Submitted:
29 June 2023
Posted:
03 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Study Population: The EPIC-Heidelberg Cohort
2.2. Assessment of Habitual Diet
2.3. Prospective Ascertainment of Mortality Endpoints
2.4. Statistical Analyses
3. Results
3.1. Cohort Characteristics
3.2. Association of non-dietary Lifestyle Factors with Mortality
3.3. Association of Lifestyle Factors with Animal Protein-rich Food-groups
3.4. Association of Animal protein-rich Foods with Mortality
4. Discussion
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Popkin, B.M. The nutrition transition and its health implications in lower-income countries. Public Heal. Nutr. 1998, 1, 5–21. [Google Scholar] [CrossRef]
- Ritchie, H.; Rosado, P.; Roser, M. Diet compositions. Available online: https://ourworldindata.org/diet-compositions (accessed on 20 April 2023).
- Schmidhuber, J.; Sur, P.; Fay, K.; Huntley, B.; Salama, J.; Lee, A.; Cornaby, L.; Horino, M.; Murray, C.; Afshin, A. The global nutrient database: Availability of macronutrients and micronutrients in 195 countries from 1980 to 2013. Lancet Planet Health 2018, 2, e353–e368. [Google Scholar] [CrossRef]
- Dehghan, M.; Mente, A.; Zhang, X.; Swaminathan, S.; Li, W.; Mohan, V.; Iqbal, R.; Kumar, R.; Wentzel-Viljoen, E.; Rosengren, A.; et al. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet 2017, 390, 2050–2062. [Google Scholar] [CrossRef]
- Penuelas, J.; Krisztin, T.; Obersteiner, M.; Huber, F.; Winner, H.; Janssens, I.A.; Ciais, P.; Sardans, J. Country-level relationships of the human intake of n and p, animal and vegetable food, and alcoholic beverages with cancer and life expectancy. Int J Environ Res Public Health 2020, 17, 7240. [Google Scholar] [CrossRef] [PubMed]
- Grasgruber, P.; Cacek, J.; Hrazdíra, E.; Hřebíčková, S.; Sebera, M. Global correlates of cardiovascular risk: A comparison of 158 countries. Nutrients 2018, 10, 411. [Google Scholar] [CrossRef]
- WHO. Probability of dying between the exact ages 30 and 70 years from cardiovascular diseases, cancer, diabetes, or chronic respiratory diseases (sdg 3.4.1). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/probability-of-dying-between-exact-ages-30-and-70-from-any-of-cardiovascular-disease-cancer-diabetes-or-chronic-respiratory-(-) (accessed on 20 April 2023).
- Wang, H.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abera, S.F.; Abraha, H.N.; GBD 2016 Mortality Collaborators; Murray, C. J.L. Global, regional, and national under-5 mortality, adult mortality, age-specific mortality, and life expectancy, 1970-2016: A systematic analysis for the global burden of disease study 2016. Lancet 2017, 390, 1084–1150. [Google Scholar] [CrossRef]
- Correa, P. Epidemiological correlations between diet and cancer frequency. Cancer Res. 1981, 41. [Google Scholar]
- Ghadirian, P.; Thouez, J.P.; PetitClerc, C. International comparisons of nutrition and mortality from pancreatic cancer. Cancer Detect Prev 1991, 15, 357–362. [Google Scholar]
- Hebert, J.R.; Rosen, A. Nutritional, socioeconomic, and reproductive factors in relation to female breast cancer mortality: Findings from a cross-national study. Cancer Detect Prev 1996, 20, 234–244. [Google Scholar] [PubMed]
- Hebert, J.R.; Landon, J.; Miller, D.R. Consumption of meat and fruit in relation to oral and esophageal cancer: A cross-national study. Nutr Cancer 1993, 19, 169–179. [Google Scholar] [CrossRef]
- Bajracharya, R.; Katzke, V.; Mukama, T.; Kaaks, R. Effect of Iso-Caloric Substitution of Animal Protein for Other Macro Nutrients on Risk of Overall, Cardiovascular and Cancer Mortality: Prospective Evaluation in EPIC-Heidelberg Cohort and Systematic Review. Nutrients 2023, 15, 794. [Google Scholar] [CrossRef]
