1. Introduction
Globally, asthma is one of the most common chronic respiratory diseases affecting people of all ages [
1]. Clinically, asthma is defined as chronic inflammation of the airways characterized by bronchial hyperresponsiveness to a wide variety of stimuli, such as pollen, cat hair, and household dust, among others. Episodic asthma attacks result in reversible airway obstruction causing symptoms such as coughing, recurrent wheezing, shortness of breath and chest tightness, among others [
2,
3]. Asthma has no cure, but good management with inhaled medications, mainly bronchodilators and steroids, in conjunction with a reduction in exposure to asthma-triggering stimuli is needed to reduce inflammation and control the disease [
4], thus allowing asthmatic people to live a normal life [
5]. Nevertheless, asthma management and control in people living in low-income countries has been reported to be inadequate [
6].
According to recent results from the Global Burden of Disease study 2019 (GBD 2019), the global prevalence of asthma was estimated at 3.54%, affecting 264.2 million people and causing 37 million new incident cases, with 461 thousand deaths worldwide in the general population during 2019 [
7]. These figures explain why asthma represents a significant global economic burden and a worrying public health problem, which needs attention to develop prevention and cost-effective management approaches in middle- and low-income countries [
2]. Therefore, there is an ongoing international and cooperative effort focus on describing the burden of asthma, as well as its control and management in different settings and locations in the world [
8,
9,
10,
11,
12]. In Mexico, although several studies and surveys have been conducted on the epidemiology of asthma [
13,
14,
15,
16,
17], these are limited to some locations, age groups, and years covered. In addition, given that Latin American countries are characterized by an enormous contrast in social, cultural, genetic, and environmental conditions both between and within localities, a heterogeneous epidemiology of asthma within a country is expected [
18]. Thus, there is a need to estimate and describe the national and subnational burden of disease caused by asthma in Mexico.
In the present study, we conducted a secondary analysis using updated and reliable data from the most recent iteration of the GBD 2019 study [
19]. Our analysis assessed the burden of disease caused by asthma in the general population of Mexico and by sex and age group from 1990 to 2019 at the national and subnational levels. The results from this study will be helpful for identifying the trends of asthma and finding any existing health disparity caused by this chronic respiratory disease. Likewise, describing the subnational pattern will be useful to guide location-specific efforts aimed at alleviating health loss due to asthma in places where the burden is the highest. Given that asthma is considered a public health issue, knowing its epidemiology represents an opportunity to respond to a growing problem by providing sustainable health management that incorporates efficient diagnosis and control measures in the most vulnerable population affected by this disease.
2. Methods
2.1. Overview of the Global Burden of Disease
The GBD 2019 study represents the most comprehensive global effort to understand the 369 leading causes of disease and injury affecting the population [
19], including the study of the risk factors associated with health loss in men and women of all age groups in 204 countries and regions [
20]. The present study was conducted in compliance with the GBD protocol as part of the GBD Mexico collaborative network [
21]. For this purpose, we used the estimations produced by the most recent iteration of the GBD 2019, which are available in the public database Global Health Data Exchange (GHDx) of the Institute for Health Metrics and Evaluation (IHME). The estimates produced by the GBD comply with the GATHER (Guidelines for Accurate and Transparent Health Estimates Reporting) statement [
22].
2.2. Case definition
According to the 10th revision of the International Statistical Classification of Diseases and Related Health Problems (ICD-10) of the World Health Organization (WHO), asthma corresponds to code J45 (J45.0, 45.1, 45.8 and 45.9). According to the GBD 2019, asthma was defined as a chronic lung disease characterized by bronchial spasms usually caused by allergic or hypersensitivity reactions that make breathing difficult. The case definition includes wheezing in the past year and self-report of a medical diagnosis (GBD 2019 two-pagers Asthma-Level 3, pp. 24-25) [
19].
2.3. Data sources for modeling
In 2019, the GBD used 2,891 data sources to estimate the fatal (2,478) and nonfatal (413) components of the global burden of asthma, which are available for consultation at the following link:
https://ghdx.healthdata.org/gbd-2019/data-input-sources. Data sources included representative surveys at the population level (national and subnational), vital record systems, scientific articles focused on describing prevalence, systematic reviews and meta-analyses, epidemiological surveillance data, information on medical claims and visits to health services. For the case of Mexico, 46 data sources were used and are listed in
Supplementary Table S1.
2.4. Estimation of the fatal component
For the fatal component that includes deaths and years of life lost (YLLs), we used the cause of death assembly model (CODEm), which is a standard and optimized GBD tool that is based on an assembly of different modeling methods. CODEm incorporates covariates that produce estimations of high predictive validity (pages 258-260, Supplementary Appendix 1 of the GBD 2019 study) [
19]. The flowchart and codes needed for estimation of the fatal component of asthma can be found at the following link:
https://ghdx.healthdata.org/gbd-2019/code/cod-2. Briefly, the process includes 1) standardization of the data sources, 2) mapping according to the ICD, 3) sex and age split, 4) redistribution of the junk codes, 5) noise reduction, and 6) generation of the database. From the database, covariates are entered (i.e., cumulative cigarette consumption for 10 and 5 years, health care access and quality index, outdoor pollution by fuels and PM2. 5,
per capita income, education, and the sociodemographic index) and models are produced to estimate 1) the number of deaths due to asthma by locality/year/age/sex and 2) the number of YLLs, which represent the sum of years of life lost due to premature death multiplied by the standard life expectancy for a locality [
23].
