1. Introduction
The pathway for sound transmission to the inner ear is divided into air conduction (AC) and bone conduction (BC), and hearing aids have been broadly classified into AC and BC hearing aids. In 2004, Hosoi reported that applying vibrations to the auricular cartilage can transmit audible sounds with clarity that is similar to that of AC or BC, leading to the development of a new type of hearing aid called cartilage conduction hearing aids (CC-HAs) [
1].
CC-HAs can amplify and transmit sound signals to the inner ear simply by attaching a vibration generator to the skin of the auricular cartilage [
2,
3]. In contrast, bone conduction hearing aids (BC-HAs) also use a vibration generator placed on the body but require strong pressure and fixation on the temporal bone [
4,
5,
6,
7,
8]. Both types of hearing aids are suitable for individuals with conductive hearing loss or mixed hearing loss, who cannot wear AC-HAs, and those who have good bone conduction thresholds, such as individuals with microtia or external auditory canal atresia .
Since the release of CC-HAs, the attachment-only method has become the preferred option and has gained popularity as an alternative to BC-HAs [
2,
3,
9,
10,
11,
12,
13,
14,
15], particularly in pediatric cases[
16]. Since 2020, safety measures, such as battery boxes, have been fully integrated, allowing the use of the device even for children under the age of 3 years. In the case of infants, there are many opportunities to re-examine the possibility of using CC-HAs after starting from BC-HAs; however, there have been no reports of starting use from infancy. Therefore, in this study, we investigate the usage and wearing progress of CC-HAs in infants and toddlers, present cases of its application from infancy, and discuss its suitability based on the growth of children.
2. Materials and Methods
2.1. Participants
This study enrolled 49 children (17 children with bilateral hearing loss and 32 children with unilateral hearing loss), including 28 boys and 21 girls, in whom trial hearing was initiated using a CC-HA before primary school age at our hospital. The guardians/parents of these children had requested the use of a CC-HA. Trial hearing was initiated between the ages of 0 (3 months old) and 11 years in children with bilateral hearing loss and between 0 (6 months old) and 10 years in those with unilateral hearing loss. The mean age of the participants was 5.02 ± 2.71 (SD) years.
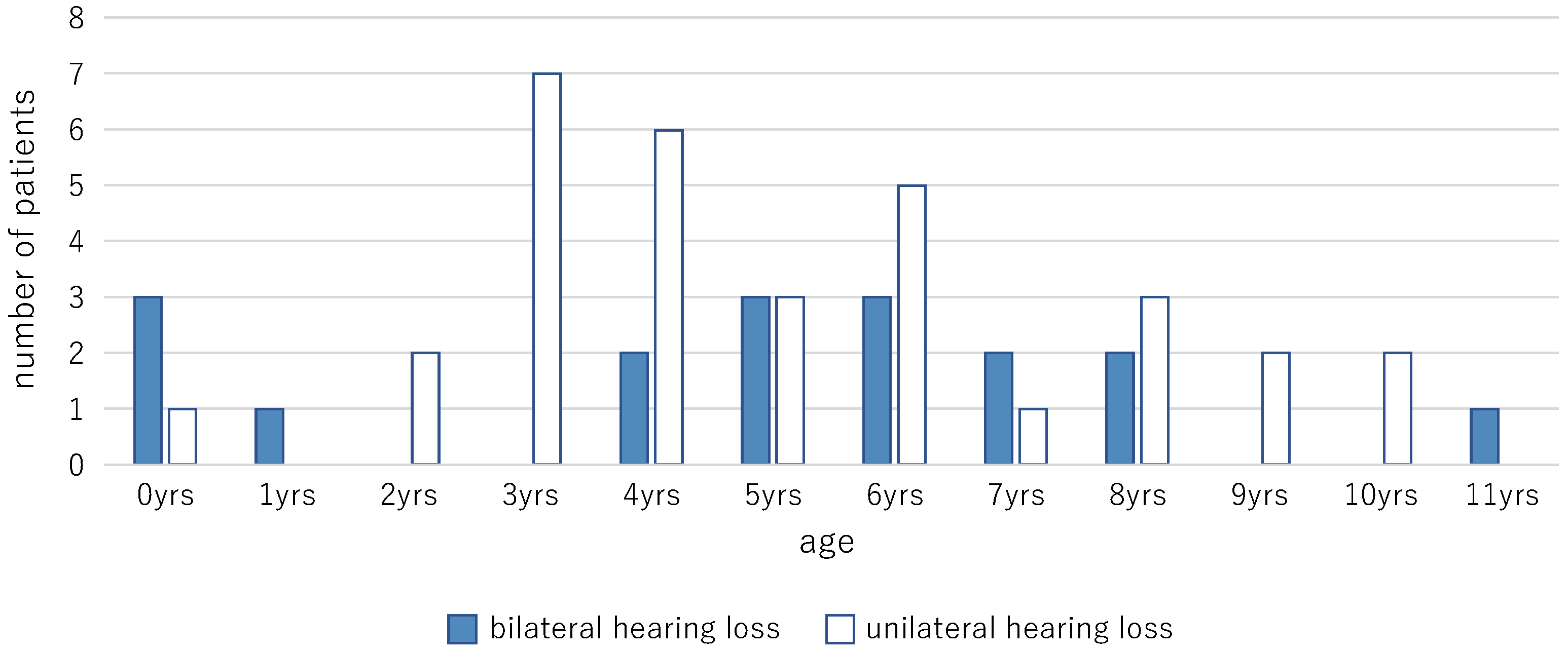
Figure 1 presents the age distribution of the participants at the time of the initiation of trial hearing.
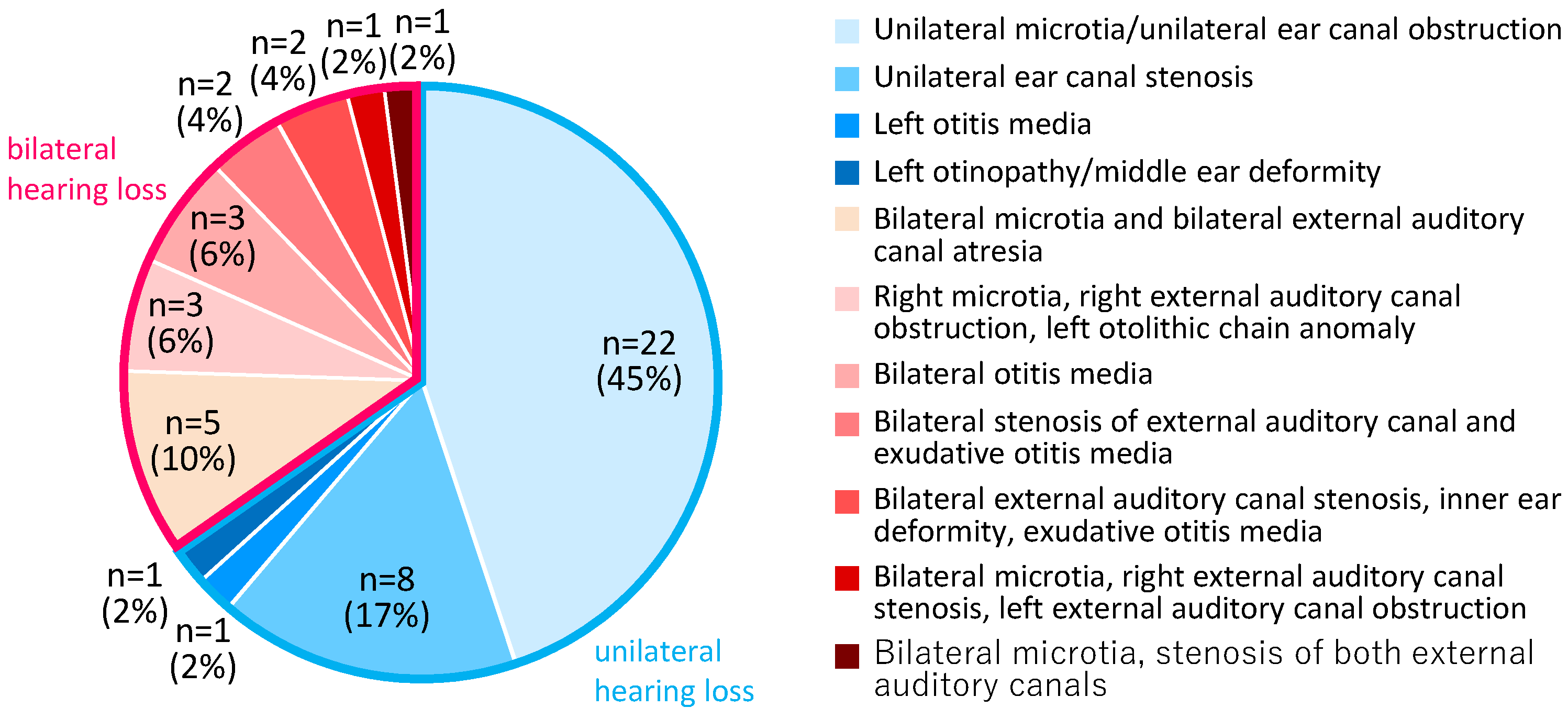
Figure 2 presents the ratios of the diagnoses of the ears fitted with CC-HA (HB-J1CC, HB-A2CC, RION Co., LTD, Tokyo, Japan).
