2. Materials, Methods and Methodology
A retrospective descriptive analysis was conducted on the menstrual cycle charts of forty-two women aged 40 to 50 from July 21, 2019, to July 21, 2023. Of forty-two women, eight of them used a quantitative hormone monitor to track their cycles. This case report will concentrate on data that was collected on those eight women and those cycle characteristics with corresponding charts and descriptions of those cycles. These eight women had a history of having normal regular cycles previously during their reproductive life. None of the eight women had a history of medical diagnoses that would have rendered their cycles irregular before entering perimenopause.
All women studied received instructions in fertility tracking from a health professional when they signed on for an educational class on the Marquette Method of Natural Family Planning.
Once the eight clients entered care on the first day of instruction, their menstrual cycles were followed every month to 2 months for the duration of this study. During the study, one woman was followed for 4 months of data collection, one woman was followed for 5 months, 2 women were followed for 6 months, one woman was followed for 8 months, one woman was followed for 10 months, one woman was followed for 12 months, and one woman was followed for 17 months. Unfortunately, because this is a retrospective analysis and not an established prospective study, actual numbers of cycles are not included in this data collection. Because older women often have cycles which can be longer than one month, the number of months does not give the actual number of cycles followed.
All women signed a consent agreement to have their cycles published into a presentation or document upon entering care. No personal identifiers were used in any of the data cycle publications.
To categorize women’s cycle types, definitions were established based on the STRAW criteria and other research [
2,
4]. Below are the definitions used to characterize cycle types of the forty two women when they entered care. It is important to note that all eight of the women using the MIRA entered care in the variable stage of reproduction, the first stage of perimenopause according to STRAW criteria.
Regular cycles: the woman was having normal cycle lengths (25-35 days) with normal LH surges approximately mid cycle (cycle day 11-16).
Postpartum cycle zero: the woman was postpartum and had not yet had menstrual cycles and had not ovulated.
Postpartum cycles: the woman was postpartum and having menstrual cycles, but they were longer and had later peak LH surges than a woman in regular cycles.
Short cycles: the woman was exhibiting shorter cycles (22-28 days) compared to when she was in regular cycles. This stage also exhibited earlier LH surges (cycle day 9-12). It is important to note that because women’s cycles can vary compared to each other, each woman compared her own previous regular cycles to this new shorter version of her cycle. This period is considered prior to entering perimenopause.
Variable cycles: the woman was exhibiting short and long cycles that varied by more than 7 days between cycles. This stage could have different characteristics within one woman. For this study, fertility tracking during this time revealed that there are distinct hormonal cycle characteristics common to this variable time that have not been distinctly outlined with the use of a quantitative hormonal monitoring device prior to now.
Greater than 60 days without cycles: the woman had a span of 60 days or greater since her last bleeding episode.
Menopause: the woman had no cycles in one year.
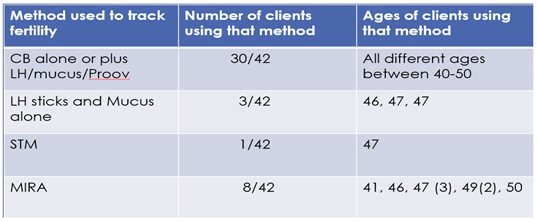
Women used different methods to track their cycles. When women entered care, they had been using various ovulation and sympto-thermal methods along with LH stand-alone wands and Progesterone stand-alone wands to track their fertility. (See
Table 1). Once they entered care, most of the women (33/42) used the Clear blue © (CB) monitor to track their cycles along with LH wands, mucus and/or Progesterone wands. Three women used only LH wands and mucus tracking. Eight women used the quantitative hormone monitor, MIRA ©, to track their fertility. Two women used both the CB monitor and the MIRA monitor at some point of their tracking.
A thorough discussion of cycle tracking biomarkers is not covered in this paper; however, it is important to discuss that the quantitative hormone monitor, MIRA ©, does allow the accurate measurement of a woman’s cyclic hormones. This device measured estrone-3-glucuronide (E3G), a urinary metabolite of estrogen, known to rise prior to the luteinizing hormone (LH) during folliculogenesis when women are in regular cycles. A comparative study of the CB monitor and the MIRA in women with regular length cycles showed that 60 out of 62 cycles had a rise in quantitative E3G of >100 ng/ml at least 5 days prior to the LH surge [
5]. This is important information for women wanting to know the beginning of their fertile window. In perimenopause women however, this rise in E3G may be shorter than 5 days and may not give enough forewarning of the impending LH surge. The short rise could be postulated to be from inadequate folliculogenesis in older women. It is unknown what percentage of these truncated E3G rises prior to the LH surge result in actual ovulation. The MIRA monitor also measures LH, follicle stimulating hormone (FSH) as well as pregnanediol glucuronide (PdG), a urinary metabolite of progesterone. It is known that LH stimulates ovulation and progesterone is a marker for post ovulation confirmation. Preliminary research with the MIRA revealed that an adequate cutoff for the beginning of the fertile window may be an E3G level of 100 ng/ml [
5].
