Submitted:
25 July 2023
Posted:
25 July 2023
You are already at the latest version
Abstract
Keywords:
Introduction
Materials and methods
Data source
Variables understudy
Statistical Analysis
Joinpoint regression for trend analysis (1990-2019)
Estimation of Age period cohort effects on CVD mortality
Results
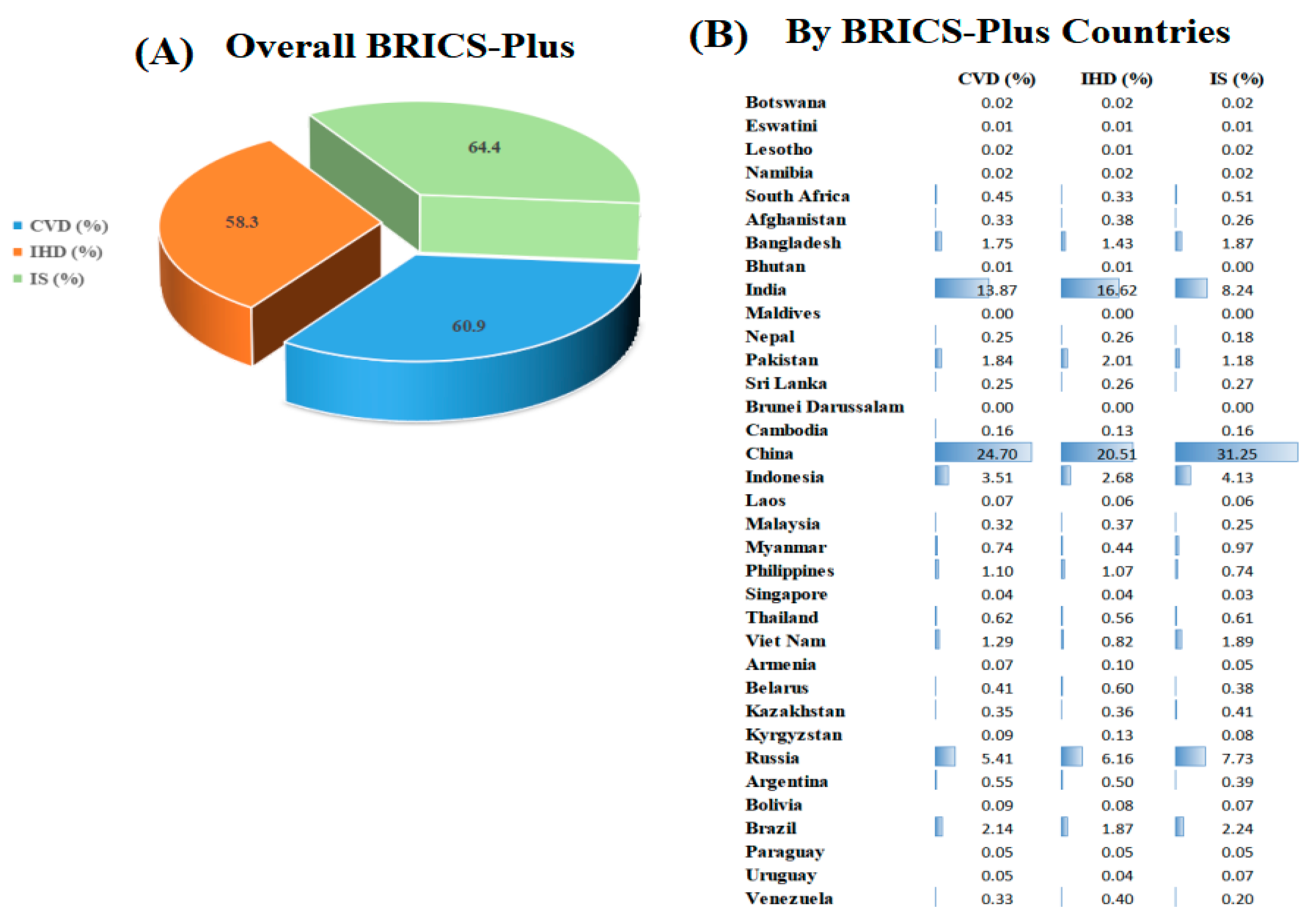
Trends of cause-specific CVD mortality
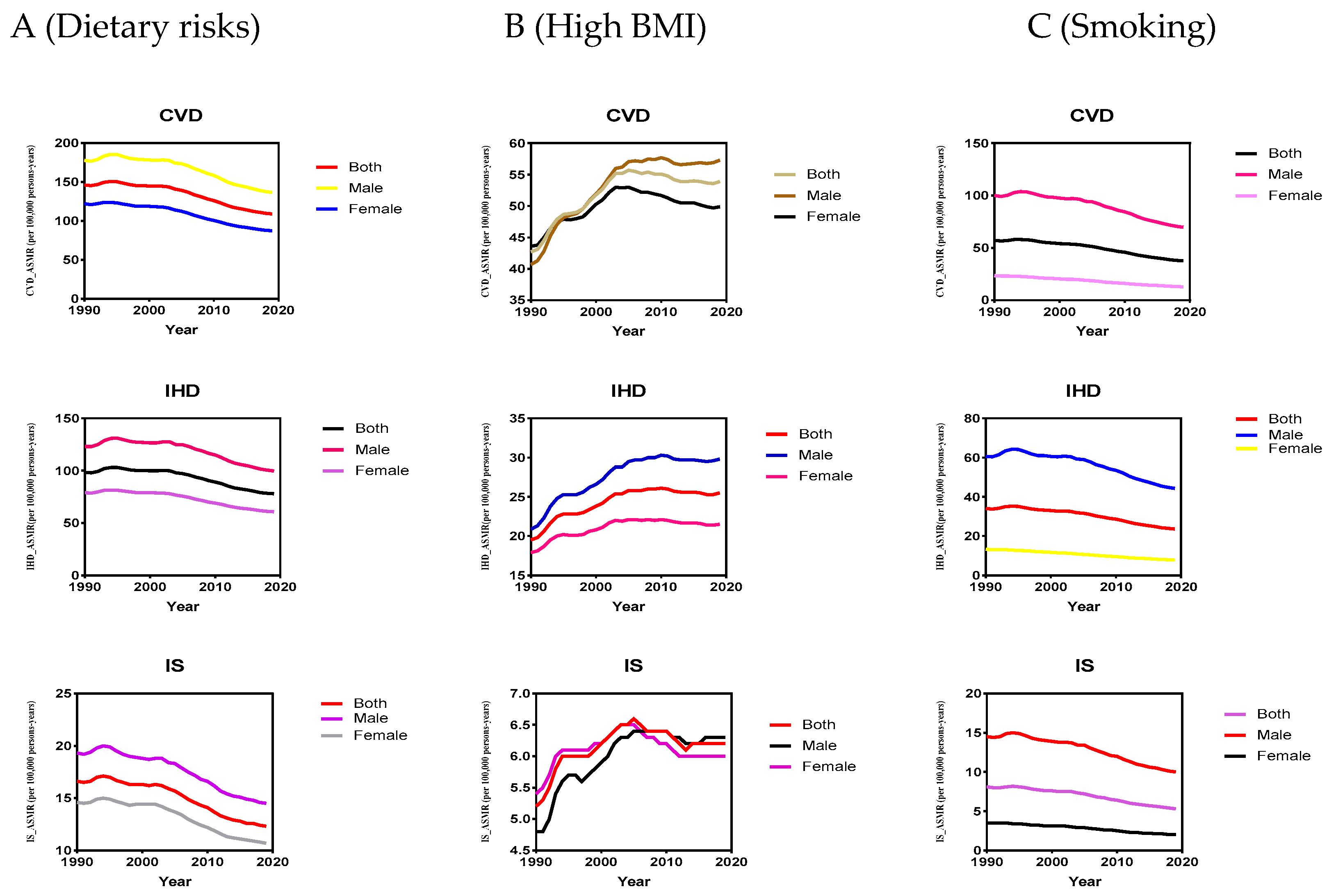
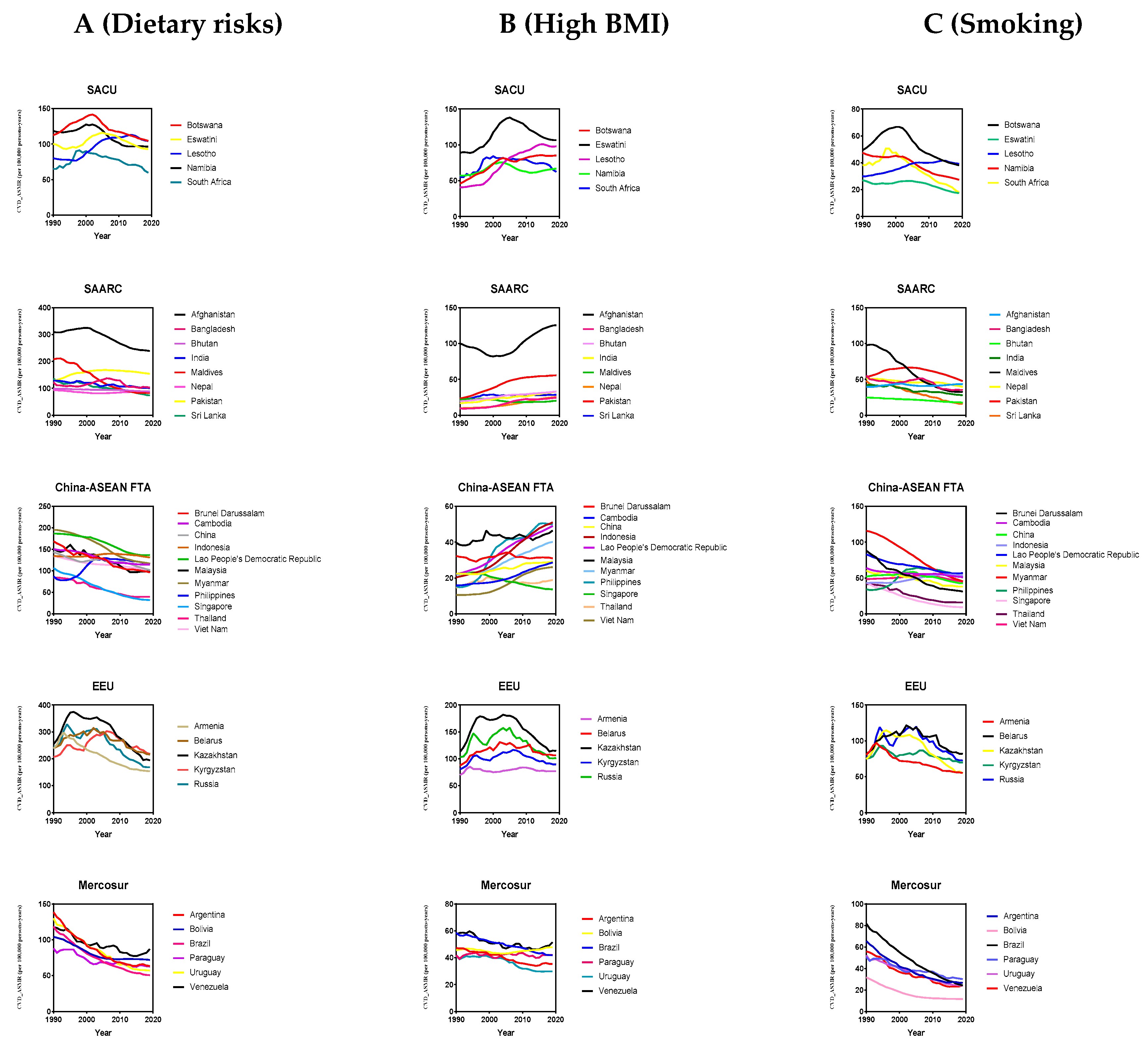
Trends of CVD mortality attributable to modifiable risk factors
Age-specific CVD burden attributable to modifiable risk factors
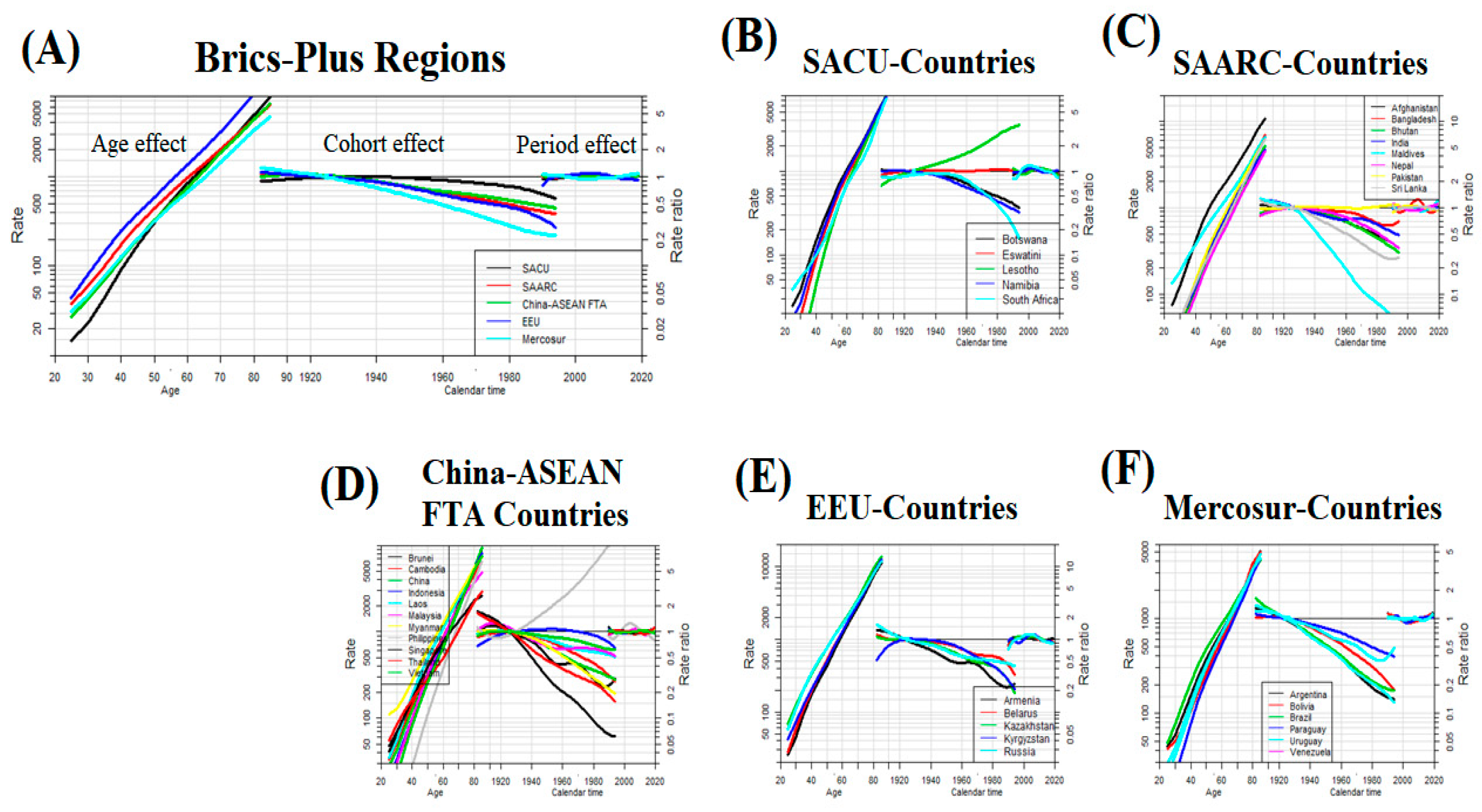
Age-period-cohort effects on CVD mortality across the BRICS-Plus
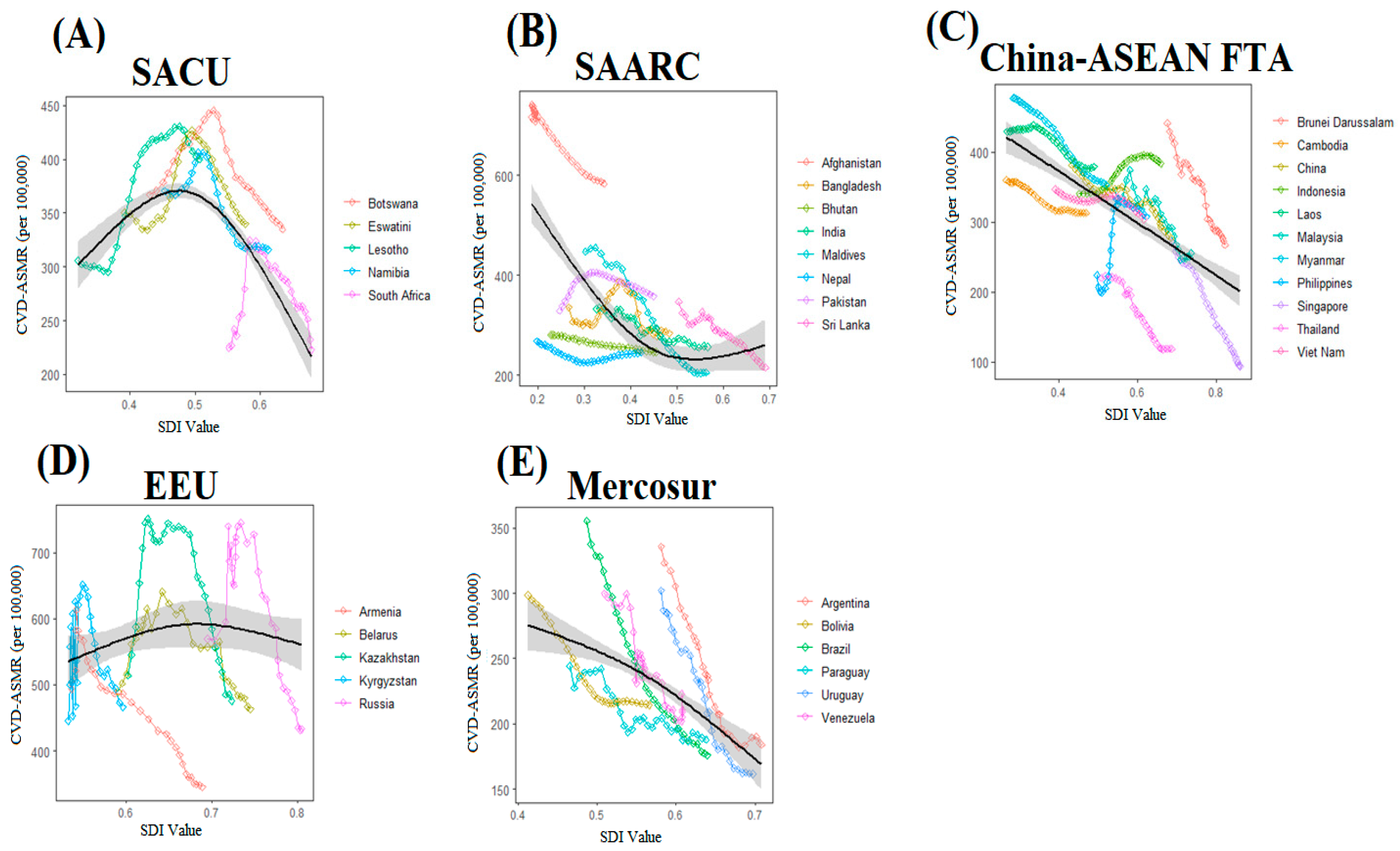
Impact of sociodemographic transitions on CVD mortality across the BRICS-Plus
Discussion
Overall CVD mortality
CVD mortality attributable to modifiable risk factors
Age-period-cohort effects on CVD mortality across the BRICS-Plus
Sociodemographic transitions and CVD mortality across the BRICS-Plus
Limitations
Conclusion and Implications
Author Contributions
Funding
Availability of data and materials
Acknowledgments
Competing interests
Ethics approval and consent to participate
Consent for publication
Abbreviations
| BRICS-Plus | Brazil, Russia, India, China, South Africa, and 30 other countries |
| WHO | World Health Organization |
| SACU | South African Customs Union |
| SAARC | South Asian Association for Regional Cooperation |
| China-ASEAN FTA | China-ASEAN Free Trade Area |
| EEU | Eurasian Economic Union |
| SDI | Sociodemographic index |
| GBD | Global Burden of Disease |
| APC | Age-period-cohort |
| ML | Maximum Likelihood |
| RR | Rate ratio |
| AAPC | Average annual percentage change |
| ASMR | Age-standardized mortality rate |
| CVD | Cardiovascular disease |
| IHD | Ischemic heart diseases |
| IS | Ischemic stroke |
| BMI | Body mass-index |
References
- Roth Gregory, A.; Mensah George, A.; Johnson Catherine, O.; Addolorato, G.; Ammirati, E.; Baddour Larry, M.; Barengo Noël, C.; Beaton Andrea, Z.; Benjamin Emelia, J.; Benziger Catherine, P.; et al. Global Burden of Cardiovascular Diseases and Risk Factors, 1990–2019. Journal of the American College of Cardiology 2020, 76, 2982–3021. [Google Scholar] [CrossRef] [PubMed]
- Lozano, R.; Naghavi, M.; Foreman, K.; Lim, S.; Shibuya, K.; Aboyans, V.; Abraham, J.; Adair, T.; Aggarwal, R.; Ahn, S.Y.; et al. Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010. The Lancet 2012, 380, 2095–2128. [Google Scholar] [CrossRef] [PubMed]