Figure 1.
Age distribution of the participants at the time of the initiation of trial hearing. (n=49).
Figure 1.
Age distribution of the participants at the time of the initiation of trial hearing. (n=49).
Figure 2.
Diagnoses of the fitted ears.
Figure 2.
Diagnoses of the fitted ears.
Among the participants with bilateral hearing loss, eight participants had conductive hearing loss, eight participants had mixed hearing loss, and one participant could not undergo bone conductometry. Among the participants with unilateral hearing loss, 29 participants had conductive hearing loss, one participant had mixed hearing loss, and two participants could not undergo bone conductometry. Among the participants with bilateral hearing loss, two participants had chromosome 21 trisomy, and one participant each had Treacher Collins syndrome, chromosome 18 trisomy, FOXP1 syndrome, and Primrose syndrome.
The presence of a history of hearing aid use was not observed in cases of unilateral hearing loss, and it was only observed in five out of the 17 cases of bilateral hearing loss (BC-HA: two cases at the age of 6 and 7, unilateral-AC-HA : one case at the age of 5).
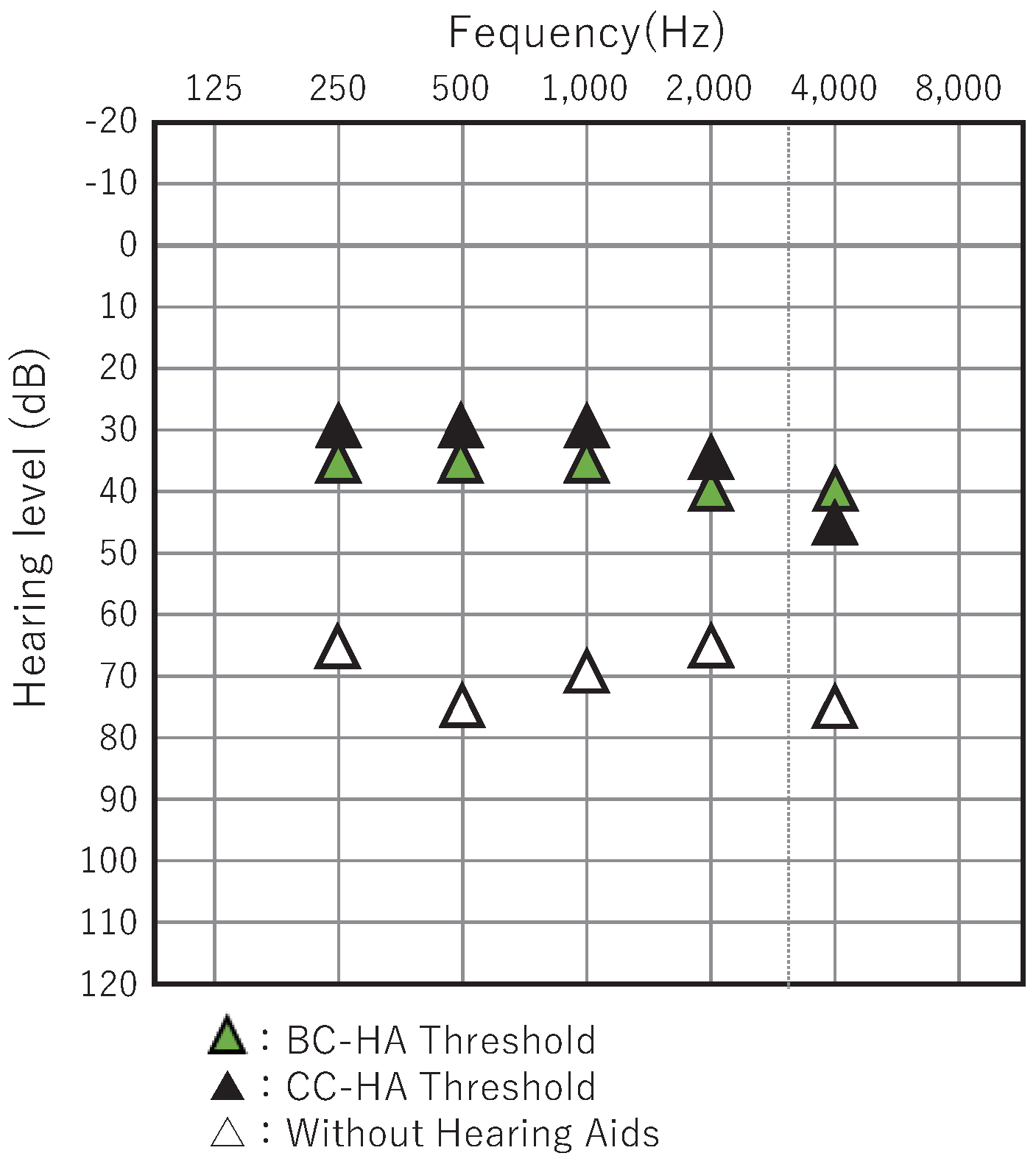
2.2. Hearing Assessment
The auditory thresholds were assessed by an experienced audiologist in a standard soundproof room using a commercially available audiometer (Model AA-HI, RION Co, LTD, Tokyo, Japan). Pure tone thresholds were determined using over-ear headphones (125 Hz to 8 kHz) for the assessment of air conductance thresholds and a calibrated bone-conducting transducer (500 Hz to 4 kHz) for the assessment of bone conductance thresholds. Sound field thresholds (SF) were evaluated to assess the effects of CC-HAs. Complementary and non-complementary hearing thresholds were assessed by introducing an azimuth angle of 0° and transmitting warble tones from a loudspeaker positioned 1 m away from the participant. As CC-HAs were fitted on only one side in participants with unilateral hearing loss, masking noise was provided to the other ear through headphones such that the test tone could not be heard. The complementary hearing threshold for CC-HAs cannot be assessed accurately in participants with unilateral hearing loss; therefore, the assessment of the hearing threshold was used as the reference value. Behavioral hearing tests, such as behavioral observation audiometry (BOA) and visual reinforcement audiometry (VRA), were used to assess the hearing ability if the participant was too young to undergo the hearing tests described above. The behavioral hearing tests were performed in a manner similar to those used in previous reports from Japan[
17].
