1. Introduction
A recent United Nations (UN) report revealed that nearly half of the world’s population does not have access to crucial healthcare services [
1]. This is largely due to over 800 million individuals allocating less than 10% of their household budget toward health expenses. As a result, millions of people worldwide are facing significant challenges and are unable to afford necessary healthcare services [
2]. The World Health Organization (WHO) Director-General has urged leaders and policymakers, particularly those from developing countries, to embrace eHealth to improve healthcare. By integrating digital health services, access to and quality of health service delivery can be enhanced, ultimately contributing to the achievement of the United Nations Sustainable Development Goals [
3,
4]. This manuscript is a revised and extended version of a paper originally published in the IOS SHTI pHealth 2022 Proceedings [
5].
eHealth utilizes digital technologies, such as information and communication technologies (ICTs) and data, to provide healthcare services [
6,
7] that encompass physical and psychological diagnosis and treatment, telepathology, vital signs monitoring, electronic prescribing, and teleconsultation [
8]. The literature has extensively documented the benefits of integrating eHealth in healthcare, such as improving healthcare delivery, efficacy, and quality of care [
9]. eHealth applications are considered a potential "game changer" that could improve access to affordable and effective healthcare services [
10,
11]. In addition, eHealth services could improve patients’ knowledge and behavior related to their health, aid in the exchange of information between healthcare providers and patients and increase coordination and consistency of care. This can result in a reduction in the cost of delivering health services [
11]. These applications have the potential to revolutionize healthcare workflows and aid in achieving Universal Health Coverage (UHC) in the long run [
12,
13].
Factors that Influence the Integration and Use of eHealth
The achievement of Universal Health Coverage largely depends on making healthcare accessible and affordable to everyone without financial barriers [
3]. eHealth application have been identified as crucial enablers of UHC, but their integration and widespread use are limited, mainly in developing countries where they are most needed [
14]. This is because of several factors, such as the high cost of IT infrastructure and a shortage of skilled personnel to adopt eHealth [
15]. A study on integrating eHealth in Tanzania found that inadequate ICT skills, high cost of ICT, under-developed IT infrastructure, and a lack of information about appropriate ICT solutions were major obstacles [
16]. While eHealth services can improve healthcare quality, factors such as insufficient budget for ICT infrastructure, security, privacy, and confidentiality concerns can hinder their integration [
17]. According to a study conducted in Cameroon, implementing a digital information system faces challenges due to centralized structures that hinder the allocation of funds for ICT equipment, especially in lower levels of the health system [
18]. According to Mars & Scott [
19], LMIC governments have limited financial resources, resulting in cautious spending on health activities. Adebesin et al. [
21] also pointed out that the lack of interoperability of Health Information systems (HIS) hinders eHealth integration. A survey on eHealth adoption in Africa showed that there is limited participation in the development of eHealth standards beyond the requirements of the International Organization for Standardization. Stiawan [
22] emphasized that the lack of information systems to exchange and share data and information among government agencies is a significant obstacle to eHealth integration. Similarly, Sluijs and colleagues [
23] observed that the absence of standards is preventing government institutions, such as hospitals, from meeting their objectives. In the hospital, the data and information needed by health personnel, such as population data, data on health insurance, and patients’ health records, are often housed in separate systems and managed by different government departments, making interoperability crucial. S. Masud et al. [
24] emphasized the importance of standardizing data and information format to achieve interoperability.
Issues with eHealth policies [
25] and leadership [
26] within the public sector have been identified as areas of concern in LMICs. Poor coordination among government departments and inadequate policies make it challenging to integrate eHealth initiatives, according to Luna et al. [
27]. In a study assessing eHealth policies in four African countries, authors noted that strategic goals were vague and lacked consolidated plans [
28]. According to Mburu et al. [
26] poor leadership in the government can impede the management of eHealth projects at the national level. Additionally, developing long-term strategies can be challenging in unstable political environments. However, the political will to embrace eHealth is growing in Sub-Saharan Africa, with the Africa Union and WHO working with LMIC governments to harmonize eHealth activities on the continent, according to Mars [
19].
Several areas of concern hinder the successful integration and use of eHealth services in healthcare. These include the lack of computer equipment and skills, poor internet connection, health workers’ resistance to technology, and unstable electricity supply [
10,
29]. Studies have found that healthcare workers may be reluctant to participate in eHealth activities due to a lack of skills and knowledge in utilizing eHealth applications. This can lead to a negative attitude towards information technologies, resulting in denial and aversion towards their use [
30,
31,
32]. This issue has been identified in Pakistan, where doctor’s low internet usage is attributed to a lack of basic IT skills. In LMIC, insufficient human resource remains a significant threat to the successful integration and use eHealth services [
33]. In addition, current eHealth capacity-building activities for IT professionals are inadequate. Studies have shown that the shortage of qualified health professionals is a chronic problem, and that adequate skills and knowledge are crucial for health personnel to use eHealth services effectively. Healthcare professionals face daily struggles in keeping up with technical developments in the constantly evolving eHealth environment if they lack essential skills [
34,
35,
36,
37].
Research conducted in LMICs suggests that enhancing the ICT skills of health personnel through education and training is crucial [
9,
38]. Previous studies have mainly concentrated on the accessibility of human resources and user-friendliness, instead of the capabilities and proficiencies of healthcare staff in eHealth across Africa and LMICs. While these studies are informative, they pose a challenge for policymakers in terms of comprehending, evaluating, and addressing the obstacles. Our review has revealed a lack of publications discussing capacity-building efforts among health personnel, emphasizing the significance of this study.
2. Objectives
This study delves into the challenges that hinder capacity-building initiatives among healthcare personnel in developing countries and suggests interventions to address them. Through an online survey, empirical data was collected for capacity-building activities in Africa. It is crucial to develop the capacity of healthcare personnel in eHealth because a well-trained workforce in this area can improve health systems delivery [
39]. The study’s findings will serve as a guide for providing health-related information and resources to BETTERHEALTH members and other organizations and as a roadmap for addressing and overcoming barriers.
