Submitted:
03 August 2023
Posted:
07 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
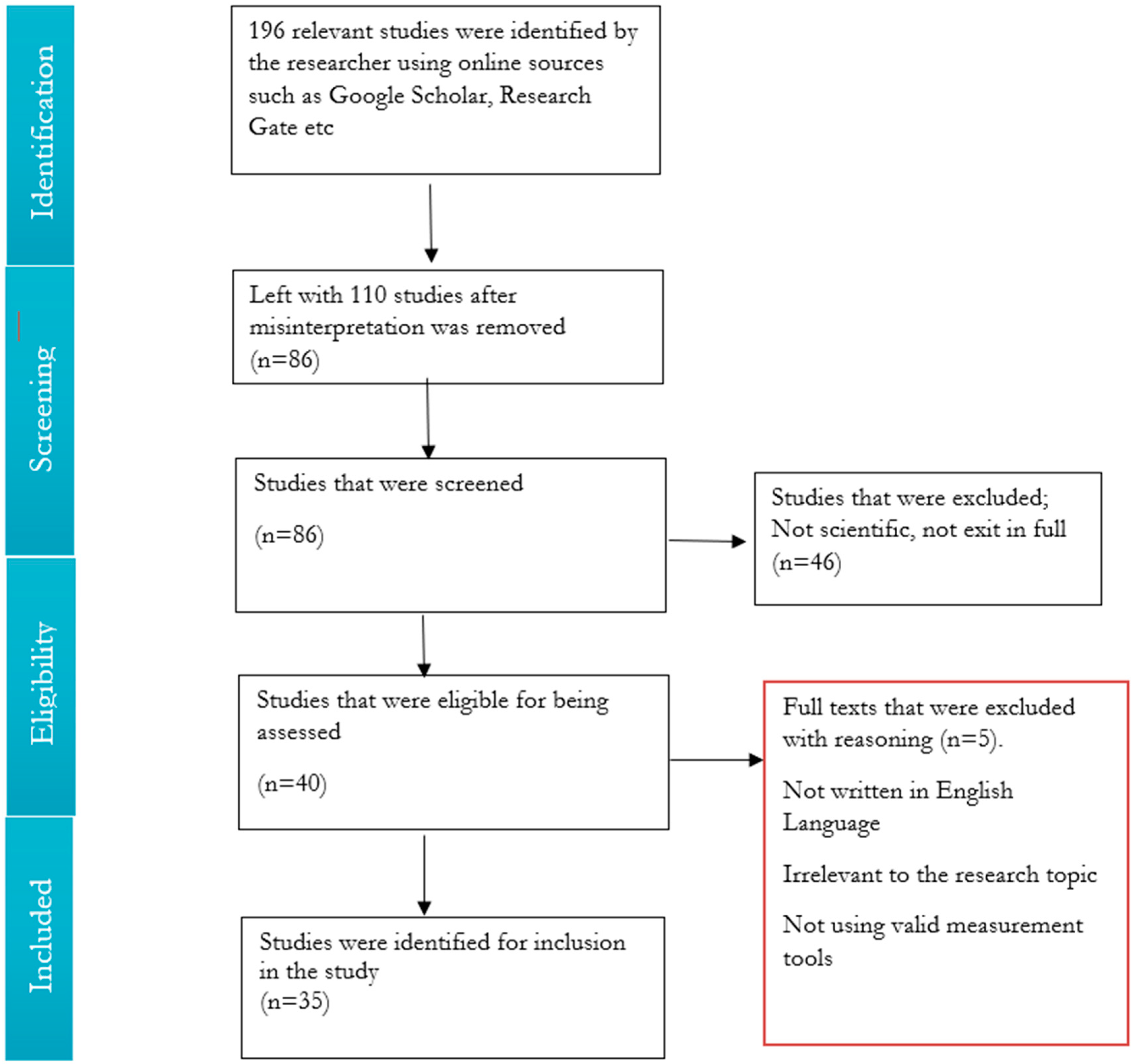
2. Methods
2.1. Study Selection Strategy
2.2. Study Design Eligible Inclusion and Exclusion Criteria
2.3. Quality of Assessment
2.4. Synthesis
| Authors/s (year) | Country of Study | Study Design | Study Aims | Sample/Population | Measures | Key Findings |
|---|---|---|---|---|---|---|
| (Adegboye et al., 2021) | London | Mixed method | The aim of this study is to understand why the COVID-19 pandemic worsened the mental health problems of vulnerable young children. | 142 participants | Surveys | The findings of this study showed that, the pandemic has worsened the mental health problems of the vulnerable children. |
| (Apisarnathanarak et al., 2020) | Thailand | Mixed methods | This study aims to look at the mental health care personnel during the COVID-19 pandemic. | 32 reports | Surveys | Health care workers had a higher mental health status. |
| (Cabrera et al., 2020) | Non-specific | Qualitative method | The aim of this study is to provide a systematic review on the impact of the pandemic on psychiatric practice. | 50 articles | Review | The results showed that, the population that was at risk included COVID-19 survivors, health care workers, old people, and population with pre-existing psychiatric disease. |
| (Cooper et al., 2020) | United Kingdom | Mixed method | The aim of this study was o conducting a thorough systematic review of the latest studies reporting on clinical findings with persons living with HIV/AIDS whom were infected with coronavirus. | 8 studies | Review | People living with HIV/AIDS were unlikely at to be a higher risk of mental health outcomes than the general population due to the pandemic if they have undetectable viral load and an adequate CD4 count. |
| (Damiano et al., 2021) | Brazil | Mixed method | This study aimed at examining at mental health strategies for preventing mental health problems on the general population during the coronavirus outbreak. | 25 (Qualitative studies) and 3 (Quantitative studies) | Review | It was discovered that in most of these studies, there was a lack of evidence and a need for additional studies with more effective design especially randomized controlled trials investigating possible interventions in mental health outcomes during the pandemic. |
| (De Brier et al., 2020) | New Zealand | Mixed method | The aim of this study is to overlook on the risks and protecting factors of mental health outcomes on health care workers during the pandemic. | 33 studies | Review | Health care workers were developing a higher risk of experiencing mental health outcomes with risk factors such as direct contact with infected patients. |
| (De Kock et al., 2021) | United Kingdom | Mixed method | This study aim is to identify the psychological impact of COVID-19 pandemic on health care, general population and management. | 24 studies | Review | Front line workers were easily infected with coronavirus; hence they had symptoms of stress and depression. |
| (Dutta el al., 2021) | India | Mixed method | The aim of this study was to look at the studies that were previously collected in order to establish the likelihood of the mental health problems among health care employees and compare findings with their study. | 33 studies | Review | This study revealed evidence that health care workers suffered from psychological and mental health problems during the pandemic due to fear of infecting their families and friends |
| (Farkas & Romaniuk 2020) | United States of America | Qualitative method | This paper aim at examining social worker, ethics and vulnerable groups during the COVID-19 pandemic. | Not specific | Not specific | The findings of this study is that every human was vulnerable to the COVID-19. |
