Submitted:
04 July 2023
Posted:
06 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Results
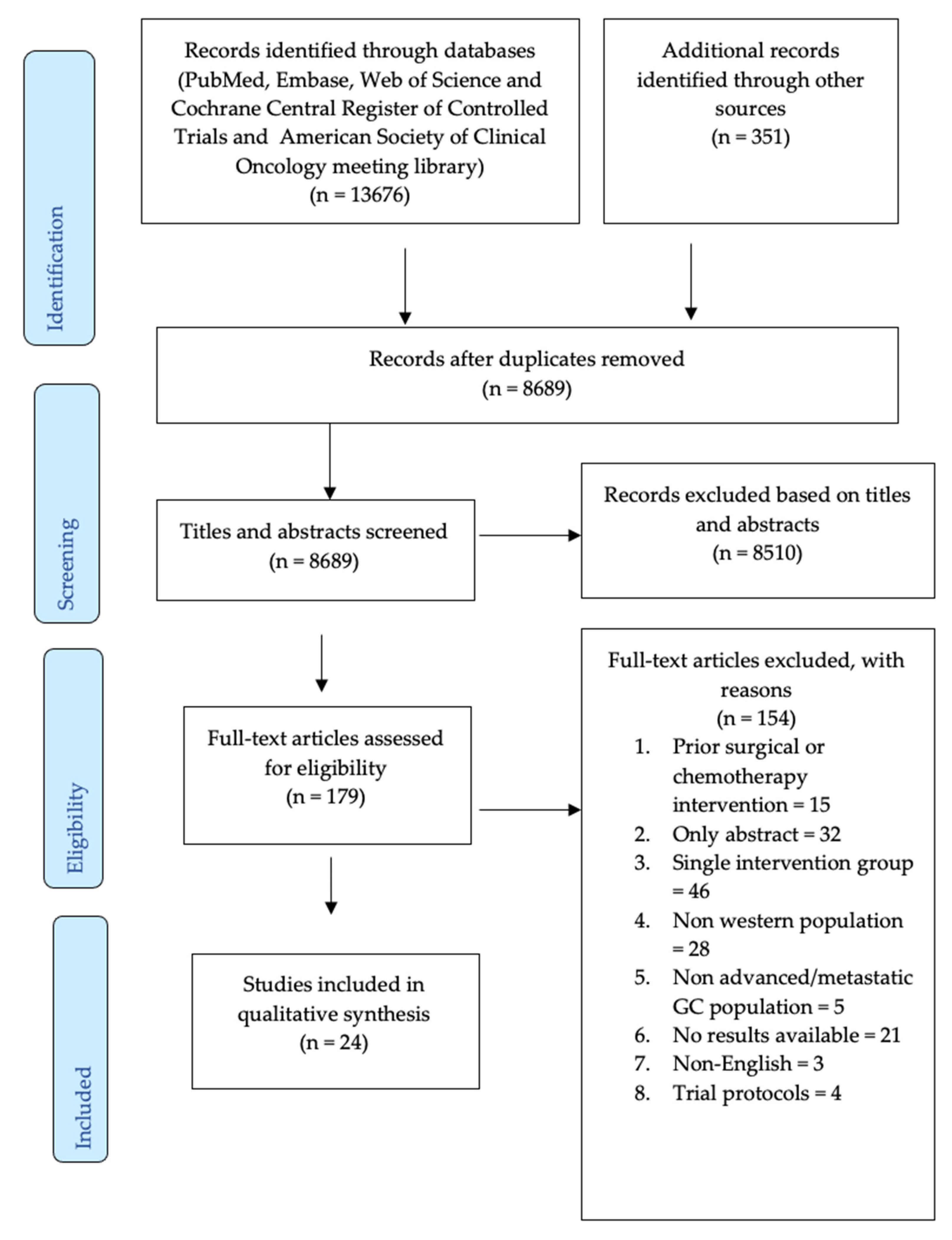
2.1. Characteristics of Included Studies
2.2. Overall survival
2.3. Progression-Free Survival
2.4. Objective response rate
2.5. Other Outcomes Reported
2.6. Adverse events and safety
2.7. Risk of bias assessment
3. Discussion
3.1. Overall survival
3.2. Progression-free survival
3.3. Objective response rate
3.4. Other outcomes
3.5. Limitations
3.6. Future research
4. Materials and Methods
4.1. Types of studies
4.2. Types of participants
4.3. Types of interventions
4.4. Types of outcome measures
4.5. Search strategy
4.6. Selection Criteria
4.7. Data extraction and management
4.8. Risk of bias assessment
4.9. Data synthesis
5. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
Appendix 1: Search Strategy for Systematic Review
-
Search: Clinical, economic, and/or humanistic outcomes of first-line systemic therapies in patients with unresectable locally advanced/metastatic gastric cancer- A Systematic ReviewCitation account (if any): EndnoteLimits: English LanguageType of publications: phase II and phase III randomized controlled trialsInclusions:P- Adults aged ≥ 18 years with stage II – IV gastric cancerI- First line systemic therapies as approved by NCCN 2022 guidelinesC- First-line systemic therapies and/or best supportive care/placeboO- Clinical: Overall survival, Progression-free survival, time to progression, objective response rate, Safety: Grade ≥3 treatment related adverse eventHumanistic: Quality of life, utility estimates, where availableExclusion: Non-English publications, observational, narrative reviews, systematic reviews, meta-analyses, and non-research publications will be excluded. Also, studies that focused exclusively on other line of therapy than first line systemic therapy. Other interventions such as radiotherapy, surgical and total neoadjuvant chemotherapy will be excluded.Limits: English language and trials conducted among western population or countries.Search Dates: Inception to May 2022PubMed((("Stomach"[Mesh] OR "stomach"[ALL] OR "Gastric"[ALL] OR "Esophagogastric"[ALL] OR "oesophagogas-tric"[ALL] OR "Gastroesophageal"[ALL] OR "gastrooesophageal"[ALL]) AND ("Neoplasms"[Mesh] OR "Carcino-ma"[Mesh] OR "Stomach Neoplasms"[Mesh] OR "Adenocarcinoma"[Mesh] OR "Cancer*"[ALL] OR "Neo-plasm*"[ALL] OR "Adenocarcinoma*"[ALL] OR "Carcinoma*"[ALL] OR "Tumor*"[ALL] OR "Neoplasm, Stom-ach"[ALL] OR "Stomach Neoplasm"[ALL] OR "Neoplasms, Stomach"[ALL] OR "Gastric Neoplasms"[ALL] OR "Gastric Neoplasm"[ALL] OR "Neoplasm, Gastric"[ALL] OR "Neoplasms, Gastric"[ALL] OR "Cancer of Stom-ach"[ALL] OR "Stomach Cancers"[ALL] OR "Gastric Cancer"[ALL] OR "Cancer, Gastric"[ALL] OR "Cancers, Gas-tric"[ALL] OR "Gastric Cancers"[ALL] OR "Stomach Cancer"[ALL] OR "Cancer, Stomach"[ALL] OR "Cancers, Stomach"[ALL]) AND ("Neoplasm Metastasis"[Mesh] OR "secondary" [Subheading] OR "Advanced"[ALL] OR "Metastatic"[ALL] OR "Metastasis"[ALL] OR "Recurrent"[ALL] OR "Unresectable"[ALL] OR "Inoperable"[ALL] OR "Incurable"[ALL] OR "Neoplasm metastasis"[ALL] OR "Secondary neoplasm*"[ALL] OR "Secondary cancer*"[ALL] OR "Secondary tumor*"[ALL] OR "Stage III"[ALL] OR "Stage IV"[ALL]) AND (("Controlled Clinical Trial" [Publi-cation Type] OR "Clinical Trials as Topic"[Mesh] OR "Clinical Trial" [Publication Type] OR "Randomized Controlled Trials as Topic"[Mesh] OR "Randomised"[ALL] OR "Randomized"[ALL] OR "Randomly"[ALL] OR "Random"[ALL] OR "Randomized controlled trial*"[ALL] OR "Controlled clinical trial*"[ALL] OR "Trial*"[ALL] OR "Clinical tri-al*"[ALL] OR "placebo"[ALL])) AND ("Drug Therapy"[Mesh] OR "Antineoplastic Agents"[Mesh] OR "Chemo-therapy, Adjuvant"[Mesh] OR "Combined Modality Therapy"[Mesh] OR "Antineoplastic Combined Chemotherapy Protocols"[Mesh] OR "Palliative Care"[Mesh] OR "Antineoplastic Agents"[ALL] OR "Drug therapy"[ALL] OR "Chemotherapy"[ALL] OR "Adjuvant chemotherapy"[ALL] OR "Antineoplastic combined chemotherapy"[ALL] OR "Palliative care"[ALL] OR "First-line therapy"[ALL] OR "first line"[ALL] OR "Supportive care"[ALL] OR "Antineoplastic Combined Chemotherapy Protocols"[ALL] OR "Systemic therapy"[ALL])EMBASE#1)'stomach'/exp OR stomach OR gastric OR Esophagogastric OR oesophagogastric OR Gastroesophageal OR gastrooesophageal#2) 'neoplasm'/exp OR 'carcinoma'/exp OR 'stomach tumor'/exp OR 'adenocarcinoma'/exp OR 'malignant neoplasm'/exp OR 'stomach cancer'/exp OR 'neoplasms' OR 'carcinoma' OR 'stomach neoplasms' OR 'adenocarcinoma' OR 'cancer*' OR 'neoplasm*' OR 'adenocarcinoma*' OR 'carcinoma*' OR 'tumor*' OR 'neoplasm, stomach' OR 'stomach neoplasm' OR 