1. Introduction
The incidence of critical threatening limb ischemia (CTLI) is increasing as the aging population and cardiovascular disease increase, leading to significant social and economic impacts [
1]. For decades, an endovascular approach has been offered for less complex lesions (TASC II A and B) and for patients at high risk for surgery. In contrast, open surgery is offered to patients with more complex lesions (TASC II C and D) and considered at low or moderate risk for surgery. However, significant improvements in endovascular technology and improving knowledge of atherosclerotic lesions have overcome these limitations. Currently, the endovascular approach is offered as a first-line strategy, even for complex lesions. However, open revascularization performed using a vein graft have demonstrated their efficacy and durability against endovascular procedures over time. Unfortunately, numerous situations exist where a suitable vein graft is unavailable, and many practitioners would prefer prosthetic grafts. Moreover, in cases where femoropopliteal bypass above the knee is required and a suitable vein is available, the tendency is to save the vein for more distal revascularizations. In this study, we sought to evaluate whether the endovascular approach for complex femoropopliteal lesions could be advantageous over prosthetic bypass in real-world practice for patients with peripheral arterial disease (PAD).
2. Materials and Methods
This retrospective investigation was performed between January 2013 and December 2021, to identify patients with symptomatic PAD. Patients who underwent open or endovascular limb revascularization for symptomatic PAD were included in the study. Clinical limb presentation was described using the Rutherford classification [
2]. Open or endovascular limb revascularization for complex femoropopliteal lesions was classified as TASC II C and D according to the Trans-Atlantic Inter-Society Consensus for the Management of Peripheral Arterial Disease [
3]. In the endovascular group, patients requiring procedures in below-the-knee (BTK) vessels aside from femoropopliteal revascularization were excluded. Finally, patients with a history of revascularization, either open or endovascular, at any level of the target lower limb arteries were excluded from this study.
The study was approved by the Institutional Review Board of the Independent Ethics Committee (IRB-IEC) and was registered with N. ER.FE.2022.15. Patient consent was waived given the retrospective nature of the study. To enhance clarity, the study ascribed to the STROBE guidelines [
4]. Data regarding demographics, comorbidities, clinical limb presentation, characteristics of the vessel target, and runoff quality before and after the procedure were collected and analysed. Characteristics of the interventions regarding vascular access, devices used, and diameters were also analysed.
Technical success was defined as evidence of successful revascularization with residual stenosis less than 30% after angioplasty and absence of flow-limiting lesions. Major amputation was defined as any lower extremity amputation through or proximal to the ankle joint. Minor amputation was defined as any lower extremity amputation distal to the ankle joint.
The primary endpoints were primary patency, freedom from clinically driven target lesion revascularization (cdTLR), freedom from major adverse limb events (MALE) [major amputation, any intervention to restore patency], freedom from major adverse cardiovascular events (MACE), and freedom from all causes of death. The secondary endpoints were length of hospital stay, duration of the procedure, and cost of materials.
Statistical analysis. Continuous variables are presented as means ± standard deviation for normally distributed data. Variables are presented as percentages. Standardized mean differences were used to compare the prevalence between groups, with statistical significance set at P values >0.05. Primary endpoints were presented by Kaplan–Meier curves, and statistical significance was evaluated by the log-rank test.
