1. Introduction
Osteoporosis is a condition associated with increased bone demineralisation that is becoming more prevalent as the population ages.[
1] Osteoporosis-related vertebral fractures (OVF) may lead to a reduction in quality of life comparable to diabetes.[2, 3] These injuries negatively affect patients' life expectancy and the amount of fracture-related deaths is comparable to and in Hungary even exceeds that of lung cancer, diabetes and chronic lower respiratory disease.[2, 4] In the European Union, 22 million women and 5.5 million men had osteoporosis in 2010, resulting in 520,000 new cases of OVF each year.[
5] OVF mostly happen due to banal, low-impact trauma.[6, 7] The clinical picture is distinctive; these fractures occur mostly in patients over 50 years old and are particularly common in postmenopausal women.[
8] In contrast to hip fractures, 90% of which are caused by falls, only 10-33% of vertebral fractures happen due to falls or other high-energy impacts, and banal activities cause most OVF: bending, stretching and lifting a light object.[9-12] In clinical practice, we use several systems to classify compression fractures to assess their severity and outcome.[13-18] Patients with severe fractures have a longer recovery time and a higher risk of neurological deficits.[19, 20]
In clinical practice, conservative medical management of vertebral fractures is always associated with bed rest and immobilization. Bedridden living reduces the function of all organ systems to varying degrees.[21-24] These effects may be more pronounced in elderly patients with poor recovery. Bone mineral density (BMD) decreases by approximately 2% per week, a particularly adverse consequence for OVF patients.[
21] Muscle strength decreases by 1-3% daily, which translates into a 10-15% decrease per week. This represents a loss of almost half of normal muscle strength in 3-5 weeks of immobilization.[
22] The lack of exercise and bedriddenness combined with pain also reduces muscle strength in the respiratory muscles and respiratory support muscles, resulting in an overall reduction in respiratory capacity of up to 25-50%.[
23] Mucociliary clearance and phlegm accumulation due to decreased cough efficiency may be associated with the development of pneumonia.[
24] Depending on the duration of immobilisation, the recovery of ventricular function may take 20-72 days.[
22]
One possibility to accelerate the rehabilitation of unstable fractures is to stabilize the fractured spinal segment with screw fixation. The main aim of surgical treatment is to stabilize the unstable structure and prevent the development or progression of neurological deficits. Several surgical techniques are available, the most common is posterior pedicle screw fixation. This method, which can be performed minimally invasively, is considered a routine treatment for OVF worldwide. The instrumentation must involve as few segments as possible to reduce the load on the adjacent vertebral bodies and the risk of disc degeneration. In short-segment stabilization, only adjacent intact segments are affected.[25-27]
Percutaneous vertebroplasty is a tool to reduce pain and stop further compression in subacute and chronic fractures.[28-30] In addition, vertebral augmentation procedures appear to be associated with prolonged patient survival, according to a study of a large number of Medicare patients in the USA.[31-33] A small number of case-control studies are available on the impact of stabilization and PVP on the survival of elderly spinal fracture patients.[
34] However, the protocol for the surgical treatment of spinal fractures varies worldwide, with more than 96% of AO A3 fractures being surgically stabilized in Germany compared to only 41% in the Netherlands.[
35] Patients with functionally stable compression fractures can begin rehabilitation earlier. This study aimed to investigate the impact of these procedures on the survival of osteoporotic patients with fragility fractures due to low-energy trauma.
2. Materials and Methods
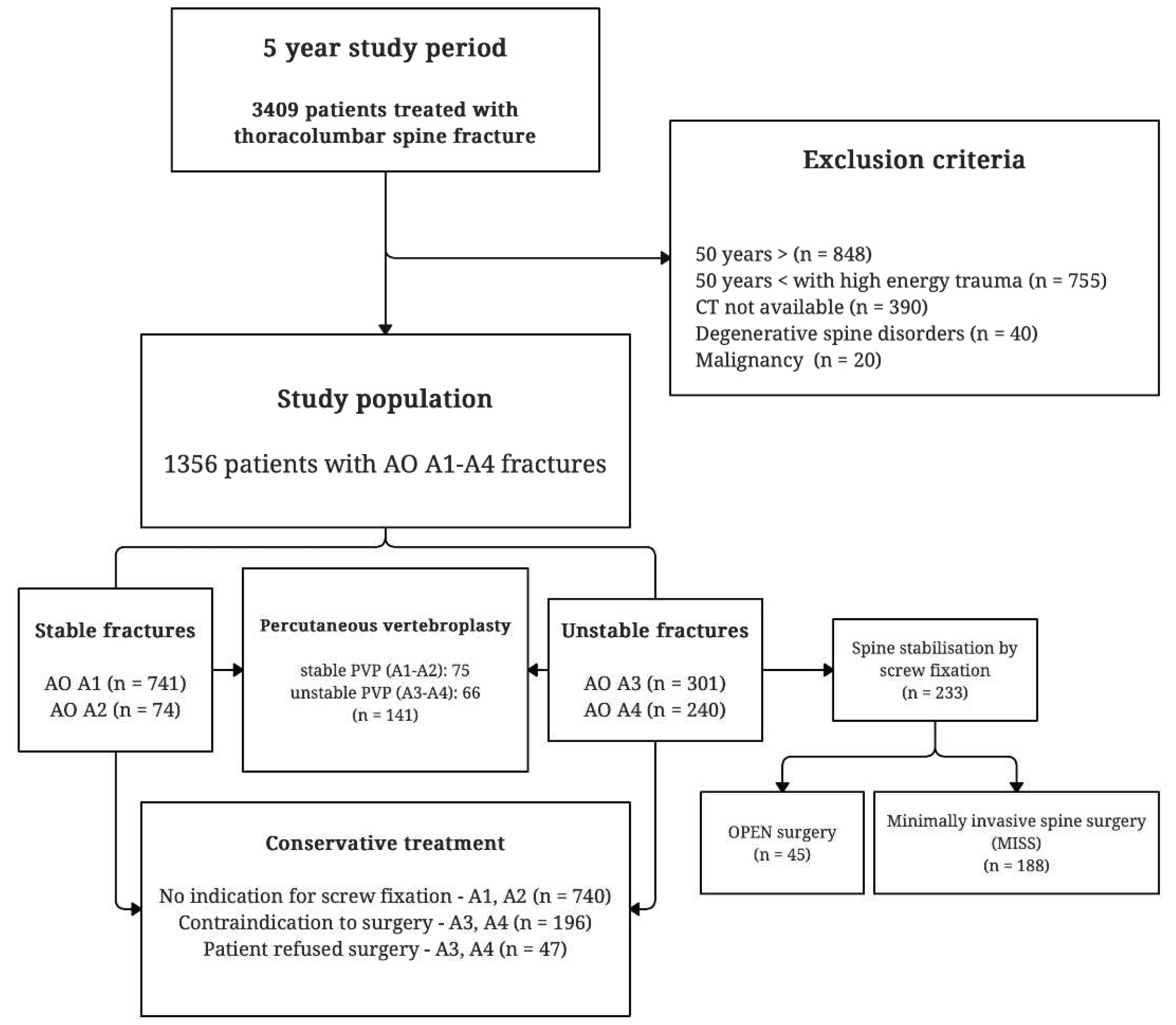
