1. Introduction
Glaucoma is a group of optic neuropathies causing irreversible damage to the optic nerve that leads to progressive and permanent loss of vision and ultimately blindness. Elevated intraocular pressure (IOP) is the main risk factor for glaucoma; it is mostly caused by an impairment of the eye’s aqueous humor (AH) through the drainage structures. Primary open-angle glaucoma (POAG) is the most common type of glaucoma in the western countries and approximately half of glaucoma cases still remain undiagnosed. Early detection and treatment are crucial as they can slow or even stop the progression of the disease. Pharmacological treatment as eye drops is the most common way to treat glaucoma to reduce IOP by decreasing AH production or increasing its outflow. If IOP control is not achieved within a physiological range by pharmacological treatment or it causes excessive undesirable effects, the surgical option is considered. The objective of the surgery is to favor the filtration and drainage of the AH [
1]. The most commonly used initial surgical technique is filtering surgery (perforating or not) that seeks to create a fistula from the subconjunctival space towards the anterior chamber of the eye in order to promote the exit of AH through it and a decrease in IOP. Hence, AH is stored in the conjunctival filtration bleb, which is a subconjunctival reservoir, and the success of the surgery depends entirely on the degree of survival and proper functioning of the bleb [
2]. An excess of subconjunctival scarring in the postoperative period leads to an early surgery failure when the bleb is obliterated. To minimize post-surgical fibrosis, the usual intraoperative administration of antimetabolites (mitomycin C or 5 fluorouracil) acts by inhibiting the proliferation of fibroblasts present mainly in Tenon’s layer. However, these drugs can in turn cause complications such as ocular hypotony due to scleral impregnation or corneal toxicity by acting in a non-specific way [
3].
In certain patients, despite using antimetabolites, a marked profibrotic tendency is observed with early changes in the conjunctival filtration bleb, which raises suspicions of its early closure. The cause of this profibrotic tendency could have a double genetic and acquired component. Among the acquired causes would be the prolonged use of hypotensive eye drops containing preservatives like benzalkonium chloride (BAK), that cause long-term toxicity of the ocular surface and the use of topical prostaglandin analogs that cause chronic hyperemia. This chronic inflammatory infiltration, located in the conjunctival epithelium and connective tissue, increases the fibroblast population as well as collagen production causing bleb obliteration. This toxic effect has been confirmed through impression cytology, immunohistochemistry and in vivo confocal microscopy, and the intensity of these changes is related to the amount of preservative administered and the duration of treatment [
4]. Likewise, patients who have undergone repeated eye surgeries or with previous inflammation conditions such as uveitis show a greater tendency to develop fibrosis and scarring of the conjunctival filtration bleb. In patients with a high degree of preoperative inflammation, pre and postoperative measures should be intensified to prevent the fibrosis that leads to surgical failure. These actions would consist of withdrawing hypotensive drugs with preservatives, using preoperative topical anti-inflammatories to reduce the degree of conjunctival inflammation or increasing antimitotic treatment, among others [
5]. But, in some patients, in spite of following those preoperative measures to treat the ocular surface before surgery, a tendency towards early bleb fibrosis is observed. As a result, surgical failure occurs even if some postoperative maneuvers are performed like needling or subconjunctival injections of antimetabolites. Therefore, apart from the acquired profibrotic factors, it is suspected that the individual susceptibility to early fibrosis of the filtration bleb could be driven by changes in the conjunctival gene expression patterns. A prospective study comparing conjunctival gene expression at different time points after surgery revealed that
IL-8,
VEGF-A,
CDKN1A,
CDKN2A, and
TGF-α resulted upregulated while others such as
MMP2,
TGF-β2,
C-MYC,
CTGF, and
IL-18 were downregulated [
6]. Upregulation of the profibrotic
VEGF-A and downregulation of antifibrotic genes, including
IFN-b1,
IL-6,
F2, and
COL3A1 have been found in glaucoma patients with surgical failure in comparison with those with surgical success [
6]. Likewise, other genes have been found upregulated (
MYOCD and
IL-6) and downregulated (
PRG4,
CD34,
IL-33,
MMP-10,
WISP2, and
COL6A6) in fibrosis conjunctival fibroblasts versus non-fibrosis conjunctival fibroblasts from patients with previous glaucoma surgery and patients with no previous surgery, respectively [
7]. Interestingly, silencing of profibrotic genes has been effective in modulating fibroblast functions [
8], and reducing the healing rate [
9]; as a result, it may increase the survival of the conjunctival filtration bleb to improve long-term glaucoma surgery [
10].