- Roth Gregory, A.; Johnson, C.; Abajobir, A.; Abd-Allah, F.; Abera Semaw, F.; Abyu, G.; Ahmed, M.; Aksut, B.; Alam, T.; Alam, K.; et al. Global, Regional, and National Burden of Cardiovascular Diseases for 10 Causes, 1990 to 2015. Journal of the American College of Cardiology 2017, 70, 1–25. [Google Scholar] [CrossRef] [PubMed]
- Zou, Z.; Cini, K.; Dong, B.; Ma, Y.; Ma, J.; Burgner, D.P.; Patton, G.C. Time trends in cardiovascular disease mortality across the BRICS: an age-period-cohort analysis of key nations with emerging economies using the global burden of disease study 2017. Circulation 2020, 141, 790–799. [Google Scholar] [CrossRef]
- Lissovolik, Y. BRICS-plus: Alternative globalization in the making. Valdai papers 2017, 69, 1–12. [Google Scholar]
- Zhao, D.; Liu, J.; Wang, M.; Zhang, X.; Zhou, M. Epidemiology of cardiovascular disease in China: current features and implications. Nature Reviews Cardiology 2019, 16, 203–212. [Google Scholar] [CrossRef]
- Ribeiro, A.L.P.; Duncan, B.B.; Brant, L.C.; Lotufo, P.A.; Mill, J.G.; Barreto, S.M. Cardiovascular health in Brazil: trends and perspectives. Circulation 2016, 133, 422–433. [Google Scholar] [CrossRef]
- Reddy, P.; Sewpaul, R.; Sifunda, S.; James, S.; Yach, D.; Resnicow, K.; Mthembu, Z.; Mbewu, A. A decade of tobacco control: The South African case of politics, health policy, health promotion and behaviour change. South African Medical Journal 2013, 103, 835–840. [Google Scholar] [CrossRef]
- Chestnov, O. World Health Organization global action plan for the prevention and control of noncommunicable diseases. Geneva, Switzerland, 2013. [Google Scholar]
- Bin, W.; Le, Z.; Mubarik, S.; Fu, G.; Wang, Y. Prediction of cardiovascular diseases mortality-and disability-adjusted life-years attributed to modifiable dietary risk factors from 1990 to 2030 among East Asian countries and the world. Frontiers in nutrition 2022, 9. [Google Scholar]
- Vos, T.; Lim, S.S.; Abbafati, C.; Abbas, K.M.; Abbasi, M.; Abbasifard, M.; Abbasi-Kangevari, M.; Abbastabar, H.; Abd-Allah, F.; Abdelalim, A.; et al. Global burden of 369 diseases and injuries in 204 countries and territories, 1990–2019: a systematic analysis for the Global Burden of Disease Study 2019. The Lancet 2020, 396, 1204–1222. [Google Scholar] [CrossRef]
- Roth, G.A.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national age-sex-specific mortality for 282 causes of death in 195 countries and territories, 1980–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2018, 392, 1736–1788. [Google Scholar] [CrossRef] [PubMed]