'neoplasms, stomach' OR 'gastric neoplasms' OR 'gastric neoplasm' OR 'neoplasm, gastric' OR 'neoplasms, gastric' OR 'cancer of stomach' OR 'stomach cancers' OR 'gastric cancer' OR 'cancer, gastric' OR 'cancers, gastric' OR 'gastric cancers' OR 'stomach cancer' OR 'cancer, stomach' OR 'cancers, stomach'#3) 'metastasis'/exp OR 'secondary'/exp OR 'advanced cancer'/exp OR 'inoperable cancer'/exp OR 'incurable cancer'/exp OR "Neoplasm Metastasis" OR "secondary" "Advanced" OR "Metastatic" OR "Metastasis" OR "Recurrent" OR "Unresectable" OR "Inoperable" OR "Incurable" OR "Neoplasm metastasis" OR "Secondary neoplasm*" OR "Secondary cancer*" OR "Secondary tumor*" OR "Stage III" OR "Stage IV"#4)'controlled clinical trial'/exp OR 'clinical trial'/exp OR 'randomized controlled trial'/exp OR 'trial'/exp OR 'placebo'/exp OR "Controlled Clinical Trial" OR "Clinical Trials as Topic" OR "Clinical Trial" OR "Randomized Controlled Trials as Topic" OR "Randomised" OR "Randomized" OR "Randomly" OR "Random" OR "Randomized controlled trial*" OR "Controlled clinical trial*" OR "Trial*" OR "Clinical trial*" OR "placebo"#5) 'drug therapy'/exp OR 'antineoplastic agent'/exp OR 'chemotherapy'/exp OR 'adjuvant chemotherapy'/exp OR 'multimodality cancer therapy'/exp OR 'palliative therapy'/exp OR 'chemotherapy'/exp OR 'first line therapy'/exp OR 'supportive care'/exp OR 'systemic therapy'/exp OR "Drug Therapy" OR "Antineoplastic Agents" OR "Chemotherapy, Adjuvant" OR "Combined Modality Therapy" OR "Antineoplastic Combined Chemotherapy Protocols" OR "Palliative Care" OR "Antineoplastic Agents" OR "Drug therapy" OR "Chemotherapy" OR "Adjuvant chemotherapy" OR "Antineoplastic combined chemotherapy" OR "Palliative care" OR "First-line therapy" OR "first line" OR "Supportive care" OR "Antineoplastic Combined Chemotherapy Protocols" OR "Systemic therapy"#1 AND #2 AND #3 AND #4 AND #5SCOPUS(TITLE-ABS-KEY (stomach OR gastric OR Esophagogastric OR gastrooesophageal)) AND (TITLE-ABS-KEY (neoplasm OR carcinoma OR tumor OR adenocarcinoma OR cancer )) AND (TITLE-ABS-KEY ( metastasis OR advanced OR {stage III} OR {stage IV})) AND (TITLE-ABS-KEY ({controlled clinical trial} OR {clinical trial} OR {randomized controlled trial} OR trial OR placebo )) AND (TITLE-ABS-KEY ({antineoplastic agent} OR chemotherapy OR {palliative therapy} OR {multimodality cancer therapy} OR {systemic therapy}))COCHRANE CENTRAL REGISTER OF CONTROLLED TRIALS( neoplasm OR carcinoma OR tumor OR adenocarcinoma OR cancer ) AND ( stomach OR gastric OR esophagogastric OR gastrooesophageal ) AND ( metastasis OR advanced OR "stage III" OR "stage IV" ) AND ( "controlled clinical trial" OR "clinical trial" OR "randomized controlled trial" OR trial OR placebo ) AND ( "antineoplastic agent" OR chemotherapy OR "palliative therapy" OR "multimodality cancer therapy" OR "systemic therapy" )CLINICAL TRIAL.GOV(Stomach cancer OR gastric cancer OR “stomach adenocarcinoma” OR “STOMACH CANCER, STAGE 3” OR “STOMACH CANCER, STAGE 4” OR “Gastroesophageal TUMOR” OR “Gastroesophageal CANCER” OR “Gastroesophageal NEOPLASM” OR “Esophageal Cancer”) AND (metastasis OR advanced OR "stage III" OR "stage IV" ) AND ( "antineoplastic agent" OR chemotherapy OR "palliative therapy" OR "multimodality cancer therapy" OR "systemic therapy" ) Filters: Phase 3 , 4ASCO MEETING LIBRARY(Keywords:advanced gastric cancer OR Keywords:metastatic gastric cancer) AND (Keywords:first line AND Keywords: systemic therapies)
References
- Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Stomach Cancer Statistics | Gastric Cancer Statistics. www.cancer.org. https://www.cancer.org/cancer/stomach-cancer/about/key-statistics.
- Hundahl SA, Phillips JL, Menck HR. The National Cancer Data Base report on poor survival of U.S. gastric carcinoma patients treated with gastrectomy. Cancer. 2000, 88, 921–932. 2000, 88, 921–932.
- Casamayor M, Morlock R, Maeda H, Anjani J. Targeted literature review of the global burden of gastric cancer. ecancermedicalscience. 2018;12. [CrossRef]
- NCCN Clinical Practice Guidelines in Oncology (NCCN Guidelines®). Nccn.org. Published January 11, 2022. https://www.nccn.org/professionals/physician_gls/pdf/gastric.pdf . 11 January.
- Gastric Cancer Treatment (PDQ®)–Health Professional Version - National Cancer Institute. www.cancer.gov. Published June 4, 2021. https://www.cancer.gov/types/stomach/hp/stomach-treatment-pdq#_81. 4 June.
- Genentech: News Features | Genentech Medicine Approved in Stomach Cancer. www.gene.com. Accessed September 29, 2021. https://www.gene.com/media/news-features/genentech-medicine-approved-in-stomach-cancer#:~:text=On%20October%2020%2C%202010%2C%20Herceptin. 29 September 2020.
