Submitted:
10 July 2023
Posted:
24 July 2023
You are already at the latest version
Abstract
Keywords:
Introduction
- The thickness of the mucosal layer in different areas of the mouth can affect implant selection of the implant/TAD’s length. When selecting a location for implantation, choosing an attached gingival site rather than a flabby mucosa is better. However, in some cases, implantation on a flabby mucosa cannot be avoided. Using a surgical guide makes locating the initial pilot hole made during the pre-drilling process easy. This saves time and effort in searching for the insertion point, as mucosa often covers it. For optimal results, it is recommended to utilize two surgical guides during the procedure: one for the pilot drill and another for the TAD. If you are considering placing TADs in the interdental bone between the roots of two teeth, it is imperative to have 0.5mm septal bone around TAD. This means that you will need at least 2.4 mm of the interdental bone to avoid damaging the roots, considering that TADs usually have a diameter of 1.4mm.
- Different TADs come in various head designs and sizes, so a surgical guide must be created to match the chosen TAD's dimensions. Laboratory technicians and clinicians must communicate to design an appropriate surgical guide. While the body of the TADs may be self-drilling, it's still recommended to use a pilot drill surgical guide to minimize any trauma to the soft tissue. This is particularly important for angulated insertion procedures to make it easier to enter the implantation site. The angle at which screws are inserted can vary depending on personal preference. Some people prefer an angle for stability, while others aim to avoid root collisions and position the screw tip apically. However, angled screw insertion is more challenging than straight insertion. A surgical guide can assist with accurate angulation insertion, and directional drilling requires a guide to prevent slipping. Designing the insertion process for easy handpiece and bur maneuvering during implantation is crucial.
- A surgical guide should have a stable position, usually using healthy teeth structure. Avoiding teeth that are compromised; therefore, periodontal health and mobility are avoided to stabilize the surgical guide.
- The force required to penetrate bone with TADs varies from 20N to 35N, depending on the diameter. Implantation typically occurs at a speed of 25Rpm, while drilling occurs at 800Rpm with water irrigation. It is better to have an immediate loading than waiting a few weeks, and it's better to load immediately rather than waiting for weeks and leaving it unloaded.
- It is mandatory to maintain sterilization and follow the aseptic procedure during the implantation process.
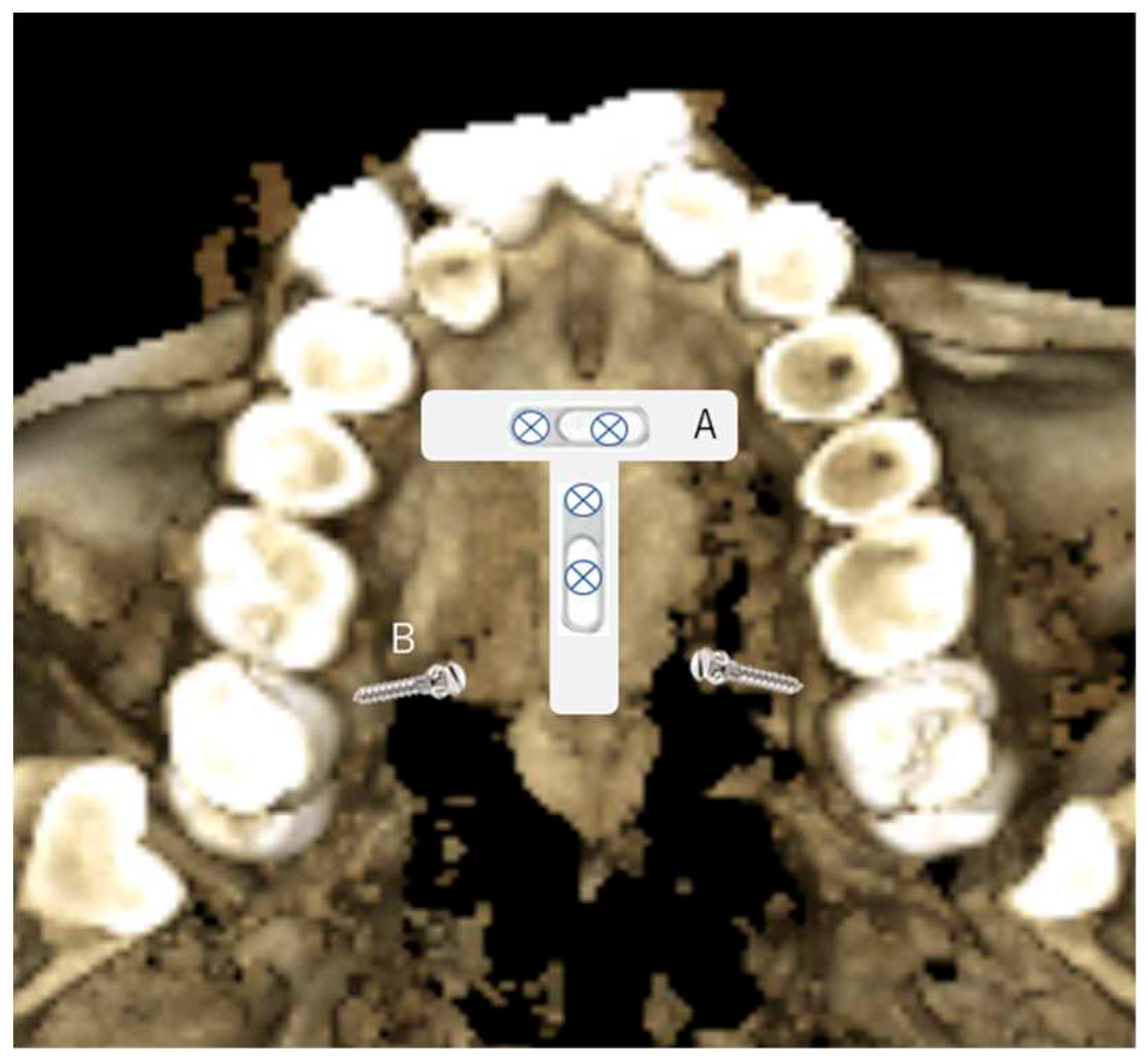
- In the maxilla, use CBCT to look for the ideal places and the palatal sites in the T-zone, as described by Wilmes (26). The Benefit’s system is two screws being used to connect a plate to make it a sturdy anchorage for a 3D movement of the upper teeth. Therefore, the two screws’ placement is critical to insert the plate easily and quickly, such as paralleling or close to the parallel to provide easy fixation. The surgical guide will facilitate the parallel insertion of TADS. TADS are placed at the best bone density in the area intended to be the anchorage placement. The other option for the TADs site in the palatal bone is between the first molar and the second bicuspid area, and the first molar has only a single palatal root (two roots on buccal) and the second bicuspid's root, which may as well be single in some clinical situations. The placement on the buccal side can also be done with the surgical guide in the anterior teeth between the central and lateral teeth for the buccal area of interdental of the bicuspids and the buccal ridge underneath the Zygomatic process.
- 2.