In essence, scarring and fibrosis can be considered an overreach of the healing process. Wound healing is a dynamic physiological mechanism consisting of different overlapping phases activated after tissue damage from disease, injury, or surgery. The incision of glaucoma filtering surgery initially causes damage to conjunctiva and to surrounding blood vessels, which initiates the inflammatory phase. At this stage, the exposure of subendothelial collagen, the presence of extracellular matrix (ECM) material and the extravasation of plasma proteins activate homeostasis. It includes formation of platelet plug, activation of the coagulation cascade, and generation of the blood clot to maintain the integrity of the vasculature [
5,
11]. The inflammatory phase is characterized by the invasion of neutrophils, monocytes, and macrophages that release different growth factors including EGF, VEGF-A, TGF-β, PDGF, GM-CSF, and FGF and inflammatory cytokines such as IL-1, IL-6, IL-8, and TNF-α [
12,
13]. Some mediators are involved in the maintenance and subsequent activation of fibroblasts that play an essential role in the production of granulation tissue and angiogenesis during the proliferative phase [
14,
15]. Upon differentiation to contractile myofibroblasts, they also promote the production of collagen and other components of the ECM and, as a result, the contraction and the closure of the wound. The final stage of the remodeling phase consists of the transition between granulation tissue and scar tissue through selective degradation of the ECM and myofibroblasts apoptosis [
16,
17]. Dysregulation of this complex network of molecular pathways could contribute to the persistent presence of myofibroblasts and to abnormal ECM deposition that characterize the fibrotic response associated with numerous diseases [
18].
In this study, we have prospectively evaluated the local expression of a panel of genes potentially associated with the development of fibrosis, and the secreted proteins they encode. We analyzed a cohort of glaucoma patients who required more than one surgical intervention in a short period of time due to early surgery failure caused by conjunctival scarring, in order to define a hyperfibrosis genotype common to all of them. To do that, we have established the genotype-phenotype correlation between gene/protein expression and the clinical evolution of the patients towards the success or failure of surgery due to early fibrosis and closure of the filtration bleb. Knowing the altered profibrotic genetic profile of our patients may allow us to identify biomarkers of conjunctival fibrosis. Our ultimate goal is to detect cases at high risk of scarring that could compromise surgery and accordingly personalize the type of surgery offered.
3. Discussion
Conjunctival fibrosis of the filtering bleb is the result of an excessive wound healing response and one of the main causes of early failure of glaucoma surgery. Despite the strategies used to deal with the acquired factors that predispose to fibrosis including treatment with antimetabolites and preoperative ocular surface preparation, a number of patients develop early postoperative conjunctival fibrosis [
5]. Thus, the profibrotic tendency has a genetic origin that would explain why some patients, who
a priori do not present signs or risk factors leading to exaggerated healing, develop an inexorable scarring at the level of the subconjunctival space that ends in surgical failure. In recent years, the presence of genetic factors and variants have been identified in patients who present hyperfibrotic phenomena in different regions of the body [
19,
20]. These patients show a great tendency to exhibit hypertrophic or keloid-type scarring skin lesions and to suffer pathologies including glomerulosclerosis and sarcoidosis [
21,
22].
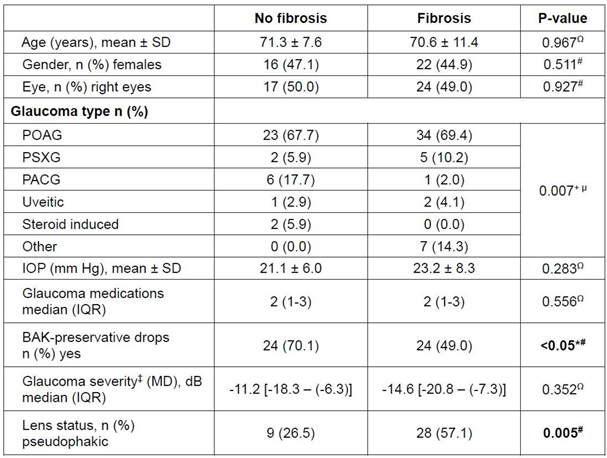
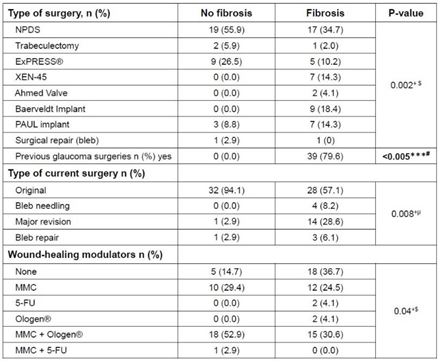
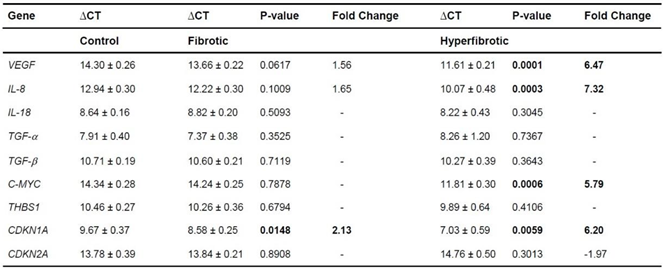
With this study we aim to contribute to identifying the genes involved in the development of conjunctival fibrosis. To do that, we quantified the expression levels of nine potentially relevant genes in fibrosis, in the conjunctiva (Tenon’s capsule) from glaucoma patients who underwent filtration surgery. Among them, we identified individuals with a clear hyperfibrosis phenotype, in whom surgery failed more than once in a short time, others with a fibrosis phenotype that had to be re-operated one time and with a slow fibrosis evolution, and those that did not present fibrosis and showed surgical success. Clinically, there were some statistically significant differences among patients with bleb fibrosis and the control (no fibrosis) group. Fibrosis patients presented a history of having previous glaucoma surgeries, need of more postoperative surgical maneuvers and the use of more wound healing modulator agents than the non-fibrosis patients. They showed more complex types of glaucoma such as the pseudoexfoliative one and required more aggressive surgeries like drainage device implantation as well. However, no differences were found regarding age, sex, eye laterality, preoperative IOP, glaucoma staging severity nor number of drugs in the preoperative hypotensive therapeutic regimen. Paradoxically, no fibrosis patients presented a significantly higher proportion of preoperative usage of BAK preserved drugs. This may be due to the fact that patients who have already had a decreased effect of their filtering surgery and need additional postoperative medication are treated more cautiously with drugs without BAK so as not to contribute to increasing conjunctival fibrosis and, with it, the complete failure of the bleb.