- Lao Y, Shen D, Zhang W, He R, Jiang M. Immune Checkpoint Inhibitors in Cancer Therapy-How to Overcome Drug Resistance? Cancers. 2022, 14, 3575. [CrossRef]
- Rodrigues S, Figueiredo C. Recent insights into the use of immune checkpoint inhibitors in gastric cancer. Porto Biomedical Journal. 2022, 7, e162. [Google Scholar] [CrossRef]
- Chen C, Zhang F, Zhou N, et al. Efficacy and safety of immune checkpoint inhibitors in advanced gastric or gastroesophageal junction cancer: a systematic review and meta-analysis. OncoImmunology. 2019, 8, e1581547. [Google Scholar] [CrossRef]
- Kang YK, Boku N, Satoh T, et al. Nivolumab in patients with advanced gastric or gastro-oesophageal junction cancer refractory to, or intolerant of, at least two previous chemotherapy regimens (ONO-4538-12, ATTRACTION-2): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet. 2017, 390, 2461–2471. [Google Scholar] [CrossRef]
- Lorenzen S, Thuss-Patience PC, Riera Knorrenschild J, et al. FOLFOX versus FOLFOX plus nivolumab and ipilimumab administered in parallel or sequentially versus FLOT plus nivolumab administered in parallel in patients with previously untreated advanced or metastatic adenocarcinoma of the stomach or gastroesophageal junction: A randomized phase 2 trial of the AIO. Journal of Clinical Oncology. 2022, 40, 4043–4043. [Google Scholar] [CrossRef]
- Patrinely JR, Johnson R, Lawless AR, et al. Chronic Immune-Related Adverse Events Following Adjuvant Anti–PD-1 Therapy for High-risk Resected Melanoma. JAMA Oncology. 2021, 7, 744. [Google Scholar] [CrossRef]
- Ter Veer E, Haj Mohammad N, Van Valkenhoef G, et al. 2369 Efficacy and safety of first line chemotherapy in Advanced EsophagoGastric Cancer (AEGC): A network meta-analysis. European Journal of Cancer. 2015, 51, S459. [CrossRef]
- Guo X, Zhao F, Ma X, et al. A comparison between triplet and doublet chemotherapy in improving the survival of patients with advanced gastric cancer: a systematic review and meta-analysis. BMC Cancer. 2019, 19. [Google Scholar] [CrossRef]
- Zhu L, Liu J, MA S. Fluoropyrimidine-Based Chemotherapy as First-Line Treatment for Advanced Gastric Cancer: a Bayesian Network Meta-Analysis. Pathology & Oncology Research. 2016, 22, 853–861. [Google Scholar] [CrossRef]
- Song H, Zhu J, Lu D. Molecular-targeted first-line therapy for advanced gastric cancer. Cochrane Database of Systematic Reviews. Published online , 2016. 19 July. [CrossRef]
- Cheng J, Cai M, Shuai X, Gao J, Wang G, Tao K. First-line systemic therapy for advanced gastric cancer: a systematic review and network meta-analysis. Therapeutic Advances in Medical Oncology. 2019, 11, 1758835919877726. [Google Scholar] [CrossRef]
- Ajani JA, Fodor MB, Tjulandin SA, et al. Phase II Multi-Institutional Randomized Trial of Docetaxel Plus Cisplatin With or Without Fluorouracil in Patients With Untreated, Advanced Gastric, or Gastroesophageal Adenocarcinoma. Journal of Clinical Oncology. 2005, 23, 5660–5667. [Google Scholar] [CrossRef] [PubMed]
- Ajani JA, Moiseyenko VM, Tjulandin S, et al. Quality of Life With Docetaxel Plus Cisplatin and Fluorouracil Compared With Cisplatin and Fluorouracil From a Phase III Trial for Advanced Gastric or Gastroesophageal Adenocarcinoma: The V-325 Study Group. Journal of Clinical Oncology. 2007, 25, 3210–3216. [Google Scholar] [CrossRef] [PubMed]
- Ajani JA, Rodriguez W, Bodoky G, et al. Multicenter Phase III Comparison of Cisplatin/S-1 With Cisplatin/Infusional Fluorouracil in Advanced Gastric or Gastroesophageal Adenocarcinoma Study: The FLAGS Trial. Journal of Clinical Oncology. 2010, 28, 1547–1553. [Google Scholar] [CrossRef]
- Al-Batran SE, Hartmann JT, Probst S, et al. Phase III trial in metastatic gastroesophageal adenocarcinoma with fluorouracil, leucovorin plus either oxaliplatin or cisplatin: a study of the Arbeitsgemeinschaft Internistische Onkologie. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 2008, 26, 1435–1442. [Google Scholar] [CrossRef]
- Al-Batran SE, Pauligk C, Homann N, et al. The feasibility of triple-drug chemotherapy combination in older adult patients with oesophagogastric cancer: A randomised trial of the Arbeitsgemeinschaft Internistische Onkologie (FLOT65+). European Journal of Cancer. 2013, 49, 835–842. [Google Scholar] [CrossRef]
- Bouché O, Raoul JL, Bonnetain F, et al. Randomized Multicenter Phase II Trial of a Biweekly Regimen of Fluorouracil and Leucovorin (LV5FU2), LV5FU2 Plus Cisplatin, or LV5FU2 Plus Irinotecan in Patients With Previously Untreated Metastatic Gastric Cancer: A Fédération Francophone de Cancérologie Digestive Group Study—FFCD 9803. Journal of Clinical Oncology. 2004, 22, 4319–4328. [Google Scholar] [CrossRef]
- Cascinu S, Galizia E, Labianca R, et al. Pegylated liposomal doxorubicin, 5-fluorouracil and cisplatin versus mitomycin-C, 5-fluorouracil and cisplatin for advanced gastric cancer: a randomized phase II trial. Cancer Chemotherapy and Pharmacology. 2010, 68, 37–43. [Google Scholar] [CrossRef]
- Catenacci DVT, Tebbutt NC, Davidenko I, et al. Rilotumumab plus epirubicin, cisplatin, and capecitabine as first-line therapy in advanced MET-positive gastric or gastro-oesophageal junction cancer (RILOMET-1): a randomised, double-blind, placebo-controlled, phase 3 trial. The Lancet Oncology. 2017, 18, 1467–1482. [Google Scholar] [CrossRef] [PubMed]
- Cocconi G, Bella M, Zironi S, et al. Fluorouracil, doxorubicin, and mitomycin combination versus PELF chemotherapy in advanced gastric cancer: a prospective randomized trial of the Italian Oncology Group for Clinical Research. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 1994, 12, 2687–2693. [Google Scholar] [CrossRef] [PubMed]
- Coombes RC, Chilvers CED, Amadori D, et al. Randomised trial of epirubicin versus fluorouracil in advanced gastric cancer. Annals of Oncology. 1994, 5, 33–36. [Google Scholar] [CrossRef] [PubMed]
- Curran D, Pozzo C, Zaluski J, et al. Quality of life of palliative chemotherapy naive patients with advanced adenocarcinoma of the stomach or esophagogastric junction treated with irinotecan combined with 5-fluorouracil and folinic acid: results of a randomised phase III trial. Quality of Life Research: An International Journal of Quality of Life Aspects of Treatment, Care and Rehabilitation. 2009, 18, 853–861. [Google Scholar] [CrossRef]
- 30. Fuchs C, Shitara K, Di Bartolomeo M, et al. Ramucirumab as First-Line Therapy in Combination with Cisplatin and Fluoropyrimidine in Patients with Metastatic Gastric or Gastro-Oesophageal Junction Adenocarcinoma (RAINFALL): A Global, Randomised, Double-Blinded, Placebo-Controlled, Phase 3 Trial. SSRN Electronic Journal. Published online 2018. [CrossRef]
- Gubanski M, Johnsson A, Fernebro E, et al. Randomized phase II study of sequential docetaxel and irinotecan with 5-fluorouracil/folinic acid (leucovorin) in patients with advanced gastric cancer: the GATAC trial. Gastric Cancer: Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2010, 13, 155–161. [Google Scholar] [CrossRef]
- Högner A, Al-Batran SE, Siveke JT, et al. Pazopanib with 5-FU and oxaliplatin as first line therapy in advanced gastric cancer: A randomized phase-II study-The PaFLO trial. A study of the Arbeitsgemeinschaft Internistische Onkologie AIO-STO-0510. International Journal of Cancer. 2022, 150, 1007–1017. [CrossRef]
- Içli F, Celik I, Aykan F, et al. A randomized Phase III trial of etoposide, epirubicin, and cisplatin versus 5-fluorouracil, epirubicin, and cisplatin in the treatment of patients with advanced gastric carcinoma. Turkish Oncology Group. Cancer. 1998;83(12):2475-2480. Accessed May 4, 2023. https://pubmed.ncbi.nlm.nih.gov/9874451/.