2.5. Estimation of the nonfatal component
The following link:
https://ghdx.healthdata.org/gbd-2019/code/nonfatal-2 presents both the flow chart and the codes used by the GBD to generate the nonfatal asthma estimates. Briefly, data processing was first performed, which consisted of 1) age and sex split, using the Meta-regression Bayesian Trimming tool (MR-BRT) to breakdown the estimates by sex proportionally to existing reports and fitting a cubic spline on age showing high values of asthma prevalence in early-age males and a subsequent increase in older-age females; 2) modeling the excess mortality rate; and 3) adjusting for bias with MR-BRT, which allowed for improved comparability between different case definitions and study designs, as well as data from medical claims and surveillance studies (pages 883-887 of Supplementary Appendix 1 of the GBD 2019 study) [
19]. Then, from the processed data, the database was generated and used in the Disease Modeling Meta-Regression 2.1 (DisMod-MR 2.1) tool by which prevalence and incidence by locality/year/age/sex were estimated. Predictor covariates included the health care access and quality index, per capita income, and the standardized exposure variable (scalar combining exposure to all asthma risk factors). Additionally, to estimate the number of years lived with disability (YLDs), prevalent cases were separated by severity into four patient groups using medical expenditure surveys: asymptomatic, controlled, partially controlled, and uncontrolled and adjusted with the disability weight according to each severity level (
Supplementary Table S2). YLDs represent the years of life lost due to disability caused by a disease and are obtained by multiplying the disability weight (0 = no health loss to 1 = death) caused by a specific sequela of the disease by the prevalence of that disease [
23].
2.6. Metrics and reporting standards
To estimate the burden of asthma in Mexico, we used publicly available data from the online query tool GHDx (
https://vizhub.healthdata.org/gbd-results/). We collected data at the national and subnational levels for the 32 states by sex and 5-year age groups for the period 1990 to 2019 [
24]. To summarize the burden of asthma, we used counts, as well as the crude and age-standardized rate per 100,000 people for prevalence, incidence, mortality, and disability-adjusted life years (DALYs). DALYs incorporate both the fatal and nonfatal burden of asthma and correspond to the sum of YLLs and YLDs. All estimations were made by locality, year, sex, and age group, with 95% uncertainty intervals (UI). For the estimates, uncertainty was propagated through each modeling step for 1,000 draws, with UIs representing the 25th and 975th percentiles of the ordered 1,000 draw distribution [
7]. In addition, we assessed trends in asthma burden using annual estimates for the 30-year time series and estimated the crude, age-standardized percent change for each measurement over the last decade (2010 to 2019). The GBD 2019 study used Python version 3.7.0 (Python Software Foundation), Stata version 15.1 (StataCorp), and R version 3.4.1 (R Foundation). We used Prism 10 (GraphPad Inc., USA) to create all graphs.
3. Results
3.1. Temporal changes in the burden of asthma in Mexico from 1990 to 2019
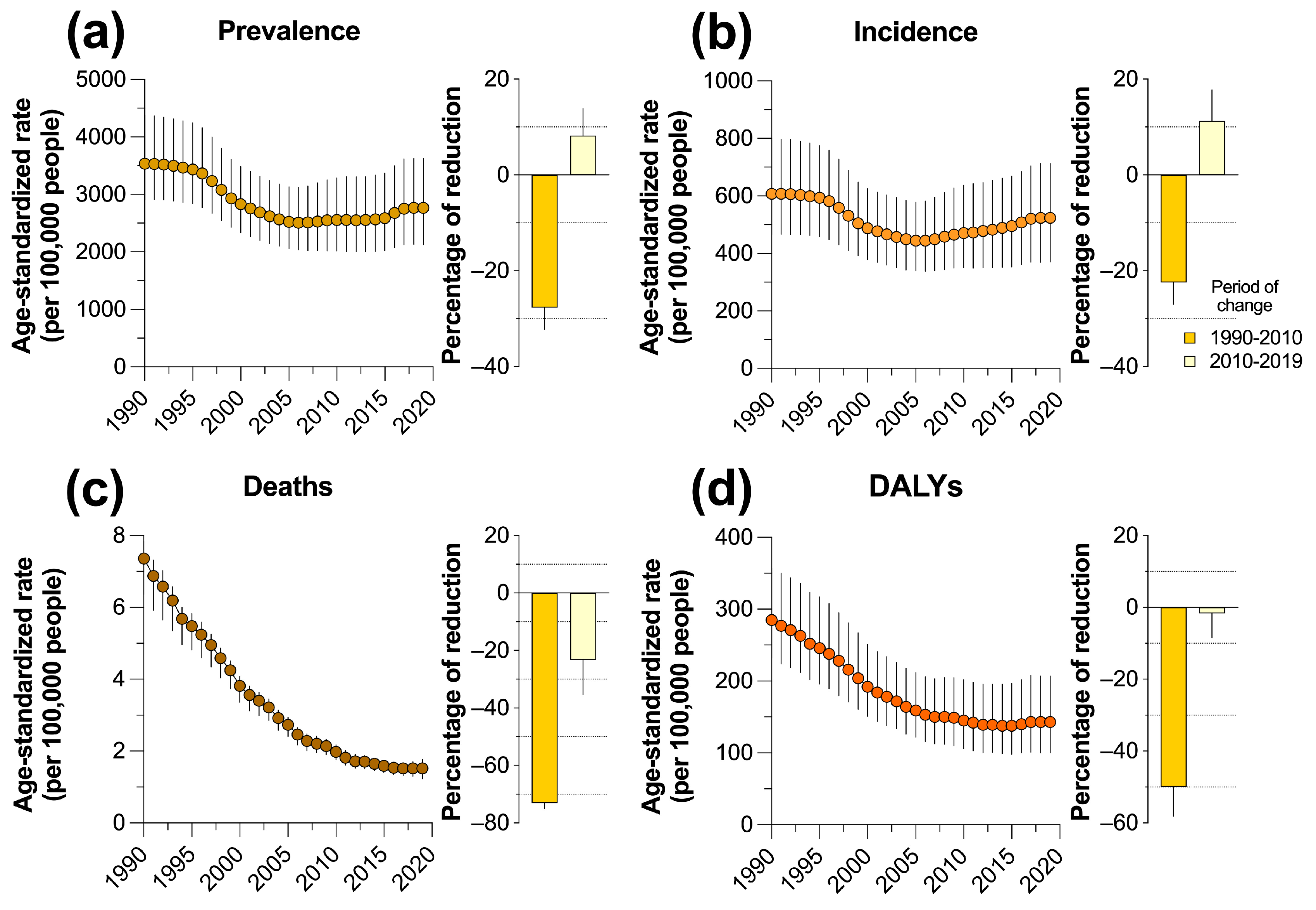
In general, changes in the crude estimates of the burden of asthma in Mexico were observed throughout the period studied. Although there was a trend toward a reduction in the number of cases from 1990 to 2000, during the last decade from 2010 to 2019, there was an increase in the national burden of asthma. The percentage of deaths due to asthma increased 1.56%, with prevalence and incidence showing the largest increase in the period (
Table 1). A similar trend was observed in the age-standardized prevalence and incidence rate per 100,000 persons, which despite the substantial reduction in the period from 1990 to 2010, there was an increase from 8.22 to 11.3%, respectively, between 2010 and 2019 (
Figure 1a,b). In contrast, both mortality and DALYs rates tended to decrease between 1990 and 2019, although in both measurements, a differential slowdown in the reduction was observed during the last decade, as the age-standardized mortality rate per 100,000 persons decreased by 23.3% (95% uncertainty interval, 11.40 to 35.38%) from 2010 to 2019 and by 1.64% (8.40 to 5.24%) the DALYs rate in the same period (
Figure 1c,d).