2.3. Adjustment and Fitting of the Devices and Ethical Standards
The devices were fitted at the Sugiuchi Clinic. The participant or the guardian was provided explanations regarding CC-HAs. Concurrently, ENT examinations, hearing tests, and imaging were conducted to confirm the HA history and indications prior to initiating trial hearing. Trial hearing with the fitted CC-HA was continued for 1–3 three months free of charge, and the participants were instructed to assess the usefulness and comfort of using CC-HA in their daily lives during the trial hearing period.
The initial adjustment of the hearing aids was performed using the Sedation level version 5 (DSL v5) procedure[
18]. This procedure and the determination of the hearing threshold for CC-HAs were similar to those for AC-HAs. After the hearing aid was tested in the outpatient setting, the hearing threshold was assessed, and the gain and output of the hearing aid were predicted. Fine adjustments were made if necessary. Subsequently, trial hearing was continued for a period of 1–2 weeks in real-life settings. The fitting condition and effectiveness of the hearing aid were evaluated during this period, and the hearing aid was readjusted based mainly on the user’s wishes. The listening tests and adjustments were repeated until the participant or the guardian made the decision regarding whether to purchase the hearing aid without any psychological burden on the participant.
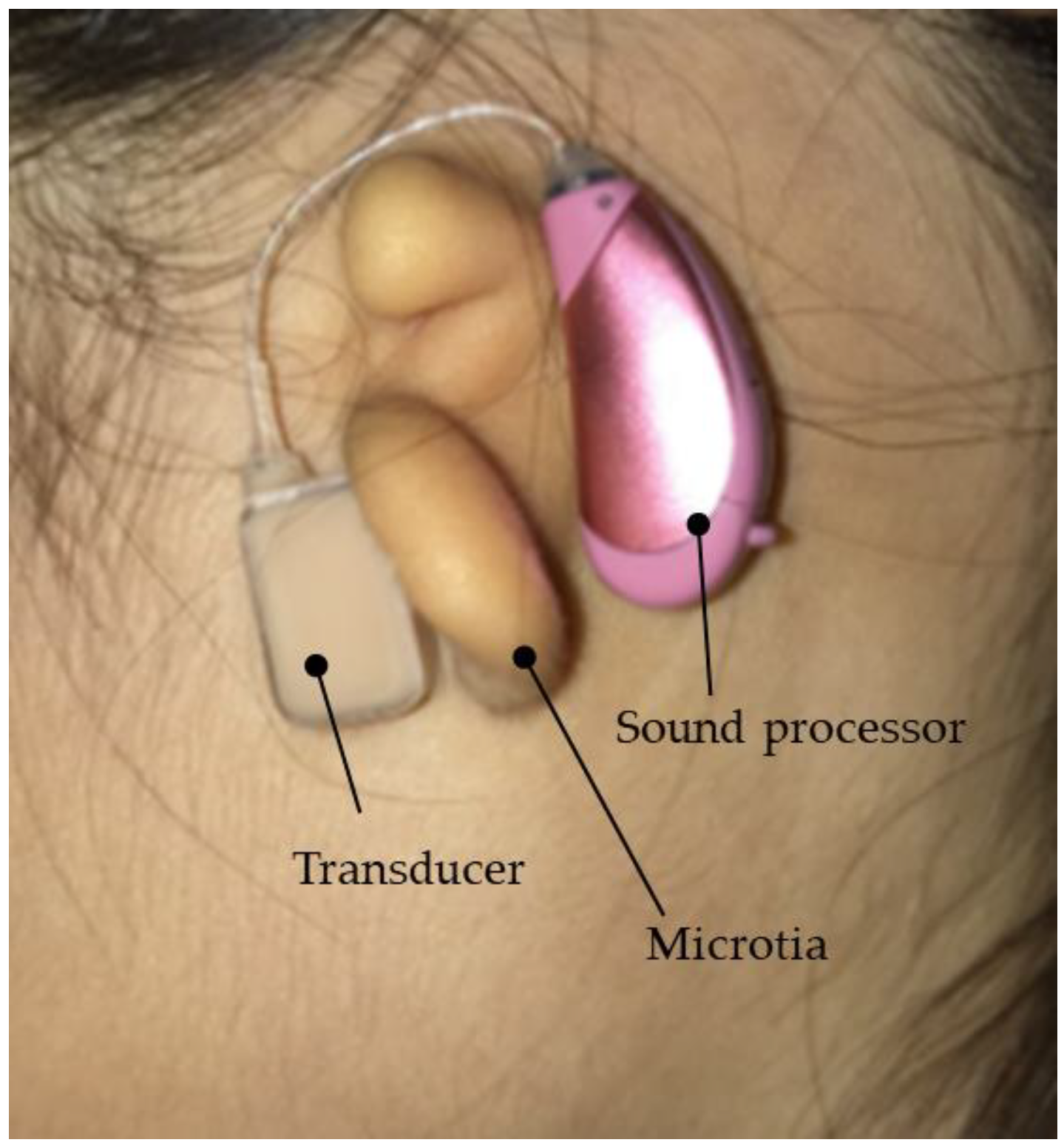
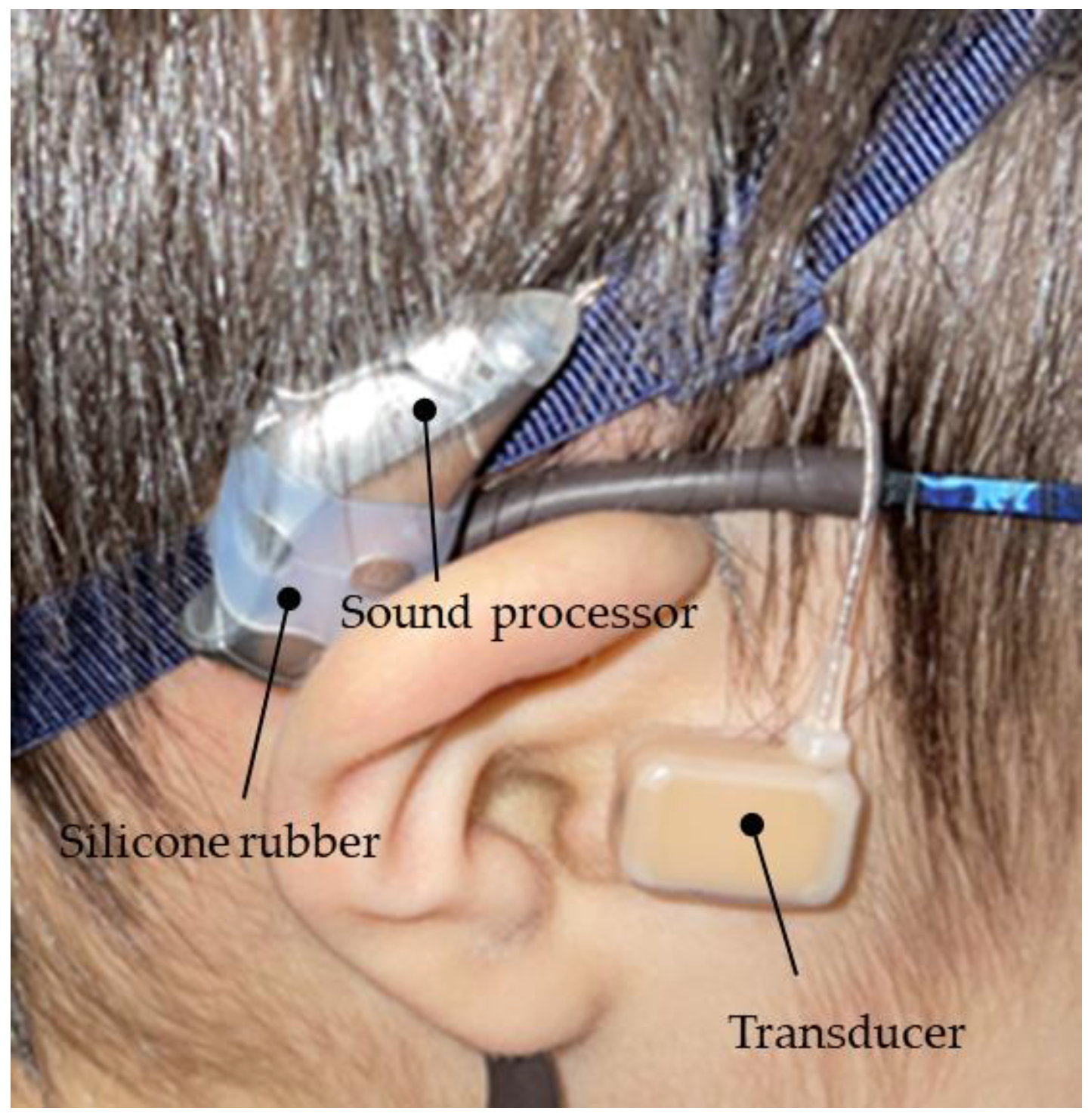
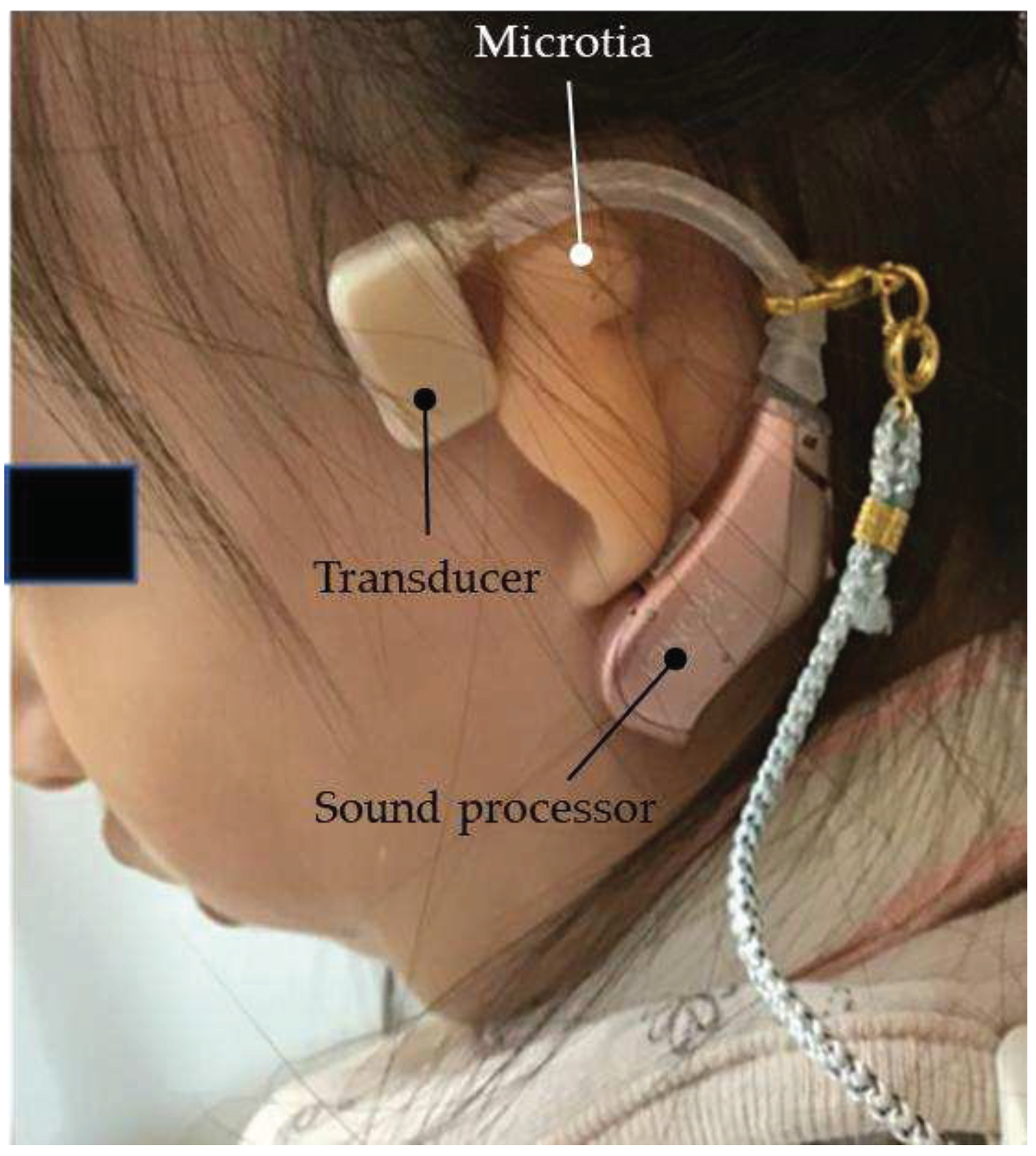
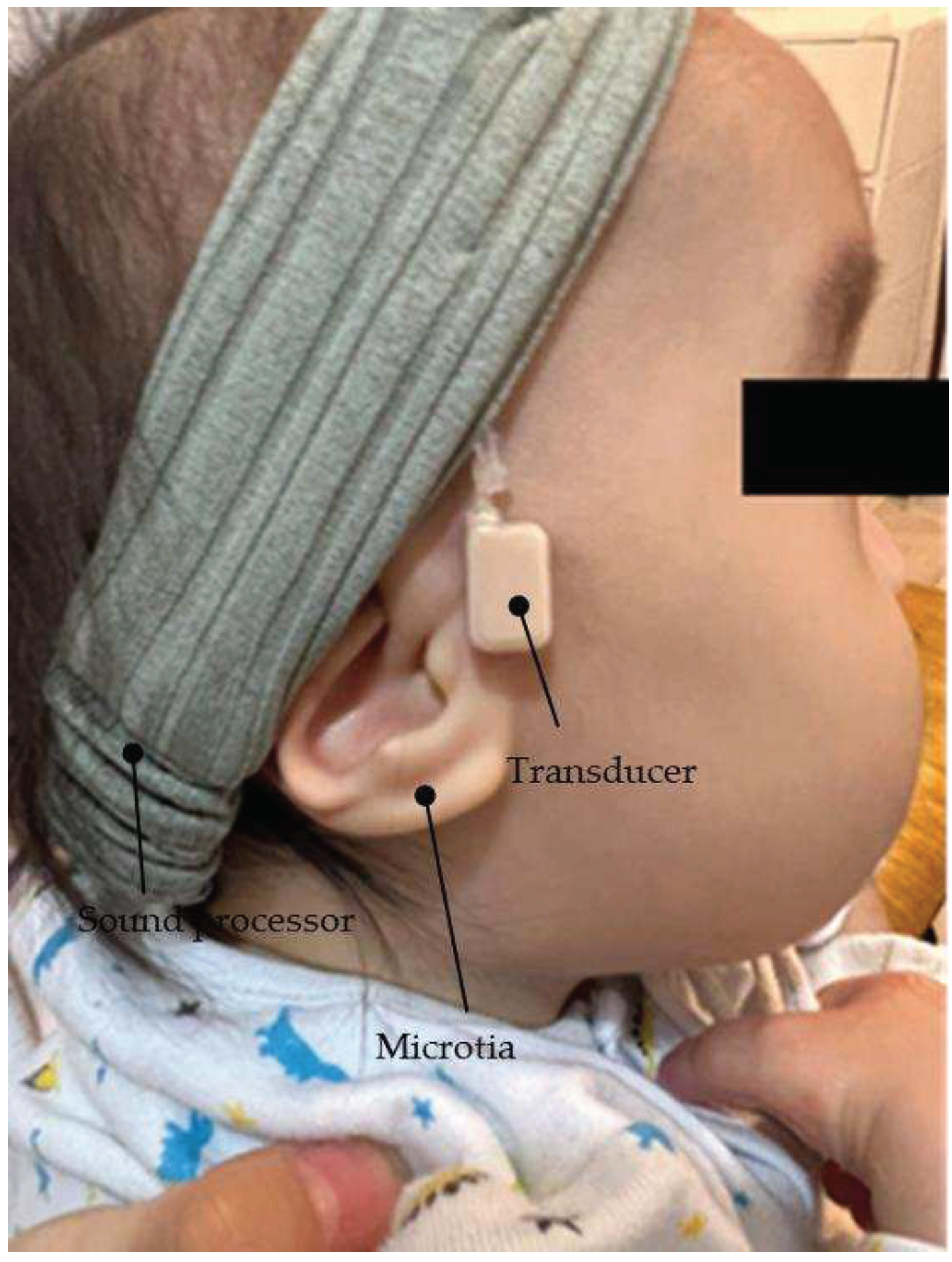
The vibration terminal (transducer) of the CC-HA was attached to the skin overlying the tragus cartilage and fixed with double-sided adhesive tape. As the morphology and location of the tragus and auricular cartilage have not been mapped well in patients with microtia or congenital aural atresia, the transducer was carefully applied to the skin overlying the cartilage near the assumed location of the tragus with a subtle concavity (
