Submitted:
20 June 2023
Posted:
21 June 2023
You are already at the latest version
Abstract
Keywords:
Introduction
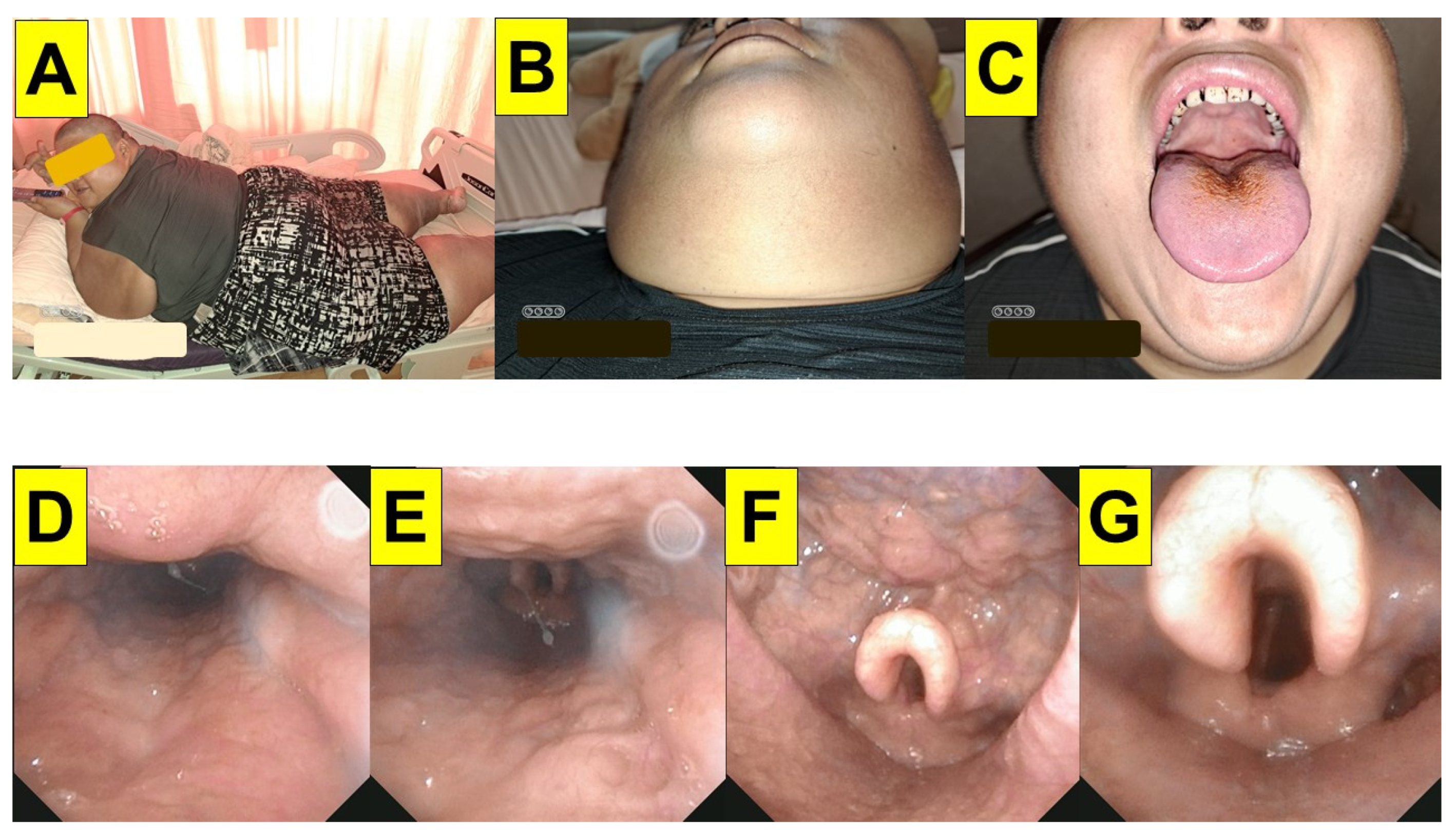
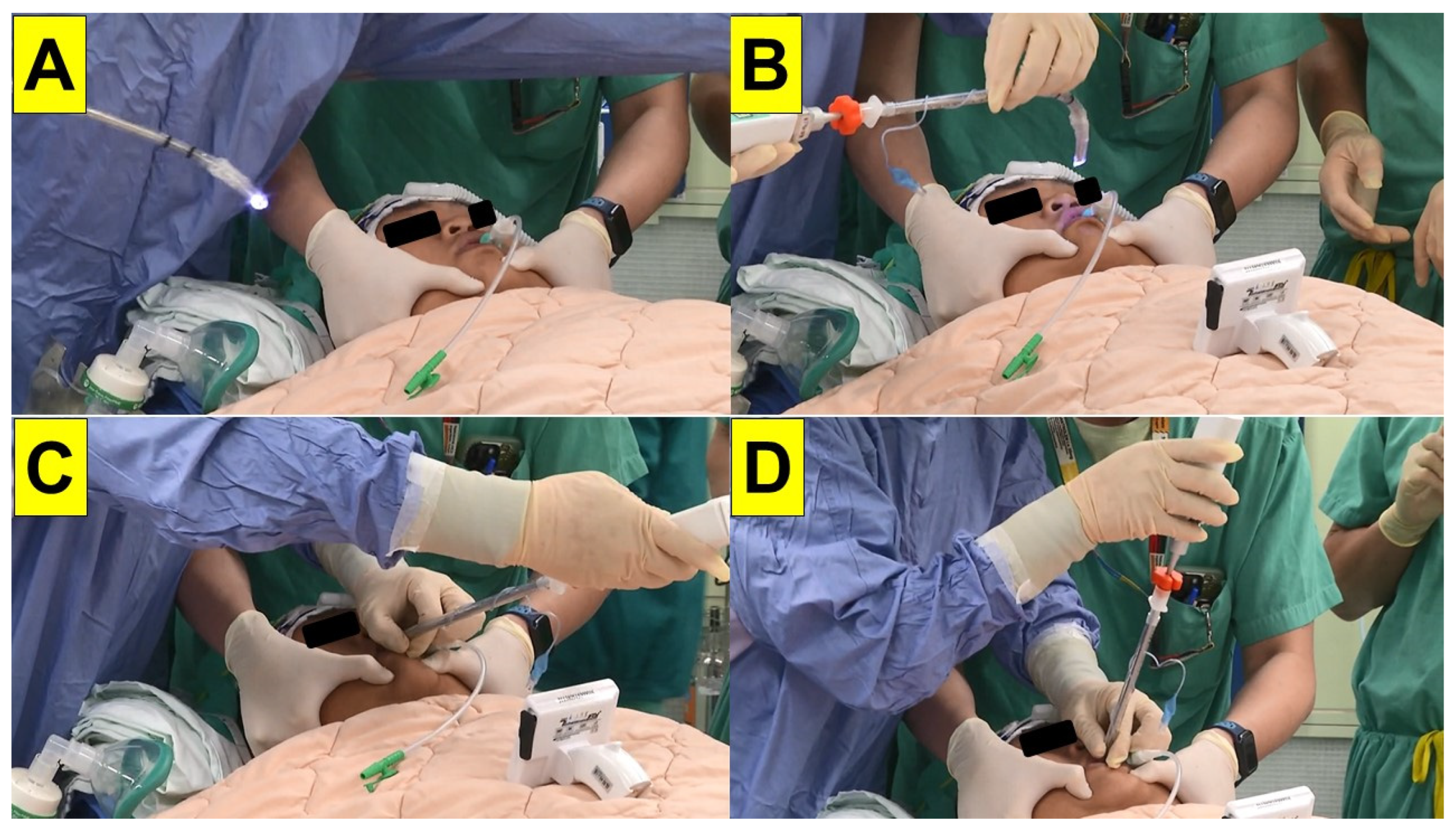
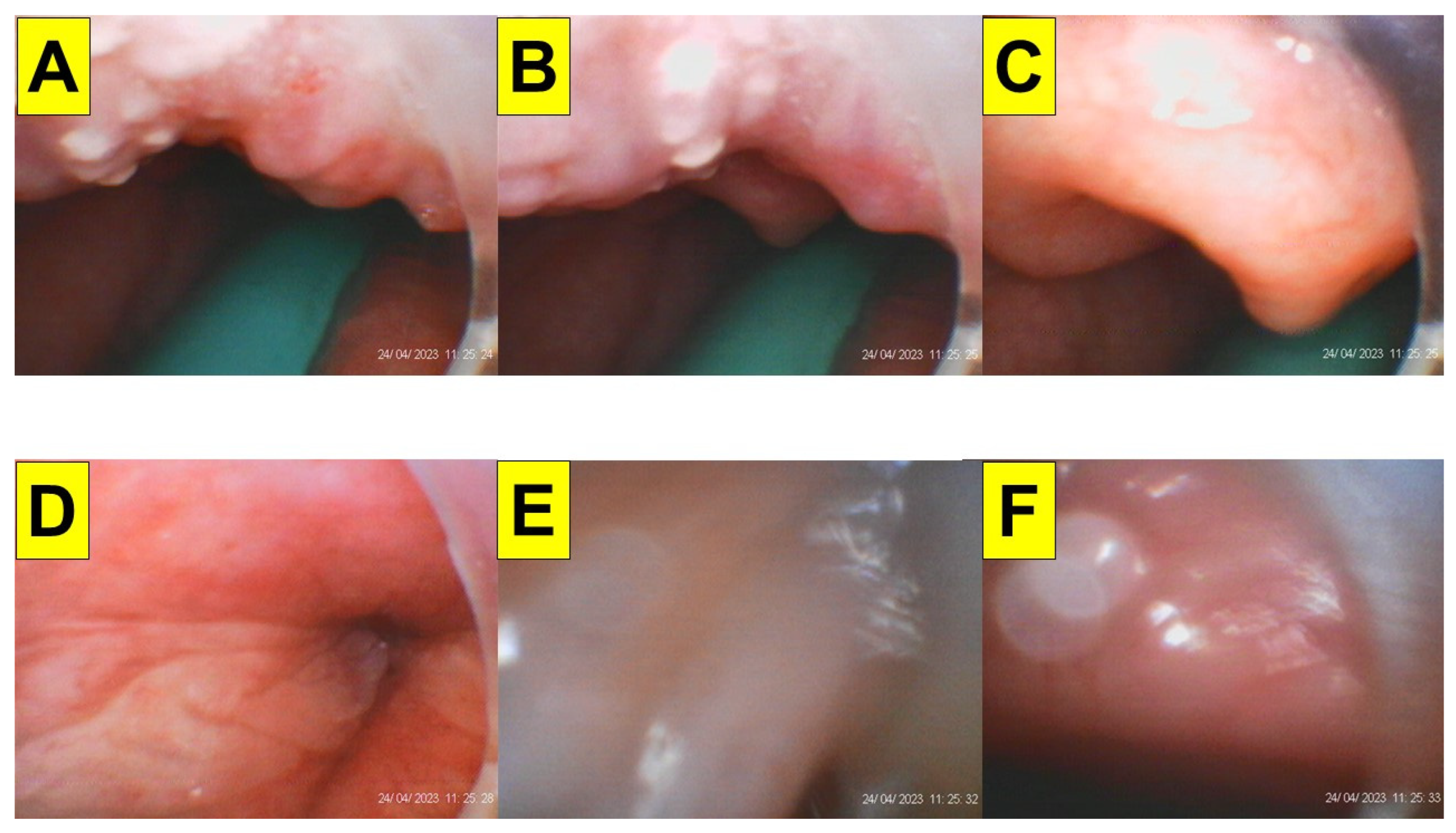
Case presentation
Discussion
| Laryngoscopy (DL/VL) | Styletubation (VS) | |
|---|---|---|
| BMI (kg/m2) |
|
103―86.9 |
| Neck circumference (cm) | 54 | |
| Mallampati class (III/IV) |
|
IV |
| Sterno-mental distance (cm) | 17 | |
| Mouth opening width (interincisor gap) (cm) | 4.5 | |
| Upper lip bite test (II/III) |
|
II |
| Pathologically enlarged, swelled, crowding oral cavity, pharynx, or larynx | NA |
|
| OSAS | + | |
| Intubation time: (DA: > 10 min) |
12 s | |
| Operator’s subjective feeling |
|
Easy, smooth, swift |
| First-pass success rate | First-pass success | |
| Number of attempts (DA: > 2 attempts) |
1 attempt | |
| Cormack-Lehane view (III/IV) | NA (POGO 100%) | |
| De-saturation | 0 | |
| Airway injuries | 0 | |
| POST | 0 | |
| IDS score | NA | |
| DA incidence in MO | 0 |
Conclusion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Leykin, Y.; Pellis, T.; Del Mestro, E.; Marzano, B.; Fanti, G.; Brodsky, J.B. Anesthetic management of morbidly obese and super-morbidly obese patients undergoing bariatric operations: hospital course and outcomes. Obes. Surg. 2006, 16, 1563–1569. [Google Scholar] [CrossRef]
- Gray, K.D.; Pomp, A.; Dakin, G.; Amanat, S.; Turnbull, Z.A.; Samuels, J.; Afaneh, C. Perioperative outcomes and anesthetic considerations of robotic bariatric surgery in a propensity-matched cohort of super obese and super-super obese patients. Surg. Endosc. 2018, 32, 4867–4873. [Google Scholar] [CrossRef]
- Wilkinson, K.H.; Helm, M.; Lak, K.; Higgins, R.M.; Gould, J.C.; Kindel, T.L. The risk of post-operative complications in super-super obesity compared to super obesity in accredited bariatric surgery centers. Obes. Surg. 2019, 29, 2964–2971. [Google Scholar] [CrossRef]