3. Results
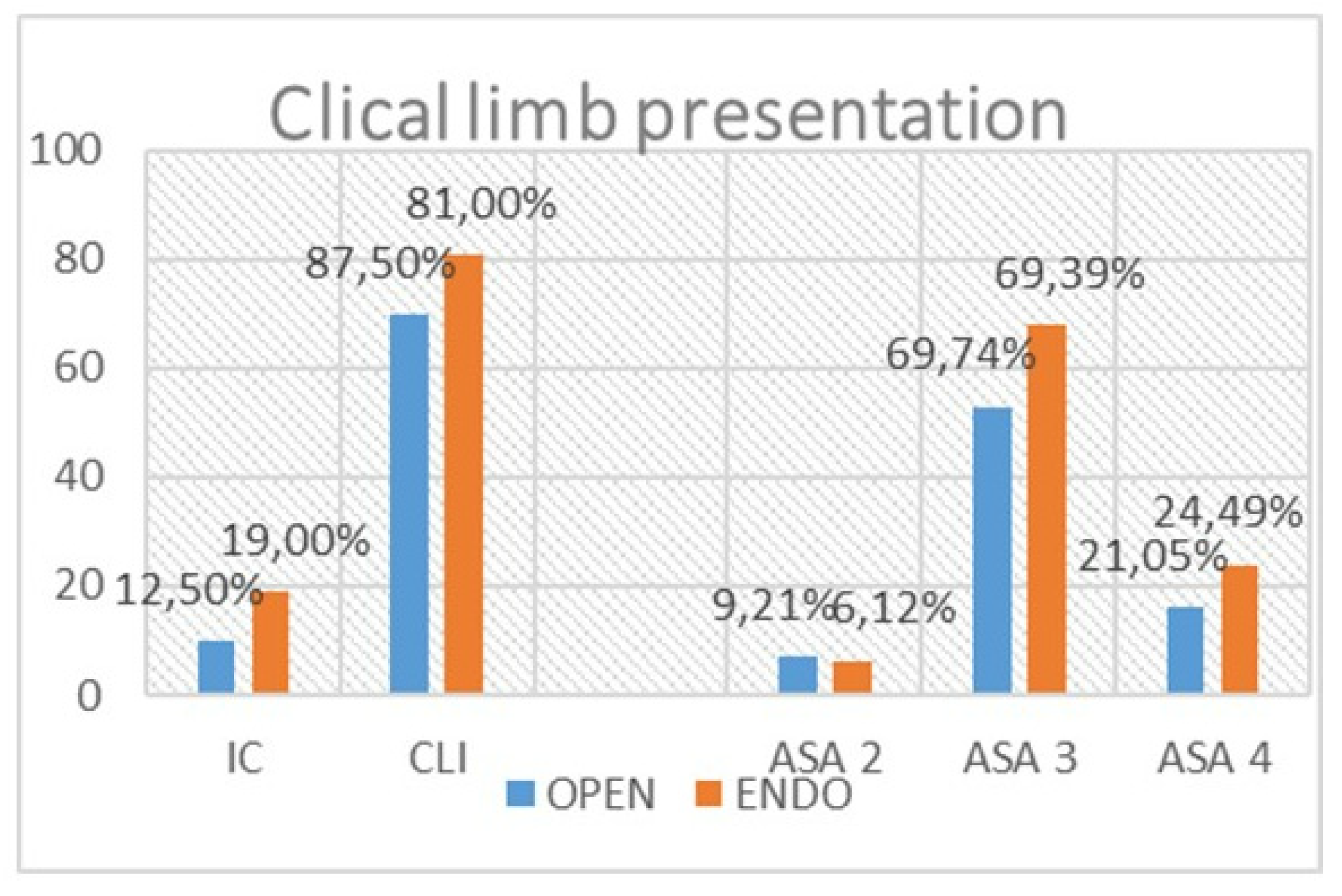
We identified 185 limbs among 174 patients suitable for comparison, wherein 105 were treated with endovascular procedures and 80 with femopopliteal prosthetic bypass. There were no significant differences between the open and endovascular groups regarding TASC II C and D lesions or clinical limb presentation (
Figure 1). In the open group, there were fewer octogenarians (p = 0.02), and no nonagenarians were treated. In the endovascular group, there was a significant prevalence of patients suffering from coronary disease (p = 0.004) [
Table 1]. Despite the differences in age and CAD rate, there were no differences when the patients were classified according to anaesthesia risk (ASA) [
Figure 1]. The median follow-up in January 2023 was 30 months (range:1–4 years) and was done in outpatients by clinical and ultrasound examinations at 1 and 6 months, and annually thereafter.
Run-off vessel quality was worse in the endovascular group, with 11 cases of desert foot, versus none in the open group (
Table 2). In contrast, there were more limbs with 3-runoff vessels in the open group (p < 0.001).