3. Methods
This study utilized a descriptive design and collected data through an online survey created with Google Forms. The survey was sent to project leaders from the four BETTEHReHEALTH hubs [Ghana (Western region), Malawi (Southern), Ethiopia (Central & Eastern), and Tunisia (Northern)] via email invitations that included a brief explanation of the survey, informed consent, and a link to participate. These leaders then forwarded the survey to eHealth organizations/institutions in their respective hubs.
The survey questions were written in English and were available for participation for two months, with three follow-up requests sent every two weeks. Responses were collected in an Excel spreadsheet and all metadata was removed to ensure anonymity. Ethical clearance for this study was granted as part of a larger BETTEHReHEALTH project. A total of 37 organizations/institutions from 13 countries responded, with one excluded from analysis for not indicating their country. The survey was divided into three sections covering eHealth capacity building activities, factors hindering eHealth capacity building, and open-ended questions for proposed suggestions to build IT skills.
The data collected was run through SPSS statistical software and analyzed via frequency analysis. Additionally, four managers were randomly chosen and informally interviewed to gain understanding of eHealth capacity-building activities within their organizations. These interviews were analyzed using content analysis, which entails identifying and categorizing themes within textual data. Commentaries from the interviews were also analyzed via this method, and the results were reinforced by quotes from the interviews. It’s important to note, however, that the survey results are only indicative of their respective organizations and cannot be applied to the wider population.
4. Findings
4.1. Characteristics of the respondents
The survey received responses from 37 organizations across 13 countries. The BETTEHReHEALTH project operates in four geographical regions, namely Western Ghana, Southern Malawi, Northern Tunisia, and Central and Eastern Ethiopia, with one hub in each. To determine the number of responses per hub, we divided the total responses among the regional hubs. The Southern region generated the highest number of responses, while the Northern and Western regions had the least number of responses. Refer to
Table 1 for more details.
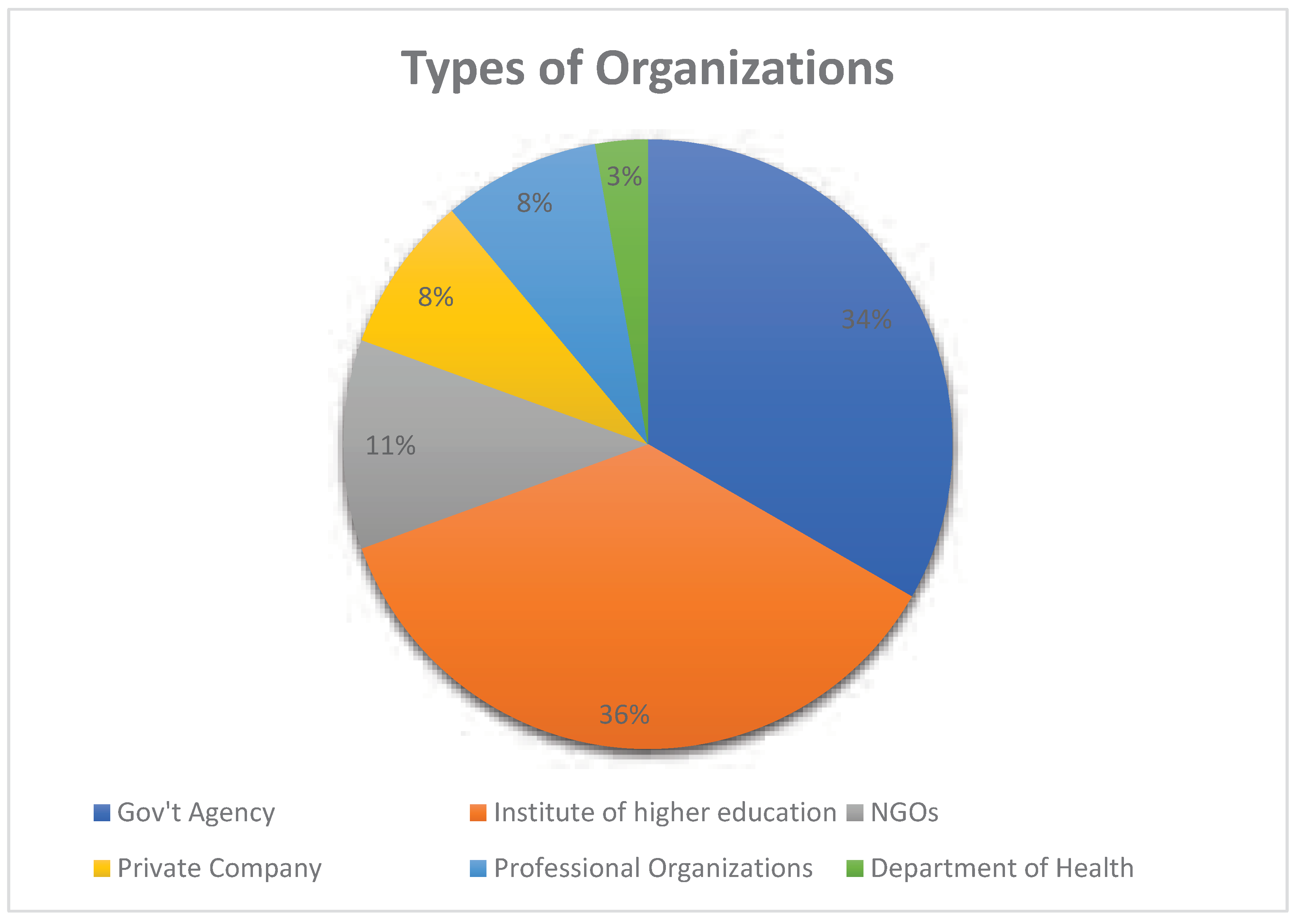
After analyzing the responses, they were sorted based on the types of organizations. The findings reveal that 36% (13) were institutes of higher education, 34% (12) were government agencies, and 11% (4) were NGOs. Refer to
Figure 1 for a visual representation.