In this retrospective study, we analyzed the clinical data of 3409 patients treated for thoracolumbar vertebral fractures in the largest trauma center in Hungary between November 2014 and October 2019. Each patient's follow-up period began when the CT scan confirmed fracture. The follow-up period lasted at least one year from CT confirmation for conservatively treated patients, and at least one year after surgery for surgically treated patients. The time of death of the patients during the follow-up period was determined based on data from the National Health Insurance Fund of Hungary. The severity of fractures was determined using hospital documentation and CT scans. Fractures were categorized using the AO Spine Classification System. The AO system divides fractures into groups based on morphological features.[
36] These fracture subgroups differ in severity, clinical signs, and outcomes.[37, 38] This study aimed to investigate spontaneous fractures and fractures caused by low-energy impact. As bone mineral density values were not available for all patients, we inferred the osteoporotic status based on the circumstances of injury, age and radiographic features.[
39] The inclusion criteria for the study were: age over 50 years, low-impact trauma or spontaneous, and AO A1-A4 compression type fracture. The exclusion criteria were the absence of CT, malignancy in medical history before and during the follow-up period, and degenerative spine pathologies, such as ankylosing spondylitis and diffuse idiopathic skeletal hyperosteosis (
Figure 1). The CT scan is not sensitive enough to determine whether a fracture is unstable or stable in idiopathic skeletal hyperosteosis and ankylosing spondylitis, requiring an additional MRI scan.[40, 41] A total of 2053 patients were excluded:848 patients were younger than 50 years old, 755 patients older than 50 years sustained high-energy trauma (such as car accidents or falls from heights), 40 patients due to degenerative spinal diseases, 20 patients due to malignancy, and 390 patients had no available high-resolution CT scan; therefore, it was not possible to determine the AO Spine severity (
Figure 1). As all AO B- and C-type fractures fell into one of the excluded groups, 1356 patients with type A1-A4 compression fractures were included in the final study population.
The handling of data in our study conforms to the European General Data Protection Regulation (GDPR). After reviewing the study design, the Ethics Committee of our hospital provided consent for this retrospective study.
Fractures of type A1-A2 were considered to be functionally stable. The risk of developing neurological deficits was low. In the case of unstable A3-A4 fractures, there is an elevated risk of neurological deficit due to the involvement of the spinal canal and immobilization caused by excessive pain. Stable AO A1-A2 fractures were treated conservatively or with PVP surgery in cases in which patients reported a visual analog scale (VAS) score of > 3/10 pain for weeks into conservative care. Conservative care was defined as the use of an external brace and adequate pain management with physiotherapy. All unstable A3-A4 fractures were stabilized by screw fixation if the patient consented to surgical care, and there were no contraindications to such procedures (
Figure 1). Some patients with unstable fractures do not consent to surgery. Most patients with unstable fractures who received conservative treatment were deemed unfit for surgery by anesthesiologists. PVP surgery was performed when an unstable fracture was discovered as an inveterate fracture with a fresh A1-A2 component, causing unremitting pain (unstable PVP group). (
Figure 1).
The study period coincided with the introduction of minimally invasive spinal stabilization at the trauma center. Patients requiring screw fixation were operated on with the open surgical technique during the first two years of the study period (November 2014 to October 2016) and solely with the minimally invasive (MISS) technique during the last two years (November 2017 – October 2019). Open and minimally invasive surgeries were performed in the third year, between November 2016 and October 2017. These surgeries were performed by the same staff in the same environment, and the characteristics of the patient population were homogenous during these five years. We compared the accessibility to surgical screw fixation in the first and last two years assuming no other difference in the underlying population compared to the surgical technique.