- Kaye, A.D.; Lingle, B.D.; Brothers, J.C.; Rodriguez, J.R.; Morris, A.G.; Greeson, E.M.; Cornett, E.M. The patient with obesity and super-super obesity: Perioperative anesthetic considerations. Saudi. J. Anaesth. 2022, 16, 332–338. [Google Scholar] [CrossRef]
- Brodsky, J.B.; Lemmens, H.J.; Brock-Utne, J.G.; Vierra, M.; Saidman, L.J. Morbid obesity and tracheal intubation. Anesth. Analg. 2002, 94, 732–736. [Google Scholar] [CrossRef] [PubMed]
- Van Zundert, A.A.; Lee, R.A. Intubation difficulties in obese patients. Anesth. Analg. 2009, 108, 1051. [Google Scholar] [CrossRef] [PubMed]
- Kristensen, M.S. Airway management and morbid obesity. Eur. J. Anaesthesiol. 2010, 27, 923–927. [Google Scholar] [CrossRef]
- De Jong, A.; Molinari, N.; Pouzeratte, Y.; Verzilli, D.; Chanques, G.; Jung, B.; Futier, E.; Perrigault, P.F.; Colson, P.; Capdevila, X.; Jaber, S. Difficult intubation in obese patients: incidence, risk factors, and complications in the operating theatre and in intensive care units. Br. J. Anaesth. 2015, 114, 297–306. [Google Scholar] [CrossRef]
- Petrini, F.; Di Giacinto, I.; Cataldo, R.; Esposito, C.; Pavoni, V.; Donato, P.; Trolio, A.; Merli, G.; Sorbello, M.; Pelosi, P. Obesity Task Force for the SIAARTI Airway Management Study Group. Perioperative and periprocedural airway management and respiratory safety for the obese patient: 2016 SIAARTI Consensus. Minerva Anestesiol. 2016, 82, 1314–1335. [Google Scholar] [PubMed]
- Wojcikiewicz, T.; Cousins, J.; Margarson, M. The bariatric airway. Br. J. Hosp. Med. (Lond). 2018, 79, 612–619. [Google Scholar] [CrossRef] [PubMed]
- Moon, T.S.; Fox, P.E.; Somasundaram, A.; Minhajuddin, A.; Gonzales, M.X.; Pak, T.J.; Ogunnaike, B. The influence of morbid obesity on difficult intubation and difficult mask ventilation. J. Anesth. 2019, 33, 96–102. [Google Scholar] [CrossRef]
- Liew, W.J.; Negar, A.; Singh, P.A. Airway management in patients suffering from morbid obesity. Saudi. J. Anaesth. 2022, 16, 314–321. [Google Scholar] [CrossRef]