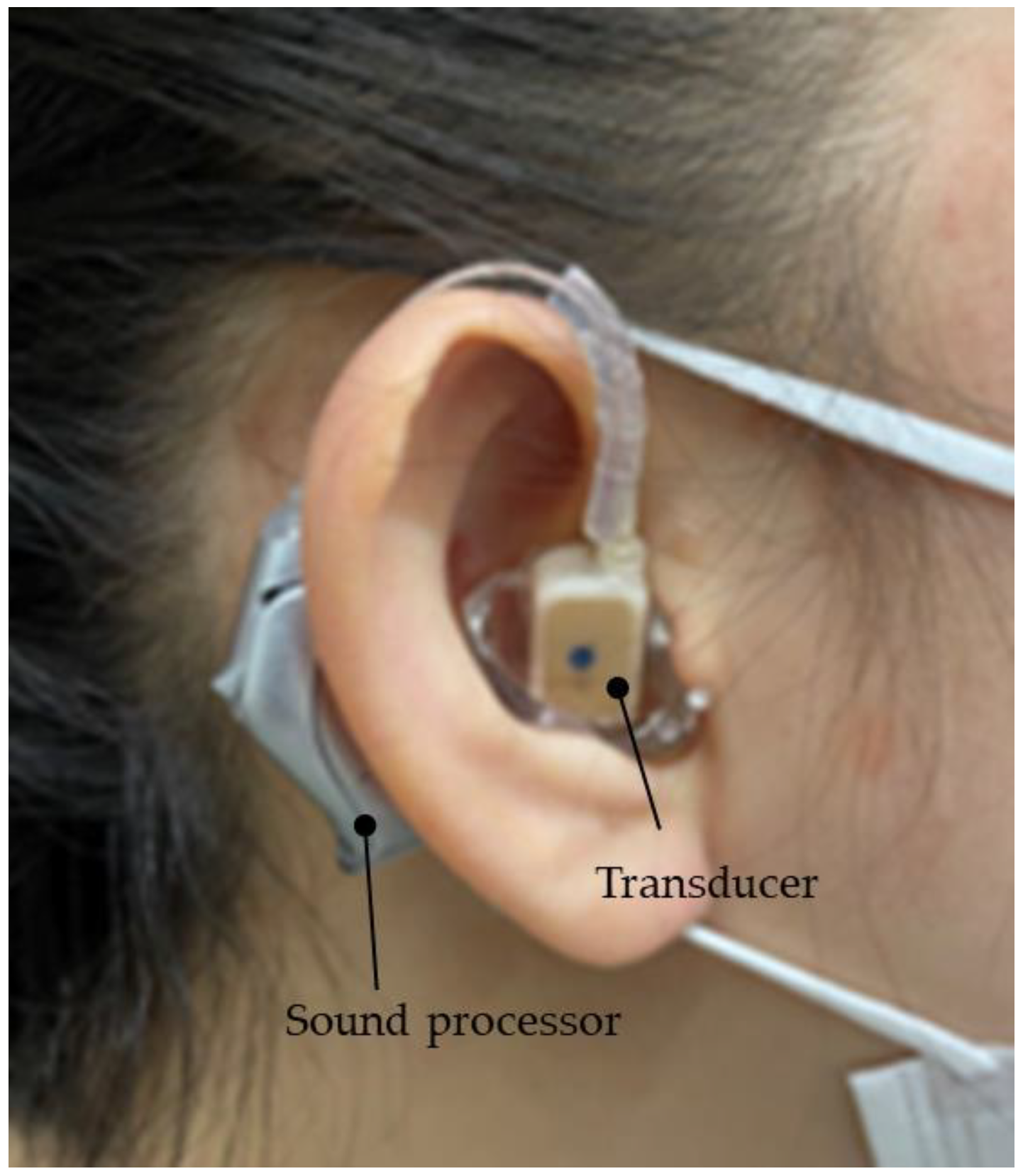
Figure 3). The sound processor of the CC-HA was affixed to the skin overlying the posterior auricle with double-sided adhesive tape. An earmold (hereafter referred to as an ear-tip) was fabricated if attachment with adhesive tape was difficult or if the attachment was unstable, and the transducer was attached to a depressed area such as the cavity of the concha (
Figure 4).
Figure 3.
Profile view (left side) of a patient with congenital external ear canal atresia fitted with a cartilage conduction hearing aid (CC-HA). The transducer and sound processor components of the CC-HA (HB-J1CC, RION Co., LTD; Tokyo, Japan) are attached to the skin using a double-sided adhesive tape.
Figure 3.
Profile view (left side) of a patient with congenital external ear canal atresia fitted with a cartilage conduction hearing aid (CC-HA). The transducer and sound processor components of the CC-HA (HB-J1CC, RION Co., LTD; Tokyo, Japan) are attached to the skin using a double-sided adhesive tape.
