1. Introduction
The cavernous sinus (CS) is a vulnerable venous space deep seated in the center of the skull-base which includes vital and highly functional neurovascular structures - internal carotid artery (ICA) and its branches, III, IV and VI cranial nerves, ophthalmic division of trigeminal nerve – therefore the detailed knowledge of its anatomy is mandatory to avoid its potentially life-threating iatrogenic injuries.
As already happened in the past with the advent of the endoscopic endonasal approaches mainly addressed to the pathologies of the midline skull base through a ventral median corridor, most recently the endoscopic transorbital route has opened a new window but mainly on the paramedian and lateral aspects of the anterior and middle cranial fossae up to the petrous apex [
1,
2].
Since the first pioneering work of Parkinson [
3] describing the surgical approach for a carotid-cavernous fistula, several anatomical studies [
4,
5,
6,
7,
8,
9,
10] and surgical series [
11,
12,
13,
14], have provided a detailed description of this dural envelope and its safe entry zones from different routes, both transcranial [
3,
15,
16,
17] and endonasal [
16,
17,
18,
19,
20], and most recently endoscopic transorbital [
21,
22,
23] also, each of them with related pro and cons.
Nevertheless, a single approach is not sufficient to expose the entire CS and simultaneously to have the proximal and distal control of the cavernous ICA, which is necessary for a safe surgery.
Tumoral, congenital, infectious/inflammatory/granulomatous, and vascular pathologies, of any size and morphology, pattern of growth and diffusion, can involve one or more compartments of the cavernous sinus and have different relationships with the structures lying within it. In this scenario, when a surgical treatment is indicated, it is mandatory for a neurosurgeon to be confident with more than one surgical route to have at disposition different working angles through the various triangles to maximize the tumor resection and minimize the risk of cranial nerves and ICA injuries, and choice the best tailored option.
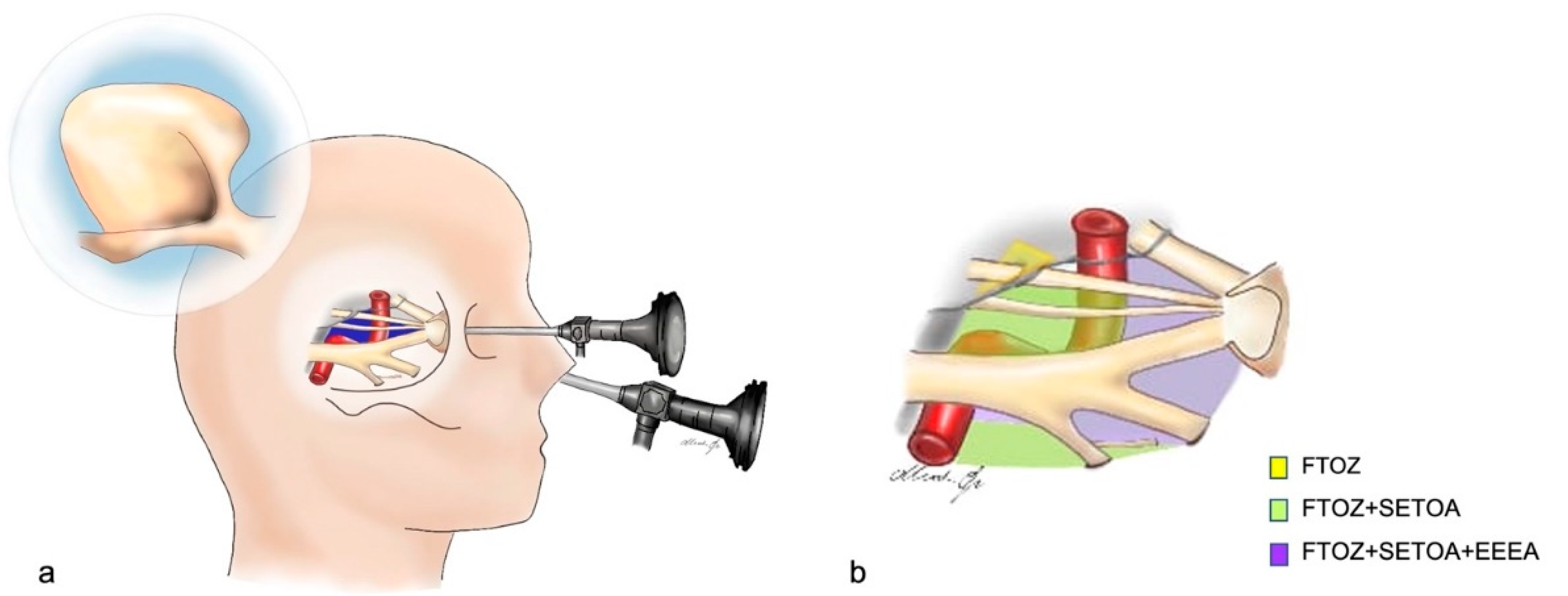
The aim of the current study was to provide an anatomical description from superior eyelid transorbital endoscopic (SETOA) perspective of the cavernous sinus and its relationship with the main neurovascular structures; furthermore, we attempted to highlight the main differences and similarities of the exposed area and its landmarks as seen from endoscopic endonasal and transcranial routes (
Figure 1). Finally, we tried to define the safe entry zones to this venous space from these three different operative corridors (
Table 1) and provide indications regarding the optimal approach according to the lesion location.
2. Materials and Methods
Anatomical dissections were performed at the Laboratory of Skull Base and Micro-neurosurgery of the Weill Cornell Neurosurgical Innovations and Training Center, New York, USA. Five adult cadaveric specimens (10 sides), embalmed and injected with red and blue latex for the arteriosus and venous blood vessels, respectively, were dissected. The fronto-temporo-orbito-zygomatic (FTOZ) approach was performed under microscopic visualization (OPMI, Zeiss, Oberkochen, Germany), whereas the extended endoscopic endonasal transsphenoidal-transethmoidal (EEEA) was performed with a rigid endoscope of 4-mm-diameter, 18 cm in length, with 0° and 30° rod lenses as optical device (Karl Storz, Tuttlingen, Germany); finally, the SETOA, after the initial step under macroscopic visualization, proceeded under endoscopic visualization. The endoscope was connected to a light source (300 W Xenon, Karl Storz) through a fiberoptic cable and to an HD camera (Endovision Telecam SL; Karl Storz).
We adopted the intracranial classification system (C1-C7) proposed by Bouthillier et al [
24]. for the description of the anatomical course of ICA and the well-known division in triangles of the cavernous sinus [
15], as referral to depict the areas of exposure.
2.1. Fronto-Temporo-Orbito-Zygomatic (FTOZ) Approach
The surgical procedure started with a curvilinear skin incision extended from 1 cm anterior to the tragus and below the zygomatic arch; to the contralateral midpupillary line and was followed by a subgaleal interfascial dissection [
25] and a retrograde subperiosteal detachment of the temporalis muscle [
26]. At this point a two-piece orbitozygomatic craniotomy according to Zabramski [
27] technique was performed; followed by the cutting of meningo-orbital band [
28] and the extradural anterior clinoidectomy [
29]. Finally; the surgical procedure was completed with the peeling of the lateral wall of the CS and the middle cranial fossa; and with the pericavernous maneuvers [
30] to expand the optic-carotid and carotid-oculomotor windows.
2.2. Superior Eyelid Transorbital Endoscopic Approach (SETOA)
A SETOA to the petrous apex was performed as previously reported in the literature [
31].