- Thota, B.; Jan, K.M.; Oh, M.W.; Moon, T.S. Airway management in patients with obesity. Saudi. J. Anaesth. 2022, 16, 76–81. [Google Scholar] [CrossRef] [PubMed]
- Juvin, P.; Lavaut, E.; Dupont, H.; Lefevre, P.; Demetriou, M.; Dumoulin, J.L.; Desmonts, J.M. Difficult tracheal intubation is more common in obese than in lean patients. Anesth. Analg. 2003, 97, 595–600. [Google Scholar] [CrossRef]
- Saasouh, W.; Laffey, K.; Turan, A.; Avitsian, R.; Zura, A.; You, J.; Zimmerman, N.M.; Szarpak, L.; Sessler, D.I.; Ruetzler, K. Degree of obesity is not associated with more than one intubation attempt: a large centre experience. Br. J. Anaesth. 2018, 120, 1110–1116. [Google Scholar] [CrossRef]
- Lundstrøm, L.H.; Møller, A.M.; Rosenstock, C.; Astrup, G.; Wetterslev, J. High body mass index is a weak predictor for difficult and failed tracheal intubation: a cohort study of 91,332 consecutive patients scheduled for direct laryngoscopy registered in the Danish Anesthesia Database. Anesthesiology. 2009, 110, 266–274. [Google Scholar] [CrossRef]
- Apfelbaum, J.L.; Hagberg, C.A.; Connis, R.T.; Abdelmalak, B.B.; Agarkar, M.; Dutton, R.P.; Fiadjoe, J.E.; Greif, R.; Klock, P.A.; Mercier, D.; Myatra, S.N.; O'Sullivan, E.P.; Rosenblatt, W.H.; Sorbello, M.; Tung, A. 2022 American Society of Anesthesiologists Practice Guidelines for Management of the Difficult Airway. Anesthesiology. 2022, 136, 31–81. [Google Scholar] [CrossRef]
- Pieters, B.M.A.; Maas, E.H.A.; Knape, J.T.A.; van Zundert, A.A.J. Videolaryngoscopy vs. direct laryngoscopy use by experienced anaesthetists in patients with known difficult airways: a systematic review and meta-analysis. Anaesthesia 2017, 72, 1532–1541. [Google Scholar] [CrossRef]
- Hansel, J.; Rogers, A.M.; Lewis, S.R.; Cook, T.M.; Smith, A.F. Videolaryngoscopy versus direct laryngoscopy for adults undergoing tracheal intubation. Cochrane Database Syst. Rev. 2022, 4, CD011136. [Google Scholar] [CrossRef]
