1. Introduction
Chemical burns are one of the most important types of burns, due to their destructive nature and ability to generate deep tissue damage, leading to necrosis, extensive scarring, and aesthetic defects. Nitric acid (NA) is a nitrogen oxoacid that is commonly used as a colorless liquid in the manufacture of inorganic and organic nitrates production of inorganic fertilizers, metal cleaners and the manufacture of ammonium nitrate explosives and chemical products [
1]. NA has also been used by podiatrists as a treatment in patients with onychomycosis, a fungal infection of the toenail [
2]. In some countries, unfortunately, NA is used for violent purposes, such as aggressions mainly against young women [
3].
Complex soft tissues defects are usually treated with various techniques including local flaps, full and split-thickness skin grafts. These techniques, however, have their own disadvantages like donor site morbidity and even risk of graft/flap failure [
4]. Acellular dermal matrices have been developed with the purpose of ameliorate organized regeneration of host tissue in different clinical contexts [
5].
Matriderm™ is a highly porous membrane composed of three-dimensionally coupled bovine collagen I,III, V and elastin that provides a scaffold to restore the skin and modulates scar formation. It can be used on a one-step procedure (depending on the thickness of the acellular dermal matrix) with a skin graft to cover defects and reduce graft loss risks [
6].
Currently, there are no reports of Matriderm™ use on chemical burns defects. Thus, we present a case of an unusual chemical burn etiology on a complex reconstructive area treated with an acellular dermal matrix (Matriderm™) and a split-thickness skin graft combined with negative wound pressure therapy.
2. Case Presentation
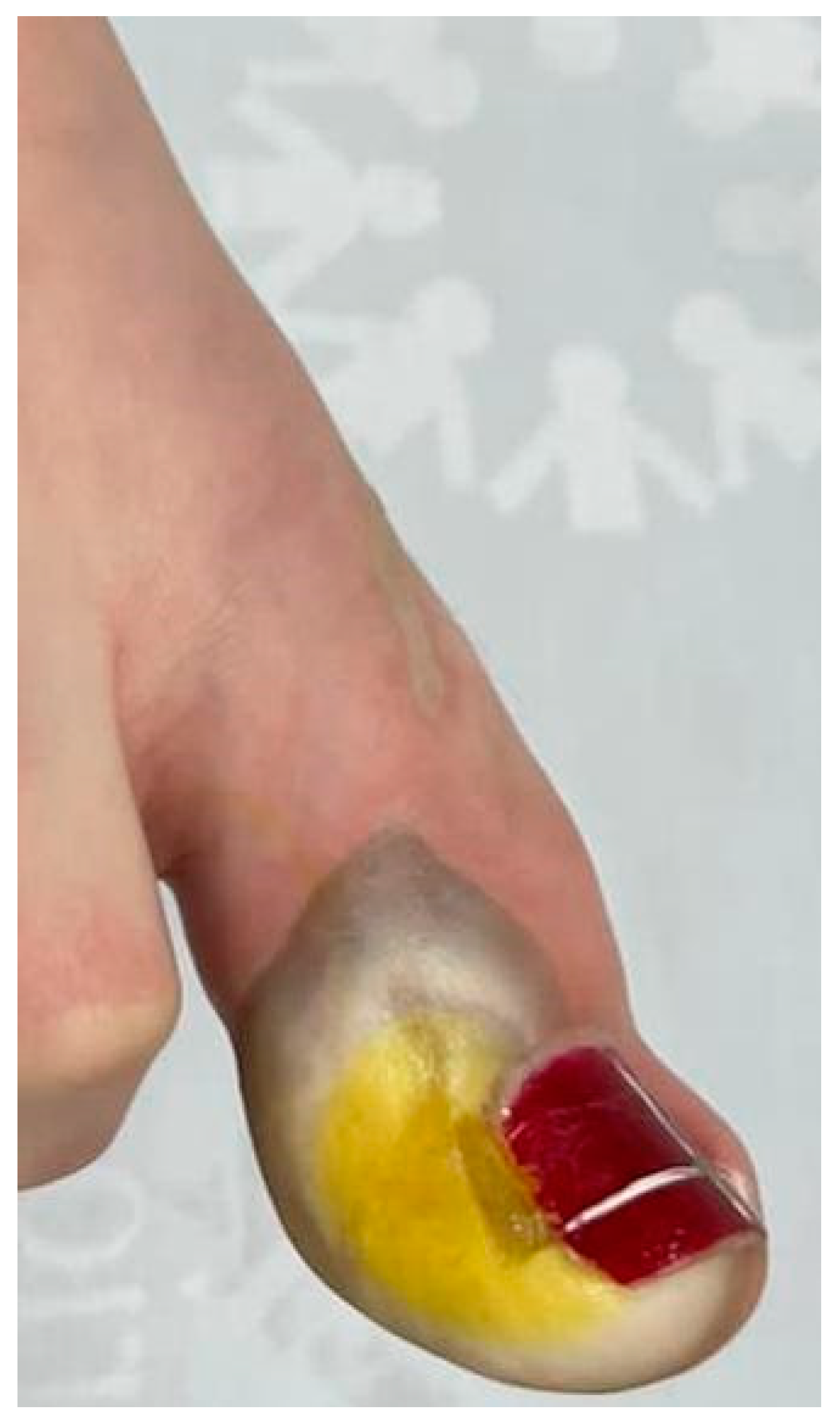
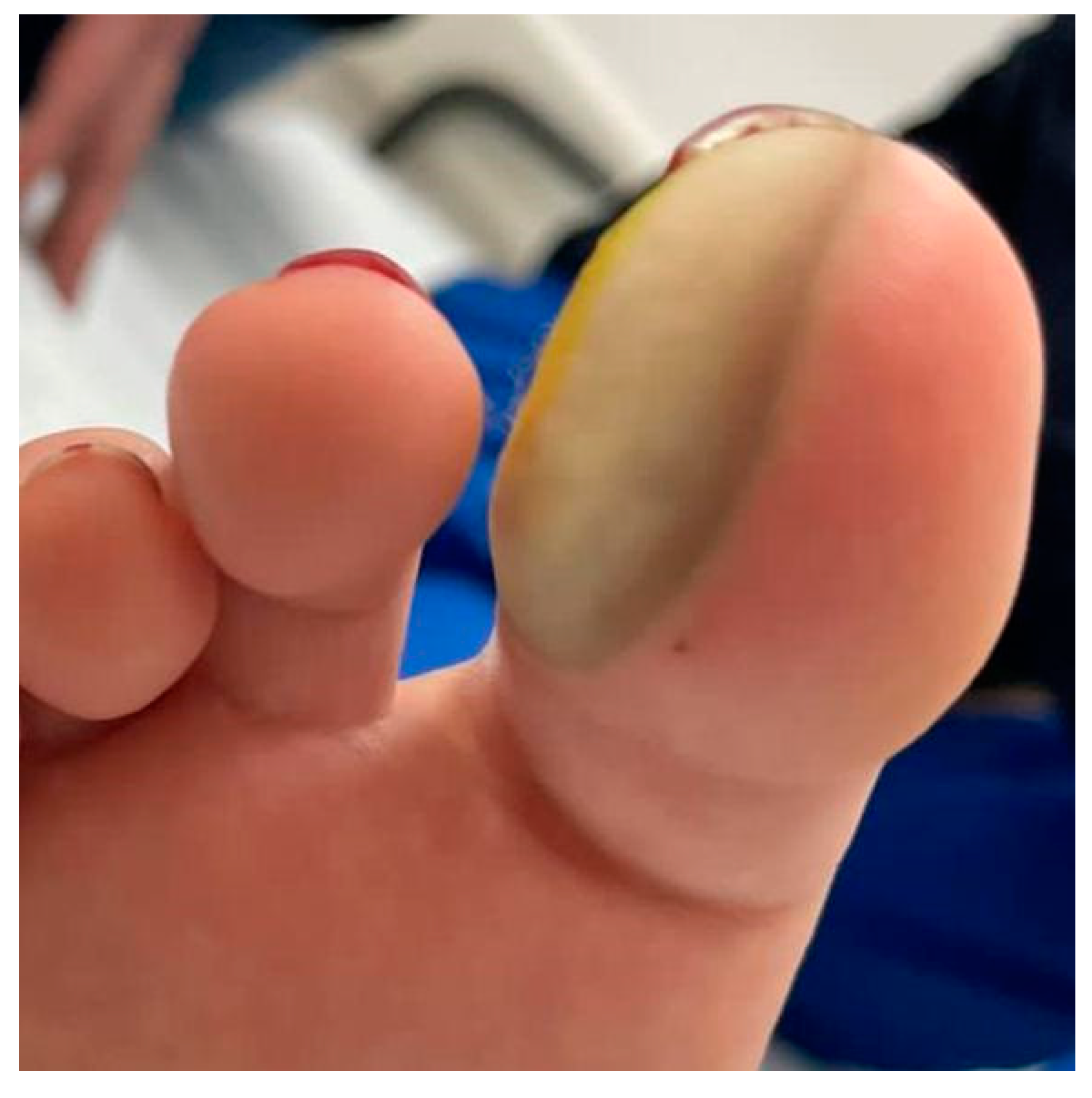
A 16-year-old woman presented to the Emergency Room with pain and color changes in the right hallux nail and skin after professedly had been injected lidocaine prior to an onychectomy 5 hours before (
Figure 1, 2). The patient was initially evaluated by pediatrics, hematology, and vascular surgery under suspicion of digital artery thrombosis
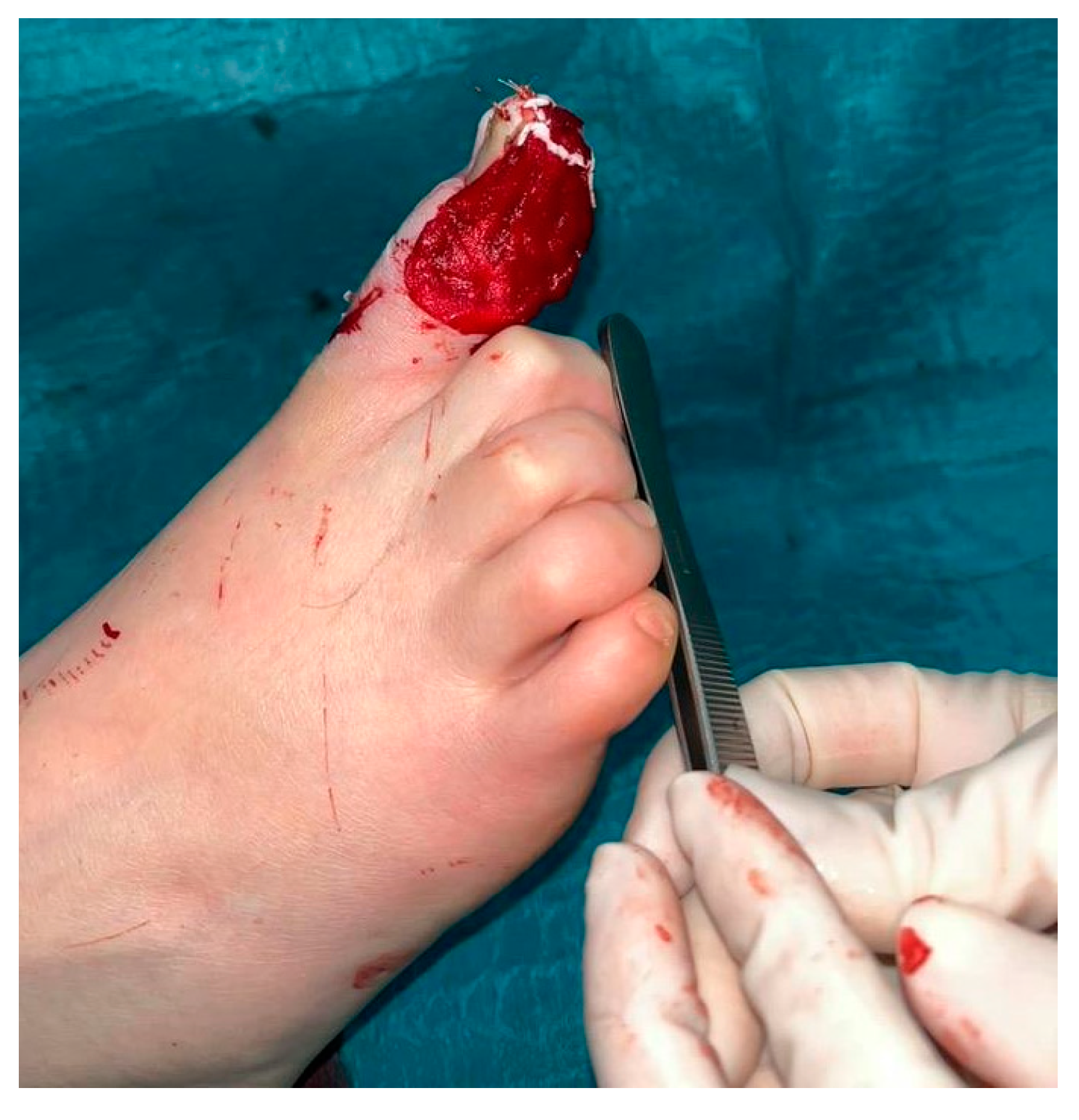
. However, 12 hours after the paraclinical results, the clinical picture was not very consistent, so the doctor who injected the anesthetic was re-questioned. The podiatrist admitted that accidentally he injected nitric acid at an unknown concentration, thus, the patient was then evaluated by a plastic surgeon who diagnosed a chemical burn hence, the patient was taken immediately to the operating room for an early wound debridement (36 hours after the injection of the chemical) (
Figure 3, 4). The patient presented with a third degree burn that compromised the medial aspect of the hallux’s skin, the distal phalanx and nail bed. Negative Pressure Wound Therapy (NPWT VAC, 3M, US) with a pressure of -125 mmHg in a continuous mode was used to improve tissue’s viability. 