1. Introduction
Exacerbated by the Covid-19 pandemic, many previously ‘elsewhere-located’ activities now take place within the home, including work, education, and healthcare. Home healthcare technologies have become increasingly popular, for example monitoring of blood pressure and heart rate, diabetes, oral health, and general fitness. In addition, many general practitioners (GPs) and other healthcare professionals now offer routine appointments via video conference. This approach to healthcare delivery offers new opportunities for research into the experience and design of healthcare experiences at home.
Many of these examples rely on digital systems capable of facilitating and making autonomous decisions regarding healthcare delivery, applied to both healthy populations and people with a variety of health conditions. This paper describes the results of a study exploring how autonomous systems (AS) embedded in devices in the home can support decision-making about health and wellbeing, and what makes these devices acceptable to users. By engaging with people who have had a stroke or those who have multiple sclerosis (MS), the study examined attitudes towards the use of AS in decision-making related to their general health and wellbeing, and especially how this relates to shared values such as trust, self-efficacy, and privacy. These two populations were chosen because they experience distinct but similar health management challenges in their everyday lives and need to manage their multiple symptoms daily. People in both groups often experience to a greater or lesser extent: memory problems, gait and mobility challenges, mental health issues, fatigue, communication problems, muscle and neuropathic pain.
To explore how AS could and should be designed to support healthcare at home, and to make engagement with this topic more tangible, online focus groups (details described later) were conducted using the idea of a ‘smart mirror’ as a concept and technology probe. This mirror was envisioned as a piece of technology installed in various spaces in a user’s home, including the bathroom, bedroom, or entrance hall, that would be able to visually assess a person with a medical condition and support them in their management of symptoms, monitor their physical and psychological state, suggest modifications to their treatment plan, interface with carers (medical professionals, family, close friends), and help with daily activities, such as providing reminders for meetings, activities, and medication among others. The focus groups revealed a range of considerations which are important for the deployment of any AS in the home, broadly considered within the contexts of digital healthcare and using technology for self-management, and the home as a space for wellbeing.
1.1. Digital healthcare
Both inside and outside the home, people make wide use of technology such as smartphones and wearable technology for self-tracking of their health and enhancing their self-knowledge, termed the ‘quantified self’ [
1,
2,
3]. Numerous aspects of health can be tracked using smart technology, including number of steps, heart rate, hours of sleep, and even stress levels; many people use these functions to maintain their general health or to assist in reaching fitness or health-related goals. This quantified self has been encouraged by the technology sector, as all smartphones are now equipped with GPS (global positioning system) technology and health-related apps, facilitating self-tracking [
4]. While this has multiple benefits in the promotion of health, novel smart technology still presents challenges in the areas of security, privacy, and trust [
5]. Thus, research exploring these facets of novel technology that aims to improve digital healthcare is crucial.
AS hold brilliant promise for improving healthcare, including patient outcomes, reducing costs, and enabling new health discoveries [
6]. While these technologies have the potential to analyse tasks beyond human capability [
7], they also have the potential to reduce the high demand of social care needs among the ageing population and those who face health challenges [
8]. There are various health conditions that can be assessed and tracked by wearable technology and apps, including type 2 diabetes, hypertension, fertility, concussion detection, traumatic brain injury, skin cancer, and mental health issues [
9,
10,
11,
12,
13,
14].
This paper describes a study exploring two populations: people who have MS and those who have had a stroke. Digital healthcare technology (primarily sensor-based equipment or wearable technology) has been created to monitor specific MS symptoms, such as poor mobility and balance, both of which contribute to increased chances of falls and decreased quality of life for these individuals [
15], conveying promising results [
16]. Other research has shown that individuals with MS may benefit from such technologies due to the feeling of regaining control over an unpredictable condition through self-tracking and improved self-knowledge [
17]. Likewise, technologies have advanced in post-stroke care, including technologies that detect gait and analyse movement, assess and guide exercises to help with balance complications, and track upper limb rehabilitation [
18,
19,
20].
In addition to enabling tracking of these conditions, smart technology can alert users and/or healthcare providers to health deterioration, which shows potential for neurodegenerative health conditions like MS, or health conditions that require long-term rehabilitation, such as a stroke. People who experience these health conditions also often develop mental health issues such as depression and anxiety that can impair their quality of life [
21,
22]. This suggests that having access to a smart device that enables monitoring of stress levels or promotes wellbeing activities such as mindfulness, may be beneficial to these potential users. The effectiveness of mindfulness for psychological symptoms and pain management has previously been shown for people with MS [
21], conveying that mindfulness components could be a desirable feature of a smart device holistically aimed to improve health and wellbeing.
1.2. Using technology for self-management
In addition to management of specific health conditions, people often use technology for self-management. AS designed for a plethora of different tasks serve to enable users to carry out everyday tasks effectively and efficiently. This might include calendar and reminder apps, smart home technologies, financial, banking and shopping apps, and so on. Such technologies can give more control to its users and consequently lead to a reduction of stress. AS for home sensing and environment control, highlighted in
Section 1.3., give people control to more easily action and automate their home environment consequently creating a better space for their health and wellbeing; showcasing how home sensing technologies can also be incorporated into digital lifestyle management.
More directly related to the health context, a form of self-management is ‘lifestyle management’, in the sense of implementing and/or maintaining lifestyle habits such as regular exercise, healthy diet, reduction of stress, and so on to address help control symptoms and prevent certain health conditions [
23]. It is a commonly used practice to help control and address symptoms of obesity [
24], diabetes [
25], hypertension [
26], depression [
27], PCOS [
28,
29], endometriosis [
30], among other conditions. To maintain the lifestyle long-term, lifestyle management can be used by itself or with other treatments such as pharmacological and behavioral treatments e.g., intensive behavioral therapy (IBT) [
23].
As behavioral approaches have limited access, can be expensive and require the person to engage face-to-face, the use of AS for lifestyle management offers an alternative solution to the challenges in sustainable and long-term implementation of lifestyle habits. These AS tend to be based on goal setting and evaluation (via the quantified self), as well as nudging for encouragement and motivation (a challenge in long-term adoption of habits) [
31]. Traditionally there are two main approaches to digital interventions for lifestyle management: app-based and web-based. Both approaches are adaptive, feedback-based and multi-media however app-based approaches have the further possibility of integrating wearable technology, GPS data, and chat boxes [
31]. Other approaches include interactive TVs [
32,
33], Voice Assistant (VA) [
34], and Smart mirror technologies [
35,
36].
This paper focuses on the latter of these technologies, a smart mirror used to examine health monitoring and management. This differs from the wearable-type technology focused on so far in that it is embedded in the home. Research into digital and augmented mirrors has explored a variety of applications, including motivating and guiding daily tasks, for example the AwareMirror [
37] which provides a personalised display during tooth brushing and the FitMirror that aims to improve mood and fitness during morning routines [
38]; posture improvement [
35]; stress detection [
36]; and on-going medical monitoring [
39]. Smart mirror technologies fall into two camps,
digital mirrors which simulate mirrors on camera-enabled digital devices such as tablets, phones and wall mounted displays, and
augmented mirrors that enhance conventional mirrors with digital capabilities, for example by placing digital displays behind half-silvered mirrors as explored here. With a reflective, mirror quality that enables self-monitoring of physical abilities, an interactive interface, and additional health monitoring, along with integration of additional data from other personal devices such as smartphones and other wearables for optimum decision-making, a smart mirror has the potential to effectively monitor health conditions in a novel way. Additionally, user wellbeing would have to be central in the mirror’s design, to promote psychologically respectful technological developments [
40].
1.3. The home as a space for wellbeing
The built environment strongly shapes social and individual behaviours and lifestyles, becoming a significant factor contributing to individuals’ health [
41]. Recognising this important role, architecture and related building design disciplines are moving towards designing spaces for wellbeing. For instance, having access to green areas and the integration of nature aspects within and surrounding buildings has been shown to improve and support physical and mental health [
42,
43,
44]. The convergence of computing and architecture have created exciting opportunities for the creation of spaces where environment conditions such as air quality, temperature, and lighting, can be sensed and adjusted to ensure comfort and ideal conditions for occupants [
45,
46]. Moreover, fast-paced advancements in sensing technologies embedded in the built environment, coupled with those carried (e.g. mobile phones) or worn (e.g. smartwatches) by individuals, have the potential to assist with the provision of healthcare. Digital healthcare developments (as discussed in the previous sections) aim to support both the general population, and more specifically, groups with dedicated needs such as older adults, people with disabilities and people with chronic health conditions. There is a longstanding interest in embedding sensing technologies for monitoring people in care homes [
47,
48], especially when dealing with delicate and deteriorating conditions such as dementia [
49,
50].
There is also a shift towards designing and adapting current and future general housing to support healthcare and wellbeing. The reasons are manyfold: ongoing strains in public health services [
51,
52]; increasing populations in need of long-term support [
53,
54]; the emergence of telemedicine and remote healthcare provision [
55]; and the increasing role of the home in modern lifestyles. The Covid-19 pandemic has increased the urgency for these adaptations; healthcare systems are still struggling to recover from the overflow of patients and lack of resources, and individuals continue to struggle with the aftermath of the pandemic and its effects on physical and mental health [
56]. We still do not fully comprehend the consequences of the virus on the human body [
57] and society at large. The numerous lockdowns and self-isolation periods also had damaging effects, both physically (e.g. decreased opportunities for moving and going out) and mentally (e.g. stress, anxiety, depression) [
58,
59]. Some argue that this pandemic has been a mass disabling event [
60].