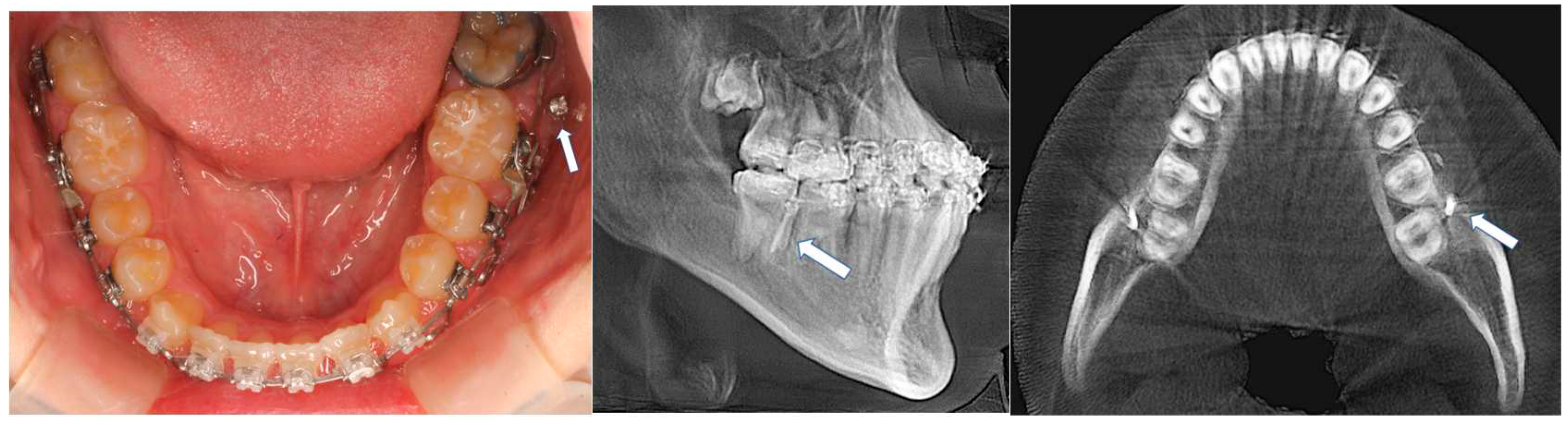
- In the mandible, TADs placement on the lingual side in the mandibular arch will be challenging, except there are torus lingualis that are large enough to provide TADs implantation; therefore, the buccal region is the only choice. The anterior part of the dental arch will have limited interdental bone availability, and the quality of bone is often questionable. A critical evaluation of available bone width is necessary before the implantation. Interdental space can be more suitable by appropriately placing the brackets to flare the crowded roots. Changing angulation of the roots beforehand is a common practice in placing TADs in the anterior region.
- 3.
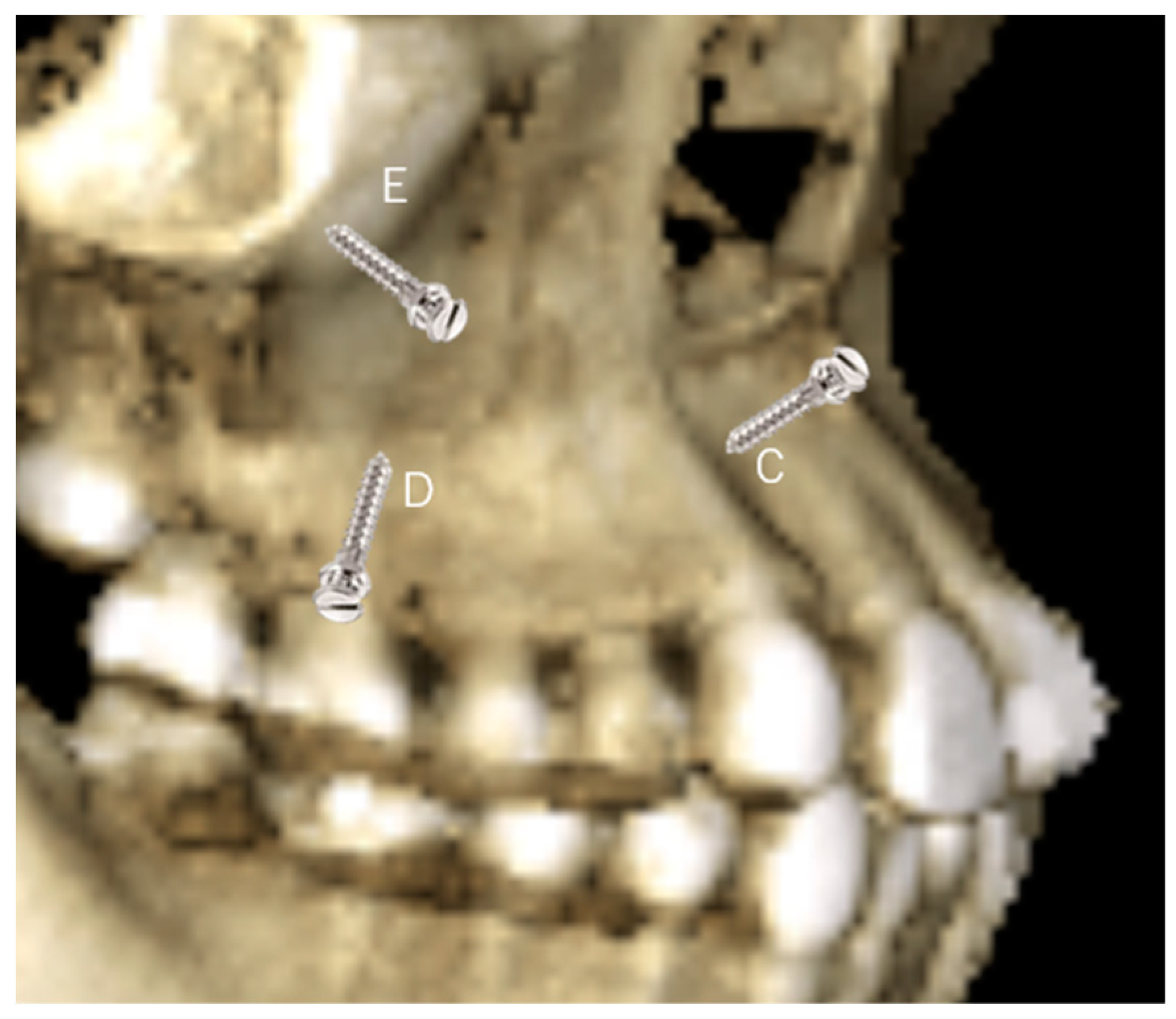
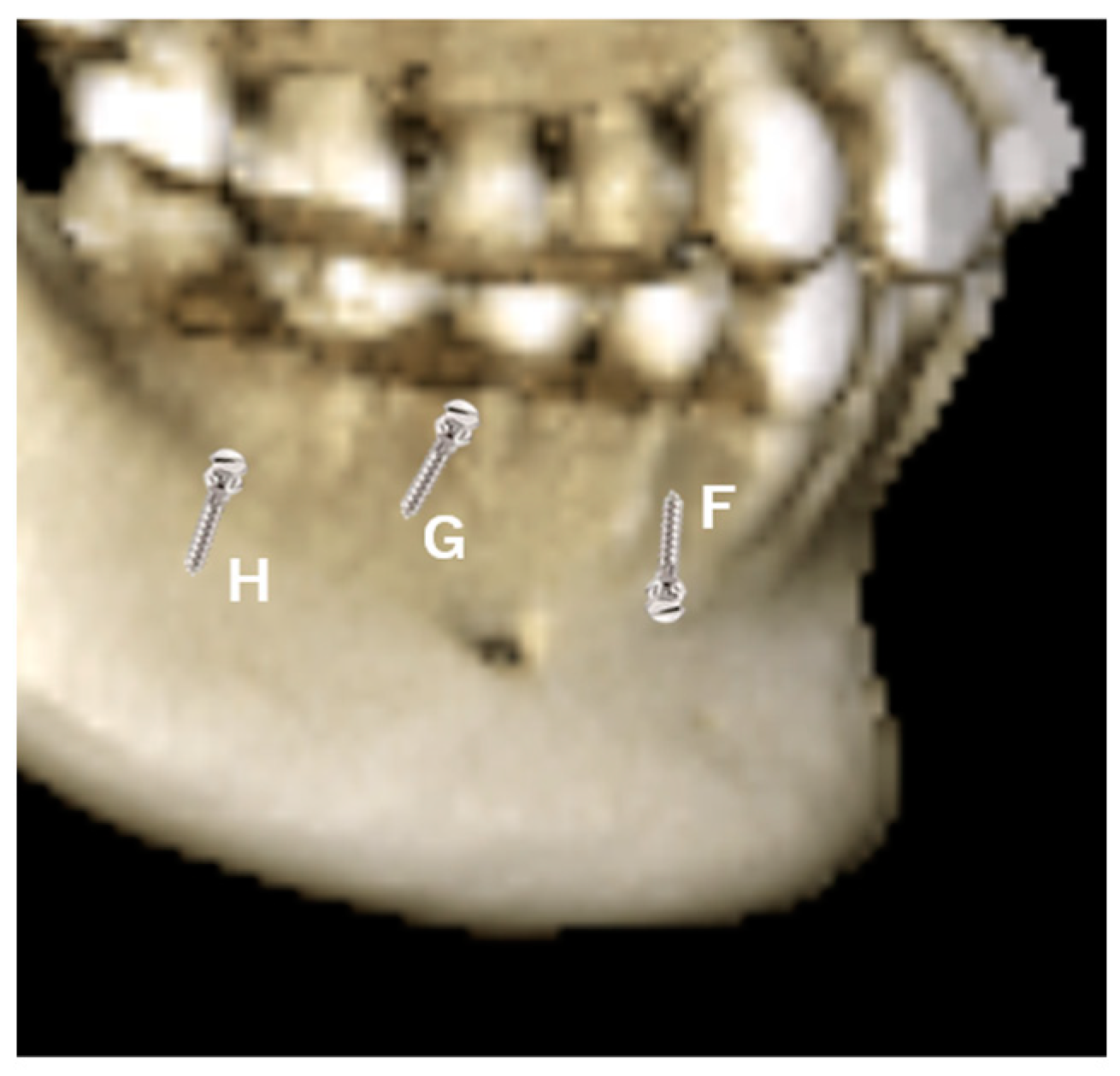