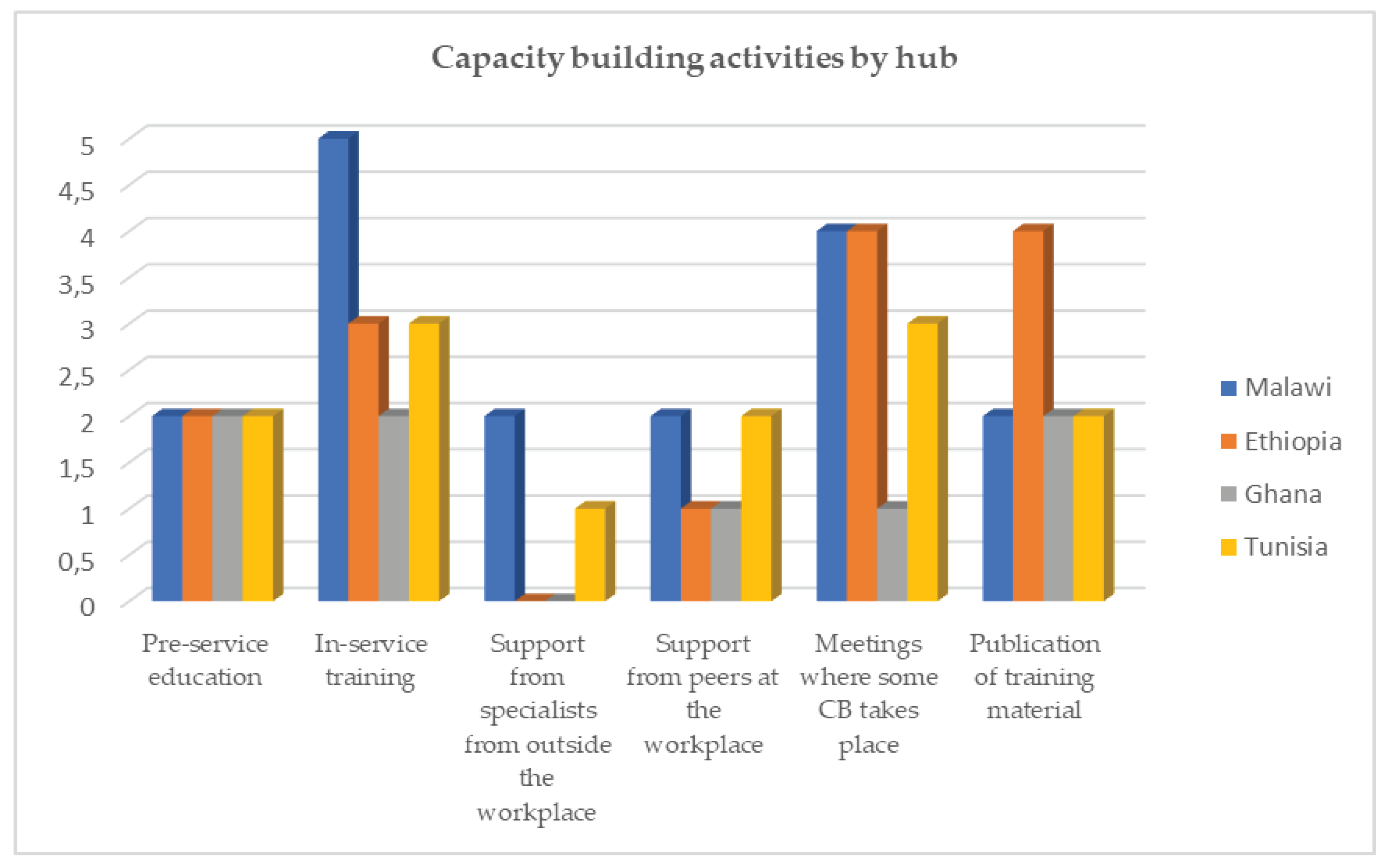
4.2. Capacity building activities
Through our evaluation of capacity-building activities, we have found that organizations engage in several types of these activities. These can include pre-education, in-service training, and support from external specialists, among other options. Although pre-education and in-service training were the most prevalent activities, we observed that "support from specialists outside the organization" was the least employed activity, as shown in
Figure 2. We asked the participants why this activity was not widely used, and one manager explained that it involves hiring a specialist, which has financial implications that most organizations cannot afford.