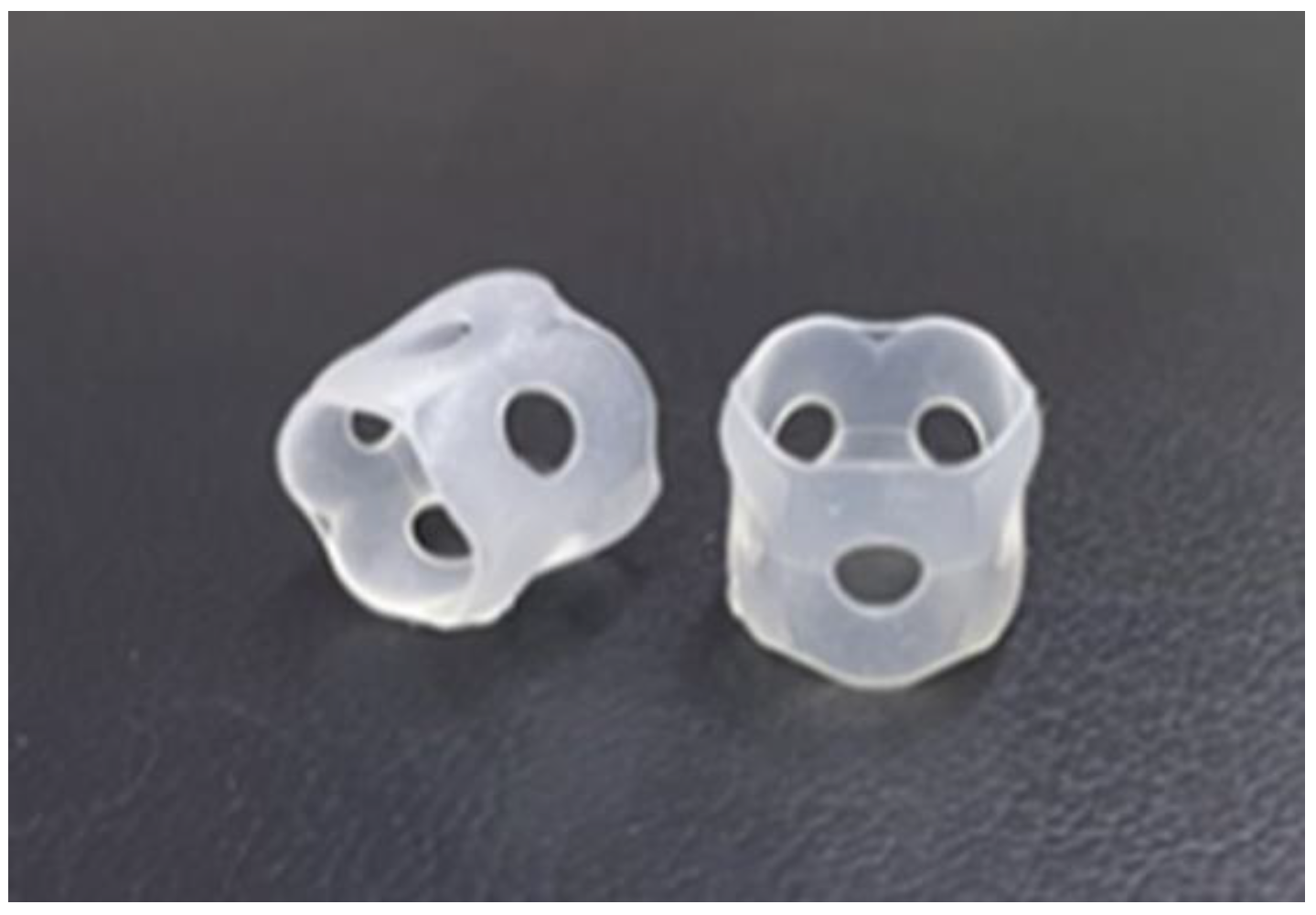
Figure 4.
Profile view (right side) of a patient with congenital external ear canal atresia fitted with a cartilage conduction hearing aid (CC-HA). The transducer (with ear tips) is attached to the skin using a double-sided adhesive tape (sound processor components of the CC-HA: HB-J1CC, RION Co., LTD; Tokyo, Japan).
Figure 4.
Profile view (right side) of a patient with congenital external ear canal atresia fitted with a cartilage conduction hearing aid (CC-HA). The transducer (with ear tips) is attached to the skin using a double-sided adhesive tape (sound processor components of the CC-HA: HB-J1CC, RION Co., LTD; Tokyo, Japan).
In principle, the initial hearing test was initiated in the manner described above. CC-HAs were attached to the posterior part of both auricles in participants with bilateral hearing loss. CC-HAs were fitted to the affected ear in participants with unilateral hearing loss similar to that in those with unilateral congenital auricular atresia. Two CC-HAs were fitted in participants with bilateral hearing loss similar to that in those with bilateral congenital auricular atresia. The test hearing conditions were the same for participants with one and two CC-HAs.
Explanations regarding the indicated hearing aids, such as bone-conduction hearing aids, BAHAs(Cochlear Limited, Sydney, Australia) and ADHEAR system(MED-EL, Innsbruck, Austria) were also provided, and demonstrations via test hearing were provided, if possible, upon request. Furthermore, the rehabilitation staff at the rehabilitation institution were provided information regarding the need for hearing aids and the model and adjustment of the hearing aids. The final decision regarding the purchase of the hearing aid was made by the parents based on the hearing aid use thresholds and the combined observations and evaluations of the parents and caregivers.
This study was conducted in accordance with the "Ethical Principles for Medical Research Involving Human Subjects" [
19]as stated in the Declaration of Helsinki and approved by the Ethics Committee of the Kanto Rosai Hospital (Approval No.: 2023-1). The details of the study were posted in the examination room of the clinic. Verbal informed consent was obtained from all participants and their guardians. The requirement for written consent was waived according to the ethical guidelines for medical and health sciences research involving human participants [
20]. The information regarding the study, including the purpose of collecting information and its use, was made publicly available or notified to the research participants. The study participants and their guardians were informed that they could refuse participation at any time and request that their data be deleted after the study was started. This information was also included in the medical records of each participant.
2.4. Purchase Rate and the Evaluation of Cases That Did and Did Not Purchase CC-HA(s)
The overall purchase rate was evaluated, and the participants were divided into two groups based on whether the CC-HA was purchased: the purchase and non-purchase groups. Information regarding the age, sex, condition of the ear fitted with the hearing aid (affected or good ear), and the mean hearing thresholds (500 Hz, 1000 Hz, and 2000 Hz) of the participants was collected and used for comparison. The participants who were too young to undergo hearing assessments, such as sound field thresholds, were excluded from the study.
2.5. A Simple Way to Improve Hearing Aid Fixation
The following methods were used when the hearing aids could not be stabilized by attaching the transducers and sound processors of CC-HAs.