With increasing numbers of people studying and working remotely, not least due to the pandemic, the home has emerged as an area that necessitates attention to promote overall wellbeing. Building design has moved towards designing salutogenic living spaces, foregrounding wellness, comfort, fitness, and mindfulness [
61]. Where buildings have had ‘passive’ strategies to increase or maintain wellbeing (e.g. open and flexible areas), digital technologies like smart mirrors and other smart appliances or devices in the home allow more active, potentially even proactive [
62], contribution of architectural space to health and wellbeing. Smart technologies embedded in the home can provide the opportunity to move beyond simple data collection for personal use towards providing active, real-time feedback and recommendations, or even interventions for occupants based on both general and individualized parameters. Nonetheless, the relationship between the home and the data collected needs to be carefully addressed, as in the context of other built environments that collect data from occupants [
63,
64].
2. Materials and Methods
At the core of this project is the consideration of the responsible ways in which technology should and could be developed to support healthcare at home, focused on maintaining the autonomy and dignity of people receiving healthcare, and as such principles of Responsible Research and Innovation (RRI) [
65] were embedded from the start. This was especially important given the multidisciplinary nature of the research team, who were approaching the project with different priorities and experiences [
66] One early exercise to establish common ground was to use Moral-IT cards, which are designed to encourage reflection and engagement in ethics-by-design [
67], to highlight potential ethical questions surrounding the development of technology. The team returned to questions posed by the cards often during the project, as prompts for discussion as well as points to consider when interrogating the results.
A principal component of RRI is the involvement of users from the beginning of the process. The team engaged with Patient and Public Involvement (PPI) groups throughout each stage of the project to ensure that the focus groups reported in this paper were appropriately designed and asked pertinent questions. Existing groups from each user population were approached in an advisory capacity, and two meetings were conducted with each to discuss the project and to gain feedback on the methods and research questions. This helped the team to understand challenges these users had when engaging with digital technologies in general and during their care, that were, then, incorporated into the study; for example, the MS group suggested that monitoring walking, talking, and gait or posture would be worth investigating with users, as they saw both positives and negatives. Both groups also pointed out practicalities for carrying out research, such as issues with having online meetings, and the importance of safeguarding and debriefing if using potentially upsetting scenarios. This enabled the research team to design the focus groups in a responsible and appropriate manner.
2.1. Participants
Participants were recruited through existing networks as well as email and social media recruitment. Participants provided consent by filling out an online form and were thanked for taking part with a £20 Amazon voucher.
2.1.1. Group A: Management of MS
Six participants with MS took part in a single focus group, ranging in age from 38 to 63 (average age 53). They were 3 males and 3 females, and all participants were white; 4 participants had at least an undergraduate degree. Participants had been diagnosed with MS between 3 and 14 years ago (average 9 years); 3 had relapsing-remitting MS, one primary progressive MS, one secondary progressive, and one declined to say. Two participants had additional conditions: trigeminal neuralgia and depression.
2.1.2. Group B: Management of post stroke care
The stroke group took part as 2 one-hour focus group sessions, due to health considerations, and some participants took part in just one of the sessions. In total, 11 participants attended the first session, although 1 withdrew consent later, and 13 participants attended the second session; 8 attended both sessions. They were 12 males and 3 females and all were white. Eight participants provided additional information: age ranged from 52 to 75 (average age 58). Two participants had at least an undergraduate degree. All had experienced one stroke and time since stroke ranged from 1 to 16 years (average time around 6 years). Four participants stated that their etiology was an infarct, 1 haemorrhage, and 2 unknown. For 5 participants the lesion was on the left, 2 on the right, and one on both. Effects included a change in dominant hand; memory loss; problems with vision; communication problems; weakness, inattention, or paralysis on one side of the body; fatigue; limp or drop foot; muscle and neuropathic pain; and spasms.
2.2. Materials and Procedure
Sessions took place online through Microsoft Teams. All were attended by a facilitator and at least one other member of the research team to monitor the group and take notes. Both groups were presented with the same materials and covered the same content, the only difference was the stroke group taking part over two sessions. At the start of the sessions, participants were assured that they did not have to discuss their medical history, or that of others, and that they were under no obligation to disclose any information they did not want to, that they did not have to provide any sensitive information, and any identifying information would be removed. Participants were also free to leave and re-join the workshop at any time or talk to one of the research team about any concerns; to ensure further safeguarding if they were to type an ‘X’ into the meeting chat then one of the workshop team would pick it up and the group would move immediately on from the discussion.
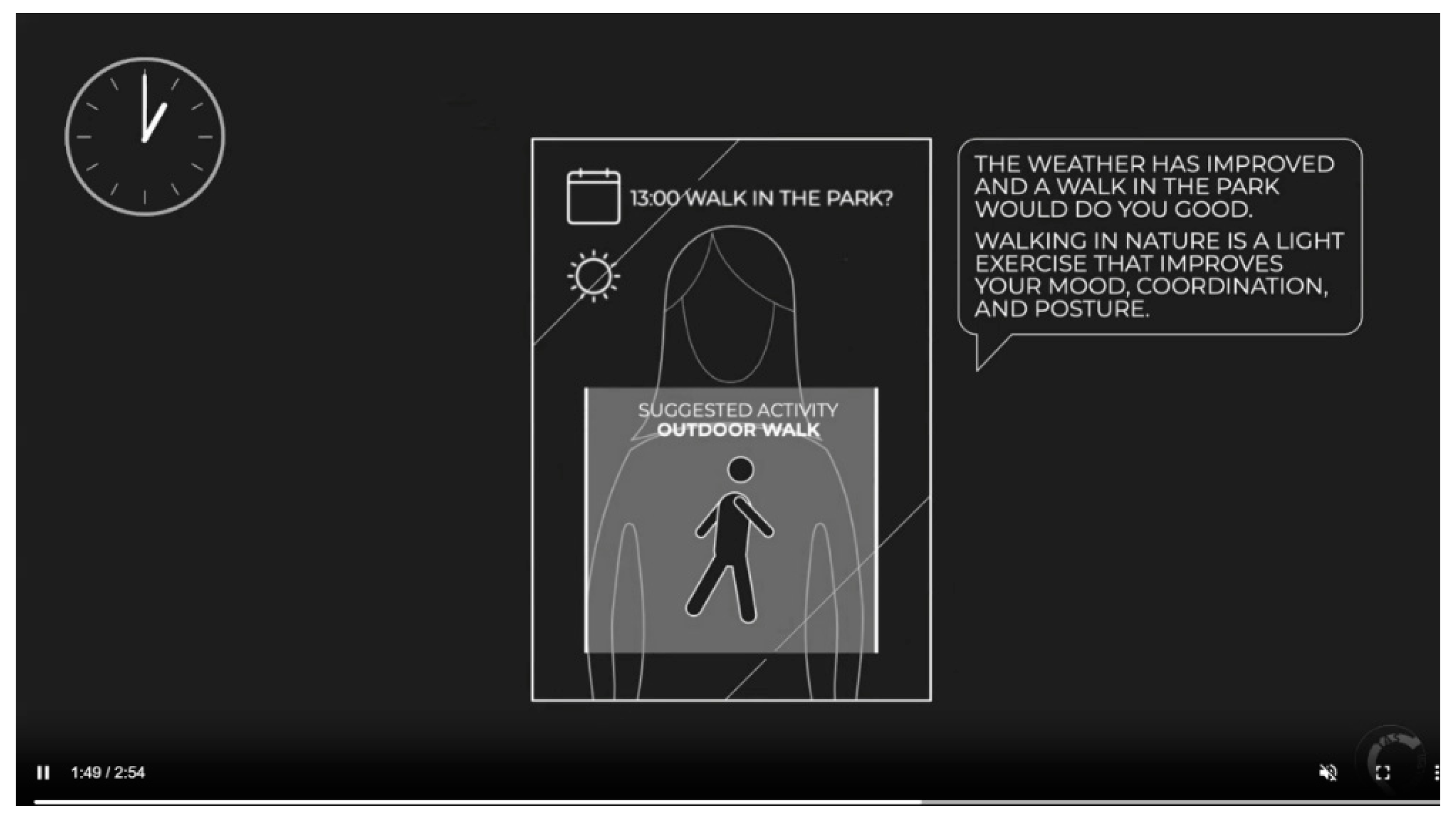
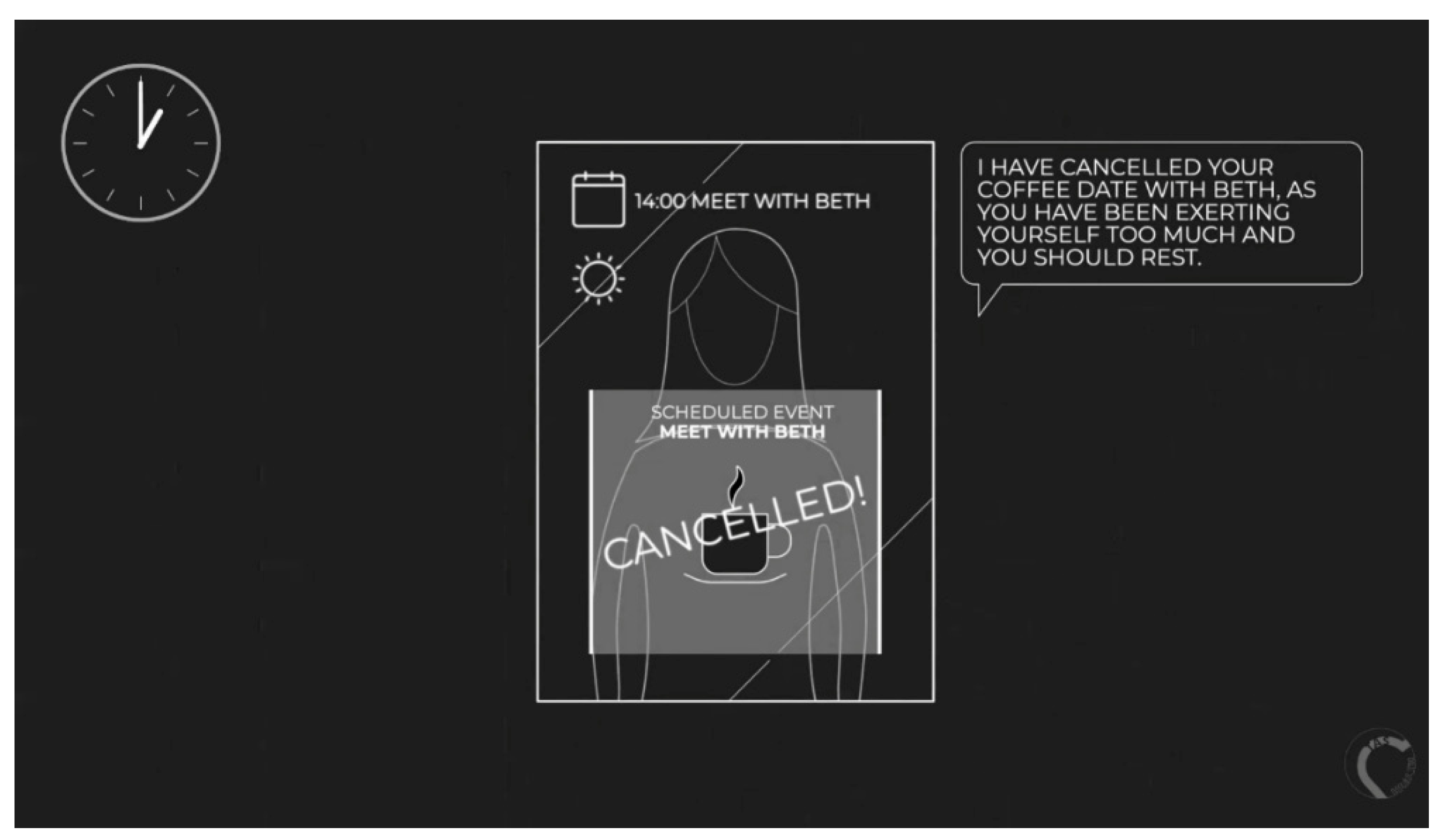
The first part of the session started with an introduction to AS and how they may be used for health, and an overview of the project. This was followed by an open discussion about participants’ current use of technology to support health and wellbeing. The second part of the session focused specifically on smart mirrors, with an introduction to smart mirrors including a video illustrating an existing example. After a brief discussion about the potential use of this technology, participants were shown a ‘positive scenario’ video describing a day-in-the-life of using the mirror for either stroke rehabilitation or monitoring of MS, where everything that happened was framed in a positive way. The transcript for this video is provided in
Appendix A and illustrated in
Figure 1. Participants were asked to discuss their feelings about the mirror based on this video. They were then presented with a ‘negative scenario’ video describing the same activities but with a negative framing (
Appendix A,
Figure 2). Participants were again asked to discuss their feelings about the mirror. The session ended with a general discussion of AS for healthcare and a summary of the benefits and drawbacks of the smart mirror.