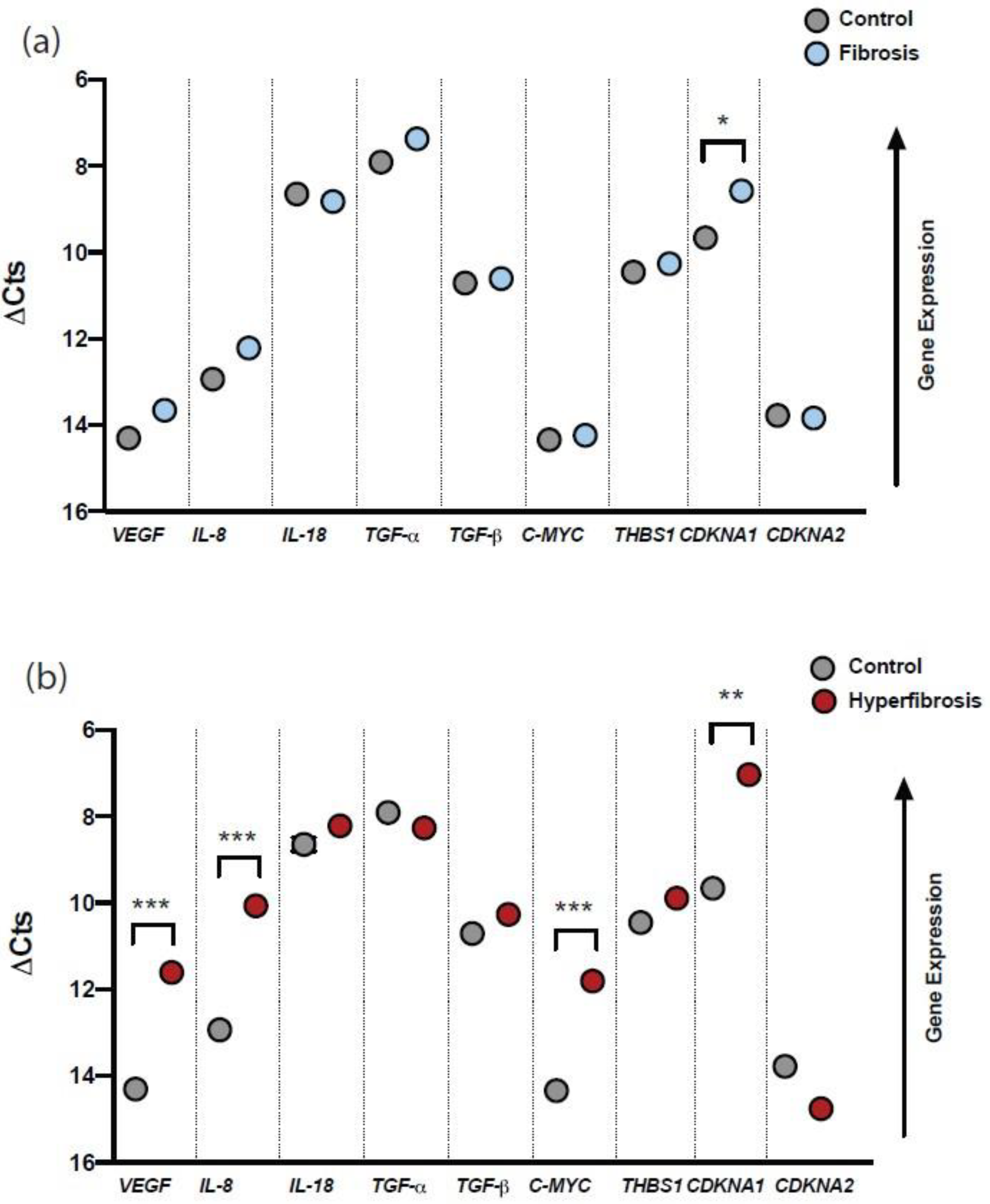
Recent studies revealed changes in conjunctival gene expression associated with the fibrosis after glaucoma filtration surgery. In a pivotal study, in which expression of 88 genes previously associated with wound healing were quantified in the conjunctiva of glaucoma patients, significant differences were found in 29 genes at an early stage after glaucoma surgery, 20 genes in the next 90 - 180 days, and 2 genes one year after surgery. During the postoperative period (15 days),
IL-8,
VEGF-A,
CDKN2A,
CDKN1A, and
TGF-α were the most upregulated genes while others like
IL-18 and
C-MYC were downregulated. Instead, at 90 days after surgery, a noteworthy number of genes such as
HIF1A,
EGFR,
C-MYC,
TGF-β1,
TGF-β2,
BCL2,
MMP2 and
PDGF, among others, were downregulated. One year after surgery, however, only the expression of
TGF-β1 and
ITG-β3 was reduced. And, in peripheral blood, the most evident changes occurred also during the first 15 days after surgery, when 12 genes (
IL-1β,
CEBPD,
HIF-1α,
ITG-β2,
TNFRSF1A and
CASP1, among others) were induced [
6]. These results suggested that conjunctival fibrosis developed after filtration surgery could have a significant genetic component driven by an altered expression of specific genes. In addition, positive regulation of many of the fibrosis-related genes seem to occur in the first few days after surgery. In our study,
VEGF-A and
IL-8, in conjunction with
CDKN1A, were the most upregulated genes in fibrosis patients. Interestingly, these changes were much more pronounced in patients with hyperfibrosis in whom
VEGF-A,
IL-8,
CDKN1A and
C-MYC were significantly induced. Therefore, this altered expression pattern may be relevant in the progression of fibrosis and the surgical outcome in glaucoma. More patients should be analyzed to corroborate whether the degree of the upregulation of these genes could be related to the severity of conjunctival fibrosis.
