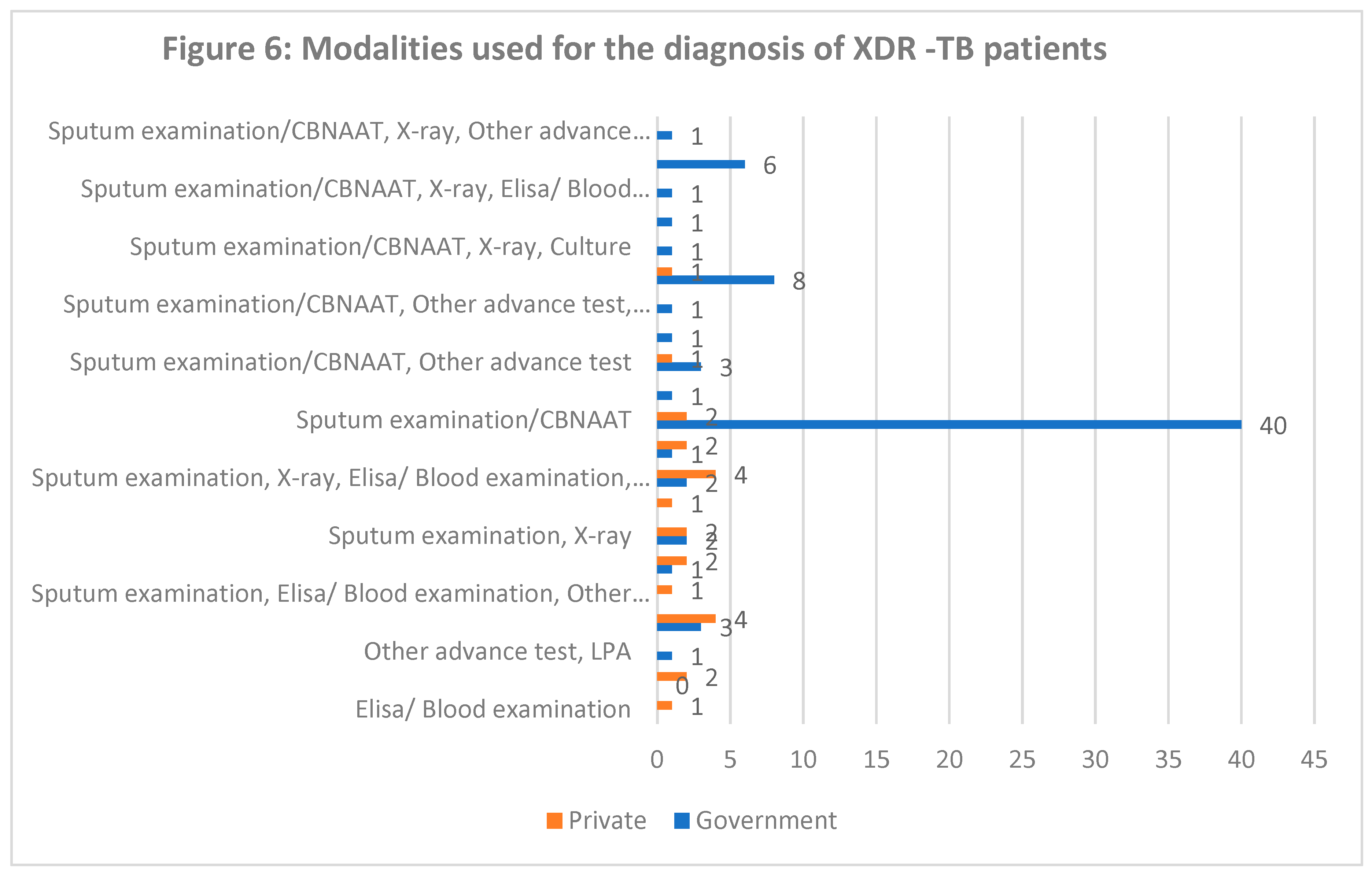
Diagnostics Used for XDR-TB (Figure 6): A Wide variation can be seen in the options for diagnosing XDR-TB with many limiting to Sputum examination, CBNAAT or even X-Ray. Only 1/3rd of the respondents identified advanced tests beyond these above tests for diagnosing XDR-TB.
- C.