- Kyu, H.H.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; Abdelalim, A.; et al. Global, regional, and national disability-adjusted life-years (DALYs) for 359 diseases and injuries and healthy life expectancy (HALE) for 195 countries and territories, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2018, 392, 1859–1922. [Google Scholar] [CrossRef] [PubMed]
- Carstensen, B.; Plummer, M.; Laara, E.; Hills, M. Carstensen MBJApfsaiePoC: Package ‘Epi’. 2013.
- Dicker, D.; Nguyen, G.; Abate, D.; Abate, K.H.; Abay, S.M.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F.; Abdela, J.; et al. Global, regional, and national age-sex-specific mortality and life expectancy, 1950–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2018, 392, 1684–1735. [Google Scholar] [CrossRef]
- Gakidou, E.; Afshin, A.; Abajobir, A.A.; Abate, K.H.; Abbafati, C.; Abbas, K.M.; Abd-Allah, F.; Abdulle, A.M.; Abera, S.F.; Aboyans, V.; et al. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet 2017, 390, 1345–1422. [Google Scholar] [CrossRef] [PubMed]
- Husain, M.J.; Datta, B.K.; Kostova, D.; Joseph, K.T.; Asma, S.; Richter, P.; Jaffe, M.G.; Kishore, S.P. Access to cardiovascular disease and hypertension medicines in developing countries: an analysis of essential medicine lists, price, availability, and affordability. Journal of the American Heart Association 2020, 9, e015302. [Google Scholar] [CrossRef]
- Brunner, H.; Cockcroft, J.R.; Deanfield, J.; Donald, A.; Ferrannini, E.; Halcox, J.; Kiowski, W.; Lüscher, T.F.; Mancia, G.; Natali, A.; et al. Endothelial function and dysfunction. Part II: Association with cardiovascular risk factors and diseases. A statement by the Working Group on Endothelins and Endothelial Factors of the European Society of Hypertension*. Journal of Hypertension 2005, 23. [Google Scholar] [CrossRef] [PubMed]
- Amiri, P.; Mohammadzadeh-Naziri, K.; Abbasi, B.; Cheraghi, L.; Jalali-Farahani, S.; Momenan, A.A.; Amouzegar, A.; Hadaegh, F.; Azizi, F. Smoking habits and incidence of cardiovascular diseases in men and women: findings of a 12 year follow up among an urban Eastern-Mediterranean population. BMC Public Health 2019, 19, 1042. [Google Scholar] [CrossRef]
- Miller, V.; Webb, P.; Cudhea, F.; Shi, P.; Zhang, J.; Reedy, J.; Erndt-Marino, J.; Coates, J.; Mozaffarian, D. Global dietary quality in 185 countries from 1990 to 2018 show wide differences by nation, age, education, and urbanicity. Nature Food 2022, 3, 694–702. [Google Scholar] [CrossRef]