- Chen, Z.; Glisic, M.; Song, M.; Aliahmad, H.A.; Zhang, X.; Moumdjian, A.C.; Gonzalez-Jaramillo, V.; Van Der Schaft, N.; Bramer, W.M.; Ikram, M.A.; et al. Dietary protein intake and all-cause and cause-specific mortality: results from the Rotterdam Study and a meta-analysis of prospective cohort studies. Eur. J. Epidemiol. 2020, 35, 411–429. [Google Scholar] [CrossRef] [PubMed]
- Virtanen, H.E.; Voutilainen, S.; Koskinen, T.T.; Mursu, J.; Kokko, P.; Ylilauri, M.P.; Tuomainen, T.-P.; Salonen, J.T.; Virtanen, J.K. Dietary proteins and protein sources and risk of death: the Kuopio Ischaemic Heart Disease Risk Factor Study. Am. J. Clin. Nutr. 2019, 109, 1462–1471. [Google Scholar] [CrossRef]
- Budhathoki, S.; Sawada, N.; Iwasaki, M.; Yamaji, T.; Goto, A.; Kotemori, A.; Ishihara, J.; Takachi, R.; Charvat, H.; Mizoue, T.; et al. Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality in a Japanese Cohort. JAMA Intern. Med. 2019, 179, 1509–1518. [Google Scholar] [CrossRef] [PubMed]
- Song, M.; Fung, T.T.; Hu, F.B.; Willett, W.C.; Longo, V.D.; Chan, A.T.; Giovannucci, E.L. Association of Animal and Plant Protein Intake With All-Cause and Cause-Specific Mortality. JAMA Intern. Med. 2016, 176, 1453–1463. [Google Scholar] [CrossRef] [PubMed]
- Wang, M.; Ma, H.; Song, Q.; Zhou, T.; Hu, Y.; Heianza, Y.; Manson, J.E.; Qi, L. Red meat consumption and all-cause and cardiovascular mortality: Results from the uk biobank study. Eur J Nutr 2022, 61, 2543–2553. [Google Scholar] [CrossRef]
- Grau, N.; Mohammadifard, N.; Hassannejhad, R.; Haghighatdoost, F.; Sadegh, M.; Talaei, M.; Sajjadi, F.; Mavrommatis, Y.; Sarrafzadegan, N. Red and processed meat consumption and risk of incident cardiovascular disease and mortality: Isfahan cohort study. Int J Food Sci Nutr 2022, 73, 503–512. [Google Scholar] [CrossRef]
- Sinha, R.; Cross, A.J.; Graubard, B.I.; Leitzmann, M.F.; Schatzkin, A. Meat intake and mortality: A prospective study of over half a million people. Arch Intern Med 2009, 169, 562–571. [Google Scholar] [CrossRef]
- Rohrmann, S.; Linseisen, J. Processed meat: The real villain? Proc Nutr Soc 2016, 75, 233–241. [Google Scholar] [CrossRef]
- Wang, X.; Lin, X.; Ouyang, Y.Y.; Liu, J.; Zhao, G.; Pan, A.; Hu, F.B. Red and processed meat consumption and mortality: Dose-response meta-analysis of prospective cohort studies. Public Health Nutr 2016, 19, 893–905. [Google Scholar] [CrossRef]
- Zhuang, P.; Jiao, J.; Wu, F.; Mao, L.; Zhang, Y. Associations of meat consumption and changes with all-cause mortality in hypertensive patients during 11.4-year follow-up: Findings from a population-based nationwide cohort. Clin. Nutr. 2020, 40, 1077–1084. [Google Scholar] [CrossRef]
- Wang, Y.; Jacobs, E.J.; Shah, R.A.; Stevens, V.L.; Gansler, T.; McCullough, M.L. Red and Processed Meat, Poultry, Fish, and Egg Intakes and Cause-Specific and All-Cause Mortality among Men with Nonmetastatic Prostate Cancer in a U.S. Cohort. Cancer Epidemiology Biomarkers Prev. 2020, 29, 1029–1038. [Google Scholar] [CrossRef]
- Dehghan, M.; Mente, A.; Rangarajan, S.; Sheridan, P.; Mohan, V.; Iqbal, R.; Gupta, R.; Lear, S.; Wentzel-Viljoen, E.; Avezum, A.; et al. Prospective Urban Rural Epidemiology (PURE). Association of dairy intake with cardiovascular disease and mortality in 21 countries from five continents (pure): A prospective cohort study. Lancet 2018, 392, 2288–2297. [Google Scholar] [CrossRef]
- Stasinopoulos, L.C.; Zhou, A.; Hyppönen, E. Association of supplemental calcium and dairy milk intake with all-cause and cause-specific mortality in the uk biobank: A prospective cohort study. Br J Nutr 2020, 123, 574–582. [Google Scholar] [CrossRef] [PubMed]