In the endovascular group, 52 procedures were performed percutaneously by puncturing the femoral artery under ultrasound guidance. Hemostasis was done using a percutaneous closure device (AngioSeal Vip, 6 Fr, Terumo). Vascular access was achieved using the femoral cutdown technique in the same group, (
Table 3). These different approaches followed another study which evaluated the outcomes between the two vascular accesses after randomization [
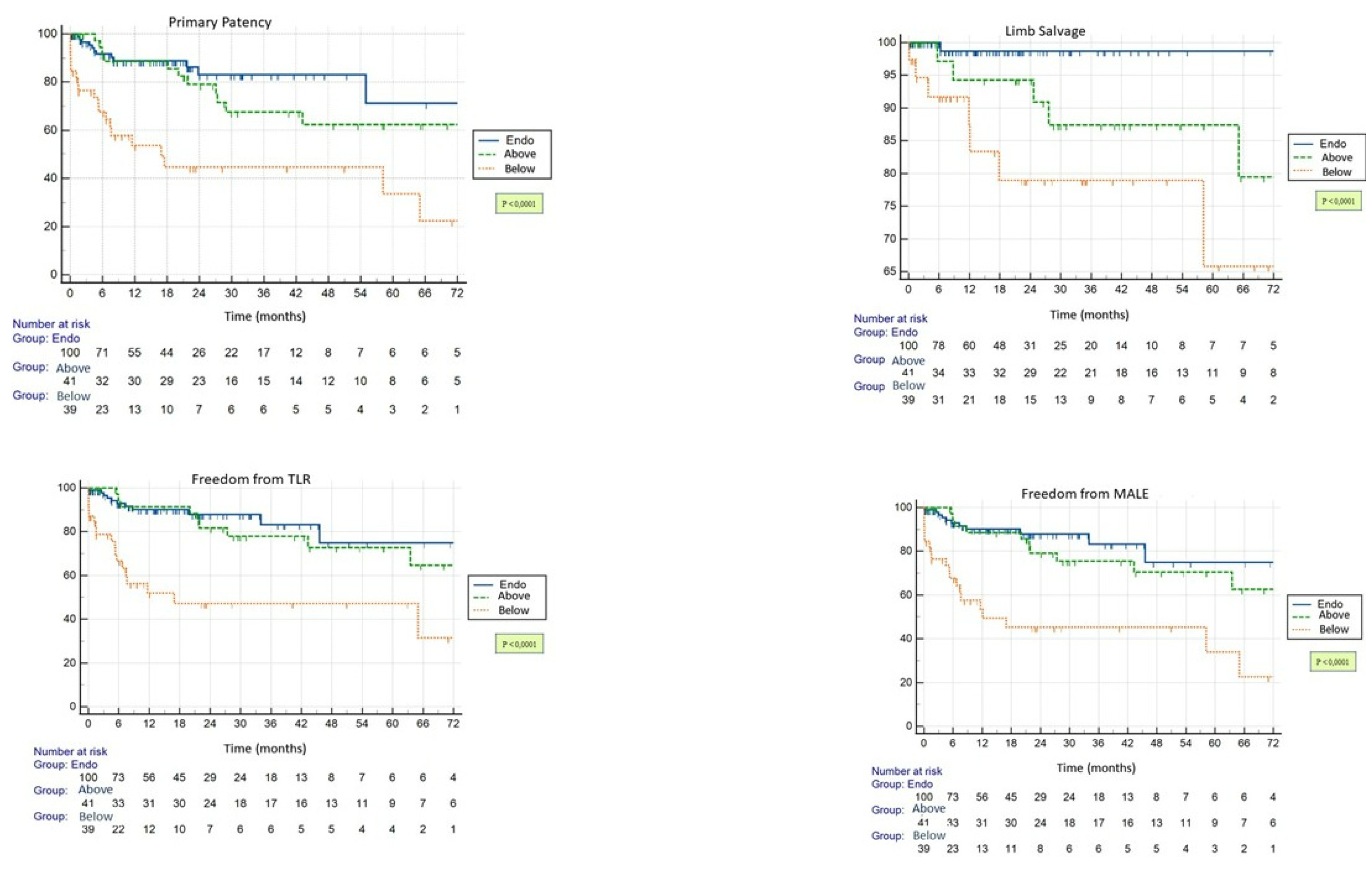
5]. The technical failure of the endovascular procedures was of 4.7% vs 0% in the open group (p = 0.003). In the endovascular group, failure occurred only in cases with totally occluded calcific lesions regardless of the extension in length. These were characterized by failure to cross the lesion with the guidewire in three cases and failure to re-enter the true lumen after crossing it subintimally in the remaining two cases. These five limbs underwent femoro-popliteal bypass above the knee in three cases using an expanded polytetrafluoroethylene (ePTFE) graft and BTK in the remaining two cases using the ipsilateral great saphenous vein. The endovascular group showed superior primary patency (p<0.0001), cdTLR (p<0.0001), MALE (p<0.0001), and freedom from limb loss (p = 0.0018) at 24 months. Further analysis for the open above-the-knee subgroup showed that the above-mentioned endpoints were similar at 12 months and favoured the endovascular group at 24 months (