The survival probabilities of the OPEN versus MISS surgery groups (Model 1) and conservatively treated stable fracture patients versus unstable fracture subgroups (Model 2) were compared using Cox proportional hazard models. As predictors, the stabilization technique type was used in Model 1, whereas fracture type and treatment modality were used in Model 2. A logistic regression model was fitted to the data (with a log link function) to assess the probability of being operated during the OPEN versus MISS periods (model 3). We used the treatment modality (conservative versus stabilization) as the outcome variable and treatment during the OPEN or MISS period as predictors. We also controlled for the effect of predictors of age, sex (all models), and days to treatment (in cube root transformed scale; Models 1 and 2) as possible confounders. No relevant and significant interaction or nonlinearity was detected; therefore, it was not included in the final models. Statistical analyses were performed using the R (R Core Team 2021) and, survival (Therneau, 2023) and survminer (Kassambara 2021) packages.
3. Results
A total of 3409 thoracolumbar fracture patients were treated in our hospital ward during the five years included in the study. Among these patients, 1356 (39.8%) met the inclusion criteria. The study group included 1071 women (79%) and 285 men (21%) with a mean age of 74.5 (SD = 10.5) (
Table 1). This extreme disproportionality of sex distribution is not unusual in the literature of osteoporotic fractures.[
1] Vertebral fractures were identified as compression fractures of the AO A1 (n=741), AO A2 (n=73), AO A3 (n=301), and AO A4 (n=241) types. Surgical treatments included percutaneous vertebroplasty in 141 patients and transpedicular screw fixation in 233 patients. The median times of hospitalization for unstable (AO A3-A4) and stable (AO A1-A2) fracture patients were 4 (IQR, 5) days and 2 (IQR, 3) days, respectively. The median hospitalization time for the entire dataset was 3 days (IQR, 2).
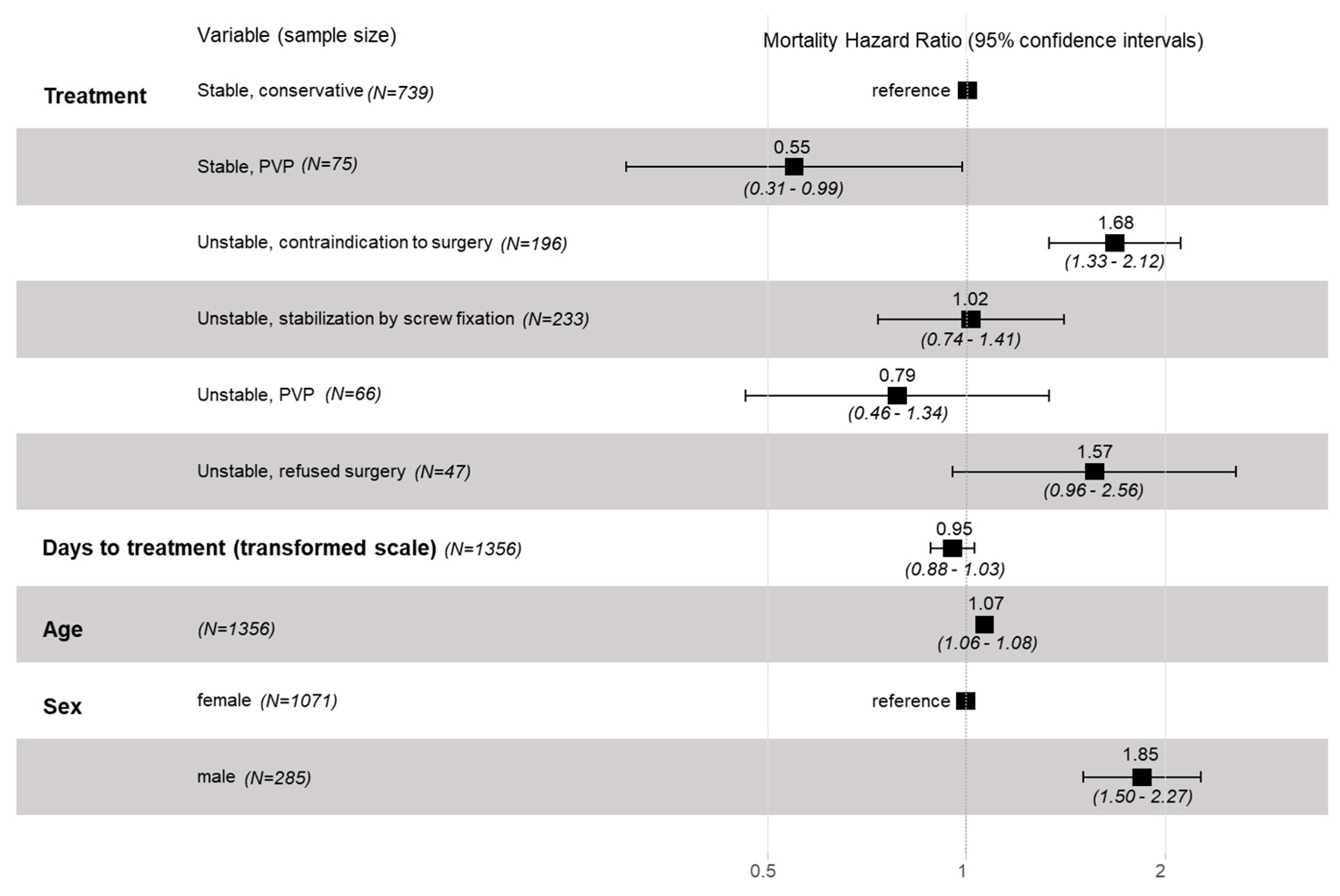
The unstable (A3-A4) fracture group accounted for 542 patients: 233 (43%) fractures were stabilized with screw fixation, 66 (12%) patients underwent PVP surgery, and 243 (45%) patients received conservative care:196 (36%) received conservative care because of contraindications to surgery or general anesthesia, and 47 (9%) patients refused screw fixation surgery despite being physically eligible for operative care. We compared the mortality hazard ratios (HRs) of each subgroup with stable and conservatively treated fractures. In the case of stable fractures, the MHR following PVP treatment was 0.55 (CI 0.31 to 0.99; P=.05). In the case of unstable fractures, patients treated conservatively due to contraindication to surgery had an MHR of 1.68 (CI 1.33 to 2.12; P<.001). Unstable fracture patients who refused surgery had an MHR of 1.57 (CI 0.96 to 2.56; P=.08). After stabilisation by transpedicular screw fixation, unstable fracture patients had an MHR of 1.02 (CI 0.74 to 1.41; P>.91), nearly identical to the stable group (
Figure 2). Regardless of the treatment modality, male patients had a significantly higher MHR of 1.85 (CI 1.50 to 2.27; P<.001) than female patients. After correcting for multiplicity (Dunnett’s method), the statistical decision only differed between the stable PVP group and the reference stable conservative group; the difference in mortality was not significant (P=.17).