3.2. Burden of asthma in Mexico in 2019 by sex
In Mexico, 3.35 million (2.59 to 4.37 million) prevalent cases of asthma were estimated in the general population in 2019 (
Table 1), of which 50.48% corresponded to women (1.69 million, 1.33 to 2.16) with a higher age-standardized rate in males than in females (2,767.1 vs. 2,746.4 prevalent cases per 100,000 persons, respectively) (
Table 2). Regarding the incidence of asthma, 606,000 new cases (433,053 to 811,132) occurred in 2019 in males and females of all ages (
Table 1), with a lower proportion of incident cases in females (48.72% of total) and a higher age-standardized incidence rate in males (537.7, 375.1 to 745.6 per 100,000 people) (
Table 2).
A total of 1,655 (3 to 1,931) people died from asthma in Mexico in 2019 (
Table 1), with women being the sex most affected by the disease, as they contributed 54.52% of the total deaths, although with a similar age-standardized rate of 1.4 and 1.2 deaths per 100,000 people for females and males, respectively (
Table 2). In addition, in the general population, the count of DALYs due to asthma was estimated at 172,041 (120,406 to 249,530), with a slightly higher burden of the disease in women than in men judging by the 88,271 DALYs (62,589 to 126,512) estimated in women, which corresponded to 51.3% of the total, and a higher age-standardized rate in females that corresponded to 143.1 (100.9 to 206.9) DALYs per 100,000 people (
Table 2).
3.3. Burden of asthma in Mexico in 2019 by age group
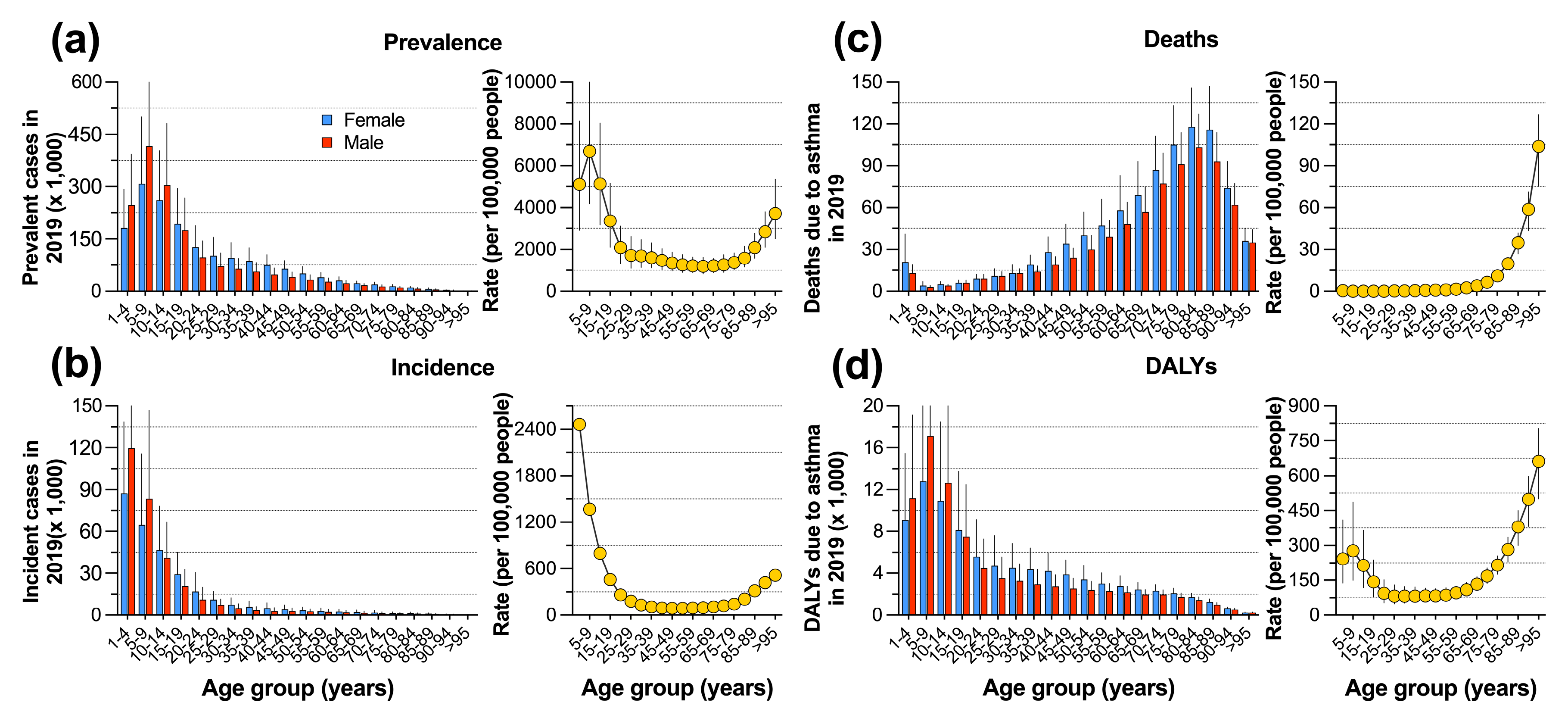
The burden of asthma in Mexico varied according to age group and sex. The three youngest age groups (1-14 years) accounted for 51.18% of the total prevalent cases (
Supplementary Table S3), with a higher contribution of cases in males than in females, a trend that was reversed for the remaining groups (
Figure 2a). The prevalence rate per 100,000 people ranged from 1,193 to 6,687 cases, with the highest value in the pediatric population aged 5-9 years and with increasing values in older adults aged 75 years and older (
Figure 2a and
Supplementary Table S4). Children under 14 years of age accounted for 73.04% of incident cases of asthma, with the peak of the distribution in infants aged 1-4 years (
Supplementary Table S3) and a higher incidence in children for the first two age groups (
Figure 2b). With a value of 2,463 (1,440 to 3,895) cases per 100,000 people, the population aged 1-4 years had the highest asthma incidence rate, which steadily decreased as age increased, although there was a trend toward higher values after age 75 years (
Figure 2b and
Supplementary Table S4).
