Submitted:
23 July 2023
Posted:
24 July 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Aims
- To evaluate risk factors associated with community-acquired Acinetobacter Pneumonia in a North Queensland cohort;
- To assess the efficacy of antibiotic therapy in community-acquired Acinetobacter pneumonia;
- To evaluate how antibiotic prescribing practices in CAAP influence mortality;
- To investigate mortality rate and factors associated with mortality.
2.2. Study Design
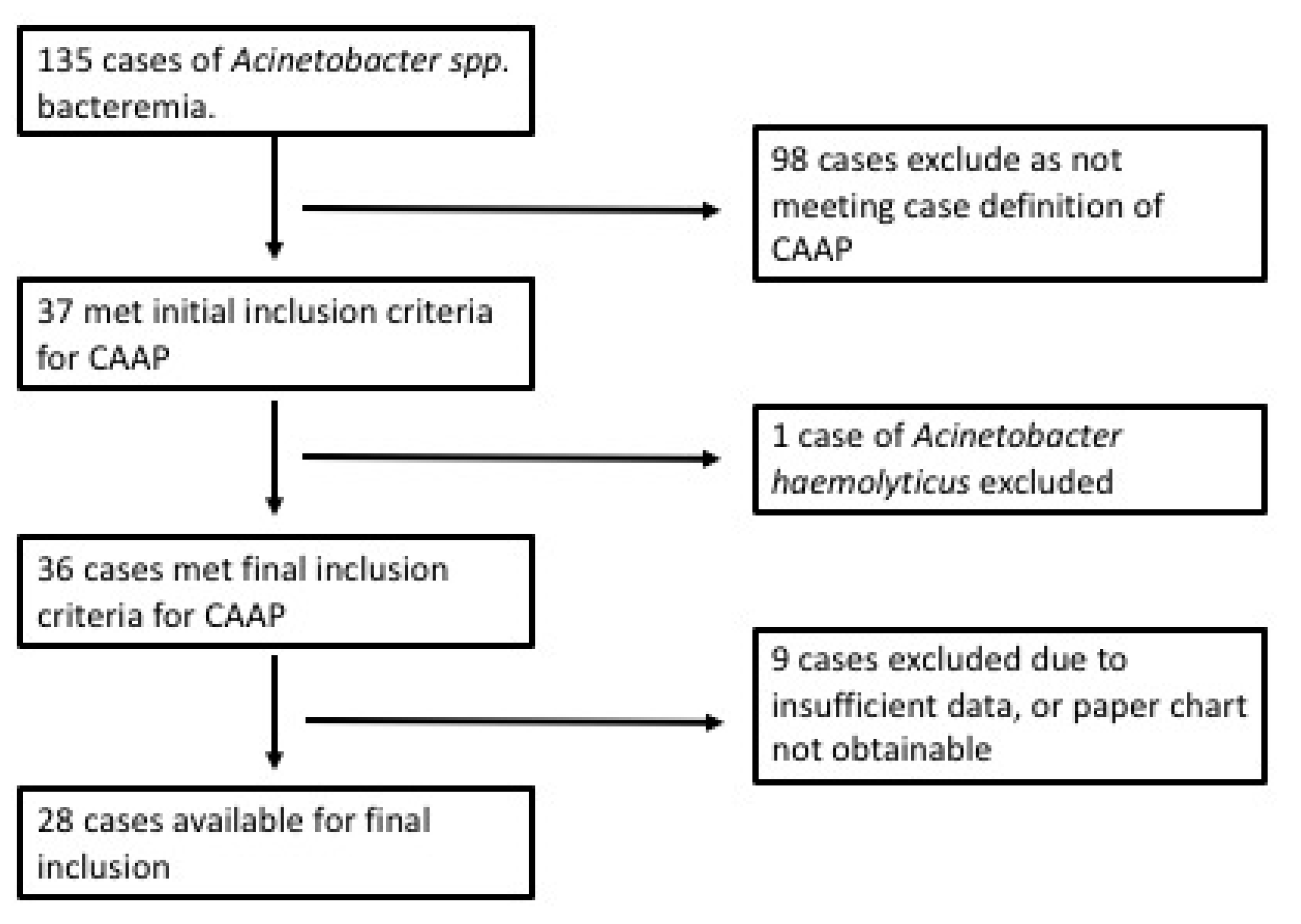
2.3. Participant recruitment and sample collection
- Blood culture positive for Acinetobacter baumannii complex;
- Clinical features consistent with pneumonia;
- Radiographic evidence of pneumonia on chest radiograph or computed tomography scan.