- Marrel, J.; Blanc, C.; Frascarolo, P.; Magnusson, L. Videolaryngoscopy improves intubation condition in morbidly obese patients. Eur. J. Anaesthesiol. 2007, 24, 1045–1049. [Google Scholar] [CrossRef] [PubMed]
- Ndoko, S.K.; Amathieu, R.; Tual, L.; Polliand, C.; Kamoun, W.; El Housseini, L.; Champault, G.; Dhonneur, G. Tracheal intubation of morbidly obese patients: a randomized trial comparing performance of Macintosh and Airtraq laryngoscopes. Br. J. Anaesth. 2008, 100, 263–268. [Google Scholar] [CrossRef]
- Maassen, R.; Lee, R.; van Zundert, A.; Cooper, R. The videolaryngoscope is less traumatic than the classic laryngoscope for a difficult airway in an obese patient. J. Anesth. 2009, 23, 445–448. [Google Scholar] [CrossRef]
- Dhonneur, G,; Abdi, W.; Ndoko, S.K.; Amathieu, R.; Risk, N.; El Housseini, L.; Polliand, C.; Champault, G.; Combes, X.; Tual, L. Video-assisted versus conventional tracheal intubation in morbidly obese patients. Obes. Surg. 2009, 19, 1096–1101. [CrossRef]
- Gaszyński, T. Clinical experience with the C-Mac videolaryngoscope in morbidly obese patients. Anaesthesiol. Intensive Ther. 2014, 46, 14–16. [Google Scholar] [CrossRef] [PubMed]
- Ranieri, D. Jr.; Zinelli, F.R.; Neubauer, A.G.; Schneider, A.P.; do Nascimento, P. Jr. Preanesthetic assessment data do not influence the time for tracheal intubation with Airtraq™ video laryngoscope in obese patients. Braz. J. Anesthesiol. 2014, 64, 190–194. [Google Scholar] [CrossRef]
- Gaszyński, T. Comparison of the glottic view during video-intubation in super obese patients: a series of cases. Ther. Clin. Risk Manag. 2016, 12, 1677–1682. [Google Scholar] [CrossRef] [PubMed]
- Yumul, R.; Elvir-Lazo, O.L.; White, P.F.; Sloninsky, A.; Kaplan, M.; Kariger, R.; Naruse, R.; Parker, N.; Pham, C.; Zhang, X.; Wender, R.H. Comparison of three video laryngoscopy devices to direct laryngoscopy for intubating obese patients: a randomized controlled trial. J. Clin. Anesth. 2016, 31, 71–77. [Google Scholar] [CrossRef] [PubMed]