2.3. Analysis
Focus groups were recorded in Microsoft Teams, the audio was extracted and transcribed using an automated transcription service. Transcripts were then checked, corrected, and thematically analysed by three researchers. The analysis was completed on Microsoft Excel and followed the process defined by Braun and Clarke [
68] consisting of 1) familiarisation with the data, 2) initial codes generation, 3) themes search, 4) themes review, 5) naming and definition of themes, and 6) report write-up. Separate initial analyses for each user group were carried out to avoid conflation of health conditions and missing relevant information particular to each group. Each separate analysis was then merged to generate one single set of themes covering both workshops. That is, steps 1-3 were conducted separately for each group, and once initial themes were developed, initial groupings were reviewed and combined to produce the final themes presented in this document. Throughout the paper, participants are referred to with a number (P1, 2, 3…) and S if they were in the stroke workshop (P1S) or M if they were in the MS workshop (P1M).
3. Results
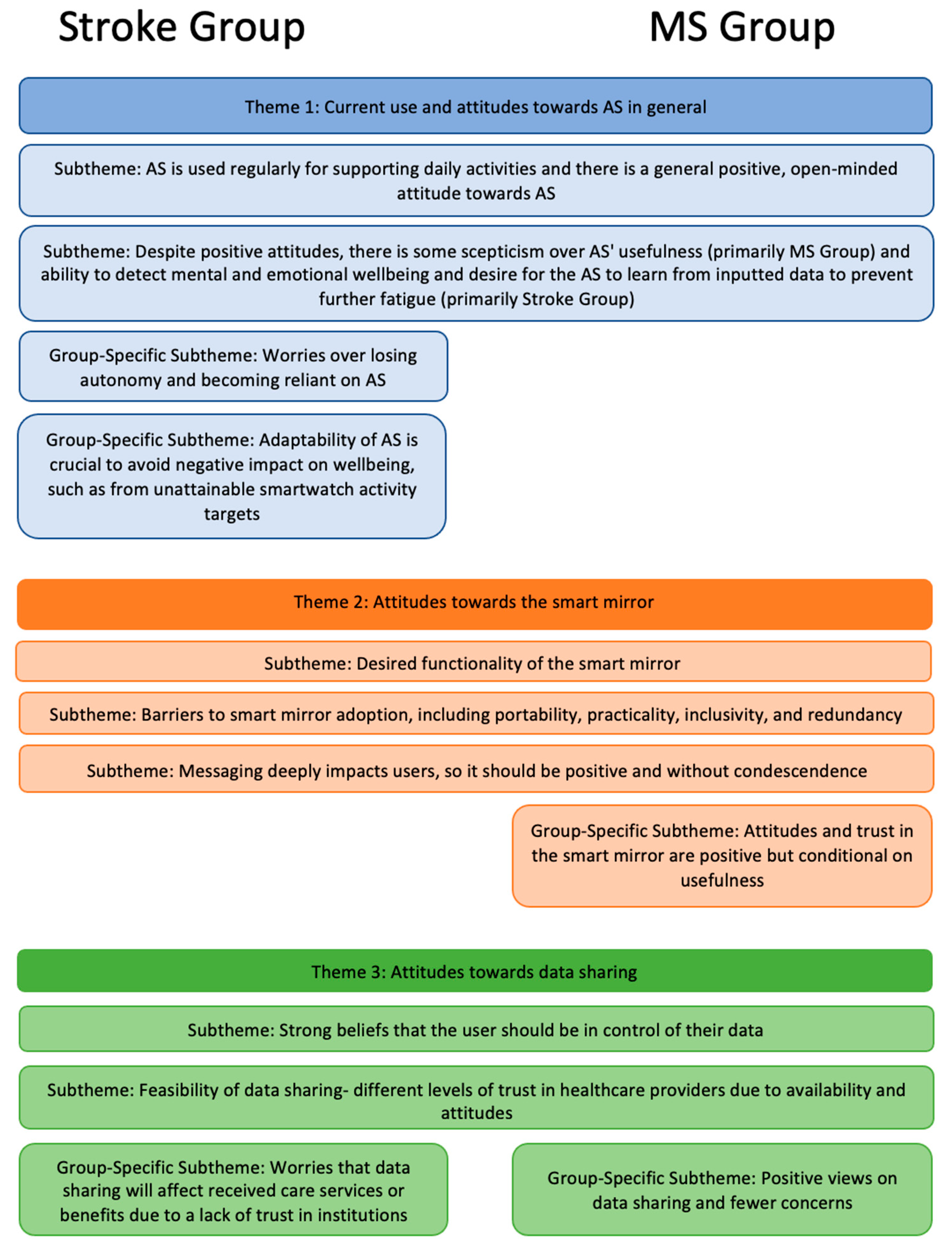
Three major themes and 11 sub-themes were developed, as summarised in
Figure 3 and described below. Note that some subthemes were only identified within a specific user group, as indicated in the figure and their descriptions.
3.1. Theme 1. Current use and attitudes towards AS in general
The first theme refers to the use of AS in participants’ day-to-day life and their overall feelings towards them. Participants reported adoption and regular use of a range of AS for a variety of purposes, for example supporting their cognitive tasks, tracking physical activities, and/or for controlling and monitoring their home, and expressed interest and curiosity towards future AS that could help support their health conditions (subtheme 1a). Several participants expressed the value of devices such as smartphones and smart speakers for setting alarms and reminders for daily tasks such as getting medication, and some also reported using calendars and notes for planning activities; these all helped with memory problems experienced by many in both groups.
“And then the other aspect of my MS is the fatigue, so I do have a smart watch which I wear to track how much I'm walking and how active I am, but also to track my sleep... so sometimes when you go through a week you know you there will be days where you feel really wiped out and it's good just to be able to check, you know, have you been walking too much? Have you not had enough sleep? But also to, you know, if you're going out of pattern, [it’s] probably worth having a conversation with your GP or a specialist.”
[P3M]
Apps for brain training and meditation were also mentioned by a couple of participants to support their cognitive and mental wellbeing. Although a low uptake of these apps among the rest of the participants was observed, there was a general agreement that they sound useful and effective. Some participants used smartwatches or fitness wristbands to monitor their daily activities, such as walking and sleep. Participants also expressed the usefulness of observing their own patterns, as although the AS does not give personalised feedback (e.g. detecting or preventing unusual levels of activity), participants recognise their own thresholds in the data collected by the AS and better understand, for example, their fatigue. They also reported the adoption of smart home technology for monitoring and controlling their environments, such as lightbulbs, plugs, thermostats, and doorbell cameras. These technologies are used in multi-person households, so although they are not necessarily meant for monitoring participants’ health, some participants expressed that they give autonomy and support, especially to those with limited mobility.
“It doesn't monitor my health at all, it's just to make my life easier. In controlling the aspects of my home, I'm completely chair-bound, wheelchair-bound. I can't walk at all. And I’ve really only got the use of one arm, so anything I can use which helps me control things is really useful. I'm on my own occasionally. My wife's my carer. She's around most of the time, but she has to go out every now and again. Um, so for when she's out, it's the only way I've got of controlling my home.”