2.4. Definitions
2.5. Statistical Analysis
2.6. Ethics
3. Results
4. Discussion
4.1. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Anstey, N.M.; Currie, B.J.; Withnall, K.M. Community-Acquired Acinetobacter Pneumonia in the Northern Territory of Australia. Clin. Infect. Dis. 1992, 14, 83–91. [Google Scholar] [CrossRef] [PubMed]
- Dexter, C.; Murray, G.L.; Paulsen, I.T.; Peleg, A.Y. Community-acquiredAcinetobacter baumannii: clinical characteristics, epidemiology and pathogenesis. Expert Rev. Anti-infective Ther. 2015, 13, 567–573. [Google Scholar] [CrossRef]
- Yang, C.-H.; Chen, K.-J.; Wang, C.-K. Community-acquired Acinetobacter pneumonia: A case report. J. Infect. 1997, 35, 316–318. [Google Scholar] [CrossRef] [PubMed]
- Antunes, L.C.; Visca, P.; Towner, K.J. Acinetobacter baumannii: evolution of a global pathogen. Pathog. Dis. 2014, 71, 292–301. [Google Scholar] [CrossRef] [PubMed]
- Gottlieb, T.; Barnes, D.J. COMMUNITY-ACQUIRED ACINETOBACTER PNEUMONIA. Aust. New Zealand J. Med. 1989, 19, 259–260. [Google Scholar] [CrossRef]
- Chen, M.-Z.; Hsueh, P.-R.; Lee, L.-N.; Yu, C.-J.; Yang, P.-C.; Luh, K.-T. Severe Community-Acquired Pneumonia due to Acinetobacter baumannii. Chest 2001, 120, 1072–1077. [Google Scholar] [CrossRef]
- Davis, J.S.; McMillan, M.; Swaminathan, A.; Kelly, J.A.; Piera, K.E.; Baird, R.W.; Currie, B.J.; Anstey, N.M. A 16-Year Prospective Study of Community-Onset Bacteremic Acinetobacter Pneumonia. Chest 2014, 146, 1038–1045. [Google Scholar] [CrossRef]
- Ong CWM, Lye DCB, et al. Severe community acquired Acinetobacter baumannii pneumonia: an emerging highly lethal infectious disease in the Asia-Pacific. Respirology. 2009, 14, 1200–1205. [CrossRef]
- Patamatamkul, S.; Klungboonkrong, V.; Praisarnti, P.; Jirakiat, K. A case-control study of community-acquired Acinetobacter baumannii pneumonia and melioidosis pneumonia in northeast Thailand: an emerging fatal disease with unique clinical features. Diagn. Microbiol. Infect. Dis. 2017, 87, 79–86. [Google Scholar] [CrossRef]
- Chusri, S.; Chongsuvivatwong, V.; Silpapojakul, K.; Singkhamanan, K.; Hortiwakul, T.; Charernmak, B.; Doi, Y. Clinical characteristics and outcomes of community and hospital-acquired Acinetobacter baumannii bacteremia. J. Microbiol. Immunol. Infect. 2019, 52, 796–806. [Google Scholar] [CrossRef]
- Lee YL, Lu MC, et al. Nationwide surveillance of antimicrobial resistance among clinically important Gram-negative bacteria, with an emphasis on carbapenems and colistin: Results from the surveillance of multicentre antimicrobial resistance in Taiwan (SMART) in 2018. Int. J. Antimicrob. Agents. 2019, 54, 318–328. [CrossRef]
- Kelly H, Buising K, et al. Electronic Therapeutic Guidelines Antibiotic [on-line]. 16th Edition. Melbourne: Therapeutic Guidelines Limited; 2019. Respiratory tract infections: community-acquired pneumonia.