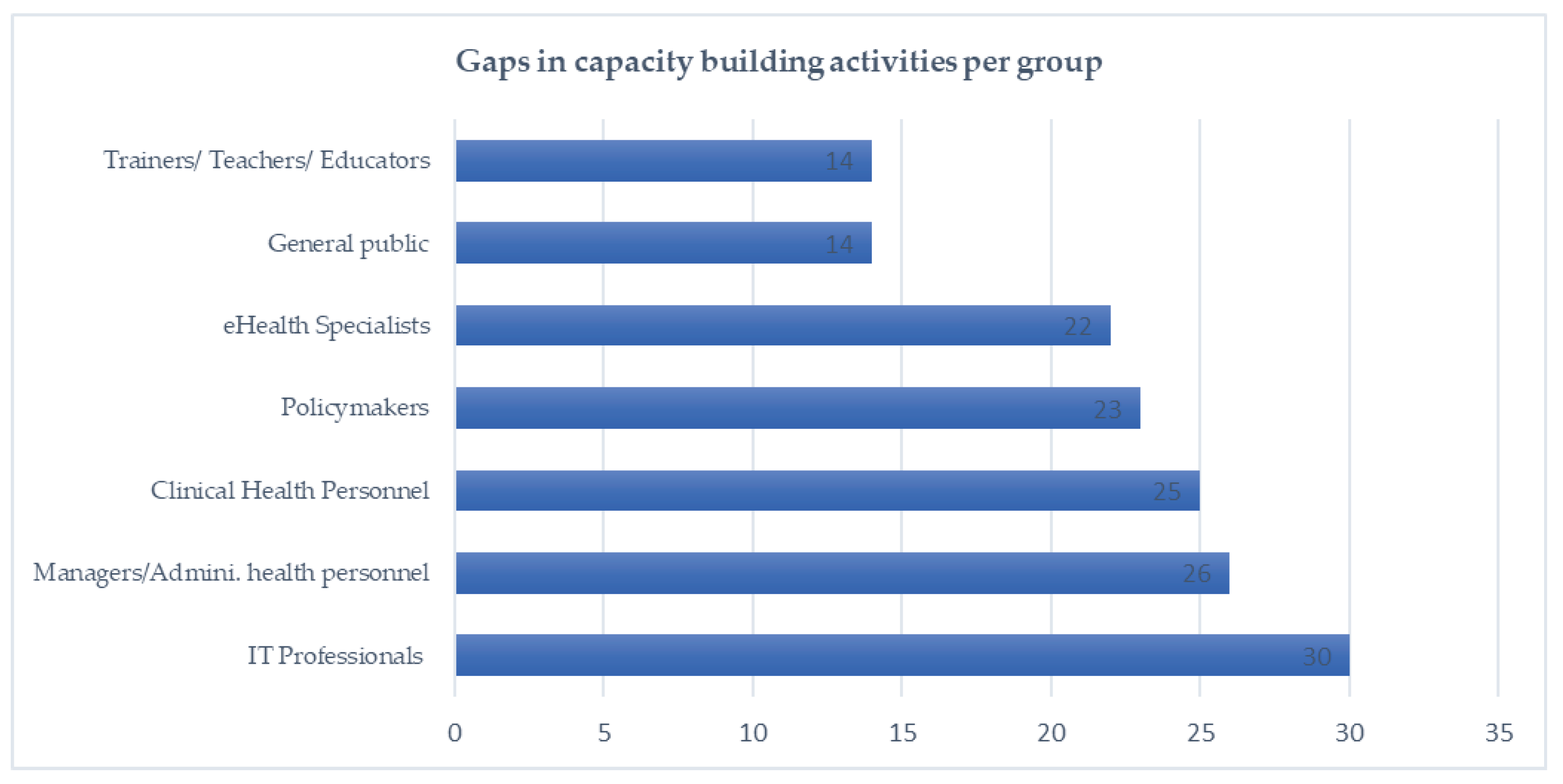
Gaps in capacity building activities
Though the organizations surveyed had different capacity-building activities, our survey observed some gaps. For instance, the current capacity-building programs do not cater to IT professionals, manager/administrative health personnel, eHealth specialists, and policymakers as shown in
Figure 3.
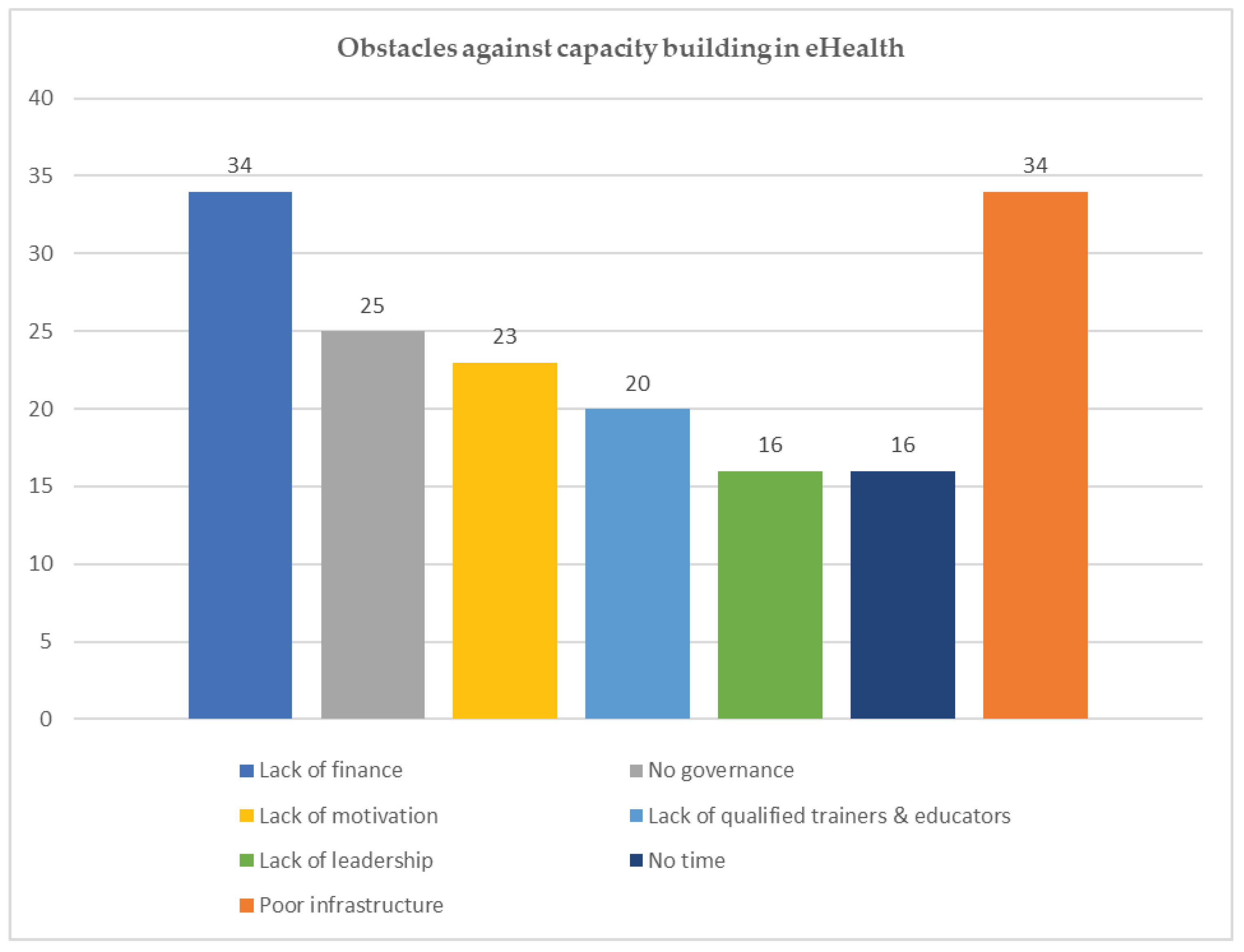
4.3. Factors impeding eHealth capacity-building activities
The importance of having digital skills is widely recognized, but our survey revealed that there are several challenges that hinder eHealth capacity-building efforts, as illustrated in
Figure 4. Specifically, we found that inadequate infrastructure and insufficient financial support were the primary obstacles, as shown in
Figure 4.