Mortality due to asthma had a different behavior, since the highest number of deaths was observed among adults older than 70 years, reaching its maximum value in persons aged 80-84 years (
Supplementary Table S3). In contrast to previous measurements, women presented an equal or higher number of deaths than men in all age groups (
Figure 2c). In the population younger than 50 years, the mortality rate per 100,000 people was close to zero but increased from age 75 years onward until reaching its peak of 104 deaths (75 to 127) in the >95 years age group (
Figure 2c and
Supplementary Table S4). Finally, the distribution of the number of DALYs and their rate per 100,000 people showed contrasting behavior between age groups (
Figure 2d), as the population <14 years accumulated the highest DALY count (
Supplementary Table S3), with a higher proportion in men. The highest rates of DALYs per 100,000 people were observed in persons >85 years (
Figure 2d and
Supplementary Table S4).
3.4. Asthma burden and trends at the subnational level
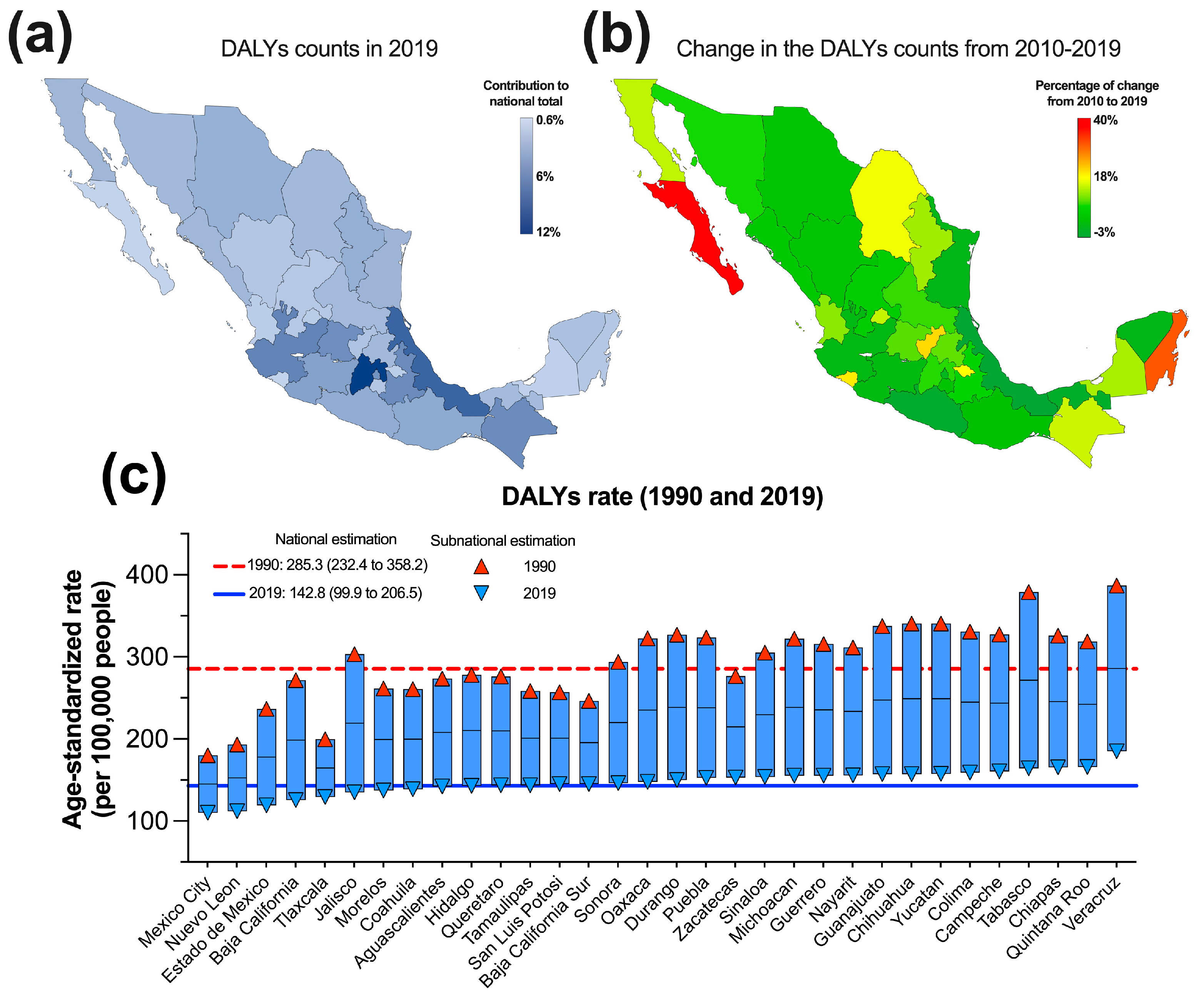
At the subnational level, there were contrasting patterns of asthma burden in men and women of all ages (
Supplementary Table S5). Among the 32 states of Mexico, the crude prevalence ranged from 21,021 to 411,104 cases and from 3,621 to 78,148 incident cases in 2019. Colima, Baja California sur, Campeche, Nayarit, and Tlaxcala had the lowest values for both estimates, while Puebla, Jalisco, Veracruz, and Mexico were characterized by the highest prevalence and incidence of the disease. To exemplify the heterogeneity of the spatial distribution of the asthma burden,
Figure 3a shows a map with the relative contribution of each state to the national total DALYs due to asthma in 2019. The map shows that the highest percentages of DALYs occurred in some entities distributed in the central belt (Jalisco, Guanajuato, Estado de Mexico City, Puebla, and Veracruz) and in the southern region of the country. However, other states, such as Colima, Morelos, and Tlaxcala, had low contributions of between 0.65 and 1.51% of the national total DALYs, even though these states are also located in the central belt of the country. Similar results were observed with the count of deaths in 2019 (
Supplementary Table S5).