A skin incision was placed in a superior eyelid wrinkle; hence, once the orbicularis oculi muscle was identified, the dissection was carried in depth up to the superior orbital rim and extended laterally up to the frontozygomatic suture. After cutting the periosteum where it became continuous with the periorbita, the dissection continued, with endoscopic assistance, in a subperiosteum/periorbital plane within the orbit until the lateral margin of the inferior and superior orbital fissures. At this point, once the zygomatic body and the intraorbital part of the greater sphenoid wing including the sagittal crest [
32] were drilled until to expose the temporal pole dura mater, an interperiosteal-dural dissection via meningo-orbital band (MOB)[
21] was performed to unlock the lateral wall of the CS up to the gasserian ganglion (GG). After cutting middle meningeal artery (MMA), the temporal pole was elevated in extradural fashion and, once the midsubtemporal ridge and the trigeminal lateral loop were identified [
33], the middle fossa anterolateral triangle was opened. Finally, an extradural anterior clinoidectomy [
34] completed the surgical procedure.
2.3. Extended Endoscopic Endonasal Transsphenoidal Transethmoidal Approach (EEEA)
An extended endoscopic endonasal transsphenoidal transethmoidal approach was performed as previously reported in the literature [
20,
35]. Conversely from the standard endoscopic endonasal transsphenoidal approach, to obtain a wider exposition of the CS, the sphenoidotomy was extended more laterally and the posterior ethmoidal cells were opened. Furthermore, to expand the operative corridor, the uncinate process was removed and the bulla ethmoidalis was opened, thus allowing to reach and remove the anterior ethmoid cells. The removal of the posterior ethmoid cells and the anterior wall of the sphenoid sinus allowed to expose the lateral wall of the sphenoid sinus with a direct trajectory, and once it was removed, the CS came into the view.
3. Results
The differences and likenesses of the various regions of the CS and the related anatomical landmarks have been analyzed to make a comparison from transcranial, endoscopic endonasal and endoscopic transorbital perspectives.
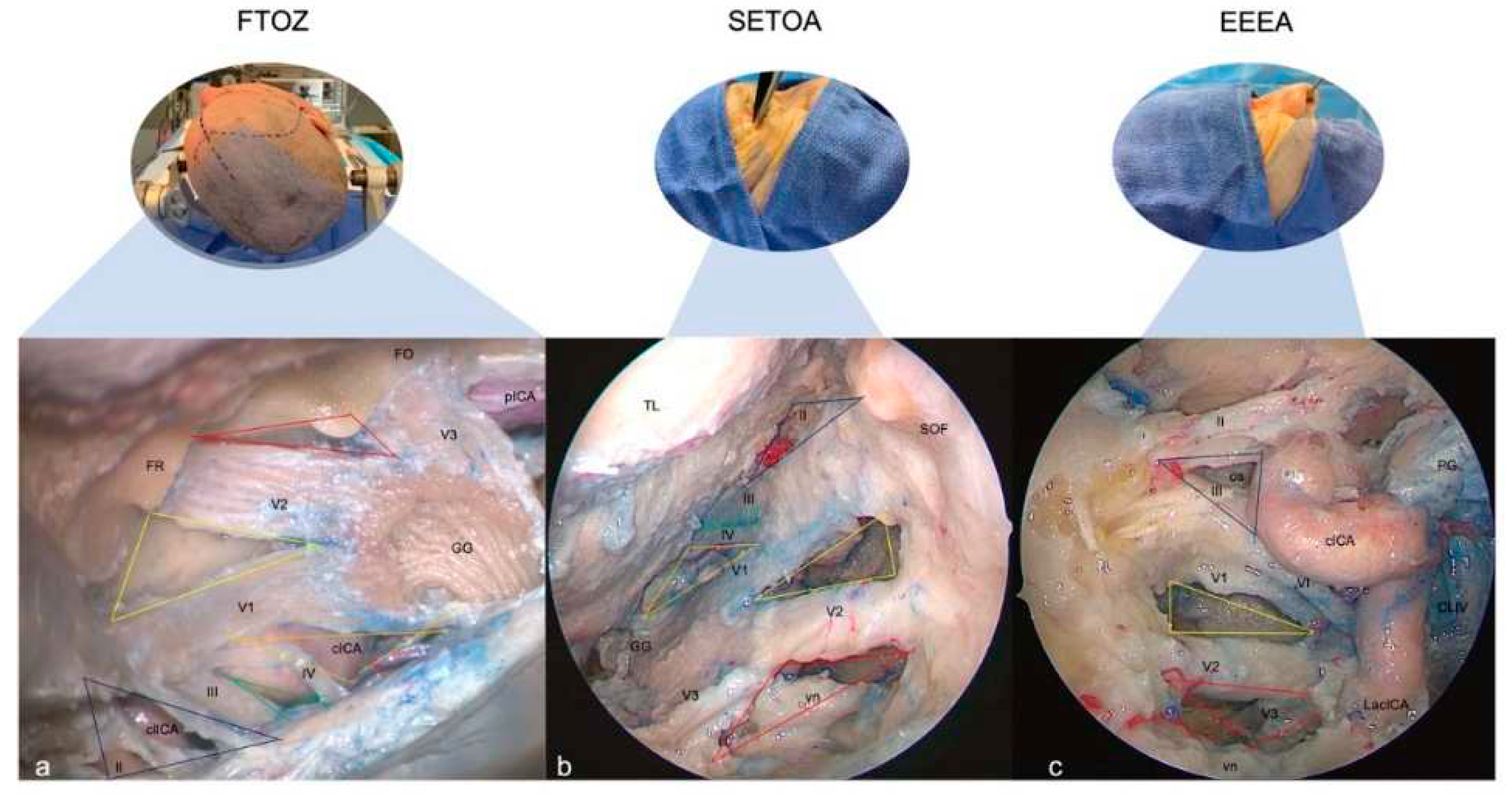
3.1. Clinoid Triangle (Dolenc’s triangle)
3.1.1. FTOZ perspective
This area is bounded by the inferior margin of the optic nerve superiorly, the superior margin of the oculomotor nerve inferiorly, and by the segment of the anterior petroclinoid dural fold between the entry point of the II and the III cranial nerves. It includes the anterior clinoid process hiding the clinoidal segment of the ICA (C5 segment [
24]) between the proximal and distal dural rings. It is needed to remove the anterior clinoidal process to expose its content (
Figure 2a,b).
3.1.2. SETOA perspective
The clinoid triangle is completely exposed through transorbital route and, after the anterior clinoidectomy, also its content is evident.
The anterior clinoid process (ACP) removal reveals a pyramidal dural pocket bounded by the dura on the superior surface of the lesser sphenoid wing (LSW), laterally, the dura on the superior surface of the LSW and attaching to the lateral edge of the planum sphenoidale, superiorly, the falciform ligament covering the proximal segment of the optic nerve (ON) after its unroofing, medially, and finally, the optic nerve dural sheath and the anterior part of the distal dural ring of the ICA, inferiorly.
The ON is observed along its posteromedial course toward the optic chiasm. The clinoidal segment of the ICA (C5 segment [
24]) between lower and upper dural rings is observed in the central part of the triangle, with the ophthalmic artery running inferomedially to the ON. Finally, the optic-carotid membrane and space are also evident (
Figure 2c,d).