| (Fiorenzato et al., 2021) | Italy | Mixed method | The aim of this study was look at the changes in cognitive and mental health outcomes and their vulnerability on the COVID-19 pandemic. | 12515 respondents | Online surveys | This study discovered results that were harmful to the society such as anxiety and depression disease burden rising to 32% and 36 %, respectively, and abnormal sleep, appetite changes, and health anxiety. |
| (Georgi et al., 2020) | Non-specific | Qualitative method | The objective of this study is to look at psychological aspects related to workplaces during the COVID-19 pandemic and address the important issues that were impacted by the pandemic in the workplace. | 37 studies | Review | The psychological conditions were impacted by long periods of isolation and uncertainty of the future on the workplaces. |
| (Hannenmann et al., 2022) | Austria | Quantitative method | The aim of this study is to look at pandemic stressors that impacted the public population such as fear of infecting each other and less workload at workplaces. | 46 studies | Review | Examined the associates between the general mental health constructs, resilience, and coping with pandemic stressors |
| (Hossain et al., 2020) | United States of America | Qualitative method | The aim of this study is to provide evidence on the mental health outcomes of quarantine and isolation due to population preventing themselves of not being infected. | 8 articles | Review | The individuals who were infected by the coronavirus were impacted with mental health problems such as mood disorder, anxiety, depression, and psychological distress etc. |
| (Iyengar et al., 2021) | United States of America | Mixed method | The aim of this is to investigate about the mental health care and postpartum of pregnant women during and after the pandemic | 91 studies | Review | Their results showed that pregnant women who tested positive for covid-19 were at risk for preterm birth. |
| (JAMA Psychiatry, 2021) | America | Mixed method | This study aims at looking at how mental health disorders has been increased due to the COVID-19 | 32 mixed studies (16 Qualitative and 16 Quantitative studies) | Review | Patients with mental health disorders were targeted as the high risk of COVID-19, by establishing disease management strategies. |
| (Kim et al., 2022) | United States of America | Mixed method | The aim of this study is look at how mental health impacted the lives of people in prison globally. | 62 studies | Review | People in prison were a high risk of the coronavirus, which led psychological impacts. |
| (Li et al., 2022) | China | Quantitative method | The objective of this study is to investigate the level of mental health and variables that affected the residents of China during and after COVID-19 pandemic. | 993 residents | Online questionnaire surveys | The results found that, the highest rate of symptoms and depression was at 37.06% and 22.86%, respectively. |
| (Min Lou et al., 2020) | China | Quantitative studies | The aim of this study was observed on psychological impacts due to COVID-19 pandemic among health care workers, general public and patients with pre-existing conditions. | 62 studies | Review | Patients with pre-existing conditions were reportedly to be significantly diagnosed with mental health problems compared to health care workers and the general public. |
| (Nearchou et al., 2020) | Ireland | Mixed method | The aim of this study was to look at the mental health of the youth during the COVID-19 pandemic. | 12 studies. | Review | The results of this study showed that the coronavirus pandemic had mental health impact on the youth which showed symptoms like depression and anxiety. |