- The implantation in the interdental bone will limit the movement of the tooth, mesial and distally. Therefore, to avoid interferences with roots, the TADs are preferred on the mandible's ridge or the mandible's oblique line (Figure 3, H), especially when en-mass retraction of the arch is desirable. The ridge of the mandible between the body and the ramus of the mandible is a favorable site for TAD placement. The tricky part is that the mandible ridge may seem insignificant in women relative to men, and modification may be needed in the surgical guide’s design. Since the placement location is a steep bone wall, manual placement will be challenging, so a surgical guide is preferred. The angulated placement of the TADs in this area and the flabby mucosa also necessitates using the surgical guide. Care must be taken during the intraoral scan as the superficial mucous membrane above the ridge must be gently stretched to record this critical area. Lacking recorded data in this area will affect the visibility of the area site, and the surgical guide cannot be planned. Implantation in this area is recommended using contra-angle motorized instruments, as the buccal cheek tissue prevents using a hand screwdriver and will obstruct the surgeon's vision. The buccal musculature, maxillary teeth, and mouth opening will limit the maneuverability of the implantation procedure. These limitations should be evaluated during a clinical examination. Considering the hindrance in lower lip movements, the placement between the four incisors should be avoided as much as possible. TADS in this area can cause painful lip ulcerations with delayed healing. The location of the canine and the first bicuspid (Figure 3, F) is an area that can fit in the