Likewise, a previous correspondence analysis revealed
VEGF-A as the only tested gene differentially expressed in the patients with surgical failure versus patients with successful surgery [
6]. VEGF-A is a glycoprotein highly expressed in acute wounds [
23] that has been involved in many processes linked to wound healing repair. It increases the rate of proliferation [
24] and migration [
25] of endothelial cells and promotes wound angiogenesis [
26] and formation of lymphatic vessels [
27]. Several studies have reported a reduction in vascularity and fibrosis during the wound healing process by neutralization of VEGF-A [
28]. Hence, anti-VEGF-A monoclonal antibodies (bevacizumab) reduce proliferation of cultured Tenon fibroblast, collagen deposition and angiogenesis in a rabbit model of trabeculectomy, improving surgical outcome [
29]. Pilot studies have also shown that the administration of bevacizumab decreases IOP in patients with neovascular glaucoma [
30]. Similarly to
VEGF-A, the chemokine
IL-8 is upregulated in the acute phase of wound healing [
31]. It plays a key role in neutrophils and T-lymphocytes chemotaxis in the inflammatory response [
32]. IL-8 also increases proliferation and migration of endothelial cells as well as wound angiogenesis [
33,
34]. Our results, in the same line as those of others [
6], show that overexpression of
VEGF-A and
IL-8 could be used as an indicator of conjunctival fibrosis following filtering surgery.
Our data also revealed an obvious dysregulation of
C-MYC and
CDKN1A expression in the conjunctiva of glaucoma patients with hyperfibrosis. Both genes, involved in the cell cycle control, were found significantly overexpressed.
CDKN1A was previously reported to be upregulated in the conjunctiva during the postoperative period of filtering surgery, although the expression of
C-MYC was reduced [
6]. It is known that the
C-MYC oncogene promotes cell growth by counteracting the action of several negative regulators of the cell cycle [
35,
36] such as
CDKN1A in a
TGF-β-dependent manner [
37]. Consistently, downregulation of
C-MYC with specific antisense RNA decreases progression of cell cycle [
38]. Interestingly, several studies suggested that the C-MYC protein could be used as a molecular marker of impaired healing in chronic wounds [
39]. On the other hand,
CDKN1A encodes for the p21 protein, a cyclin-dependent kinase inhibitor, that has been associated with cell cycle arrest. Induction of p21 inhibits cell proliferation and reduces the progression of some tumors [
40]. Thus, upregulation of
CDKN1A in the conjunctiva could be part of a response mechanism to counteract fibrosis. In addition to elevated expressions of
CDKN1A in fibrotic tissues [
41], genetic variants of
CDKN1A have been also identified associated with a greater risk of suffering from idiopathic pulmonary fibrosis [
39].
As other profibrotic genes,
TGF-β1 is abundantly expressed during wound healing where it seems to be involved in all stages. It stimulates fibroblasts activation, the synthesis and deposition of collagen I and fibronectin, in addition to the formation of granulation tissue [
42]. At lower concentrations, it has been described that TGF-β1 induces proliferation and migration of fibroblasts from Tenon’s capsule [
43] and its transformation to myofibroblasts [
44,
45]. Its potent ability to enhance inflammation, angiogenesis and collagen production have placed it as one of the key factors in the pathophysiology of ocular fibrosis [
46]. Although we did not find changes in
TGF-β1 expression in the conjunctiva of patients with hyperfibrosis, it could perform its function in the response to wound healing. It is important to point out that, when
TGF-β1 is induced it stimulates the expression of
CTGF that plays an essential function in the scarring response.