In addition to spatial heterogeneity, there were also temporal disparities in the changes in the crude estimates of asthma burden from 2010 to 2019 among the 32 states of Mexico (
Supplementary Table S6). First, crude prevalence and incidence cases tended to increase in all localities at the subnational level, with percentages varying between 2.58 and 40.23 for the former and 0.43 and 33.74 for the latter from 2010 to 2019. Second, the change in the count of DALYs and asthma deaths presented a contrasting behavior because Baja California Sur, Quintana Roo, Queretaro, and Colima showed considerable increases of between 20 and 40% in the number of DALYs, whereas only Veracruz, Guerrero, and Tabasco showed a slight reduction during the period (
Figure 3b). In contrast, 10 of the 32 states of the country showed a reduction in the number of deaths due to asthma during the same decade of analysis (
Supplementary Table S6).
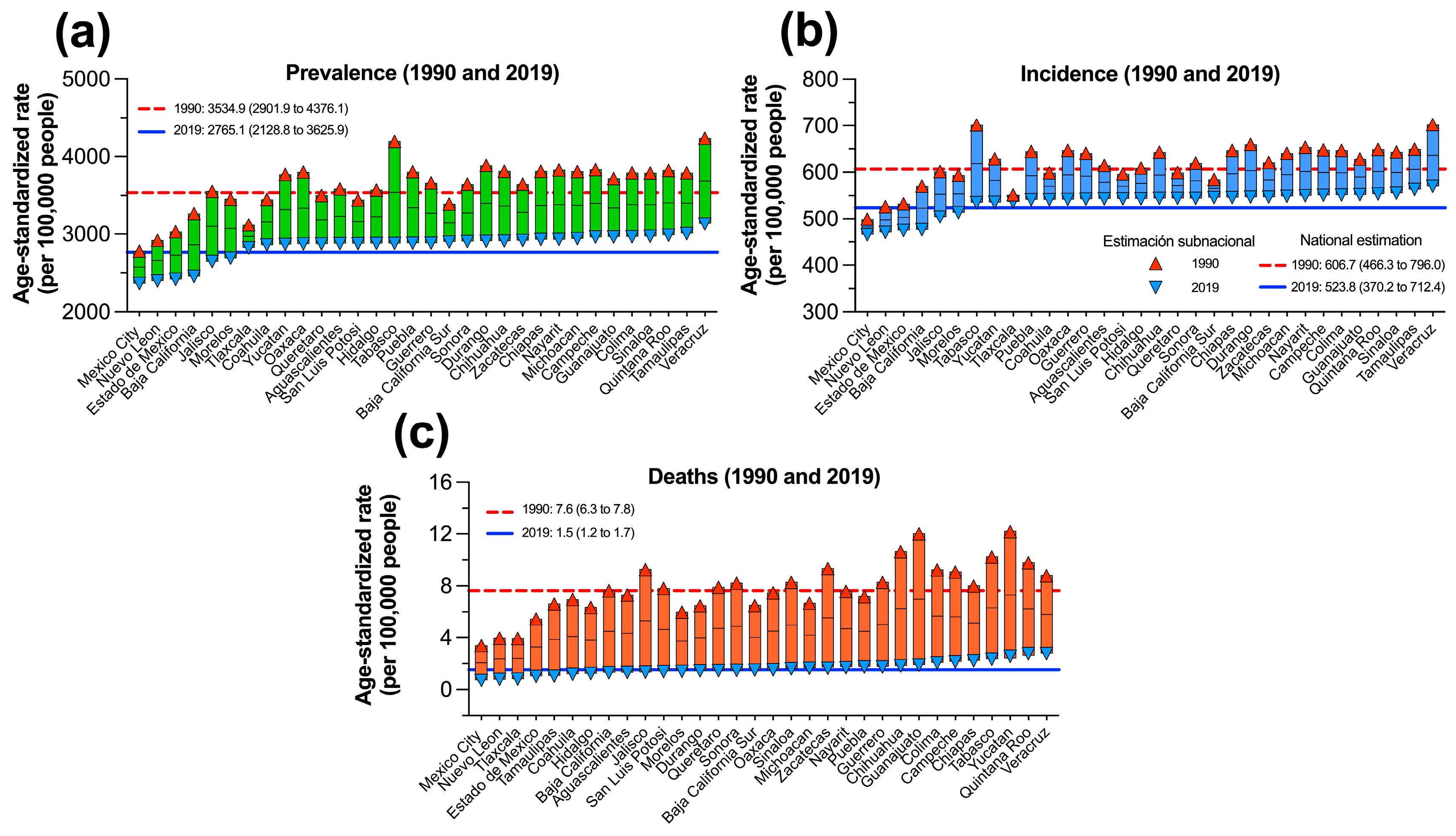
Finally, to comparatively analyze the change in asthma burden between states and the national benchmark, the age-standardized rate (per 100,000 people) for the beginning and end of the period (1990 and 2019) was plotted for each state and compared against the national average. In
Figure 3c, a high initial disparity was observed with rates ranging from 386.9 to 180.19 DALYs per 100,000 people, which declined to comparable estimates (109.94 to 184.95) in 2019 in all states, among which nine were below the national average. Similar results are displayed in
Figure 4, which summarizes the change in the age-standardized prevalence, incidence, and mortality rates per 100,000 people at the subnational level from 1990 to 2019. In general, there were high and heterogeneous estimates at the beginning of the period, which decreased consistently across states by 2019. Only six states had standardized prevalence and incidence rates below the national average in 2019, while 15 states had an asthma mortality rate below the national benchmark. Mexico City, Nuevo Leon, and Estado de Mexico consistently ranked below the national average, while Quintana Roo and Veracruz were the two states with the highest values for all three measures.