3. Results and Discussion:
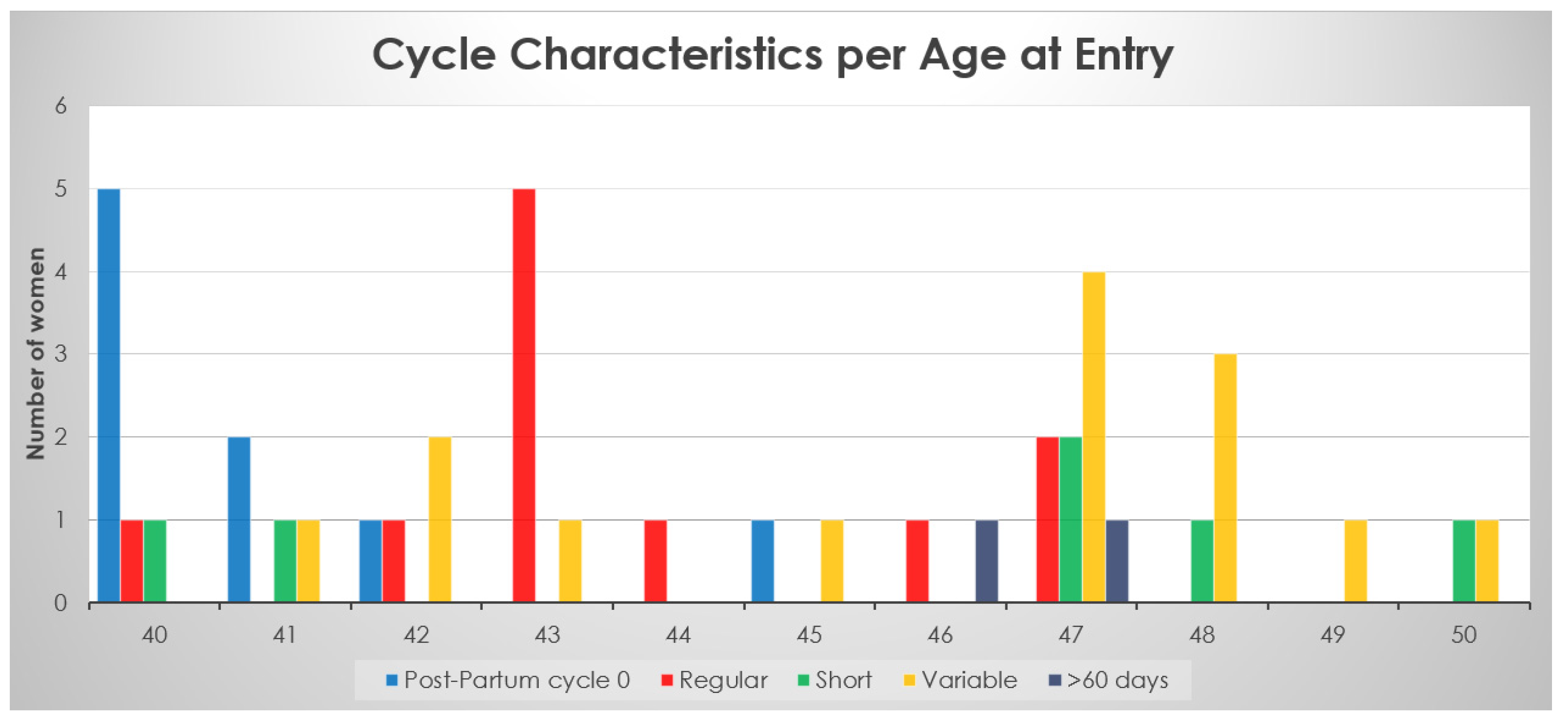
Figure 1 shows the forty-two women’s cycle types categorized according to when they entered care. All eight women using the quantitative hormone monitor entered cycles at a variable stage of perimenopause irrespective of age. Their ages ranged from 41 to 50. Although this case report looks specifically at the eight women in variable reproductive state, it is important to note that all 42 women entered care at various stages of reproduction.
Table 1.
Types of Fertility tracking used for forty-two women.
Table 1.
Types of Fertility tracking used for forty-two women.
Figure 1.
Age, number of women, and their cycles characterized at entry of care (forty-two women).
Figure 1.
Age, number of women, and their cycles characterized at entry of care (forty-two women).
The salient points about cycle characteristics of all forty two women compared to age at entry of care was that most women of any age could be in any category of cycles. Most postpartum women were younger at ages of 40-42, however one woman was postpartum at 45. Women who were older, aged 47 to 50, were more likely to be in a variable stage of reproduction, however one woman who was 50 was in shortened reproductive cycles, which is prior to the variable stage according to the STRAW criteria. There were no women in regular cycles past the age of 47. Of these women aged 40 to 50, 14 entered care in the variable stage, 11 entered care in regular cycles, 9 entered as postpartum cycle zero, 6 entered as short cycles (last stage of reproductive cycles) and 2 entered care when they had bleeds greater than 60 days between cycles.
While being followed, some women transitioned to another phase of their cycles (13/42).
One woman went through menopause early at 44 years old and transitioned quickly from variable stage cycles to > 60 days and had no more cycles after that stage, which put her in Menopause. Of note, her own mother entered menopause in her 40’s as well.
There were no women in regular cycles past the age of 47. The variable stage of reproduction was seen more commonly in women over the age of 46, however women aged 41, 42, 43, and 45 were already in the variable stage of reproduction at entry to care.