CTGF is highly expressed in some fibrotic tissues [
13] enhancing proliferation and differentiation of Tenon’s capsule fibroblasts and promoting the deposition of extracellular matrix (ECM) components [
47]. In our hands, we could not amplify
CTFG in conjunctiva tissue samples from patients without fibrosis, probably due to its low expression. We focused our investigation in a very specific panel of genes representative of the different phases of the fibrotic response in the maximum number of glaucoma patients. Thus, we quantified genes coding for different inflammatory cytokines (
IL-8,
IL-18), growth factors (
VEGF-A,
TGF-α,
TGF-β), proteins involved in cell cycle control (
C-MYC,
CDKN1A,
CDKN2A) and tissue repair (
THBS1). In another study, in which a panel of one hundred genes was examined, a distinct group of differentially expressed genes was identified in fibrotic conjunctival fibroblasts from glaucoma patients with previous surgery versus non-fibrotic fibroblasts from patients without previous surgery. The authors found
MYOCD,
LMO3,
IL-6, and
RELB significantly upregulated and
PRG4,
CD34,
IL-33,
MMP-10,
WISP2,
COL6A6, and
IGFBP5 markedly downregulated in fibrotic fibroblasts. This definitely broadened the list of genes potentially associated with the development of post-surgery conjunctival fibrosis and supports inflammation, ECM remodeling, smooth muscle contraction and oncogene expression as biological pathways underlying the fibrotic process [
7].
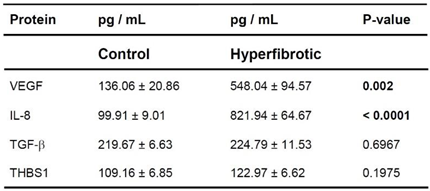
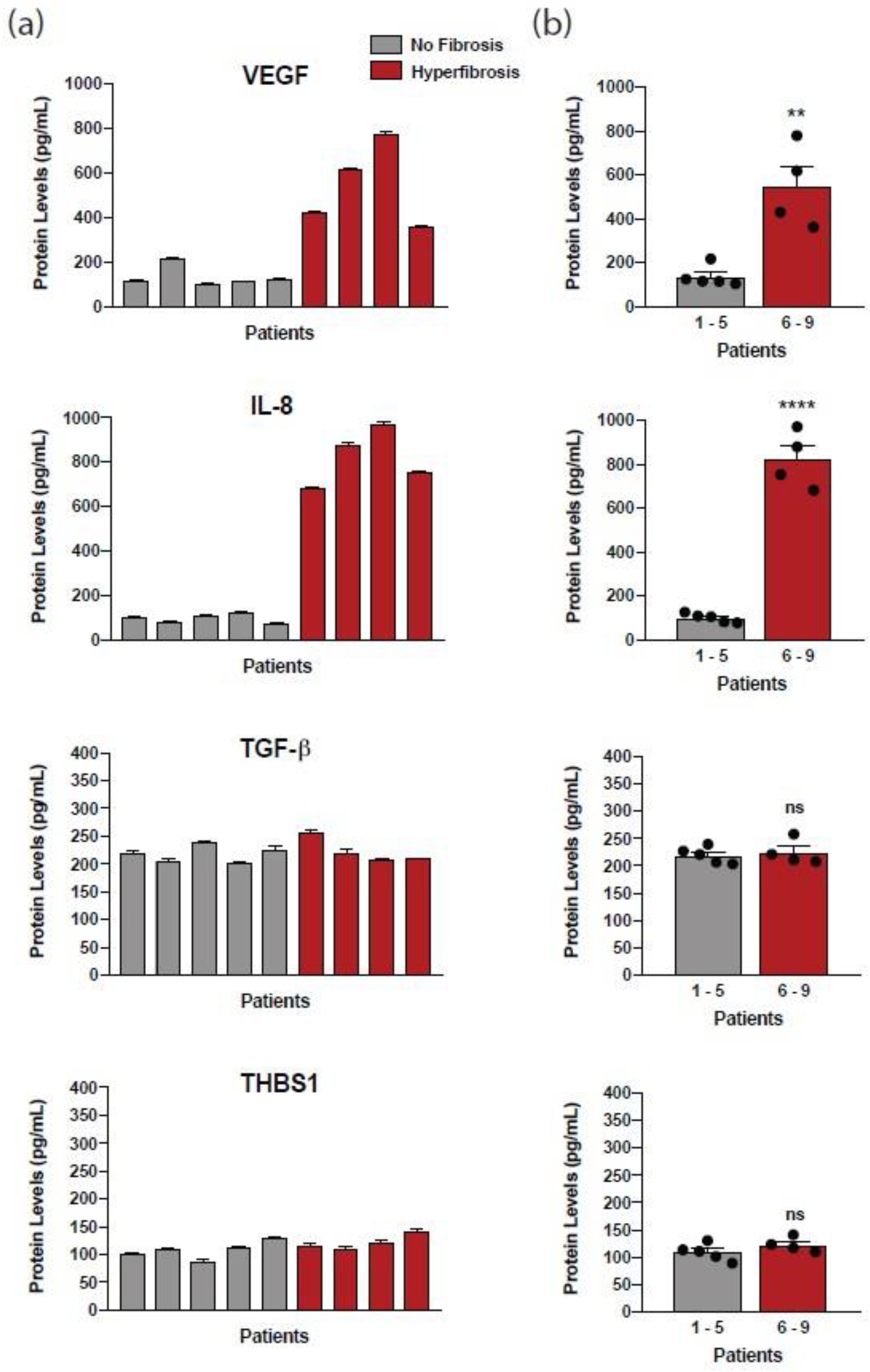
In order to correlate the altered gene expression profile in fibrosis with protein levels, we quantified VEGF-A, IL-8, TGF-β, and THBS1 in the supernatants of cultured fibroblasts from patients. As in gene expression, and despite individual differences, we found a significant increase of secreted VEGF-A and IL-8 in fibroblasts of patients with hyperfibrosis versus control patients. In contrast, we did not find significant changes in TGF-β and THBS1 as occurred with the genes coding these proteins. Although there is strong evidence for using mRNA quantification to determine the relative importance of genes in a given process [
48], it is convenient to corroborate gene expression changes by measuring protein levels. Given that after a filtering surgery the AH is drained to the subconjunctival tissue, quantification of specific proteins associated with fibrosis in the AH could be crucial to identify patients at risk of surgical failure. Indeed, high levels of IL-8, VEGF-A, PDGF, TGF-β, and TGF-α have been found in AH of glaucoma patients [
49,
50]. Because VEGF-A neutralization with bevacizumab reduced excessive scarring after glaucoma surgery [
29], elevated protein levels of VEGF-A in the AH could be a useful indicator of poor surgical outcome in patients. At present, it is possible to quantify protein levels in tears in non-invasive procedures and the tear protein profile is being studied for the diagnosis of uveitis [
51] and dry eye [
52]. The identification of a valid profibrotic marker in tears or by impression cytology in the preoperative period could help us to personalize the surgical treatment of our patients, to choose a non-filtering procedure in those with a high risk of early fibrosis or to adjust the dose and the type of antimetabolites used.