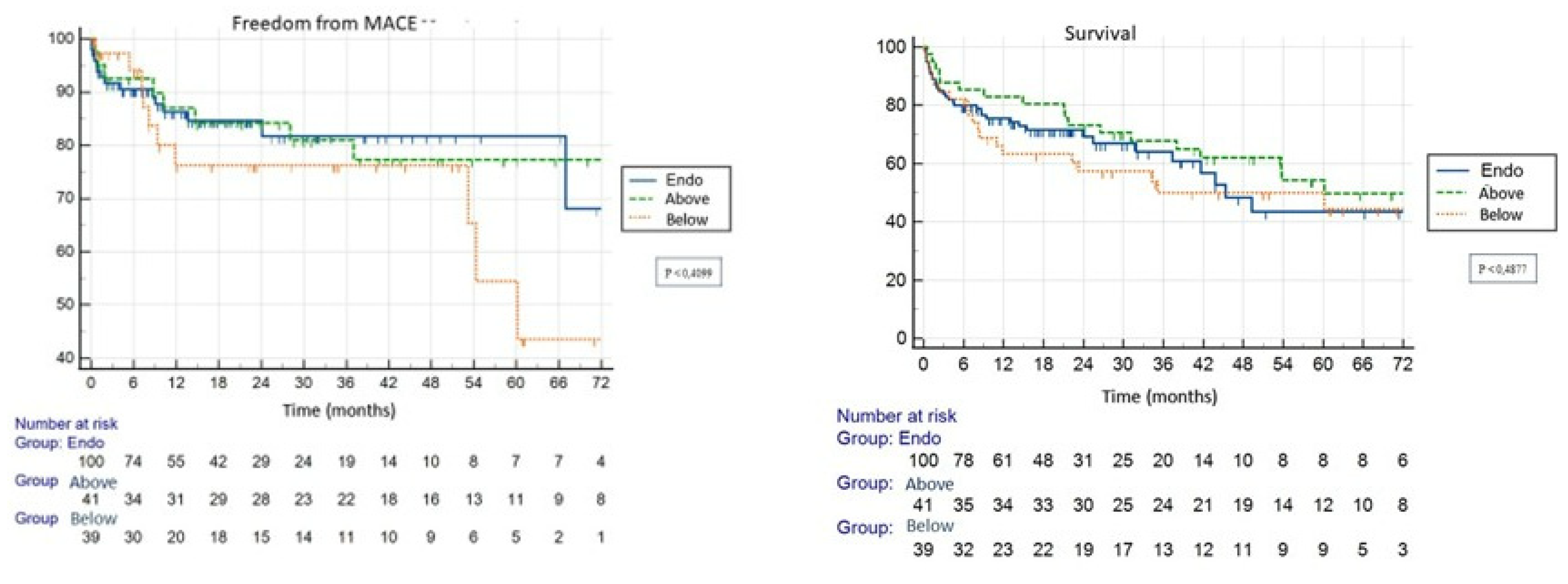
Figure 2). Freedom from MACE and survival rates were similar in both groups (
Figure 3). The procedural time and in-hospital stay were longer in the open group than in the endovascular group (p<0.0001 and p<0.001, respectively). Patients presenting with post-procedural haemoglobin loss was more evident in the open group. For the open surgery group, there were more complications related to vascular access and groin incision, including dehiscence, infection, lymphorrhea, and hematoma (
Table 4). In the percutaneous group there were two groin hematomas which were managed conservatively by compression and in one case there was acute thrombosis due to unsuccessful percutaneous closure device deployment. Finally, the procedural cost was 10-fold lower in the endovascular bypass group than in the prosthetic bypass group. All prosthetic grafts consisted of ePTFE. In the open group, the cost of the material used did not differ from one procedure to another and ranged from 2500 to 3000 euros. In contrast, in the endovascular group, expenditures depended on the type and number of devices used, such as guidewires, balloons, and stents. For a standard procedure, expenditures fluctuated around 243
150 euros and increased for paclitaxel-coated devices varying from 590 to 850 euros, bare metal stents + 340 euro, and on the number of stents delivered.