3.1.3. EEEA perspective
This area is bounded by the optic nerve above, and the oculomotor nerve below the optic strut. The base of this triangle is represented by the distal part of horizontal segment and the anterior bend of the cavernous ICA (C4-C5 segments [
24]). The content of this triangle is the optic strut or optic-carotid recess (
Figure 2e).
3.2. Oculomotor Triangle (Hakuba’s triangle)
3.2.1. FTOZ perspective
This triangle forms the posterior part of the roof of the cavernous sinus. Its boundaries are the interclinoid dural fold medially and, the anterior and posterior petroclinoid dural folds, laterally and posteriorly, respectively.
3.2.2. SETOA perspective
This area, even after anterior clinoidectomy is scarcely recognizable from this surgical corridor.
3.2.3. EEEA perspective
This triangle is not identifiable also after gentle medial displacement of the ICA.
3.3. Supratrochlear Triangle (Paramedian)
3.3.1. FTOZ perspective
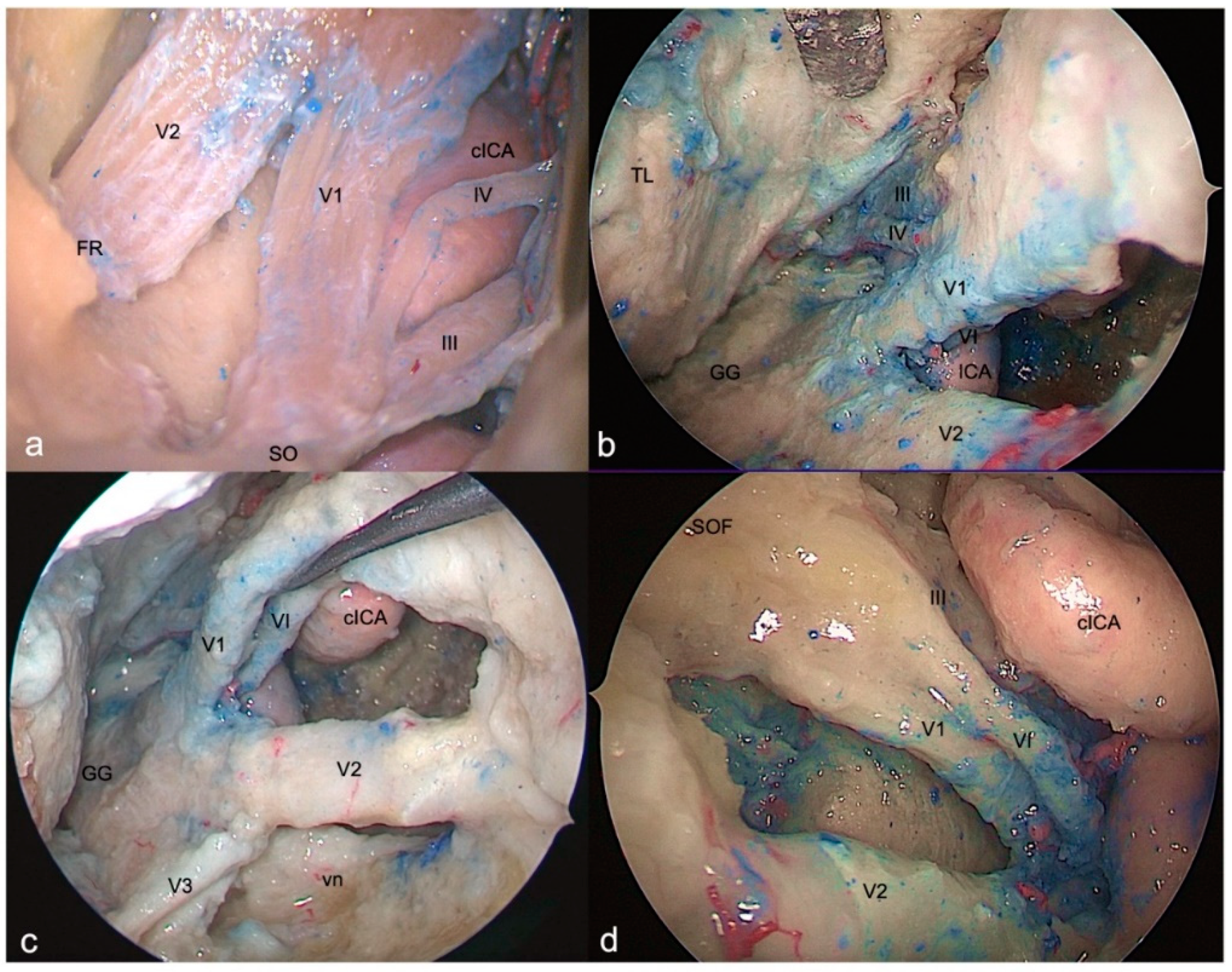
This area is bounded by the inferior border of the oculomotor nerve superiorly, the superior border of the trochlear nerve inferiorly and, by the segment of the dura of the roof of the cavernous sinus between the entry points of these two nerves. Its content is represented by the horizontal cavernous ICA (
Figure 3a).
3.3.2. SETOA perspective
This triangle and its boundaries are completely exposed via the transorbital corridor just after interperiosteal-dural dissection of the lateral wall of the CS. It’s a very narrow space hiding medially the horizontal segment of the cavernous ICA (C4 segment [
24]) (
Figure 3b).
3.3.3. EEEA perspective
Just the apex of this triangle, where III and IV cranial nerves converge toward the SOF, can be exposed and it’s needed to displace the ICA medially and/or the cranial nerves laterally (
Figure 3c).
3.4. Infratrochlear Triangle (Parkinson’s triangle)
3.4.1. FTOZ perspective
This triangle is delimited superiorly by the lower margin of the trochlear nerve, inferiorly by the upper margin of V1 and posteriorly by the line connecting the point where the trochlear nerve enters the roof of cavernous sinus and the point where the trigeminal nerve enters the Meckel’s cave. This region hosts the posterior bend of the cavernous ICA (C4 segment [
24]) with its branches (meningohypophyseal trunk) (
Figure 3a).
3.4.2. SETOA perspective
This region and its content are completely exposed via transorbital route; just after interperiosteal-dura dissection of the lateral wall of the CS, the antero-lateral aspect of the superior half of the ascending segment of the cavernous ICA is evident. Furthermore, after a gentle downward retraction of the proximal part of V1 is possible to identify the sixth cranial neve exiting from the Dorello’s canal under the Gruber’s ligament and coursing anteriorly in the lateral wall of the CS medially to V1. Displacing gently upward the trochlear nerve, it is possible to expose the meningohypophyseal trunk (MHT) arising from the posterior bend of cavernous ICA (C4 segment [
24]) (
Figure 3b).
3.4.3. EEEA perspective
Only the anterior narrow space of this triangle and its content, represented by the inferolateral trunk of the cavernous ICA (C4 segment [
24]), are evident, because of the abducens nerve which covers the ophthalmic division of trigeminal nerve and of the horizontal tract of the cavernous ICA which obstacles the access to the posterior compartment (
Figure 3c).