| (Negri et al., 2023) | Italy and Poland | Mixed method | This study aim was to focus on the psychological process such as core belief violation, meaning made of the pandemic, vulnerability, and mortality perception. | 680 participants | Online surveys | The results of study revealed that mental processes (core belief violation, pandemic, vulnerability, and mortality perception) influenced the intensity of mental health outcomes greater than COVID-19 stressors and demographic combined. |
| (Nochaiwong et al., 2021) | Thailand | Quantitative method | The aim of this study is to overlook on the mental health problems during the pandemic nationally and globally. | 32 studies and 398,771 participants | Review | The findings demonstrated that the risk of mental health disorder and psychological impacts differs significantly between nations, especially with different regions, as measured by the global index of coronavirus readiness, disparities and economic vulnerability indices. |
| (Rizeq et al., 2021) | Canada | Mixed method | The aim of this study was to investigate on the impacts of pre-existing psychological and economic vulnerability on the mental health outcomes and stress on the families during the pandemic. | 427 participants | Surveys | The global health crisis had a negative effect on how households operate, and it also affects the anxiety and mental health of parents and children. |
| (Salazar et al., 2020) | United Kingdom | Mixed method | The aim of this study was to look at impacts of coronavirus symptoms on physical and mental health outcomes of health care workers. | 40 studies | Review | The findings of this study confirmed that health care workers are also considered as essential as a fragile population which it had higher physical and mental health burden during the COVID-19 pandemic. |
| (Shaukat et al., 2020) | Pakistan | Mixed method | The goal of this study is to summarize the evidence on health care workers on how the physical and mental health impacted their lives during the COVID-19 pandemic. | 10 studies | Review | This shows that health care workers were at direct risk of the physical and psychological effects in regard of taking care of patients who were infected with COVID-19. |
| (Simon et al., 2021) | Austria | Mixed method | This study focused on the Austrian adult residents about their experiences during the coronavirus lockdown. | 560 residents | Online surveys | The findings showed that 31% of residents showed poor mental well-being whilst 30% of residents with history of receiving mental health treatment received it during lockdown. |
| (Stephanie et al., 2022) | United States of America | Mixed method | This study concentrated on looking at the factors that influence the negative mental health outcomes, especially focused on the similarities between pregnant and non-pregnant women compared to male, in addition to subjective/perception issues e.g fear and worry and social vulnerabilities. | 740,640 participants | Surveys | The findings of this study identified that pregnant women were much higher risk of experiencing negative mental health outcomes than males during the COVID-19 pandemic. |
| (Theberath et al., 2022) | United States of America | Mixed method | This study focused on the effects of mental health on children and adolescents who have already diagnosed with psychiatric disorder. | 35 studies | Review | Female children were at a higher risk of experiencing domestic abuse and also young adolescents who preferred outdoor activities were at a higher risk of experiencing anxiety and depression symptoms during the pandemic. |