- TREATMENT OF DRUG RESISTANT TB:
-
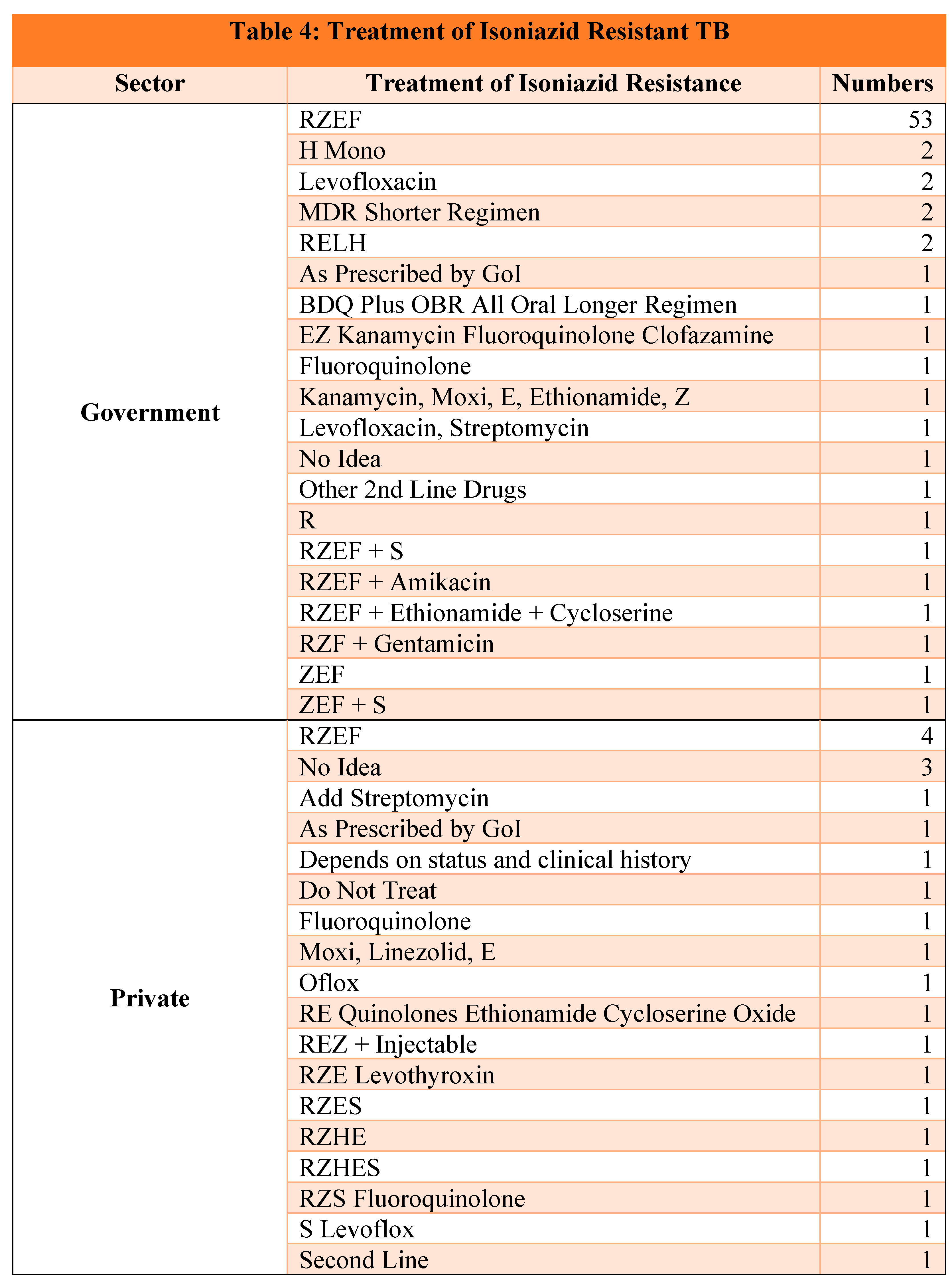
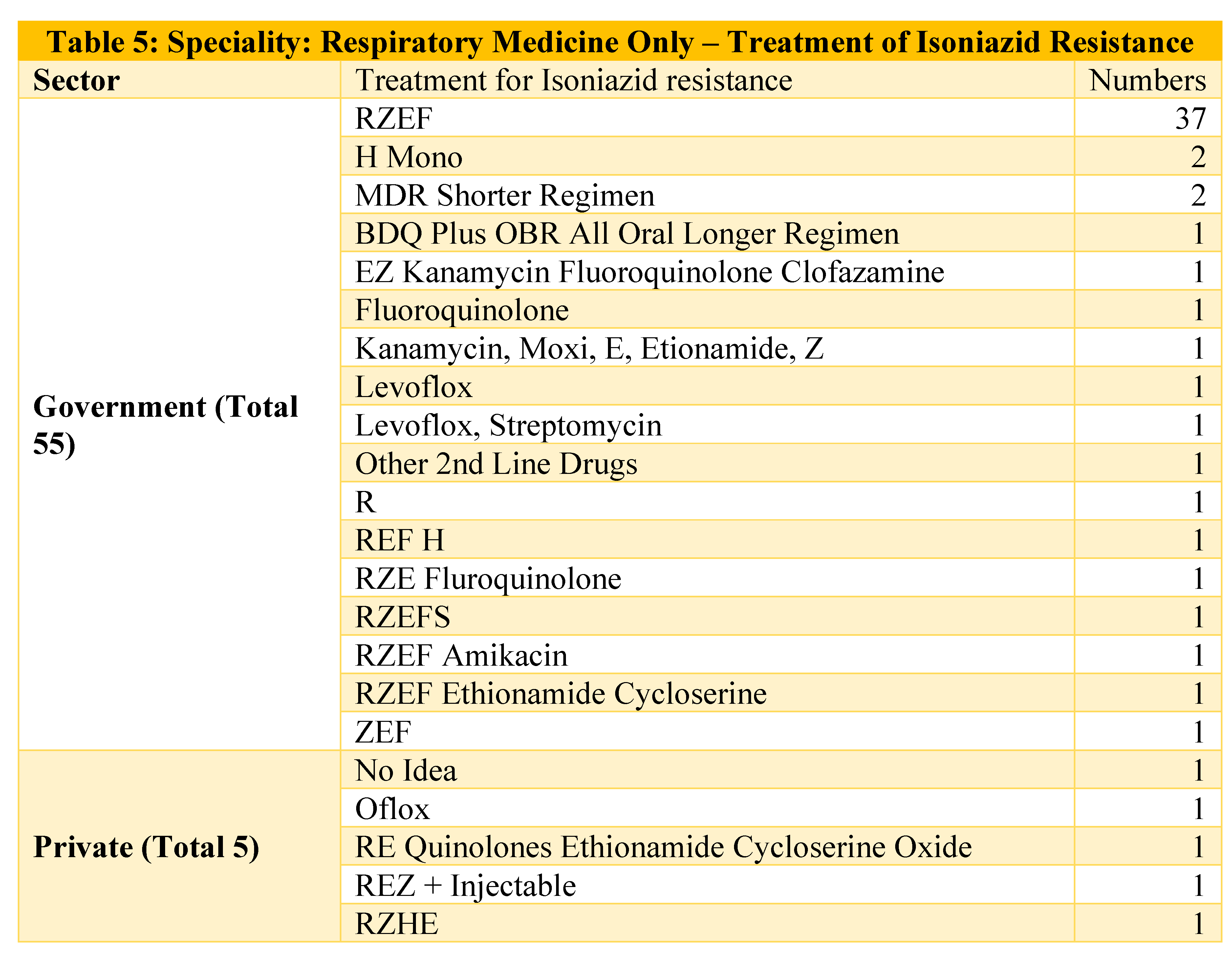
Treatment of Isoniazid Resistant TB (Table 4): On one hand 70% of the government doctors were able to correctly identify the combination of Rifampicin, Pyrazinamide, Ethambutol and Fluoroquinolone as the treatment of choice for Isoniazid resistant TB, on the other hand only 17% of private doctors were able to do so