- Hoshijima, H.; Denawa, Y.; Tominaga, A.; Nakamura, C.; Shiga, T.; Nagasaka, H. Videolaryngoscope versus Macintosh laryngoscope for tracheal intubation in adults with obesity: A systematic review and meta-analysis. J. Clin. Anesth. 2018, 44, 69–75. [Google Scholar] [CrossRef]
- Arslan, Z.İ.; Yörükoğlu, H.U. Tracheal intubation with the McGrath MAC X-blade videolaryngoscope in morbidly obese and nonobese patients. Turk. J. Med. Sci. 2019, 49, 1540–1546. [Google Scholar] [CrossRef]
- Brozek, T.; Bruthans, J.; Porizka, M.; Blaha, J.; Ulrichova, J.; Michalek, P. A Randomized comparison of non-channeled GlidescopeTM Titanium versus channeled KingVisionTM videolaryngoscope for orotracheal intubation in obese patients with BMI > 35 kg·m-2. Diagnostics (Basel). 2020, 10, 1024. [Google Scholar] [CrossRef]
- Andersen, L.H.; Rovsing, L.; Olsen, K.S. GlideScope videolaryngoscope vs. Macintosh direct laryngoscope for intubation of morbidly obese patients: a randomized trial. Acta Anaesthesiol. Scand. 2011, 55, 1090–1097. [Google Scholar] [CrossRef]
- Abdallah, R.; Galway, U.; You, J.; Kurz, A.; Sessler, D.I.; Doyle, D.J. A randomized comparison between the Pentax AWS video laryngoscope and the Macintosh laryngoscope in morbidly obese patients. Anesth. Analg. 2011, 113, 1082–1087. [Google Scholar] [CrossRef] [PubMed]
- Ander, F.; Magnuson, A.; Berggren, L.; Ahlstrand, R.; de Leon, A. Time-to-intubation in obese patients. A randomized study comparing direct laryngoscopy and videolaryngoscopy in experienced anesthetists. Minerva Anestesiol. 2017, 83, 906–913. [Google Scholar] [CrossRef]
- Castillo-Monzón, C.G.; Marroquín-Valz, H.A.; Fernández-Villacañas-Marín, M.; Moreno-Cascales, M.; García-Rojo, B.; Candia-Arana, C.A. Comparison of the macintosh and airtraq laryngoscopes in morbidly obese patients: a randomized and prospective study. J. Clin. Anesth. 2017, 36, 136–141. [Google Scholar] [CrossRef] [PubMed]
- Nicholson, A.; Smith, A.F.; Lewis, S.R.; Cook, T.M. Tracheal intubation with a flexible intubation scope versus other intubation techniques for obese patients requiring general anaesthesia. Cochrane Database Syst. Rev. 2014, 17, CD010320. [Google Scholar] [CrossRef] [PubMed]