In this study, our objective was to shed light on the identification of crucial genes in the development of conjunctival fibrosis in order to find potential biomarkers, useful for its diagnosis and treatment. We believe that, one important contribution of our study was the careful ocular surface preparation in the preoperative period in order to eliminate the bias of the preoperative inflammation that is closely linked with postoperative fibrosis and can
per se trigger the expression of profibrotic conjunctival gene expression by itself. Under the same conditions, we are recruiting glaucoma patients with different results from filtering surgery to collect tear samples. In the near future, we intend to quantify fibrosis markers with techniques that allow us to test a large number of patients. Finally, it is noteworthy that gene silencing of distinct profibrotic agents has been found effective in decreasing the healing rate of the postoperative filtration bleb [
53]. A further understanding of the cellular and molecular basis of ocular scarring would contribute to the design of new pharmacological treatments and gene-based therapies for conjunctival fibrosis.
4. Materials and Methods
4.1. Patients
We included 88 conjunctival tissue samples from 86 individuals (n=34 control, n=3 cataracts, n=41 fibrosis, and n=8 hyperfibrosis), of which 38 (44.2%) were females and 48 were males, with a mean age of 70.9 ± 10.0 years. Patients were recruited from the Institut Clínic d’Oftalmologia (ICOF) at Hospital Clínic de Barcelona, Innova Ocular-ICO, and Hospital de Viladecans (Barcelona, Spain). All analyzed patients were scheduled for glaucoma surgery alone or in combination with cataract surgery except three patients who had only cataract surgery and not glaucoma (patients 3-5, in whom protein levels were quantified). As it is our routine practice, all patients underwent preoperative ocular surface preparation with one or more of the following steps according to the degree of ocular surface disease present. Patients were treated with topical anti-inflammatory treatment (mild steroids, cyclosporine, ectoine), artificial tears with hyaluronate acid, palpebral hygiene and the use of topical hypotensive drugs with preservatives was substituted by its preservative-free counterparts at least two weeks before surgery. Besides, prostaglandin analogs were withdrawn one or two weeks before surgery if possible, and in some cases oral carbonic anhydrase inhibitors were administered.
The exclusion criteria were patients affected by any kind of active intraocular inflammation such as chronic uveitis, history of severe ocular comorbidities or several previous interventions (retinal, corneal pathologies and surgeries among others) that could increase greatly the likelihood of glaucoma surgical failure. Clinically, patients were classified into three groups after surgery according to the degree of surgical failure caused by the presence of early conjunctival fibrosis. It was diagnosed by slit lamp evaluation of the patient, optical coherence tomography (OCT) testing of the conjunctival bleb and finding an inadequate level of IOP that required secondary surgical procedures due to bleb fibrosis.
4.2. Experimental Groups
Glaucoma patients were classified into three experimental groups: control, fibrosis and hyperfibrosis patients. Control patients had successfully undergone a single glaucoma surgery, as they did not develop conjunctival fibrosis at least during the first year of follow-up. Patients were considered as no fibrosis patients if they presented a favorable postoperative evolution with no morphologic nor tomographic signs of bleb fibrosis (diffuse, non-vascularized bleb, presence of microcysts, etc.). On the other hand, the fibrosis group presented signs of bleb fibrosis (flattened, corkscrew vessels, Tenon cyst, etc.) from the first postoperative month onwards that led to failure of glaucoma surgery and had to be re-operated after the first postoperative month. Finally, the hyperfibrosis group of patients included those who showed signs of surgical failure due to early bleb scarring before the first postoperative month and needed one or more surgical maneuvers/re-interventions in a short period of time. We quantified conjunctival gene expression (n=32 control, n=41 fibrosis, and n=6 hyperfibrosis) and protein levels from supernatants of primary cultures of patient’s fibroblast (n=2 control, n=3 cataract, and n=4 hyperfibrosis). Two glaucoma patients with hyperfibrosis could be analyzed by PCR and ELISA, and they are counted in both groups. For the demographic statistical analysis, the hyperfibrosis patients were included in the fibrosis group (
Table 1).