[P1M]
Where participants recognised shortcomings of the systems that they regularly use or gaps not addressed by technologies yet, they exhibited an overall general positive attitude towards future AS, suggesting ideas related to automating detection of personal patterns to notify users about sleep or walk trends going over certain thresholds and help to prevent fatigue, and further support their care and carers.
However, some people were skeptical of the capabilities of current and future AS for detecting and supporting non-physical states, expressing a desire for AS that can learn from data entered manually about emotional and mental states (subtheme 1b). Some participants entirely dismissed certain AS as inappropriate to support their health. For example, smartwatches and fitness wristbands are seen as pointless for those whose mobility is severely reduced. Some people in the MS group declared they did not know of any technology that could support their MS symptoms, despite being generally open-minded to AS and keeping themselves up to date with recent advancements. A salient topic throughout the sessions was the fatigue experienced by participants, for example participants in the stroke group extensively discussed ‘neuro-fatigue’ as commonly resulting from experiencing a stroke. There was consensus that it would be highly valuable to have AS that could help prevent and ease physical and mental fatigue, as well as emotional distress.
“I think this is where it gets really complicated because it's not just high activity or what you do in a day. So, I consider myself quite able physically and communication-wise, and I feel very fortunate for that but you saw me really struggle with the word 'alarm' today. Now that is because I'm really tired at the moment. I've had a lot going on in my head and physically for various different reasons.”
[P6S]
However, participants also found it difficult to picture how fatigue symptoms or emotional conditions like depression could not be easily detected by AS. Participants in both groups suggested that future AS should allow users to manually enter data about their emotional and mental states, so that it could learn from it and subsequently help to monitor and support them. They further proposed systems that could prompt entering data like a diary, using metaphors such as ‘battery-level’ to explain their energy states.
“So, a regular person, a non-stroke survivor, starts with a fairly full battery at the beginning of the day, whereas a stroke survivor typically starts with less [...] Because of that, the stroke survivor, the levels of fatigue kick in sooner than someone else's. And then you've got the added complication of neuro-fatigue. But if there was a way to potentially have that information, that whether there is qualitative or quantitative data information in the system somehow, so the system then learnt by that, urm, and then set you goals which took that into account, that would be, I mean, it would be really clever”
[P1S]
Additionally, two other subthemes specific to the stroke group were generated. Firstly, participants expressed concerns about becoming reliant on AS and losing their autonomy (subtheme 1c). In contrast to people in the MS group whose technology use for controlling and monitoring their home was seen as a way to gain independence and support, participants in the stroke group expressed strong concerns about losing their autonomy to AS if they depend too much on them. “It's more important for you to be independent than use this device obviously.” [P5S]. They felt that although technology is useful, it is important for them to complete tasks for themselves and push themselves physically and mentally to avoid becoming reliant on technology.
“You mustn't have these, too many of these benefits and these machines, otherwise you'll be sitting in the chair all day and it'll make a cup of tea for you.”
[P3S]
This could be explained by the physical differences between people in both groups, where those in the MS session reported more constrained mobility than those in the stroke group. Additionally, stroke participants often talked about having to re-learn tasks and re-wire their brains, which they felt would be harder if they relied on technology for common tasks.
Lastly, participants in the stroke group profoundly remarked on the need for integrating adaptability in AS design, not only to fit individual goals and needs but subsequently, to support emotional wellbeing (subtheme 1d). Whilst smartwatch users reported that tracking their daily steps could evoke feelings of happiness and pride, participants in the stroke group pointed out that the pre-set goals can seem unattainable and cause negative impact on participants’ emotional wellbeing.
“You're going to think ‘well I should be aiming for this’, and ‘I can't even do this’, so I think achievability [is key], and that's going to be individual obviously to the person because it's depending on everybody's needs.”.
[P6S]
These experiences become annoying and frustrating for participants and can push some to give up using the devices altogether. Adaptability could be based on the system learning automatically, but the ability to manually change goals and ‘correct’ assumptions made by the AS was highly important. Such flexibility needs to consider not only the differences between individuals but also how their physical and mental condition changes from day to day.
“I think also [name], you know, what you're able to do on Monday may drastically vary on another day, mightn’t it. So, if you're not able to change the goals and it's changing them for you, one day I'm capable of doing loads and another day I'm not. I'm done by about 11 o'clock.”
[P5S]
3.2. Theme 2. Attitudes towards the smart mirror
The second theme encompasses the participants’ feelings and attitudes towards the concept of a smart mirror. A range of desired functions were expressed (subtheme 2a). Both participant groups believed the smart mirror could potentially be especially useful for those with memory problems and those with mobility issues that could be picked up and monitored by the smart mirror.
“You know it's like... it's handy for those that've got a memory problem”
[P8S]
“As a prompt, it would be really good... I go far too long with a warped body, as it were”
[P2S]
Personal stories from the participants spoke to this potential useful feature, including a participant who reported spending long periods of time without seeing any other people and so suggested the smart mirror would be a useful tool to diagnose mobility issues such as issues with posture or gait, that would otherwise be missed until the next appointment with a healthcare provider. Another desired feature of the smart mirror would be to combine and summarise information from multiple sources and devices, including gathering data from external sources, such as patient records from the NHS, information from the individual through other devices, and through self-report input.
“I think that numerous data sets plus some way of getting in your NHS diagnosis – where you are on the scale or your different attributes. If all of those datasets feed through, I can see it actually being really, really helpful.”
[P3M]
This would also save the user from having to check multiple devices throughout the day for alarms, reminders, and other features. Participants also highlighted that a range of input methods would be needed to include those with a variety of physical problems, such as voice-activation for those with tremors, poor dexterity or other physical disabilities and other alternative activation functions for those with speech problems.
While most participants had largely positive views on the smart mirror concept and proposed ideas about what would make it useful, there were inevitably views that expressed concerns that would hinder adoption. Drawbacks included a lack of portability and hence inclusivity and practicality, as well as a sense of redundancy from having multiple technological devices that do the same job (subtheme 2b). To many participants, the mirror being in a fixed location was a major issue with its usefulness, as the AS would fail to capture activity done away from the smart mirror, and it would be easy to mislead the smart mirror by acting differently in front of it. In order to circumnavigate these issues, multiple smart mirrors would be needed around the home which may be expensive and impractical, and participants suggested it would be crucial to have the smart mirror linked to other, more portable devices. Many participants expressed concern over the practicality of setting up the smart mirror if the user was elderly or disabled in any way, as not every individual would have someone to help them set it up. Moreover, the smart mirror would need the user to have sufficient space in the home to complete exercises in front of it, thus inclusivity is lacking for those with limited living spaces.
“I think it's really important [name] saying how he's got a small space, so if it was to be a mirror, it wouldn't really work for him. And this is where my concern would be, that it's not all inclusive, and I think it's a really, really great idea, but I think the mirror idea needs possibly to be scrapped because I don't think that makes it accessible for everybody.”
[P2M]
There were also concerns that the mirror could not provide value to users in all stages of their medical condition journey, including those with and without regular check-ins with care providers, and those with differing needs. The final drawback discussed by both groups was the issue of technology redundancy and being overwhelmed by multiple devices. Multiple participants felt that the smart mirror was not distinguishable in function from other AS such as smartphones, smart speakers like Alexa, or tablets.
“I know my health flags; I know I've got my computer. I've got an Alexa that does most of that and a little screen on it. So, I don't understand what purpose there is [to the smart mirror]” [P8S].
Additionally, participants felt that having multiple technological devices along with the smart mirror would feel overwhelming and add to the mental fatigue felt by individuals with a medical condition such as MS or recovering from a stroke; participants felt technology is taxing for the older generation anyway, but with the addition of a medical condition that involves fatigue, the idea of the smart mirror along with other devices felt very overwhelming and unnecessary.
Participants also emphasized that messaging should be framed to avoid condescension or disrespect (subtheme 2c). For those who have a medical condition or have experienced a life-changing medical episode such as a stroke, there are consequences that can seriously affect mental wellbeing, such as having lower confidence and being more prone to depression and low mood. Therefore, the tone and content of messaging from the smart mirror should be positive, gentle, and encouraging to benefit wellbeing, rather than having an instructing, condescending, or demanding tone that may result in negative impact on the user’s mental health and wellbeing.
“It would reduce me to tears if it didn't have a very gentle approach, because when I'm having my bad days I already know I'm having a bad day and I know I can't get a coffee with my friend and that's horrible as it is. I don't need some flipping gadgets saying "and don't do this” ...I know that I'd be really upset and it would probably put me to the floor to be honest with you.”
[P2M]
“I think there's also something about how the, what the content of them – the message, whether it's a text message, whether it comes up on your phone. So, if you were expecting to hit 5000 steps because you have, you had like normal days before and you didn't quite do it, it should say in that sort of way, it should have a positive spin on it.”
[P1S]
Finally, specifically in the MS group, participants felt that attitudes towards the smart mirror would depend largely on how useful it was to the individual (subtheme 2d). For example, some participants would want a trial period of the smart mirror before purchasing it to assess its usefulness before committing to the technology. Similarly, the participants’ trust in the smart mirror would be conditional on trust in where the technology and the data it used was coming from, such as having high trust in the NHS. “Well, I would assume that it's coming from a trustworthy source, whoever's programming it, is that coming from the NHS? Or who's putting information into it?” [P2M]
3.3. Theme 3. Attitudes towards data sharing
The third theme combines the different views on data sharing within the context of health monitoring. Overall, there is a willingness to share data with healthcare professionals, if it is under the control of the participants (subtheme 3a), as different people feel comfortable sharing different types of data under diverse circumstances.