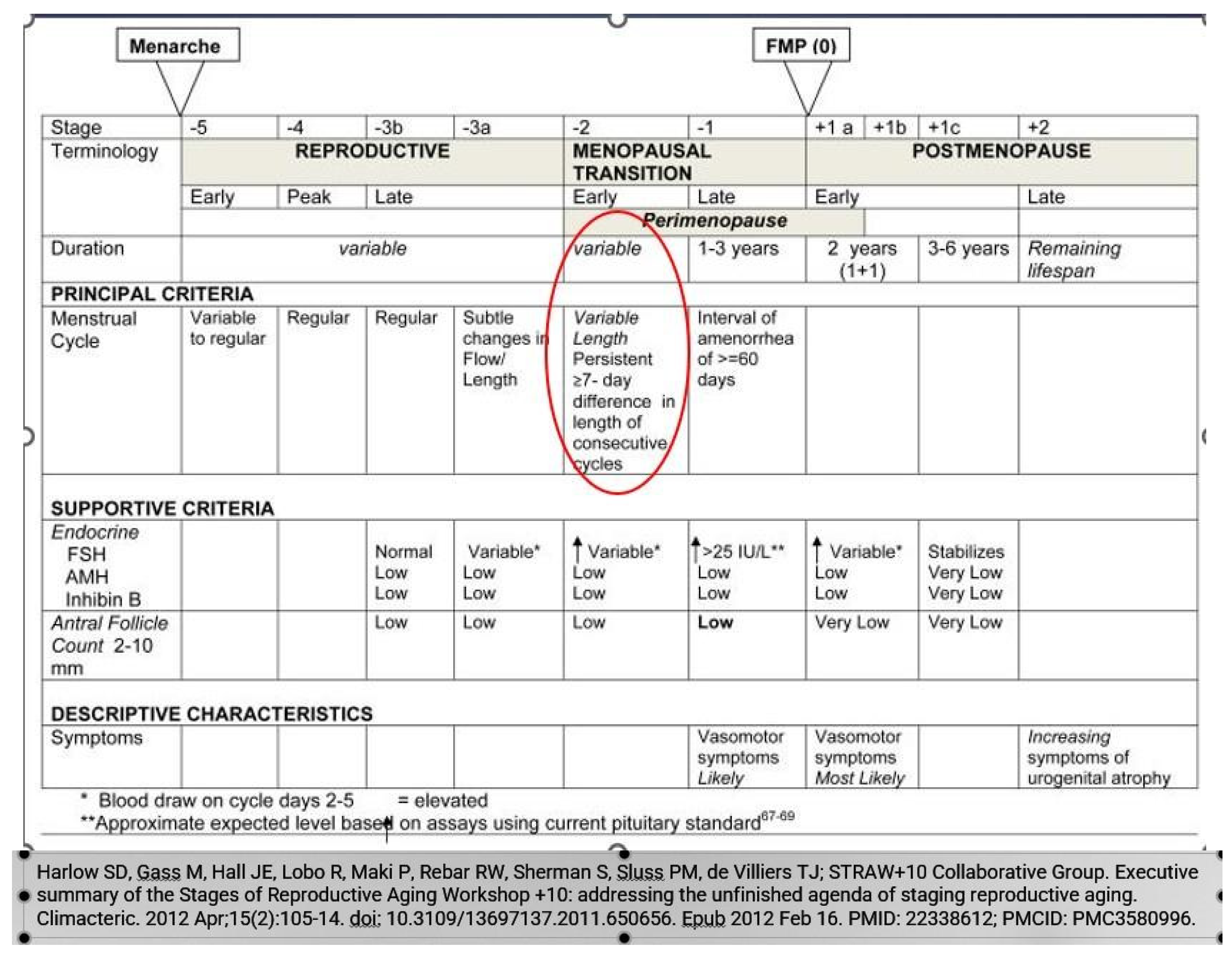
Variable Cycle Stage Characteristics: According to the STRAW study, the variable cycle stage is the first stage of Perimenopause and is when cycles begin to vary by more than 7 days within a 10-month period [
2]. See
Figure 2. However, some cycles in these older women can still be ovulatory within this variable STRAW stage. When analyzing the forty-two women’s menstrual cycles, patterns were seen to delineate some unique hormonal and bleeding characteristics of this period, even within that variability. This is novel information of the characteristics of this stage of reproduction and helps us to better characterize women’s cycles. See
Table 2.
Figure 2.
Stages of Reproductive Aging in Women (STRAW); Variable Stage is 1st stage of Perimenopause. (Used with permission).
Figure 2.
Stages of Reproductive Aging in Women (STRAW); Variable Stage is 1st stage of Perimenopause. (Used with permission).
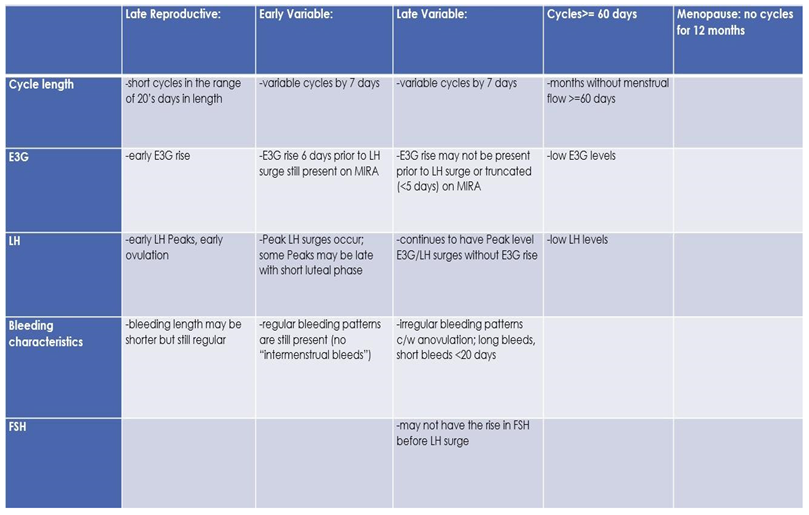
Table 2.