4.3. Study Design
We conducted a prospective, interventional study of the wound-healing gene expression and protein expression profile of 86 different patients who underwent glaucoma surgery and three cataract patients (
Table 1). The analysis included the correlation of the conjunctival expression of genes and proteins potentially associated with conjunctival fibrosis (until one year or more after the intervention), and the success or failure of the surgery. Patients affected with medically uncontrolled glaucoma or with a previous filtering glaucoma procedure were scheduled for glaucoma surgery and, after receiving preoperative ocular surface preparation (described above), they were operated with different glaucoma techniques according to the characteristics of their glaucoma (
Table 2). From each patient, a single conjunctival tissue sample was collected during the glaucoma operation, performed by two surgeons (EM, NV-A) who used identical pre- and post-operative protocols and surgical techniques.
Clinical data of the patients were recorded preoperatively, intraoperatively and at each follow-up visit (24h, 1 week, 1, 3, 6 months, and 1 year) in order to detect early bleb fibrosis. Data were collected from the complete preoperative ophthalmological examination that included visual acuity using Snellen optotypes; refraction with auto-refractometer; intraocular pressure by Goldmann applanation tonometer; ultrasound pachymetry; gonioscopy with a gonioscopy lens; fundus by direct visualization of the optic disc and retinography with a non-mydriatic camera; visual field with Sita Standard 24-2 protocol with Humphrey perimeter; Optical coherence tomography of the Cirrus optic nerve and ganglion cell layer. The number and duration of previous ocular hypotensive agents as well as the history of previous ocular pathologies and interventions were collected. An assessment of the ocular surface status by slit lamp examination and the presence of dry eye disease (corneal fluorescein staining according to Oxford scale, Schirmer test, break up time) were performed in order to determine the type and quantity of preoperative ocular surface preparation needed in each case.
Regarding the surgical data, the type of intervention performed, the prostheses used, the need for the use of antimetabolite drugs, their dose and concentration, the existence of per-operative complications such as excessive bleeding, tissue fragility, etc. were annotated. At each postoperative control visit, a complete ophthalmological examination was carried out with the tests mentioned above, and, in particular, a photograph of the filtration bleb with the anterior pole camera and an examination of its internal structure by means of optical coherence tomography. Swept-Source (Triton, Topcon Healthcare) was used in order to anticipate early conjunctival failure as early as possible. If signs of early failure of the conjunctival bleb were observed, post-operative maneuvers were carried out to inhibit or decrease fibrosis at this level such as subconjunctival punctures of antimetabolites (5-fluorouracil or mitomycin C), needlings with a 30 G needle in the slit lamp or in the operating room, surgical revisions of the bleb or new surgeries with a matrix implant of subconjunctival collagen Ologen® (Equipsa, Madrid, Spain).
4.4. Sample Collection and Primary Cell Cultures
During each intervention, a block of conjunctival and Tenon tissue with a surface area of 2x2 mm was obtained from glaucoma patients. Tissues intended to study local gene expression by quantitative real-time PCR were maintained in RNAlater® (Invitrogen, ThermoFisher Scientific) at room temperature for two days to stabilize RNA until extraction. For protein quantification in supernatants from cultured fibroblasts, tissue samples were kept in complete low glucose DMEM supplemented with 20% FBS, 100 mg/mL, L-glutamine, 100 U.I./mL penicillin and 100 μg/mL streptomycin for a maximum of 2 h until primary cell cultures were performed. Conjunctival fibroblasts were obtained using the explant method. Briefly, tissue was cut into small pieces, carefully attached to the bottom of a 35-mm dish, and covered with the same DMEM medium under a glass coverslip. Dishes were incubated in a humidified 5% CO2 atmosphere at 37°C and the medium was changed every other day. Cells were allowed to grow at confluence from the explant for a period of 2 weeks. Fibroblasts were passaged with Trypsin-EDTA to a T-25 flask, and were maintained in the same medium with 10% FBS. Cell supernatants were collected on day 7 of this first passage. All reagents were obtained from Sigma (Madrid, Spain).
4.5. RNA Extraction and Reverse Transcription Reaction
Total RNA extraction was conducted with the NucleoSpin RNA from Macherey-Nagel (Düren, Germany). Reverse transcription reactions to generate cDNA were carried out with spectrophotometrically measured RNA (300 ng, Nanodrop, Thermo Fisher Scientific, Waltham, MA) using the SuperScriptTM IV First-Strand Synthesis System (Invitrogen, Thermo Fisher Scientific) according the manufacturer’s recommendations.