implantation choice. This location is between anterior and posterior dental arch segments and thus will provide an excellent place to resolve both anterior and posterior malocclusion. Depending on the extraction case or non-extraction case, considerations can be different, and placement in the extraction site of the bicuspid and adjacent area is required to avoid proximity to vital structures in the mentalis foramen. In Figure 3, G location is possible when there is a need to retract the anterior teeth after an extraction case when implantation of the ridge of the mandible is difficult or impossible due to the younger age of the patient. However, implantation at a young age, e.g., under 12, is risky as bone metabolism is still high in this area.
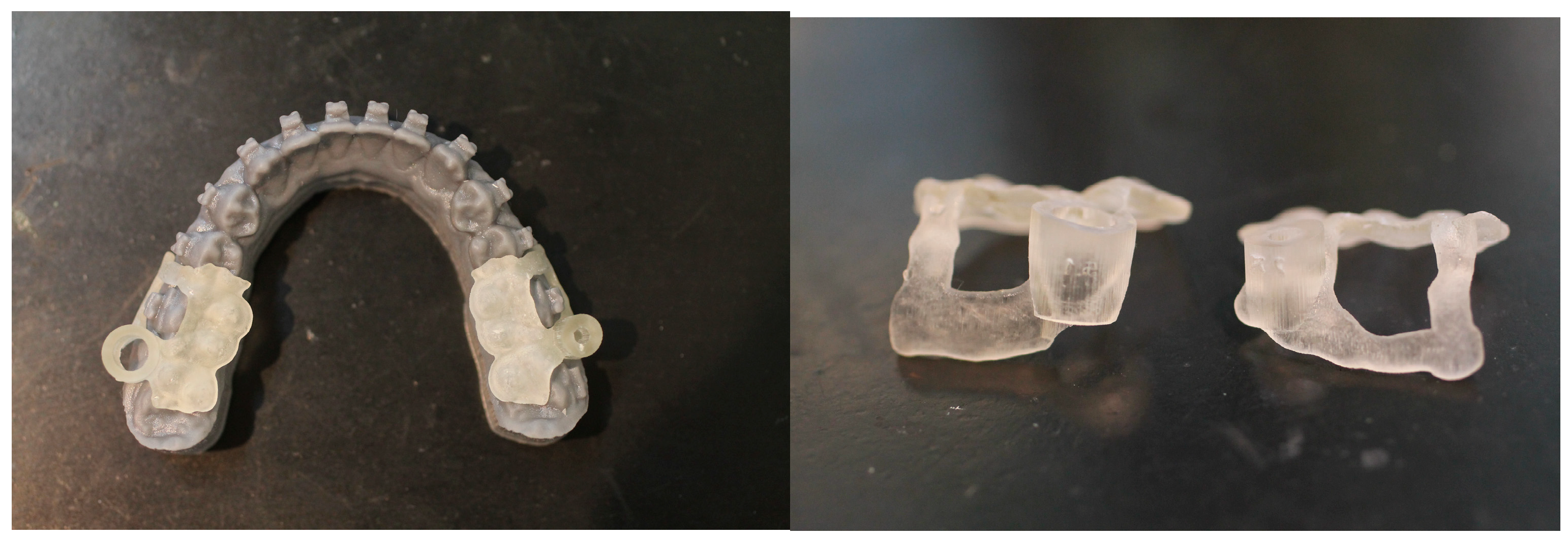
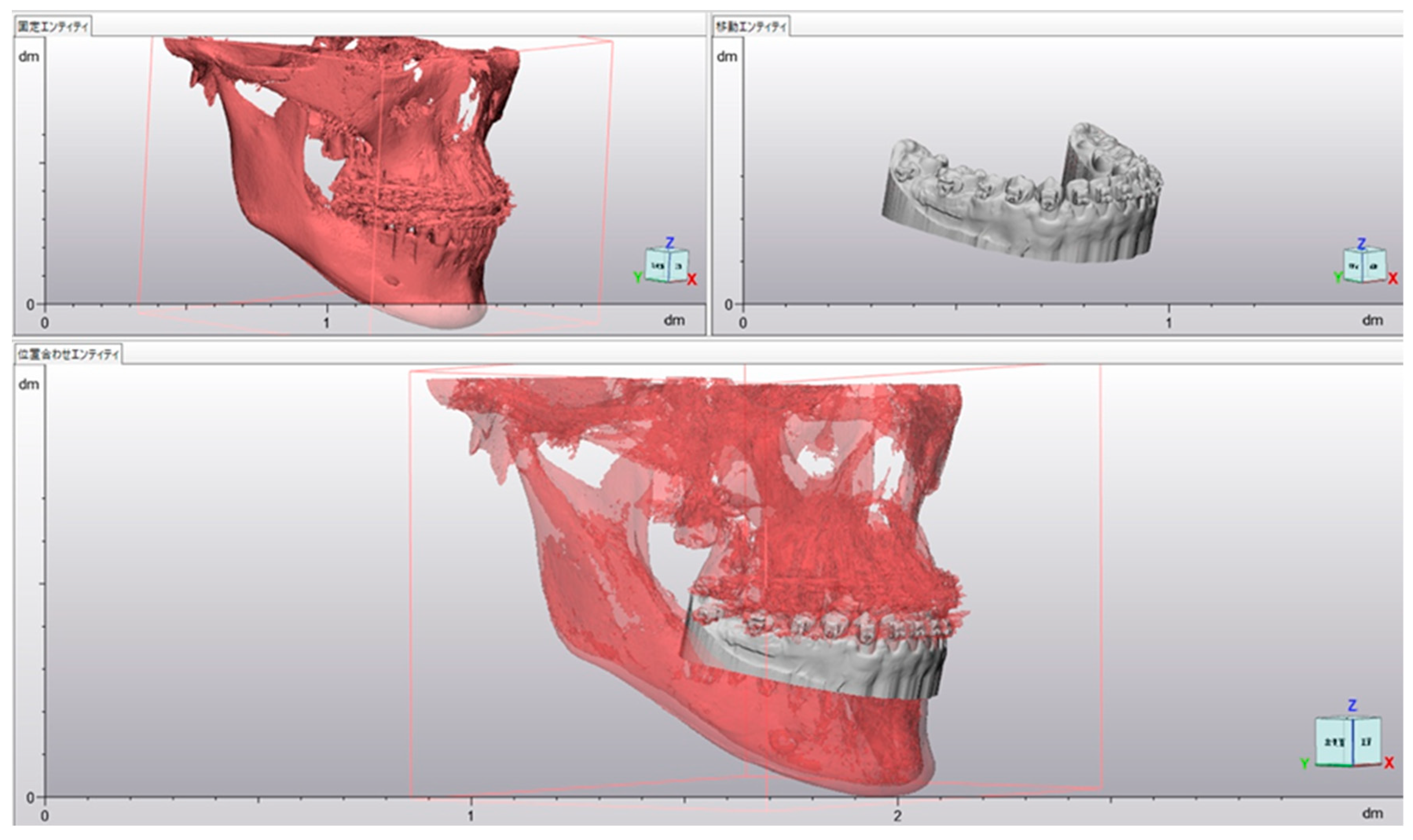