- Murray, C.J. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis forthe Global Burden of Disease Study. Lancet 2019, 393, 1958–1972. [Google Scholar]
- Jousilahti, P.; Laatikainen, T.; Salomaa, V.; Pietilä, A.; Vartiainen, E.; Puska, P. 40-year CHD mortality trends and the role of risk factors in mortality decline: the North Karelia project experience. Global heart 2016, 11, 207–212. [Google Scholar] [CrossRef]
- Ford, E.S.; Capewell, S. Proportion of the decline in cardiovascular mortality disease due to prevention versus treatment: public health versus clinical care. Annual review of public health 2011, 32, 5–22. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Devlin, H.M.; Smith, B.; Imperatore, G.; Thomas, W.; Lobelo, F.; Ali, M.K.; Norris, K.; Gruss, S.; Bardenheier, B. Effect of lifestyle interventions on cardiovascular risk factors among adults without impaired glucose tolerance or diabetes: A systematic review and meta-analysis. PloS one 2017, 12, e0176436. [Google Scholar] [CrossRef] [PubMed]
- Wang, Z.; Hu, S.; Sang, S.; Luo, L.; Yu, C. Age–period–cohort analysis of stroke mortality in China: data from the Global Burden of Disease Study 2013. Stroke 2017, 48, 271–275. [Google Scholar] [CrossRef] [PubMed]
- Rosenberg, P.S.; Anderson, W.F. Proportional hazards models and age–period–cohort analysis of cancer rates. Statistics in medicine 2010, 29, 1228–1238. [Google Scholar] [CrossRef]
- Rodgers, J.L.; Jones, J.; Bolleddu, S.I.; Vanthenapalli, S.; Rodgers, L.E.; Shah, K.; Karia, K.; Panguluri, S.K. Cardiovascular Risks Associated with Gender and Aging. J Cardiovasc Dev Dis 2019, 6. [Google Scholar] [CrossRef] [PubMed]
- Yazdanyar, A.; Newman, A.B. The burden of cardiovascular disease in the elderly: morbidity, mortality, and costs. Clinics in geriatric medicine 2009, 25, 563–577. [Google Scholar] [CrossRef]
- Stefler, D.; Azarova, A.; Irdam, D.; Scheiring, G.; Murphy, M.; McKee, M.; King, L.; Bobak, M. Smoking, alcohol and cancer mortality in Eastern European men: Findings from the PrivMort retrospective cohort study. International journal of cancer 2018, 143, 1128–1133. [Google Scholar] [CrossRef]
- Starodubov, V.I.; Marczak, L.B.; Varavikova, E.; Bikbov, B.; Ermakov, S.P.; Gall, J.; Glenn, S.D.; Griswold, M.; Idrisov, B.; Kravchenko, M. The burden of disease in Russia from 1980 to 2016: a systematic analysis for the Global Burden of Disease Study 2016. The Lancet 2018, 392, 1138–1146. [Google Scholar] [CrossRef]
- Nichol J: HEALTH-RELATED ISSUES IN RUSSIA AND EURASIA: CONTEXT AND ISSUES FOR CONGRESS. Russia, China Eurasia 2011, 27, 367.
