1. Introduction
Though regular exercise training is considered an important health-promoting and disease-preventive measure, strenuous long-lasting exercise may lead to unfavorable changes, including heart rate (HR) disturbances [
1]. Many cardiologists are of the opinion that extreme endurance exercise performed by professional and even ambitious leisure-time athletes could be dangerous [
2] and even provoke sudden cardiac death [
3]. Wearable HR monitors (HRMs) are increasingly used by professional and leisure-time athletes, as well as by cardiac patients, to monitor HR during exercise. A HRM may notify the user if it detects abnormal HR; thus, it potentially protects against dangerous incidents [
4,
5]. On the other hand, they may also sometimes provide false information, suggesting serious heart rhythm disturbances during exercise even in healthy, asymptomatic individuals [
6]. Diagnosis is in some cases very difficult, as is illustrated by the present case concerning a professional marathon-runner.
2. Materials and Methods
Subject characteristics and health history
A 36-year-old marathon runner (height, 1.73 m; weight, 66 kg; body mass index, 21.72 kg/m2) came to the Center for Sports Cardiology (CSC) in Pułtusk, Poland, seeking a diagnosis for his cardiac problems. The athlete has had an active life since childhood, has been running regularly for 20 years, and has run approximately 90,000-100,000 km in his lifetime. As part of his daily training over the past year, he has run an average of 20 km/day. During his 20-year sports career he has successfully competed many times in Polish, European, and World Championships, very often winning medals in long-distance running, marathons, and ultramarathons (both cross-country, mountain, and street running). An extensive sports biography and the athlete’s personal records can be found on the official website of the Polish Athletics Association and in
Table S1 (
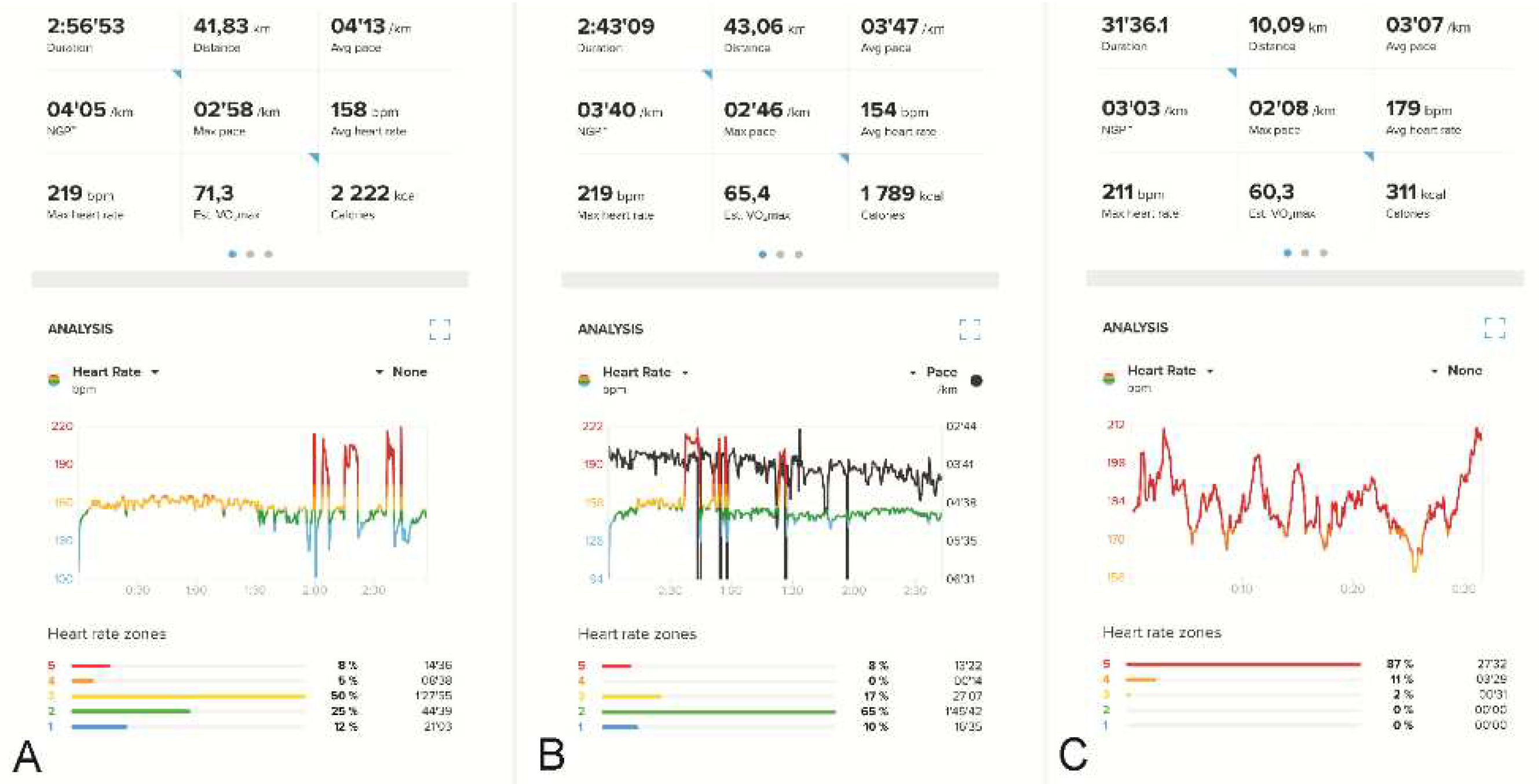
Supplementary Materials). Before 2019, the athlete had never experienced any noticeable arrhythmia. He had used HRMs for many years, with no unexpected HR spikes either when training or competing. As a junior in 2004 and 2005, however, he fainted twice while competing. Then, in 2019, during an intense training run in Kyrgyzstan (1,700 meters above sea level), his HRM recorded a tachyarrhythmic seizure for the first time, with his HR suddenly increasing to over 200 bpm. This tachyarrhythmia made it impossible to continue training but subsided after about 30 