- Christiansen K, Currie B, et al. Therapeutic Guidelines Antibiotic. 11th Edition. Melbourne: Therapeutic Guidelines Limited; 2000. Respiratory tract infections: lower; p. 141-149.
- Moulds R, Boutlis C, et al. Therapeutic Guidelines Antibiotic. 15th Edition. Melbourne: Therapeutic Guidelines Limited; 2014. Respiratory tract infections: community-acquired pneumonia; p. 153-180.
- Lee, A.; Hanson, J.; Fox, P.; Spice, G.; Russell, D.; Boyd, P. A decentralised, multidisciplinary model of care facilitates treatment of hepatitis C in regional Australia. J. Virus Erad. 2018, 4, 160–164. [Google Scholar] [CrossRef]
- Anstey, N.M.; Currie, B.J.; Hassell, M.; Palmer, D.; Dwyer, B.; Seifert, H. Community-Acquired Bacteremic Acinetobacter Pneumonia in Tropical Australia Is Caused by Diverse Strains of Acinetobacter baumannii, with Carriage in the Throat in At-Risk Groups. J. Clin. Microbiol. 2002, 40, 685–686. [Google Scholar] [CrossRef] [PubMed]
- Charles, P.G.P.; Wolfe, R.; Whitby, M.; Fine, M.J.; Fuller, A.J.; Stirling, R.; Wright, A.A.; Ramirez, J.A.; Christiansen, K.J.; Waterer, G.W.; et al. SMART-COP: A Tool for Predicting the Need for Intensive Respiratory or Vasopressor Support in Community-Acquired Pneumonia. Clin. Infect. Dis. 2008, 47, 375–384. [Google Scholar] [CrossRef]
- Wang, J.-T.; McDonald, L.C.; Chang, S.-C.; Ho, M. Community-Acquired Acinetobacter baumannii Bacteremia in Adult Patients in Taiwan. J. Clin. Microbiol. 2002, 40, 1526–1529. [Google Scholar] [CrossRef]
- Leung, W.-S.; Chu, C.-M.; Tsang, K.-Y.; Lo, F.-H.; Lo, K.-F.; Ho, P.-L. Fulminant Community-Acquired Acinetobacter baumannii Pneumonia as a Distinct Clinical Syndrome. Chest 2006, 129, 102–109. [Google Scholar] [CrossRef]
- Falagas, M.E.; Karveli, E.A.; Kelesidis, I.; Kelesidis, T. Community-acquired Acinetobacter infections. Eur. J. Clin. Microbiol. Infect. Dis. 2007, 26, 857–868. [Google Scholar] [CrossRef]
- Sia TLL, Chua H. Case series: Fulminant community-acquired Acinetobacter pneumonia. Med J Malaysia. 2020, 75, 186–188.
- Asai, N.; Sakanashi, D.; Suematsu, H.; Kato, H.; Watanabe, H.; Shiota, A.; Hagihara, M.; Koizumi, Y.; Yamagishi, Y.; Mikamo, H. Clinical manifestations and risk factors of community-onset Acinetobacter species pneumonia in Japan; case control study in a single institute in Japan. J. Infect. Chemother. 2019, 25, 639–642. [Google Scholar] [CrossRef]
- Australian Bureau of Meteorology. Climate statistics for Australian sites: Queensland [Internet]. Australian Government. 2019. Available from: http://www.bom.gov.au/climate/averages/tables/ca_qld_names.