- Rechel, B.; McKee, M. Health reform in central and eastern Europe and the former Soviet Union. The Lancet 2009, 374, 1186–1195. [Google Scholar] [CrossRef]
- Grigoriev, P.; Meslé, F.; Shkolnikov, V.M.; Andreev, E.; Fihel, A.; Pechholdova, M.; Vallin, J. The recent mortality decline in Russia: beginning of the cardiovascular revolution? Population Development review 2014, 40, 107–129. [Google Scholar] [CrossRef]
- Movsisyan, N.K.; Vinciguerra, M.; Medina-Inojosa, J.R.; Lopez-Jimenez, F. Cardiovascular Diseases in Central and Eastern Europe: A Call for More Surveillance and Evidence-Based Health Promotion. Ann Glob Health 2020, 86, 21. [Google Scholar] [CrossRef]
- World Health, O. WHO country cooperation strategy at a glance: Lesotho. In. Geneva: World Health Organization; 2018.
- Tseole, N.P. Understanding modifiable risk factors for non-communicable diseases among adult men in Maseru, Lesotho. 2018.
- Angeles-Agdeppa, I.; Sun, Y.; Tanda, K.V. Dietary pattern and nutrient intakes in association with non-communicable disease risk factors among Filipino adults: a cross-sectional study. Nutrition Journal 2020, 19, 79. [Google Scholar] [CrossRef]
- Bellew, B.; Antonio, M.; Limpin, M.; Alzona, L.; Trinidad, F.; Dorotheo, U.; Yapchiongco, R.; Garcia, R.; Anden, A.A. Addressing the tobacco epidemic in the Philippines: progress since ratification of the WHO FCTC. Public Health Action 2013, 3, 103–108. [Google Scholar] [CrossRef] [PubMed]
- Lim, S.S.; Allen, K.; Bhutta, Z.A.; Dandona, L.; Forouzanfar, M.H.; Fullman, N.; Gething, P.W.; Goldberg, E.M.; Hay, S.I.; Holmberg, M.; et al. Measuring the health-related Sustainable Development Goals in 188 countries: a baseline analysis from the Global Burden of Disease Study 2015. The Lancet 2016, 388, 1813–1850. [Google Scholar] [CrossRef]
- Omram, A.R. The epidemiologic transition: a theory of the epidemiology of population change. Bulletin of the World Health Organization 2001, 79, 161–170. [Google Scholar]
- Jagannathan, R.; Patel, S.A.; Ali, M.K.; Narayan, K. Global updates on cardiovascular disease mortality trends and attribution of traditional risk factors. Current diabetes reports 2019, 19, 1–12. [Google Scholar] [CrossRef]
- Li, Z.; Lin, L.; Wu, H.; Yan, L.; Wang, H.; Yang, H.; Li, H. Global, regional, and national death, and disability-adjusted life-years (DALYs) for cardiovascular disease in 2017 and trends and risk analysis from 1990 to 2017 using the global burden of disease study and implications for prevention. Frontiers in public health 2021, 9. [Google Scholar] [CrossRef]
- Afshin, A.; Sur, P.J.; Fay, K.A.; Cornaby, L.; Ferrara, G.; Salama, J.S.; Mullany, E.C.; Abate, K.H.; Abbafati, C.; Abebe, Z.; et al. Health effects of dietary risks in 195 countries, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. The Lancet 2019, 393, 1958–1972. [Google Scholar] [CrossRef]
| CVD | ASMR/100,000 | Deaths, n×1000 | ||||
|---|---|---|---|---|---|---|
| 1990 (95%UI) | 2019 (95%UI) | AAPC (95%CI) | 1990 (95%UI) | 2019 (95%UI) | AAPC (95%CI) | |
| BRICS-Plus | 367 (407, 326) | 296 (346, 248) | -0.7 (-0.8, -0.6) | 6197 (6798, 5610) | 11310 (12896, 9704) |
2.1 (1.9, 2.3) |
| SACU | ||||||
| Botswana | 366 (448, 302) | 334 (425, 258) | -0.3 (-0.4, -0.2) | 1.6 (2.1, 1.3) | 3.5 (4.5, 2.6) | 2.6 (2.4, 2.7) |
| Eswatini | 350 (405, 293) | 339 (441, 258) | -0.1 (-0.4, 0.2) | 0.8 (0.9, 0.6) | 1.5 (2.1, 1.1) | 2.0 (1.8, 2.3) |
| Lesotho | 305 (354, 261) | 399 (497, 311) | 0.9 (0.8, 1.0) | 2.5 (2.9, 2.1) | 4.1 (5.1, 3.1) | 1.6 (1.4, 1.7) |
| Namibia | 370 (425, 313) | 316 (381, 263) | -0.5 (-0.7, -0.4) | 2.2 (2.5, 1.8) | 3.7 (4.5, 3.1) | 1.8 (1.6, 2.0) |
| South Africa | 225 (244, 202) | 222 (236, 203) | -0.1 (-0.6, 0.6) | 42 (46, 38) | 82 (87, 76) | 2.3 (1.7, 2.9) |