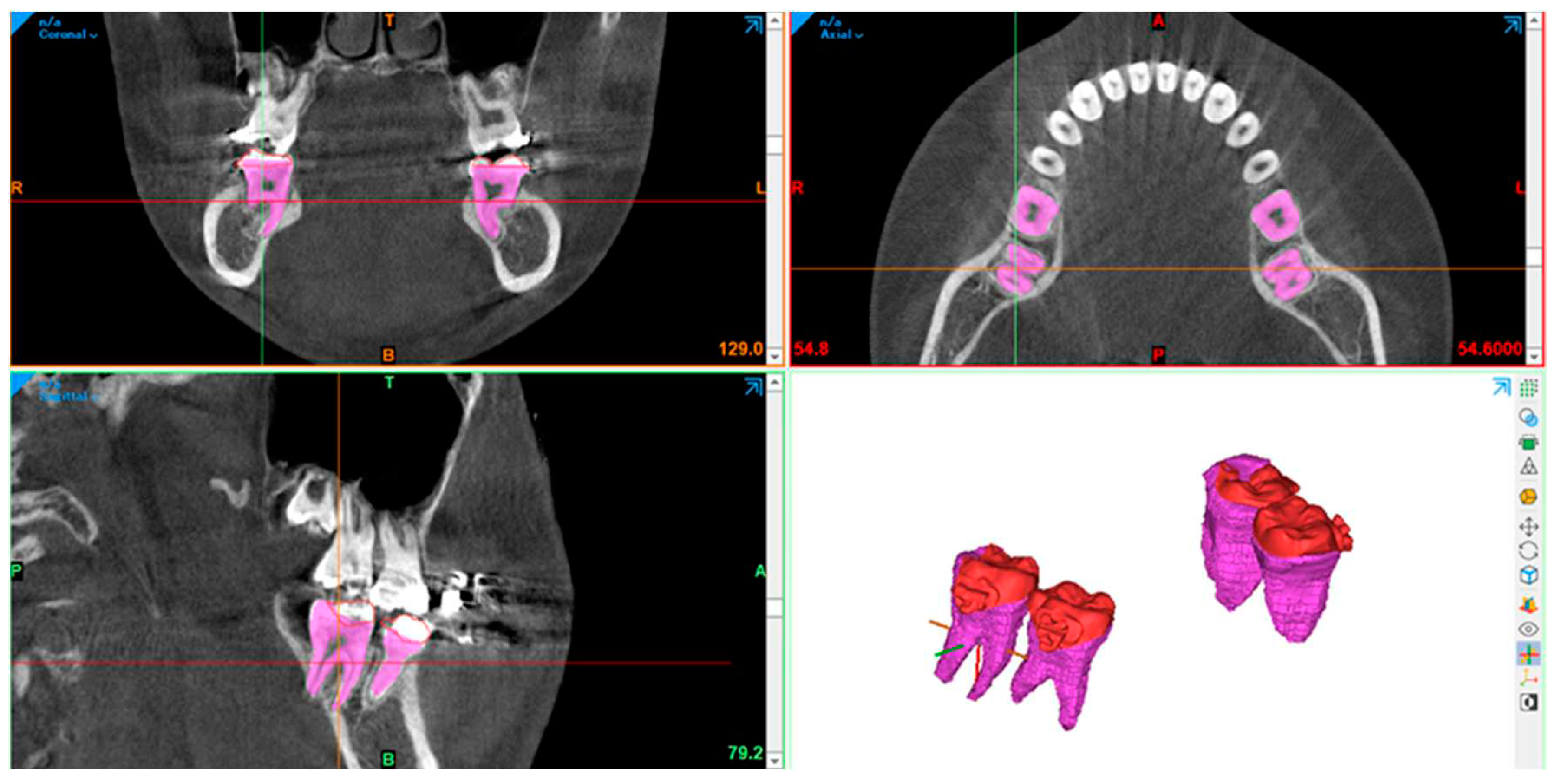
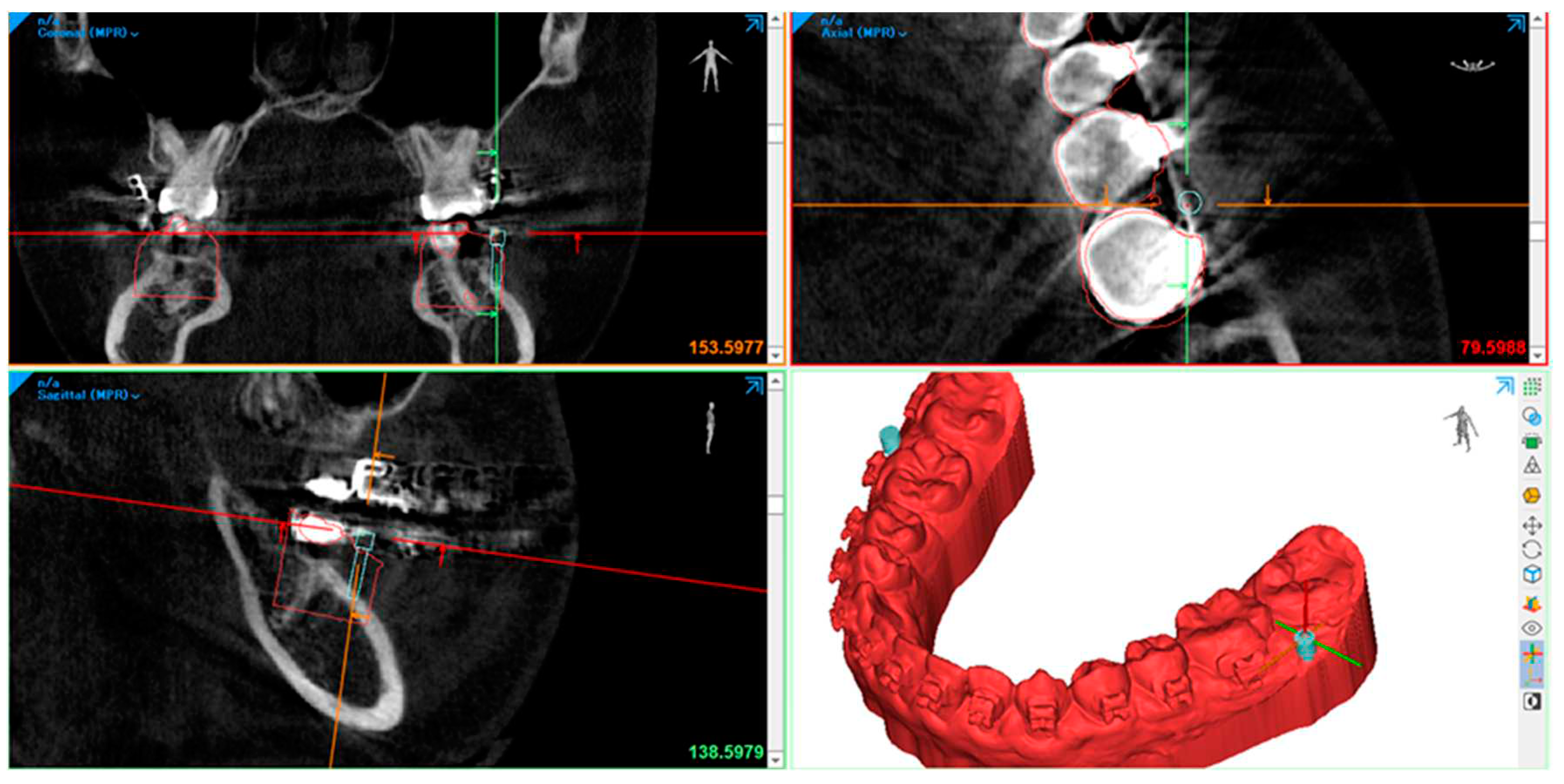
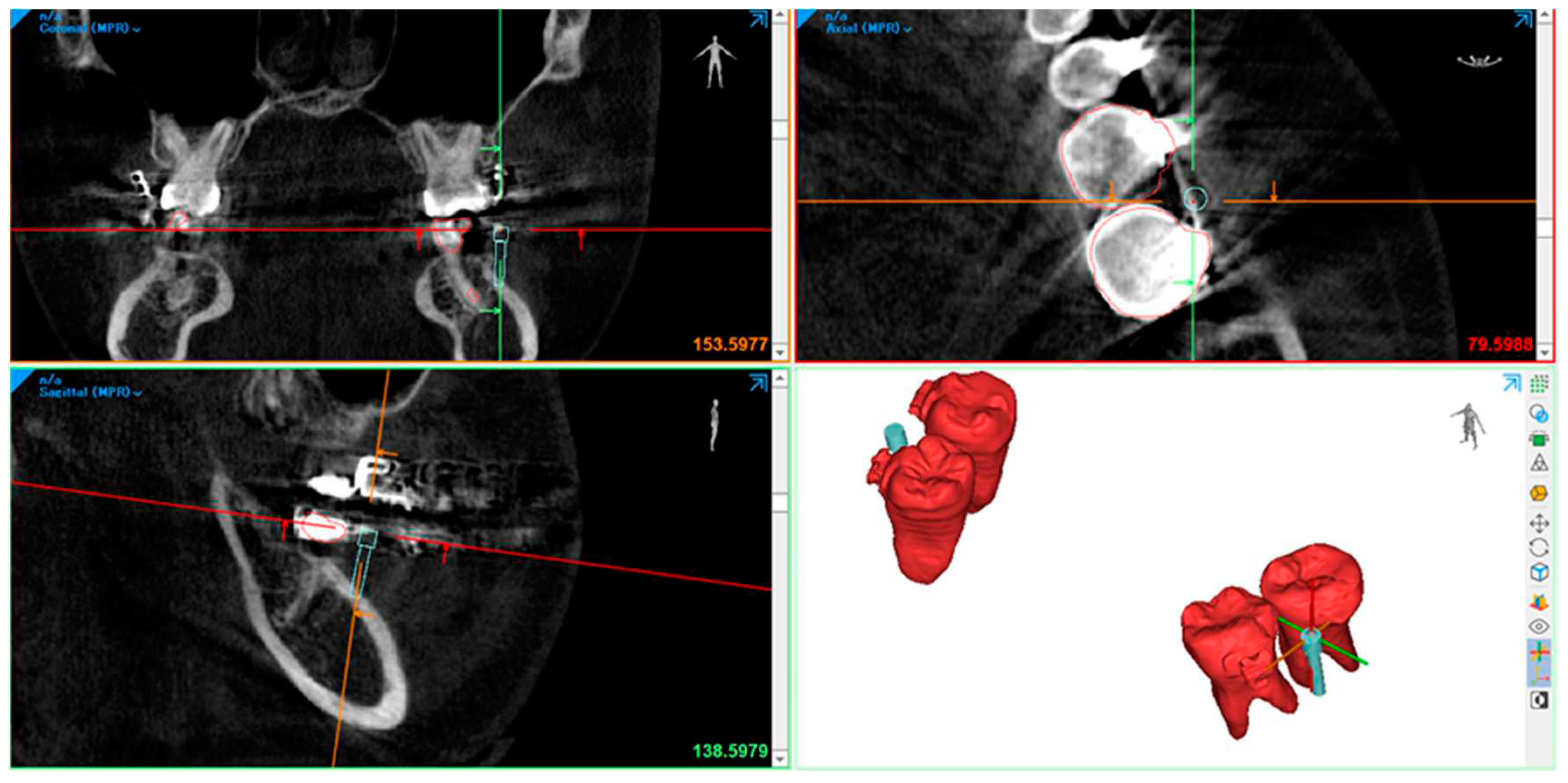
- We used an intra-oral scan for the SLT and a CBCT X-ray machine for the DICOM data to obtain a digital impression. afterward, we superimposed the STL and DICOM data using a commercialized application.
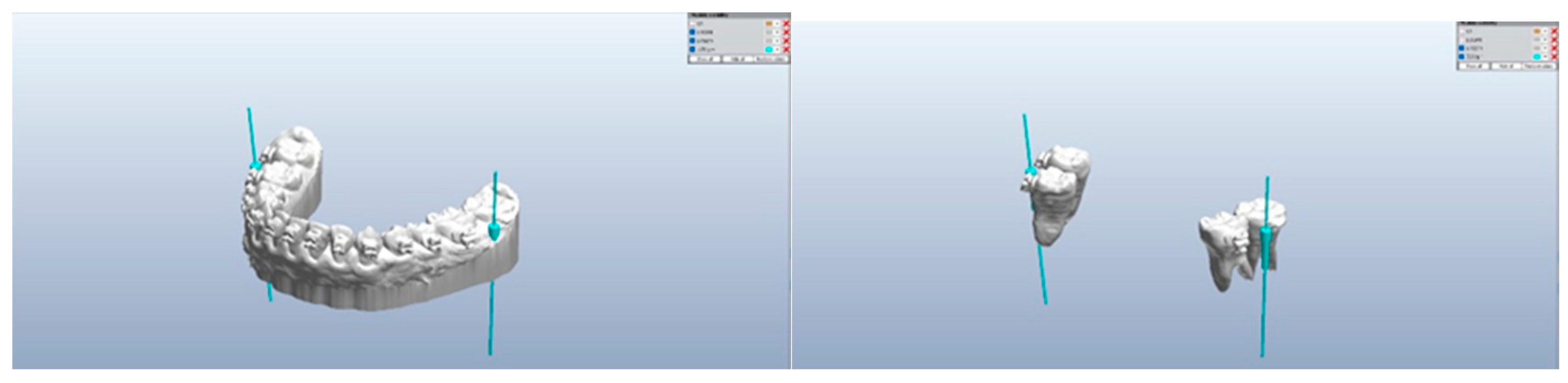
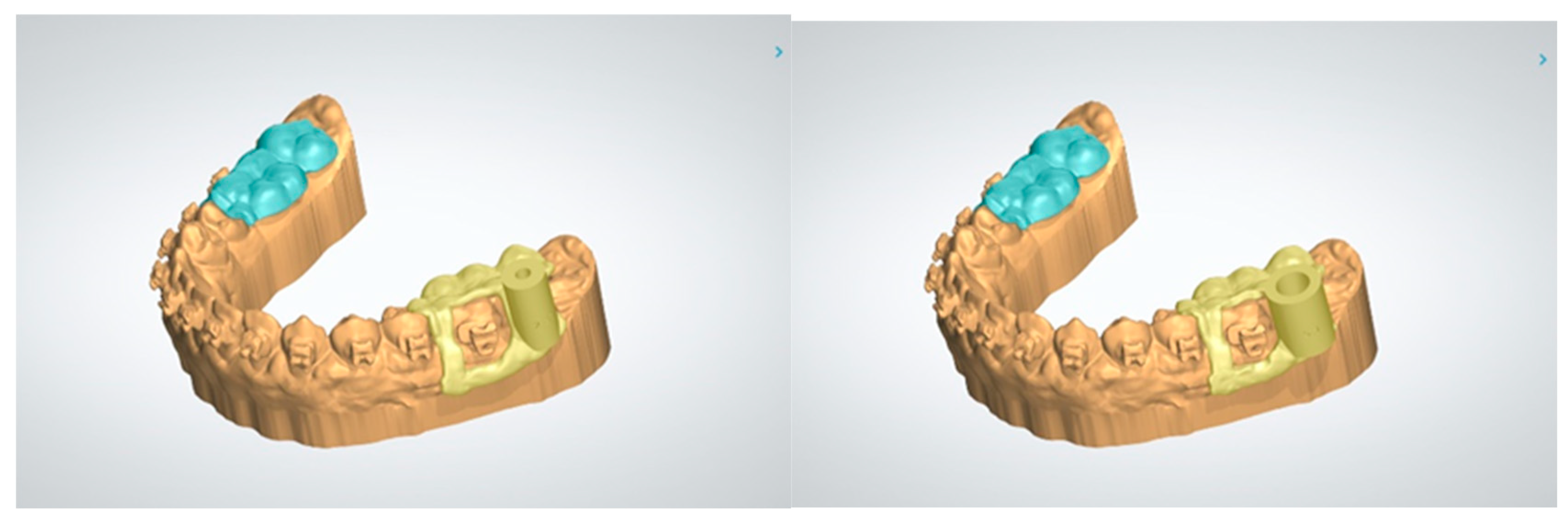
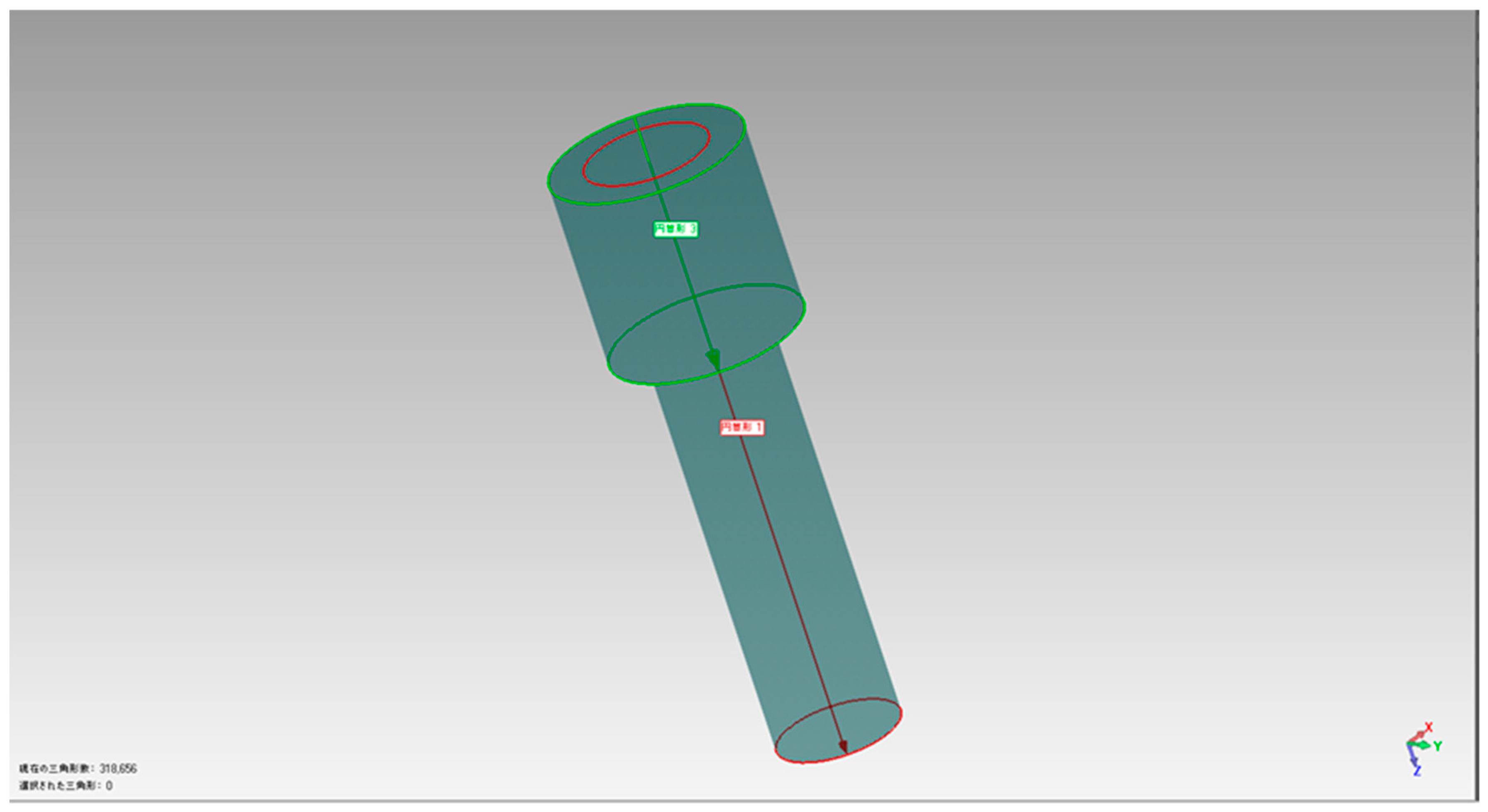
- The 3-Shape software completes the process of designing a surgical guide. By utilizing software, the diameter of the drilling bur and screw holder can be determined, ensuring no contact with the roots during the procedure. The 3-shape software simulates the screw placement within the bone's anatomic area. This simulation helps determine the tube design required for drilling and screw implantation.