“I think it has to be the user. That's what personally I would think because somebody else could abuse the situation.”
[P7S]
The conditions that would have to be met for different participants to be willing to share their data range from the ability to review the data before sharing it with healthcare professionals, the option to opt out of sending data to GPs, data being anonymized before sharing and the option to only share specific types of data.
“You need to have some control over it, either to be able to say ‘no, I don't want the data to go’... or to know that it's gonna go by the right routes and be anonymized.”
[P4M]
Some participants also only felt comfortable sharing their data with specific healthcare professionals (for example, sharing data with physiotherapists but not GPs). While the specific conditions vary, all have the commonality of giving control of the data to the user.
Participants from both groups also raised points regarding the feasibility of data sharing in terms of availability and attitudes of different healthcare providers (subtheme 3b). There were concerns about the use and practicalities associated with sharing the data, for example some were skeptical that healthcare professionals would have time to review any data that was shared.
“But how often is it, the doctors are very busy, would they have time to look at it? If they've got ten people on their books that have got a mirror, and they're all supplying data, how do they deal with it? They're overstretched as it is.” [P8S]
If data was to be shared with healthcare professionals, there is an expectation that this data would be used to inform their individual treatment.
“I want the NHS to actually be doing something on the other end rather than just providing data to them for them to collate. I want it to go to, you know, I want it to go to my consultant. I want it to be looked at for my annual reviews and things like that. I'd like it to go to the GP because you know, if it's not being used for beneficial purpose, there's really not much point giving it to them.”
[P3M]
The variation of attitudes towards data sharing is further seen in Themes 3c and 3d. Some participants from the Stroke group did not have such positive attitudes, caused by worries about the consequences of data sharing with medical institutions, in particular the effect on receiving care services and benefits (subtheme 3c). They expressed concerns that it could affect their access to services such as not getting physiotherapy appointments or Government benefits if the data that was reported was interpreted as them not needing health or economic support.
“I think you'd have to be very careful though because it might catch you on a real good day, you know, and sort of take that as an example, report it back to your doctor. Then all your benefits go, if you're on benefits of any sort, you know.”
[P5S]
A lack of trust was also conveyed as participants questioned the intentions of the mirror manufacturer and the need to collect personal data, which had a subsequent effect on the likelihood and willingness of participants to share their data. Interestingly, these concerns were only mentioned by participants from the Stroke Group, whereas participants in the MS Group were more open-minded towards data sharing (subtheme 3d), but again positive attitudes towards the smart mirror are conditional on its usefulness to the individuals and if it benefitted others and the medical community. A few participants had several years of taking part in medical research, thus feeling comfortable sharing their data with the hope that it could advance scientific knowledge and support for people with their condition in the future. Moreover, they reported being happy to share their data with their health care professionals to improve their own care. However, they are less comfortable sharing their data with other stakeholders outside of the health care institutions. Having their information sold to third-party companies, especially if it was not anonymised, would not be happily approved.
“I was gonna say for me personally I have no problems with the NHS having my full data, it’s when it gets outside of the realms of the NHS, I'm not comfortable with the data being shared. It would have to be anonymous outside of the NHS.”
[P3M]
4. Discussion
Using design fictions, our study of people with MS and those who recover from a stroke elicited their current use of technology in their healthcare regime and their attitudes towards future autonomous healthcare systems integrated into smart appliances, especially a smart mirror, in the home. Our findings describe a complex landscape of tensions between advantages and disadvantages of a smart mirror being involved in personal healthcare at home, the intricacies and details of which we discuss in the following and synthesize into design recommendations.
4.1. The current use of and perceptions about AS
Many participants already made use of a range of technologies to control and monitor their home, such as lightbulbs, plugs, thermostats, doorbell cameras, and other smart home technologies. These devices helped them to feel a sense of autonomy and support, especially where they had limited mobility or other physical issues. This is consistent with findings from Ayobi et al [
17], showing that people with health issues can benefit from AS and self-tracking behaviours due to gaining a sense of control over unpredictable conditions. However, technology is not a solution for all participants, as some MS participants found AS to be inadequate to their circumstances. This showcases the importance of integration of AS for healthcare within the specific circumstances of the user, and need for diversity and flexibility of AS. An important point, especially among the participants in the stroke group, was that overuse and overdependence on such smart technologies may lead to a loss of autonomy and a detriment to their health, hence they were reluctant to add any additional technology to their routines.
4.1.1. The ecosystem of devices used for lifestyle and self-management.
Participants often discussed the value of using smart phones and smart speakers for setting alarms and reminders for daily tasks such as remembering to take medication, and calendars and notes for planning activities. This helped them to deal with the memory problems experienced by many in both groups. A couple of participants also discussed apps for brain training and meditation to support cognitive and mental wellbeing, reverberating the desire for mindfulness activities in health apps discussed by Di Cara et al [
21]. Others used smartwatches or fitness bands to monitor their daily activities such as walking and sleeping. However, most of the time they did not speak of these technologies in terms of ‘healthcare’, often stating that they did not use any technology to support their physical or mental health.
Combined with the range of in-home devices in use by many participants, it is clear that they have created for themselves an ecosystem of devices that help them to manage their day-to-day lives and their health conditions. On the surface, this seems to suggest a form of ubiquitous computing similar to Mark Weiser’s vision [
69], with a multitude of (networked) computing devices within reach at all times. However, unlike in Weiser’s vision, there was a clear distinction for participants between lifestyle management technologies and specific healthcare devices. Some, especially in the MS group, stated they did not know of any technology that could support their symptoms, despite using a range of devices and having a general open-mindedness towards future developments. This highlights how the quantified self is not accessible to all people currently, potentially rendering some “statistically invisible” depending on how the AS data is used. It also highlights an opportunity to make the link between lifestyle management/the quantified self and their healthcare regime more legible to users by (1) increasing applications to different symptoms, (2) more directly connecting and contributing to their healthcare, and (3) /networking the different devices to increase their value in a user’s healthcare regime.
4.2. The addition of smart mirrors to support physical and mental health
A major point that emerged throughout the focus groups was that everyone has a unique journey through their health diagnoses, and individual experiences of having a medical condition need to be considered in the design of AS. The consensus among most participants, especially in the Stroke Group, was that the AS would need to be flexible and inclusive to adapt to the user’s unique abilities. And while the technology is adaptative [
31], it is so only within a very constrained setting. MS can be a degenerative condition and hence people at different stages will have different needs from the AS. Participants in the Stroke Group also acknowledged the importance of the AS needing to consider or be adaptable to the different stages of the journey one experiences when having a medical condition. Attitudes towards the smart mirror depended greatly on its’ perceived usefulness to the specific healthcare journey of the individual. Overall, technology such as the smart mirror has the potential to help with daily life and reduce stress and neuro-fatigue, in turn improving general wellbeing, which will likely have positive effects on specific medical conditions, such as MS. However, the design needs to consider specific use cases of those who can benefit from it the most, while also being “non-fatiguing”. This could, for example, be achieved by technology, including smart mirrors, being unobtrusive and operating in the “background”, which would “not require active attention”, as described by Weiser [
69]. Moreover, any health technology should take into consideration economical, physical, and social external factors [
70].
Whilst both groups felt that a smart mirror might be potentially useful to those with memory problems, and as lifestyle management to prevent and support fatigue, the major appeal of the smart mirror concept was for physical therapy, gait analysis, and other physical support, especially in between healthcare appointments. This is echoed in the literature, given that AS for these conditions have so far focused on mobility and balance, gait and movement analysis, and limb rehabilitation [
16,
18,
19,
20]. Given the desire to not become overly reliant on technology, such features should be designed to be non-addictive, and with the aim of becoming redundant by training users to not need the technology.
The relationship between technology, health professionals, patients, and wider health considerations was also highly important to participants. Some were concerned that the mirror would not provide value for users who did not have regular contact with care providers, including GPs and physiotherapists, who could oversee the use of the mirror and input or modify care plans. Conversely, there was skepticism that even those who regularly saw a care professional would see any added value. This was often because they felt that GPs were particularly so overstretched that they would not have time to review the vast quantities of data that could be shared, and hence there was no point in sharing it if it was not to be used to improve their individual care. There was an overwhelming sense that health institutions do not have the capacity to undertake this approach to health; it is important that AS is designed to support and not overwhelm the healthcare professionals as well as the user. This could be done through automated visualisations, AS that could highlight changes and anomalies, and that could connect to health records and reports from patients to provide a useful overview/dashboard. Whilst many would be most comfortable sharing data with physiotherapists, a further concern, especially among the stroke group, was that any data sharing could be used to remove rather than support care, for example by making them lower priority for appointments. In a wider sense there was also fear it could be used to deny their claims for Government benefits, if the data indicated they were improving or did not hit a threshold for support. These last two points illustrate a lack of trust in government and (healthcare) institutions, rather than the technology itself.