seconds. While in Kyrgyzstan, he suffered severe pneumonia, confirmed radiologically after the end of the sports camp. Afterwards, he continued experiencing instances of tachyarrhythmia, almost exclusively during competitions. Each time, the athlete felt a sensation of irregular heartbeat and observed an increase in his HR on his HRM. The arrhythmia generally occurred in the last phase of extreme effort (e.g., at the 30th km of a marathon), when the running pace was around 3:15-3:20 min/km and the HR around 172–175 bpm. A high temperature, rough route, or jerky pace increased the likelihood of arrhythmia. Subsequently, it happened also at lower HR values (
Figure 1A,B).
Apart from the documented HRM data, this cardiac arrhythmia was otherwise confirmed only once, by ambulance nurses (but without an electrocardiogram [ECG]) who were called in after the athlete fainted at the 32nd km of the Polish Marathon Championship in 2021 (verbal information). He was afterwards intensively tested in reference cardiology centers, including countless ECGs, numerous stress-tests, echocardiography, cardiac magnetic resonance imaging (MRI) and, eventually, an electrophysiology study. The test results were considered borderline for an athlete’s heart, thus precluding a diagnosis of heart disease. Numerous attempts were made to record potential arrhythmias in the athlete. The athlete twice competed in a marathon and a half-marathon, simultaneously wearing a Holter ECG and a sports HRM, albeit without showing tachyarrhythmia. Two exercise tests were performed, on a treadmill and a bicycle, without arrhythmias. An electrophysiological study did not provoke an arrhythmia attack.Furthermore, the readings recorded by the HRM were called into question and treated as artifacts, which are often very difficult to distinguish from an undisturbed recording [
7] (
Figure 1C). The clinical data from the patient’s history, although quite convincing, were not confirmed by additional examinations. Some doctors suspected the athlete exhibited Munchhausen syndrome (MS). Meanwhile, the athlete continued to compete and experienced arrhythmia attacks that effectively disqualified him from competing for top places. Arrhythmias of up to 230 bpm appeared with increasing frequency, with concomitant clinical complaints. By the end of 2022, instances of arrhythmia were occurring at shorter distances (10 km) and sometimes also during training sessions. The runner provided written informed consent to participate in the analysis and for his data to be published.