and there was a lot of variation in their treatment choices which is a clear indicator of low awareness regarding drug resistant TB treatment.
-
Even when we see the options given by Respiratory Medicine specialists we see a wide variation in the responses. (Table 5)
-
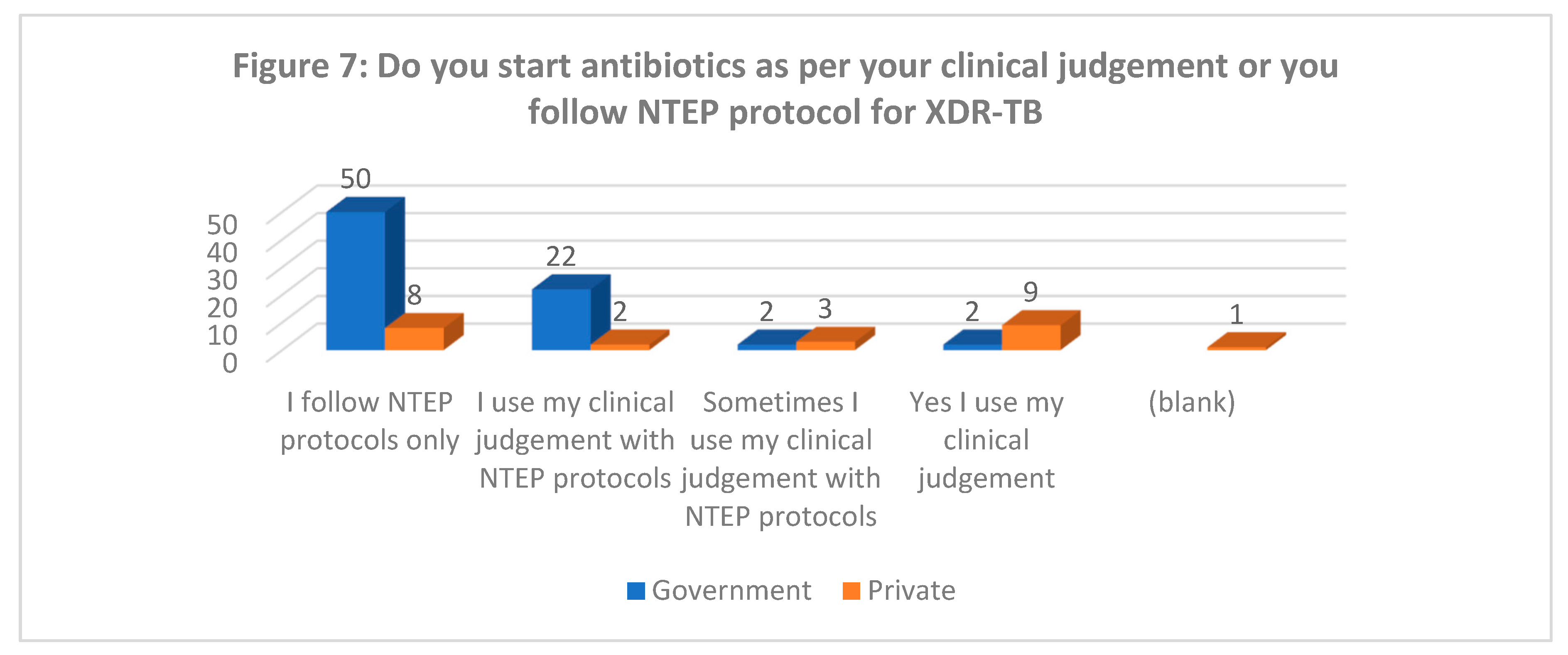
Whether following standardized regimen (Figure 7): Although majority (95%) of government doctors follow NTEP prescribed