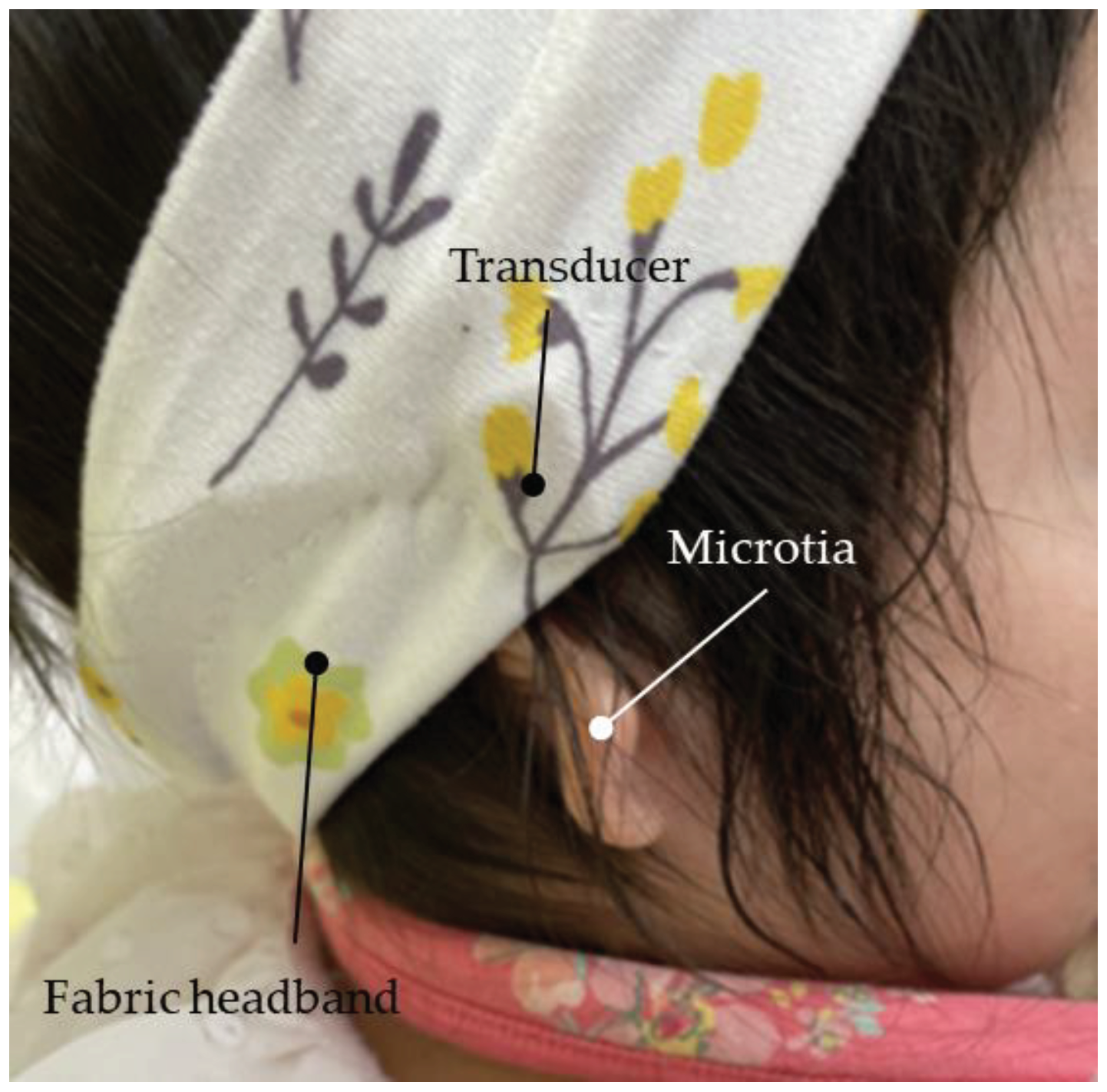
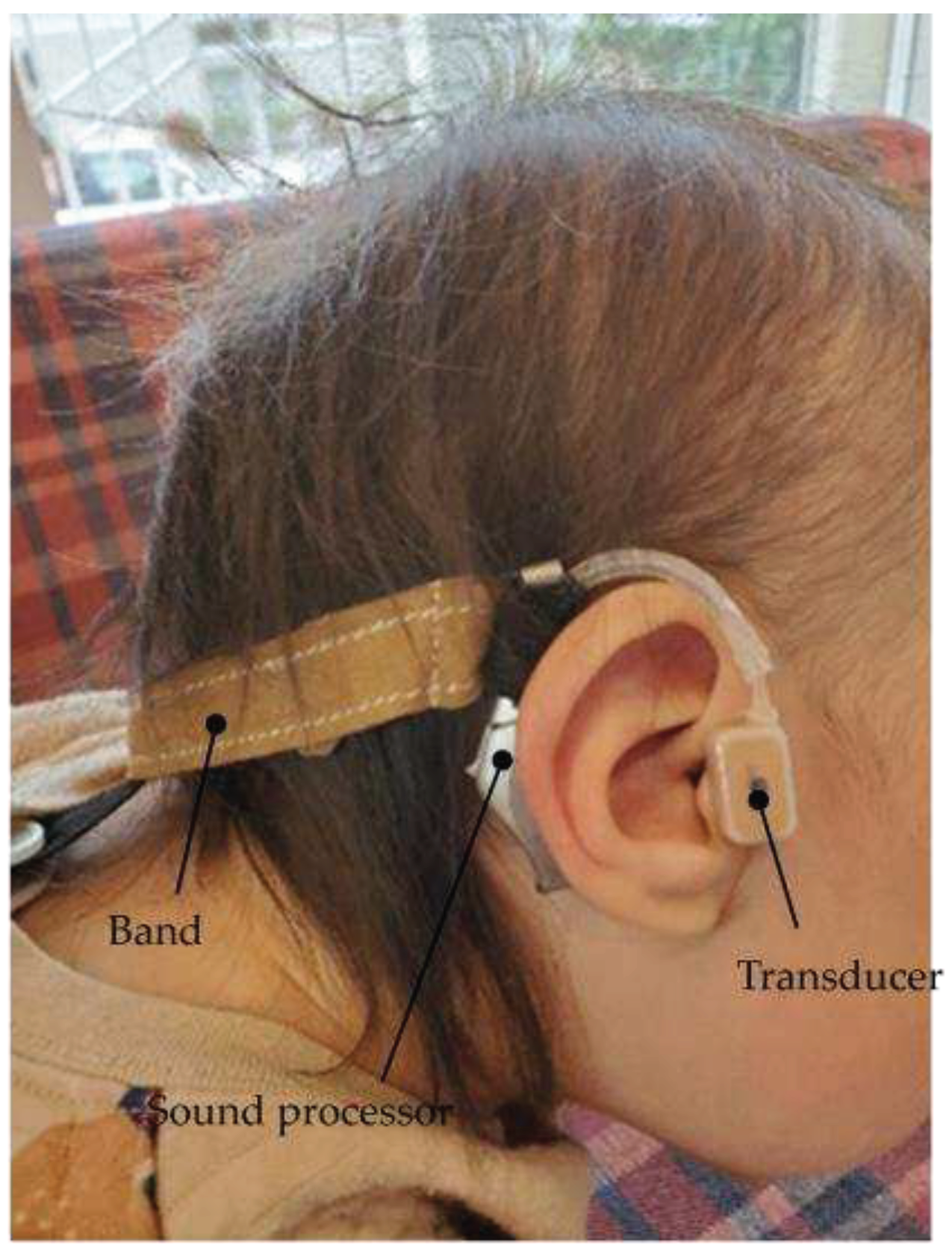
2.5.1. Use of a Hairband
In this method, a silicone rubber was sewn onto a commercially available flat rubber-like hair band to which the hearing aid body was fixed. The transducer was subsequently attached with a double-sided adhesive tape (
Figure 5 and
Figure 6).
Figure 5.
Profile view (right side) of a patient with Downs syndrome who has bilateral external ear canal stenosis with exudative otitis media and congenital external ear canal atresia fitted with a cartilage conduction hearing aid (fixed onto the headband with silicone rubber). The transducer is attached to the skin using a double-sided adhesive tape.
Figure 5.
Profile view (right side) of a patient with Downs syndrome who has bilateral external ear canal stenosis with exudative otitis media and congenital external ear canal atresia fitted with a cartilage conduction hearing aid (fixed onto the headband with silicone rubber). The transducer is attached to the skin using a double-sided adhesive tape.
Figure 6.
Silicone rubber, which is sold as a stationery item, can be used for attaching the main body of the hearing aid to the temple of the glasses or headbands.
Figure 6.
Silicone rubber, which is sold as a stationery item, can be used for attaching the main body of the hearing aid to the temple of the glasses or headbands.
2.5.2. Use of Eyeglasses
In this method, the sound processor of the CC-HA was fixed to the temple of the glasses with rubber or silicone rubber, and the transducer was attached subsequently (
Figure 7).
Figure 7.
Profile view (left side) of a patient with bilateral external auditory canal stenosis with exudative otitis media wearing a cartilage conduction hearing aid fixed to the temples of glasses. The transducer is attached to the skin using a double-sided adhesive tape.
Figure 7.
Profile view (left side) of a patient with bilateral external auditory canal stenosis with exudative otitis media wearing a cartilage conduction hearing aid fixed to the temples of glasses. The transducer is attached to the skin using a double-sided adhesive tape.
2.6. Evaluation after Purchase
The participants or their guardians who purchased CC-HA were interviewed during the consultation to understand the post-purchase status, and the participants were evaluated. The questions included the duration of hearing aid use, the effectiveness of hearing aid use, and their requests regarding hearing aid use. Questions and options regarding the duration of hearing aid use and the effectiveness of hearing aid use were determined in advance.