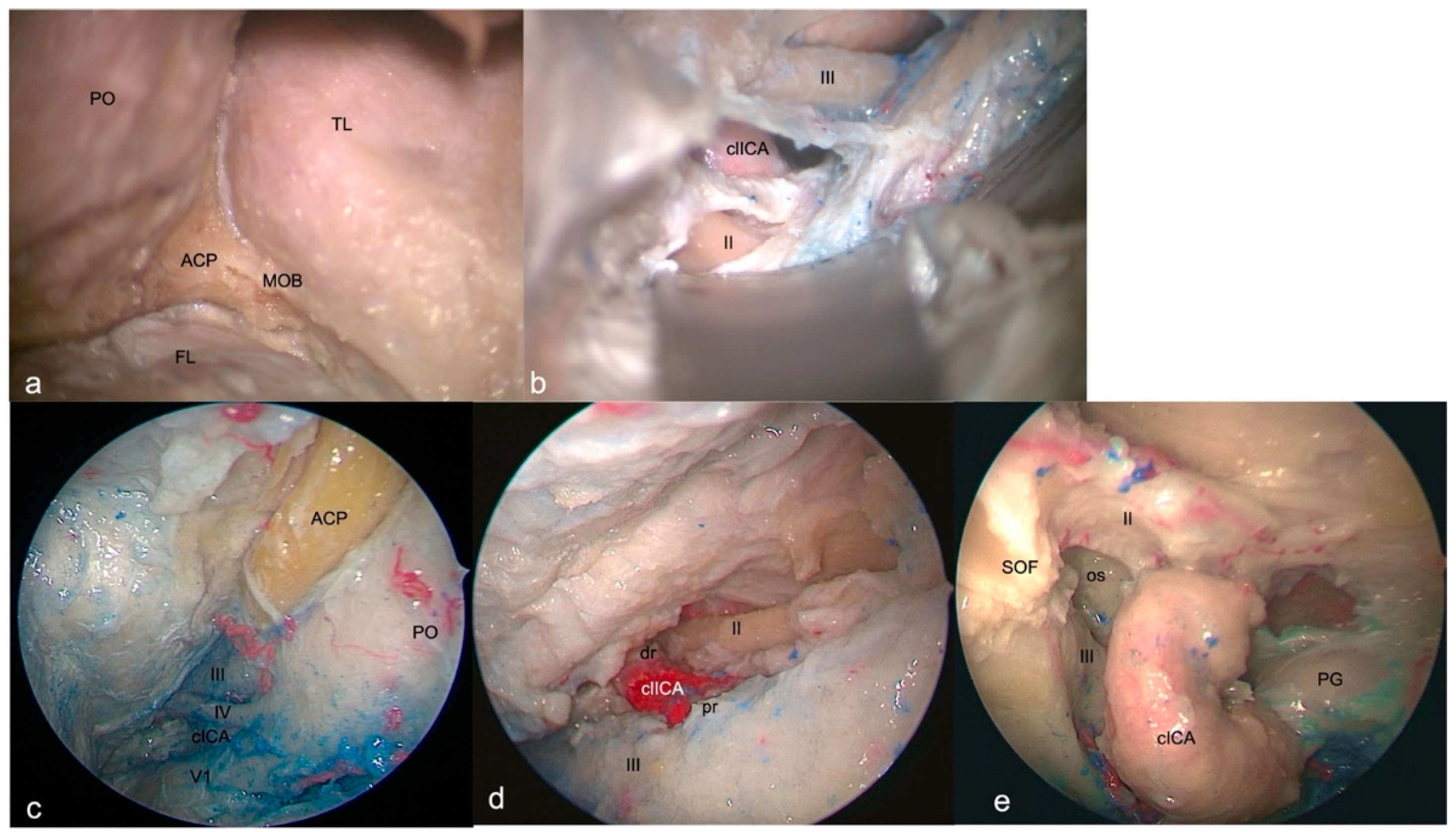
3.5. Anteromedial Triangle (Mullan’s triangle)
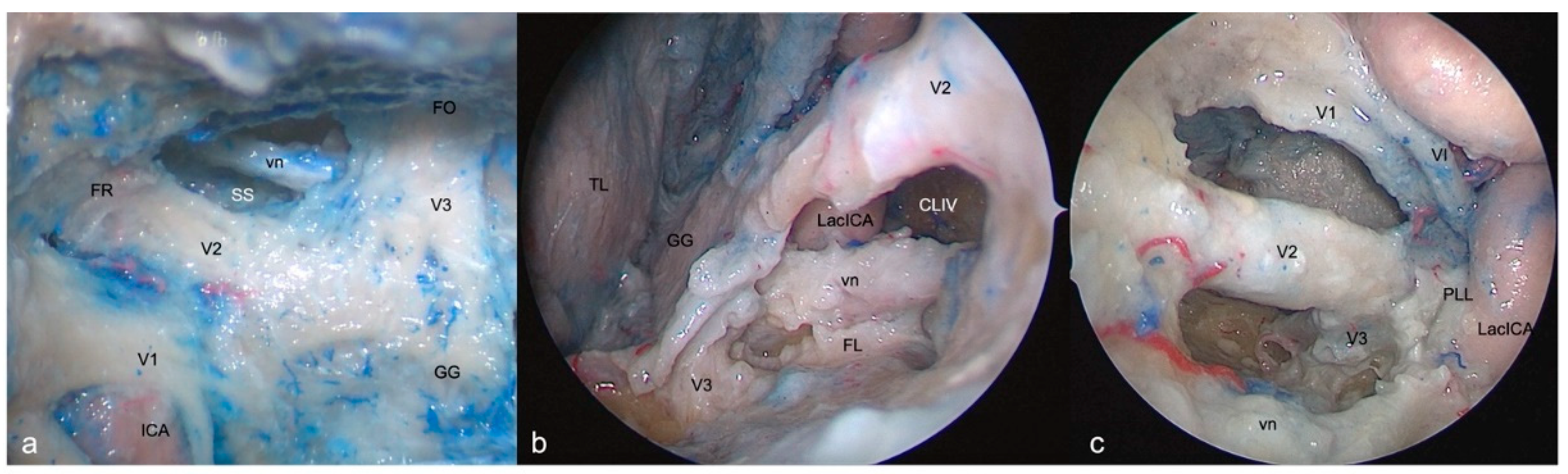
3.5.1. FTOZ perspective
This region is delimited superiorly by the lower margin of V1, inferiorly by the upper margin of V2 and anteriorly by the line connecting the point where the ophthalmic nerve enters superior orbital fissure and the point where the maxillary nerve enters foramen rotundum (
Figure 4a). The removal of the outer bony shell of this triangle leads into the sphenoid sinus.
3.5.2. SETOA perspective
This region comes immediately into the endoscopic view after interperiosteal-dura dissection of the lateral wall of CS and is the largest safe entry zone to the CS. Unlike the transcranial fronto-temporal point of view, where no segments of ICA are visible in this area, the SETOA allows to disclose in the depth, at the apex of this triangle, where V1 and V2 converge, the inferior half of the posterior ascending segment of the cavernous ICA (C4 segment [
24]) after exiting the foramen lacerum, surrounded by sympathetic fibers of the carotid plexus, passing medially to the petro-lingual ligament, to reach the cavernous sinus (
Figure 4b). In this triangle, the VI cranial nerve courses almost horizontally, medially to V1 and laterally to the ICA, towards the SOF, and can be visualized after gentle upward retraction of V1 (
Figure 4c). One fundamental landmark to guide surgical dissection of the anteromedial triangle, avoiding entering the CS space is the foramen rotundum, which is encountered after resection of the sagittal crest, that discloses V2 inferiorly and outside the CS. Surgical dissection must be performed between the two trigeminal branches at the level of the superior edge of V2, dissecting the perineurium covering the two nerves in an antero-posterior direction, to free the two branches and mobilizing the ophthalmic nerve superiorly, expanding the space between them to get access to the postero-inferior portion of the CS.