Proposed cycle characteristics of pre perimenopause and perimenopause stages.
Table 2.
Proposed cycle characteristics of pre perimenopause and perimenopause stages.
When looking specifically at the variable stage of perimenopause, women have characteristics earlier that may differ slightly than later as they progress through this stage. There can be some overlap between an earlier variable and a late variable stage as even women in late variable stages may still exhibit regular ovulatory cycles. They may still have normal E3G rises 5 days prior to the LH surge which can give an adequate fertile window prior to the LH surge. Some peak LH surges may be later in the cycle and those cycles may have shorter luteal phases with longer cycles compared to others.
As women progress in the variable stage of perimenopause, they can see truncated E3G rises prior to the LH surge which may not give an adequate warning of the beginning of the fertile window. They can also see continuous high E3G levels coinciding with high LH levels. It is uncertain if these types of cycles are ovulatory. In what can be assumed to be anovulatory cycles, there can be continuous low levels of both E3G and LH as well. Another characteristic of these variable cycles are double LH peaks, with one peak LH usually greater than a subsequent or previous one and these LH peaks are usually close together in the cycle. It can be postulated that the greater LH peak is thought to be more likely the true stimulation to ovulation compared to its smaller near additional surge.
There can also be irregular bleeding patterns with short time frames between one bleed and the next bleed with no discernable LH Peak. These short episodes may not be ovulatory. PdG levels may be elevated after a true ovulatory cycle, however, in one paper by O’Connor, et al, as women age, their PdG levels decline [
3]. Declining PdG levels may make it harder to determine if a cycle in this stage is truly ovulatory or anovulatory.
In this section, there will be examples of these types of variable cycles of the eight women out of the forty-two who were tracking with the quantitative monitor. It is important to also note that all charts in these examples are from the variable stage of reproduction. Even in this unpredictable stage, there were some cycles in these women that appeared regular and ovulatory, even in women of older ages. See Figure 3 through 11.
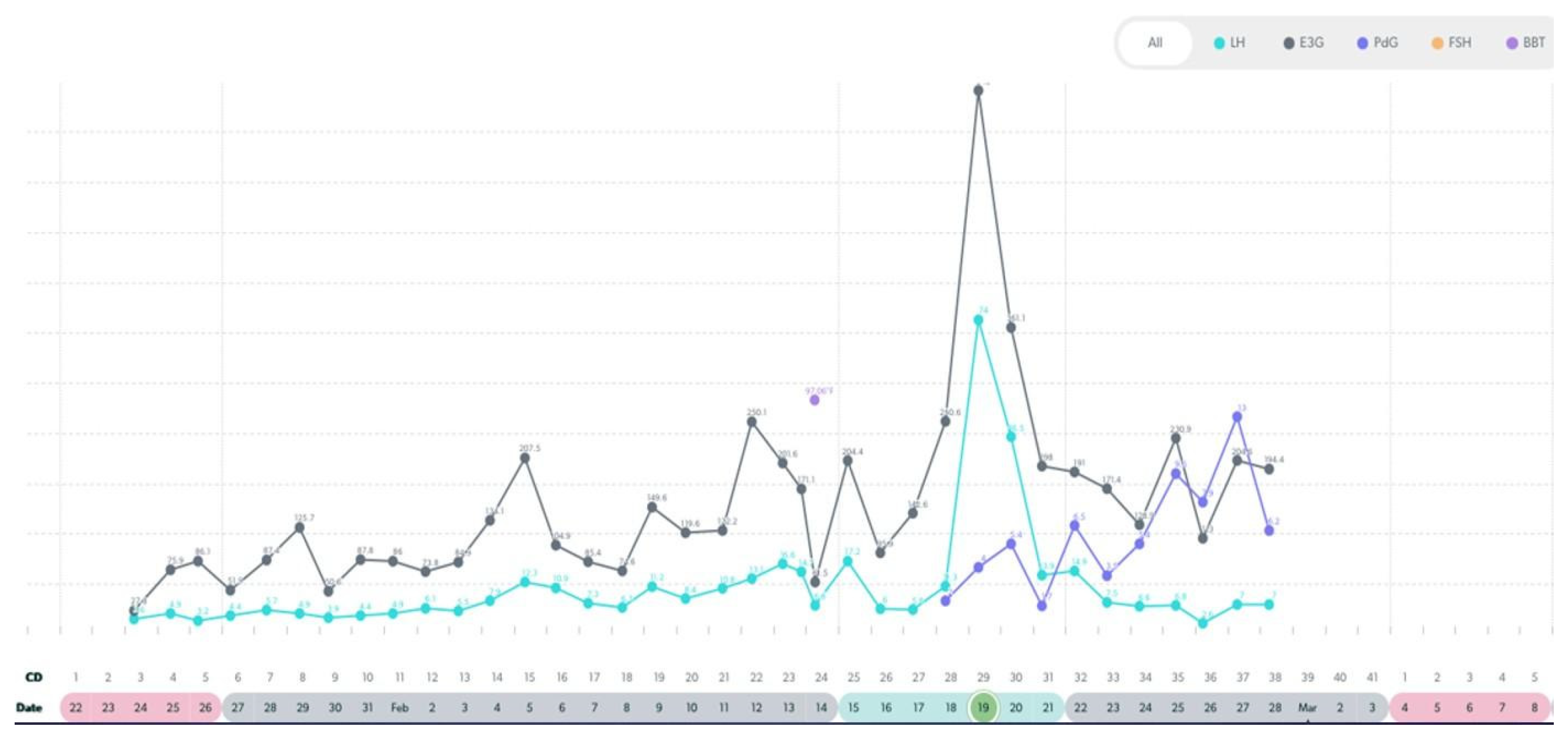
Figure 3.