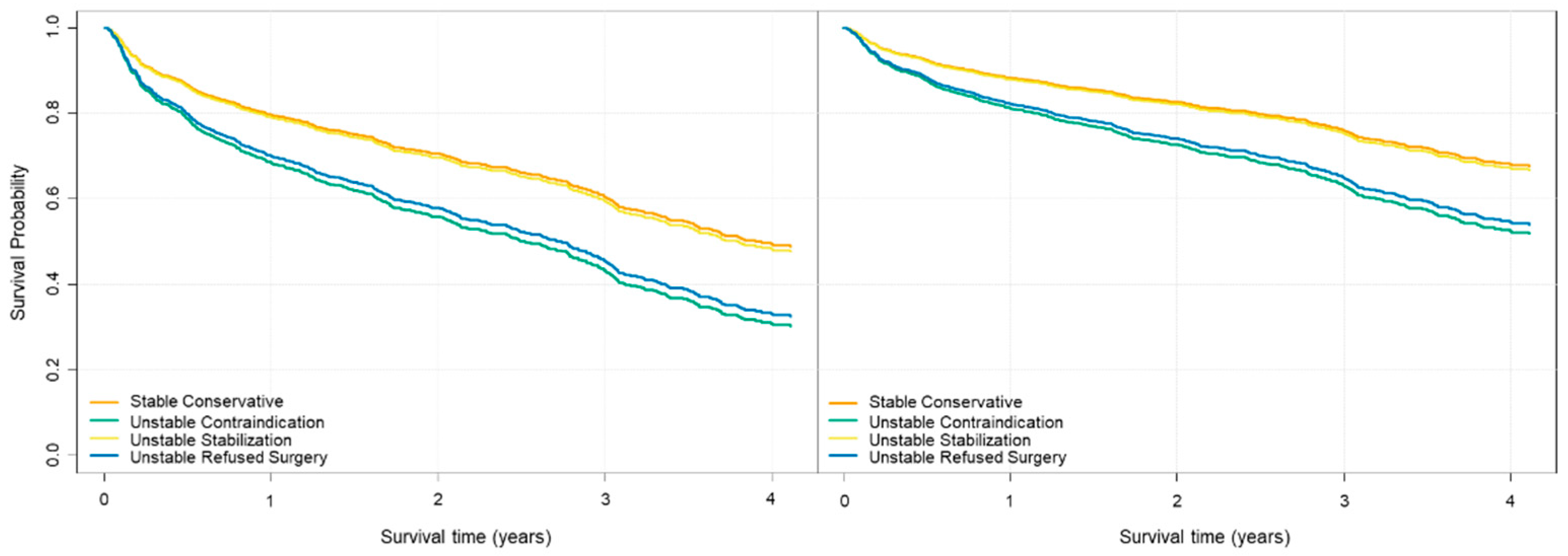
Cox model-based survival curves showed that the survival of patients with stabilized unstable fractures was nearly identical to that of patients with stable fractures. In contrast, the conservatively treated unstable group had clinically relevant lower long-term survival rates (
Figure 3).
