1. Introduction
Vaccination is one of medical science’s greatest achievements [
1]. Nation wide vaccination programs for children, specifically, constituted one of the most successful public health policies in human history, leading to the eradication or control of several terrible diseases of the past [
2]. Yet, not everyone is eager or even willing to have themselves and their children vaccinated. In fact, as recently as 2019 the World Health Organization identified vaccination hesitance as one of the 10 greatest threats to global health [
3].
Vaccination hesitance can have many different roots, with trypanophobia (the fear for needles) and the overall discomfort experienced during the vaccination procedure among the leading ones [
4]. With this fear being a lot more common in toddlers [
5] it is only natural that children experience high levels of discomfort during procedures that include needles, such as the vaccination [
6]. Pediatricians from the American Academy of Pediatrics found that 75% of parents sought to delay vaccination due to concerns of their child’s discomfort [
7], with approximately 45% of the children aged 4–6 years showing serious distress during vaccination [
8]. 10% of the population totally avoids vaccination due to the fear for needles [
9].
In this work we aim to limit and if possible totally alleviate the discomfort experienced by children during the vaccination procedure. Other researchers have already established that the pain and fear children experience during immunisation can be affected by external factors such as parents’ behaviour [
10,
11], breastfeeding [
12,
13,
14] (for younger children), being distracted [
15], receiving a massage [
16], different body positions [
17], sweeteners [
18,
19] and so on.
Herein, addressing this problem, we have present an eXtended Reality (XR) application, VaccineHero. This application aims to enhance the childhood vaccination process by significantly reducing, if not entirely eliminating, the distress and negative emotions typically associated with it. VaccineHero captivates its young users with a 90-second narrative, timed to coincide with the duration of a typical vaccination. Within this immersive virtual world, toddlers take on the role of VaccineHero, an avatar navigating through an adventurous environment that seamlessly merges elements of both virtual and physical reality. The application serves a dual purpose, providing an engaging distraction for the child while also acting as a practical aid for healthcare professionals, ensuring a more streamlined and less distressing vaccination process.
The remaining of this article is organised as follows: Once we review the relevant state of the art in
Section 2, we move on to
Section 3 in which we present in detail our proposal, including the use-case scenario, the architecture of the system and some interesting details regarding its implementation.
Section 4 details the evaluation of the system, comprising the clinical trials of VaccineHero together and the analysis of the gathered data. Finally, in
Section 5 we list our concluding remarks and suggest directions for further research.
2. Relevant literature
The times when medicine was a siloed science are long gone. For more than a century now, medicine has been progressing hand in hand with technology [
20] and reaping the benefits of advancements in other fields. And quite often technological breakthroughs have been followed by related medical breakthroughs or even by the creation of new medical domains.
Advances in electromagnetic radiation lead to the development of medical imaging [
21]. Advances in mobile technology introduced us to tele-medicine [
22]. Advances in machine learning gave birth to clinical decision support systems [
23]. And of course the current advances in artificial intelligence, as seen in tools such as ChatGPT, are expected to again revolutionise healthcare [
24].
Similarly, advances in VR technology are having an impact in varuous areas of the medical field [
25,
26,
27]. The dominant medical application of VR technology is in education [
28,
29,
30], primarily for the training of surgeons [
31,
32]. But that is not the only application domain. For example, in rehabilitation, VR can help children with cerebral palsy regain their walking abilities [
33] or stroke patients to regain control of their arm movements [
34]; for older adults in nursing homes, VR can assist in memory training [
35]; and burn victims’ acute pain during treatment can be reduced via the use of suitable VR applications [
36].
In this work we focus specifically on the use of VR to assist in children’s vaccination. That is not a fundamentally new concept either. For example, in Saudi Arabia the Ministry of Health launched a VR initiative to help children overcome fear of immunisation and blood drawing in 2018 [
37]. But, to the best of our knowledge, no data have been published regarding either the specifics of the plan or the effectiveness of the implementation. Similarly, the Ogilvy company in Brazil announced in 2018 the development of a VR solution to support children’s vaccination [
38]. But there is no indication of the tool ever reaching the market or of its actual effectiveness.