| (Tso et al., 2020) | Hong Kong | Quantitative method | This study aims at identifying a vulnerable general population of children. | 29,202 children | Online surveys | This study identified that the risk of a child psychosocial problems were at a higher level that with a children who has special needs. |
| (Uphoff et al., 2021) | Islam Republic of Iran | Mixed method | The primary objective of this study was to produce the impact of coronavirus pandemic upon mental health for population that is considered to be a higher risk of negative mental health outcomes. | 25 studies | Review | The symptoms of mental health problems such as depression, anxiety, sleep problems etc, were reported to be high among the samples of health care workers, COVID-19 patients, and children and adolescents. |
| (Veazie et al ., 2022) | United States of America | Mixed method | This study at addressing how women were seeking help other than men, and older people were a higher risk of coronavirus, which led to symptoms of feeling depressed. | 19 studies | Review | Adults who were hospitalized during the pandemic had higher chances of dying and many men did not seek help in management facilities |
| (Vizheh et al., 2020) | Switzerland | Mixed method | Mental health care suffered psychological illness. And people who were losing their were also significantly impacted by the mental illness. | 11 studies | Review | Health care workers felt more pressure and mental illness. |
| (Vindegaard & Benros, 2020) | Denmark | Mixed method | The psychiatric symptoms due to COVID-19 pandemic was evaluated on the infected and non- infected groups of people. | 43 studies | Review | The group who had less psychiatric symptoms were reported to be the female gender. |
| (Wang et al., 2021) | China | Quantitative method | The aim of this study was to identify factors that are driven by mental health outcomes among the population and the vulnerable groups under the COVID-19 pandemic. | 56,679 participants | Online surveys | The findings of the study showed that the most vulnerable on COVI-19 were people were a population with a pre-existing condition disease, health care workers, population living in a most affected place, infected patients, and financial unstable population. |
| (Xiong et al., 2020) | Canada | Qualitative method | This systematic review aims to synthesize extant literature that reports on the effects of COVID-19 on psychological outcomes of the general population and its associated risk factors | 19 studies | Review | Relatively high rates of symptoms of anxiety, depression, post-traumatic stress disorder psychological distress, and stress |
| (Yan et al., 2021) | China | Quantitative method | The purpose of this study was to determine on the incidence of negative mental health outcomes among health care workers during the COVID-19 pandemic and to investigate the spread of anxiety and depression symptoms. | 35 articles | Surveys | During the COVID-19 outbreak, health care workers experienced a high rate of negative mental health symptoms. |
3. Results
3.1. Study Characteristics
3.1.1. Location
3.1.2. Aims of the Study
3.2. Study Methodology
3.2.1. Study Sample
3.2.2. Nature of Study and Design
3.3. Findings
4. Discussion
5. Conclusion
References
- Adegboye D, Williams F, Collishaw S, et al (2021) Understanding why the COVID-19 pandemic increases mental health difficulties in vulnerable yung children. Available at: https://doi.org/10.1111/jcv2.12005. [CrossRef]
- Anakpo, G., & Mishi, S. (2021). Business response to COVID-19 impact: Effectiveness analysis in South Africa. . South. Afr. J. Entrep. Small Bus. Manag. 2021, 13, 7.