regimen for treating XDR-TB, the private doctors were divided in their treatment choices with almost similar (~40%) each following NTEP regimen or follow their own clinical judgement. This is similar to the various regimen found in various studies for treatment of TB [16].
-
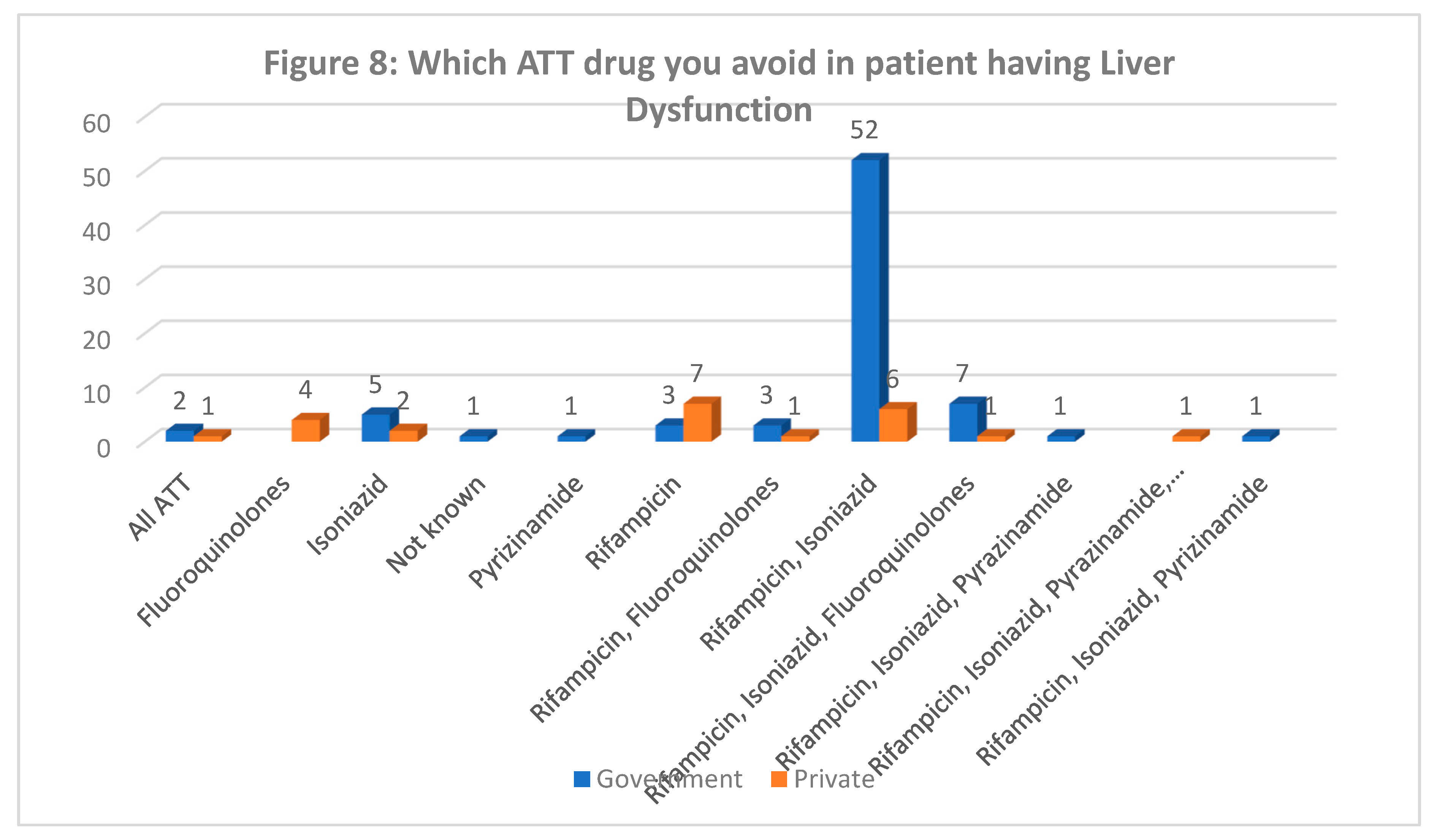
Drugs to be used in Liver Dysfunction (Figure 8): While 68% government doctors identified rifampicin and isoniazid to be