Study Protocol
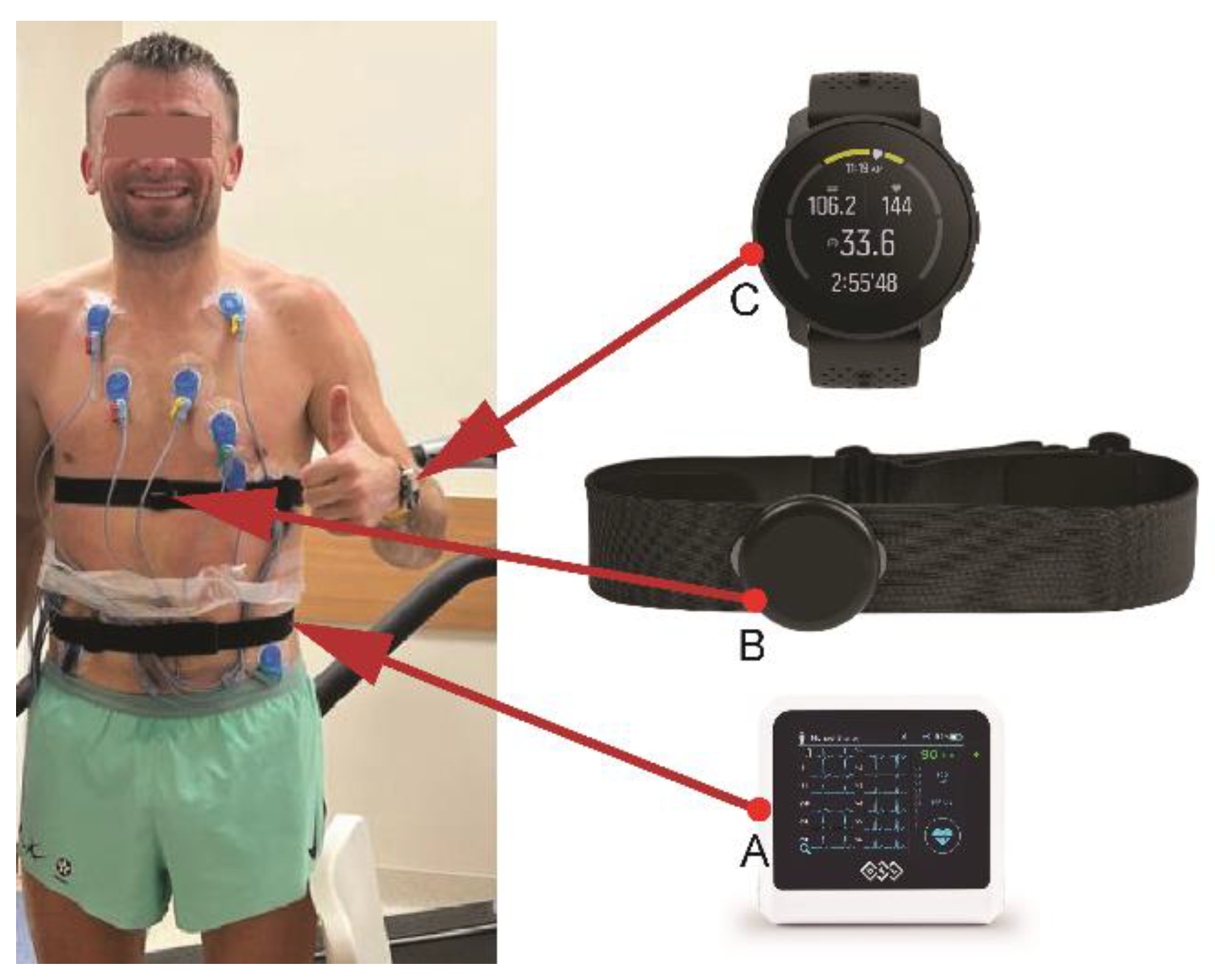
We performed a treadmill exercise test following an individualized protocol, with the main goal of provoking an arrhythmia. An additional goal was to assess the reliability of the sports HRM the athlete used on a daily basis by comparing its measurements to those indicated on the ECG during the exercise test. When the maximum treadmill speed was reached, the treadmill angle was adjusted (between 10 and 18%). Exercise was continued until refusal or provoked arrhythmia. During the test, the athlete wore his normal sports HRM (Smartwatch Suunto 9 Peak with Suunto Smart Heart Rate Belt [Suunto Oy, Vantaa, Finland]), in order to assess the consistency of HRM readings during exercise. We used ECG indications from the exercise testing system as an HR reference.