4.6. Gene Primers
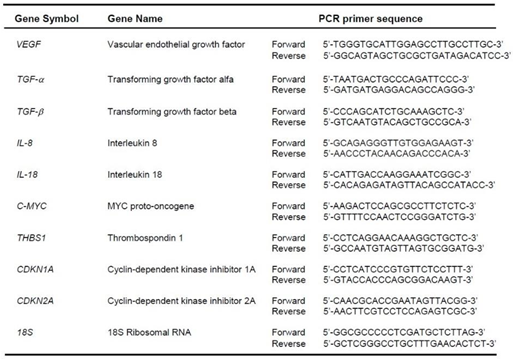
Primer sets for fibrosis-related genes as well as the ribosomal 18S RNA were designed using the Primer Designing Tool of the National Center for Biotechnology Information (NCBI) and purchased from Invitrogen (ThermoFisher Scientific) (
Table 5). Target specificity was obtained by performing Basic Local Alignment Search Tool (BLAST) comparisons against the entire nucleotide database (
http://www.ncbi.nlm.nih.gov).
Table 5.
Analyzed genes and PCR primer sequences.
Table 5.
Analyzed genes and PCR primer sequences.
4.7. Quantitative Real-Time PCR
Normalized mRNA quantification was performed by relative quantitative real-time PCR technology with Fast SYBR™ Green Master Mix using an ABI Prism® 7500 Fast Real-Time PCR System and the 7500 System SDS software (Applied Biosystems, ThermoFisher Scientific). Melting curves were carried out to determine melting temperatures in order to check the specificity of the amplified products. All experiments were performed by triplicate. Results are shown as ΔCT; therefore, values are inversely proportional to expression levels. Fold changes between fibrosis/hyperfibrosis versus control samples were calculated by the formula 2−ΔΔCT, where CT is the cycle at threshold (automatic measurement), ΔCT is CT of the assayed gene minus CT of the endogenous control (18S rRNA), and ΔΔCT is the ΔCT of the normalized assayed gene in the fibrosis / hyperfibrosis samples minus the ΔCT of the same gene in the control one (calibrator). RQ values >1 correspond to increased fold changes. RQ values <1 correspond to a fraction of the gene expression and were converted to decreased fold changes by the formula −1/2−ΔΔCT.
4.8. Protein Quantification by ELISA
VEGF-A, IL-8, TGF-β1 and THBS proteins were determined in cell supernatants using Human ELISA assays (catalog numbers KHG0111, KHC0081, BMS249-4, EHTHBS1, respectively, Invitrogen, ThermoFisher Scientific). Collected DMEM from fibroblast’s cultures were centrifuged at 18,000 g for 5 min at 4°C and preserved at -80°C until quantification. The absorbance was measured at a wavelength of 450 nm using a Spark® multimode microplate reader (Tecan, Männedorf, Switzerland). Two independent experiments with two biological replicates each were performed. All ELISA experiments were carried out according to the manufacturer’s protocols by one technologist.
4.9. Statistical Analysis
The Shapiro-Wilk test was used to determine the normality of the distribution. The baseline characteristics were described using the mean ± standard deviation (SD), or the median (interquartile range) for quantitative data, and number (percentage) for categorical variables. Different groups were compared using either independent t-test or Mann-Whitney U test for continuous variables, and χ2 and Fisher’s exact test for categorical variables as appropriate. In multiple comparisons with significant results, post hoc analysis with Bonferroni’s correction was applied after pairwise comparison Gene and protein quantification data was presented as the mean ± standard error of the mean (SEM). For all tests, statistical significance was set at two-tailed P value and 95% confidence interval, *p < 0.05, **p < 0.01, and ***p < 0.001). Statistical tests were performed with GraphPad Prism 9.0 software (GraphPad Software, San Diego, CA) and Stata v14.1 (StataCorp, College Station, TX).
Appendix A
Gene names (in alphabetical order)
BCL2 BCL2 apoptosis regulator
CASP1 Caspase 1
CD34 CD34 molecule
CDKN1A Cyclin dependent kinase inhibitor 1A
CDKN2A Cyclin dependent kinase inhibitor 2A
CEBPD CCAAT enhancer binding protein delta
C-MYC MYC binding protein
COL3A1 Collagen type III alpha 1 chain
COL6A6 Collagen type VI alpha 6 chain
CTGF Connective tissue growth factor
EGF Epidermal growth factor
EGFR Epidermal growth factor receptor
FGF Fibroblast growth factor 1
F2 Coagulation factor II, thrombin
GM-CSF Colony stimulating factor 2
HIF-1α MIR31 host gene
IFN-b1 Interferon epsilon beta 1
IGFBP5 Insulin like growth factor binding protein 5
IL-1 Interleukin 1
IL-1β Interleukin 1 beta
IL-6 Interleukin 6
IL-8 Interleukin 8
IL-18 Interleukin 18
IL-33 Interleukin 33
ITG-β2 Integrin subunit beta 2
ITG-β3 Integrin subunit beta 3
LMO3 LIM domain only 3
MMP-2 Matrix metallopeptidase 2
MMP-10 Matrix metallopeptidase 10
MYOCD Myocardin
PDGF Platelet derived growth factor subunit A
PRG4 Proteoglycan 4
RELB RELB proto-oncogene, NF-kB subunit
TGF-α Transforming growth factor alpha
TGF-β Transforming growth factor beta
TGF-β2 Transforming growth factor beta 2
THBS1 Thrombospondin 1
TNFRSF1A TNF receptor superfamily member 1A
VEGF-A Vascular endothelial growth factor A
WISP2 CCN5 Cellular communication network factor 5