- Janjigian YY, Shitara K, Moehler M, et al. First-line nivolumab plus chemotherapy versus chemotherapy alone for advanced gastric, gastro-oesophageal junction, and oesophageal adenocarcinoma (CheckMate 649): a randomised, open-label, phase 3 trial. The Lancet. 2021, 398, 27–40. [Google Scholar] [CrossRef]
- Kang YK ., Kang WK ., Shin DB ., et al. Capecitabine/cisplatin versus 5-fluorouracil/cisplatin as first-line therapy in patients with advanced gastric cancer: a randomised phase III noninferiority trial. Annals of Oncology. 2009, 20, 666–673. [CrossRef]
- Ochenduszko S, Puskulluoglu M, Konopka K, et al. Comparison of efficacy and safety of first-line palliative chemotherapy with EOX and mDCF regimens in patients with locally advanced inoperable or metastatic HER2-negative gastric or gastroesophageal junction adenocarcinoma: a randomized phase 3 trial. Medical Oncology. 2015, 32. [Google Scholar] [CrossRef]
- Petersen PC, Petersen LN, Vogelius I, Bjerregaard JK, Baeksgaard L. A randomized phase 2 trial of first-line docetaxel, carboplatin, capecitabine (CTX) and epirubicin, oxaliplatin, capecitabine (EOX) in advanced esophagogastric adenocarcinoma. Acta Oncologica (Stockholm, Sweden). 2021, 60, 948–953. [Google Scholar] [CrossRef] [PubMed]
- Roth AD, Fazio N, Stupp R, et al. Docetaxel, Cisplatin, and Fluorouracil; Docetaxel and Cisplatin; and Epirubicin, Cisplatin, and Fluorouracil As Systemic Treatment for Advanced Gastric Carcinoma: A Randomized Phase II Trial of the Swiss Group for Clinical Cancer Research. Journal of Clinical Oncology. 2007, 25, 3217–3223. [Google Scholar] [CrossRef] [PubMed]
- Shitara K, Van Cutsem E, Bang YJ, et al. Efficacy and Safety of Pembrolizumab or Pembrolizumab Plus Chemotherapy vs Chemotherapy Alone for Patients With First-line, Advanced Gastric Cancer: The KEYNOTE-062 Phase 3 Randomized Clinical Trial. JAMA oncology. 2020, 6, 1571–1580. [Google Scholar] [CrossRef] [PubMed]
- Shitara K, Doi T, Hosaka H, et al. Efficacy and safety of trifluridine/tipiracil in older and younger patients with metastatic gastric or gastroesophageal junction cancer: subgroup analysis of a randomized phase 3 study (TAGS). Gastric Cancer: Official Journal of the International Gastric Cancer Association and the Japanese Gastric Cancer Association. 2022, 25, 586–597. [Google Scholar] [CrossRef]
- Van Cutsem E, Moiseyenko VM, Tjulandin S, et al. Phase III Study of Docetaxel and Cisplatin Plus Fluorouracil Compared With Cisplatin and Fluorouracil As First-Line Therapy for Advanced Gastric Cancer: A Report of the V325 Study Group. Journal of Clinical Oncology. 2006, 24, 4991–4997. [Google Scholar] [CrossRef] [PubMed]
- Webb A, Cunningham D, Scarffe JH, et al. Randomized trial comparing epirubicin, cisplatin, and fluorouracil versus fluorouracil, doxorubicin, and methotrexate in advanced esophagogastric cancer. Journal of Clinical Oncology: Official Journal of the American Society of Clinical Oncology. 1997, 15, 261–267. [Google Scholar] [CrossRef] [PubMed]
- Sterne JAC, Savović J, Page MJ, et al. RoB 2: a revised tool for assessing risk of bias in randomised trials. BMJ 2019, l4898. [CrossRef]
- Cheng J, Cai M, Shuai X, Gao J, Wang G, Tao K. First-Line Systemic Therapy for Advanced Gastric Cancer: A Systematic Review and Network Meta-Analysis of 118 Randomized Controlled Trials. SSRN Electronic Journal. 2018. [CrossRef]
- Wagner AD, Grothe W, Haerting J, Kleber G, Grothey A, Fleig WE. Chemotherapy in Advanced Gastric Cancer: A Systematic Review and Meta-Analysis Based on Aggregate Data. Journal of Clinical Oncology. 2006, 24, 2903–2909. [Google Scholar] [CrossRef]
- CheckMate 649: Long-Term Data Support Nivolumab Plus Chemotherapy but Not Nivolumab Plus Ipilimumab in Gastric Cancer - The ASCO Post. ascopost.com. Published October 25, 2021. Accessed June 10, 2022. https://ascopost.com/issues/october-25-2021/checkmate-649-long-term-data-support-nivolumab-plus-chemotherapy-but-not-nivolumab-plus-ipilimumab-in-gastric-cancer/#:~:text=Objective%20response%20rates%20were%2060. 25 October.
- 47. Takashima A, Iizumi S, Boku N. Survival after failure of first-line chemotherapy in advanced gastric cancer patients: differences between Japan and the rest of the world. Japanese Journal of Clinical Oncology. 2017;47(7):583-589. [CrossRef]
- Koizumi W. Chemotherapy for advanced gastric cancer: review of global and Japanese status. Gastrointestinal cancer research : GCR. 2007;1(5):197-203. Accessed August 16, 2022. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC2632531.
- Elimova E, Wyrwicz L, Blum SI, et al. Health-related quality of life (HRQOL) in patients (pts) with advanced gastric cancer/gastroesophageal junction cancer (GC/GEJC) or esophageal adenocarcinoma (EAC): Results of nivolumab plus chemotherapy (NIVO+chemo) versus chemo from CheckMate 649. Journal of Clinical Oncology. 2021, 39(28_suppl):167-167. [CrossRef]
- van Amelsfoort RM, van der Sluis K, Schats W, et al. Health-Related Quality of Life in Locally Advanced Gastric Cancer: A Systematic Review. Cancers. 2021, 13, 5934. [Google Scholar] [CrossRef] [PubMed]
- Park R, Da Silva LL, Saeed A. Immunotherapy Predictive Molecular Markers in Advanced Gastroesophageal Cancer: MSI and Beyond. Cancers. 2021, 13, 1715. [Google Scholar] [CrossRef] [PubMed]
- Common Terminology Criteria for Adverse Events (CTCAE) Common Terminology Criteria for Adverse Events (CTCAE) V5.0.; 2017. https://ctep.cancer.gov/protocoldevelopment/electronic_applications/docs/CTCAE_v5_Quick_Reference_5x7.pdf.
| Author, year | Country | Phase | Study design | Total N | Treatment arms | Age Median (range) |
Males, n (%) |
|---|---|---|---|---|---|---|---|
| Ajani, 200519 | Multiple | II | Open label | 155 | Docetaxel-cisplatin | 57 (21-83) | 114 (74) |
| Docetaxel-cisplatin-fluorouracil | |||||||
| Ajani, 200720 |
Multiple | III | Open label | 445 | Docetaxel-cisplatin-fluorouracil | 55 (26-79) | (71.9) |
| Cisplatin-fluorouracil | 55 (25-76) | (70.5) | |||||
| Ajani, 201021 | Multiple | III | Open label | 1029 | Cisplatin-S1 | 59.0 (18,85)+ | 729 (70.8) |
| Cisplatin-fluorouracil | |||||||
| Al-Batran, 200822 | Germany + Switzerland |
III |
NR | 220 | Fluorouracil-leucovorin-oxaliplatin | 64 (33-86) | 64 (57) |
| Fluorouracil-leucovorin-cisplatin | 64 (27-85) | 81 (75) | |||||