- Wu, C.-L.; Ku, S.-C.; Yang, K.-Y.; Fang, W.-F.; Tu, C.-Y.; Chen, C.-W.; Hsu, K.-H.; Fan, W.-C.; Lin, M.-C.; Chen, W.; et al. Antimicrobial drug-resistant microbes associated with hospitalized community-acquired and healthcare-associated pneumonia: A multi-center study in Taiwan. J. Formos. Med Assoc. 2013, 112, 31–40. [Google Scholar] [CrossRef]
- Gandhi, J.A.; Ekhar, V.V.; Asplund, M.B.; Abdulkareem, A.F.; Ahmadi, M.; Coelho, C.; Martinez, L.R. Alcohol Enhances Acinetobacter baumannii-Associated Pneumonia and Systemic Dissemination by Impairing Neutrophil Antimicrobial Activity in a Murine Model of Infection. PLOS ONE 2014, 9, e95707. [Google Scholar] [CrossRef] [PubMed]
- Meumann, E.M.; Anstey, N.M.; Currie, B.J.; Piera, K.A.; Kenyon, J.J.; Hall, R.M.; Davis, J.S.; Sarovich, D.S. Genomic epidemiology of severe community-onset Acinetobacter baumannii infection. Microb. Genom. 2019, 5. [Google Scholar] [CrossRef]
- Wong, D.; Nielsen, T.B.; Bonomo, R.A.; Pantapalangkoor, P.; Luna, B.; Spellberg, B. Clinical and Pathophysiological Overview of Acinetobacter Infections: a Century of Challenges. Clin. Microbiol. Rev. 2017, 30, 409–447. [Google Scholar] [CrossRef]
- Munoz-Price, L.S.; Weinstein, R.A. Acinetobacter Infection. New Engl. J. Med. 2008, 358, 1271–1281. [Google Scholar] [CrossRef] [PubMed]
- Eveillard, M.; Kempf, M.; Belmonte, O.; Pailhoriès, H.; Joly-Guillou, M.-L. Reservoirs of Acinetobacter baumannii outside the hospital and potential involvement in emerging human community-acquired infections. Int. J. Infect. Dis. 2013, 17, e802–e805. [Google Scholar] [CrossRef] [PubMed]
- Kim, Y.A.; Kim, J.J.; Won, D.J.; Lee, K. Seasonal and Temperature-Associated Increase in Community-Onset Acinetobacter baumannii Complex Colonization or Infection. Ann. Lab. Med. 2018, 38, 266–270. [Google Scholar] [CrossRef]
- Cheng, A.C.; Currie, B.J.; Dance, D.A.B.; Funnell, S.G.P.; Limmathurotsakul, D.; Simpson, A.J.H.; Peacock, S.J. Clinical Definitions of Melioidosis. Am. J. Trop. Med. Hyg. 2013, 88, 411–413. [Google Scholar] [CrossRef]
- Mu, J.-J.; Cheng, P.-Y.; Chen, P.-S.; Chen, Y.-L. The occurrence of melioidosis is related to different climatic conditions in distinct topographical areas of Taiwan. Epidemiology Infect. 2013, 142, 415–423. [Google Scholar] [CrossRef]
- Currie, B.J.; Jacups, S.P. Intensity of Rainfall and Severity of Melioidosis, Australia. Emerg. Infect. Dis. 2003, 9, 1538–1542. [Google Scholar] [CrossRef]
| Patient Characteristic | Proportion of patients, n = 28 (%), [IQR] |
|---|---|
| Age in years, median, [IQR] | 43, [36.8-51.3] |
| Male | 19 (67.9) |
| Indigenous Australian | 23 (82.1) |
| Resident of Cairns | 9 (32.1) |
| Wet Season Disease | 18 (64.3) |