3.5.3. EEEA perspective
This area and its content, represented by venous structures, are completely exposed after bone removal of the lateral wall of the sphenoid sinus, with V1 partially hidden by the sixth cranial nerve. The apex of this triangle, where V1 and V2 converge, can be disclosed after medial displacement of the lacerum (C3 segment [
24]) and posterior ascending tract of the cavernous (C4 segment [
24]) segments of ICA (
Figure 4d).
3.6. Anterolateral Triangle
3.6.1. FTOZ perspective
This area is bounded by the lower border of V2, superiorly, the upper border of V3, inferiorly and by the line which connects the foramina rotundum and ovale. The drilling of its medial wall exposes the sphenoid sinus (
Figure 5a).
3.6.2. SETOA perspective
The opening of this triangle allows to disclose the vidian nerve and artery in the homonymous canal along their course up to the anterolateral edge of the foramen lacerum, where the posterior opening of the canal is filled with cartilaginous tissue that blends into the more medially positioned cartilage filling the foramen lacerum. The lacerum segment of ICA, at its transition zone from the horizontal petrous to the ascending cavernous segment, medially to the petrolingual ligament, and the related carotid sympathetic plexus, can be exposed also (
Figure 5b). As already recently described by our group [
36], it is possible to appreciate a space limited by the inferior border of V2, superiorly, the superior border of V3, posteriorly, the line crossing the most anterior limit of exposure of the vidian nerve and joining the foramen rotundum and the point where the greater wing joints the body of the sphenoid bone, anteriorly, and the line between this last point and the foramen ovale posteriorly. This area includes two windows divided by the course of the vidian nerve until where it blends into the cartilaginous tissue of the FL under the trigeminal nerve, and which unfolds different corridors:
a wider superior window (“supravidian”), which discloses two corridors in relationship to the lacerum segments of the ICA: a “medial supravidian corridor” leading to the lower clivus, and a “lateral supravidian corridor” leading, after gentle lateralization of the gasserian ganglion, to the medial aspect of the Meckel’s cave and the terminal portion of the horizontal petrous ICA (pICA).
a narrow inferior window (“infravidian”): which includes the inferior portion of the foramen lacerum distally, and the sphenoid sinus proximally.
3.6.3. EEEA perspective
Whereas V2 is disclosed from the origin up to the foramen rotundum, V3 is recognizable only in its course from the origin at the Gasserian ganglion up to the entrance the foramen ovale (
Figure 5c).
4. Discussion
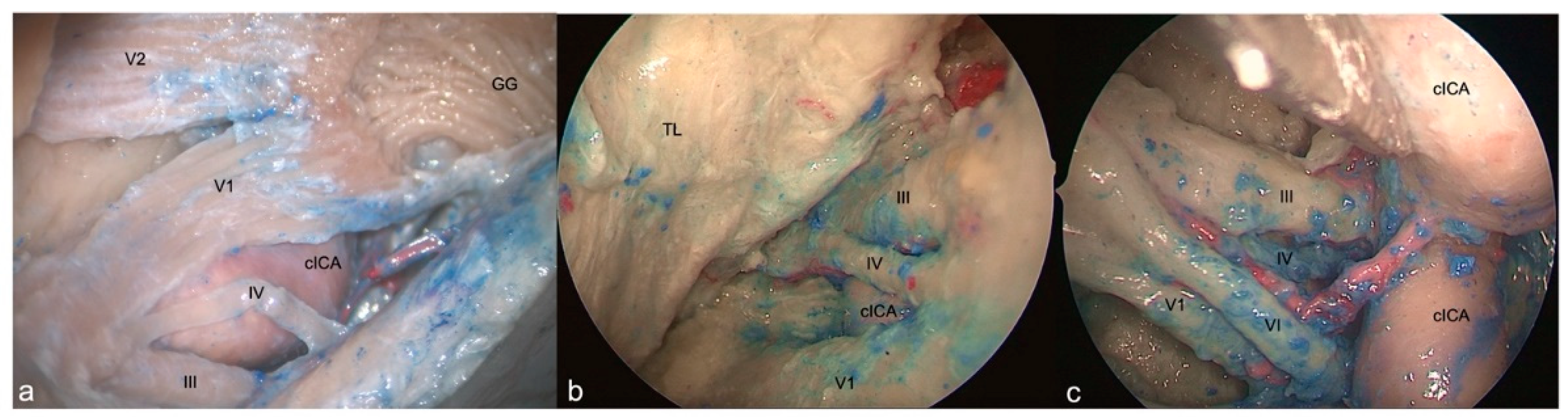
4.1. Anatomical considerations
The oculomotor triangle can be clearly exposed and expanded by opening the optic-carotid and carotid-oculomotor windows, only through transcranial approach, whereas it is scarcely identifiable from SETOA and EEEA in normal conditions; albeit Nunes et al [
37]. have described an endoscopic endonasal transoculomotor triangle approach for adenomas invading the parapeduncolar space in which the lesion created the corridor.
To expose the clinoidal triangle and its content, the anterior clinoidectomy is necessary for both SETOA and FTOZ. Unlike the transcranial route, the extradural clinoidectomy via transorbital does not have anatomic landmarks, and the limits of the ACP base drive the drilling [
34]. Unlike the transcranial and transorbital approaches, during EEEA the ICA comes into the view in front of the ACP, just after exposing the posterior wall of the sphenoid sinus. We consider safe the access to this area from all the three operative corridors (green traffic light -
Table 1).
The transorbital corridor provides the same exposure of the supra- and infratrochlear triangles content compared to the transcranial route, but with different working angle, and providing a better control on the anterior aspect of the posterior ascending segment of the cavernous ICA. The EEEA allows to expose just the apex of the supratrochlear triangle, but the displacement of the ICA medially and/or the cranial nerves laterally is required; concerning the Parkinson’s triangle, the horizontal cavernous ICA and the VI nerve partially obstruct its exposure. We consider the access to both these triangles relatively safe from all the three corridors (yellow traffic light –
Table 1), taking into the account the superficial course of the ICA and MHT in this region from each perspective although different.
The anteromedial triangle is the largest opened window on the CS from SETOA. Unlike the transcranial, the endoscopic transorbital route allows to expose through this triangle the anterior aspect of the inferior half of the posterior ascending segment of the cavernous ICA after exiting the foramen lacerum, surrounded by sympathetic fibers of the carotid plexus; the VI cranial nerve also, along its almost horizontal course, medially to V1 and laterally to the ICA, towards the SOF, can be visualized after gentle upward retraction of V1. We consider safe the access to this area from EEEA and FTOZ (green traffic light –
Table 1), whereas you should be more careful when using the transorbital corridor (yellow traffic light –
Table 1) for the proximity of the inferior border of the horizontal segment of the cavernous ICA partially hiding by V2 and the inferior segment of posterior ascending cavernous ICA in the deep of the triangle.
The opening of the anterolateral triangle through SETOA, discloses a space which can be divided into a wider superior window (“supravidian”) and a narrow inferior window (“infravidian”): the supravidian window allows the direct access to the lacerum segment of the ICA and the related carotid sympathetic plexus; furthermore, this space discloses two different corridors: the
medial supravidian corridor leading to the lower clivus and the
medial supravidian corridor leading to the Meckel’s cave and the terminal portion of the horizontal petrous ICA, respectively medial and lateral to the lacerum ICA. We consider safe the access to this area from all three (FTOZ, SETOA and EEEA) surgical routes (green traffic light –
Table 1).