Figure 2 shows the athlete with the tested HRM.
Some of the sports HRM measurements were tested and compared with a Holter ECG. A team of doctors and technicians with extensive experience in the analysis of HRM measurements used by athletes of various disciplines training under different conditions [
8,
9,
10] analyzed the results.
3. Results
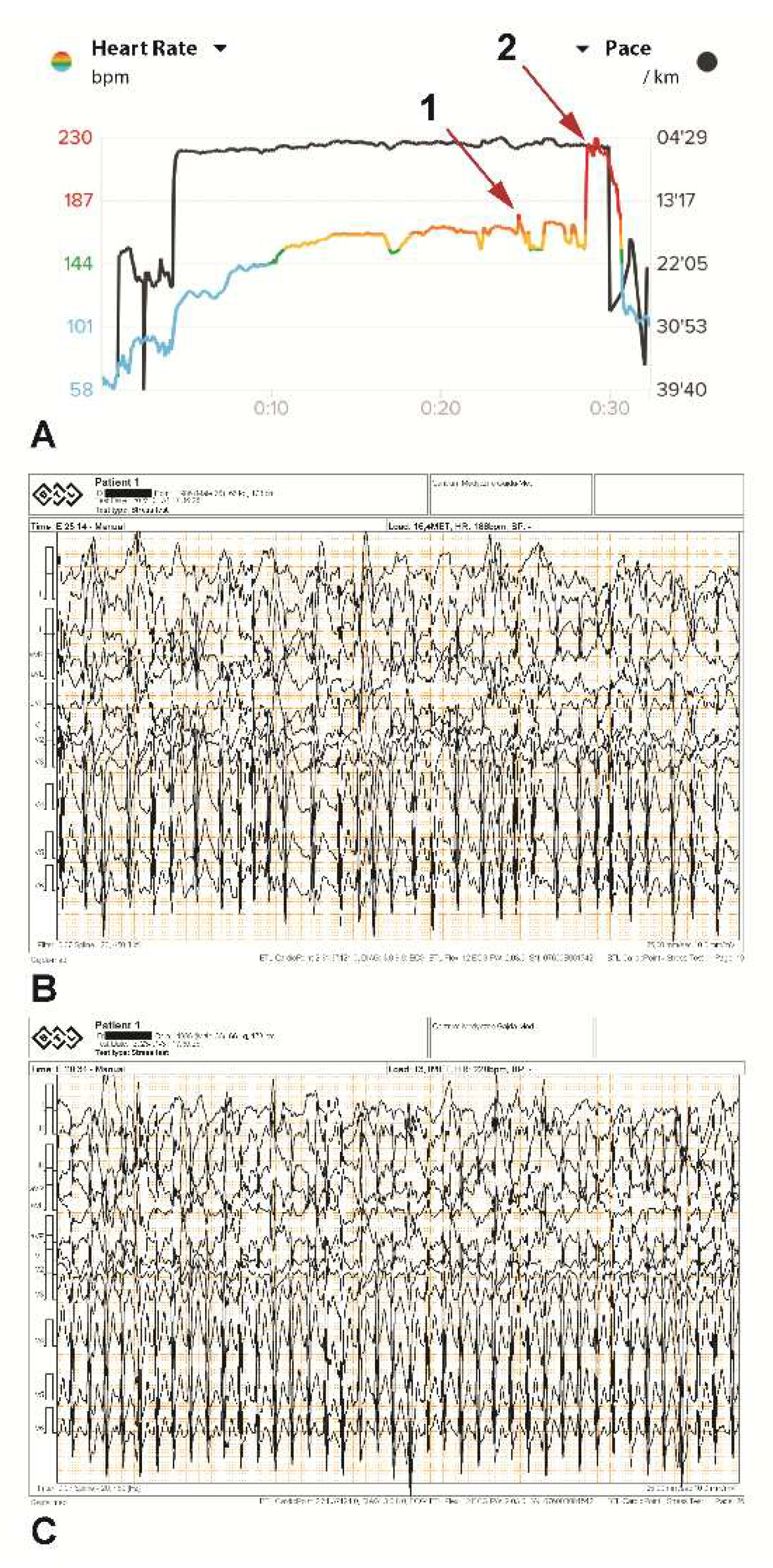
In minute 17 of the treadmill exercise stress test, the maximum treadmill speed (9.7 km/h) was reached, and the treadmill angle was adjusted (between 10 and 18%). A stable heart rate of 172–175 bpm was reached in minute 15. The highest temporary metabolic equivalent of task (MET) load of 18.1 was achieved in minute 18 and corresponded to 63 ml/kg/min VO2max. In minute 25, a brief supraventricular tachycardia (SVT) paroxysm of several seconds was noted on both devices simultaneously, with a rhythm of 187 bpm (
Figure 3A [arrow 1] and 3B). Exercise was continued by changing the angle of the treadmill so that the athlete continued as long as possible at submaximal load. In minute 28, the SVT paroxysm occurred again at a rate of 230 bpm, with the same rhythm being indicated by the HRM (
Figure 3A [arrow 2] and
Figure 3C). The athlete continued the effort for more than one minute without slowing down, despite persistent irregular tachyarrhythmia (possible atrial fibrillation), increasing weakness, and a strong feeling of palpitations. The tachyarrhythmia ceased immediately after the exercise stopped. No typical ischemic ST changes were observed. Multiple increasing supraventricular and single ventricular beats were noted during exercise, as were numerous artifacts resulting from vibrations. Both the HRM and the Holter ECG showed the same HR values.