- O'Sullivan, T.A.; Hafekost, K.; Mitrou, F.; Lawrence, D. Food sources of saturated fat and the association with mortality: A meta-analysis. Am J Public Health 2013, 103, e31–e42. [Google Scholar] [CrossRef]
- Soedamah-Muthu, S.S.; Ding, E.L.; Al-Delaimy, W.K.; Hu, F.B.; Engberink, M.F.; Willett, W.C.; Geleijnse, J.M. Milk and dairy consumption and incidence of cardiovascular diseases and all-cause mortality: Dose-response meta-analysis of prospective cohort studies. The American journal of clinical nutrition 2011, 93, 158–171. [Google Scholar] [CrossRef]
- Larsson, S.C.; Crippa, A.; Orsini, N.; Wolk, A.; Michaëlsson, K. Milk consumption and mortality from all causes, cardiovascular disease, and cancer: A systematic review and meta-analysis. Nutrients 2015, 7, 7749–7763. [Google Scholar] [CrossRef]
- Riboli, E.; Hunt, K.; Slimani, N.; Ferrari, P.; Norat, T.; Fahey, M.; Charrondière, U.; Hémon, B.; Casagrande, C.; Vignat, J.; et al. European Prospective Investigation into Cancer and Nutrition (EPIC): study populations and data collection. Public Health Nutr. 2002, 5, 1113–1124. [Google Scholar] [CrossRef] [PubMed]
- Boeing, H.; Korfmann, A.; Bergmann, M.M. Recruitment procedures of epic-germany. European investigation into cancer and nutrition. Ann Nutr Metab 1999, 43, 205–215. [Google Scholar] [CrossRef]
- Boeing, H.; Wahrendorf, J.; Becker, N. EPIC-Germany – A Source for Studies into Diet and Risk of Chronic Diseases. Ann. Nutr. Metab. 1999, 43, 195–204. [Google Scholar] [CrossRef] [PubMed]
- Bohlscheid-Thomas, S.; Hoting, I.; Boeing, H.; Wahrendorf, J. Reproducibility and relative validity of energy and macronutrient intake of a food frequency questionnaire developed for the German part of the EPIC project. European Prospective Investigation into Cancer and Nutrition. Leuk. Res. 1997, 26, 71S–81. [Google Scholar] [CrossRef] [PubMed]
- Kaaks, R.; Slimani, N.; Riboli, E. Pilot phase studies on the accuracy of dietary intake measurements in the EPIC project: overall evaluation of results. European Prospective Investigation into Cancer and Nutrition. Leuk. Res. 1997, 26, 26S–36. [Google Scholar] [CrossRef] [PubMed]
- Bohlscheid-Thomas, S.; Hoting, I.; Boeing, H.; Wahrendorf, J. Reproducibility and relative validity of food group intake in a food frequency questionnaire developed for the German part of the EPIC project. European Prospective Investigation into Cancer and Nutrition. Leuk. Res. 1997, 26, 59S–70. [Google Scholar] [CrossRef] [PubMed]
- Deharveng, G.; Charrondière, U.; Slimani, N.; Southgate, D.; Riboli, E. Comparison of nutrients in the food composition tables available in the nine European countries participating in EPIC. Eur. J. Clin. Nutr. 1999, 53, 60–79. [Google Scholar] [CrossRef]
- Pesch, B.; Kendzia, B.; Gustavsson, P.; Jöckel, K.H.; Johnen, G.; Pohlabeln, H.; Olsson, A.; Ahrens, W.; Gross, I.M.; Brüske, I.; et al. Cigarette smoking and lung cancer--relative risk estimates for the major histological types from a pooled analysis of case-control studies. Int J Cancer 2012, 131, 1210–1219. [Google Scholar] [CrossRef]
- Choi, S.Y.; Kahyo, H. Effect of Cigarette Smoking and Alcohol Consumption in the Aetiology of Cancer of the Oral Cavity, Pharynx and Larynx. Leuk. Res. 1991, 20, 878–885. [Google Scholar] [CrossRef]
- Liu, X.; Peveri, G.; Bosetti, C.; Bagnardi, V.; Specchia, C.; Gallus, S.; Lugo, A. Dose-response relationships between cigarette smoking and kidney cancer: A systematic review and meta-analysis. Crit. Rev. Oncol. 2019, 142, 86–93. [Google Scholar] [CrossRef]