avoided in liver dysfunction, the opinion was divided in the private sector doctors which points to reduced awareness among private doctors as compared to government doctors.
- D.
- INFECTION CONTROL PRACTICES & XDR-TB:
-
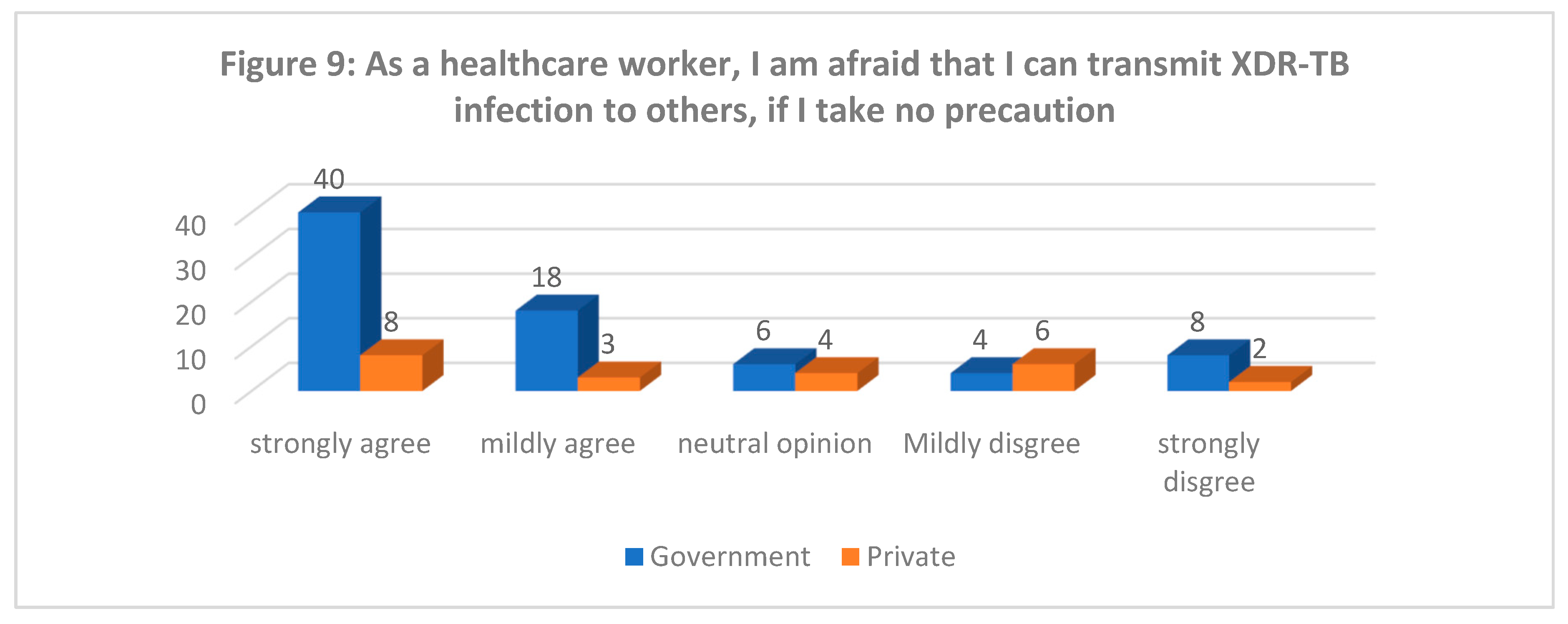
Risk as a Healthcare Worker (Figure 9): 53% government and 35% private doctors strongly agree that until they take precautions, they can transmit XDR infection to others.