| Al-Batran, 201323 | Germany | III | Open label | 143 | Fluorouracil-leucovorin-oxaliplatin-docetaxel | 69 | 51 (71) |
| Fluorouracil-leucovorin-oxaliplatin | 70 | 45 (63) | |||||
| Bouche, 200424 | France | III | Open label | 136 | Leucovorin–5-flurouracil | 64 (45-75) | (82) |
| Leucovorin–5-flurouracil–cisplatin | 64 (43-76) | (80) | |||||
| Leucovorin–5-flurouracil-irinotecan | 65 (37-76) | (84) | |||||
| Cascinu, 201025 | Italy | II | NR | 78 | 5-flurouracil-cisplatin-doxorubicin | 63 (33-75) | 50 (64) |
| 5-flurouracil-cisplatin-mitomycin | |||||||
| Catenacci, 201726 | Multiple | III | double-blind, placebo | 609 | Rilotumumab-epirubicin-cisplatin-capecitabine | 61 (28-84) | (67) |
| Placebo-epirubicin-cisplatin-capecitabine | 59 (26-81) | (72) | |||||
| Cocconi, 199427 |
Italy | III | NR | 130 | Cisplatin-epirubicin-leucovorin-flurouracil | 62 (28-74) | 60 (71) |
| Fluorouracil-doxorubicin-mitomycin | 65 (40-75) | 42 (81) | |||||
| Coombes, 199428 | United Kingdom | NR | NR | 69 | Epirubicin | 59.9 (9.3)* | 27 (7.5)* |
| Fluorouracil | 55.6 (9.2)* | 24 (7.3)* | |||||
| Curran, 200929 | Multiple | III | NR | 333 | Irinotecan-fluorouracil | NR | NR |
| Cisplatin-fluorouracil | |||||||
| Fuchs, 201930 | Multiple | III | double-blind, placebo | 645 | Ramucirumab-flurouracil-cisplatin | 60 (51-68) | 214 (66) |
| Placebo-flurouracil-cisplatin | 62 (54-68) | 215 (67) | |||||
| Gubanski, 201031 | Sweden | II | Crossover | 80 | Irinotecan-5-fluorouracil-leucovorin | 63 (39-79) | (67) |
| Docetaxel-leucovorin | 64 (42-75) | (87) | |||||
| Högner, 202132 | Germany | II | Open label | 87 | Pazopanib-5-fluorouracil-oxaliplatin | 65 | 37 (72) |
| Fluorouracil-leucovorin-oxaliplatin | 60 | 17 (63) | |||||
| Icli, 199833 | Turkey | III | NR | 131 | Etoposide-epirubicin-cisplatin | 52.7 (9.2)* | (68.8) |
| 5-fluorouracil-epirubicin-cisplatin | 52.7 (9.4)* | (59.7) | |||||
| Janjigian, 202134 | Multiple | III | Open label | 1581 | Nivolumab-capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 62 (54-69) | 540 (68) |
| Capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 61 (53-68) | 560 (71) | |||||
| Kang, 200935 | Multiple | III | Open label | 316 | Cisplatin-capecitabine | 56 (26-74) | 103 (64) |
| Cisplatin-fluorouracil | 56 (22-73) | 108 (69) | |||||
| Ochend- uszko, 201536 |
Poland | III | NR | 56 | Epirubicin-oxaliplatin-capecitabine | 57.9 (10.8) | 16 (55) |
| Docetaxel-cisplatin-5-fluorouracil-leucovorin | 60.3 (9.11) | 13 (48) | |||||
| Petersen, 202137 | Denmark | II | Open label | 110 | Docetaxel-carboplatin-capecitabine | 64 (36-79) | 79 (81) |
| Epirubicin-oxaliplatin-capecitabine | |||||||
| Roth, 200738 | Multiple | II | 3-arm | 119 | Epirubicin-cisplatin-flurouracil | 59 (32-71) | 75 |
| Docetaxel-cisplatin | 58 (40-70) | 76 | |||||
| Docetaxel-cisplatin-fluorouracil | 61 (35-78) | 61 | |||||
| Shitara, 202039 | Multiple | II | Open label | 763 | Pembrolizumab | 61 (20-83) | 180 (70.3) |
| Pembrolizumab-cisplatin-capecitabine-fluorouracil | 62 (22-83) | 195 (75.9) | |||||
| Placebo-cisplatin-capecitabine-fluorouracil | 62.5 (23-87) | 179 (71.6) | |||||
| Shitara, 202240 | Multiple | III | Open label | 813 | Nivolumab- ipilimumab |
62 (22‒84) | 278 (68) |
| Capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 61 (23‒90) | 280 (69) | |||||
| Van Cutsem, 200641 | Multiple | III | Open label | 457 | Docetaxel-cisplatin-fluorouracil Cisplatin-fluorouracil |
55 (25-79) | 317 (71) |
| Webb, 199742 | United Kingdom | II | Open label | 256 | Epirubicin-cisplatin-flurouracil | 59 (35-79) | 99 |
| Fluorouracil-doxorubicin-methotrexate | 60 (29-78) | 110 |
| Author, year | Tumor location-stomach gastric, n (%) | Disease stage, n (%) |
No. of organs involved in metastases,n (%) | ECOG status n (%) | Outcomes | |||
|---|---|---|---|---|---|---|---|---|
| Locally advanced | Metastatic | 1-2 | >2 | 0-1 | ≥2 | |||
| Ajani, 200519 | 106 (68) | 5 (3) |
147 (95) | 84 (61) | 61 (39) | 66 (43) | NR | Complete response, Objective response rate, Overall survival, partial response, Time to progression |
| Ajani, 200720 |
NR | 12 (3) | 430 (97) | (53.8) | (45.2) | 80 (36) | NR | Time to 5% deterioration of global health status from baseline |
| (54.9) | (44.6) | 81 (36) | NR | |||||
| Ajani, 201021 | 855 (83.1) | 43 (4.2) |
1085 (95.7) | NR | NR | 1029 (58.6) | NR | Overall survival, Progression-free survival, Response rate |
| Al-Batran, 200822 | 92 (82) | 3 (2.7) | 109 (97.3) | 59 (52.7) | 53 (47.4) | 103 (92) | 9 (8) | Overall survival, Progression-free survival, Response rate |
| 10 (9.3) | 98 (90.7) | 63 (58.3) | 45 (41.7) | 97 (90) | 11 (10) | |||
| Al-Batran, 201323 | 45 (63) | 22 (31) | 50 (69) | Median = 2 | 67 (93) | 5 (7) | Objective response rate | |
| 22 (32) | 49 (68) | 65 (92) | 6 (9) | |||||
| Bouche, 200424 | (71) | NR | NR | (80) | (20) | (73) | (27) | Overall survival, Progression-free survival, Response rate |
| (70) | (85) | (15) | (75) | (25) | ||||
| (67) | (83) | (17) | (78) | (22) | ||||
| Cascinu, 201125 | 69 (89) | 8 (10) | 70 (89) | NR | NR | 73 (93.7) | 5 (6.3) | Objective response rate, Overall survival, Time to progression |
| Catenacci, 201726 | 227 (75) | NR | 284 (93) | NR | NR | 304 (100) | 0 (0) | Duration of response, Overall survival, Progression-free survival, Time to progression |
| 195 (64) | NR | 283 (93) | 304 (100) | 1 (<1) | ||||
| Cocconi, 199427 |
NR | NR | NR | NR | NR | NR | 5 (6) | Duration of response, Objective response rate, Overall survival, Time to progression |
| NR | 5 (10) | |||||||
| Coombes, 199428 | NR | NR | NR | NR | NR | NR | NR | Overall survival |
| Curran, 200929 | NR | NR | NR | NR | NR | NR | NR | Quality of life, Time to progression |
| Fuchs, 201930 | 242 (74) | NR | NR | 243 (75) | 81 (25) | 326 (100) | NR | Objective response rate, Overall survival, Progression-free survival, Time to progression |
| 239 (75) | 242 (76) | 76 (24) | 319 (100) | NR | ||||
| Gubanski, 201031 | NR | NR | NR | NR | NR | (88) | (1) | Overall survival, Progression-free survival |
| NR | NR | NR | NR | NR | (99) | (18) | ||
| Högner, 202132 | 21 (41) | NR | NR | 15 (27) | 6 (71) | NR | NR | Objective response rate, Overall survival, Progression-free survival |
| 19 (70) | 13 (48) | 14 (51) | ||||||