Variable Cycle with MIRA: 41 yo delayed LH peak, 41 day cycle length, PdG rise post ovulation.
Figure 3.
Variable Cycle with MIRA: 41 yo delayed LH peak, 41 day cycle length, PdG rise post ovulation.
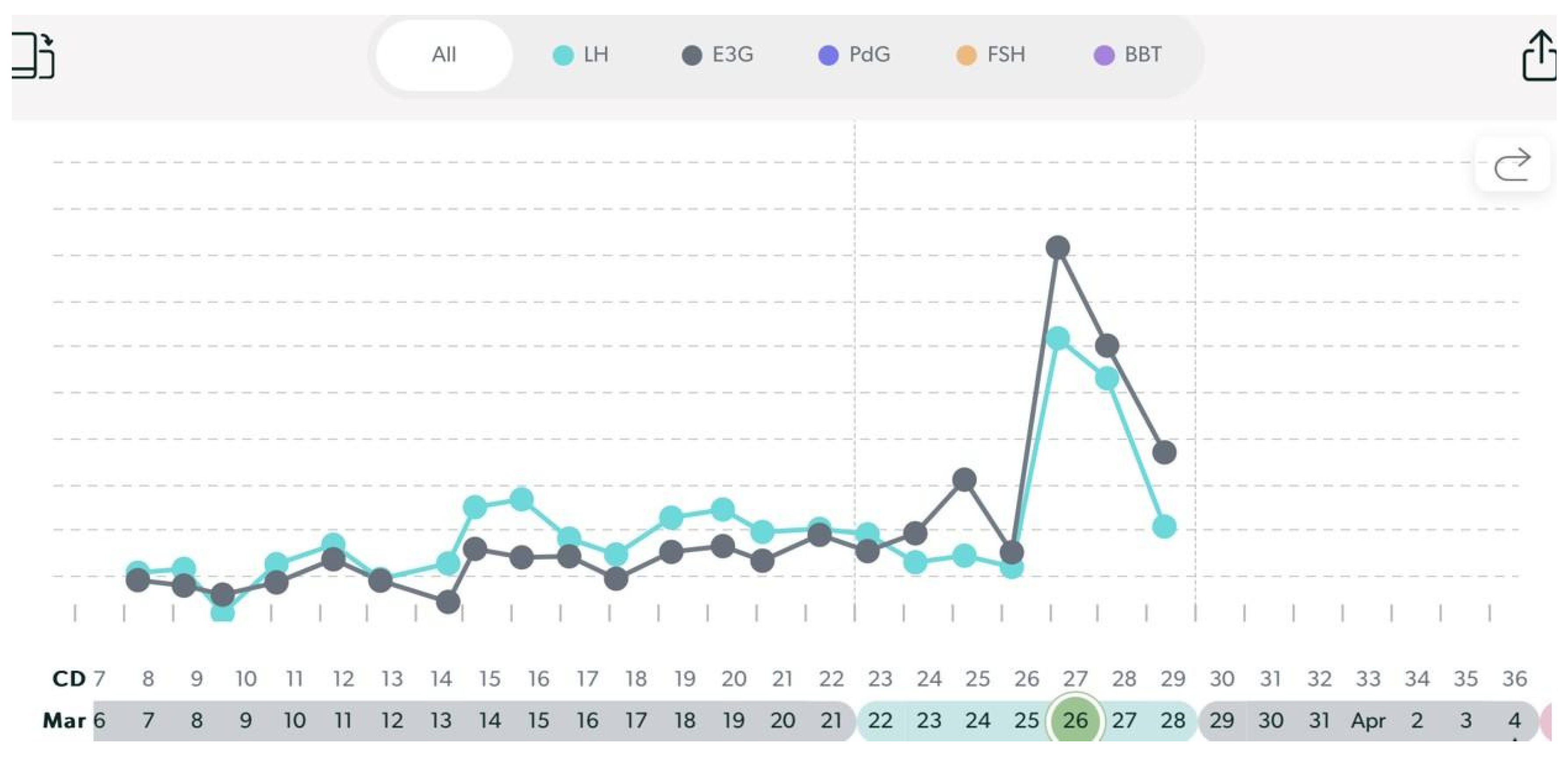
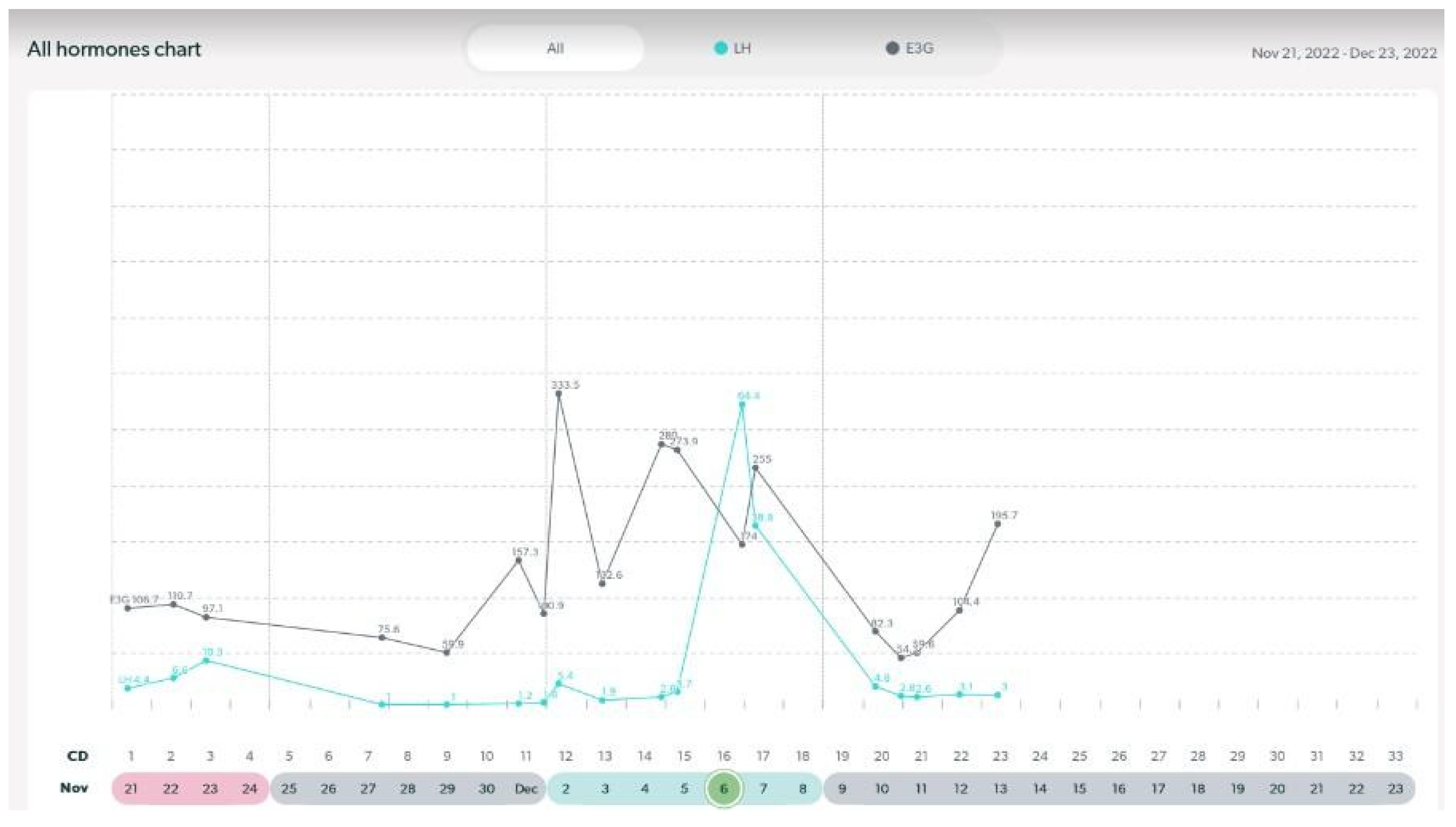
Figure 4.
Variable Cycle with MIRA: 47 yo with truncated E3G rise to LH peak, 36 day cycle.
Figure 4.
Variable Cycle with MIRA: 47 yo with truncated E3G rise to LH peak, 36 day cycle.