- Islami, F.; Fedirko, V.; Tramacere, I.; Bagnardi, V.; Jenab, M.; Scotti, L.; Rota, M.; Corrao, G.; Garavello, W.; Schüz, J.; et al. Alcohol drinking and esophageal squamous cell carcinoma with focus on light-drinkers and never-smokers: A systematic review and meta-analysis. Int. J. Cancer 2010, 129, 2473–2484. [Google Scholar] [CrossRef]
- Liu, Y.; De, A. Multiple Imputation by Fully Conditional Specification for Dealing with Missing Data in a Large Epidemiologic Study. Int. J. Stat. Med Res. 2015, 4, 287–295. [Google Scholar] [CrossRef]
- Huang, J.; Liao, L.M.; Weinstein, S.J.; Sinha, R.; Graubard, B.I.; Albanes, D. Association Between Plant and Animal Protein Intake and Overall and Cause-Specific Mortality. JAMA Intern. Med. 2020, 180, 1173. [Google Scholar] [CrossRef]
- Brandt, P.A.v.d. Red meat, processed meat, and other dietary protein sources and risk of overall and cause-specific mortality in the netherlands cohort study. European journal of epidemiology 2019, 34, 351–369. [Google Scholar] [CrossRef] [PubMed]
- Lu, Y.; Sugawara, Y.; Matsuyama, S.; Fukao, A.; Tsuji, I. Association of dairy intake with all-cause, cancer, and cardiovascular disease mortality in japanese adults: A 25-year population-based cohort. Eur J Nutr 2022, 61, 1285–1297. [Google Scholar] [CrossRef] [PubMed]
- Battaglia Richi, E.; Baumer, B.; Conrad, B.; Darioli, R.; Schmid, A.; Keller, U. Health risks associated with meat consumption: A review of epidemiological studies. Int J Vitam Nutr Res 2015, 85, 70–78. [Google Scholar] [CrossRef] [PubMed]
- Larsson, S.C.; Orsini, N. Red meat and processed meat consumption and all-cause mortality: A meta-analysis. Am J Epidemiol 2014, 179, 282–289. [Google Scholar] [CrossRef]
| Characteristics | Total N (%) |
Men N (%) |
Women N (%) |
|---|---|---|---|
| n | 22,748 | 10,600 (46.6) | 12,148 (53.4) |
| Age at recruitment (years, inter-quartile range) | 51.1 (43.5-57.5) | 52.8 (46.4-58.1) | 48.7 (41.7-56.7) |
| Smoking intensity | |||
| Never | 9,722 (42.7) | 3,545 (33.4) | 6,177 (50.8) |
| Former (quit > 10 years) | 5,208 (22.8) | 3,005 (28.3) | 2,203 (18.1) |
| Former (quit ≤ 10 years) | 2,509 (11.0) | 1,329 (12.5) | 1,180 (9.7) |
| Current (≤ 15 cig. Per day) | 2,550 (11.2) | 921 (8.6) | 1,629 (13.4) |
| Current (> 15 cig. Per day) | 2,339 (10.2) | 1,402 (13.2) | 937 (7.7) |
| Pipe/cigar/occasional | 420 (1.8) | 398 (3.7) | 22 (0.1) |
| Waist circumference level * | |||
| Low waist circumference | 11,016 (48.4) | 4,673 (44.0) | 6,343 (52.2) |
| Moderate waist circumference | 5,922 (26.0) | 3,204 (30.2) | 2,718 (22.3) |
| High waist circumference | 5,810 (25.5) | 2,723 (25.6) | 3,087 (25.4) |
| Body mass index | |||
| <25 | 10,040 (44.1) | 3,297 (31.1) | 6,743 (55.5) |
| ≥25-<30 | 9,120 (40.0) | 5,491 (51.8) | 3,629 (29.8) |
| ≥30 | 3,588 (15.7) | 1,812 (17.0) | 1,776 (14.6) |
| Level of formal education | |||
| University degree | 6,962 (30.6) | 3,952 (37.2) | 3,010 (24.7) |
| Secondary school | 1,639 (7.2) | 594 (5.6) | 1,045 (8.6) |
| Technical school | 7,709 (33.8) | 2,826 (26.6) | 4,883 (40.2) |
| Primary school or none | 6,438 (28.3) | 3,228 (30.4) | 3,210 (26.4) |
| Physical activity level | |||
| Inactive | 2,590 (11.3) | 1,129 (10.6) | 1,461 (12.0) |
| Moderately inactive | 7,951 (34.9) | 3,575 (33.7) | 4,376 (36.0) |
| Moderately active | 6,563 (28.8) | 3,076 (29.0) | 3,487 (28.7) |
| Active | 5,644 (24.8) | 2,820 (26.6) | 2,824 (23.2) |
| Alcohol consumption | |||
| Never | 342 (1.5) | 74 (0.7) | 268 (2.2) |
| Former | 851 (3.7) | 436 (4.1) | 415 (3.4) |
| >0-6 (M)/>0-3 (W) | 5,384 (23.6) | 1,282 (12.0) | 4,102 (33.7) |