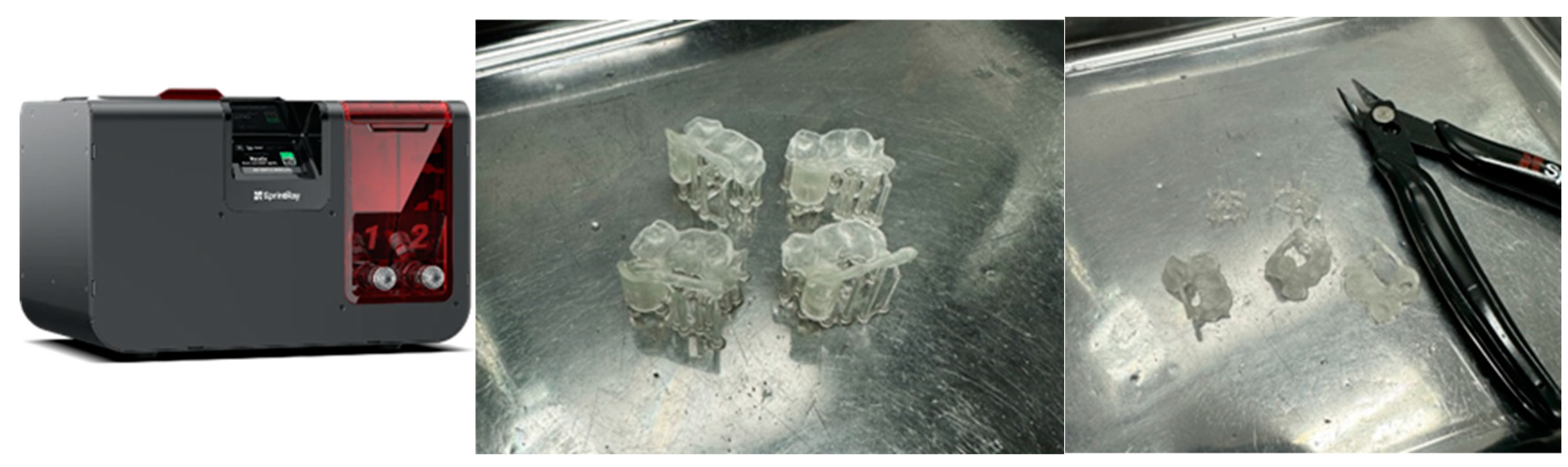
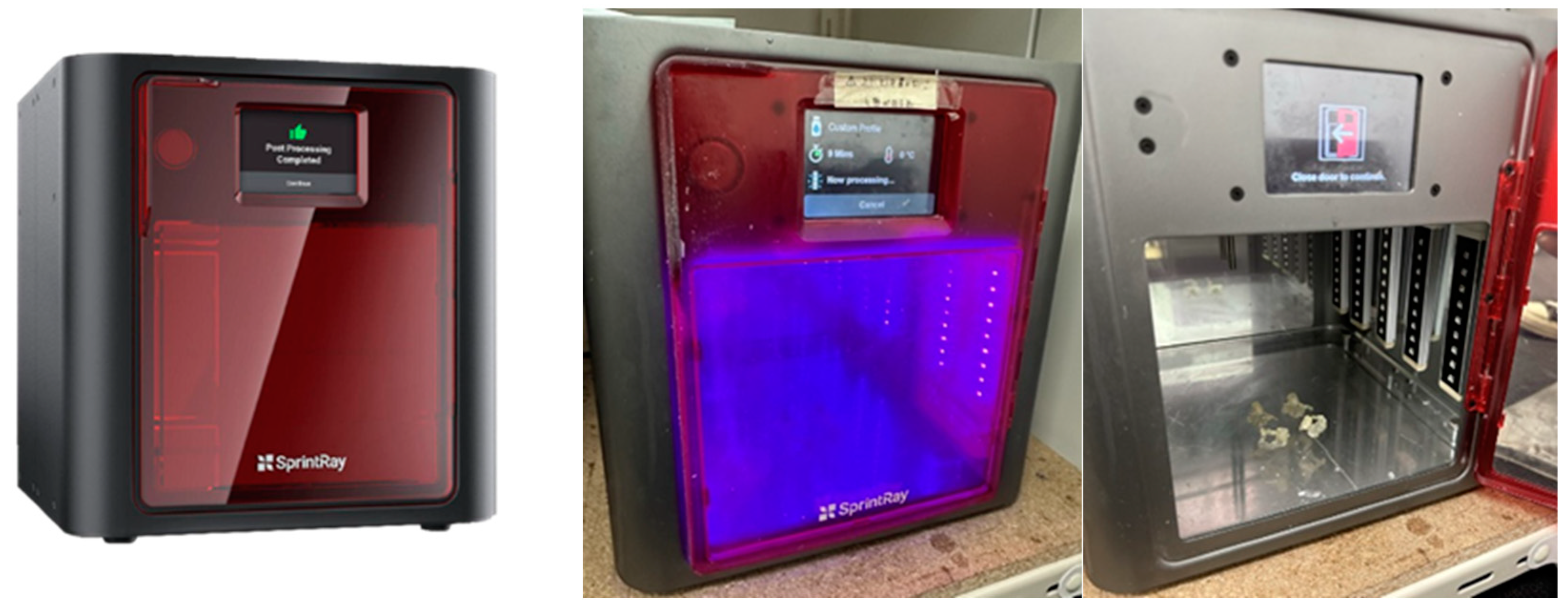
- Easy to print in a 3-D printer.
- Cleaning, washing, drying, and cutting of the supporting pillars, followed by post-curing.
- Checking and testing the surgical guide of both the drilling guide and screw holder guide is then placed upon the model of the jaw to check its fitness. When there are brackets, holes can be made to avoid retentions.

2. Printing


Conclusion
References
- 1. Mah J, Bergstrand F. Temporary anchorage devices: a status report. J Clin Orthod. 2005 Mar;39(3):132-6; discussion 136; quiz 153. PMID: 15888950.
- Bearn DR, Alharbi F. British Orthodontic Society national audit of temporary anchorage devices (T.A.D.s): report of the first thousand T.A.D.s placed. J Orthod. 2015 Sep;42(3):214-9. [CrossRef]
- Ahmed V KS, Rooban T, Krishnaswamy NR, Mani K, Kalladka G. Root damage and repair in patients with temporary skeletal anchorage devices. Am J Orthod Dentofacial Orthop. 2012 May;141(5):547-55. doi: 10.1016/j.ajodo.2011.11.014. [CrossRef]
- Çelik Güler Ö, Malkoç S. Effects of orthodontic force on root surface damage caused by contact with temporary anchorage devices and on the repair process. Korean J Orthod. 2019 Mar;49(2):106-115. doi: 10.4041/kjod.2019.49.2.106. Epub 2019 Mar 19. [CrossRef]
- Marc Schätzle, Roland Männchen, Marcel Zwahlen, Niklaus P. Lang Survival and failure rates of orthodontic temporary anchorage devices: a systematic review Clinical Oral Implants Research 09 November 2009 Wiley. [CrossRef]
- Yi-Jane Chen, Hao-Hueng Chang, Hsing-Yi Lin, Eddie Hsian-Hua Lai, Hsin-Chia Hung, Chung-Chen Jane Yao Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices 16 October 2008. [CrossRef]
- Manuel Nienkemper, Björn Ludwig, Risk of root damage after using lateral cephalogram and intraoral scan for guided insertion of palatal miniscrews, Head & Face Medicine, 10.1186/s13005-022-00335-0, 18, 1, (2022). [CrossRef]
- Elena Riad Deglow, Miriam O′Connor Esteban, Álvaro Zubizarreta-Macho, Sofĺa Hernández Montero, Georgia Tzironi, Francesc Abella Sans, Alberto Albaladejo Martínez, Novel digital technique to analyze the accuracy and intraoperative complications of orthodontic self-tapping and self-drilling microscrews placement techniques: An in vitro study, American Journal of Orthodontics and Dentofacial Orthopedics, 10.1016/j.ajodo.2021.03.020, 162, 2, (201-207), (2022). [CrossRef]
- Sarah Abu Arqub, Vaibhav Gandhi, Shivam Mehta, Ledjo Palo, Madhur Upadhyay, Sumit Yadav, Survival estimates and risk factors for failure of palatal and buccal mini-implants, The Angle Orthodontist, 10.2319/090720-777.1, 91, 6, (756-763), (2021). [CrossRef]
- Amin Golshah, Kimia Gorji, Nafiseh Nikkerdar, Effect of miniscrew insertion angle in the maxillary buccal plate on its clinical survival: a randomized clinical trial, Progress in Orthodontics, 10.1186/s40510-021-00370-8, 22, 1, (2021). [CrossRef]
- Amin Golshah, Mahya Salahshour, Nafiseh Nikkerdar, Interradicular distance and alveolar bone thickness for miniscrew insertion: a CBCT study of Persian adults with different sagittal skeletal patterns, B.M.C. Oral Health, 10.1186/s12903-021-01891-8, 21, 1, (2021). [CrossRef]
- Diana Milena Ramírez-Ossa, Natalia Escobar-Correa, Maria Antonia Ramírez-Bustamante, Andrés A. Agudelo-Suárez, An Umbrella Review Of The Effectiveness Of Temporary Anchorage Devices And The Factors That Contribute To Their Success Or Failure, Journal of Evidence Based Dental Practice, 10.1016/j.jebdp.2020.101402, (101402), (2020). [CrossRef]
- Barbara Kirnbauer, Petra Rugani, Elisabeth Santigli, Philipp Tepesch, Kamran Ali, Norbert Jakse, Fully guided placement of orthodontic miniscrews— a technical report, Australasian Orthodontic Journal, 10.21307/aoj-2020-035, 35, 1, (71-74), (2021). [CrossRef]
- Vercruyssen M, Laleman I, Jacobs R, Quirynen M. Computer-supported implant planning and guided surgery: a narrative review. Clin. Oral Impl. Res. 26 (Suppl. 11), 2015, 69–76. [CrossRef]
- Hämmerle CHF, Cordaro L, van Assche N, Benic GI, Bornstein M, Gamper F, Gotfredsen K, Harris D, Hürzeler M, Jacobs R,Kapos T, Kohal RJ, Patzelt S.B.M., Sailer I, Tahmaseb A, Vercruyssen M, Wismeijer D. Digital technologies to support planning, treatment, and fabrication processes and outcome assessments in implant dentistry. Summary and consensus statements. The 4th E.A.O. consensus conference 2015. Clin. Oral Impl. Res. 26 (s11), 2015, 97–101. [CrossRef]
- Apostolakis, D., Kourakis, G. CAD/CAM implant surgical guides: maximum errors in implant positioning attributable to the properties of the metal sleeve/osteotomy drill combination. Int J Implant Dent 4, 34 (2018). [CrossRef]
- Park HS, Lee YJ, Jeong SH, Kwon TG. Bone density of the alveolar and basal bone in the maxilla and the mandible. Am J Orthod Dentofacial Orthop. 2006. [CrossRef]
- Cho WH. Influence of the operator's experience and drilling sites on the root contact during drilling for micro-implants insertion [thesis]. Daegu, Korea: Kyungpook University; 2005.