48 hours after the first surgery, the patient was taken to the OR again, granulation tissue started to grow, but the distal phalanx of the hallux had necrosis and was completely exposed, therefore, a new debridement which included also cutting of the necrotic portion of the phalanx was performed. Eight days after the first surgery the remaining tissue was vital and the burn injury was auto-limitated, however, the phalanx was still exposed, thus Matriderm™ (MatriDerm® MedSkin Solution Dr. Suwelack AG, Billerbeck, Germany) dermal substitute and a split-thickness skin graft were used to cover the defect and bolstered with negative pressure wound therapy NPWT Granufoam Silver with a continuous pressure of -125mmHg (
Figure 5, 6). The patient had an adequate recovery, a complete coverage of the lesion, and was discharged for outpatient follow-up (
Figure 7,
Figure 8,
Figure 9).
3. Discussion
Although chemical burns represent only a small number of all type of burns that are seen in medical practice, they are potentially life-threatening with serious aesthetic and functional consequences and count for up to 30% of all deaths from burns. Given the sociodemographic context of chemical burns related to aggression and unprompted violent attacks, the accurate management instated for these types of burns is essential in medical practice. Chemical burns are caused by corrosive agents like acids or alkali leading to extensive tissue damage [
7]. The complete management of these burns is of vital importance to achieve a successful recovery and management. Furthermore, great toe defects represent a challenge to the plastic surgeon, where loss of tissue and bone over the fingertip leaves a deformed and shortened toe [
8].
Full skin defects are related to an increased risk of infection, necrosis, and loss of further tissue. Wound healing is a process that proceeds gradually and ultimately aims to recover the skin barrier. Reconstruction of the dermis plays an important role in the recovery of wounds. In the end, full thickness skin grafts are generally regarded as the mainstay standard of treatment. However, the limitations regarding the undesirable outcomes of scars and hypertrophic scarring, poor elasticity, and limitations in joint movement due to contractures could be a turning point in the standard of practice for these types of patients, additionally, when there is bone exposure a skin graft is not an option [
6].
In this case, the use of NA initiated a prothrombotic process with third degree burns that created a full thickness skin defect in the hallux and in the nail bed. The use of a dermal substitute reconstructed the defect with an adequate range of movement in the hallux and metatarsal joint. The use of Matriderm™ could be instated in the treatment of third-degree acute chemical burns in areas where there are limited reconstructive options. During the acute phase of burn treatment, dermal substitutes reconstruct defects with adequate functional and cosmetic long-term results increasing the patients´ quality of life . In the setting of chronic wounds, dermal substitutes are used to reconstruct and improve burn scars and other defects [
4].