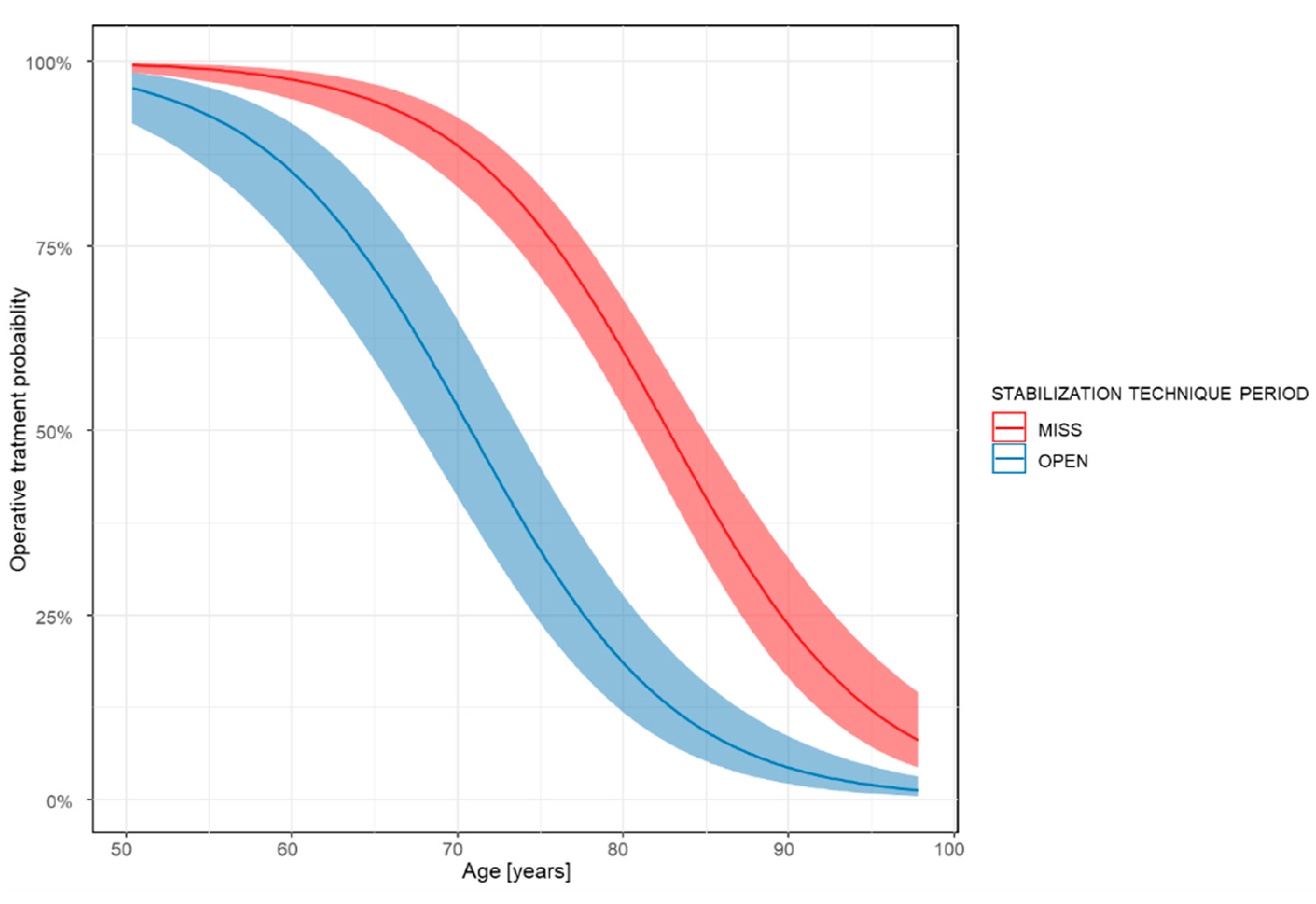
Regarding the comparison of the surgical screw fixation techniques, we found that in the first two years (OPEN period), we treated 124 patients with unstable A3-A4 fractures and 45 (36%) could receive surgical screw fixation. In the last two years of the observation period (MISS period), we treated 288 patients with unstable thoracolumbar fractures, and 188 (65%) underwent surgical screw fixation. The average age of operated patients was 67.44 (SD = 9.07) years for OPEN and 72.24 (SD = 8.76) years for MISS. Age (OR 0.87; CI 0.82 to 0.88; P<.001) and, more importantly, the stabilization technique (OR 0.25; CI 0.08 to 0.26; P<.001) were significant in determining whether the surgery occurred. The patient’s sex did not significantly influence the odds of surgical care (OR 0.87; 0.39 to 1.44; P=.58).
Figure 4 illustrates the odds ratio of surgery relative to patient age for the OPEN and MISS techniques. We also observed a considerable difference in the recovery length between the two techniques. The median time of hospitalization after open surgery was 10 (IQR 7) and after minimally invasive surgery, it was 6 (IQR 4). We also compared mortality following stabilization with either the MISS or OPEN techniques and found no significant difference (OR 0.91; CI 0.44 to 1.89; P=.79).
4. Discussion
Contrary to previous publications, our study emphasizes the structural and functional stability of fractures, treatment modalities, and their influence on mortality.[6, 20, 42-44]
We investigated how severity (AO Spine Classification) and consequent treatment influence the mortality of fragility fracture patients.[36, 45-48] The data on the association between fracture severity and survival are scarce in the international literature. Our own data and statistical analysis showed that the severity of the fracture, degree of instability, and restoration of spinal stability might influence patient survival. Stable fractures (AO A1-A2) and fractures stabilized using the MISS or OPEN technique, both in women and men, had significantly better survival rates than unstable A3-A4 fractures left unoperated. The indications for percutaneous vertebroplasty (PVP) are severe and focal spinal pain without radicular symptoms.[
49] We used PVP for acute A1-A2 fractures with a VAS score > 3/10, and when the A3-A4 unstable fracture was discovered as an inveterate fracture with a fresh component causing unremitting pain. We found significantly better MHR in the stable A1-A2 group after PVP and no difference in the unstable PVP group compared to the stable conservatively treated patients.
According to Cooper, osteoporotic vertebral fractures are less the cause of death, rather a consequence of comorbidities that independently increase the mortality hazard.[
50] Our own clinical results contradict this, since the two non-operated unstable fracture groups, which refused surgery and that of anaesthesiological contraindication, had nearly identical MHR. However, the surgically stabilized group had a more favorable MHR than the stable fracture group. Therefore, we conclude that, in addition to comorbidities, unstable fractures and the resulting pathological conditions have a negative impact on survival.