4. Discussion
Atherosclerotic complex femoropopliteal lesions have been traditionally treated with femoropopliteal bypass, with vein grafts being used as conduits having the best results based on long-term patency [
6,
14]. However, several situations lead to choosing a prosthetic graft, such as unavailability of a suitable vein graft. In select above-the-knee cases, femoropopliteal bypass is required, and most surgeons tend to spare the vein for more distal revascularization. However, the endovascular approach, once reserved for short lesions (TASC II A and B) and frail patients, is currently considered as an alternative to open surgery, even for complex lesions in many centres. This has become possible owing to the continuous technological advancement in the endovascular field, bringing numerous devices dedicated to each stage of the procedure, thus leading to a substantial improvement in outcomes based on technical success and long-term primary patency [
7,
8,
9,
10,
11]. In this study, we aimed to evaluate whether the endovascular approach for long complex lesions could be advantageous for femoro-popliteal prosthetic bypasses regardless of lesion features and anesthesiologic risk. The value of this study is related to the homogeneity of both groups regarding treated lesions, territory affected, clinical limb presentation, and ASA risk.
In our study regarding technical success, open surgery was superior in completing revascularization. Technical failure in our experience was mainly influenced by calcification of the lesions. Calcium is considered a strong predictor of technical failure and patency loss, and several models have been presented to predict outcomes such as the peripheral artery scoring system (PACSS) and Fanelli score [
12,
13]. Regarding this aspect, only complete vessel occlusion influenced technical success rather than extension of the length of the calcifications. We believe that these lesions are the most challenging to cross, and in most cases, the subintimal approach is the only strategy. However, the technical failure rate in our study (4.7%) was significantly lower than the 20% technical success rate for endovascular procedures reported in the BASIL I trial which compared the outcomes in the open and endovascular arms for complex femoro-popliteal lesions [
14]. However, the data reported in this study should be considered outdated as the technical success with new devices is approximately 99%. The main technical issues in these cases are related mainly to failure in crossing the lesion. Moreover, in some cases it is crossed in a subintimal manner to find the reentry point distally. To overcome these issues, guidewires for specific lesions and stages of the procedure have been developed, and are available in every operating room and angiographic suite. Moreover, to overcome the reentry issue in the market there are several devices have been proven safety and efficacy in terms of technical success [
15]. Another issue consists of delivering the devices such as balloons and stents once the lesion has been crossed with a guidewire. In these cases, using atherectomy to remove, even partially, the plaque becomes useful to deliver the above-mentioned devices [
16,
17]. In conclusion, on one hand, these devices substantially increase procedural cost but also increases the success rate of the endovascular procedure for complex lesions. Several studies have reported the need for adjunctive procedures such as atherectomy and provisional stents when dealing with complex femoropopliteal lesions [
18].
Another aspect widely adopted in many centers involves offering endovascular treatment as a minimally invasive approach for frail patients, as is observed in our study. In our cohort, patients treated endovascularly had significantly more comorbidities, while older patients and nonagenarians were not treated using the open approach. However, this choice should be justified in cases where open arm offers better clinical and long-term outcomes based on primary patency, cdTLR, MALE, and survival. Angioplasty with simple old plain balloons is known to offer poor results for long lesions. Here, the need for adjunctive procedures is performed, such as utilising drug-coated devices to improve clinical outcomes [
11,
19,
20,
21,
22,
23]. In the Basil I trial, drug-coated devices or provisional stents were not used which may explain the poor outcomes, in terms of primary patency in the endovascular arm. Overall, the open approach did not have advantages over the endovascular group as the overall long-term outcomes were worse in the open group. In the above-the-knee subgroup, the outcomes, in terms of primary patency, were similar within the first 24 months and then favored the endovascular arm thereafter. In these patients, an endovascular first-line strategy would have been beneficial in terms of operating time, intraoperative blood loss, fast functional recovery, and early discharge. Moreover, in our study, the endovascular approach was beneficial for vascular access management and complications. In this aspect, percutaneous procedures, especially those supported by ultrasound guidance during arterial puncturing and using a percutaneous closure device to perform hemostasis, significantly favored the endovascular choice, even in hostile groins [
5,
21,
23].