The effective dermal replacement in special areas is prioritized in these burns given the fact that dermal tissue will not regenerate into normal dermis in vivo after full thickness dermal injuries. Application of a dermal substitute underneath the autologous skin graft may improve the wound healing process since the thickness of the dermal component contributes to prevent increased secondary wound contraction [5-6]. Nonetheless, there are reports that the substitute might affect the graft take when the reconstruction is performed in one surgical time. The explanation is that the acellular dermal matrix may act as a barrier for vascular ingrowth and may danger the diffusion of nutrients to the graft secondary to the increased distance between the wound bed and the graft [
9]. In a burn patient, the risk of graft´s loss is increased because of the distribute shock where the intravascular volume depletion with increased tissue edema and increased systemic vascular resistance affects the tissue perfusion. As explained above, vascular ingrowth and populating the matrix with host fibroblasts is central to the successful incorporation. NPWT has been employed to support and accelerate this process [
10]. The negative pressure wound therapy helps to bolster the acellular dermal matrix, to decrease edema by draining the excess of fluid, to increase local perfusion and to stimulate neoangiogenesis. Molnar [
11] described the acceleration of matrix incorporation with the use of negative pressure wound therapy. In this patient, the use of Negative Pressure Wound Therapy (NPWT VAC, 3M, US) promoted neovascularization and take of the dermal substitute in a short time, sterile protection of the wound and provided a bolster for the acellular dermal matrix as well as the skin graft. The use of negative pressure wound therapy in burn patients is common, given the fact that it improves skin graft take. In a study developed by Petkar [
12], he concluded that negative pressure dressing improves graft take in burn patients and can particularly be contemplated when the conditions of the wound bed are less-than-ideal. For this patient the use of an acellular dermal matrix combined with negative pressure wound therapy assisted in an overall better recovery and improvement of quality of life.
Reconstructing the hallux using flaps can be a challenging procedure due to the complex anatomy and functional requirements of the big toe. Flap reconstruction involves transferring healthy tissue from a donor site to replace damaged or missing tissue in the recipient site.
Several factors contribute to the complexity of hallux reconstruction. These include the need to restore weight-bearing function, preservation of sensory innervation, and achieving an aesthetic outcome. Additionally, maintaining proper alignment and stability of the joint is crucial to ensure proper foot biomechanics.
Regional flaps, such as the dorsalis pedis flap, can be utilized when a larger defect requires a flap with a wider reach. This type of flap involves transferring tissue from a nearby region, such as the foot or ankle, to reconstruct the hallux.
In more complex cases, distant flaps may be necessary. Distant flaps involve transferring tissue from a distant site, such as the groin or forearm, to reconstruct the hallux. These flaps provide a greater amount of tissue for reconstruction but require longer operative times and may involve microvascular anastomosis.
To the best of our knowledge, this is the first paper that directly correlates the use of a dermal substitute and negative pressure wound therapy in the management of a chemical burn in the acute phase. This was a challenging case since the injury was in a very distal and difficult area with limited reconstructive options and bone exposure. Furthermore, chemical burns by themselves are also challenging because the injury continuous to progress until the entire chemical is extracted from the tissues and, in this case, the chemical was injected with depth engagement worsening. The amputation was a possibility in this patient which depended on the progression of the chemical burn and the limited reconstructive options. Fortunately, an early debridement of the necrotic tissue with applied technology such as negative pressure wound therapy helped to limit the progression of the burn and to prepare the wound bed for definite reconstruction [
13]. In the reconstructive phase, the use of acellular dermal matrix to cover a defect with bone exposure decreases the need for complex reconstructive procedures with secondary donor areas which could increase the comorbidity of the procedure. Once again, in this reconstructive phase the negative pressure wound therapy helped to bolster the acellular dermal matrix as well as the graft with an adequate graft take after 7 days. This case report, in conclusion, illustrates a viable reconstruction approach for a challenging area to manage, such as the hallux.
4. Conclusions
Chemical burns are frequent and pose high physical and psychological implications for patients and high costs of treatment. These types of burns can often lead to complex defects where multiple surgical procedures must be done to minimize the potential of a severe deformation. Novel solutions for the management of this type of lesions are available such as acellular dermal matrices and negative pressure wound therapy, the combination of these therapies proved to be highly efficient in this case report. One important advantage of the chosen reconstructive options is that we avoided complex donor areas and complex surgical procedures that could increase the complications during the postoperative follow up time. The functional and cosmetic results were adequate from the patient´s and the surgeon´s view.