| >6-12 (M)/>3-12 (W) | 6,769 (29.7) | 1,614 (15.2) | 5,155 (42.4) |
| >12-24 | 4,680 (20.5) | 3,042 (28.7) | 1,638 (13.4) |
| >24 | 4,722 (20.7) | 4,152 (39.1) | 570 (4.6) |
| Total energy intake (kcal), mean, SD | 1971.3 (632.0) | 2223.5 (666.1) | 1751.3 (506.9) |
| Red meat (g/d), mean, SD | 31.7 (29.7) | 41.6 (35.0) | 23.0 (20.6) |
| Processed meat (g/d), mean, SD | 51.8 (40.6) | 64.4 (45.8) | 40.9 (31.6) |
| Poultry (g/d), mean, SD | 12.5 (14.1) | 13.9 (15.4) | 11.3 (12.7) |
| Cheese (g/d), mean, SD | 29.8 (21.6) | 29.4 (22.6) | 30.1 (20.6) |
| Milk (g/d), mean, SD | 82.4 (138.8) | 81.9 (154.1) | 82.9 (124.0) |
| Overall death | 3486 (15.3) | 2259 (21.3) | 1227 (10.1) |
| Cardiovascular death | 932 (4.1) | 649 (6.1) | 283 (2.3) |
| Cancer death | 1572 (6.9) | 972 (9.1) | 600 (4.9) |
| Strongly smoking-related cancer deaths | 365 (1.6) | 263 (2.4) | 102 (0.8) |
| Strongly alcohol-related cancer deaths | 73 (0.3) | 58 (0.5) | 15 (0.1) |
| Other deaths | 982 (4.3) | 638 (6.0) | 344 (2.8) |
| Overall mortality nCASES=3,486 |
Cardiovascular mortality nCASES=932 |
Cancer mortality | Other mortality nCASES=982 |
|||||
| Overall cancer mortality nCASES=1,572 |
Strongly smoking-related cancer deaths nCASES=365 |
Strongly smoking and alcohol-related cancer deaths nCASES=73 |
Other cancer-related mortality a ncases=1,207 |
|||||
|
Smoking intensity |
Never | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | Former (quit > 10 years) | 1.07(0.98-1.17) | 1.03(0.86-1.23) | 1.11(0.97-1.28) | 1.97(1.32-2.93) * | 1.68(0.79-3.56) | 1.04(0.89-1.21) | 1.01(0.85-1.21) |
| Former (quit ≤ 10 years) | 1.46(1.30-1.64) * | 1.41(1.11-1.78) * | 1.42(1.19-1.70) * | 3.75(2.41-5.82) * | 2.41(0.99-5.87) | 1.21(0.99-1.49) | 1.39(1.10-1.75) * | |
| Current (≤ 15 cig. Per day) | 2.07(1.85-2.30) * | 2.12(1.70-2.64) * | 1.86(1.57-2.21) * | 6.46(4.32-9.65) * | 2.35(0.89-6.23) | 1.47(1.21-1.79) * | 2.18(1.77-2.69) * | |
| Current (> 15 cig. Per day) | 3.62(3.29-3.98) * | 3.65(3.02-4.42) * | 3.52(3.04-4.07) * | 20.77(14.76-29.22) * | 10.41(5.26-20.59) * | 1.97(1.63-2.37) * | 3.76(3.12-4.53) * | |
| Waist circumference level b | <80/<94 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | 80-<88/94<102 | 1.16(1.07-1.26) * | 1.42(1.19-1.70) * | 1.11(0.98-1.26) | 0.87(0.67-1.12) * | 0.57(0.31-1.08) | 1.23(1.06-1.42) * | 1.01(0.85-1.20) |
| ≥88/≥102 | 1.73(1.61-1.87) * | 2.29(1.95-2.69) * | 1.42(1.26-1.60) * | 1.13(0.88-1.44) | 1.08(0.63-1.85) | 1.55(1.35-1.78) * | 1.82(1.57-2.11) * | |
| Body mass index level | <25 | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | ≥25-<30 | 1.13(1.05-1.23) * | 1.34(1.14-1.59) * | 1.12(0.99-1.25) | 0.82(0.65-1.03) | 0.63(0.38-1.06) | 1.27(1.11-1.46) * | 1.02(0.87-1.19) |
| ≥30 | 1.76(1.62-1.93) * | 2.44(2.04-2.91) * | 1.45(1.26-1.67) * | 0.80(0.59-1.10) | 0.78(0.40-1.54) | 1.75(1.49-2.05) * | 1.75(1.48-2.07) * | |
| Level of formal education | University degree | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | Secondary school | 1.48(1.26-1.73) * | 1.55(1.11-2.17) * | 1.41(1.11-1.78) * | 1.42(0.79-2.56) | 1.91(0.62-5.89) | 1.38(1.07-1.79) * | 1.48(1.08-2.02) * |
| Technical school | 1.41(1.29-1.55) * | 1.43(1.18-1.74) * | 1.36(1.18-1.56) * | 2.26(1.66-3.09) * | 2.03(1.02-4.07) * | 1.21(1.04-1.41) * | 1.51(1.26-1.80) * | |
| Primary school or none | 1.81(1.66-1.97) * | 2.18(1.83-2.61) * | 1.60(1.40-1.83) * | 3.03(2.25-4.09) * | 3.15(1.65-6.01) * | 1.39(1.20-1.62) * | 1.76(1.48-2.09) * | |
| Model 2 | Secondary school | 1.32(1.13-1.54) * | 1.37(0.98-1.92) | 1.27(1.01-1.61) * | 1.10(0.61-1.98) | 1.59(0.51-4.92) | 1.29(1.00-1.67) * | 1.32(0.97-1.81) |