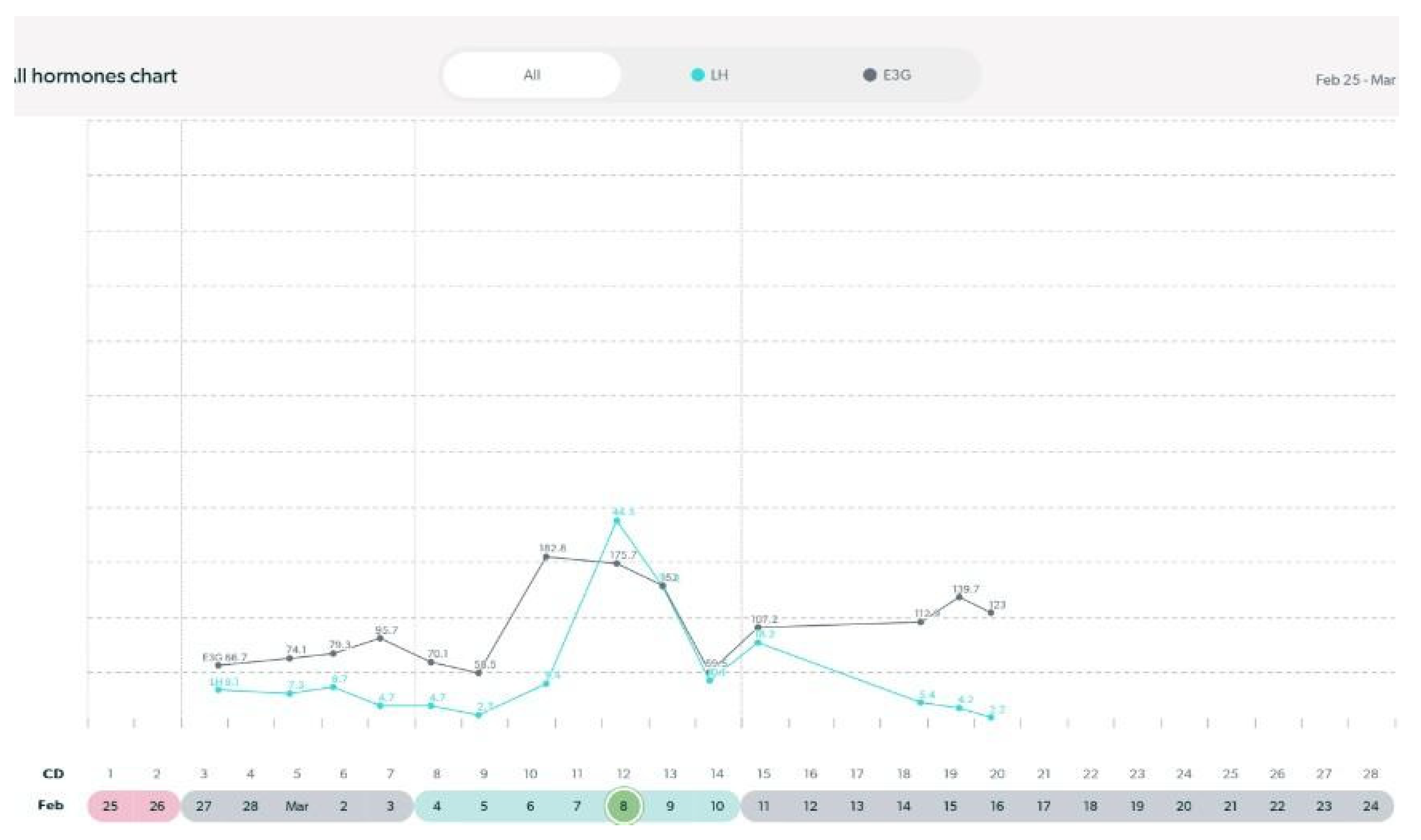
Figure 5.
Variable cycle with MIRA: 48 yo with truncated E3G rise prior to LH surge.
Figure 5.
Variable cycle with MIRA: 48 yo with truncated E3G rise prior to LH surge.
Figure 6.
Variable cycle with MIRA: 50 yo with low E3G and low LH: likely anovulatory.
Figure 6.
Variable cycle with MIRA: 50 yo with low E3G and low LH: likely anovulatory.
Figure 7.