- Aikins, N.L.; Ganesh, R.; Springmann, K.E.; Lunn, J.J.; Solis-Keus, J. Difficult airway management and the novice physician. J. Emerg. Trauma Shock. 2010, 3, 3,9–12. [Google Scholar] [CrossRef]
- Abdelmalak, B.B.; Bernstein, E.; Egan, C.; Abdallah, R.; You, J.; Sessler, D.I.; Doyle, D.J. GlideScope® vs flexible fibreoptic scope for elective intubation in obese patients. Anaesthesia. 2011, 66, 550–555. [Google Scholar] [CrossRef]
- Abdellatif, A.A.; Ali, M.A. GlideScope videolaryngoscope versus flexible fiberoptic bronchoscope for awake intubation of morbidly obese patient with predicted difficult intubation. Middle East J. Anaesthesiol. 2014, 22, 385–392. [Google Scholar]
- Gaszynski, T.; Pietrzyk, M.; Szewczyk, T.; Gaszynska, E. A comparison of performance of endotracheal intubation using the Levitan FPS optical stylet or Lary-Flex videolaryngoscope in morbidly obese patients. Scientific World Journal. 2014, 2014, 207591. [Google Scholar] [CrossRef]
- Chung, M.Y.; Park, B.; Seo, J.; Kim, C.J. Successful airway management with combined use of McGrath® MAC video laryngoscope and fiberoptic bronchoscope in a severe obese patient with huge goiter-a case report. Korean J. Anesthesiol. 2018, 71, 232–236. [Google Scholar] [CrossRef]
- Luk, H.N.; Qu, J.Z.; Shikani, A. Styletubation: The paradigmatic role of video-assisted intubating stylet technique for routine tracheal intubation. Asian J. Anesthesiol. 2023. Apr 20. [Google Scholar] [CrossRef]
- Gaszynski, T. Standard clinical tests for predicting difficult intubation are not useful among morbidly obese patients. Anesth. Analg. 2004, 99, 956. [Google Scholar] [CrossRef] [PubMed]
- Dixit, A.; Kulshrestha, M.; Mathews, J.J.; Bhandari, M. Are the obese difficult to intubate? Br. J. Anaesth. 2014, 112, 770–771. [Google Scholar] [CrossRef] [PubMed]