| Technical school | 1.22(1.12-1.34) * | 1.19(0.98-1.45) | 1.21(1.05-1.39) * | 1.85(1.35-2.53) * | 1.88(0.93-3.78) | 1.10(0.94-1.29) | 1.30(1.08-1.55) * | |
| Primary school or none | 1.50(1.37-1.64) * | 1.72(1.43-2.06) * | 1.39(1.21-1.59) * | 2.46(1.81-3.35) * | 2.92(1.50-5.69) * | 1.22(1.05-1.43) * | 1.44(1.21-1.72) * | |
| Physical activity level | Inactive | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | Moderately inactive | 0.68(0.62-0.74) * | 0.75(0.62-0.90) * | 0.78(0.67-0.92) * | 0.66(0.48-0.90) * | 0.70(0.33-1.49) | 0.82(0.69-0.98) * | 0.53(0.44-0.63) * |
| Moderately active | 0.65(0.58-0.71) * | 0.62(0.51-0.76) * | 0.82(0.70-0.96) * | 0.71(0.51-0.98) * | 0.85(0.40-1.82) | 0.86(0.72-1.03) | 0.50(0.41-0.60) * | |
| Active | 0.68(0.61-0.75) * | 0.65(0.52-0.79) * | 0.77(0.65-0.91) * | 0.65(0.46-0.91) * | 0.84(0.39-1.83) | 0.82(0.68-0.99) * | 0.61 (0.51-0.74) * | |
| Alcohol consumption c | Currently low | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| Model 1 | Currently moderately low | 1.46(1.14-1.87) * | 1.49(0.90-2.45) | 1.01(0.64-1.59) | 1.01(0.31-3.26) | - | 1.09(0.67-1.79) | 1.83(1.18-2.86) * |
| Currently moderately high | 2.29(1.99-2.64) * | 2.00(1.49-2.69) * | 2.02(1.61-2.54) * | 4.13(2.67-6.39) * | 16.73(6.05-46.25) * | 1.64(1.25-2.16) * | 2.89(2.24-3.74) * | |
| Currently high | 0.86(0.77-0.95) * | 0.80(0.65-0.99) * | 0.90(0.77-1.05) | 1.04(0.72-1.50) | 1.67(0.58-4.83) | 0.86(0.72-1.02) | 0.85(0.69-1.04) | |
| Former | 0.90(0.81-1.01) | 0.87(0.69-1.08) | 0.96(0.81-1.14) | 0.98(0.66-1.45) | 1.53(0.51-4.52) | 0.96(0.80-1.16) | 0.89(0.72-1.11) | |
| Never | 1.40(1.26-1.56) * | 1.39(1.13-1.72) * | 1.42(1.21-1.67) * | 2.16(1.51-3.07) * | 3.61(1.34-9.76) * | 1.24(1.03-1.50) * | 1.42(1.16-1.74) * | |
| Red meat | Processed meat | Poultry | Cheese | Milk | |||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
|
Smoking status |
Never | 29.4 | 48.6 | 12.3 | 29.6 | 80.8 | |||||
| Former (quit > 10 years) | +2.4 | +8.1% | +3.3 | +6.8% | +0.2 | +1.6% | +1.1 | +3.7% | -3.4 | -4.2% | |
| Former (quit ≤ 10 years) | +2.3 | +7.8% | +5.1 | +10.5% | +1 | +8.1% | +1.3 | +4.3% | +1.9 | +2.3% | |
| Current (≤ 15 cig. Per day) | +0.7 | +2.3% | +3.2 | +6.6% | -0.2 | -1.6 | +0.6 | +2.0% | +4.9 | +6.0% | |
| Current (> 15 cig. Per day) | +13 | +44.2% | +14.7 | +30.3% | +0.7 | +5.6% | -3.1 | -10.4% | +15.6 | +19.3% | |
| Waist circumference b | <80/<94 | 27.2 | 45.6 | 11.5 | 31 | 86.2 | |||||
| 80-<88/94-<102 | +6.6 | +24.4% | +9.1 | +19.9% | +1.3 | +11.3% | -2.3 | -7.4% | -9.7 | -11.2% | |
| ≥88/≥102 | +11.7 | +43.3% | +15.3 | +33.5% | +2.6 | +22.6% | -2.4 | -7.7% | -5.0 | -5.8% | |
| Body mass index | <25 | 25.3 | 43.2 | 11.1 | 31.6 | 85.4 | |||||
| 25-<30 | +9.9 | +39.2% | +12.9 | +29.7% | +2.1 | +18.9% | -3.2 | -10.1% | -6.3 | -7.3% | |
| ≥30 | +16.2 | +64.2% | +21.5 | +49.6% | +3.5 | +31.5% | -3.4 | -10.7% | -3.0 | -3.5% | |
| Educational level | University degree | 29.9 | 46.8 | 12.4 | 34 | 94.6 | |||||
| Secondary school | -2.7 | -9.0% | -0.5 | -1.0% | +0.5 | +4.0% | -0.5 | -1.4% | +2.5 | +2.6% | |
| Technical school | +0.3 | +1.0% | +4.3 | +9.1% | 0 | 0% | -5.8 | -17.0% | -17.6 | -18.6% | |
| Primary school or no formal education | +6.7 | +22.7% | +12.9 | +27.5% | +0.6 | +4.8% | -8.2 | -24.0% | -21.6 | -22.1% | |
| Physical activity | Active | 30.4 | 51.8 | 12.2 | 30.4 | 91.6 | |||||
| Moderately active | +1 | +3.2% | -0.4 | -0.7% | +0.4 | +3.2% | -0.2 | -0.6% | -12.6 | -13.7% | |
| Moderately inactive | +1.7 | +5.5% | +0.4 | +0.7% | +0.4 | +3.2% | -0.9 | -2.9% | -13 | -14.1% | |
| inactive | +3.6 | +11.8% | +0.2 | +0.3% | +0.4 | +3.2% | -1.9 | -6.2% | -8.9 | -9.7% | |