Regarding surgical techniques, minimally invasive percutaneous pedicle screw fixation yields similar results to those of traditional open surgery and has the advantages of less trauma, bleeding, pain, and rapid postoperative recovery.[51, 52] The percutaneous approach presents better results for some clinical and radiological outcomes than the open approach and even reduces the complication rate.[
53] According to our results, the operative technique is less of a modifying factor, and the resulting spinal stability plays a more important role in survival. No significant difference was found between the survival of patients who underwent MISS and those who underwent OPEN procedures. Furthermore, our data show that using the MISS procedure, a higher number of patients with an older average age was more suitable for general anesthesia and surgery than the OPEN procedure. The rate of unstable fractures was much higher in the MISS group, especially in patients aged > 70 years. We also observed a considerable difference in the length of hospitalization between the two techniques. After OPEN surgery, the median hospitalization time was 4 days longer than that of the MISS procedure.
Regarding hip fractures, it has been shown multiple times that early surgery might result in early mobilization and lower 1-year mortality.[
54] According to Colais et al, the survival of patients operated within two days for hip fracture had a significantly better 1-year survival than patients operated later or not at all. In our study, we obtained similar results for unstable thoracolumbar spinal fractures stabilized by surgery and not operated unstable fractures.[
55]
5. Conclusions
Based on our results, we conclude that there is a correlation between spinal fracture severity (AO fracture subtype), structural stability, and survival. The survival rate of patients who had an unstable fracture but were surgically stabilized was nearly identical to that of patients with stable AO A1-A2 fractures. Patients who refused surgical screw fixation had a clinically relevant lower mean survival rate, although the difference was not statistically significant. The MISS and OPEN surgical techniques used for stabilization produced nearly identical results in MHR. The difference lies in the lower complication rates and higher number of patients eligible for surgery using the minimally invasive approach.
6. Limitations
This study had several limitations. Our retrospective observational results did not examine independent mortality risks due to individual patient comorbidities. This was somewhat compensated by the large study population and the fact that we could explore many cases from virtually all age groups between 50 and 99 years. Another limitation of our OPEN vs. MISS comparison was that the OPEN group was considerably smaller than the MISS group (n= 45 and 188, respectively). Moreover, our mortality data did not distinguish between deaths directly related to thoracolumbar fractures and deaths from unrelated causes.
Survival is not the only or most critical outcome for frail elderly patients. Our dataset did not include important patient-reported outcome measures such as quality of life, loss of independence, socioeconomic burden, or human flourishing. Further prospective studies are needed to establish the impact of spinal stabilization on survival and confirm our results.
Author Contributions
Conceptualization, Á.V.; methodology, Á.J. and Á.V.; validation, Á.J., D.S.V.; formal analysis, D.S.V.; investigation, Á.J., D.S.; resources, Á.J., D.S.V.; data curation, Á.J., D.S.V.; writing—original draft preparation, Á.J., D.S., Á.V.; writing—review and editing, Á.J., D.S., Á.V.; visualization, D.S.V.; supervision, Á.V.; project administration, Á.V. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding. Ádám Juhász and Dávid Süvegh receives a regular scholarship from Semmelweis University, Budapest [grant number EFOP-3.6.3-VEKOP-16-2017-00009].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of Péterfy Sándor Utcai Kórház-Rendelőintézet és Baleseti Központ (Registration number: 02/2021, 2021.01.06).
Informed Consent Statement
Patient consent was waived due to the retrospective nature of the study, the GDPR-compliant anonym database and the patients receiving the standard protocol care.
Data Availability Statement
The anonymized dataset on which the statistical analysis is based is not publicly available, but will be provided upon request to the editorial board.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cummings SR, Melton LJ. Epidemiology and outcomes of osteoporotic fractures. Lancet. 2002; 359(Suppl 9319): 1761-7. [CrossRef]
- Salaffi F, Stancati A, Carotti M, et al. [The impact of vertebral fractures on quality of life in postmenopausal women with osteoporosis. Validity of the Italian version of mini-Osteoporosis Quality of Life Questionnaire.]. Reumatismo. 2005; 57(Suppl 2): 83-96. [CrossRef]
- Voko Z, Gaspar K, Inotai A, et al. Osteoporotic fractures may impair life as much as the complications of diabetes. J Eval Clin Pract. 2017; 23(Suppl 6): 1375-1380. [CrossRef]
- Willers C, Norton N, Harvey NC, et al. Osteoporosis in Europe: a compendium of country-specific reports. Arch Osteoporos. 2022; 17(Suppl 1): 23. [CrossRef]
- Hernlund E, Svedbom A, Ivergard M, et al. Osteoporosis in the European Union: medical management, epidemiology and economic burden. A report prepared in collaboration with the International Osteoporosis Foundation (IOF) and the European Federation of Pharmaceutical Industry Associations (EFPIA). Arch Osteoporos. 2013; 8: 136. [CrossRef]
- Johnell O, Kanis JA, Oden A, et al. Mortality after osteoporotic fractures. Osteoporos Int. 2004; 15(Suppl 1): 38-42. [CrossRef]
- Kanis JA, Cooper C, Rizzoli R, et al. European guidance for the diagnosis and management of osteoporosis in postmenopausal women. Osteoporos Int. 2019; 30(Suppl 1): 3-44. [CrossRef]
- Chen H, Pan W, Zhang Y, et al. [Epidemiological and clinical characteristics analysis of 681 cases of thoracolumbar osteoporotic vertebral compression fractures]. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi. 2022; 36(Suppl 7): 873-880. [CrossRef]
- Cumming RG, Klineberg RJ. Fall frequency and characteristics and the risk of hip fractures. J Am Geriatr Soc. 1994; 42(Suppl 7): 774-8. [CrossRef]
- Grisso JA, Kelsey JL, Strom BL, et al. Risk factors for falls as a cause of hip fracture in women. The Northeast Hip Fracture Study Group. N Engl J Med. 1991; 324(Suppl 19): 1326-31. [CrossRef]
- Cooper C, Atkinson EJ, O'Fallon WM, et al. Incidence of clinically diagnosed vertebral fractures: a population-based study in Rochester, Minnesota, 1985-1989. J Bone Miner Res. 1992; 7(Suppl 2): 221-7. [CrossRef]
- Cummings SR, Black DM, Nevitt MC, et al. Appendicular bone density and age predict hip fracture in women. The Study of Osteoporotic Fractures Research Group. JAMA. 1990; 263(Suppl 5): 665-8.