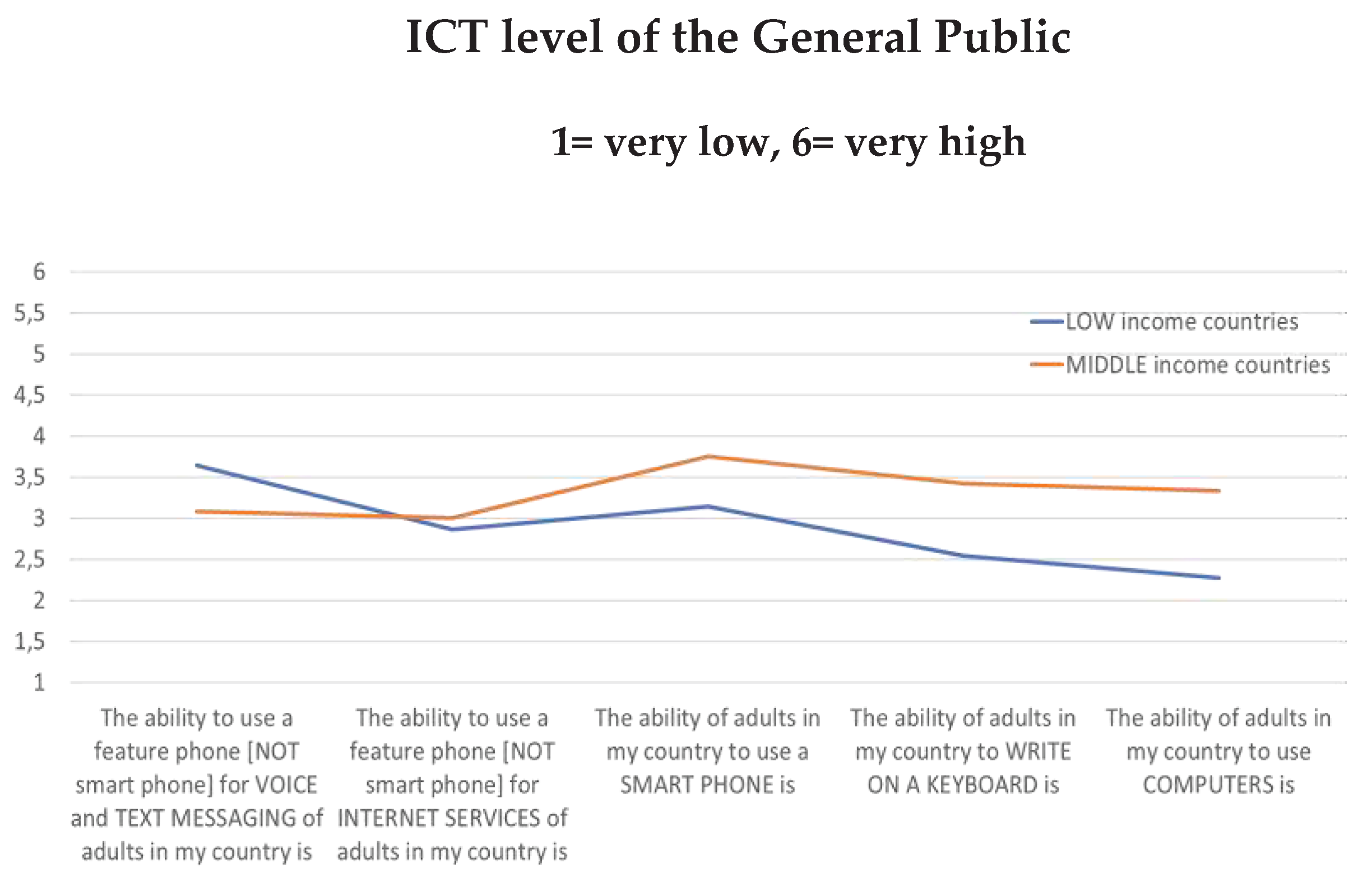
Health Workers’ IT Literacy
Regardless of their profession or level of digital expertise, it is widely agreed that possessing eHealth skills will greatly impact an individual’s career. IT skills were found to be the most valuable digital skills in a recent survey. We analyzed the data according to the income levels of various countries. Our findings indicate that a greater number of individuals in LMICs have access to and use smartphones as compared to computers. As a result, more people are becoming proficient in using smartphones, as depicted in
Figure 5.