- Anakpo, G., & Mishi, S. (2022). Hesitancy of COVID-19 vaccines: Rapid systematic review of the measurement, predictors, and preventive strategies. Human Vaccines & Immunotherapeutics, DOI: https://10.1080/21645515.2022.2074716. [CrossRef]
- Anakpo, G., Hlungwane, F., & Mishi, S. (2023). The Impact of COVID-19 and Related Policy Measures on The Livelihood Strategies in Rural South Africa. Afr. Agenda .
- Anakpo, G., Nqwayibana, Z., & Mishi, S. (2023). The Impact of Work-from-Home on Employee Performance and Productivity: A Systematic Review. Sustainability, , 15(5), 4529.
- Apisarnathanarak A, Thatrimontrichai A & Weber D (2021) Mental health among healthcare personnel during COVID-19 in Asia. Available at: https://doi.org/10.1016/j.jfma.2021.01.023. [CrossRef]
- Benjamin F, Delport V, Shelley A & Nicolette V(2022). Mental health care services in rural South Africa: a systematic review. Available at: https://doi.org.10.1080/15332985.2021.1927283.
- BMJ (2020) Preferred reporting for systematic review and meta-analysis of diagnostic test accuracy studies (PRISMA-DTA): explanation, elaboration, and checklist. Available at: https://doi.org/10.1136/bmj.m2632. [CrossRef]
- Bourmistrova, N. W., Solomon, T., Braude, P., Strawbridge, R., & Carter, B. (2022). Long-term effects of COVID-19 on mental health: A systematic review. Journal of affective disorders, 299, 118-125.
- Brooks S, Webster R, Smith L, Woodland L, Wessley S, Greenberg N., et al. (2020). The psycholological impact of quarantine and how to reduce it: rapid review of the evidence. Available at: https://doi.1016/S0140-6736(20)30460-8.
- Cabrera A, Lakshmipriya K & Scott A (2020). Corona virus and its implications for psychiatry: A rapid review of the early literature. Available at: www.psychosomaticjournal.org.
- Damarell A, Morgan D & Tieman, J. (2020). General practitioner strategies for managing patients with multimorbidity: a systematic review and thematic synthesis of qualitative research. Available at: https://doi.org/10.1186/s12875-020-01197-8. [CrossRef]
- Damiano RF, Di Santi T, Beach S, Pan PM, Lucchetti AL, Smith FA, et al. ( 2021) Mental health interventions following COVID-19 and other coronavirus: a systematic review of current recommendations and meta-analysis of randomized controlled trials. Available at: https://dx.doi.org/org/10.1590/1516-4446-2020-1582. [CrossRef]
- De Brier N, Stroobants S, Vandekerckhove P & De Buck E (2020). Factors affecting mental health of health care workers during coronavirus disease outbreak (SARS,MERS & COVID-19): A rapid systematic review. Available at: https://doi.org/10.1371/journal.pone.0244052. [CrossRef]
- De Kock J, Latham A, Leslie J, Grindle M, Munoz S., et al. (2021)., A rapid review of the impact of COVID-19 on the mental health of healthcare workers: implications for supporting psychological well-being. Available at: https://doi.org/10.1186/s12889-020-10070-3. [CrossRef]
- Dutta A, Sharma A, Torres-Castro R, Pachori H & Mishra S (2021). Mental health outcomes among health-care workers dealing with COVID-19/severe acute respiratory syndrome 2 pandemic: A systematic review and meta-analysis.
- Farkas J.K & Romaniuk R (2020) Social Worker, Ethics and Vulnerable Groups in the Time of Coronavirus and Covid-19. Available at: DOI:10.14746/sr.2020.4.2.05. [CrossRef]
- Fiorenzato E, Zabberoni S, Costa A & Cona G (2021) Cognitive and mental health changes and their vulnerability factors related to Covid-19 lockdown in Italy. Available at: https://doi.org/10.1371/journal.pone.0246204. [CrossRef]
- Giorgi G, Leca L.I, Alessio F, Finstad G.L et al. (2020). Covid-19-Related Mental Health Effects in the Workplace: A narrative review.