| SAARC | ||||||
| Afghanistan | 716 (829, 608) | 583 (681, 473) | -0.7 (-0.8, -0.6) | 44 (52, 37) | 61 (75, 49) | 1.1 (1.0, 1.2) |
| Bangladesh | 335 (374, 290) | 283 (341, 220) | -0.4 (-0.9, 0.1) | 138 (154, 119) | 324 (394, 250) | 3.2 (2.8, 3.7) |
| Bhutan | 280 (343, 220) | 246 (286, 198) | -0.5 (-0.5, -0.4) | 0.5 (0.7, 0.4) | 1.2 (1.4, 0.9) | 2.6 (2.5, 2.7) |
| India | 332 (371, 297) | 256 (292, 220) | -1.0 (-1.6, -0.3) | 1201 (1328, 1080) | 2574 (2940, 2215) |
2.7 (1.9, 3.4) |
| Maldives | 446 (481, 414) | 205 (239, 174) | -2.7 (-3.0, -2.4) | 0.3 (0.3, 0.2) | 0.5 (0.6, 0.4) | 1.6 (1.4, 1.9) |
| Nepal | 267 (332, 218) | 245 (286, 199) | -0.3 (-0.4, -0.2) | 21 (26, 17) | 46 (54, 37) | 2.7 (2.5, 2.8) |
| Pakistan | 329 (381, 279) | 357 (423, 307) | 0.3 (0.3, 0.4) | 172 (197, 147) | 341 (405, 291) | 2.4 (2.3, 2.4) |
| Sri Lanka | 346 (372, 318) | 215 (270, 163) | -1.6 (-2.0, -1.3) | 30 (32, 27) | 46 (59, 35) | 1.5 (1.2, 1.9) |
| China-ASEAN FTA | ||||||
| Brunei Darussalam | 441 (475, 404) | 266 (296, 240) | -1.7 (-2.2, -1.2) | 0.3 (0.3, 0.2) | 0.5 (0.5, 0.4) | 1.6 (1.4, 1.8) |
| Cambodia | 359 (412, 313) | 312 (349, 265) | -0.5 (-0.5, -0.4) | 13 (15, 12) | 30 (34, 25) | 2.7 (2.6, 2.8) |
| China | 381 (426, 341) | 276 (312, 239) | -1.1 (-1.4, -0.8) | 2423 (2712, 2165) | 4584 (5209, 3955) |
2.2 (1.9, 2.6) |
| Indonesia | 340 (375, 301) | 383 (418, 328) | 0.4 (0.4, 0.5) | 278 (304, 250) | 651 (721, 554) | 3.0 (2.9, 3.0) |
| Laos | 428 (517, 348) | 379 (440, 318) | -0.4 (-0.5, -0.4) | 7.5 (9.1, 6.1) | 13 (16, 11) | 2.0 (2.0, 2.1) |
| Malaysia | 347 (363, 326) | 255 (309, 207) | -1.0 (-1.7, -0.3) | 28 (29, 26) | 58 (71, 47) | 2.6 (1.7, 3.4) |
| Myanmar | 477 (570, 400) | 352 (401, 313) | -1.1 (-1.1, -1.0) | 96 (116, 79) | 138 (159, 120) | 1.2 (1.1, 1.3) |
| Philippines | 223 (246, 200) | 307 (356, 254) | 1.3 (0.8, 1.7) | 45 (53, 41) | 204 (241, 165) | 5.5 (5.1, 5.8) |
| Singapore | 271 (280, 254) | 93 (100, 81) | -3.6 (-3.9, -3.3) | 5.1 (5.2, 4.8) | 6.8 (7.3, 6.1) | 1.1 (0.9, 1.3) |
| Thailand | 219 (244, 196) | 118 (150, 90) | -2.1 (-2.5, -1.7) | 63 (71, 57) | 115 (147, 88) | 2.0 (1.7, 2.4) |
| Viet Nam | 346 (405, 293) | 303 (348, 258) | -0.4 (-0.5, -0.4) | 124 (145, 104) | 240 (278, 202) | 2.3 (2.3, 2.4) |
| EEU | ||||||
| Armenia | 493 (510, 462) | 345 (396, 295) | -1.3 (-1.7, -0.8) | 10.6 (10.9, 10.1) | 13 (15, 11) | 0.7 (0.3, 1.1) |
| Belarus | 489 (506, 459) | 463 (571, 381) | -0.2 (-0.7, 0.3) | 59 (61, 56) | 75 (92, 62) | 0.8 (0.3, 1.3) |
| Kazakhstan | 513 (534, 485) | 476 (531, 421) | -0.3 (-0.6, 0.1) | 56 (58, 53) | 65 (73, 57) | 0.4 (-0.1, 0.8) |
| Kyrgyzstan | 445 (470, 415) | 466 (517, 416) | 0.2 (-0.4, 0.8) | 12 (13, 12) | 17 (19, 15) | 1.1 (0.3, 1.8) |
| Russia | 569 (584, 540) | 432 (485, 378) | -1.0 (-2.0, 0.1) | 890 (908, 856) | 1004 (1126, 880) | 0.4 (-0.6, 1.4) |
| Mercosur | ||||||
| Argentina | 335 (347, 315) | 183 (194, 168) | -2.0 (-2.5, -1.5) | 98 (101, 93) | 101 (107, 93) | 0.1 (-0.4, 0.6) |
| Bolivia | 298 (354, 244) | 214 (265, 161) | -1.1 (-1.2, -1.0) | 8.2 (9.8, 6.6) | 15 (19, 11) | 2.3 (2.2, 2.3) |
| Brazil | 355 (367, 332) | 175 (184, 158) | -2.4 (-2.6, -2.2) | 269 (277, 257) | 397 (417, 361) | 1.4 (1.1, 1.6) |
| Paraguay | 244 (269, 211) | 187 (235, 147) | -0.8 (-1.4, -0.1) | 5.1 (5.5, 4.3) | 9.9 (12.4, 7.8) | 2.4 (1.8, 3.1) |
| Uruguay | 302 (313, 282) | 161 (170, 146) | -2.1 (-2.5, -1.7) | 11 (11, 10) | 10 (10, 8) | -0.4 (-0.8, -0.1) |
| Venezuela | 299 (312, 279) | 222 (279, 176) | -1.0 (-1.9, -0.1) | 25 (26, 24) | 61 (77, 48) | 3.0 (2.1, 3.9) |
| Population | CVD (ASMR/100,000) | ||
|---|---|---|---|
| Dietary risks (AAPC (95%CI) | High BMI (AAPC (95%CI) | Smoking (AAPC (95%CI) | |