4. Discussion
Our results indicate that asthma should be considered a public health problem because it affected 3.35 million people in Mexico by 2019. This value corresponds to a prevalence of 2.85% (2.2 to 3.72%) among the Mexican population, which despite being lower than the global prevalence of 3.53% (3.01 to 4.16) and to the countries from Central America whose prevalence ranged from 3.25% (2.49 to 4.25) in Guatemala to 5.69% (4.61 to 7.03) in El Salvador [
24], still causes a significant health loss in the country.
Even though asthma is considered an urban-related disease in Latin American countries [
18], our results indicate that low-income countries from the Central America region had higher asthma prevalence estimations. Therefore, not only the urban environment but also poverty and lack of health care access might contribute to the higher burden of asthma in countries from the region. Similarly, the idea that rural areas of countries from Latin America are protected against asthma and thus have a lower prevalence contrasts with our results, as judged by the higher values of asthma prevalence in countries from Central America, which are characterized by a greater proportion of rural areas [
25]. However, this discrepancy in the region could also be explained by fast urbanization and migration from rural locations, which are demographic factors likely to drive the asthma epidemic in the region [
18]. Factors that could explain the regional disparity found in the GBD results might be related to case definition differences between countries, the number and quality of data input sources used to model the burden, and the years covered for each country.
According to our results, the burden of asthma in Mexico showed a contrasting temporal pattern during the last decade from 2010 to 2019; the prevalence increased by 8.2%, as did the incidence by 11.3%, whereas mortality and DALYs decreased by 23.3 and 1.6%, respectively. Although the incidence and prevalence of asthma has remained stable, there have been some variations in different geographic regions of the world [
26]. Generally, low-income countries have a higher frequency of respiratory diseases, including asthma. Nevertheless, some authors have observed unexpected changes in the prevalence of asthma, which has decreased in low-income countries but increased in middle-income countries. In contrast, in high-income and upper-middle-income countries, the prevalence of asthma remains stable [
26]. A simple explanation is that the underdiagnosis of asthma is common in low- and middle-income countries. However, several endogenous factors could change the prevalence of asthma among countries, such as ethnicity [
27], pulmonary microbiome [
28], depression, anxiety, and emotional stress [
29]. Additionally, exogenous risk factors could influence the changes in the prevalence of asthma, such as exposure to microbes, pollens, smoke, dust, and much more, or protector factors, such as early infancy contact with farm animals [
30]. Additionally, increased pollution, ongoing climate change, and global warming are factors also related to the differences seen in asthma prevalence during recent decades [
11,
31]. Indeed, air pollution associated with urbanization and the change to a Western diet are risk factors for asthma development [
32].
Asthma remains a public health problem worldwide, which varies broadly globally because in adults, the prevalence ranges from 0.2 to 21.0% and from 2.8 to 37.6% in children between 6 and 7 years of age [
33]. Other studies have shown differences in the prevalence of asthma among adolescents ranging from 0.9% in India to 21.3% in South Africa [
34]. In contrast, the prevalence of childhood asthma in China appears to be very low (0.9 to 1.5%) [
35]. Our results indicated a sex and age disparity in the burden of asthma because this respiratory disease differentially affected females and males according to age group. Asthma prevalence was higher in boys than girls between the ages of 1 and 14 years of age. A similar result was observed in incidence, which exhibited higher values among boys from 1 to 9 years of age. Nonetheless, the values were inverted after puberty, with prevalence and incidence being higher in females than in males. These results concur with a well-documented sex bias in asthma prevalence [
36,
37] and the highest incidence of asthma occurring in childhood at an average age of 10 years [
38].
Further national and subnational representative studies are needed in Mexico to assess the origin of the geographic differences documented in this study. Mexico lacks a national asthma strategy, which could help reduce the local disparities reported in our study [
39]. In addition, without an adequate diagnosis and control of the disease, there will be a continuous growth of uncontrolled asthma that will result in excessive health loss and economic burden [
40], especially among the most vulnerable population, thus increasing the gap between people lacking access to health care. Therefore, providing more sustainable health management for asthma control should help reduce the preventable burden caused by this disease and concomitantly increase the quality of life of patients as well as reduce the cost associated with uncontrolled asthma.
5. Limitations
We found four main limitations to our study. 1) the reduced number of data input sources used to model the burden of asthma, 2) the lack of national and subnational representative studies to which to compare our results, 3) the high level of uncertainty found in several locations and years covered due to scarcity of input sources for those states, and 4) the lack of results from the GBD split by severity of the disease.
6. Conclusions
In Mexico, asthma represents a public health problem that has shown an increasing trend in incidence and prevalence. The burden of this disease differentially affects males and females of distinct age groups, with the highest incidence, prevalence, and DALYs at early stages of life and the highest mortality due to asthma at older years of age. These results and the existence of geographic disparities highlight the need for both a national strategy and a subnational asthma control plan to reduce preventable health loss and reduce the gap among the affected population from each state. In addition, raising awareness regarding the appropriate diagnosis and control management by care providers will benefit patients to improve their quality of life.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Table S1: List of the 46 data input sources from Mexico used by the GBD to estimate the burden of asthma. Supplementary Table S2: Health state and disability weights defined by the GBD. Supplementary Table S3: Estimates (counts with 95% UI) of prevalence, incidence, mortality and DALYs due to asthma in Mexico by age group in 2019. Supplementary Table S4: Prevalence, incidence, mortality and DALYs rate (with 95% UI) due to asthma per 100,000 people in Mexico by age group in 2019. Supplementary Table S5: Estimates (counts with 95% UI) of prevalence, incidence, mortality, and DALYs due to asthma in men and women of all ages at the subnational level in 2019. Supplementary Table S6: Percent change from 2010 to 2019 in estimates of prevalence, incidence, mortality, and DALYs due to asthma at the subnational level.