- Kuroda S, Yamada K, Deguchi T, Hashimoto T, Kyung H-M, Takano-Yamamoto T. Root proximity is a major factor for screw failure in orthodontic anchorage. Am J Orthod Dentofacial Orthop. 2006. [CrossRef]
- Arisan V, Karabuda CZ, Mumcu E, Özdemir T. Implant positioning errors in freehand and computer-aided placement methods: a single-blind clinical comparative study. Int J Oral Maxillofac Implants. 2013 Jan-Feb;28(1):190-204. PMID: 23377066. [CrossRef]
- Willmann, B. Wilmes, D. Drescher, Düsseldorf, Digitale Mini-Implantat getragene Suprakonstruktionen – Design und Workflows J. Compr. Dentof. Orthod. + Orthop. (COO) Umf. Dentof. Orthod. u. Kieferorthop. (UOO) No. 3-4 / 2019 (c).
- Willmann, B. Wilmes, D. Drescher, Clinical use of digital Workflow Exemplified by Mini Implant. Inf. Orthod Kieferorthop 2020; 52: 121-127.
- S. Graf, S. Vasudavan, B. Wilmes CAD/CAM Metallic Printing of a Skeletally Anchored Upper Molar Distalizer JCO/2020, 140-149.
- Petrey JS, Saunders MM, Kluemper GT, Cunningham LL, Beeman CS. Temporary anchorage device insertion variables: effects on retention. Angle Orthod. 2010 Jul;80(4):446-53. doi: 10.2319/070309-376.1. PMID: 20482347; PMCID: PMC8966450. [CrossRef]
- Yan Chen, Ji-Wan Lee, Woo-Hyung Cho, Hee-Moon Kyung Potential of self-drilling orthodontic microimplants under immediate loading. AJO-DO Vol. 137Issue 4p496–502 2010. [CrossRef]
- Wilmes B, Ludwig B, Vasudavan S, Nienkemper M, Drescher D. The T-Zone: Median vs. Paramedian Insertion of Palatal Mini-Implants. J Clin Orthod. 2016 Sep;50(9):543-551. PMID: 27809213Özer AlkanYeşim Kaya The thickness of posterior buccal attached gingiva at common miniscrew insertion sites in subjects with different facial types. AJO-DO Vol. 156Issue 6p800–807, 2019. [CrossRef]
- Ka Fai Andy WongYifan Lin. Thickness of buccal attached gingiva at miniscrew insertion sites Vol. 158Issue 2p160–161 Published online: 2020. [CrossRef]
- Chen YJ, Chang HH, Lin HY, Lai EH, Hung HC, Yao CC. Stability of miniplates and miniscrews used for orthodontic anchorage: experience with 492 temporary anchorage devices. Clin Oral Implants Res. 2008 Nov;19(11):1188-96. PMID: 18983323. [CrossRef]
- Mormann WH, Brandestini M, Lutz F, Barbakow F.Chairside Computer Aided Direct Ceramic Inlays. Quintessence Int 1989;20:329-339.
- Impellizzeri, A.; Horodynski, M.; De Stefano, A.; Palaia, G.; Polimeni, A.; Romeo, U.; Guercio-Monaco, E.; Galluccio, G. CBCT and Intra-Oral Scanner: The Advantages of 3D Technologies in Orthodontic Treatment. Int. J. Environ. Res. Public Healthy 2020, 17, 9428. [CrossRef]
- Aristides BM. Advances in digital technology and orthodontics: A reference to the invisalign method.Med Sci Monit 2005;11:139-142.
- Wiechmann D, Rummel V, Thalheim A, Simon JS, Wiechmann L.Customized Brackets And Arch wires For Lingual Orthodontic Treatment.Am J Orthod Dentofac Orthop 2003;124:593-599. [CrossRef]
- Liu H, Liu D, Wang G, Wang C, Zhao Z.Accuracy of surgical positioning of orthodontic mini screws with a computer-aided design and manufacturing template. Am JOrthod Dentofac Orthop 2010;137:728e1-28e10. [CrossRef]
- Bae MJ, Kim JY, Park JT, Cha JY, Kim HJ, Yu HS, Hwang CJ. Accuracy of miniscrew surgical guides assessed from cone-beam computed tomography and digital models. Am J Orthod Dentofac Orthop. 2013;143(6):893–901. [CrossRef]
- Möhlhenrich SC, Brandt M, Kniha K, Prescher A, Hölzle F, Modabber A, Wolf M, Peters F. Accuracy of orthodontic mini-implants placed at the anterior palate by tooth-borne or gingiva-borne guide support: a cadaveric study. Clin Oral Investig. 2019;23(12):4425–31. [CrossRef]
- Cassetta M, Giansanti M. Accelerating orthodontic tooth movement: a new, minimally-invasive corticotomy technique using a 3D-printed surgical template. Med Oral Patol Oral Cir Bucal. 2016;21(4):e483–7. [CrossRef]
- Cassetta M, Altieri F, Di Giorgio R, Barbato E. Palatal orthodontic miniscrew insertion using a CAD-CAM surgical guide: description of a technique. Int J Oral Maxillofac Surg. 2018;47(9):1195–8. [CrossRef]
- Iodice G, Nanda R, Drago S, Repetto L, Tonoli G, Silvestrini-Biavati A, Migliorati M. Accuracy of direct insertion of TADs in the anterior palate with respect to a 3D-assisted digital insertion virtual planning. Orthod Craniofac Res. 2022;25(2):192–8. [CrossRef]
- Möhlhenrich, S.C.; Brandt, M.; Kniha, K.; Bock, A.; Prescher, A.; Hölzle, F.; dabber, A.; Danesh, G. Suitability of virtual plaster models superimposed with the lateral cephalogram for guided paramedian orthodontic mini-implant placement with regard to the bone support. J. Orofac. Orthop. Fortschr. Der Kieferorthopädie 2020, 81, 340–349. [CrossRef]
- Davidowitz G, Kotick PG. (2011), "The use of CAD/CAM in dentistry.", Dent Clin North Am, 55 (3): 559–570, doi:10.1016/j.cden.2011.02.011, PMID 21726690. [CrossRef]
- Lee, R.J.; Weissheimer, A.; Pham, J.; Go, L.; Menezes, L.; Redmond, W.R.; Loos, J.F.; Sameshima, G.T.; Tong, H. Three-dimensional monitoring of root movement during orthodontic treatment. Am. J. Orthod. Dentofac. Orthop. 2015, 147, 132–142. [CrossRef]
- Cassetta M, Giansanti M. Accelerating orthodontic tooth movement: A new, minimally-invasive corticotomy technique using a 3D-printed surgical template. Med Oral Patol Oral Cir Bucal. 2016 Jul 1;21(4):e483-7. PMID: 27031067; PMCID: PMC4920463. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