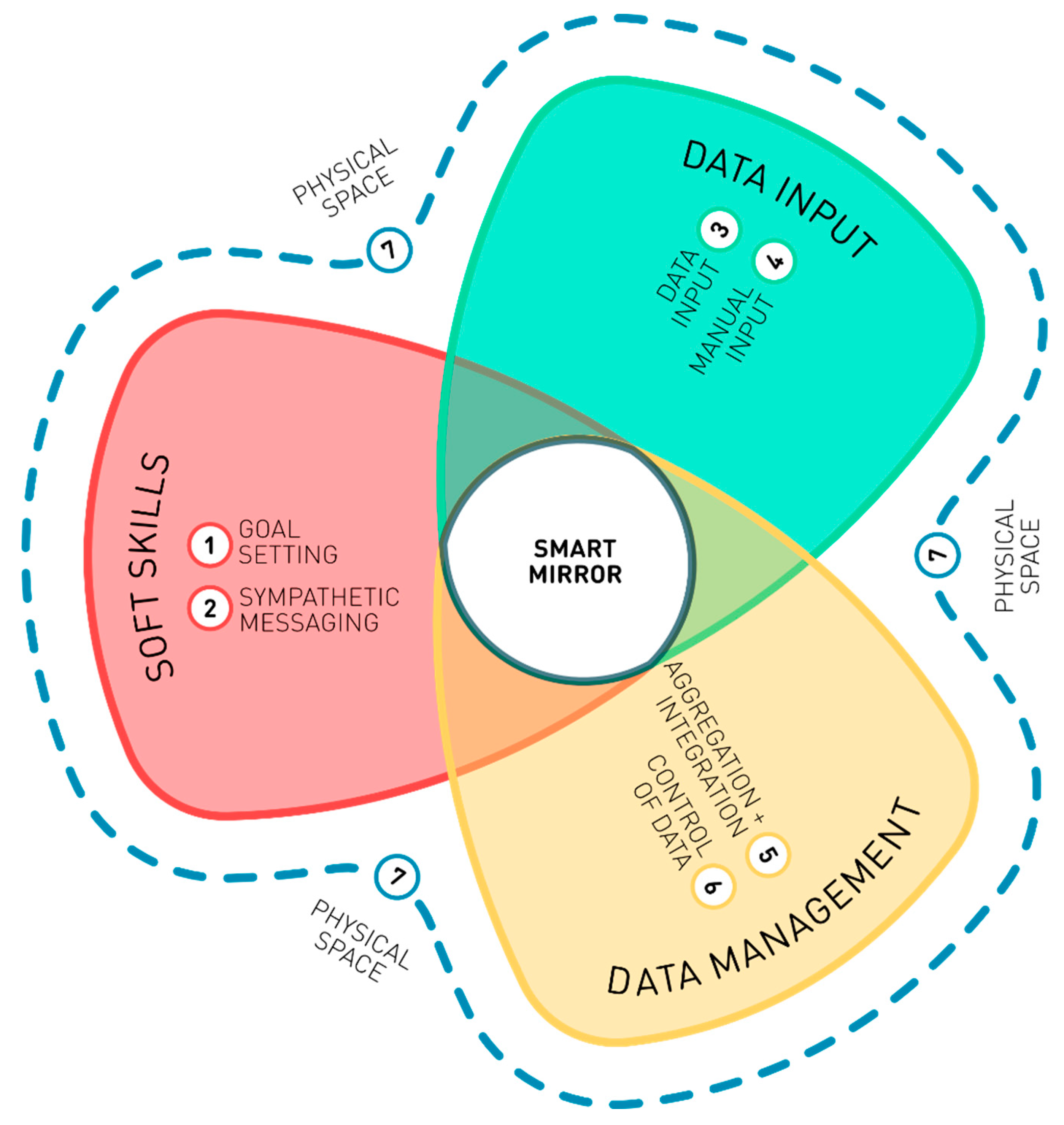
4.2.1. Recommendations for necessary technical features of a smart mirror
Participants made a series of recommendations for features that would be necessary to smart mirror adoption, which is shown in
Figure 4.
Goal setting. The goals for activity and other tasks should be user-led and variable based on user data, as autonomous goal setting is often tailored to the average individual and does not consider symptoms such as fatigue which can lead to a negative impact on wellbeing for the user if the goal is unattainable.
Sympathetic messaging. Messaging should be framed to be sympathetic, uncondescending/respectful, and encouraging. Participants emphasized that people with health concerns often have lower confidence and be more prone to depression and low mood, and that messaging that was instructing or demanding may have negative impact on the user’s mental health and wellbeing.
Input methods. It is vital that a smart mirror supports a variety of input methods, to be inclusive to those with a variety of physical problems. These include voice-activation, keyboard, and touch screens, to support people with speech problems, tremors, poor dexterity and so on.
Manual entry. The smart mirror should allow manual entry of emotional and mental states including fatigue, with prompts to enter data, for example indicating wellness levels at the start of the day and at points throughout. This data would need to be aggregated with the automatically collected data for the AS to learn about the users’ needs. This also highlights the need for technology to be user-led and enhance rather than undermine autonomy.
Aggregation and integration. A smart mirror should connect to, aggregate, and display data from other devices, to automate detection of individual patterns, and notify users when patterns changed or when thresholds were reached. This includes pulling data from patient records, manual input, and smart home devices, as well as mobile phones and smart watches. Such seamless integration could help to prevent fatigue, and support care management, by saving the user from having to check multiple devices throughout the day for alarms, reminders, and other features.
Control of data. Sharing of data should always be in control of the participants, including which data to share and with whom, as well as levels of anonymisation and aggregation.
Physical space. A smart mirror should be physically and functionally accessible. It should be located in space appropriate for it to function. For example, if assessing gait or posture, there should be sufficient space in front of the mirror for a person to walk or stand at the required distance from the mirror.
4.2.2. Perceived barriers to use a smart mirror
Participants also highlighted several potentially adverse or unexpected outcomes which could be barriers to the user of a smart mirror.
Lack of portability and practicality. The mirror being in a fixed location is a major issue for its perceived usefulness, with concerns that it would fail to capture important activities. Multiple smart mirrors would be needed around the home, which may be impractical and expensive, and hence the need for the smart mirror to be linked to other, more portable devices.
Lack of accessibility and inclusivity. Setting up a smart mirror may be difficult or impossible for users who are elderly or disabled in any way, as not everyone has someone to help them set it up. The smart mirror would also require a sufficient amount of space to collect certain data, or to facilitate tasks such as exercises, limiting its’ inclusivity.
Redundancy and the overwhelming nature of multiple devices. There was a strong sense that a smart mirror would be redundant given that most people already have multiple technological devices that do the same job, and that the additional of more devices would be overwhelming and add to mental fatigue throughout the day.
Lack of trust in data sharing. As discussed in section 4.2, participants had strong feelings about sharing data with healthcare systems, including a fear that such sharing may lead to a removal of vital services. This lack of trust was also evident in sharing with others, outside of the healthcare setting, especially device manufacturers.
5. Conclusion
New appliances, such as a smart mirror, offer opportunities to support healthcare at home. However, as our stakeholder engagement has revealed, such technology requires careful design in terms of hardware (e.g., the device’s precise location in the home) and software (e.g., responding appropriately to highly personal and variable health conditions). Our study was limited to two patient groups of people with MS and people who have had a stroke. Engaging patient groups with different conditions and focusing on a diversity of AS systems will likely extend and help to make our design recommendations more comprehensive and robust. A next step of our research will be the design and physical deployment of a smart mirror in a real-world context to test our design recommendations.
Author Contributions
Conceptualization, all authors.; methodology, all authors.; formal analysis, G.R.C, A.R.P. and C.P; investigation, L.D, P.B, G.R.C., C.P, and A.R.P.; ; resources, L.D, N.J., and P.B.; data curation, all authors.; writing—original draft preparation, L.D, G.R.C, A.R.P., C.P. and N.J.; writing—review and editing, L.D, G.R.C, A.R.P., C.P., N.J, R.N, and P.B.; visualization, N.J.; supervision, L.D and N.J; project administration, L.D and N.J.; funding acquisition, L.D, N.J, A-M.H., R.N., D.C-K., S.C., and S.B. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Engineering and Physical Sciences Research Council, grant number EP/V00784X/1.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Research Ethics Committee of The School of Computer Science at the University of Nottingham (ref CS-2020-R67 approved 14th October 2021).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Qualitative data (transcripts) from the focus groups is unavailable due to privacy and ethical concerns.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results.
Appendix A
A.1. Positive Scenario Video Script
Jenny has a smart mirror installed in her home. She uses it for monitoring her health after she had a stroke. Every morning, when Jenny wakes up, she activates the mirror, and it greets her with a friendly ‘hello’ and a summary of the day ahead for her. Throughout the day, the mirror helps out by providing reminders for events by linking to Jenny’s calendar, recognising when Jenny is standing in front of it and monitoring posture and facial expression, making suggestions for what to do based on the data it has collected over time, and guiding Jenny through daily exercises and mindfulness activities. At 10am, the mirror reminds Jenny that it is time for her to take her medication. It also reminds her to order another prescription and offers to do that for her. Later in the day, when Jenny enters the bathroom, the mirror praises Jenny for the improvement in her posture and asks how she is feeling today. After lunch, the mirror suggests a nice walk as the weather is good and the data shows that a few short walks a week is good for Jenny’s symptoms. At 4pm, the mirror suggests some gentle exercises to maintain her good posture. It guides Jenny through them a couple of times to make her comfortable. Then it does a short meditation with her to wind down. At the end of the day, the mirror prompts Jenny that it is close to her bedtime and suggests some calming activities to wind down. Before bed, the mirror displays the day’s data to Jenny and asks her if she would like to share it with any of her designated contacts.
A.2. Negative Scenario Video Script
Jenny has a smart mirror installed in her home. She uses it for monitoring her health after she had a stroke. Every morning, when Jenny wakes up, the mirror recognises that she is up and promptly provides a list of things to do for the day ahead of her. Throughout the day, the mirror provides regular notifications which Jenny must respond to. It provides reminders for events by linking to Jenny’s calendar, recognises when Jenny is standing in front of it and monitoring posture and facial expression, makes suggestions for what to do based on the data it has collected over time, and guides Jenny through daily exercises and mindfulness activities. At 10am, the mirror tells Jenny that it is time to take her medication. As she does not immediately respond it prompts her several more times. Later in the day, when Jenny enters the bathroom, the mirror berates her and tells her that her posture has gotten worse. It tells her that she should check in more often. After lunch, the mirror tells Jenny to cancel her plans as she has been overdoing it. It removes a coffee date from her calendar. At 4pm, the mirror tells Jenny that she should do some extra exercises due to her posture measurements earlier. It skips the mindfulness activities for that day, prioritising the exercise. This cannot be overridden. At the end of the day, the mirror tells Jenny that it is her bedtime and begins a countdown for turning off the television and main lights. Before bed, the mirror sends all of the data it has collected over the day to the manufacturer of the mirror and to Jenny’s GP.