| Dry Season Disease | 10 (35.7) |
| Clinical features | |
| Pleurisy | 18 (64.3) |
| Pyrexia (>38 degrees) | 16 (57.1) |
| Muco-Purulent or Purulent Sputum | 11 (47.8) |
| Blood-stained Sputum | 11 (47.8) |
| Severity | |
| ICU admission | 16 (57.1) |
| SMART-COP (moderate to severe) | 25 (89.3) |
| SMART-COP, median and [IQR] | 6, [4-8] |
| Hypoxaemia | 20 (71.4) |
| Shock | 10 (35.7) |
| Death | 8 (28.6) |
| Risk Factors for CAAP | |
| Current tobacco Use | 23 (82.1) |
| Hazardous Alcohol Consumption | 20 (71.4) |
| Hazardous Alcohol & Tobacco Use | 17 (60.7) |
| Chronic Lung disease | 7 (25) |
| Heart Failure | 4 (14.3) |
| Diabetes Mellitus | 3 (10.7) |
| Chronic Kidney Disease | 4 (14.3) |
| Immunosuppression | 1 (3.6) |
| Malignancy | 1 (3.6) |
| ≥ 2 Risk Factors | 25 (89.3) |
| Test | Median [IQR] | Above Normal (%) | Below Normal (%) | Normal Reference Range |
|---|---|---|---|---|
| White Cell Count | 11.8 [7.8-17.4] | 14/28 (50) | 5/28 (17.9) | 4-11 × 109/L |
| Haemoglobin | 136 [121-146] | 0 (0) | 7/28 (25) | 135-175/120-155 (M/F) g/L |
| Neutrophils | 9.37 [5.46-15.5] | 16/28 (57.1) | 5/28 (17.9) | 2-7.5 × 109/L |
| Lymphocytes | 0.53 [0.41-0.93] | 0 (0) | 21/28 (75) | 1.5-4 × 109/L |
| Platelets | 177 [91.3-221] | 1/28 (3.57) | 12/28 (42.9) | 150-400 × 109/L |
| Albumin | 29.5 [25-33.5] | 0 (0) | 21/28 (75) | 35-50 g/L |
| C-Reactive Protein | 154 [63-231] | 21/22 (95.5) | 0 (0) | <5 mg/L |
| Risk Factor (RF) | Number (%) of those with RF who died | p-value |
|---|---|---|
| Shock | 3/10 (30) | 0.615 |
| Chronic Lung Disease | 3/7 (42.9) | 0.411 |
| Multi-Lobar Pneumonia | 3/16 (18.8) | 0.183 |
| Non-targeted ABs D1 | 4/8 (50) | 0.123 |
| Hazardous Alcohol Consumption | 6/20 (30) | 0.589 |
| Hazardous Alcohol & Tobacco Consumption | 4/17 (23.5) | 0.376 |
| Tobacco Consumption | 4/23 (17.4) | 0.015* |
| SMART-COP >/= 5 (Severe) | 4/18 (22.2) | 0.284 |
| Multiple Risk Factors >2 | 7/25 (28) | 0.652 |
| Overall mortality | 8/28 {28.6%} |
| Antibiotic Practice | No. | Died: Number (% sample/% total deaths) |
Died < 24 hours | Mean LOS | ICU | Median SMART-COP on Admission |
|---|---|---|---|---|---|---|
| Meropenem D1 | 10 | 2 (7.1/25) | 1 | 17.8 | 8 | 8 |
| Gentamicin D1 | 4 | 1 (3.6/12.5) | 1 | 16.5 | 2 | 6.5 |
| Both D1 | 3 | 0 | 0 | 22.7 | 2 | 6 |
| Total Mero/Gent D1 | 17 | 3 (10.7/37.5) | 2 | 18.3 | 12 | 7 |
| Delay to either | 9 | 4 (14.3/50) | 1 | 10 | 3 | 4 |
| Delay Gentamicin | 3 | 0 | 0 | 10.3 | 0 | 3 |
| Delay Meropenem | 5 | 3 (10.7/37.5) | 0 | 10.6 | 3 | 4 |
| Delay Both | 1 | 1 (3.6/12.5) | 0 | 6 | 0 | 2 |
| Mero D1 delay gent | 1 | 1 (3.6/12.5) | 0 | 25 | 1 | 8 |
| Gent D1 delay mero | 3 | 0 | 0 | 21.7 | 2 | 6 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