- ○
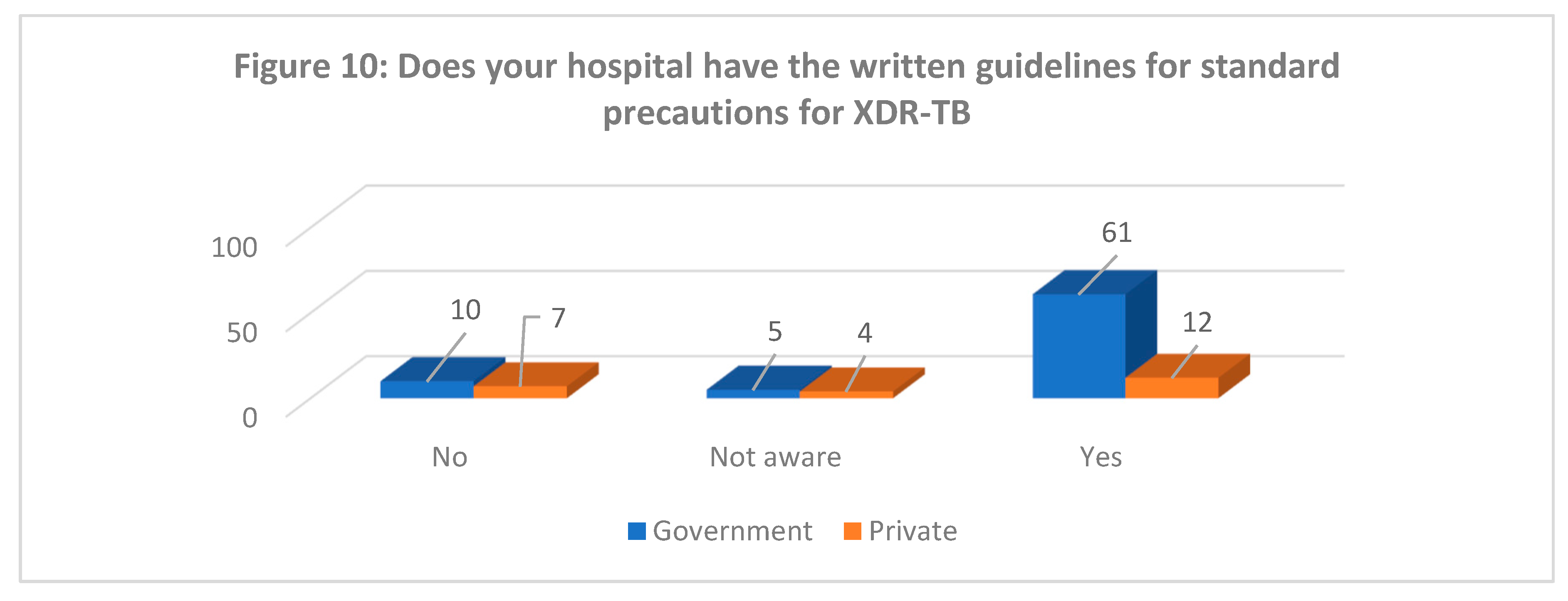
- Knowledge of Standard Guidelines for XDR-TB prevention: Majority (83%) of the Government and 57% of private doctors pointed out correctly the standard precautions to prevent transmission.
- ○
- Use of Personal Protective Equipment (PPE) while dealing with XDR (Figure 11): 61% and 54% of government and private doctors respectively informed regarding routinely using PPE while dealing with XDR patients.
- ○
-
Isolation of XDR-TB from other patients: While 91% of government doctors said they isolate XDR-TB patients, only 58% private doctors did so.