- Riad, W.; Vaez, M.N.; Raveendran, R.; Tam, A.D.; Quereshy, F.A.; Chung, F.; Wong, D.T. Neck circumference as a predictor of difficult intubation and difficult mask ventilation in morbidly obese patients: A prospective observational study. Eur. J. Anaesthesiol. 2016, 33, 244–249. [Google Scholar] [CrossRef] [PubMed]
- Siriussawakul, A.; Limpawattana, P. A validation study of the intubation difficulty scale for obese patients. J. Clin. Anesth. 2016, 33, 86–91. [Google Scholar] [CrossRef] [PubMed]
- Siriussawakul, A.; Maboonyanon, P.; Kueprakone, S.; Samankatiwat, S.; Komoltri, C.; Thanakiattiwibun, C. Predictive performance of a multivariable difficult intubation model for obese patients. PLoS One 2018, 13, e0203142. [Google Scholar] [CrossRef]
- Lavi, R.; Segal, D.; Ziser, A. Predicting difficult airways using the intubation difficulty scale: a study comparing obese and non-obese patients. J. Clin. Anesth. 2009, 21, 264–267. [Google Scholar] [CrossRef]
- Pieters, B.; Maassen, R.; Van Eig, E.; Maathuis, B.; Van Den Dobbelsteen, J.; Van Zundert, A. Indirect videolaryngoscopy using Macintosh blades in patients with non-anticipated difficult airways results in significantly lower forces exerted on teeth relative to classic direct laryngoscopy: a randomized crossover trial. Minerva Anestesiol. 2015, 81, 846–854. [Google Scholar]
- Kleine-Brueggeney, M.; Greif, R.; Schoettker, P.; Savoldelli, G.L.; Nabecker, S.; Theiler, L.G. Evaluation of six videolaryngoscopes in 720 patients with a simulated difficult airway: a multicentre randomized controlled trial. Br. J. Anaesth. 2016, 116, 670–679. [Google Scholar] [CrossRef]
- Aziz, M.F.; Bayman, E.O.; Van Tienderen, M.M.; Todd, M.M.; StAGE Investigator Group; Brambrink AM. Predictors of difficult videolaryngoscopy with GlideScope® or C-MAC® with D-blade: secondary analysis from a large comparative videolaryngoscopy trial. Br. J. Anaesth. 2016, 117, 118–123. [Google Scholar] [CrossRef]