| BRICS-Plus | -1.0 (-1.1, -0.9) | 0.8 (0.7, 1.0) | -1.4 (-1.5, -1.3) |
| SACU | |||
| Botswana | -0.2 (-0.3, -0.1) | 2.1 (1.8, 2.5) | -0.9 (-1.0, -0.8) |
| Eswatini | -0.3 (-0.6, -0.1) | 0.6 (0.1, 1.1) | -1.6 (-1.8, -1.3) |
| Lesotho | 0.9 (0.8, 1.0) | 3.1 (2.9, 3.3) | 1.0 (0.8, 1.1) |
| Namibia | -0.7 (-0.8, -0.6) | 0.6 (0.4, 0.8) | -1.8 (-2.0, -1.7) |
| South Africa | -0.3 (-0.9, 0.4) | 0.4 (-0.2, 1.1) | -2.5 (-3.2, -1.8) |
| SAARC | |||
| Afghanistan | -0.9 (-0.9, -0.8) | 0.8 (0.5, 1.0) | 0.4 (0.3, 0.5) |
| Bangladesh | -0.4 (-0.9, 0.1) | 3.2 (2.8, 3.7) | -1.4 (-1.8, -1.0) |
| Bhutan | -0.4 (-0.5, -0.3) | 1.9 (1.8, 2.0) | -1.1 (-1.3, -1.0) |
| India | -0.8 (-1.6, -0.1) | 2.4 (2.0, 2.7) | -1.4 (-2.0, -0.8) |
| Maldives | -3.2 (-3.5, -2.9) | -0.3 (-0.5, -0.1) | -3.8 (-4.1, -3.5) |
| Nepal | -0.2 (-0.4, -0.1) | 3.4 (3.3, 3.5) | -0.9 (-1.0, -0.8) |
| Pakistan | 0.7 (0.6, 0.7) | 3.1 (2.9, 3.2) | -0.4 (-0.5, -0.3) |
| Sri Lanka | -2.1 (-2.5, -1.6) | 0.7 (0.3, 1.0) | -3.8 (-4.3, -3.3) |
| China-ASEAN FTA | |||
| Brunei Darussalam | -1.9 (-2.4, -1.5) | -0.1 (-0.3, 0.1) | -3.6 (-3.9, -3.3) |
| Cambodia | -0.9 (-1.0, -0.9) | 2.1 (2.0, 2.2) | -0.8 (-0.8, -0.7) |
| China | -1.2 (-1.5, -0.9) | 0.9 (0.4, 1.4) | -0.7 (-1.2, -0.3) |
| Indonesia | -0.1 (-0.2, -0.1) | 3.2 (3.2, 3.3) | 0.7 (0.7, 0.8) |
| Laos | -1.1 (-1.2, -1.0) | 2.8 (2.7, 2.9) | -1.3 (-1.4, -1.2) |
| Malaysia | -1.3 (-2.0, -0.7) | 0.6 (0.2, 1.0) | -1.5 (-2.2, -0.7) |
| Myanmar | -1.8 (-1.8, -1.7) | 2.2 (2.0, 2.3) | -3.2 (-3.3, -3.1) |
| Philippines | 1.1 (0.7, 1.6) | 4.3 (3.5, 5.1) | 1.5 (1.2, 1.8) |
| Singapore | -4.1 (-4.3, -3.8) | -1.6 (-1.9, -1.4) | -5.3 (-5.6, -5.0) |
| Thailand | -2.6 (-2.9, -2.2) | 0.9 (0.5, 1.3) | -3.4 (-4.2, -2.6) |
| Viet Nam | -1.0 (-1.0, -0.9) | 3.3 (3.1, 3.5) | -0.3 (-0.3, -0.2) |
| EEU | |||
| Armenia | -1.5 (-1.8, -1.2) | 0.3 (-0.1, 0.6) | -1.4 (-1.7, -1.0) |
| Belarus | -0.3 (-0.9, 0.3) | 0.6 (0.1, 1.2) | -0.1 (-1.2, 1.0) |
| Kazakhstan | -0.9 (-1.2, -0.6) | 0.1 (-0.3, 0.4) | -1.0 (-1.4, -0.5) |
| Kyrgyzstan | 0.3 (-0.4, 0.9) | 0.3 (-0.3, 0.9) | -0.2 (-0.7, 0.2) |
| Russia | -1.3 (-2.4, -0.2) | 0.1 (-1.0, 1.0) | -0.1 (-1.2, 1.1) |
| Mercosur | |||
| Argentina | -2.6 (-2.9, -2.3) | -0.9 (-1.4, -0.5) | -3.0 (-3.3, -2.8) |
| Bolivia | -1.2 (-1.4, -1.1) | 0.2 (0.1, 0.3) | -3.4 (-3.5, -3.3) |
| Brazil | -2.9 (-3.1, -2.7) | -1.1 (-1.4, -0.8) | -4.1 (-4.3, -3.8) |
| Paraguay | -1.1 (-1.8, -0.4) | 0.1 (-0.8, 0.9) | -1.7 (-2.4, -1.1) |
| Uruguay | -2.8 (-3.2, -2.3) | -1.0 (-1.4, -0.7) | -2.6 (-3.1, -2.0) |
| Venezuela | -1.2 (-1.7, -0.6) | -0.4 (-1.0, 0.1) | -3.0 (-3.6, -2.4) |
| Population | Male (AAPC (95%CI) | Female (AAPC (95%CI) | ||||
|---|---|---|---|---|---|---|
| Dietary risks | High BMI | Smoking | Dietary risks | High BMI | Smoking | |
| BRICS-Plus | -0.9 (-1.0, -0.8) | 1.2 (1.0,1.4) | -1.2 (-1.4, -1.1) | -1.1 (-1.2, -1.0) | 0.5 (0.3, 0.6) | -2.1 (-2.2, -2.0) |
| SACU | ||||||
| Botswana | -0.2 (-0.4, 0.1) | 3.2 (2.9, 3.5) | -0.7 (-1.0, -0.5) | -0.2 (-0.8, 0.3) | 1.6 (0.8, 2.6) | -1.1 (-1.9, -0.2) |
| Eswatini | -0.2 (-0.4, -0.1) | 1.3 (0.9, 1.7) | -1.5 (-1.6, -1.3) | -0.4 (-0.7, -0.1) | -0.1 (-0.5, 0.4) | -1.4 (-1.6, -1.2) |
| Lesotho | 0.7 (0.6, 0.8) | 3.7 (3.4, 4.1) | 1.1 (0.8, 1.3) | 1.0 (0.8, 1.3) | 2.6 (2.3, 2.9) | 1.0 (0.7, 1.3) |
| Namibia | -0.4 (-0.5, -0.2) | 1.4 (1.2, 1.6) | -1.6 (-1.7, -1.4) | -1.0 (-1.1, -0.8) | 0.1 (-0.2, 0.2) | -2.1 (-2.3, -1.9) |
| South Africa | -0.3 (-0.8, 0.1) | 1.1 (0.5, 1.6) | -2.2 (-2.8, -1.5) | -0.3 (-1.0, 0.4) | 0.1 (-0.7, 0.8) | -3.1 (-3.9, -2.3) |
| SAARC | ||||||
| Afghanistan | -1.0 (-1.1, -0.9) | 1.1 (0.9, 1.3) | 0.4 (0.3, 0.5) | -0.7 (-0.8, -0.6) | 0.5 (0.2, 0.8) | 0.8 (0.6, 1.0) |
| Bangladesh | -0.2 (-0.7, 0.3) | 3.9 (3.5, 4.3) | -1.2 (-1.6, -0.7) | -0.7 (-1.4, -0.1) | 2.8 (2.4, 3.3) | -1.9 (-2.4, -1.5) |