| Icli, 199833 | NR | 17.2 | 82.8 | NR | NR | (65.6) | (34.4) | Objective response rate, Overall survival |
| 20.9 | 79.1 | (68.6) | (31.4) | |||||
| Janjigian, 202134 | 544 (70) | 27 (3) | 757 (96) | 164 (21) | 602 (76) | NR | NR | Overall survival, Progression-free survival |
| 556 (70) | 34 (4) | 756 (95) | 183 (23) | 583 (74) | ||||
| Kang, 200935 | NR | NR | NR | 127 (80) | 32 (20) | Median=1 (0-1) |
NR | Duration of response, Objective response rate, Overall survival, Progression-free survival |
| 126 (80) | 27 (20) | |||||||
| Ochend-uszko, 201536 | NR | 1 (4) | 28 (97) | 27 (91) | 2 (7) | 26 (89) | 3 (10) | Overall survival, Progression-free survival |
| 3 (11) | 24 (89) | 23 (85) | 4 (15) | 25 (93) | 2 (7) | |||
| Petersen, 202137 | 25 (26) | 10 (10) | 88 (89) | 54 (55) | 44 (45) | 98 (100) | NR | Overall survival, Progression-free survival |
| Roth, 200738 | NR | NR | (83) | (90) | (9) | NR | NR | Overall survival, Quality of life, Time to progression |
| (82) | (79) | (21) | ||||||
| (95) | (84) | (15) | ||||||
| Shitara, 202039 | 176 (68.8) | NR | NR | NR | NR | NR | NR | NR |
| 170 (66.1) | ||||||||
| 181 (72.4) | ||||||||
| Shitara, 202240 | 282 (69) | 14 (3) | 391 (96) | 83 (20) | 100 (25) | 409 (100) | NR | Duration of response, Overall survival, Progression-free survival, Quality of life |
| 282 (70) | 18 (4) | 386 (96) | 326 (80) | 304 (75) | 404 (100) | NR | ||
| Van Cutsem, 200641 | NR | 12 (3) | 43 (97) | 242 (54) | 200 (45) | 161 (36) | NR | Objective response rate, Overall survival, Time to progression |
| Webb, 199742 | 72 (57) | 47 (37) | 79 (63) | NR | NR | 96 (76) | 30 (24) | Objective response rate, Overall survival, Quality of life |
| 73 (56) | 51 (40) | 79 (60) | 97 (75) | 32 (25) | ||||
| Author, year | Treatment arms | n for each arm | Overall survival, months | Progression free survival, months | Objective response rate, % | Other outcomes | ||||
|---|---|---|---|---|---|---|---|---|---|---|
| Median | HR (95% CI); p | Median | HR (95% CI); p | Median | p value | Description | HR (95% CI); p | |||
| Ajani, 200519 | Docetaxel-cisplatin | 76 | 9.6 | 1.19 (0.83-1.69) | NR | NR | 26 | NR | Time to progression: 5.9 months | 0.80 (0.52-1.22) |
| Docetaxel-cisplatin-fluorouracil | 79 | 10.5 | NR | NR | 43 | Time to progression: 5 months | ||||
| Ajani, 200720 | Docetaxel-cisplatin-fluorouracil | 85 | NR | NR | NR | NR | NR | NR | Time to 5% deterioration of global health status from baseline: 6.5 months | 1.45 (1.08-1.93) p=0.01 |
| Cisplatin-fluorouracil | 104 | NR | NR | NR | NR | NR | NR | Time to 5% deterioration of global health status from baseline: 4.2 months | ||
| Ajani, 201021 | Cisplatin-S1 | 521 | 8.6 | 0.92 (0.80-1.05) 0.20 | 4.8 | 0.99 (0.86-1.14) | 29.0 |
NR |
Median duration of response: 6.5 months | 0.77 (0.57-1.03) |
| Cisplatin-fluorouracil | 508 | 7.9 | 5.5 | 32.0 | Median duration of response: 5.8 months | |||||
| Al-Batran, 200822 | Fluorouracil-leucovorin-oxaliplatin | 112 | 10.7 (8.5-13.9) | p=0.51 | 5.8 (4.5-6.6) | NR | 34.8 | NR |
NR | NR |
| Fluorouracil-leucovorin-cisplatin | 102 | 8.8 (7.7-12.0) | 3.9 (3.1-4.8) | 24.50 | NR | NR | ||||
| Al-Batran, 201323 | Fluorouracil-leucovorin-oxaliplatin-docetaxel | 72 | NR | NR | NR | NR | 48.6 (36.7-60.7) | p=0.02 | Quality of life global health status scores at 0, 8, 16 and 24 weeks: 56.5 ± 24.4, 53.6 ± 19.9,56.8 ± 19.5 and 53.7 ± 22.8 | No significant differences between arms |
| Fluorouracil-leucovorin-oxaliplatin | 71 | NR | NR | NR | NR | 28.2 (18.1-40.1) | Quality of life global health status scores at 0, 8, 16 and 24 weeks: 49.4 ± 24.7,58.2 ± 19.8, 53.3 ± 21.0 and 55.5 ± 16.9 | |||
| Bouche, 200424 | Leucovorin–5-flurouracil | 45 | 6.8 (2.6-11.1) | NR | 3.2 (1.8-4.6) | NR | 13 (3.4-23.3) | NR |
Mean difference in global quality of life scores between Leucovorin–5-flurouracil vs Leucovorin–5-flurouracil-irinotecan = 2.2.Mean difference in global quality of life scores between Leucovorin–5-flurouracil–cisplatin vs Leucovorin–5-flurouracil-irinotecan = 0.8 | Treatment effect: 0.89; p<0.01 |
| Leucovorin–5-flurouracil–cisplatin | 44 | 9.5 (6.9-12.2) | NR | 4.9 (3.5-6.3) | 27 (14.1-40.4) | |||||
| Leucovorin–5-flurouracil-irinotecan | 45 | 11.3 (9.3-13.3) | NR | 6.9 (5.5-8.3) | 40 (25.7-54.3) | |||||
| Cascinu, 201125 | 5-flurouracil-cisplatin-doxorubicin | 39 | 12.1 | 0.63 (0.34-0.91) p=0.02 | NR | NR | 64.1 (48-77) | p=0.04 | Time to progression: 7.9 month | 0.62, (0.37-0.97) p=0.04 |
| 5-flurouracil-cisplatin-mitomycin | 39 | 8.3 | NR | NR | 39 (24-54) | Time to progression: 5.1 months | ||||
| Catenacci, 201726 | Rilotumumab-epirubicin-cisplatin-capecitabine | 298 | 8·8 (7·7–10·2) | 1·34 (1·10–1·63) p<0·01) | 5·6 (5·3–5·9) | 1·26 (1·04–1·51) | 29·8 (24·3–35·7) | NR | Time to progression: 6·1 month (95% CI=5·7–7·9) Duration of response: 2·8 months (IQR=2·7–2·9) |
1·24 (0·96–1·59) p=0·10 |
| Placebo-epirubicin-cisplatin-capecitabine | 299 | 10·7 (9·6–12·4) | 6·0 (5·7–7·2) | 44·6 (38·5–50·8) | Time to progression: 7·1 month (5·9–7·9)Duration of response: 2·8 months (2·6–2·9) | |||||
| Cocconi, 199427 | Cisplatin-epirubicin-leucovorin-flurouracil | 85 | 8.1 (0.2-33.5) | p=0.24 | NR | NR | 43 | P<0.01 | Time to progression: 4.7 month (0.2-26.5) | p=0.58 |
| Fluorouracil-doxorubicin-mitomycin | 52 | 5.6 (0.5-49.1) | NR | NR | 15 | 2.6 month (0.5-33.2) | ||||
| Coombes, 199428 | Epirubicin | 36 | 88.2% died | p=0.65 | NR | NR | NR | NR | NR | NR |
| Fluorouracil | 33 | 3.9% died | NR | NR | NR | NR | NR | NR | ||
| Curran, 200929 | Irinotecan-fluorouracil | 172 | NR | NR | NR | NR | NR | NR | Time to progression: 5 month; Global health status mean 62.4 (20.1) | p=0.088; p=0.061 |
| Cisplatin-fluorouracil | 165 | NR | NR | NR | NR | NR | NR | Time to progression: 4.2 months; Global health status mean- 56.9 (21.1) | ||
| Fuchs, 201930 | Ramucirumab-flurouracil-cisplatin | 326 | 11·2 (9·9–11·9) |
0·96 (0·80–1·16) p=0·67 | 5·7 (5·5–6·5) | 0.75, (0.61–0.94) p=0.01 | 41.1 (35.8-46.4) | p=0.17 | Time to progression: 6.8 month(5.9-7.7) | p=0.70 (0.57-0.86) |
| Placebo-flurouracil-cisplatin | 319 | 10·7 (9·5–11·9) | 5·4 (4·5–5·7) |
36.4 (31.1-41.6) | Time to progression: 5.8 months (5.6-6.4) | |||||
| Gubanski, 201031 | Irinotecan-5-fluorouracil-leucovorin | 39 | 11.5 | p=0.3 | 4.9 | NR | NR | NR | NR | NR |