Variable cycle with MIRA: 47 yo with late double LH Peak, PdG rise post ovulation.
Figure 7.
Variable cycle with MIRA: 47 yo with late double LH Peak, PdG rise post ovulation.
Figure 8.
Variable cycle with MIRA: 50 yo with continuous high E3G and LH.
Figure 8.
Variable cycle with MIRA: 50 yo with continuous high E3G and LH.
Figure 9.
Variable cycle with MIRA: 48 yo with regular cycle; >= 5 day E3G rise prior to LH surge.
Figure 9.
Variable cycle with MIRA: 48 yo with regular cycle; >= 5 day E3G rise prior to LH surge.
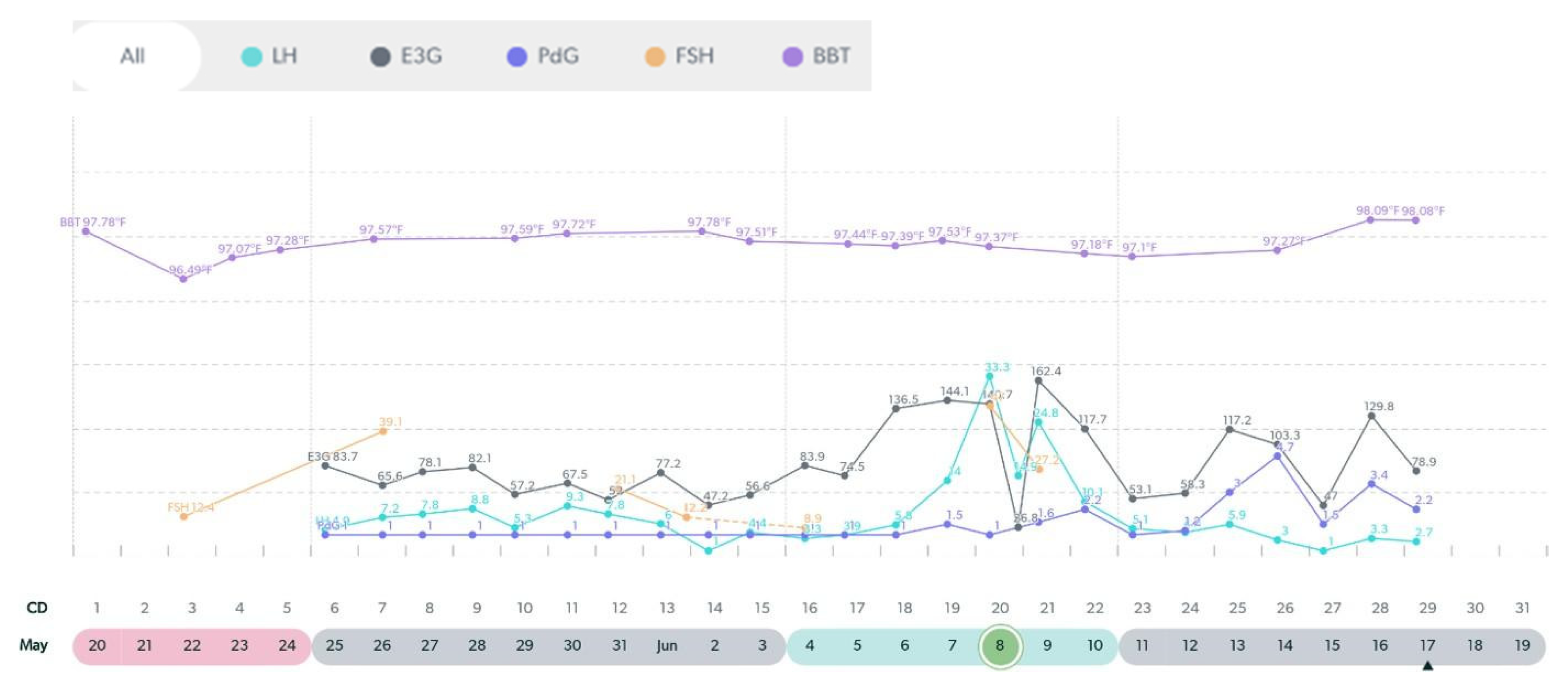
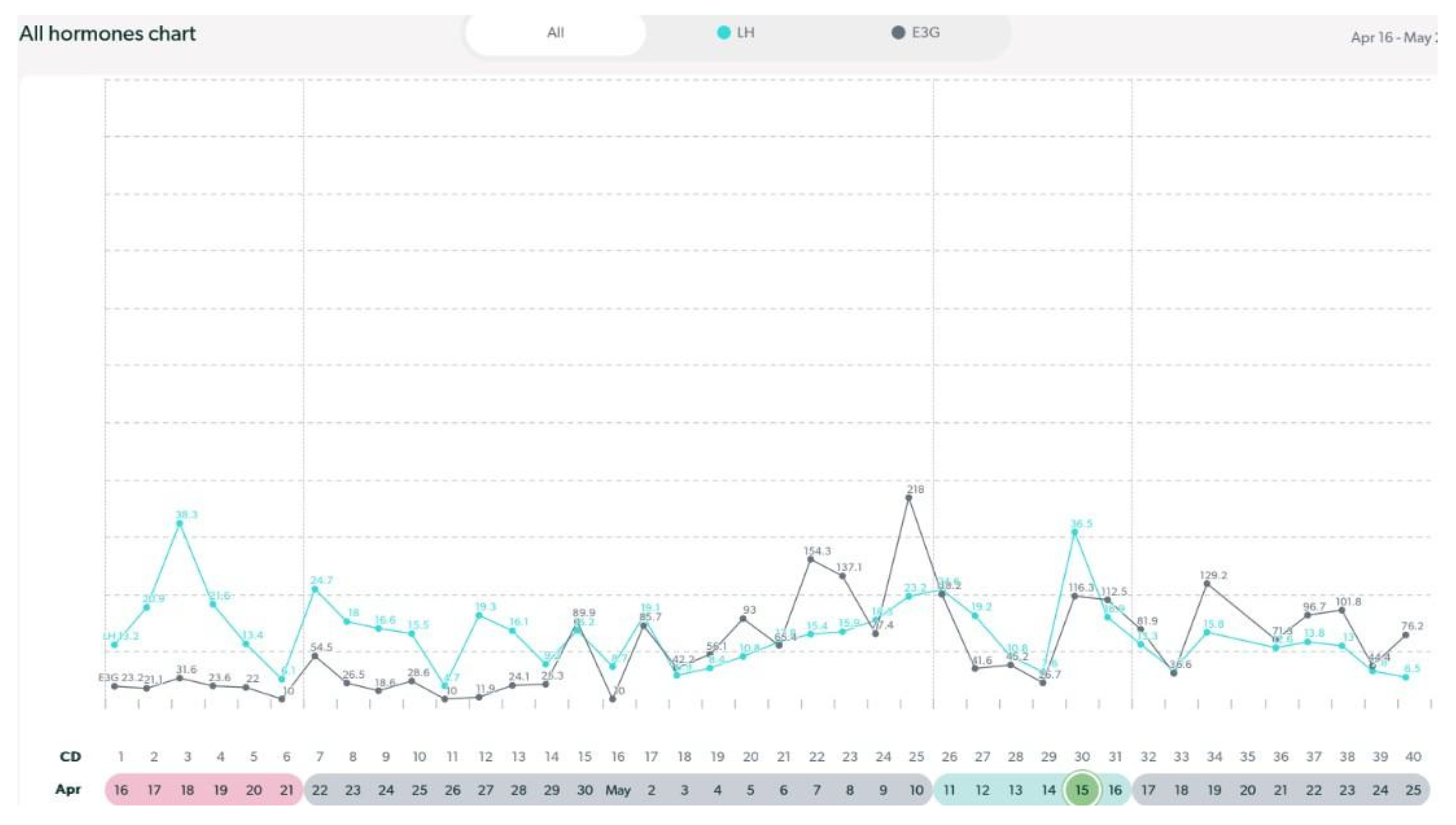
Figure 10.
Variable cycle with MIRA: 50 yo with multiple LH surges, high E3G.
Figure 10.
Variable cycle with MIRA: 50 yo with multiple LH surges, high E3G.
Figure 11.
Variable cycle with MIRA: 49 yo with late LH peak, no PdG rise, 29 day cycle.
Figure 11.
Variable cycle with MIRA: 49 yo with late LH peak, no PdG rise, 29 day cycle.