-
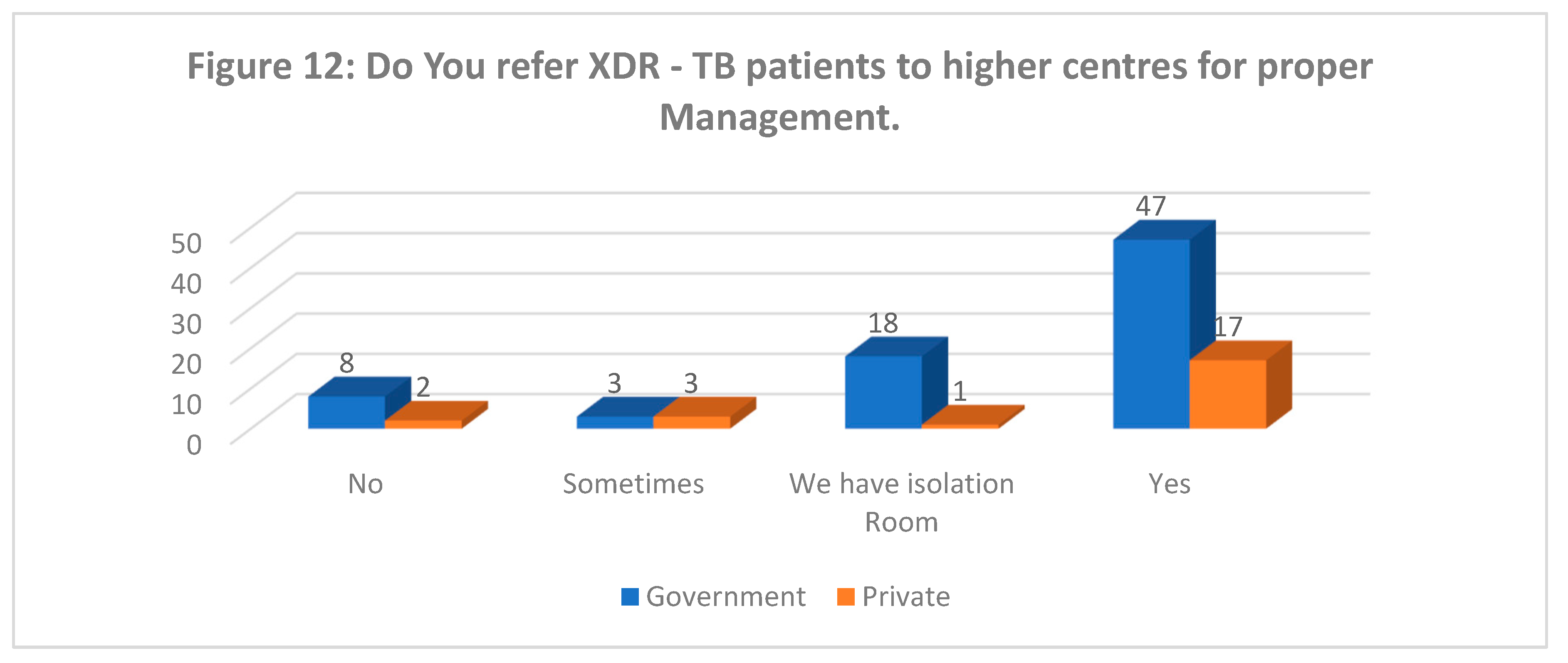
Referral to higher centre for management of XDR-TB (Figure 12): Despite understanding the risk associated with XDR-TB few doctors (10%) still do not refer these patients to higher centres for management even though they may not have isolation facilities available in their hospital.
DISCUSSION:
- A. Drug resistant TB: its transmission and extent of problem
- B. Case definition/ diagnosis of drug resistant TB
- C. Treatment of drug resistant TB
- D. Infection control practices & XDR-TB
CONCLUSION:
References
- Thakur G, Thakur S, Thakur H. Status and challenges for tuberculosis control in India - Stakeholders' perspective. Indian J Tuberc. 2021;68(3):334-339.
- Subbaraman R, Nathavitharana RR, Satyanarayana S, et al. The Tuberculosis Cascade of Care in India's Public Sector: A Systematic Review and Meta-analysis. PLoS Med. 2016;13(10):e1002149. Published 2016 Oct 25. [CrossRef]
- Prasad R, Singh A, Balasubramanian V, Gupta N. Extensively drug-resistant tuberculosis in India: Current evidence on diagnosis & management. Indian J Med Res. 2017;145(3):271-293.
- Dhamnetiya D, Patel P, Jha RP, Shri N, Singh M, Bhattacharyya K. Trends in incidence and mortality of tuberculosis in India over past three decades: a joinpoint and age-period-cohort analysis. BMC Pulm Med. 2021;21(1):375. Published 2021 Nov 16. [CrossRef]
- Schito M, Migliori GB, Fletcher HA, et al. Perspectives on Advances in Tuberculosis Diagnostics, Drugs, and Vaccines. Clin Infect Dis. 2015;61Suppl 3(Suppl 3):S102-S118. [CrossRef]
- Michael JS, John TJ. Extensively drug-resistant tuberculosis in India: a review. Indian J Med Res. 2012;136(4):599-604.