In the case of current bioengineered skin substitutes, to date, there is none that replace the skin in its entirety. Objectively proving that they can improve cutaneous scars in comparison to the use of split-thickness grafts alone is one of the milestones that remains to be achieved. Awareness of the importance on the management of chemical burns among the medical community is needed to promote research on the use of these type of solutions in a more controlled and experimental environment.
Author Contributions
Viviana Gomez: Plastic surgeon in charge of the case; brought the idea for the case report; manuscript reviewing and editing. David Camacho: Manuscript writing, literature review. Ana Camargo: Manuscript writing, literature review. Cesar Cardona: Manuscript writing, literature review.
Funding
This research received no external funding.
Institutional Review Board Statement
The case report was approved by the Institutional Ethics Committee of FUNDACION SANTA FE DE BOGOTA.
Informed Consent Statement
Informed consent was obtained from the patient involved in the report.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Kolios L, Striepling E, Kolios G, Rudolf KD, Dresing K, Dörges J, Stürmer KM, Stürmer EK. The nitric acid burn trauma of the skin. J Plast Reconstr Aesthet Surg. 2010 Apr;63(4):e358-63. [CrossRef] [PubMed]
- Marcos-Tejedor, F.; Santos-Carnicero, N.; Mayordomo, R. Preliminary Evidence of the Efficacy of Nitric Acid Treatment in Onychomycosis. International Journal of Environmental Research and Public Health 2021, 18, 13371. [CrossRef]
- Gaviria-Castellanos, J.L., V. Gómez-Ortega, and P. Gutiérrez. “Quemaduras Químicas Por Agresión: Características e Incidencia Recogidas En El Hospital Simón Bolívar, Bogotá, Colombia.” Cirugía Plástica Ibero-Latinoamericana 41, no. 1 (March 2015): 73–82. [CrossRef]
- Janis, J.E.; Nahabedian, M.Y. Acellular Dermal Matrices in Surgery. Plastic and Reconstructive Surgery 2012, 130, 7S-8S. [CrossRef]
- Petrie, K.; Cox, C.T.; Becker, B.C.; MacKay, B.J. Clinical Applications of Acellular Dermal Matrices: A Review. Scars, Burns & Healing 2022, 8, 205951312110383. [CrossRef]
- Min, J.H.; Yun, I.S.; Lew, D.H.; Roh, T.S.; Lee, W.J. The Use of Matriderm and Autologous Skin Graft in the Treatment of Full Thickness Skin Defects. Archives of Plastic Surgery 2014, 41, 330–336. [CrossRef]
- Walsh, K.; Hughes, I.; Dheansa, B. Management of Chemical Burns. British Journal of Hospital Medicine 2022, 83, 1–12. [CrossRef]
- Sahin, C.; Karagoz, H.; Sever, C.; Kulahci, Y.; Ulkur, E. Reconstruction of the Great Toe Tip Defect with a Pedicled Heterodigital Artery Flap. Aesthetic Plastic Surgery 2013, 37, 421–423. [CrossRef]
- Ryssel H, Gazyakan E, Germann G, Ohlbauer M. The use of MatriDerm in early excision and simultaneous autologous skin grafting in burns--a pilot study. Burns. 2008 Feb;34(1):93-7. [CrossRef] [PubMed]
- Menn ZK, Lee E, Klebuc MJ. Acellular dermal matrix and negative pressure wound therapy: a tissue-engineered alternative to free tissue transfer in the compromised host. J Reconstr Microsurg. 2012 Feb;28(2):139-44. [CrossRef] [PubMed]
- Molnar JA, DeFranzo AJ, Hadaegh A, Morykwas MJ, Shen P, Argenta LC. Acceleration of Integra incorporation in complex tissue defects with subatmospheric pressure. Plast Reconstr Surg. 2004 Apr 15;113(5):1339-46. [CrossRef] [PubMed]
- Petkar KS, Dhanraj P, Kingsly PM, Sreekar H, Lakshmanarao A, Lamba S, Shetty R, Zachariah JR. A prospective randomized controlled trial comparing negative pressure dressing and conventional dressing methods on split-thickness skin grafts in burned patients. Burns. 2011 Sep;37(6):925-9. [CrossRef] [PubMed]
- Ardila MP, Gómez-Ortega V. Negative Pressure Wound Therapy as an Artificial Leech to Save a Congestive Flap: Case Report. Plast Reconstr Surg Glob Open. 2022 Mar 7;10(3):e4162. [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).