| Docetaxel-leucovorin | 39 | 10.6 | 5.0 | NR | NR | NR | NR | |||
| Högner, 202232 | Pazopanib-5-fluorouracil-oxaliplatin | 51 | 10.2 (5.5-14.9) | 1.01 (0.62-1.65)p=0.95 | 4.7 (2.9-6.5) | 0.96 (0.60-1.55) p=0.88 |
25 | NR | NR | NR |
| Fluorouracil-leucovorin-oxaliplatin | 27 | 7.3 (4.9-9.7) | 4.5 (1.8-7.1) | 26 | NR | NR | ||||
| Icli, 199833 | Etoposide-epirubicin-cisplatin | 64 | 6.0 | p>0.05 | NR | NR | 20.30 | p=0.63 | NR | NR |
| 5-fluorouracil-epirubicin-cisplatin | 67 | 5.0 | NR | NR | 15.30 | NR | NR | |||
| Janjigian, 202134 | Nivolumab-capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 789 | 13·1 (6·7–19·1) | 0·71 (0·59–0·86) p<0·01 | 7·7 (7·0–9·2) | 0·68 (0·56–0·81) p<0·01 | NR | NR | NR | NR |
| Capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 792 | 11·1 (5·8–16·1) | 6·1 (5·6–6·9) | NR | NR | NR | NR | |||
| Kang, 200935 | Cisplatin-capecitabine | 160 | 10.4 (9.1–11.0) | 0.85, (0.65–1.11) | 5.6 (4.9–7.3) | 0.81, (0.63–1.04) p<0.01 | 46 (38-55) | 1.80 (1.11–2.94) p=0.02 | Mean duration of response:7.6 months | 0.88 (0.56–1.36) p=0.55 |
| Cisplatin-fluorouracil | 156 | 8.9 (7.3–10.2) | 5.0 (4.2–6.3) | 32 (24-41) | Mean duration of response: 6.2 months | |||||
| Ochenduszko, 201536 | Epirubicin-oxaliplatin-capecitabine | 29 | 9.5 | p=0.14 | 6.4 | p=0.44 | NR | NR | NR | NR |
| Docetaxel-cisplatin-5-fluorouracil-leucovorin | 27 | 11.9 | 6.8 | NR | NR | NR | NR | |||
| Petersen, 202137 | Docetaxel-carboplatin-capecitabine | 49 | 9.8 (8.2-11.0) | NR | 6.1 (5.5-7.1) | NR | NR | NR | NR | NR |
| Epirubicin-oxaliplatin-capecitabine | 49 | 10.2 (8.0-11.9) | NR | 5.1 (4.3-7.0) | NR | NR | NR | NR | ||
| Roth, 200738 | Epirubicin-cisplatin-flurouracil | 40 | 8.3 (7.2-13.0) | NR | NR | NR | NR | NR | Time to progression: 4.9 (3.2-6.1) months | NR |
| Docetaxel-cisplatin | 38 | 11 (7.8-12.5) | NR | NR | NR | NR | NR | Time to progression: 3.6 (2.8-4.5) months | ||
| Docetaxel-cisplatin-fluorouracil | 41 | 10.4 (8.3-12.0) | NR | NR | NR | NR | NR | Time to progression: 4.6 (3.5-5.6) months | ||
| Shitara, 202039 | Pembrolizumab | 256 | 10.6 (7.7-13.8) |
0.91 (0.69-1.18) 0.85 (0.70-1.03) |
2.0 (1.5-2.8) |
1.66 (1.37-2.01) 0.84 (0.70-1.02) p=0.04 |
NR | NR | NR | NR |
| Pembrolizumab-cisplatin-capecitabine-fluorouracil | 257 | 12.5 (10.8-13.9) | 6.9 (5.7-7.3) | NR | NR | NR | NR | |||
| Placebo-cisplatin-capecitabine-fluorouracil | 250 | 11.1 (9.2-12.8) | 6.4 (5.7-7.0) | NR | NR | NR | NR | |||
| Shitara, 202240 | Nivolumab- ipilimumab |
409 | 11.2 (9.2-13.4) | 0.89 (0.71-1.10) p=0.23 | 2.8 (2.6-3.6) | 1.66 (1.40-1.95) | NR | NR | Duration of response: 13.8 months (9.4-17.7) | NR |
| Capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 404 | 11.6 (10.1-12.7) | 7.1 (6.9-8.2) | NR | NR | Duration of response: 6.8 months (5.6-7.2) | NR | |||
| Van Cutsem, 200641 | Docetaxel-cisplatin-fluorouracil | 221 | 9.2 (8.4-10.6) | 1.29 (1.0-1.6) p=0.02 | NR | NR | 81 (37) | p=0.01 | Time to progression: 5.6 (4.9-5.9) months | 1.47 (1.19-1.82) |
| Cisplatin-fluorouracil | 224 | 8.6 (7.2-9.5) | NR | NR | 57 (25) | Time to progression: 3.7 (3.4-4.5) months | ||||
| Webb, 199742 | Epirubicin-cisplatin-flurouracil | 111 | 8.9 | NR | NR | NR | 45 (36-54) | p<0.01 | NR | NR |
| Fluorouracil-doxorubicin-methotrexate | 108 | 5.7 | NR | NR | NR | 21 (13-29) | NR | NR | ||
| Author, year | Sample size | Treatment arms | Neutropenia, n (%) | Anemia, n (%) | Thrombocytopenia, n (%) | Leukopenia, n (%) | Nausea, n (%) | Vomiting, n (%) | Diarrhea, n (%) | Fatigue, n (%) |
|---|---|---|---|---|---|---|---|---|---|---|
| Ajani, 200519 | 76 | Docetaxel-cisplatin-fluorouracil | 65 (87) | 24 (32) | 1 (1) | 49 (65) | 8 (11) | NR | 4 (5) | NR |
| 79 | Docetaxel-cisplatin | 66 (86) | 22 (29) | 9 (12) | 53 (69) | 16 (20) | NR | 16 (20) | NR | |
| Ajani, 201021 | 521 | Cisplatin-S1 | 167 (32) | 107 (21) | 43 (8) | 71 (14) | 39 (8) | 41 (8) | NR | 64 (12) |
| 508 | Cisplatin-fluorouracil | 320 (64) | 105 (21) | 68 (14) | 167 (3) | 49 (10) | 49 (10) | NR | 67 (13) | |
| Al-Batran, 200822 | 112 | Fluorouracil-leucovorin-oxaliplatin | 13 (12) | 3 (3) | 4.5 (4) | 7 (6) | 5 (5) | 3 (3) | 7 (6) | 4 (4) |
| 102 | Fluorouracil-leucovorin-cisplatin | 15 (15) | 7 (7) | 4 (4) | 12 (12) | 9 (9) | 6 (6) | 5 (5) | 7 (7) | |
| Al-Batran, 201323 | 72 | Fluorouracil-leucovorin-oxaliplatin-docetaxel | 38 (53) | 8 (11) | 2 (3) | 21 (29) | 15 (21) | 3 (4) | 6 (8) | 8 (11) |
| 71 | Fluorouracil-leucovorin-oxaliplatin | 9 (13) | 3 (4) | 2 (3) | 4 (6) | 5 (7) | 1 (2) | 1 (2) | 5 (7) | |
| Bouche, 200424 | 45 | Leucovorin–5-flurouracil | (11) | (16) | (2) | NR | (18) | NR | (2) | NR |
| 44 | Leucovorin–5-flurouracil-cisplatin | (61) | (30) | (2) | NR | (23) | NR | (2) | NR | |
| 45 | Leucovorin–5-flurouracil-irinotecan | (40) | (16) | (0) | NR | (9) | NR | (22) | NR | |
| Cascinu, 201125 | 39 | 5-flurouracil-cisplatin-doxorubicin | 6 (15) | 0 (0) | 2 (5) | NR | 1 (3) | NR | 0 (0) | NR |
| 39 | 5-flurouracil-cisplatin-mitomycin-C | 10 (26) | 0 (0) | 8 (21) | NR | 1 (3) | NR | 1 (3) | NR | |
| Catenacci, 201726 | 298 | Rilotumumab-epirubicin- cisplatin-capecitabine | 111 (37) | 97 (33) | NR | NR | 128 (43) | 100 (34) | 61 (20) | 103 (35) |
| 299 | Placebo-epirubicin-cisplatin-capecitabine | 126 (42) | 125 (42) | NR | NR | 153 (51) | 98 (33) | 81 (27) | 100 (33) | |
| Cocconi, 199427 | 85 | Cisplatin-epirubicin-leucovorin-flurouracil | 8 (9) | 1 (1) | 4 | NR | 17 | 10 (37) | 3 (11) | NR |
| 52 | Fluorouracil-doxorubicin-mitomycin | 0 (0) | 1 (2) | 0 | NR | 4 | 2 (8) | 2 (8) | NR | |
| Curran, 200929 | 172 | Irinotecan-fluorouracil | (24.8) | NR | (2) | NR | NR | NR | (22) | NR |
| 165 | Cisplatin-fluorouracil | (51.6) | NR | (12) | NR | NR | NR | (7) | NR | |
| Fuchs, 201930 | 326 | Ramucirumab-fluorouracil-cisplatin | 85 (26) | 39 (12) | 25 (8) | NR | 22 (7) | 21 (7) | 15 (5) | 27 (8) |
| 319 | Placebo-fluorouracil-cisplatin | 85 (27) | 44 (14) | 11 (4) | NR | 26 (8) | 31 (10) | 23 (7) | 25 (9) | |
| Gubanski,201031 | 39 | Irinotecan-5-fluorouracil-leucovorin | NR | NR | NR | NR | (4) | NR | (5) | (9) |
| 39 | Docetaxel-leucovorin | NR | NR | NR | NR | (12) | NR | (2) | (3) | |
| Högner, 202232 | 51 | Pazopanib-5-fluorouracil-oxaliplatin | 12 (24) | 1 (2) | 1 (2) | 3 (6) | 8 (16) | 3 (6) | 1 (2) | 4 (8) |