Figure 6.
a) Graphic draw showing: the fronto-temporo-orbito-zygomatic (FTOZ), endoscopic transorbital (SETOA) and endoscopic endonasal (EEEA) approaches to the cavernous sinus; b) graphic draw of the cavernous sinus and its exposure areas from the three approaches through the different triangles.
Figure 6.
a) Graphic draw showing: the fronto-temporo-orbito-zygomatic (FTOZ), endoscopic transorbital (SETOA) and endoscopic endonasal (EEEA) approaches to the cavernous sinus; b) graphic draw of the cavernous sinus and its exposure areas from the three approaches through the different triangles.
4.2. Surgical nuances
Among the more or less recent classifications of the compartments of the CS [
4,
38,
39], in agreement with that one provided by Harris et al [
4], we considered three main venous spaces in relationship with the course of the cavernous ICA: posterosuperior, anteroinferior and medial compartments.
The FTOZ allows the access to the CS through its roof and lateral wall using the clinoidal and oculomotor, and supra and infratrochlear triangles, respectively [
40].
Clinoidal triangle represents the lower floor of the anterior portion of the roof of the cavernous sinus and is commonly used to approach paraclinoid or carotid-ophthalmic aneurysms; its exposition requires the intra or extradural removal of the ACP and care must be taken to the clinoidal ICA and to the unroofing of the optic canal during this maneuver. The exposure of this area continues with the opening the optic sheath and the distal dural ring. The oculomotor triangle represents the posterior part of the roof of the cavernous sinus, and it is usually used as corridor to access basilar tip aneurysms and tumors inside the cavernous sinus; its exposition requires the opening of the oculomotor cistern, the incision of the carotid-oculomotor membrane and the incision of the dura of the triangle; care must be taken to identify the MHT.
The simultaneous opening of these two triangles allow to manage lesions involving the lateral, posterosuperior and medial compartments of the CS.
The FTOZ, allows to access the posterosuperior and anteroinferior compartments of the CS, also through its lateral wall by opening the supra- and/or infratrochlear triangles, just after the peeling of the middle fossa; care is recommended to identify the VI c.n. exiting the Dorello’s canal through the Parkinson triangle.
The EEEA allows the access to the posterosuperior and anterior compartments of the CS through its medial (sellar) and anterior (sphenoidal) walls thanks to a medial-to-lateral [
41] and an anterior-to-posterior trajectories [
38], respectively. To access the posterior compartment, the opening of the sellar dura and the cutting of the inferior hypophyseal artery are required; the access to the anteroinferior compartment is facilitated by using transpterygoid approach.
The exposure area of the lateral wall of the CS from EEEA is greatly influenced by the ICA position: because of its localization inside the CS, the ICA comes into the endoscopic view before of the lateral wall of the CS so representing an obstacle for the visualization of the posterior content of the CS lateral wall, mainly of the supra- and infratrochlear triangles. Conversely, the anterior part of the clinoidal, the entire anteromedial and the upper part of the anterolateral triangles are exposed and provide potential pathways from this route to the middle cranial fossa.
As this route mainly indicated for midline skull base pathologies, its main risks and drawback approaching the CS are related to the lateral extension, i.e. pituitary adenomas with CS invasion, and include the injury of the ICA, of the cranial nerves, CSF leak and limited resection rate.
The interperiosteal-dural dissection from anterior to posterior via MOB [
21] during SETOA provides a shorter and direct route, and follows a natural sagittal plane which allows to expose the entire lateral wall of the CS without violating its neurovascular compartment and with an optimal angle of attack [
21]. The MOB represents the key landmark in identification of the CS via SETOA. If from one side the extradural endoscopic transsphenoidal and transethmoidal approaches offer a direct access to the anterior portion of the cavernous sinus, from the other side the lateral and posterior walls instead represent a challenge from this route [
20,
42,
43].
The transorbital approach respects the principles of the modern skull-base minimally invasive techniques: flattening the skull-base and using the extradural space to approach the target lesion reducing the brain retraction [
44]. Nevertheless, a mandatory consideration must be kept in mind in exposing the CS: the width of the surgical corridor. This route, albeit providing a wide visualization, uses a narrow (and single if compared to the EEEA) surgical corridor that imposes limitations on the surgical freedom and working angles, therefore it is mainly suitable for small lesions involving the CS at its posterosuperior and anteroinferior lateral compartments, through the supra- and infratrochlear, and anteromedial and anterolateral triangles, respectively [
42].
The relationship of lesion and cranial nerves in the lateral wall, the anatomical course of the ICA and the displacement of the ICA by the pathology guide the choice of the approach[
42]: lesions that displace laterally the cranial nerves, are more suitable for EEEA; lesions that displace medially the cranial nerves are more suitable for FTOZ and SETOA.
The most serious and potentially life-threatening complication is represented by the iatrogenic injury of the ICA, whose incidence ranges from 3% to 8% [
45] in conventional open approaches and lesser than 1% during EEEA [
46]; no data are reported about the transorbital route for the recent adoption of this technique in the neurosurgical field; therefore, unnecessary exposure of the ICA must be avoided.
4.3. Limitations of this study
Pure anatomical studies have the common limitation related to the cadaveric specimens. The property of cadaveric tissue considerably differs from real anatomy: variability in size and pneumatization of the sphenoid sinus, trajectory of the internal carotid artery and cranial nerves, bony protuberances of the skull base. However, the main anatomical relationships among cavernous sinus and its neurovascular structures are valid and reliable.
5. Conclusions
The three operative corridors investigated provide three different points of view of the same anatomical region; each of them has its pro and cons; some areas of the cavernous sinus are better exposed from one approach, others from another one.
In this scenario, the transorbital endoscopic can be considered a safe complementary route to the well-established transcranial and endoscopic endonasal ones exploring the cavernous sinus. Nevertheless, as any new technique, it requires a learning curve and further clinical series are expected to validate these findings.
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable. Any portion of the paper has not been previously elsewhere presented nor published.
Availability of data and materials
Data of the current original research are available from the corresponding author on reasonable request.
Author Contributions
Sergio Corvino: Conception, Anatomical dissection, Data collection, Data Review, Drafting manuscript, Reviewed drafted manuscript; Study supervision; Pedro L. Villanueva-Solórzano: anatomical dissection; Martina Offi: graphic draw; Motonobu Nonaka: anatomical dissection; Daniele Armocida: anatomical dissection; Matteo de Notaris: conception; Giorgio Iaconetta, Felice Esposito, LM Cavallo, Study supervision.
Funding
The authors declare that no funding was received for this work.
Acknowledgments
Thanks to the Laboratory of Skull Base and Micro-neurosurgery of the Weill Cornell Neurosurgical Innovations and Training Center, New York, USA.
Conflicts of Interest
All authors deny any financial and not-financial competing interests.