We had also previously tested the accuracy of the athlete’s HRM measurements when worn simultaneously with a Holter ECG. The HRM showed the same maximum, minimum, average, and momentary values of HR indicated by the Holter ECG.
4. Discussion
We confirmed the presence of cardiac arrhythmia in an experienced high-performance marathon runner. Despite having always been considered healthy, unexpected increases in HR readings on his sports HRMs in recent years, combined with a feeling of palpitations and weakness, were preventing him from continuing endurance efforts. Numerous ECGs (S1), Holter ECGs (S2), an echocardiography study (S3), an MRI (S4), several treadmill and bicycle exercise tests, and finally a cardiac electrophysiology study (S5) (in
Supplementary Materials) failed to reveal cardiac arrhythmias. These tests also provided no grounds for establishing a diagnosis excluding the athlete from further sports competition. Given that no diagnosis could be confirmed, the possibility of the symptoms being simulated in order to justify his lack of success in competitions (MS) was entertained. MS, also called “factitious disorder imposed on self,” is a psychiatric disorder in which a person assumes the role of a sick patient without the intention of external gain (e.g. time off from work, medications) [
11]. A number of cases of MS have been described in the literature, including patients who simulate cardiac symptoms, like HR disturbances (cardiopathia fantastica) [
12,
13,
14]. Diagnosis is always difficult, and in several cases, patients have visited numerous hospitals and sometimes been subjected to unnecessary, costly, and even risky diagnostic procedures [
13]. Clarke and Melnick examined cases of this sort and concluded that “all the patients are psychopaths” (1958) [
15]. However, MS was definitively ruled out in the present case.