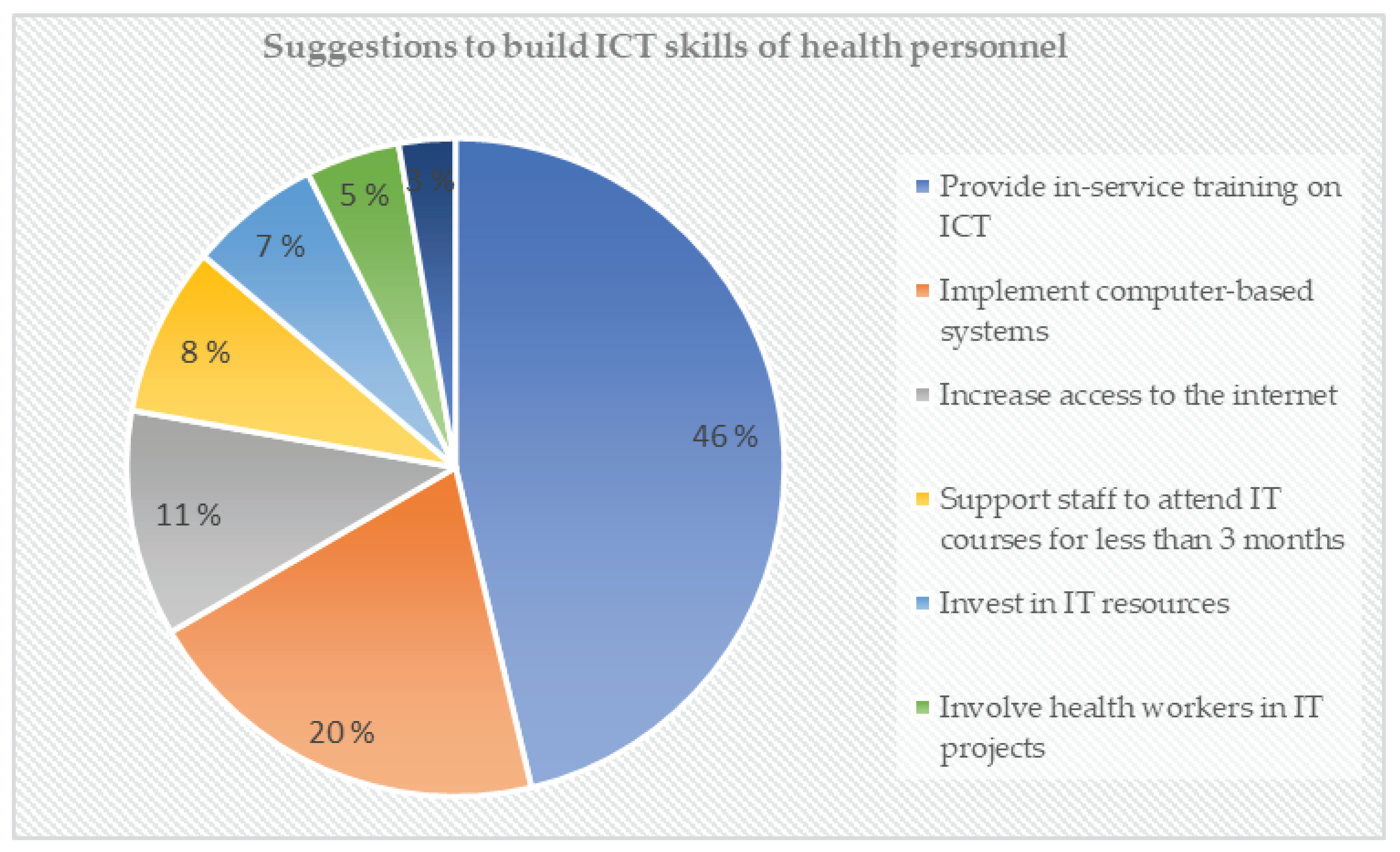
4.4. Suggestions to Build ICT Skills of health personnel
After analyzing the interviews, the most common suggestions were to provide in-service training on ICT, introduce computer-based systems, and improve Internet access. One respondent emphasized the significance of providing healthcare workers with digital skills and visual presentation training, while another stressed the need for more training activities in the eHealth field. For more recommendations, please see
Figure 6.
5. Discussion
The purpose of the study was to explore the challenges that health workers in the BETTEReHEALTH community face in creating initiatives for developing eHealth capabilities. The study showed that there are several barriers hindering capacity-building programs, which may be due to the absence of adequate eHealth policies regarding capacity building [
20]. Policies play a critical role in achieving agreement on eHealth goals and prioritizing initiatives [
40]. However, the research found that eHealth policies in LMICs are broad and do not clearly define the roles and responsibilities of various stakeholders.
For instance, the absence of adequate eHealth policies in Ethiopia and Ghana has resulted in the government and research communities adopting disparate approaches to the implementation of mHealth infrastructure [
41]. It is important for policymakers to proactively develop policies that enable the efficient planning and implementation of eHealth programs. This will ensure their smooth and reliable execution[
42].
Our survey revealed that there are several types of eHealth trainings available. However, the number of training activities available for policymakers, IT professionals, and managers is very limited. This aligns with a previous study conducted by [
35] which emphasized the need for continuous and practical capacity building for IT specialists and professionals. Our recent online survey discovered various obstacles that hinder capacity-building activities. These obstacles stem from different factors, ranging from macro-level systemic issues like insufficient infrastructure, low budget, weak government policies, and poor governance at the national level, to micro-level individual barriers like lack of time, skills, and motivation. These findings align with those of other researchers who emphasize the critical role of national eHealth policies in bridging the gaps in eHealth activities [
19,
20,
33,
42,
43]. It’s worth noting that while having enough finance is crucial in developing infrastructure, paying for technological tools, training workshops, and hiring qualified personnel, in order to achieve optimal results, proper policies, unwavering political dedication, and effective leadership are necessary when utilizing this resource [
36].
Our survey found that individuals in rural areas who have access to smartphones and other technologies tend to develop more IT skills compared to their skills in using computers and keyboards. These findings align with previous studies that suggest high mobile service penetration can aid healthcare efforts in areas with limited resources [
44]. Respondents also recommended improving staff IT skills. However, there appears to be a discrepancy between the suggestions for building health personnel’s ICT skills in section 4.6 and the factors influencing eHealth capacity building in section 4.3. The skills and knowledge of health personnel are vital because without them, eHealth tools are not effectively utilized. The American Medical Informatics Association has suggested a thorough solution to address proficiency deficiencies by incorporating digital skills training into the early stages of students’ education. The training should be obligatory and integrated into the existing educational curriculum.