- Hannemann J, Abdalrahman A, Erim Y, Morawa E, Jerg-Bretkze L, Beschoner P, et al. (2022) The impact of the COVID-19 pandemic on the mental health of medical staff considering the interplay of pandemic burden and psychosocial resources- A rapid systematic review. Available at: https://doi.org/10.1371/journal.pone.0264290. [CrossRef]
- Hossain M.M, Sultana A & Purohit N (2020). Mental health outcomes of quarantine and isolation for infection prevention : A systematic umbrella review of the global evidence. Available at: https://doi.org/10.4178/epih.e2020038. [CrossRef]
- Iyengar U, Jaiprakash B, Haitsuka H & Kim S (2021) One Year Into The Pandemic: A systematic Review of Perinatal Mental Health Outcomes During COVID-19. Available at: https://doi.org/10.3389/fpsyt.2021.674194. [CrossRef]
- Jafta, K., Anakpo, G., & Syden, M. (2022). Income and poverty implications of Covid-19 pandemic and coping strategies: the case of South Africa. Africagrowth Agenda, 19(3), 4-7.
- JAMA Psychiatry (2021) Association between mental health disorders and mortality among patients with COVID-19 in 7 countries: A systematic review and meta-analysis. Available at: https://jamanetwork.com/on06/27/2023.
- Kim H, Hughes E, Cavanagh A, Norris E, Gao A, Bondy SJ, et al. (2022) The health impacts of the OVID-19 pandemic on adults who experience imprisonment globally: A mixed methods systematic review. Available at: https://doi.org/10.1371/journal.pone.0268866. [CrossRef]
- Komanisi, E., Anakpo, G., & Syden, M. (2022). Vulnerability to COVID-19 impacts in South Africa: analysis of the socio-economic characteristics. Africagrowth Agenda, 19(2), 10-12.
- Li S.M, Guo B.B, Yang Q.P, Yin J.Y et al (2023) Predictive factors for enhanced community mental health vulnerability in this COVID-19 pandemic era. Available at: https://doi.org/10.1093/qjmed/hcac191. [CrossRef]
- Min L, Guo L, Yu M, Jiang W & Wang H (2020). The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public- A systematic review and meta-analysis. Available at: https://doi.org/10.1016/j.psychres.2020.113190. [CrossRef]
- Mishi, S., Anakpo, G., Matekenya, W., & Tshabalala, N. (2023). COVID-19 Vaccine Hesitancy and Implications on Economic Recovery.
- Mishi, S., Matekenya, W., Anakpo, G., & Tshabalala, N. (2023). COVID-19 Vaccine Hesitancy and the Role of Information: Lessons from South Africa.
- Mishi, S., Tshabalala, N., Anakpo, G., & Matekenya, W. (2023). COVID-19 Experiences and Coping Strategies: The Case of Differently Sized Businesses in South Africa. Sustainability, 15(10), 8016.
- Nearchou F, Flinn C, Niland R, Subramaniam S.S & Hennessy E (2020) Exploring the impact of COVID-19 on mental health outcomes in children and adolescents: A systematic review.
- Negri A, Conte F, Caldiroli C.L, Neimeyer R.A & Castiglioni M (2023) Psychological Factors Explaining the COVID-19 Pandemic Impact on Mental Health: The Role of Meaningful, Beliefs, and Perceptions of Vulnerability and Mortality. Available at: https://doi.org/org/10.3390/bs13020162. [CrossRef]
- Nochaiwong S, Ruengorn C, Thavorn K, Hutton B, Awiphan R et al. (2021) Global prevalence of mental health issues among the general population during the coronavirus disease-2019 pandemic: A systematic review and meta-analysis. Available at: https://doi.org/10.1038/s41598-021-89700-8. [CrossRef]
- Pragholapati, A. (2020). Mental health in pandemic covid-19. Available at SSRN, 3596311.
- Salazar de P.G, Serrano V.J, Catalan A, Arango C, Moreno C et al. (2020) Impact of coronavirus syndromes on physical and mental health of health care workers: A systematic review and meta-analysis. Available at: https://doi.org/10.16/j.jad.2020.06.022.