Finally, in-hospital stay has become an important goal of public health management which aims to reduce in-hospital management costs and favor patient turnover. Another aspect to deal with is the cost of the materials used in the open group which resulted in higher expenses compared with standard endovascular procedure. Since we did not use expensive devices, such as atherectomy, lithotripsy, intravascular ultrasound, or re-entry devices, it may explain the aforementioned differences. However, the cost of the open group was related to our attitude toward using ePTFE grafts which are expensive.
Limitations of this Study. The main limitation of this study is its retrospective nature. Moreover, the presence of a subgroup wherein vein grafts were used may have beneficial to this study. However, applying specific criteria helped us obtain two homogeneous groups for comparison. Additionally, the many endpoints contributed to the overall completeness of this study.
5. Conclusions
Endovascular procedures are safe in patients at high risk for surgery and show good outcomes at 24 months. Considering the better long-term results in many endpoints of endovascular procedures over prosthetic bypasses, they could be considered the first-line treatment for femoropopliteal complex lesions. Open procedures can be considered as second-line after failure of an endovascular approach in the same arterial territory.
Funding
This study was not supported by any funding.
Institutional Review Board Statement
The study was approved by the Institutional Review Board of the Independent Ethics Committee (IRB-IEC) and was registered with N. ER.FE.2022.15.
Informed Consent Statement
Patient consent was waived given the retrospective nature of the study. To enhance clarity, the study ascribed to the STROBE guidelines.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Conte MS, Bradbury AW, Kolh P, White JV, Dick F, Fitridge R, et al. Global Vascular Guidelines on the Management of Chronic Limb-Threatening Ischemia. Eur J Vasc Endovasc Surg 2019;58(1S):S1-S109.e33. [CrossRef]
- Rutherford RB, Baker JD, Ernst C, Johnston KW, Porter JM, Ahn S, Jones DN. Recommended standards for reports dealing with lower extremity ischemia: revised version. J Vasc Surg. 1997 Sep;26(3):517-38. Erratum in: J Vasc Surg 2001 Apr;33(4):805. [CrossRef] [PubMed]
- Norgren L, Hiatt WR, Dormandy JA, Nehler MR, Harris KA, Fowkes FGR, et al. Inter-Society Consensus for the Management of Peripheral Arterial Disease (TASC II). Eur J Vasc Endovasc Surg 2007;33 Suppl 1:S1-75. [CrossRef]
- Von Elm, E.; Altman, D.G.; Egger, M.; Pocock, S.J.; Gøtzsche, P.C.; Vandenbroucke, J.P.; Strobe Initiative STROBE Initiative.Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observa-tional studies. BMJ 2007, 335, 806–808.
- Zenunaj G, Traina L, Acciarri P, Mucignat M, Scian S, Alesiani F, Gasbarro V Superficial Femoral Artery Access for Infrainguinal Antegrade Endovascular Interventions in the Hostile Groin: A Prospective Randomized Study. Ann Vasc Surg 2022:S0890-5096(22)00200-X. [CrossRef]
- Troisi N, Blasis G, Salvini M, Michelagnoli S, Setacci C; LIMBSAVE registry Collaborative Group. Preliminary six-month outcomes of LIMBSAVE (treatment of critical Limb IscheMia with infragenicular Bypass adopting in situ SAphenous VEin technique) registry. Vascular. 2021 Aug;29(4):589-596. [CrossRef] [PubMed]
- van Reijen NS, Ponchant K, Ubbink DT, Koelemay MJW. Editor’s Choice - The Prognostic Value of the WIfI Classification in Patients with Chronic Limb Threatening Ischaemia: A Systematic Review and Meta-Analysis. Eur J Vasc Endovasc Surg 2019;58(3):362–71. [CrossRef]
- Schillinger M, Sabeti S, Loewe C, Dick P, Amighi J, Mlekusch W, et al. Balloon angioplasty versus implantation of nitinol stents in the superficial femoral artery. N Engl J Med 2006;354(18):1879–88. [CrossRef]