To improve the capacity of future eHealth professionals, a partnership was established with five universities - Eduardo Mondlane in Mozambique, University of the Western Cape in South Africa, University of Dar Es Salaam in Tanzania, University of Malawi, and University of Gondar in Ethiopia, through the DEDICATED project (HISP Centre & Department of Informatics) [
45]. They have designed ten eHealth modules, which will be taught to both under and post-graduate students at these universities. Research has shown that local capacity-building initiatives are effective strategies to develop skilled human resources [
9,
46]. Therefore, existing educational curricula for health personnel should focus more on training eHealth skills. However, training alone cannot succeed without strong eHealth policies and committed leaders.
6. Conclusions
The healthcare industry is dynamic and demands competent professionals who can adapt to its ever-changing requirement. However, in order to fully utilize eHealth education and training services, there must be sufficient funding, infrastructure, leadership, governance, and a pool of qualified human resources at the national level. Despite the potential benefits of integrating eHealth services, LMICs face numerous obstacles. Our study highlights the importance of versatile capacity-building programs that cater to the diverse needs of health personnel and adapt to the local context. This research contributes to the conversation on promoting innovation and building eHealth capacity among public health and healthcare professionals. However, it is important to note that our study had a limited sample size of 37 respondents from 15 African countries. Future studies should aim to increase the sample size for more comprehensive results. Nevertheless, our findings are consistent with previous research.
Author Contributions
J.K.; developed the survey and collected the data; F.N.A.; analyzed the data, writing – original draft preparation; J, K., F.N.A; writing -review and editing. All authors have read and agree to the published version of the manuscript.
Funding
The project was funded by the European Union’s Horizon 2020 program under grant agreement No 101017450 (
https://betterehealth.eu/).
Informed Consent Statement
Informed consent from the participants was obtained by BETTEReHEALTH regional hub managers from the various hubs as part of the project.
Acknowledgement
We are grateful to the BETTEReHEALTH Consortium members and partners who participated in the online survey.
Conflict of Interest
None.
References
- Labrique, A.B.; Wadhwani, C.; Williams, K.A.; Lamptey, P.; Hesp, C.; Luk, R.; Aerts, A. Best practices in scaling digital health in low and middle income countries. Glob. Health 2018, 14, 1–8. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Fifty-eighth World Health Assembly, Geneva, 16-25 may 2005: resolutions and decisions, annex [Internet]. WHO; 2005. Available online: https://apps.who.int/iris/handle/10665/20398.
- WHO. Global strategy on digital health 2020-2025. WHO; 2021.
- Manyazewal, T.; Woldeamanuel, Y.; Blumberg, H.M.; Fekadu, A.; Marconi, V.C. The potential use of digital health technologies in the African context: a systematic review of evidence from Ethiopia. npj Digit. Med. 2021, 4, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Asah FN, Kaasbøll JJ, Anthun KS. Obstacles of eHealth Capacity Building and Innovation Promotion Initiative in African Countries. Stud Health Technol Inform. 2022;299:33–43. [CrossRef]
- G Eysenbach. What is e-health? J Med Internet Res.; 2001.
- World Health Organization. Global action plan on physical activity 2018-2030: more active people for a healthier world. World Health Organization; 2019.
- Kluge E-HW. Chapter 5 - Framework considerations. In: Kluge E-HW, editor. Electron Health Rec [Internet]. Academic Press; 2020. p. 105–133. Available online: https://www.sciencedirect.com/science/article/pii/B9780128220450000058.
- 9. Koivu A, Mavengere N, Ruohonen M, et al. Exploring the Information and ICT Skills of Health Professionals in Low- and Middle-Income Countries. In: Brinda T, Mavengere N, Haukijarvi I, et al., editors. 2016. p. 152–162. [CrossRef]
- Vishwanath, A.; Scamurra, S.D. Barriers to the adoption of electronic health records: using concept mapping to develop a comprehensive empirical model. Health Informatics J. 2007, 13, 119–134. [Google Scholar] [CrossRef] [PubMed]
- Mehl GL, Tamrat T, Bhardwaj S, et al. Digital health vision: could MomConnect provide a pragmatic starting point for achieving universal health coverage in South Africa and elsewhere? BMJ Glob Health. 2018;3:e000626.
- Al-Shorbaji, N. Improving Healthcare Access through Digital Health: The Use of Information and Communication Technologies [Internet]. Healthc. Access. IntechOpen; 2021 [cited 2022 Jul 14]. Available online: https://www.intechopen.com/chapters/undefined/state.item.id.
- Kraus, S.; Schiavone, F.; Pluzhnikova, A.; Invernizzi, A.C. Digital transformation in healthcare: Analyzing the current state-of-research. J. Bus. Res. 2020, 123, 557–567. [Google Scholar] [CrossRef]
- World Health Organization. Seventh meeting of the European Health Information Initiative Steering Group: Copenhagen, Denmark, 21–22 March 2017. World Health Organization. Regional Office for Europe; 2017.
- van Gemert-Pijnen JE, Wynchank S, Covvey HD, et al. Improving the credibility of electronic health technologies. Bull World Health Organ. 2012;1:323-323A.
- Hamad WB. CURRENT Position and Challenges of E-health in Tanzania: A review of literature. 2019;7:14.
- Anderson JG. Social, ethical and legal barriers to e-health. Int J Med Inf. 2007;76:480–483.
- Asah FN. Challenges and Approaches of Implementing Standard Health Indicators in Hierarchical Organizations: A multisited study. 2021.