We decided to use an individualized protocol designed to replicate a prolonged run during a sports competition. During the exercise test, the pace and incline of the treadmill were altered to sustain submaximal effort for as long as possible with the goal of inducing arrhythmia, which did indeed occur. The arrhythmia described was irregular supraventricular tachycardia (FA Paroxysmal possible) with a ventricular rhythm of 230 bpm and appeared permanently at a HR of 172-175 bpm in minute 28 of the test (corresponding to kilometer 10 in a real race). The athlete was able to continue at the same load level for one more minute, despite rapidly increasing fatigue and a feeling of palpitations. The tachycardia did not subside spontaneously but only when the effort ceased.
The above situation accurately reflected what the athlete experienced in running competitions, when the attack subsided after stopping or after a significant decrease in running pace but recurred when the athlete tried to resume running at the previous pace. During the test, the athlete wore the same HRM he used to wear in the sports competitions, and during the entire test, it indicated exactly the same HR values as the ECG from the exercise test. A test performed previously using a Holter ECG also showed a convergence in HR with the HRM, thus eliminating the notion that the HRM readings might be an artifact. Incorrect HRM readings can be so annoying when participating in long runs that some top athletes quit using HRMs during competition altogether [
16,
17]. In our opinion, HRM readings should be considered reliable when coincident with clinical symptoms, as in this case. The athlete has been informed that he should absolutely refrain from competing in sports and performing maximal and submaximal efforts until diagnostics are completed and a final diagnosis is established.
5. Conclusions
In conclusion, attempting to confirm the presence of arrhythmia induced by extreme endurance exercise in well-trained endurance athletes can in some cases pose a significant diagnostic challenge. Sports HRM indications suggesting paroxysms of rapid tachyarrhythmias during extreme effort in a symptomatic marathon runner cannot be neglected and should be verified during subsequent exercise tests mimicking real-life endurance sports competitions.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Figure S1: ECG test result; Video S3. Echocardiography results; Figure S4 MRI results; Figure S5. Cardiac electrophysiology study; Table S1. The athlete’s personal records.
Author Contributions
R.G. conceived of and designed the study. R.G. performed and analyzed a diagnostic stress test. E.K.B. conducted and analyzed the ECG and Holter ECG. R.G. and J.G. collected the data. R.G. and M.S. analyzed and interpreted the data. R.G., JG., B.K., P.K., M.S., W.D., and MK analyzed the literature and drafted the manuscript. All authors revised the manuscript and approved the final version.
Funding
This research received no external funding.
Institutional Review Board Statement
Ethical review and approval were waived for this study due to the nature of the study.
Informed Consent Statement
Written informed consent has been obtained from the patient to publish this paper.
Data Availability Statement
The data presented in this study are available in Gajda R, et al. 2023. Exercise-induced arrhythmia or Munchhausen syndrome in a marathon runner?