Abbreviations
| SETOA |
Superior Eyelid Transorbital Endoscopic Approach |
| EEEA |
Extended Endoscopic Endonasal Approach |
| ICA |
Internal Carotid Artery |
| GG |
Gasserian Ganglion |
| MOB |
Meningo-Orbital Band |
| MMA |
Middle Meningeal Artery |
| CS |
Cavernous Sinus |
| FL |
Foramen Lacerum |
| PL |
Petrolingual Ligament |
| vn |
vidian nerve |
| pICA |
petrous Internal Carotid Artery |
| FTOZ |
Fronto-Temporo-Orbito-Zygomatic |
| MC |
Meckel Cave |
References
- Vural, A.; Carobbio, A.L.C.; Ferrari, M.; Rampinelli, V.; Schreiber, A.; Mattavelli, D.; Doglietto, F.; Buffoli, B.; Rodella, L.F.; Taboni, S.; et al. Transorbital endoscopic approaches to the skull base: a systematic literature review and anatomical description. Neurosurg Rev 2021. [Google Scholar] [CrossRef]
- Corvino, S.; Guizzardi, G.; Sacco, M.; Corrivetti, F.; Bove, I.; Enseñat, J.; Colamaria, A.; Prats-Galino, A.; Solari, D.; Cavallo, L.M.; et al. The feasibility of three port endonasal, transorbital, and sublabial approach to the petroclival region: neurosurgical audit and multiportal anatomic quantitative investigation. Acta Neurochir (Wien) 2023. [Google Scholar] [CrossRef] [PubMed]
- Parkinson, D. A surgical approach to the cavernous portion of the carotid artery. Anatomical studies and case report. J Neurosurg 1965, 23, 474–483. [Google Scholar] [CrossRef] [PubMed]
- Harris, F.S.; Rhoton, A.L. Anatomy of the cavernous sinus. A microsurgical study. J Neurosurg 1976, 45, 169–180. [Google Scholar] [CrossRef] [PubMed]
- Inoue, T.; Rhoton, A.L.; Theele, D.; Barry, M.E. Surgical approaches to the cavernous sinus: a microsurgical study. Neurosurgery 1990, 26, 903–932. [Google Scholar] [CrossRef]
- Xu, Z.; Wei, X.; Zhao, C. [Microsurgical anatomical study of the wall of the cavernous sinus]. Zhonghua Yi Xue Za Zhi 1996, 76, 855–858. [Google Scholar]
- Jian, F.Z.; Santoro, A.; Innocenzi, G.; Wang, X.W.; Liu, S.S.; Cantore, G. Frontotemporal orbitozygomatic craniotomy to exposure the cavernous sinus and its surrounding regions. Microsurgical anatomy. J Neurosurg Sci 2001, 45, 19–28. [Google Scholar]
- Yasuda, A.; Campero, A.; Martins, C.; Rhoton, A.L.; Ribas, G.C. The medial wall of the cavernous sinus: microsurgical anatomy. Neurosurgery 2004, 55, 179–189. [Google Scholar] [CrossRef]
- Isolan, G.R.; Krayenbühl, N.; de Oliveira, E.; Al-Mefty, O. Microsurgical Anatomy of the Cavernous Sinus: Measurements of the Triangles in and around It. Skull Base 2007, 17, 357–367. [Google Scholar] [CrossRef]
- Sekhar, L.N.; Burgess, J.; Akin, O. Anatomical study of the cavernous sinus emphasizing operative approaches and related vascular and neural reconstruction. Neurosurgery 1987, 21, 806–816. [Google Scholar] [CrossRef]
- Al-Mefty, O.; Smith, R.R. Surgery of tumors invading the cavernous sinus. Surg Neurol 1988, 30, 370–381. [Google Scholar] [CrossRef] [PubMed]
- Cusimano, M.D.; Sekhar, L.N.; Sen, C.N.; Pomonis, S.; Wright, D.C.; Biglan, A.W.; Jannetta, P.J. The results of surgery for benign tumors of the cavernous sinus. Neurosurgery 1995, 37, 1–9. [Google Scholar] [CrossRef] [PubMed]
- Dolenc, V. Direct microsurgical repair of intracavernous vascular lesions. J Neurosurg 1983, 58, 824–831. [Google Scholar] [CrossRef]
- Hakuba, A. Direct approaches to vascular lesions in the cavernous sinus via the medial triangle. 1987.
- Rhoton, A.L. The cavernous sinus, the cavernous venous plexus, and the carotid collar. Neurosurgery 2002, 51, S375–410. [Google Scholar] [CrossRef] [PubMed]
- Doglietto, F.; Lauretti, L.; Frank, G.; Pasquini, E.; Fernandez, E.; Tschabitscher, M.; Maira, G. Microscopic and endoscopic extracranial approaches to the cavernous sinus: anatomic study. Neurosurgery 2009, 64, 413–421. [Google Scholar] [CrossRef] [PubMed]
- Chowdhury, F.; Haque, M.; Kawsar, K.; Ara, S.; Mohammod, Q.; Sarker, M.; Goel, A. Transcranial microsurgical and endoscopic endonasal cavernous sinus (CS) anatomy: a cadaveric study. J Neurol Surg A Cent Eur Neurosurg 2012, 73, 296–306. [Google Scholar] [CrossRef]
- Alfieri, A.; Jho, H.D. Endoscopic endonasal approaches to the cavernous sinus: surgical approaches. Neurosurgery 2001, 49, 354–360. [Google Scholar] [CrossRef]
- Alfieri, A.; Jho, H.D. Endoscopic endonasal cavernous sinus surgery: an anatomic study. Neurosurgery 2001, 48, 827–836. [Google Scholar]
- Cavallo, L.M.; Cappabianca, P.; Galzio, R.; Iaconetta, G.; de Divitiis, E.; Tschabitscher, M. Endoscopic transnasal approach to the cavernous sinus versus transcranial route: anatomic study. Neurosurgery 2005, 56, 379–389. [Google Scholar] [CrossRef]
- Dallan, I.; Di Somma, A.; Prats-Galino, A.; Solari, D.; Alobid, I.; Turri-Zanoni, M.; Fiacchini, G.; Castelnuovo, P.; Catapano, G.; de Notaris, M. Endoscopic transorbital route to the cavernous sinus through the meningo-orbital band: a descriptive anatomical study. J Neurosurg 2017, 127, 622–629. [Google Scholar] [CrossRef]
- Santos, C.; Guizzardi, G.; Di Somma, A.; Lopez, P.; Mato, D.; Enseñat, J.; Prats-Galino, A. Comparison of Accessibility to Cavernous Sinus Areas Throughout Endonasal, Transorbital, and Transcranial Approaches: Anatomic Study With Quantitative Analysis. Oper Neurosurg (Hagerstown) 2022. [Google Scholar] [CrossRef] [PubMed]
- Jung, I.H.; Yoo, J.; Choi, S.; Lim, S.H.; Ko, J.; Roh, T.H.; Hong, J.B.; Kim, E.H. Endoscopic transorbital approach to the cavernous sinus: Cadaveric anatomy study and clinical application. Front Oncol 2022, 12, 962598. [Google Scholar] [CrossRef] [PubMed]
- Bouthillier, A.; van Loveren, H.R.; Keller, J.T. Segments of the internal carotid artery: a new classification. Neurosurgery 1996, 38, 425–432. [Google Scholar] [CrossRef] [PubMed]
- Yaşargil, M.G.; Reichman, M.V.; Kubik, S. Preservation of the frontotemporal branch of the facial nerve using the interfascial temporalis flap for pterional craniotomy. Technical article. J Neurosurg 1987, 67, 463–466. [Google Scholar] [CrossRef]