- Ryu YJ. Diagnosis of pulmonary tuberculosis: recent advances and diagnostic algorithms. Tuberc Respir Dis (Seoul). 2015;78(2):64-71. [CrossRef]
- Sachdeva K, Shrivastava T. CBNAAT: A Boon for Early Diagnosis of Tuberculosis-Head and Neck. Indian J Otolaryngol Head Neck Surg. 2018;70(4):572-577. [CrossRef]
- Che Y, Song Q, Yang T, Ping G, Yu M. Fluoroquinolone resistance in multidrug-resistant Mycobacterium tuberculosis independent of fluoroquinolone use. Eur Respir J. 2017;50(6):1701633. Published 2017 Dec 7.
- Paleckyte, A., Dissanayake, O., Mpagama, S. et al. Reducing the risk of tuberculosis transmission for HCWs in high incidence settings. Antimicrob Resist Infect Control 10, 106 (2021).
- Sharma SK, Jelly P, Bhadoria AS, Thakur K, Gawande K. Awareness and perception regarding tuberculosis among patients and their relatives attending a tertiary care hospital in Uttarakhand: A hospital-based exploratory survey. J Family Med Prim Care. 2020;9(3):1555-1561. Published 2020 Mar 26. [CrossRef]
- J. R. Andrews, N. S. Shah, N. Gandhi, T. Moll, and G. Friedland, “Multidrug-resistant and extensively drug-resistant tuberculosis: implications for the HIV epidemic and antiretroviral therapy rollout in South Africa,” Journal of Infectious Diseases, vol. 196, no. 3, pp. S482–S490, 2007.
- Steingart K, Schiller I, Horne D, Pai M, Boehme, CC, Dendukuri N. Xpert® MTB/RIF assay for pulmonary tuberculosis and rifampicin resistance in adults (Review). Cochrane Database Syst Rev 2014;(1).CD 009593.
- Migliori GB, Nardell E, Yedilbayev A, D’Ambrosio L, Centis R, Tadolini M, et al. Reducing tuberculosis transmission: a consensus document from the World Health Organization Regional Office for Europe. Eur Respir J 2019;53:1900391. [CrossRef]
- Schaberg T, Rebhan K, Lode H. Risk factors for side effects of isoniazid-rifampicin and pyrazinamide in patients hospitalized for pulmonary tuberculosis. Eur Respir J. 1996;9:2026–30.
- Zarir F. Udwadia, Lancelot M. Pinto, Mukund W. Uplekar. Tuberculosis Management by Private Practitioners in Mumbai, India: Has Anything Changed in Two Decades?; Plos One Published: August 9, 2010; https://. [CrossRef]
- TUBERCULOSIS CONTROL MEASURES IN URBAN INDIA STRENGTHENING DELIVERY OF COMPREHENSIVE PRIMARY HEALTH SERVICES. Ranjani Gopinath, Rajesh Bhatia, Sonalini Khetrapal, Sungsup Ra, and Giridhara R. Babu, No 80, December 2020; ADB SOUTH ASIA WORKING PAPER SERIES. (ADB: ASIAN DEVELOPMENT BANK).
- Global Tuberculosis Report 2020, World Health Organization.
- https://www.who.int/news-room/fact-sheets/detail/tuberculosis.
- India TB Report 2022, Ministry of Health and Family Welfare, Government of India.
- Tushar Sahasrabudhe, Tinku Joseph, Shailesh Meshram, Ankur Pathak. Awareness about MDR-TB in private medical practitioners of Pune City, European Respiratory Journal 2012 40: P2683.
- National Strategic Plan for Tuberculosis Elimination 2017-2025, Central TB Division, Ministry of Health & Family Welfare, Government of India.
- Manjula Kanakaraju, Sharath Burugina Nagaraja, Srinath Satyanarayana, Yella Ramesh Babu, Akshaya Kibballi Madhukeshwar, Somashekar Narasimhaiah, "Chest Radiography and Xpert MTB/RIF® Testing in Persons with Presumptive Pulmonary TB: Gaps and Challenges from a District in Karnataka, India", Tuberculosis Research and Treatment, vol. 2020, Article ID 5632810, 10 pages, 2020. [CrossRef]
- Ramya Ananthakrishnan, M. D'Arcy Richardson, Susan van den Hof, Radha Rangaswamy, Rajeswaran Thiagesan, Sheela Auguesteen and Netty Kamp. Successfully Engaging Private Providers to Improve Diagnosis, Notification, and Treatment of TB and Drug-Resistant TB: The EQUIP Public-Private Model in Chennai, India. Global Health: Science and Practice March 2019, 7(1):41-53. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).