| 27 | Fluorouracil-leucovorin-oxaliplatin | 1 (4) | 3 (11) | 3 (11) | NR | NR | 2 (7) | 2 (7) | 1 (4) | |
| Icli, 199833 | 64 | Etoposide-epirubicin-cisplatin | NR | NR | NR | NR | (6.3) | NR | (1.6) | NR |
| 67 | 5-fluorouracil-epirubicin-cisplatin | NR | NR | NR | NR | (9) | NR | (1.5) | NR | |
| Janjigian, 202134 | 789 | Nivolumab-capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 31 (4) | 3 (<1) | 4 (1) | NR | 0 (0) | 2 (<1) | 2 (<1) | 0 (0) |
| 792 | Capecitabine-oxaliplatin or leucovorin-fluorouracil-oxaliplatin | 23 (3) | 1 (<1) | 1 (1) | NR | 0 (0) | 0 (0) | 0 (0) | 19 (1) | |
| Kang, 200935 | 160 | Cisplatin-capecitabine | 25 (16) | NR | NR | 4 (3) | 3 (2) | 11 (7) | 8 (5) | 1 (<1) |
| 156 | Cisplatin- fluorouracil | 29 (19) | NR | NR | 6 (4) | 4 (3) | 13 (8) | 7 (5) | 4 (<3) | |
| Ochenduszko, 201536 | 29 | Epirubicin-oxaliplatin-capecitabine | 21 (72) | 2 (7) | 0 (0) | 2 (7) | 1 (4) | 0 (0) | 1 (4) | 2 (7) |
| 26 | Docetaxel-cisplatin-5-fluorouracil-leucovorin | 13 (50) | 2 (7) | 0 (0) | 3 (12) | 10 (29) | 0 (0) | 1 (4) | 1 (4) | |
| Petersen, 202137 | 49 | Docetaxel-carboplatin-capecitabine | 42 (82) | 3 (6) | NR | NR | 0 (0) | NR | 4 (8) | 3 (6) |
| 49 | Epirubicin-oxaliplatin-capecitabine | 42 (82) | 3 (6) | NR | NR | 0 (0) | NR | 4 (8) | 3 (6) | |
| Roth, 200738 | 40 | Epirubicin-cisplatin-flurouracil | (59) | NR | (3) | NR | NR | NR | (6) | NR |
| 38 | Docetaxel-cisplatin | (76) | NR | (0) | NR | NR | NR | (3) | NR | |
| 41 | Docetaxel-cisplatin-flurouracil | (80) | NR | (3) | NR | NR | NR | (15) | NR | |
| Shitara, 202039 | 254 | Pembrolizumab | 0 (0) | NR | 0 (0) | 0 (0) | 1 (0.4) | 0(0) | 1 (1) | 1 (0) |
| 250 | Pembrolizumab-cisplatin-capecitabine-fluorouracil | 63 (25) | NR | 7 (3) | 7 (3) | 19 (8) | 12(5) | 12 (5) | 19 (8) | |
| 244 | Placebo-cisplatin-capecitabine-fluorouracil | 68 (28) | NR | 6 (3) | 10 (4) | 18 (7) | 14(6) | 14 (6) | 14 (6) | |
| Shitara, 202240 | 403 | Nivolumab-ipilimumab | 1 (<1) | 5 (1) | 1 (<1) | 0 (0) | 6 (1) | 4(1) | 11 (3) | 11 (3) |
| 389 | Capecitabine-oxaliplatin or Leucovorin-fluorouracil-oxaliplatin | 44 (11) | 9 (2) | 7 (2) | 9 (2) | 16 (4) | 11(3) | 15 (4) | 8 (2) | |
| Van Cutsem, 200641 | 221 | Docetaxel-cisplatin-fluorouracil | 181 (82) | 40 (18) | 17 (8) | 144 (65) | 32 (14) | NR | 43 (19) | NR |
| 224 | Cisplatin- fluorouracil | 126 (57) | 57 (26) | 30 (13) | 70 (31) | 38 (17) | NR | 18 (8) | NR | |
| Webb, 199742 | 126 | Epirubicin-cisplatin-flurouracil | NR | (8) | (4) | (36) | (17) | NR | (6) | NR |
| 130 | Fluorouracil-doxorubicin-methotrexate | NR | (10) | (8) | (39) | (5) | NR | (7) | NR |
| Author, Year | Randomization | Deviations from intended intervention | Missing outcome data | Measurement of outcome | Selection of reported results | Overall |
|---|---|---|---|---|---|---|
| Ajani, 200519 | Low | Some | Some | Low | Low | Some |
| Ajani, 200720 | Low | Low | Some | Low | Low | Some |
| Ajani, 201021 | Low | Low | Some | Low | Low | Some |
| Al-Batran, 200822 | Some | Some | Low | Low | Low | Some |
| Al-Batran, 201323 | Low | Low | Low | Low | Low | Low |
| Bouche, 200424 | Low | Low | Low | Low | Low | Low |
| Cascinu, 201125 | Low | Low | Low | Low | Low | Low |
| Catenacci, 201726 | Low | Low | Low | Low | Low | Low |
| Cocconi, 199427 | Low | Low | Some | Low | Low | Some |
| Coombes, 199428 | Some | Low | Low | Low | Low | Some |
| Deng, 201329 | Low | Low | Low | Low | Low | Low |
| Fuchs, 201930 | Low | Low | Some | Low | Low | Some |
| Gubanski, 201031 | Low | Low | Low | Low | Low | Low |
| Högner, 202232 | Low | Low | Low | Low | Low | Low |
| Icli, 199833 | Low | Low | Some | Low | Low | Some |
| Janjigian, 202134 | Low | Low | Low | Low | Low | Low |
| Kang, 200935 | Low | Some | Some | Low | Low | Some |
| Ochenduszko, 201536 | Low | Low | Low | Low | Low | Low |
| Petersen, 202137 | Low | Some | Some | Low | Low | Some |
| Roth, 200738 | Some | Some | Low | Low | Low | Some |
| Shitara, 202039 | Low | Low | Low | Low | Low | Low |
| Shitara, 202240 | Low | Low | Low | Low | Low | Low |
| Van Cutsem, 200641 | Low | Low | Some | Low | Low | Some |
| Webb, 199742 | Some | Low | Low | Low | Some | Some |
| ("Stomach"[Mesh] OR "stomach"[ALL] OR "Gastric"[ALL] OR "Esophagogastric"[ALL] OR "oesophagogastric"[ALL] OR "Gastroesophageal"[ALL] OR "gastrooesophageal"[ALL]) AND ("Neoplasms"[Mesh] OR "Carcinoma"[Mesh] OR "Stomach Neoplasms"[Mesh] OR "Adenocarcinoma"[Mesh] OR "Cancer*"[ALL] OR "Neoplasm*"[ALL] OR "Adenocarcinoma*"[ALL] OR "Carcinoma*"[ALL] OR "Tumor*"[ALL] OR "Neoplasm, Stomach"[ALL] OR "Stomach Neoplasm"[ALL] OR "Neoplasms, Stomach"[ALL] OR "Gastric Neoplasms"[ALL] OR "Gastric Neoplasm"[ALL] OR "Neoplasm, Gastric"[ALL] OR "Neoplasms, Gastric"[ALL] OR "Cancer of Stomach"[ALL] OR "Stomach Cancers"[ALL] OR "Gastric Cancer"[ALL] OR "Cancer, Gastric"[ALL] OR "Cancers, Gastric"[ALL] OR "Gastric Cancers"[ALL] OR "Stomach Cancer"[ALL] OR "Cancer, Stomach"[ALL] OR "Cancers, Stomach"[ALL]) AND ("Neoplasm Metastasis"[Mesh] OR "secondary" [Subheading] OR "Advanced"[ALL] OR "Metastatic"[ALL] OR "Metastasis"[ALL] OR "Recurrent"[ALL] OR "Unresectable"[ALL] OR "Inoperable"[ALL] OR "Incurable"[ALL] OR "Neoplasm metastasis"[ALL] OR "Secondary neoplasm*"[ALL] OR "Secondary cancer*"[ALL] OR "Secondary tumor*"[ALL] OR "Stage III"[ALL] OR "Stage IV"[ALL]) AND (("Controlled Clinical Trial" [Publication Type] OR "Clinical Trials as Topic"[Mesh] OR "Clinical Trial" [Publication Type] OR "Randomized Controlled Trials as Topic"[Mesh] OR "Randomised"[ALL] OR "Randomized"[ALL] OR "Randomly"[ALL] OR "Random"[ALL] OR "Randomized controlled trial*"[ALL] OR "Controlled clinical trial*"[ALL] OR "Trial*"[ALL] OR "Clinical trial*"[ALL] OR "placebo"[ALL])) AND ("Drug Therapy"[Mesh] OR "Antineoplastic Agents"[Mesh] OR "Chemotherapy, Adjuvant"[Mesh] OR "Combined Modality Therapy"[Mesh] OR "Antineoplastic Combined Chemotherapy Protocols"[Mesh] OR "Palliative Care"[Mesh] OR "Antineoplastic Agents"[ALL] OR "Drug therapy"[ALL] OR "Chemotherapy"[ALL] OR "Adjuvant chemotherapy"[ALL] OR "Antineoplastic combined chemotherapy"[ALL] OR "Palliative care"[ALL] OR "First-line therapy"[ALL] OR "first line"[ALL] OR "Supportive care"[ALL] OR "Antineoplastic Combined Chemotherapy Protocols"[ALL] OR "Systemic therapy"[ALL]) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