- McAfee PC, Yuan HA, Fredrickson BE, et al. The value of computed tomography in thoracolumbar fractures. An analysis of one hundred consecutive cases and a new classification. J Bone Joint Surg Am. 1983; 65(Suppl 4): 461-73.
- Denis F. The three column spine and its significance in the classification of acute thoracolumbar spinal injuries. Spine (Phila Pa 1976). 1983; 8(Suppl 8): 817-31. [CrossRef]
- Magerl F, Aebi M, Gertzbein SD, et al. A comprehensive classification of thoracic and lumbar injuries. Eur Spine J. 1994; 3(Suppl 4): 184-201. [CrossRef]
- Oner FC, Ramos LM, Simmermacher RK, et al. Classification of thoracic and lumbar spine fractures: problems of reproducibility. A study of 53 patients using CT and MRI. Eur Spine J. 2002; 11(Suppl 3): 235-45. [CrossRef]
- McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine (Phila Pa 1976). 1994; 19(Suppl 15): 1741-4. [CrossRef]
- Vaccaro AR, Lehman RA, Jr., Hurlbert RJ, et al. A new classification of thoracolumbar injuries: the importance of injury morphology, the integrity of the posterior ligamentous complex, and neurologic status. Spine (Phila Pa 1976). 2005; 30(Suppl 20): 2325-33. [CrossRef]
- Anandasivam NS, Ondeck NT, Bagi PS, et al. Spinal fractures and/or spinal cord injuries are associated with orthopedic and internal organ injuries in proximity to the spinal injury. N Am Spine Soc J. 2021; 6: 100057. [CrossRef]
- Kado DM, Browner WS, Palermo L, et al. Vertebral fractures and mortality in older women: a prospective study. Study of Osteoporotic Fractures Research Group. Arch Intern Med. 1999; 159(Suppl 11): 1215-20. [CrossRef]
- Babayev M, Lachmann E, Nagler W. The controversy surrounding sacral insufficiency fractures: to ambulate or not to ambulate? Am J Phys Med Rehabil. 2000; 79(Suppl 4): 404-9. [CrossRef]
- Dittmer DK, Teasell R. Complications of immobilization and bed rest. Part 1: Musculoskeletal and cardiovascular complications. Can Fam Physician. 1993; 39: 1428-32, 1435-7.
- Teasell R, Dittmer DK. Complications of immobilization and bed rest. Part 2: Other complications. Can Fam Physician. 1993; 39: 1440-2, 1445-6.
- Harper CM, Lyles YM. Physiology and complications of bed rest. J Am Geriatr Soc. 1988; 36(Suppl 11): 1047-54. [CrossRef]
- Sanderson PL, Fraser RD, Hall DJ, et al. Short segment fixation of thoracolumbar burst fractures without fusion. Eur Spine J. 1999; 8(Suppl 6): 495-500. [CrossRef]
- Gelb D, Ludwig S, Karp JE, et al. Successful treatment of thoracolumbar fractures with short-segment pedicle instrumentation. J Spinal Disord Tech. 2010; 23(Suppl 5): 293-301. [CrossRef]
- Shen WJ, Liu TJ, Shen YS. Nonoperative treatment versus posterior fixation for thoracolumbar junction burst fractures without neurologic deficit. Spine (Phila Pa 1976). 2001; 26(Suppl 9): 1038-45. [CrossRef]
- Hulme PA, Krebs J, Ferguson SJ, et al. Vertebroplasty and kyphoplasty: a systematic review of 69 clinical studies. Spine (Phila Pa 1976). 2006; 31(Suppl 17): 1983-2001. [CrossRef]
- Voormolen MH, Lohle PN, Lampmann LE, et al. Prospective clinical follow-up after percutaneous vertebroplasty in patients with painful osteoporotic vertebral compression fractures. J Vasc Interv Radiol. 2006; 17(Suppl 8): 1313-20. [CrossRef]
- Yang EZ, Xu JG, Huang GZ, et al. Percutaneous Vertebroplasty Versus Conservative Treatment in Aged Patients With Acute Osteoporotic Vertebral Compression Fractures: A Prospective Randomized Controlled Clinical Study. Spine (Phila Pa 1976). 2016; 41(Suppl 8): 653-60. [CrossRef]
- Edidin AA, Ong KL, Lau E, et al. Morbidity and Mortality After Vertebral Fractures: Comparison of Vertebral Augmentation and Nonoperative Management in the Medicare Population. Spine (Phila Pa 1976). 2015; 40(Suppl 15): 1228-41. [CrossRef]
- Park JS, Park YS. Survival analysis and risk factors of new vertebral fracture after vertebroplasty for osteoporotic vertebral compression fracture. Spine J. 2021; 21(Suppl 8): 1355-1361. [CrossRef]
- Hinde K, Maingard J, Hirsch JA, et al. Mortality Outcomes of Vertebral Augmentation (Vertebroplasty and/or Balloon Kyphoplasty) for Osteoporotic Vertebral Compression Fractures: A Systematic Review and Meta-Analysis. Radiology. 2020; 295(Suppl 1): 96-103. [CrossRef]
- Wiedl A, Forch S, Fenwick A, et al. [Importance of surgical treatment of thoracolumbar vertebral fractures for the survival probability of orthogeriatric patients]. Unfallchirurg. 2021; 124(Suppl 4): 303-310. [CrossRef]
- Pishnamaz M, Curfs I, Balosu S, et al. Two-Nation Comparison of Classification and Treatment of Thoracolumbar Fractures: An Internet-Based Multicenter Study Among Spine Surgeons. Spine (Phila Pa 1976). 2015; 40(Suppl 22): 1749-56. [CrossRef]
- Reinhold M, Audige L, Schnake KJ, et al. AO spine injury classification system: a revision proposal for the thoracic and lumbar spine. Eur Spine J. 2013; 22(Suppl 10): 2184-201. [CrossRef]
- Kepler CK, Vaccaro AR, Schroeder GD, et al. The Thoracolumbar AOSpine Injury Score. Global Spine J. 2016; 6(Suppl 4): 329-34. [CrossRef]
- Divi SN, Schroeder GD, Oner FC, et al. AOSpine-Spine Trauma Classification System: The Value of Modifiers: A Narrative Review With Commentary on Evolving Descriptive Principles. Global Spine J. 2019; 9(Suppl 1 Suppl): 77S-88S. [CrossRef]
- Brown JP, Josse RG. 2002 clinical practice guidelines for the diagnosis and management of osteoporosis in Canada. Cmaj. 2002; 167(Suppl 10 Suppl): S1-34.