- Schieren, M.; Kleinschmidt, J.; Schmutz, A.; Loop, T.; Staat, M.; Gatzweiler, K.H.; Wappler, F.; Defosse, J. Comparison of forces acting on maxillary incisors during tracheal intubation with different laryngoscopy techniques: a blinded manikin study. Anaesthesia. 2019, 74, 1563–1571. [Google Scholar] [CrossRef] [PubMed]
- Luk, H.N.; Luk, H.N.; Qu, J.Z.; Shikani, A. A paradigm shift of airway management: The role of video-assisted intubating stylet technique. In: Jessica Lovich-Sapola (Ed.), Advances in Tracheal Intubation [Working Title]. IntechOpen [Internet] London, United Kingdom. 2022. [Google Scholar] [CrossRef]
- Tsai, P.B.; Luk, H.N. Plastic sheet and video intubating stylet: A technical note. Asian J. Anesthesiol. 2021, 59, 117–121. [Google Scholar] [CrossRef] [PubMed]
- Tsay, P.J.; Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted intubating stylet technique for difficult intubation: A Case Series Report. Healthcare (Basel). 2022, 10, 741. [Google Scholar] [CrossRef] [PubMed]
- Shih, T.L.; Koay, K.P.; Hu, C.Y.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of the Shikani video-assisted intubating stylet technique in patients with restricted neck mobility. Healthcare (Basel). 2022, 10, 1688. [Google Scholar] [CrossRef] [PubMed]
- Yang, C.P.; Luk, H.N.; Qu, J.Z.; Shikani, A. The use of a video-assisted intubating stylet technique in a critically ill and contagious COVID-19 patient. Healthcare (Basel). 2022, 10, 388. [Google Scholar] [CrossRef]
- Huang, C.H.; Su, I.M.; Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-assisted stylet intubation with a plastic sheet barrier, a safe and simple technique for tracheal intubation of COVID-19 patients. Healthcare (Basel). 2022, 10, 1105. [Google Scholar] [CrossRef]
- Jhuang, B.J.; Luk, H.N.; Qu, J.Z.; Shikani, A. Video-twin technique for airway management, combining video-intubating stylet with videolaryngoscope: A case series report and review of the literature. Healthcare (Basel). 2022, 10, 2175. [Google Scholar] [CrossRef]

Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