| Bhutan | -0.2 (-0.3, -0.1) | 2.5 (2.4, 2.7) | -1.1 (-1.2, -1.0) | -0.7 (-0.8, -0.7) | 1.4 (1.3, 1.5) | -1.8 (-2.0, -1.7) |
| India | -0.7 (-1.4, -0.1) | 2.6 (2.1, 3.0) | -1.3 (-1.9, -0.6) | -0.8 (-1.7, 0.1) | 2.1 (1.7, 2.5) | -1.0 (-1.7, -0.3) |
| Maldives | -2.8 (-3.1, -2.6) | 0.4 (0.2, 0.6) | -3.4 (-3.6, -3.1) | -3.7 (-4.3, -3.0) | -1.3 (-2.0, -0.6) | -5.2 (-6.0, -4.3) |
| Nepal | 0.3 (0.2, 0.4) | 4.2 (4.1, 4.3) | -0.3 (-0.5, -0.2) | -1.0 (-1.1, -0.9) | 2.6 (2.4, 2.7) | -1.7 (-1.8, -1.7) |
| Pakistan | 1.0 (0.9, 1.1) | 3.5 (3.4, 3.7) | -0.1 (-0.2, 0.1) | 0.3 (0.3, 0.4) | 2.6 (2.4, 2.7) | -0.9 (-1.0, -0.8) |
| Sri Lanka | -2.0 (-2.5, -1.5) | 0.6 (0.1, 1.1) | -3.4 (-3.9, -2.8) | -1.8 (-2.4, -1.1) | 0.7 (0.3, 1.1) | -3.9 (-4.5, -3.3) |
| China-ASEAN FTA | ||||||
| Brunei Darussalam | -1.7 (-2.6, -0.8) | 0.2 (-0.5, 0.8) | -3.4 (-4.1, -2.6) | -1.9 (-2.3, -1.4) | -0.3 (-0.6, -0.1) | -3.8 (-4.1, -3.6) |
| Cambodia | -0.7 (-0.8, -0.7) | 2.8 (2.7, 3.0) | -0.5 (-0.6, -0.5) | -1.1 (-1.2, -1.1) | 1.5 (1.4, 1.7) | -1.0 (-1.1, -1.0) |
| China | -0.8 (-1.1, -0.5) | 1.5 (1.3, 1.7) | -0.7 (-1.0, -0.5) | -1.7 (-1.9, -1.4) | 0.2 (-0.1, 0.5) | -0.6 (-1.0, -0.2) |
| Indonesia | 0.2 (0.1, 0.2) | 3.6 (3.5, 3.7) | 0.8 (0.7, 0.9) | -0.4 (-0.5, -0.4) | 2.9 (2.8, 3.1) | 0.7 (0.5, 0.8) |
| Laos | -1.1 (-1.2, -1.1) | 3.2 (3.1, 3.4) | -1.3 (-1.3, -1.2) | -1.1 (-1.2, -1.0) | 2.4 (2.3, 2.5) | -1.9 (-2.0, -1.8) |
| Malaysia | -1.2 (-2.1, -0.3) | 1.0 (0.6, 1.5) | -1.5 (-2.3, -0.7) | -1.5 (-2.2, -0.9) | 0.1 (-0.5, 0.5) | -2.3 (-3.1, -1.5) |
| Myanmar | -1.5 (-1.6, -1.4) | 2.3 (2.2, 2.5) | -2.6 (-2.7, -2.5) | -2.0 (-2.0, -1.9) | 1.9 (1.8, 2.1) | -4.1 (-4.2, -4.0) |
| Philippines | 1.5 (1.2, 1.7) | 4.5 (3.4, 5.6) | 1.8 (1.5, 2.1) | 0.7 (0.2, 1.1) | 4.0 (3.4, 4.7) | 0.9 (0.5, 1.3) |
| Singapore | -3.9 (-4.3, -3.6) | -1.3 (-1.5, -1.1) | -5.3 (-5.5, -5.0) | -4.4 (-4.7, -4.0) | -2.2 (-2.6, -1.8) | -6.2 (-6.5, -5.9) |
| Thailand | -2.5 (-3.3, -1.7) | 1.4 (0.9, 1.9) | -3.2 (-4.0, -2.4) | -2.8 (-3.1, -2.5) | 0.3 (-0.1, 0.5) | -5.1 (-5.4, -4.7) |
| Viet Nam | -0.6 (-0.7, -0.6) | 4.1 (3.8, 4.3) | -0.2 (-0.3, -0.2) | -1.5 (-1.5, -1.4) | 2.3 (2.2, 2.4) | -1.3 (-1.4, -1.2) |
| EEU | ||||||
| Armenia | -1.3 (-1.7, -1.0) | 1.1 (0.8, 1.3) | -1.4 (-1.9, -0.9) | -1.7 (-2.0, -1.4) | -0.3 (-0.8, 0.1) | -2.5 (-2.9, -2.1) |
| Belarus | -0.1 (-0.5, 0.4) | 1.4 (0.7, 2.0) | -0.1 (-0.7, 0.6) | -0.6 (-1.1, -0.2) | 0.1 (-0.3, 0.6) | -0.7 (-1.3, -0.1) |
| Kazakhstan | -1.0 (-1.3, -0.6) | 0.4 (-0.1, 0.8) | -1.1 (-1.6, -0.7) | -0.9 (-1.2, -0.6) | -0.2 (-0.5, 0.1) | -1.2 (-1.6, -0.8) |
| Kyrgyzstan | 0.1 (-0.7, 0.8) | 0.7 (0.2, 1.1) | -0.4 (-0.9, 0.1) | 0.3 (-0.3, 0.9) | 0.1 (-0.6, 0.7) | -0.3 (-0.9, 0.3) |
| Russia | -1.4 (-2.4, -0.3) | 0.4 (-0.7, 1.5) | -0.6 (-1.7, 0.6) | -1.5 (-2.6, -0.4) | -0.4 (-1.4, 0.6) | 0.4 (-0.6, 1.4) |
| Mercosur | ||||||
| Argentina | -2.6 (-2.9, -2.3) | -1.0 (-1.4, -0.6) | -3.1 (-3.4, -2.8) | -2.6 (-3.0, -2.3) | -0.9 (-1.3, -0.6) | -2.9 (-3.2, -2.7) |
| Bolivia | -1.4 (-1.5, -1.2) | 0.4 (0.3, 0.5) | -3.4 (-3.6, -3.3) | -1.2 (-1.4, -1.0) | -0.1 (-0.1, 0.1) | -3.8 (-4.0, -3.7) |
| Brazil | -2.7 (-2.9, -2.5) | -0.9 (-1.1, -0.7) | -3.9 (-4.2, -3.6) | -3.0 (-3.2, -2.8) | -1.4 (-1.7, -1.1) | -4.2 (-4.5, -3.9) |
| Paraguay | -0.7 (-1.4, 0.1) | 0.6 (-0.3, 1.5) | -1.4 (-2.1, -0.8) | -1.5 (-2.2, -0.8) | -0.5 (-1.3, 0.3) | -2.4 (-3.0, -1.7) |
| Uruguay | -2.6 (-3.2, -2.0) | -1.0 (-1.4, -0.6) | -2.6 (-2.9, -2.2) | -2.9 (-3.3, -2.4) | -1.1 (-1.5, -0.7) | -2.4 (-2.7, -2.1) |
| Venezuela | -0.9 (-1.7, -0.1) | -0.1 (-1.3, 1.1) | -2.7 (-3.5, -2.0) | -1.6 (-2.0, -1.2) | -0.9 (-1.4, -0.5) | -3.4 (-3.8, -3.0) |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