- Dick P, Wallner H, Sabeti S, Loewe C, Mlekusch W, Lammer J, et al. Balloon angioplasty versus stenting with nitinol stents in intermediate length superficial femoral artery lesions. Catheter Cardiovasc Interv 2009;74(7):1090–5. [CrossRef]
- Laird JR, Katzen BT, Scheinert D, Lammer J, Carpenter J, Buchbinder M, et al. Nitinol stent implantation versus balloon angioplasty for lesions in the superficial femoral artery and proximal popliteal artery: twelve-month results from the RESILIENT randomized trial. Circ Cardiovasc Interv 2010;3(3):267–76. [CrossRef]
- Bausback Y, Wittig T, Schmidt A, Zeller T, Bosiers M, Peeters P, et al. Drug-Eluting Stent Versus Drug-Coated Balloon Revascularization in Patients With Femoropopliteal Arterial Disease. J Am Coll Cardiol 2019;73(6):667–79. [CrossRef]
- Okuno S, Iida O, Shiraki T, Fujita M, Masuda M, Okamoto S, Ishihara T, Nanto K, Kanda T, Takahara M, Uematsu M. Impact of Calcification on Clinical Outcomes After Endovascular Therapy for Superficial Femoral Artery Disease: Assessment Using the Peripheral Artery Calcification Scoring System. J Endovasc Ther. 2016 Oct;23(5):731-7. doi: 10.1177/1526602816656612. Epub 2016 Jul 1. PMID: 27369975. [CrossRef] [PubMed]
- Fanelli F, Cannavale A, Gazzetti M, Lucatelli P, Wlderk A, Cirelli C, d'Adamo A, Salvatori FM. Calcium burden assessment and impact on drug-eluting balloons in peripheral arterial disease. Cardiovasc Intervent Radiol. 2014 Aug;37(4):898-907. [CrossRef] [PubMed]
- Bradbury AW, Adam DJ, Bell J, Forbes JF, Fowkes FGR, Gillespie I, et al. Bypass versus Angioplasty in Severe Ischaemia of the Leg (BASIL) trial: Analysis of amputation free and overall survival by treatment received. J Vasc Surg 2010;51(5 Suppl):18S-31S. [CrossRef]
- Mulholland D, Thulasidasan N, Patel A, Katsanos K, Diamantopoulos A. The Outback Re-Entry Device. A Pictorial Review. Vasc Endovascular Surg 2021;55(6):593–600. [CrossRef]
- Bhat TM, Afari ME, Garcia LA. Atherectomy in Peripheral Artery Disease: A Review. J Invasive Cardiol 2017;29(4):135–44.
- Wardle BG, Ambler GK, Radwan RW, Hinchliffe RJ, Twine CP. Atherectomy for peripheral arterial disease. Cochrane Database Syst Rev 2020;9:CD006680. [CrossRef]
- Zenunaj G, Traina L, Acciarri P, Mario Cosacco A, Alesiani F, Baldazzi G, Gasbarro V. Primary Drug-Coated Balloon Versus Drug-Eluting Stent for Native Atherosclerotic Femoropopliteal Lesions: A Systematic Review and Meta-Analysis. Ann Vasc Surg. 2023 May;92:294-303. [CrossRef] [PubMed]
- Tepe G, Laird J, Schneider P, Brodmann M, Krishnan P, Micari A, et al. Drug-coated balloon versus standard percutaneous transluminal angioplasty for the treatment of superficial femoral and popliteal peripheral artery disease: 12-month results from the IN.PACT SFA randomized trial. Circulation 2015;131(5):495–502. [CrossRef]
- Jaff MR, Rosenfield K, Scheinert D, Rocha-Singh K, Benenati J, Nehler M, et al. Drug-coated balloons to improve femoropopliteal artery patency: Rationale and design of the LEVANT 2 trial. Am Heart J 2015;169(4):479–85. [CrossRef]
- Chaudhuri A, York A, Dey R. Percutaneous vascular closure using an anchored collagen plug provides effective haemostasis following both antegrade and retrograde femoral arterial punctures. Eur J Vasc Endovasc Surg 2014;48(2):220–5. [CrossRef]
- Noori VJ, Eldrup-Jørgensen J. A systematic review of vascular closure devices for femoral artery puncture sites. J Vasc Surg 2018;68(3):887–99. [CrossRef]
- Zenunaj G, Traina L, Acciarri P, Spataro C, Gasbarro V. Revascularisation through the obturator foramen of lower limbs with a compromised ipsilateral groin due to infection. Ann R Coll Surg Engl 2020;102(1):14–7. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).