- Whang PG, Goldberg G, Lawrence JP, et al. The management of spinal injuries in patients with ankylosing spondylitis or diffuse idiopathic skeletal hyperostosis: a comparison of treatment methods and clinical outcomes. J Spinal Disord Tech. 2009; 22(Suppl 2): 77-85. [CrossRef]
- Rustagi T, Drazin D, Oner C, et al. Fractures in Spinal Ankylosing Disorders: A Narrative Review of Disease and Injury Types, Treatment Techniques, and Outcomes. J Orthop Trauma. 2017; 31 Suppl 4: S57-S74. [CrossRef]
- Lavelle EA, Cheney R, Lavelle WF. Mortality Prediction in a Vertebral Compression Fracture Population: the ASA Physical Status Score versus the Charlson Comorbidity Index. Int J Spine Surg. 2015; 9: 63. [CrossRef]
- Shah S, Goregaonkar AB. Conservative Management of Osteoporotic Vertebral Fractures: A Prospective Study of Thirty Patients. Cureus. 2016; 8(Suppl 3): e542. [CrossRef]
- Park SM, Ahn SH, Kim HY, et al. Incidence and mortality of subsequent vertebral fractures: analysis of claims data of the Korea National Health Insurance Service from 2007 to 2016. Spine J. 2020; 20(Suppl 2): 225-233. [CrossRef]
- Rajasekaran S, Kanna RM, Schnake KJ, et al. Osteoporotic Thoracolumbar Fractures-How Are They Different?-Classification and Treatment Algorithm. J Orthop Trauma. 2017; 31 Suppl 4: S49-S56. [CrossRef]
- Court-Brown CM, Caesar B. Epidemiology of adult fractures: A review. Injury. 2006; 37(Suppl 8): 691-7. [CrossRef]
- Vaccaro AR, Oner C, Kepler CK, et al. AOSpine thoracolumbar spine injury classification system: fracture description, neurological status, and key modifiers. Spine (Phila Pa 1976). 2013; 38(Suppl 23): 2028-37. [CrossRef]
- Kim TY, Jang S, Park CM, et al. Trends of Incidence, Mortality, and Future Projection of Spinal Fractures in Korea Using Nationwide Claims Data. J Korean Med Sci. 2016; 31(Suppl 5): 801-5. [CrossRef]
- DePalma MJ, Slipman CW. CHAPTER 44 - Vertebroplasty. In: Interventional Spine, 2008. [CrossRef]
- Cooper C. The crippling consequences of fractures and their impact on quality of life. Am J Med. 1997; 103(Suppl 2A): 12S-17S; discussion 17S-19S. [CrossRef]
- Gong Y, Fu G, Li B, et al. Comparison of the effects of minimally invasive percutaneous pedicle screws osteosynthesis and open surgery on repairing the pain, inflammation and recovery of thoracolumbar vertebra fracture. Exp Ther Med. 2017; 14(Suppl 5): 4091-4096. [CrossRef]
- Sun XY, Zhang XN, Hai Y. Percutaneous versus traditional and paraspinal posterior open approaches for treatment of thoracolumbar fractures without neurologic deficit: a meta-analysis. Eur Spine J. 2017; 26(Suppl 5): 1418-1431. [CrossRef]
- Kreinest M, Rillig J, Grutzner PA, et al. Analysis of complications and perioperative data after open or percutaneous dorsal instrumentation following traumatic spinal fracture of the thoracic and lumbar spine: a retrospective cohort study including 491 patients. Eur Spine J. 2017; 26(Suppl 5): 1535-1540. [CrossRef]
- Chong CP, Savige JA, Lim WK. Medical problems in hip fracture patients. Arch Orthop Trauma Surg. 2010; 130(Suppl 11): 1355-61. [CrossRef]
- Colais P, Di Martino M, Fusco D, et al. The effect of early surgery after hip fracture on 1-year mortality. BMC Geriatr. 2015; 15: 141. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).