| Alcohol intakec | Never | 26.6 | 44.6 | 11.1 | 26.8 | 107.2 | |||||
| Former | +4.8 | +17.9% | +9.5 | +20.8% | +1.3 | +11.2% | +2.2 | +8.2% | -6.2 | -5.9% | |
| >0-6 (M)/>0-3 (W) | -1.2 | -4.4% | -1.7 | -3.7% | -0.3 | -2.5% | +2.0 | +7.4% | -15.6 | -14.8% | |
| >6-12 (M)/>3-12 (W) | -0.4 | -1.4% | -0.8 | -1.7% | +0.3 | +2.5% | +3.6 | +13.4% | -22.1 | -21.0% | |
| >12-24 | +7.6 | +28.4% | +9.8 | +21.5% | +1.2 | +10.3% | +3.5 | +13.0% | -25.9 | -24.7% | |
| >24 | +17.7 | +66.2% | +22.3 | +49.0% | +2.7 | +23.2% | +3.0 | +11.1% | -31.7 | -30.2% | |
| Overall mortality nCASES=3768 |
Cardiovascular mortality nCASES=932 |
Cancer mortality | Other mortality nCASES=982 |
|||||
| Overall cancer mortality nCASES=1572 |
Strongly smoking-related cancer deaths nCASES=365 |
Strongly smoking and alcohol-related cancer deaths nCASES=73 |
Other cancer-related mortality a ncases=1,207 |
|||||
| Red meat | ||||||||
| Model 1 b | 1st tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2nd tertile | 1.02(0.94-1.11) | 1.18(0.98-1.41) | 1.00(0.88-1.14) | 0.94(0.71-1.26) | 0.86(0.45-1.66) | 1.03(0.88-1.19) | 0.92(0.78-1.09) | |
| 3rd tertile | 1.25(1.15-1.36) * | 1.40(1.17-1.67) * | 1.20(1.05-1.37) | 1.20(0.91-1.58) | 1.04(0.56-1.93) | 1.21(1.04-1.40) * | 1.20(1.01-1.41) * | |
| P trend | <.001 | <.001 | 0.004 | 0.13 | 0.80 | 0.01 | 0.01 | |
| Model 2 c | 2nd tertile | 0.92(0.85-1.01) | 1.02(0.85-1.22) | 0.93(0.82-1.07) | 0.86(0.64-1.15) | 0.82(0.42-1.59) | 0.96(0.82-1.11) | 0.86(0.72-1.02) |
| 3rd tertile | 1.00(0.92-1.09) | 1.04(0.86-1.24) | 1.00(0.88-1.15) | 0.90(0.68-1.20) | 0.88(0.46-1.66) | 1.03(0.88-1.21) | 0.98(0.83-1.17) | |
| P trend | 0.72 | 0.66 | 0.81 | 0.58 | 0.75 | 0.59 | 0.90 | |
| Processed meat | ||||||||
| Model 1 | 1st tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2nd tertile | 1.09(1.00-1.19) * | 1.31(1.09-1.57) * | 1.12(0.98-1.27) | 1.23(0.92-1.63) | 1.41(0.67-2.96) | 1.09(0.94-1.26) | 0.99(0.84-1.16) | |
| 3rd tertile | 1.27(1.17-1.39) * | 1.76(1.46-2.12) * | 1.20(1.05-1.38) * | 1.29(0.96-1.73) | 2.14(1.05-4.37) * | 1.20(1.03-1.40) * | 1.11(0.94-1.32) | |
| P trend | <.001 | <.001 | 0.007 | 0.09 | 0.025 | 0.01 | 0.19 | |
| Model 2 | 2nd tertile | 0.98(0.90-1.07) | 1.13(0.94-1.36) | 1.04(0.91-1.19) | 1.09(0.81-1.45) | 1.30(0.61-2.77) | 1.02(0.88-1.18) | 0.89(0.75-1.05) |
| 3rd tertile | 1.06(0.97-1.16) | 1.36(1.13-1.64) * | 1.06(0.92-1.22) | 1.09(0.81-1.48) | 1.04(0.98-4.26) | 1.06(0.90-1.24) | 0.92(0.77-1.09) | |
| P trend | 0.16 | <.001 | 0.41 | 0.57 | 0.037 | 0.46 | 0.39 | |
| Poultry | ||||||||
| Model 1 | 1st tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2nd tertile | 0.97(0.90-1.05) | 1.01(0.86-1.18) | 0.97(0.86-1.09) | 0.71(0.55-0.92) * | 1.03(0.60-1.77) | 1.07(0.93-1.22) | 0.93(0.80-1.08) | |
| 3rd tertile | 0.93(0.86-1.00) | 0.89(0.76-1.05) | 0.93(0.83-1.06) | 0.84(0.66-1.08) | 0.63(0.34-1.15) | 0.97(0.84-1.12) | 0.88(0.75-1.03) | |
| P trend | 0.07 | 0.20 | 0.31 | 0.18 | 0.13 | 0.73 | 0.11 | |
| Model 2 | 2nd tertile | 0.99(0.91-1.07) | 1.02(0.87-1.19) | 0.99(0.87-1.11) | 0.80(0.62-1.04) | 1.15(0.66-1.98) | 1.07(0.93-1.22) | 0.95(0.81-1.10) |
| 3rd tertile | 0.92(0.85-1.00) | 0.87(0.74-1.02) | 0.95(0.84-1.07) | 0.98(0.76-1.26) | 0.75(0.41-1.37) | 0.95(0.82-1.09) | 0.88(0.75-1.03) | |
| P trend | 0.06 | 0.09 | 0.43 | 0.88 | 0.36 | 0.48 | 0.11 | |
| Cheese | ||||||||
| Model 1 | 1st tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2nd tertile | 0.85(0.79-0.92) * | 0.80(0.68-0.93) * | 0.79(0.70-0.89) * | 0.64(0.50-0.82) * | 0.73(0.41-1.29) | 0.85(0.74-0.98) * | 1.06(0.91-1.23) | |