References
- Belliger, A.; Krieger, D.J. From Quantified to Qualified Self: A Fictional Dialogue at the Mall. Digital Culture & Society 2016, 2, 25–40. [Google Scholar] [CrossRef]
- Browne, M. Quantified Self; Dublin City Council (Arts Office), 2011; ISBN 978-0-9554281-5-9. [Google Scholar]
- Lupton, D. The Quantified Self; John Wiley & Sons, 2016; ISBN 978-1-5095-0060-4. [Google Scholar]
- Meißner, S. Effects of Quantified Self Beyond Self-Optimization. In Lifelogging: Digital self-tracking and Lifelogging - between disruptive technology and cultural transformation; Selke, S., Ed.; Springer Fachmedien: Wiesbaden, 2016; pp. 235–248. ISBN 978-3-658-13137-1. [Google Scholar]
- Spanakis, E.G.; Santana, S.; Tsiknakis, M.; Marias, K.; Sakkalis, V.; Teixeira, A.; Janssen, J.H.; Jong, H. de; Tziraki, C. Technology-Based Innovations to Foster Personalized Healthy Lifestyles and Well-Being: A Targeted Review. Journal of Medical Internet Research 2016, 18, e4863. [Google Scholar] [CrossRef]
- Hesketh, R. Trusted Autonomous Systems in Healthcare: A Policy Landscape Review; 2021.
- OECD Trustworthy AI in Health: Background Paper for the G20 AI Dialogue, Digital Economy Task Force; Saudi Arabia, 2020;
- Tan, S.Y.; Taeihagh, A. Governing the Adoption of Robotics and Autonomous Systems in Long-Term Care in Singapore. Policy and Society 2021, 40, 211–231. [Google Scholar] [CrossRef]
- Avram, R.; Olgin, J.E.; Kuhar, P.; Hughes, J.W.; Marcus, G.M.; Pletcher, M.J.; Aschbacher, K.; Tison, G.H. A Digital Biomarker of Diabetes from Smartphone-Based Vascular Signals. Nat Med 2020, 26, 1576–1582. [Google Scholar] [CrossRef]
- Brigham and Women’s Hospital Brigham Researchers Develop Smartphone-Based Ovulation Test. Available online: https://www.brighamandwomens.org/about-bwh/newsroom/press-releases-detail?id=3221 (accessed on 26 June 2023).
- Chatrati, S.P.; Hossain, G.; Goyal, A.; Bhan, A.; Bhattacharya, S.; Gaurav, D.; Tiwari, S.M. Smart Home Health Monitoring System for Predicting Type 2 Diabetes and Hypertension. Journal of King Saud University - Computer and Information Sciences 2022, 34, 862–870. [Google Scholar] [CrossRef]
- Esteva, A.; Kuprel, B.; Novoa, R.A.; Ko, J.; Swetter, S.M.; Blau, H.M.; Thrun, S. Dermatologist-Level Classification of Skin Cancer with Deep Neural Networks. Nature 2017, 542, 115–118. [Google Scholar] [CrossRef]
- Mariakakis, A.; Baudin, J.; Whitmire, E.; Mehta, V.; Banks, M.A.; Law, A.; Mcgrath, L.; Patel, S.N. PupilScreen: Using Smartphones to Assess Traumatic Brain Injury. Proc. ACM Interact. Mob. Wearable Ubiquitous Technol. 2017, 1, 81:1–81:27. [Google Scholar] [CrossRef]
- Wang, K.; Varma, D.S.; Prosperi, M. A Systematic Review of the Effectiveness of Mobile Apps for Monitoring and Management of Mental Health Symptoms or Disorders. Journal of Psychiatric Research 2018, 107, 73–78. [Google Scholar] [CrossRef]
- Tulipani, L.J.; Meyer, B.; Allen, D.; Solomon, A.J.; McGinnis, R.S. Evaluation of Unsupervised 30-Second Chair Stand Test Performance Assessed by Wearable Sensors to Predict Fall Status in Multiple Sclerosis. Gait & Posture 2022, 94, 19–25. [Google Scholar] [CrossRef]
- Sun, R.; McGinnis, R.; Sosnoff, J.J. Novel Technology for Mobility and Balance Tracking in Patients with Multiple Sclerosis: A Systematic Review. Expert Review of Neurotherapeutics 2018, 18, 887–898. [Google Scholar] [CrossRef]
- Ayobi, A.; Marshall, P.; Cox, A.L.; Chen, Y. Quantifying the Body and Caring for the Mind: Self-Tracking in Multiple Sclerosis. In Proceedings of the Proceedings of the 2017 CHI Conference on Human Factors in Computing Systems; Association for Computing Machinery: New York, NY, USA, May 2, 2017; pp. 6889–6901. [Google Scholar]
- Cha, K.; Wang, J.; Li, Y.; Shen, L.; Chen, Z.; Long, J. A Novel Upper-Limb Tracking System in a Virtual Environment for Stroke Rehabilitation. Journal of NeuroEngineering and Rehabilitation 2021, 18, 166. [Google Scholar] [CrossRef] [PubMed]
- Lloréns, R.; Alcañiz, M.; Colomer, C.; Navarro, M.D. Balance Recovery Through Virtual Stepping Exercises Using Kinect Skeleton Tracking: A Follow-Up Study With Chronic Stroke Patients. In Annual Review of Cybertherapy and Telemedicine 2012; IOS Press, 2012; pp. 108–112. [Google Scholar]
- Zheng, H.; Black, N.D.; Harris, N.D. Position-Sensing Technologies for Movement Analysis in Stroke Rehabilitation. Med. Biol. Eng. Comput. 2005, 43, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Di Cara, M.; Grezzo, D.; Palmeri, R.; Lo Buono, V.; Cartella, E.; Micchia, K.; Formica, C.; Rifici, C.; Sessa, E.; D’Aleo, G.; et al. Psychological Well-Being in People with Multiple Sclerosis: A Descriptive Review of the Effects Obtained with Mindfulness Interventions. Neurol Sci 2022, 43, 211–217. [Google Scholar] [CrossRef] [PubMed]
- Wijeratne, T.; Sales, C. Understanding Why Post-Stroke Depression May Be the Norm Rather Than the Exception: The Anatomical and Neuroinflammatory Correlates of Post-Stroke Depression. Journal of Clinical Medicine 2021, 10, 1674. [Google Scholar] [CrossRef]
- Skolnik, N.S.; Horn, D.B. Lifestyle Management. Journal of Family Practice 2016, 65, SS13–SS13. [Google Scholar]
- Rippe, J.M.; Crossley, S.; Ringer, R. Obesity as a Chronic Disease: Modern Medical and Lifestyle Management. J Am Diet Assoc 1998, 98, S9–15. [Google Scholar] [CrossRef] [PubMed]
- American Diabetes Association 4. Lifestyle Management: Standards of Medical Care in Diabetes—2018. Diabetes Care 2017, 41, S38–S50. [Google Scholar] [CrossRef]
- Huang, N.; Duggan, K.; Harman, J. Lifestyle Management of Hypertension. Aust Prescr 2008, 31, 150–153. [Google Scholar] [CrossRef]
- Berk, M.; Sarris, J.; Coulson, C.E.; Jacka, F.N. Lifestyle Management of Unipolar Depression. Acta Psychiatr Scand Suppl 2013, 38–54. [Google Scholar] [CrossRef]
- Hoeger, K.M. Obesity and Lifestyle Management in Polycystic Ovary Syndrome. Clin Obstet Gynecol 2007, 50, 277–294. [Google Scholar] [CrossRef]
- Kaundal, A.; Renjhen, P.; Kumari, R.; Kaundal, A.; Renjhen, P.; Sr, R.K. Awareness of Lifestyle Modifications in the Management of Polycystic Ovarian Syndrome: A Hospital-Based Descriptive Cross-Sectional Study. Cureus 2023, 15. [Google Scholar] [CrossRef] [PubMed]
- Habib, N.; Buzzaccarini, G.; Centini, G.; Moawad, G.N.; Ceccaldi, P.-F.; Gitas, G.; Alkatout, I.; Gullo, G.; Terzic, S.; Sleiman, Z. Impact of Lifestyle and Diet on Endometriosis: A Fresh Look to a Busy Corner. Prz Menopauzalny 2022, 21, 124–132. [Google Scholar] [CrossRef]
- Chatterjee, A.; Prinz, A.; Gerdes, M.; Martinez, S. Digital Interventions on Healthy Lifestyle Management: Systematic Review. J Med Internet Res 2021, 23, e26931. [Google Scholar] [CrossRef] [PubMed]
- Maglaveras, N.; Chouvarda, I.; Koutkias, V.; Lekka, I.; Tsakali, M.; Tsetoglou, S.; Maglavera, S.; Leondaridis, L.; Zeevi, B.; Danelli, V.; et al. Citizen Centered Health and Lifestyle Management via Interactive TV: The PANACEIA-ITV Health System. In Proceedings of the AMIA 2003 Symposium Proceedings; 2003; pp. 415–419. [Google Scholar]
- Karagiannis, G.E.; Stamatopoulos, V.G.; Roussos, G.; Kotis, T.; Gatzoulis, M.A. Health and Lifestyle Management via Interactive TV in Patients with Severe Chronic Cardiovascular Diseases. J Telemed Telecare 2006, 12, 17–19. [Google Scholar] [CrossRef]
- Sezgin, E.; Militello, L.K.; Huang, Y.; Lin, S. A Scoping Review of Patient-Facing, Behavioral Health Interventions with Voice Assistant Technology Targeting Self-Management and Healthy Lifestyle Behaviors. Transl Behav Med 2020, 10, 606–628. [Google Scholar] [CrossRef]
- Cvetkoska, B.; Marina, N.; Bogatinoska, D.C.; Mitreski, Z. Smart Mirror E-Health Assistant — Posture Analyze Algorithm Proposed Model for Upright Posture. In Proceedings of the IEEE EUROCON 2017 -17th International Conference on Smart Technologies; July 2017; pp. 507–512.