Acknowledgments
The authors thank the marathon-runner who consented to the use of his medical data in this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Graziano, F.; Juhasz, V.; Brunetti, G.; et al. May Strenuous Endurance Sports Activity Damage the Cardiovascular System of Healthy Athletes? A Narrative Review. J Cardiovasc Dev Dis 2022, 9(10), 347. [Google Scholar] [CrossRef] [PubMed]
- La Gerche A, Claessen G, Dymarkowski S, et al. Exercise-induced right ventricular dysfunction is associated with ventricular arrhythmias in endurance athletes. Eur Heart J 2015, 36(30), 1998-2010. [CrossRef]
- La Gerche, A. Exercise-Induced Arrhythmogenic (Right Ventricular) Cardiomyopathy Is Real…if you Consider it. JACC Cardiovasc Imaging 2021, 14(1), 159–161. [Google Scholar] [CrossRef] [PubMed]
- Płoszczyca K, Czuba M, Chalimoniuk M, Gajda R, Baranowski M. Red Blood Cell 2,3-Diphosphoglycerate Decreases in Response to a 30 km Time Trial Under Hypoxia in Cyclists. Front Physiol 2021, 12, 670977. [CrossRef] [PubMed]
- Jagodzińska M, Szperl M, Ponińska J, Kosiec A, Gajda R, Kukla P, Biernacka EK. Coexistence of Andersen-Tawil Syndrome with Polymorphisms in hERG1 Gene (K897T) and SCN5A Gene (H558R) in One Family. Ann Noninvasive Electrocardiol 2016, 21(2), 189-95. [CrossRef]
- Gajda, R. Is Continuous ECG Recording on Heart Rate Monitors the Most Expected Function by Endurance Athletes, Coaches, and Doctors? Diagnostics (Basel) 2020, 10, 867. [Google Scholar] [CrossRef] [PubMed]
- Gajda R, Biernacka EK, Drygas W. Are heart rate monitors valuable tools for diagnosing arrhythmias in endurance athletes? Scand J Med Sci Sports 2018, 28, 496–516. [CrossRef] [PubMed]
- Gajda, R. Heart Rate Monitor Instead of Ablation? Atrioventricular Nodal Re-Entrant Tachycardia in a Leisure-Time Triathlete: 6-Year Follow-Up. Diagnostics 2020, 10, 391. [Google Scholar] [CrossRef] [PubMed]
- Gajda R, Knechtle B, Gębska-Kuczerowska A, et al. Amateur Athlete with Sinus Arrest and Severe Bradycardia Diagnosed through a Heart Rate Monitor: A Six-Year Observation-The Necessity of Shared Decision-Making in Heart Rhythm Therapy Management. Int J Environ Res Public Health 2022, 19(16), 10367. [CrossRef]
- Gajda R, Kowalik E, Rybka S, et al. Evaluation of the heart function of swimmers subjected to exhaustive repetitive endurance efforts during a 500-km relay. Front Physiol 2019, 10, 296. [CrossRef] [PubMed]
- Weber B, Gokarakonda SB, Doyle MQ. Munchausen Syndrome. 2022 Jul 4. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2022.
- Dickinson EJ, Evans TR. Cardiac Munchausen’s syndrome. J R Soc Med 1987, 80(10), 630-633. [CrossRef]
- Hamdan, M.; Hart, K.; Fitzpatrick, A. Munchausen’s syndrome by telemetry. Am Heart J 1996, 131, 1046–1047. [Google Scholar] [CrossRef] [PubMed]
- Cheng, TO. Munchausen syndrome presenting as cardiovascular disease (cardiopathia fantastica). Am J Cardiol 2003, 91(10), 1290. [Google Scholar] [CrossRef] [PubMed]
- Clarke, E.; Melnick, S.C. The Munchausen syndrome or the problem of hospital hoboes. Am J Med 1985, 25(1), 6–12. [Google Scholar] [CrossRef] [PubMed]
- Gajda, R.; Walasek, P.; Jarmuszewski, M. Right Knee-The Weakest Point of the Best Ultramarathon Runners of the World? A Case Study. Int J Environ Res Public Health 2020, 17(16), 5955. [Google Scholar] [CrossRef] [PubMed]
- Gajda R, Klisiewicz A, Matsibora V, Piotrowska-Kownacka D, Biernacka EK. Heart of the World's Top Ultramarathon Runner-Not Necessarily Much Different from Normal. Diagnostics (Basel) 2020, 10(2), 73. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).