| 3rd tertile | 0.80(0.74-0.87) * | 0.80(0.68-0.94) * | 0.79(0.70-0.89) * | 0.55(0.43-0.72) * | 0.69(0.40-1.22) | 0.87(0.76-1.00) | 0.81(0.69-0.96) * | |
| P trend | <.001 | .005 | <.001 | <.001 | 0.20 | 0.05 | 0.01 | |
| Model 2 | 2nd tertile | 0.94(0.87-1.02) | 0.90(0.76-1.05) | 0.86(0.76-0.98) * | 0.80(0.62-1.03) | 0.90(0.50-1.59) | 0.91(0.79-1.04) | 1.16(1.00-1.35) |
| 3rd tertile | 0.94(0.87-1.02) | 0.96(0.82-1.13) | 0.91(0.80-1.03) | 0.78(0.60-1.02) | 0.98(0.55-1.74) | 0.95(0.83-1.10) | 0.96(0.82-1.14) | |
| P trend | 0.14 | 0.61 | 0.13 | 0.06 | 0.93 | 0.51 | 0.79 | |
| Milk | ||||||||
| Model 1 | 1st tertile | Ref | Ref | Ref | Ref | Ref | Ref | Ref |
| 2nd tertile | 0.87(0.81-0.94) * | 0.84(0.71-0.98) * | 0.89(0.79-1.00) | 0.82(0.63-1.05) | 0.86(0.50-1.46) | 0.90(0.78-1.03) | 0.88(0.75-1.02) | |
| 3rd tertile | 0.88(0.81-0.95) * | 0.91(0.78-1.07) | 0.83(0.73-0.93) * | 0.81(0.63-1.04) | 0.57(0.32-1.03) | 0.82(0.71-0.94) | 0.86(0.74-1.00) | |
| P trend | 0.001 | 0.23 | 0.002 | 0.09 | 0.068 | 0.006 | 0.06 | |
| Model 2 | 2nd tertile | 0.92(0.85-0.99) | 0.87(0.75-1.03) | 0.94(0.83-1.06) | 0.91(0.71-1.17) | 0.94(0.55-1.62) | 0.93(0.81-1.06) | 0.93(0.80-1.08) |
| 3rd tertile | 0.95(0.88-1.03) | 0.99(0.85-1.16) | 0.89(0.79-1.01) | 0.93(0.72-1.19) | 0.67(0.37-1.21) | 0.87(0.75-1.00) | 0.93(0.80-1.09) | |
| P trend | 0.23 | 0.86 | 0.08 | 0.55 | 0.19 | 0.05 | 0.40 | |
| Overall mortality nCASES=3768 |
Cardiovascular mortality nCASES=932 |
Cancer mortality | Other mortality nCASES=982 |
|||||
| Cancer mortality nCASES=1,572 |
Strongly smoking-related cancer deaths nCASES=365 |
Strongly smoking and alcohol-related cancer deaths nCASES=73 |
Other cancer-related mortality a ncases=1,207 |
|||||
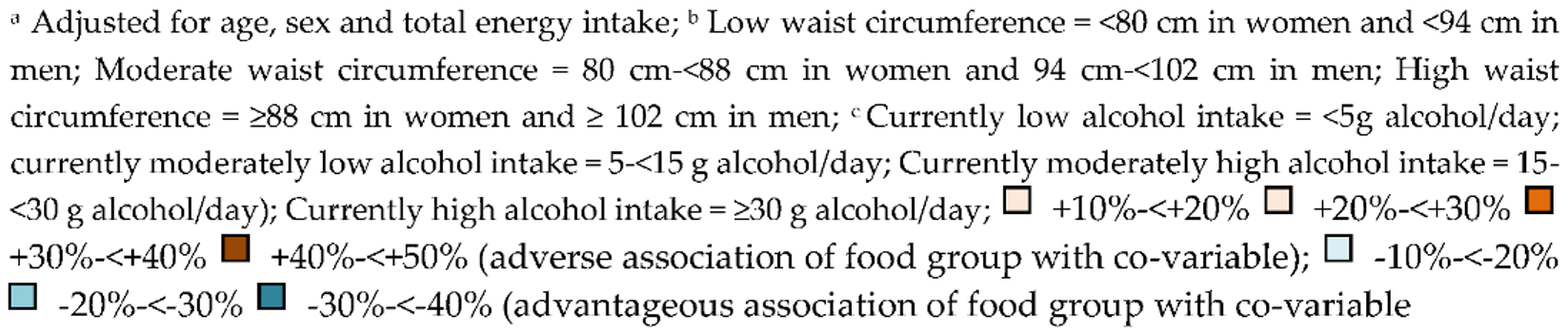
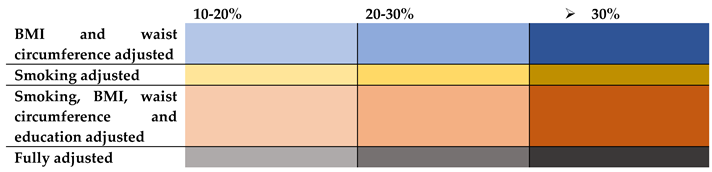
| Red meat | BMI and waist circumference | 10.4 % | 16.4 % | 5.8 % | 5.8 % | 15.3 % | 9.0 % | 11.6 % |
| Smoking | 8 % | 8.5 % | 8.3 % | 22.5 % | 18.2 % | 4.1 % | 8.3 % | |
| Smoking, BMI, waist circumference, and education | 19.2 % | 25.7 % | 15.8 % | 24.1 % | 15.3 % | 14.0 % | 20 % | |
| Fully adjusted | 20 % | 25.7 % | 16.6 % | 25 % | 15.3 % | 14.8 % | 18.3 % | |
| Processed meat | BMI and waist circumference | 10.2 % | 15.9 % | 5.8 % | 6.2 % | 14.0 % | 9.1 % | 11.7 % |
| Smoking | 3.9 % | 3.9 % | 4.1 % | 12.4 % | 9.3 % | 1.6 % | 4.5 % | |
| Smoking, BMI, waist circumference, and education | 17.3 % | 22.7 % | 12.5 % | 18.6 % | 10.7 % | 12.5 % | 18.9 % | |
| Fully adjusted | 16.5 % | 22.7 % | 11.6 % | 15.5 % | 51.4 % | 11.6 % | 17.1 % | |
| Poultry | BMI and waist circumference | 5.3% | 6.7 % | 2.1 % | 3.5 % | 6.3 % | 4.1 % | 4.5 % |
| Smoking | 3.2% | 4.4 % | 4.3 % | 10.7 % | 9.5 % | 2.0 % | 3.4 % | |
| Smoking, BMI, waist circumference, and education | 2.1 % | 3.3 % | 1.0 % | 15.4 % | 15.8 % | 3.0 % | 1.1 % | |
| Fully adjusted | 1.0 % | 2.2 % | 2.1 % | 16.6 % | 19.0 % | 2.0 % | 0 % | |
| Cheese | BMI and waist circumference | 2.5 % | 3.7 % | 1.2 % | 1.81 % | 4.3 % | 2.2 % | 3.7 % |
| Smoking | 7.5 % | 8.7 % | 7.5 % | 25.4 % | 20.2 % | 3.4 % | 8.6 % | |
| Smoking, BMI, waist circumference, and education | 16.2 % | 20 % | 13.9 % | 40 % | 36.2 % | 8.0 % | 17.2 % | |
| Fully adjusted | 17.5 % | 20 % | 15.1 % | 78.1 % | 42.0 % | 9.1 % | 18.5 % | |
| Milk | BMI and waist circumference | 2.2 % | 3.2 % | 1.2 % | 1.23 % | 1.7 % | 1.2 % | 2.3 % |
| Smoking | 1.1 % | 2.1 % | 1.2 % | 4.9 % | 5.2 % | 1.2 % | 2.3 % | |
| Smoking, BMI, waist circumference, and education | 5.6 % | 7.6 % | 4.8 % | 9.8 % | 10.5 % | 3.6 % | 5.8 % | |
| Fully adjusted | 7.9 % | 8.7 % | 7.2 % | 14.8 % | 17.5 % | 6.0 % | 8.1 % | |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