- Oikawa, S.; Mizuno, M.; Muraoka, S.; Kobayashi, S. Retrograde dissection of the temporalis muscle preventing muscle atrophy for pterional craniotomy. Technical note. J Neurosurg 1996, 84, 297–299. [Google Scholar] [CrossRef]
- Zabramski, J.M.; Kiriş, T.; Sankhla, S.K.; Cabiol, J.; Spetzler, R.F. Orbitozygomatic craniotomy. Technical note. J Neurosurg 1998, 89, 336–341. [Google Scholar] [CrossRef]
- Fukuda, H.; Evins, A.I.; Burrell, J.C.; Iwasaki, K.; Stieg, P.E.; Bernardo, A. The Meningo-Orbital Band: Microsurgical Anatomy and Surgical Detachment of the Membranous Structures through a Frontotemporal Craniotomy with Removal of the Anterior Clinoid Process. J Neurol Surg B Skull Base 2014, 75, 125–132. [Google Scholar] [CrossRef]
- Froelich, S.C.; Aziz, K.M.; Levine, N.B.; Theodosopoulos, P.V.; van Loveren, H.R.; Keller, J.T. Refinement of the extradural anterior clinoidectomy: surgical anatomy of the orbitotemporal periosteal fold. Neurosurgery 2007, 61, 179–185. [Google Scholar] [CrossRef]
- Bernardo, A.; Evins, A.I.; Barbagli, G.; Kim, M.G.; Kim, N.; Xia, J.J.; Nonaka, M.; Stieg, P.E. Tailored Surgical Access to the Cavernous Sinus and Parasellar Region: Assessment of Cavernous Sinus Entry Corridors and the Periclinoid and Pericavernous Surgical Maneuvers. World Neurosurg 2022. [Google Scholar] [CrossRef]
- Di Somma, A.; Andaluz, N.; Cavallo, L.M.; Topczewski, T.E.; Frio, F.; Gerardi, R.M.; Pineda, J.; Solari, D.; Enseñat, J.; Prats-Galino, A.; et al. Endoscopic transorbital route to the petrous apex: a feasibility anatomic study. Acta Neurochir (Wien) 2018, 160, 707–720. [Google Scholar] [CrossRef]
- Corrivetti, F.; de Notaris, M.; Di Somma, A.; Dallan, I.; Enseñat, J.; Topczewski, T.; Solari, D.; Cavallo, L.M.; Cappabianca, P.; Prats-Galino, A. "Sagittal Crest": Definition, Stepwise Dissection, and Clinical Implications From a Transorbital Perspective. Oper Neurosurg (Hagerstown) 2022, 22, e206–e212. [Google Scholar] [CrossRef] [PubMed]
- Wanibuchi, M.; Murakami, G.; Yamashita, T.; Minamida, Y.; Fukushima, T.; Friedman, A.H.; Fujimiya, M.; Houkin, K. Midsubtemporal ridge as a predictor of the lateral loop formed by the maxillary nerve and mandibular nerve: a cadaveric morphological study. Neurosurgery 2011, 69, ons95–98. [Google Scholar] [CrossRef] [PubMed]
- López, C.B.; Di Somma, A.; Cepeda, S.; Arrese, I.; Sarabia, R.; Agustín, J.H.; Topczewski, T.E.; Enseñat, J.; Prats-Galino, A. Extradural anterior clinoidectomy through endoscopic transorbital approach: laboratory investigation for surgical perspective. Acta Neurochir (Wien) 2021, 163, 2177–2188. [Google Scholar] [CrossRef]
- Cavallo, L.M.; de Divitiis, O.; Aydin, S.; Messina, A.; Esposito, F.; Iaconetta, G.; Talat, K.; Cappabianca, P.; Tschabitscher, M. Extended endoscopic endonasal transsphenoidal approach to the suprasellar area: anatomic considerations--part 1. Neurosurgery 2008, 62, 1202–1212. [Google Scholar] [CrossRef]
- Corvino, S.; Armocida, D.; Offi, M.; Pennisi, G.; Burattini, B.; Villareal-Mondragon, A.; Esposito, F.; Cavallo, L.; de Notaris, M. The Anterolateral Triangle as Window on The Foramen Lacerum from Transorbital Corridor. Anatomical Study and Technical Nuances 2023. [Google Scholar] [CrossRef]
- Ferrareze Nunes, C.; Lieber, S.; Truong, H.Q.; Zenonos, G.; Wang, E.W.; Snyderman, C.H.; Gardner, P.A.; Fernandez-Miranda, J.C. Endoscopic endonasal transoculomotor triangle approach for adenomas invading the parapeduncular space: surgical anatomy, technical nuances, and case series. J Neurosurg 2018, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Miranda, J.C.; Zwagerman, N.T.; Abhinav, K.; Lieber, S.; Wang, E.W.; Snyderman, C.H.; Gardner, P.A. Cavernous sinus compartments from the endoscopic endonasal approach: anatomical considerations and surgical relevance to adenoma surgery. J Neurosurg 2018, 129, 430–441. [Google Scholar] [CrossRef]
- Almeida, J.P.; de Andrade, E.; Reghin-Neto, M.; Radovanovic, I.; Recinos, P.F.; Kshettry, V.R. From Above and Below: The Microsurgical Anatomy of Endoscopic Endonasal and Transcranial Microsurgical Approaches to the Parasellar Region. World Neurosurg 2022, 159, e139–e160. [Google Scholar] [CrossRef]
- Yasuda, A.; Campero, A.; Martins, C.; Rhoton, A.L.; de Oliveira, E.; Ribas, G.C. Microsurgical anatomy and approaches to the cavernous sinus. Neurosurgery 2005, 56, 4–27. [Google Scholar] [CrossRef]
- Woodworth, G.F.; Patel, K.S.; Shin, B.; Burkhardt, J.K.; Tsiouris, A.J.; McCoul, E.D.; Anand, V.K.; Schwartz, T.H. Surgical outcomes using a medial-to-lateral endonasal endoscopic approach to pituitary adenomas invading the cavernous sinus. J Neurosurg 2014, 120, 1086–1094. [Google Scholar] [CrossRef]
- Lee, M.H.; Hong, S.D.; Woo, K.I.; Kim, Y.D.; Choi, J.W.; Seol, H.J.; Lee, J.I.; Shin, H.J.; Nam, D.H.; Kong, D.S. Endoscopic Endonasal Versus Transorbital Surgery for Middle Cranial Fossa Tumors: Comparison of Clinical Outcomes Based on Surgical Corridors. World Neurosurg 2019, 122, e1491–e1504. [Google Scholar] [CrossRef]
- Komatsu, F.; Komatsu, M.; Inoue, T.; Tschabitscher, M. Endoscopic supraorbital extradural approach to the cavernous sinus: a cadaver study. J Neurosurg 2011, 114, 1331–1337. [Google Scholar] [CrossRef] [PubMed]
- Corvino, S.; Sacco, M.; Somma, T.; al., e. Functional and clinical outcomes after superior eyelid transorbital endoscopic approach for spheno-orbital meningiomas: illustrative case and literature review. 2023.
- Inamasu, J.; Guiot, B.H. Iatrogenic carotid artery injury in neurosurgery. Neurosurg Rev 2005, 28, 239–247. [Google Scholar] [CrossRef] [PubMed]
- AlQahtani, A.; London, N.R.; Castelnuovo, P.; Locatelli, D.; Stamm, A.; Cohen-Gadol, A.A.; Elbosraty, H.; Casiano, R.; Morcos, J.; Pasquini, E.; et al. Assessment of Factors Associated With Internal Carotid Injury in Expanded Endoscopic Endonasal Skull Base Surgery. JAMA Otolaryngol Head Neck Surg 2020, 146, 364–372. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).