Author Contributions
To define authorship, we used CRediT taxonomy. Conceptualization, ALB, RL, and DD; methodology, SABO, DMBC, and VACR; software and visualization, PEHC, FJT, FGV, and DAFZ; formal analysis, ALB, DAFZ, and DD; investigation and writing—review and editing, ALB, RL, PEHC and DD; data curation, JAD; writing—original draft preparation, ALB, RL, and DD; project administration, RL and DD. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Data Availability Statement
Acknowledgments
Ana Lopez-Bago is a postgraduate student from the Posgrado en Ciencias Biológicas at the Facultad de Medicina of the Universidad Nacional Autónoma de México and performed the present study as a partial fulfilment of the requirements for obtaining her Ph.D. degree.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Soriano, J.B.; Kendrick, P.J.; Paulson, K.R.; Gupta, V.; Abrams, E.M.; Adedoyin, R.A.; Adhikari, T.B.; Advani, S.M.; Agrawal, A.; Ahmadian, E. Prevalence and attributable health burden of chronic respiratory diseases, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet Respiratory Medicine 2020, 8, 585–596. [Google Scholar] [CrossRef] [PubMed]
- Brasier, A.R. Heterogeneity in asthma, 1 ed.; Humana New York: New York, 2014.
- Garcia-Garcia, M.L.; Rey, C.C.; del Rosal Rabes, T. Pediatric asthma and viral infection. Archivos de Bronconeumología (English Edition) 2016, 52, 269–273. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Asthma; WHO: Geneve, 15/12/2022 2022.
- Bush, A. Management of asthma in children. Minerva Pediatrica 2018, 70, 13. [Google Scholar] [CrossRef]
- Garcia-Marcos, L.; Chiang, C.Y.; Asher, M.I.; Marks, G.B.; El Sony, A.; Masekela, R.; Bissell, K.; Ellwood, E.; Ellwood, P.; Pearce, N.; et al. Asthma management and control in children, adolescents, and adults in 25 countries: a Global Asthma Network Phase I cross-sectional study. Lancet Glob Health 2023, 11, e218–e228. [Google Scholar] [CrossRef] [PubMed]
- Momtazmanesh, S.; Moghaddam, S.S.; Ghamari, S.-H.; Rad, E.M.; Rezaei, N.; Shobeiri, P.; Aali, A.; Abbasi-Kangevari, M.; Abbasi-Kangevari, Z.; Abdelmasseh, M. Global burden of chronic respiratory diseases and risk factors, 1990–2019: an update from the Global Burden of Disease Study 2019. EClinicalMedicine 2023, 59. [Google Scholar] [CrossRef] [PubMed]
- Hansen, S.; von Bülow, A.; Sandin, P.; Ernstsson, O.; Janson, C.; Lehtimäki, L.; Kankaanranta, H.; Ulrik, C.; Aarli, B.B.; Wahl, H.F. Prevalence and management of severe asthma in the Nordic countries: findings from the NORDSTAR cohort. ERJ Open Research 2023, 9. [Google Scholar] [CrossRef]
- Sanz, A.B.; Martinez-Torres, A.; Díaz, C.G.; Varela, Á.L.-S.; Belinchón, F.J.P.; Aguinaga-Ontoso, I.; Garcia-Marcos, L.; España, G.G. Prevalence and temporal evolution of asthma symptoms in Spain. Global Asthma Network (GAN) study. Anales de Pediatría (English Edition) 2022, 97, 161–171. [Google Scholar]
- Mortimer, K.; Reddel, H.K.; Pitrez, P.M.; Bateman, E.D. Asthma management in low and middle income countries: case for change. European Respiratory Journal 2022, 60. [Google Scholar] [CrossRef]
- Skevaki, C.; Ngocho, J.S.; Amour, C.; Schmid-Grendelmeier, P.; Mmbaga, B.T.; Renz, H. Epidemiology and management of asthma and atopic dermatitis in Sub-Saharan Africa. Journal of Allergy and Clinical Immunology 2021, 148, 1378–1386. [Google Scholar] [CrossRef]
- Tosca, M.A.; Marseglia, G.L.; Ciprandi, G. The real-world “ControL’Asma” study: a nationwide taskforce on asthma control in children and adolescents. Allergologia et Immunopathologia 2021, 49, 32–39. [Google Scholar] [CrossRef]
- Baeza Bacab, M.A.; Albertos Alpuche, N.E. Prevalencia de asma en niños escolares de Mérida, Yucatán. Revista Panamericana de Salud Pública 1997, 2, 299–302. [Google Scholar] [PubMed]
- Pérez, G.L.; Maciel, B.M.M.; López, J.H.; Covarrubias, F.M.; López, J.L.; Aguilar, G.; Pérez, J.L.R.; Medina, L.L.; Vargas, F. Prevalencia de las enfermedades alérgicas en la Ciudad de México. Revista Alergia de Mexico 2009, 56. [Google Scholar]
- Bedolla-Barajas, M.; Morales-Romero, J.; Robles-Figueroa, M.; Fregoso-Fregoso, M. Asma en adolescentes tardíos del occidente de México: prevalencia y factores asociados. Archivos de Bronconeumología 2013, 49, 47–53. [Google Scholar] [CrossRef]
- Blanca Estela, D.-R.-N.; Arturo, B.; Nayely, R.-N.; Elsy Maureen, N.-R.; Roberto, G.-A.; Philippa, E.; Luis, G.-M.; Omar Josué, S.-R.; Valente Juan, M.-P.; Beatriz Del Carmen, R.-G.; et al. Global Asthma Network Phase I study in Mexico: prevalence of asthma symptoms, risk factors and altitude associations—a cross-sectional study. BMJ Open Respiratory Research 2020, 7, e000658. [Google Scholar]
- Ramirez-Leyva, D.H.; Díaz-Sánchez, L.; Citlaly-Ochoa, M.; Ornelas-Aguirre, J.M. Patterns of allergen sensitization in patients with asthma in Yaqui Valley, Mexico. Journal of asthma 2022, 59, 1319–1327. [Google Scholar] [CrossRef]
- Cooper, P.; Rodrigues, L.; Cruz, A.; Barreto, M. Asthma in Latin America: a public heath challenge and research opportunity. Allergy 2009, 64, 5–17. [Google Scholar] [CrossRef] [PubMed]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1204–1222. [Google Scholar]
- Murray, C.J.L.; Aravkin, A.Y.; Zheng, P.; Abbafati, C.; Abbas, K.M.; Abbasi-Kangevari, M.; Abd-Allah, F.; Abdelalim, A.; Abdollahi, M.; Abdollahpour, I.; et al. Global burden of 87 risk factors in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1223–1249. [Google Scholar]
- Beltran-Ontiveros, S.A.; Fernandez-Galindo, M.A.; Moreno-Ortiz, J.M.; Contreras-Gutierrez, J.A.; Madueña-Molina, J.; Arambula-Meraz, E.; Leal-Leon, E.; Becerril-Camacho, D.M.; Picos-Cardenas, V.J.; Angulo-Rojo, C. Incidence, Mortality, and Trends of Prostate Cancer in Mexico from 2000 to 2019: Results from the Global Burden of Disease Study 2019. Cancers 2022, 14, 3184. [Google Scholar] [CrossRef]
- Stevens, G.A.; Alkema, L.; Black, R.E.; Boerma, J.T.; Collins, G.S.; Ezzati, M.; Grove, J.T.; Hogan, D.R.; Hogan, M.C.; Horton, R.; et al. Guidelines for Accurate and Transparent Health Estimates Reporting: the GATHER statement. PLoS Medicine 2016, 13, e1002056. [Google Scholar]
- James, S.L.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A. Global, regional, and national incidence, prevalence, and years lived with disability for 354 diseases and injuries for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2018, 392, 1789–1858. [Google Scholar] [CrossRef]
- GBD Collaborative Network. Global Burden of Disease Study 2019 (GBD 2019) Results. Available online: http://ghdx.healthdata.org/gbd-results-tool (accessed on 21/01/2022).