- Rachakonda, L.; Rajkumar, P.; Mohanty, S.P.; Kougianos, E. IMirror: A Smart Mirror for Stress Detection in the IoMT Framework for Advancements in Smart Cities. In Proceedings of the 2020 IEEE International Smart Cities Conference (ISC2); September 2020; pp. 1–7. [Google Scholar]
- Fujinami, K.; Kawsar, F.; Nakajima, T. AwareMirror: A Personalized Display Using a Mirror. In Proceedings of the Pervasive Computing; Gellersen, H.-W., Want, R., Schmidt, A., Eds.; Springer: Berlin, Heidelberg, 2005; pp. 315–332. [Google Scholar]
- Besserer, D.; Bäurle, J.; Nikic, A.; Honold, F.; Schüssel, F.; Weber, M. Fitmirror: A Smart Mirror for Positive Affect in Everyday User Morning Routines. In Proceedings of the Proceedings of the Workshop on Multimodal Analyses enabling Artificial Agents in Human-Machine Interaction; Association for Computing Machinery: New York, NY, USA, 12 November 2016; pp. 48–55. [Google Scholar]
- Poh, M.-Z.; McDuff, D.; Picard, R. A Medical Mirror for Non-Contact Health Monitoring. In Proceedings of the ACM SIGGRAPH 2011 Emerging Technologies; Association for Computing Machinery: New York, NY, USA, 7 August 2011; p. 1. [Google Scholar]
- Calvo, R.A.; Peters, D. Design for Wellbeing - Tools for Research, Practice and Ethics. In Proceedings of the Extended Abstracts of the 2019 CHI Conference on Human Factors in Computing Systems; Association for Computing Machinery: New York, NY, USA, 2 May 2019; pp. 1–5. [Google Scholar]
- Architecture and Health: Guiding Principles for Practice; Battisto, D. , Wilhelm, J.J., Eds.; Routledge: New York, 2019; ISBN 978-0-429-02116-9. [Google Scholar]
- Astell-Burt, T.; Feng, X. Association of Urban Green Space With Mental Health and General Health Among Adults in Australia. JAMA Network Open 2019, 2, e198209. [Google Scholar] [CrossRef] [PubMed]
- Marques, B.; McIntosh, J.; Chanse, V. Improving Community Health and Wellbeing Through Multi-Functional Green Infrastructure in Cities Undergoing Densification. Acta Horticulturae et Regiotecturae 2020, 23, 101–107. [Google Scholar] [CrossRef]
- Nielsen, T.S.; Hansen, K.B. Do Green Areas Affect Health? Results from a Danish Survey on the Use of Green Areas and Health Indicators. Health & Place 2007, 13, 839–850. [Google Scholar] [CrossRef]
- Jazizadeh, F.; Kavulya, G.; Klein, L.; Becerik-Gerber, B. Continuous Sensing of Occupant Perception of Indoor Ambient Factors. 2012, 161–168. [CrossRef]
- Dong, B.; Prakash, V.; Feng, F.; O’Neill, Z. A Review of Smart Building Sensing System for Better Indoor Environment Control. Energy and Buildings 2019, 199, 29–46. [Google Scholar] [CrossRef]
- Costa, Â.; Castillo, J.C.; Novais, P.; Fernández-Caballero, A.; Simoes, R. Sensor-Driven Agenda for Intelligent Home Care of the Elderly. Expert Systems with Applications 2012, 39, 12192–12204. [Google Scholar] [CrossRef]
- Moraitou, M.; Pateli, A.; Fotiou, S. Smart Health Caring Home: A Systematic Review of Smart Home Care for Elders and Chronic Disease Patients. Adv Exp Med Biol 2017, 989, 255–264. [Google Scholar] [CrossRef] [PubMed]
- Demir, E.; Köseoğlu, E.; Sokullu, R.; Şeker, B. Smart Home Assistant for Ambient Assisted Living of Elderly People with Dementia. Procedia Computer Science 2017, 113, 609–614. [Google Scholar] [CrossRef]
- Tiersen, F.; Batey, P.; Harrison, M.J.C.; Naar, L.; Serban, A.-I.; Daniels, S.J.C.; Calvo, R.A. Smart Home Sensing and Monitoring in Households With Dementia: User-Centered Design Approach. JMIR Aging 2021, 4, e27047. [Google Scholar] [CrossRef] [PubMed]
- McIntyre, D.; Chow, C.K. Waiting Time as an Indicator for Health Services Under Strain: A Narrative Review. INQUIRY: The Journal of Health Care Organization, Provision, and Financing 2020, 57. [Google Scholar] [CrossRef] [PubMed]
- Cooksley, T.; Clarke, S.; Dean, J.; Hawthorne, K.; James, A.; Tzortziou-Brown, V.; Boyle, A. NHS Crisis: Rebuilding the NHS Needs Urgent Action. BMJ 2023, 380, 1. [Google Scholar] [CrossRef] [PubMed]
- Fuster, V. Changing Demographics. Journal of the American College of Cardiology 2017, 69, 3002–3005. [Google Scholar] [CrossRef]
- World Health Organization Ageing and Health. Available online: https://www.who.int/news-room/fact-sheets/detail/ageing-and-health (accessed on 26 June 2023).
- Perisetti, A.; Goyal, H. Successful Distancing: Telemedicine in Gastroenterology and Hepatology During the COVID-19 Pandemic. Dig Dis Sci 2021, 66, 945–953. [Google Scholar] [CrossRef]
- Shanbehzadeh, S.; Tavahomi, M.; Zanjari, N.; Ebrahimi-Takamjani, I.; Amiri-arimi, S. Physical and Mental Health Complications Post-COVID-19: Scoping Review. Journal of Psychosomatic Research 2021, 147, 110525. [Google Scholar] [CrossRef]
- Kumar, A.; Narayan, R.K.; Prasoon, P.; Kumari, C.; Kaur, G.; Kumar, S.; Kulandhasamy, M.; Sesham, K.; Pareek, V.; Faiq, M.A.; et al. COVID-19 Mechanisms in the Human Body—What We Know So Far. Frontiers in Immunology 2021, 12. [Google Scholar] [CrossRef]
- Violant-Holz, V.; Gallego-Jiménez, M.G.; González-González, C.S.; Muñoz-Violant, S.; Rodríguez, M.J.; Sansano-Nadal, O.; Guerra-Balic, M. Psychological Health and Physical Activity Levels during the COVID-19 Pandemic: A Systematic Review. International Journal of Environmental Research and Public Health 2020, 17, 9419. [Google Scholar] [CrossRef]
- Marashi, M.Y.; Nicholson, E.; Ogrodnik, M.; Fenesi, B.; Heisz, J.J. A Mental Health Paradox: Mental Health Was Both a Motivator and Barrier to Physical Activity during the COVID-19 Pandemic. PLOS ONE 2021, 16, e0239244. [Google Scholar] [CrossRef] [PubMed]
- Werneck, G.L. Long-Term Mass Population Effects of the COVID-19 Pandemic: A Long Way to Go. Cad. Saúde Pública 2022, 38, e00115222. [Google Scholar] [CrossRef] [PubMed]
- Chi, C.G.; Chi, O.H.; Ouyang, Z. Wellness Hotel: Conceptualization, Scale Development, and Validation. International Journal of Hospitality Management 2020, 89, 102404. [Google Scholar] [CrossRef]
- Oosterhuis, K.; Biloria, N. Interactions with Proactive Architectural Spaces: The Muscle Projects. Commun. ACM 2008, 51, 70–78. [Google Scholar] [CrossRef]
- Jäger, N.; Schnädelbach, H.; Hale, J.; Kirk, D.; Glover, K. Reciprocal Control in Adaptive Environments. Interacting with Computers 2017, 29, 512–529. [Google Scholar] [CrossRef]
- Schnädelbach, H.; Jäger, N.; Urquhart, L. Adaptive Architecture and Personal Data. ACM Trans. Comput.-Hum. Interact. 2019, 26, 12:1–12:31. [Google Scholar] [CrossRef]
- UKRI Framework for Responsible Research and Innovation. Available online: https://www.ukri.org/about-us/epsrc/our-policies-and-standards/framework-for-responsible-innovation/ (accessed on 26 June 2023).
- Jäger, N.; Dowthwaite, L.; Barnard, P.; Hughes, A.-M.; das Nair, R.; Crepaz-Keay, D.; Cobb, S.; Lang, A.; Vayani, F.; Benford, S. Reflections on RRI in “TAS for Health at Home. ” Journal of Responsible Technology 2022, 12, 100049. [Google Scholar] [CrossRef]
- Urquhart, L.; Craigon, P. The Moral-IT Deck: A Tool for Ethics by Design. Journal of Responsible Innovation 2021, 8, 94–126. [Google Scholar] [CrossRef]
- Braun, V.; Clarke, V. Using Thematic Analysis in Psychology. Qualitative Research in Psychology 2006, 3, 77–101. [Google Scholar] [CrossRef]
- Weiser, M. The Computer for the 21st Century. 1991, 1, 19–25. 25. [CrossRef]
- Costa-García, Á.; Okajima, S.; Yang, N.; Ueda, S.; Shimoda, S. Current Trends and Challenges towards the Digital Health Era. In Proceedings of the 2022 IEEE International Conference on Advanced Robotics and Its Social Impacts (ARSO); May 2022; pp. 1–5.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).