4. Discussion
This study aimed to evaluate the effectiveness and fitting/wearing status of CC-HA in children with hearing loss and examine the indication for hearing aids in children as they grow older. The primary finding of this study was that it is possible to continuously and stably wear hearing aids from infancy by devising a fitting method while monitoring the developmental status and wearing conditions. The discovery of the cartilage conduction pathway has uncovered new possibilities in auditory function. There are three possible transmission pathways for acoustic energy traveling from a cartilage conduction transducer to the cochlea [
14]. The first is the AC pathway from the transducer to the eardrum, which includes the resonance effect in the canal (air pathway) as the transducer also generates a low-level air-borne signal. The second pathway involves both air and cartilage conduction. Vibrations of the aural cartilage and the tissue surrounding the external auditory canal generate sound in the ear canal that reaches the eardrum via AC (cartilage-air pathway). The third pathway involves bone and cartilage conduction via the skull from the transducer to the cochlea (cartilage-bone pathway). The air and cartilage-bone pathways are common routes that operate based on the same principles that pertain to regular air and bone conduction hearing, respectively. In contrast, the cartilage-air pathway is not a common sound conduction route. CC-HAs are being utilized as a new hearing aid, primarily in Japan. The greatest advantage of using CC-HAs in clinical settings is that its transducer is significantly smaller and lighter compared with that of conventional BC-HA. Moreover, it does not require compression fixation, which enables CC-HAs to be attached to the skin to deliver sound vibrations into the ear.
Nishiyama et al. investigated adult candidates eligible for using CC-HA [
15] and concluded that patients with external auditory canal stenosis or anotia are the most suitable candidates. They also reported positive results in children with similar ear conditions [
16].
We initiated trial hearing of CC-HA in 49 cases ranging from infants to elementary school students, and 36 cases proceeded to decide and utilize the device. During the promotion of the suitability of CC-HA for infants and young children, particularly those with developmental disorders, we encountered difficulties in achieving stable attachment using the recommended methods of adhesion or ear tips alone. Initially, we proposed attaching the transducer using double-sided tape and securing it further with tape [
16]; however, this did not result in a stable attachment. Therefore, taking inspiration from the headbands used for BC-HA, we collaborated with the participants’ mothers and created prototypes of CC-HA headbands, which quickly made it possible to wear the device. Based on this experience, we found that attaching the hearing aid to the temples of glasses or using a favorite headband proved to be successful in other cases.
Treacher Collins syndrome (as seen in Case 1), also known as mandibulofacial dysostosis, is an autosomal dominant inherited genetic disorder with an incidence of 1 in 50,000 [
22,
23]. Common symptoms of this syndrome include hypoplasia of the facial bones, especially the mandible and zygoma, drooping cleft palate, lid coloboma, and cleft palate [
24]. Conductive hearing loss is observed in 50% of patients and is attributed to malformations of the outer and middle ear [
25,
26]. Previous studies have reported auditory rehabilitation in such patients using BC-HAs or BAHAs. The importance of early auditory rehabilitation to ensure appropriate development of language and learning is well-known [
27,
28,
29,
30]; however, the use of BC-HAs is associated with local pain, discomfort, and concerns related to appearance [
7,
12]. BAHAs require surgery [
31,
32], and the protrusion of the implant is a disadvantage in terms of appearance [
12]. In contrast, the use of CC-HAs is not associated with such problems and is considered an effective alternative to AC-HAs. In this study, a headband was used as an adaptation for wearing the device. Initially, concerns were raised regarding headband shifting; however, no issues regarding shifting were encountered over the study period. It is believed that factors, such as the child being calm, having minimal body movements during infancy or other life stages, or being at a stage of having greater understanding, may also have influenced the results.
FOXP1 syndrome (seen in Case 2) is associated with intellectual disability, language impairment, autism spectrum disorder, myotonia and mild dysplasia, and congenital abnormalities of the brain, heart, and urinary system. Cases of hearing loss have been reported with this syndrome. Lozano et al. reported that all individuals with FOXP1 syndrome must be evaluated for hearing loss and promptly provided with hearing replacement [
33]. CC-HA was effective in the treatment of hearing loss in a patient with trisomy of chromosome 18. Trisomy of chromosome 18 is the second most frequent autosomal disorder after Down syndrome and 22q11.2 deletion syndrome, with a reported frequency of 1 in 3,500–8,500 live births. The prognosis is often poor [
34,
35]; however, marked improvement in vital prognosis has been reported. Sato et al. have reported the importance of fitting hearing aids in these patients with documented hearing loss. With advances in newborn hearing screening tests and early detection of hearing loss, it would be desirable for hearing aids to be worn safely, without burden, and consistently from age 0, even in cases where AC-HAs are difficult to apply, such as in patients with atresia of the external auditory canal.
In this study, there were five participants with bilateral hearing loss who had a history of using hearing aids prior to the CC-HA trial. Four participants had used bilateral BC-HA, and one participant had used AC-HA on the side without external auditory canal stenosis. The preference for switching to CC-HA primarily came from caregivers due to limited wearing time and concerns regarding aesthetic aspects and discomfort caused by the pressure of the BC transducer in BC-HA. Among the three participants with bilateral microtia and external auditory canal atresia, all participants except one, who was awaiting a transition to CC-HA after auricular reconstruction surgery, immediately transitioned to CC-HA. In one participant with unilateral microtia, external auditory canal stenosis, and contralateral ear ossicular malformation, external auditory canal enlargement was observed during the process of making an ear impression for CC-HA, resulting in the selection of AC-HA. In cases of bilateral hearing loss with microtia, external auditory canal closure, or stenosis since birth, conventional BC-HAs (with cloth headbands) are commonly chosen by both medical professionals and caregivers, as they appear to be easier to wear and readily available. However, CC-HAs offer the potential for stable use from infancy by adapting the wearing method as the child grows, and it is expected to have wider applications. This adaptation requires repeated prototyping. Moreover, collaboration with the parents, especially the mother, is essential, as it is the mother who observes the child's behavior and experiences the benefits of wearing the hearing aid. The support and involvement of healthcare professionals and caregivers are crucial in increasing the motivation for wearing the hearing aid and encouraging active utilization.
Evaluation of the post-purchase experience revealed that in participants with bilateral hearing loss, hearing aids were used almost throughout the day. Moreover, both the individuals and their surroundings experienced positive effects from the usage. Similar results were observed in participants with unilateral hearing loss; however, there were some instances of shorter wearing times. It was demonstrated that educational and medical support are crucial for the effective use of hearing aids, particularly in cases of unilateral hearing loss. Additionally, a higher proportion of individuals with unilateral hearing loss reported perceiving the benefits of wearing the hearing aid compared with those who had bilateral hearing loss, which may be attributed to the presence of non-usage periods, making the effects of the hearing aid more noticeable. This is also believed to reflect the binaural hearing effects indicated by Kaga et al. [
36]. As for the challenges related to the hearing aids, participants with bilateral and unilateral hearing loss identified improvement in the adhesive wearing method, particularly addressing issues with sweat and difficulties in reapplication, as future tasks.
The participants with unilateral hearing loss had no history of using hearing aids, and CC-HA was the first hearing aid selected for these participants as there were limited options available in terms of other models as they required surgical intervention. In recent years, implants, such as the BAHA Attract system (Cochlear Limited), Bonebridge (MED-EL, Innsbruck, Austria), and Sophono (Medtronic, Dublin, Ireland), have been developed. In the case of children, the decision for surgery is primarily made by the caregivers (parents). However, the use of CC-HA as a policy until the age when the child's own will can be taken into consideration is also an important option.