- Rizeq J, Korczak D.J, Cost K.T, Anagnostou E et al (2021) Vulnerability pathways to mental health outcomes in children and parents during the Covid-19. Available at: https://doi.org/10.1007/s12144-021-02459-z. [CrossRef]
- Saarni, S. I., Suvisaari, J., Sintonen, H., Pirkola, S., Koskinen, S., Aromaa, A., & Lönnqvist, J. (2007). Impact of psychiatric disorders on health-related quality of life: general population survey. The British journal of psychiatry, 190(4), 326-332.
- Shaukat N, Mnasoor D & Razzak J (2020) Physical and mental health impacts of COVID-19 on health care workers: A scoping review. Available at:https://doi.org/10.1186/s12245-020-00299-5. [CrossRef]
- Simon J, Helter T.M, White R.G, Boor van der C & Laszewska A (2021) Impacts of the Covid-19 lockdown and relevant vulnerabilities on capability well-being, mental health and social support:an Astrian survey study. Available at: https://doi.org/10.1186/s12889-021-10351-5. [CrossRef]
- Stephanie A.G, HARRIS c.t, Fitzpatrick K.M & Kothari A (2022) Social and behavioral vulnerability, pregnancy, and negative mental health outcomes in the U.S during the Covid-19 pandemic. Available at:http://www.aimspress.com/journal/aimsph.
- Theberath M, Bauer D, Chen W, Salinas M et al. (2022) Effects of COVID-19 pandemic on mental health of children and adolescents: A systematic review of survey studies. Available at: https://journals.sagepub.com/home/smo.
- TJ Cooper, Woodward BL, Alom S & Harky A (2020) Coronavirus disease 2019 (COVID-19) outcomes in HIVE/AIDS: A systematic review.
- Tso W.Y, Wong R.S, Tung K.T.S, Rao N et al (2022) Vulnerability and resilience in children during the COVID-19 pandemic.
- Uphoff EP, Lambardo C, Johnston G, Weeks L, Rodgers M, Dawson S, et al. (2021) Mental health among healthcare workers and other vulnerable groups during the COVID-19 pandemic and other coronavirus outbreak: A rapid systematic review. Available at: https://doi.org/10.1371/journal.pone.0254821. [CrossRef]
- Veazie S, Lafavor B, Vela K, Young S, Sayer A, Carlson K & O’Neil M (2022) Mental health outcomes of adults hospitalized for COVID-19: A systematic review. Available at: https://doi.org/10.1016/j.jadr.2022.100312. [CrossRef]
- Veldhuis, C. B., Nesoff, E. D., McKowen, A. L. W., Rice, D. R., Ghoneima, H., Wootton, A. R., ... & Anderson, J. C. (2021). Addressing the critical need for long-term mental health data during the COVID-19 pandemic: changes in mental health from April to September 2020. Preventive Medicine, 146, 106465.
- Vindegaard N & Benros E (2020) COVID-19 pandemic and mental health consequences: Systematic review of the current evidence: Available at: https://doi.org/10.1016/j.bbi.2020.05.048. [CrossRef]
- Vizheh M, Qorbani M, Arzaghi S, Muhidini S, Javanmard Z & Esmaeili M (2020) The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. Available at: https://doi.org/10.1007/s40200-020-00643-9. [CrossRef]
- World Health Organization (2020). WHO Director-General’s opening remarks at the media briefing on COVID-19. Available at: https://www.who.int/director-general/speeches/detail/who-director-general-opening-remarks-at-the-media-briefing-on-covid-19.
- Xiong J, Lipsitz O, Nasri F, Lui L et al., (2020) Impact of COVID-19 pandemic on mental health in the general population: A systematic review. Available at: https://doi.org/10.1016/j.jad.2020.08.001. [CrossRef]
- Yi-Ying C & Assefa Y (2021) The heterogeneity of the COVID-19 pandemic and national responses: an explanatory mixed methods study.
- Yan H, Ding Y & Guo W (2021) Mental health of medical staff during the coronavirus disease 2019 pandemic: A systematic review and meta-analysis.
- Wang Y, Shi L, Que J, Lu Q et al (2021) The impact of quarantine on mental health status among general population in China during the Covid-19 pandemic. Available at: https://doi.org/10.1038/s41380-021-01019-y. [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