- Schei, M.A.; Hessen, J.O.; Smith, K.R.; Bruce, N.; McCracken, J.; Lopez, V. Childhood asthma and indoor woodsmoke from cooking in Guatemala. Journal of Exposure Science & Environmental Epidemiology 2004, 14, S110–S117. [Google Scholar] [CrossRef]
- Pijnenburg, M.W.; Nantanda, R. Rising and falling prevalence of asthma symptoms. The Lancet 2021, 398, 1542–1543. [Google Scholar] [CrossRef]
- Martinez, A.; de la Rosa, R.; Mujahid, M.; Thakur, N. Structural racism and its pathways to asthma and atopic dermatitis. Journal of Allergy and Clinical Immunology 2021, 148, 1112–1120. [Google Scholar] [CrossRef]
- Chung, K.F. Airway microbial dysbiosis in asthmatic patients: a target for prevention and treatment? Journal of Allergy and Clinical Immunology 2017, 139, 1071–1081. [Google Scholar] [CrossRef]
- Rehman, A.; Amin, F.; Sadeeqa, S. Prevalence of asthma and its management: A review. The Journal of the Pakistan Medical Association 2018, 68, 1823–1827. [Google Scholar] [PubMed]
- Vedanthan, P.K.; Mahesh, P.A.; Vedanthan, R.; Holla, A.D.; Liu, A.H. Effect of animal contact and microbial exposures on the prevalence of atopy and asthma in urban vs rural children in India. Annals of Allergy, Asthma & Immunology 2006, 96, 571–578. [Google Scholar] [CrossRef]
- D’Amato, G.; Holgate, S.T.; Pawankar, R.; Ledford, D.K.; Cecchi, L.; Al-Ahmad, M.; Al-Enezi, F.; Al-Muhsen, S.; Ansotegui, I.; Baena-Cagnani, C.E. Meteorological conditions, climate change, new emerging factors, and asthma and related allergic disorders. A statement of the World Allergy Organization. World Allergy Organization Journal 2015, 8, 1–52. [Google Scholar] [CrossRef]
- Krishna, M.T.; Mahesh, P.A.; Vedanthan, P.K.; Mehta, V.; Moitra, S.; Christopher, D.J. Pediatric allergic diseases in the Indian subcontinent—Epidemiology, risk factors and current challenges. Pediatric Allergy and Immunology 2020, 31, 735–744. [Google Scholar] [CrossRef]
- To, T.; Stanojevic, S.; Moores, G.; Gershon, A.S.; Bateman, E.D.; Cruz, A.A.; Boulet, L.-P. Global asthma prevalence in adults: findings from the cross-sectional world health survey. BMC public health 2012, 12, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Asher, M.I.; Rutter, C.E.; Bissell, K.; Chiang, C.-Y.; El Sony, A.; Ellwood, E.; Ellwood, P.; García-Marcos, L.; Marks, G.B.; Morales, E. Worldwide trends in the burden of asthma symptoms in school-aged children: Global Asthma Network Phase I cross-sectional study. The Lancet 2021, 398, 1569–1580. [Google Scholar] [CrossRef] [PubMed]
- Yangzong, Y.; Shi, Z.; Nafstad, P.; Håheim, L.L.; Luobu, O.; Bjertness, E. The prevalence of childhood asthma in China: a systematic review. BMC public health 2012, 12, 1–10. [Google Scholar] [CrossRef]
- Shah, R.; Newcomb, D.C. Sex bias in asthma prevalence and pathogenesis. Frontiers in immunology 2018, 9, 2997. [Google Scholar] [CrossRef] [PubMed]
- De Martinis, M.; Sirufo, M.M.; Suppa, M.; Di Silvestre, D.; Ginaldi, L. Sex and gender aspects for patient stratification in allergy prevention and treatment. International journal of molecular sciences 2020, 21, 1535. [Google Scholar] [CrossRef] [PubMed]
- Honkamäki, J.; Hisinger-Mölkänen, H.; Ilmarinen, P.; Piirilä, P.; Tuomisto, L.E.; Andersén, H.; Huhtala, H.; Sovijärvi, A.; Backman, H.; Lundbäck, B. Age-and gender-specific incidence of new asthma diagnosis from childhood to late adulthood. Respiratory medicine 2019, 154, 56–62. [Google Scholar] [CrossRef]
- Asher, I.; Haahtela, T.; Selroos, O.; Ellwood, P.; Ellwood, E. Global Asthma Network survey suggests more national asthma strategies could reduce burden of asthma. Allergologia et Immunopathologia 2017, 45, 105–114. [Google Scholar] [CrossRef] [PubMed]
- Yaghoubi, M.; Adibi, A.; Safari, A.; FitzGerald, J.M.; Sadatsafavi, M. The projected economic and health burden of uncontrolled asthma in the United States. American journal of respiratory and critical care medicine 2019, 200, 1102–1112. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).