- Mars, M. Building the capacity to build capacity in e-health in sub-Saharan Africa: the KwaZulu-Natal experience. Telemed E-Health. 2012;18:32–37.
- Mars, M.; Scott, R.E. Global E-Health Policy: A Work In Progress. Health Aff. 2010, 29, 237–243. [Google Scholar] [CrossRef] [PubMed]
- Adebesin F, Kotzé P, Van Greunen D, et al. Barriers & challenges to the adoption of E-Health standards in Africa. 2013.
- Amin, M.M.; Sutrisman, A.; Stiawan, D.; Ermatita, E.; Alzahrani, M.Y.; Budiarto, R. Interoperability framework for integrated e-health services. Bull. Electr. Eng. Informatics 2020, 9, 354–361. [Google Scholar] [CrossRef]
- Sluijs, M.B.; Veeken, H.; Overbeke, A.J.P.M. [Deficient information in developing countries: Internet alone is no solution]. Ned. Tijdschr. voor Geneeskd. 2006, 150. [Google Scholar]
- Masud, M.; Hossain, M.S.; Alamri, A. Data Interoperability and Multimedia Content Management in e-Health Systems. IEEE Trans. Inf. Technol. Biomed. 2012, 16, 1015–1023. [Google Scholar] [CrossRef] [PubMed]
- Ahern, D.K.; Kreslake, J.M.; Phalen, J.M.; Bock, B. What Is eHealth (6): Perspectives on the Evolution of eHealth Research. J. Med Internet Res. 2006, 8, e4. [Google Scholar] [CrossRef] [PubMed]
- Mburu, S.; Kamau, O. Mburu S, Kamau O. Framework for Development and Implementation of Digital Health Policies to Accelerate the Attainment of Sustainable Development Goals: Case of Kenya eHealth Policy (2016-2030). J Health Inform Afr [Internet]. 2018 [cited 2022 Jul 25];5. [CrossRef]
- Luna, D.; Almerares, A.; Mayan, J.C.; de Quirós, F.G.B.; Otero, C. Health Informatics in Developing Countries: Going beyond Pilot Practices to Sustainable Implementations: A Review of the Current Challenges. Health Informatics Res. 2014, 20, 3–10. [Google Scholar] [CrossRef] [PubMed]
- 28. Larbi D, Anthun KS, Asah FN, et al. Assessing Strategic Priority Factors in eHealth Policies of Four African Countries. IEEE; 2022. p. 1–9. [CrossRef]
- Jamil, S. From digital divide to digital inclusion: Challenges for wide-ranging digitalization in Pakistan. Telecommun. Policy 2021, 45, 102206. [Google Scholar] [CrossRef]
- Staton R, Bautista A, Harwell J, et al. Computerized provider order entry awareness for nursing: unintended consequences and remediation plan. CIN Comput Inform Nurs. 2013;31:401–405.
- Alshahrani, A.; Stewart, D.; MacLure, K. A systematic review of the adoption and acceptance of eHealth in Saudi Arabia: Views of multiple stakeholders. Int. J. Med Informatics 2019, 128, 7–17. [Google Scholar] [CrossRef] [PubMed]
- Asangansi, Macleod B, Meremikwu M. Improving the routine HMIS in Nigeria through mobile technology for community data collection. Journal of Health Informatics in Developing Countries. 2013;76–87.
- 33. Qureshi QA, Shah B, Kundi GM, et al. Infrastructural barriers to e-health implementation in developing countries. Eur. J. Sustain. Dev. 2013, 2, 163. [CrossRef]
- Cardellino, P.; Finch, E. Evidence of systematic approaches to innovation in facilities management. J. Facil. Manag. 2006, 4, 150–166. [Google Scholar] [CrossRef]
- Steen L, Mao X. Digital skills for health professionals. 2016. p. 37–47.
- Detmer. Capacity Building in e-Health and Health Informatics: A Review of the Global Vision and Informatics Educational Initiatives of the American Medical Informatics Association. 2010.
- Shegaw, AM. Analysing the Challenges of IS implementation in public health institutions of a developing country: the need for flexible strategies. Journal of Health Informatics in Developing Countries. 2010;4.
- Tchao, Acquah, Kotey, et al. On Telemedicine Implementations in Ghana. Int J Adv Comput Sci Appl. 2019;10:193–201.
- Curioso, W.H. Building Capacity and Training for Digital Health: Challenges and Opportunities in Latin America. J. Med Internet Res. 2019, 21, e16513. [Google Scholar] [CrossRef] [PubMed]
- Larbi D, Anthun KS, Asah FN, et al. Assessing Strategic Priority Factors in eHealth Policies of Four African Countries. IEEE; 2022. p. 1–9. [CrossRef]
- Mengiste SA, Antypas K, Johannessen MR, et al. Research Landscape and Research Priorities in eHealth in four African Countries-A survey. EGOV-CeDEM-EPart 2022. 2022;130.
- Khoja, S.; Durrani, H.; Nayani, P.; Fahim, A. Scope of Policy Issues in eHealth: Results From a Structured Literature Review. J. Med Internet Res. 2012, 14, e1633. [Google Scholar] [CrossRef] [PubMed]
- Omary Z, Lupiana D, Mtenzi F, et al. Analysis of the challenges affecting e-healthcare adoption in developing countries: A case of Tanzania. Int J Inf Stud. 2010;2:38–50.
- Vatsalan D, Arunatileka S, Chapman K, et al. Mobile technologies for enhancing eHealth solutions in developing countries. IEEE; 2010. p. 84–89. [CrossRef]
- DEDICATED Project 2020. Unpublished.
- Ledikwe, J.H.; Grignon, J.; Lebelonyane, R.; Ludick, S.; Matshediso, E.; Sento, B.W.; Sharma, A.; Semo, B.-W. Improving the quality of health information: a qualitative assessment of data management and reporting systems in Botswana. Health Res. Policy Syst. 2014, 12, 7–7. [Google Scholar] [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).