A more recent work that uses VR to help with children’s vaccination and actually reports on the achieved results was published in 2022 [
39]. This work is fundamentally different from our approach, in the sense it uses VR as a mood setting tool before the vaccination and not as an experience that is concurrent to the actual vaccination. More importantly, it examines the experience solely from the point of view of the medical professional, examining only the opinions of the nurses and not assessing how the children actually experience the vaccination process.
Thus, our study of the relevant literature identifies a clear research gap and unanswered research questions: Can VR be used to enhance the vaccination procedure, as experienced by the children? And, if yes, how? We provide an answer to these questions in this work, in the following sections.
3. The VaccineHero system
3.1. Concept and use case scenario
Research has shown that distraction is a very effective way to mitigate both fear and pain associated with vaccination in children [
40]. With VaccineHero we build on this notion and design a system and vaccination procedure that aims to keep the child distracted throughout the vaccination process.
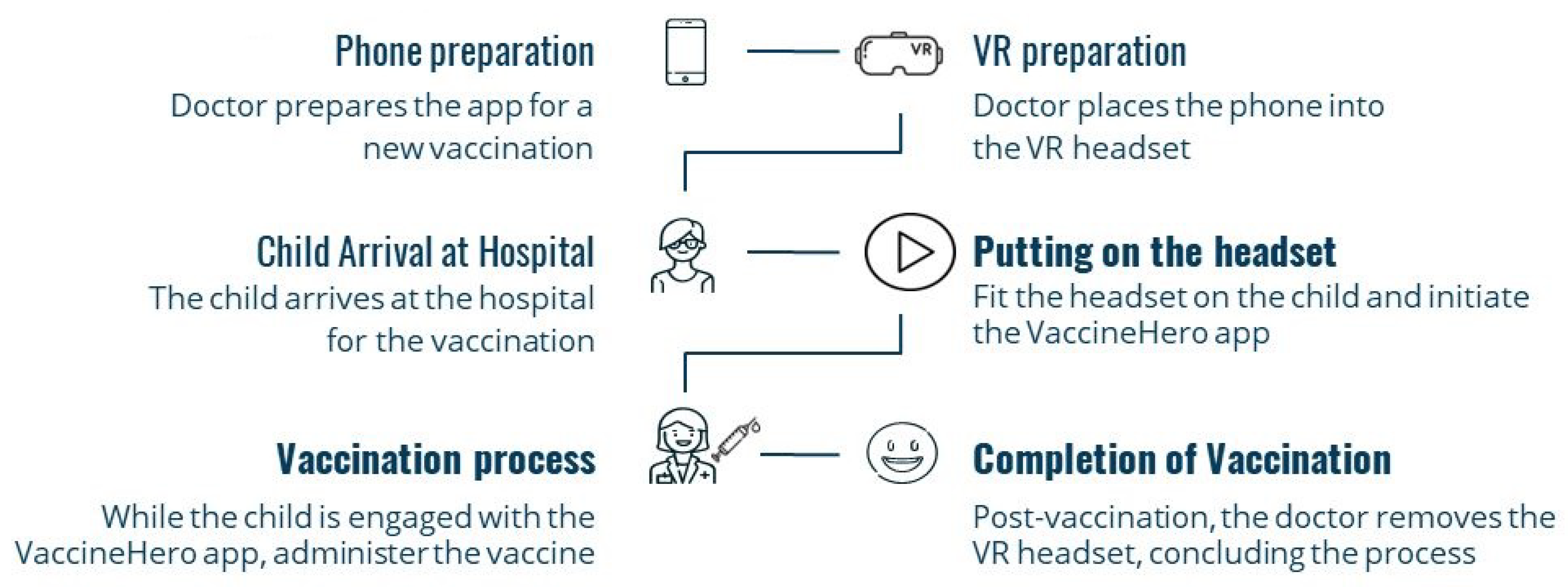
More specifically, in our proposal vaccination follows the flow of
Figure 1. During office set up, the VaccineHero app is loaded on an Android phone and the phone is placed in a headset. The headset is of a smaller size, so that it is suitable for children. Offices that receive children of different ages may have multiple headsets of different sizes ready to use.
Upon arrival at the clinic or doctor’s office, a child is fitted with a VR headset, so that no time is spent contemplating the vaccination procedure and starting to worry. The VR content starts to play and the child assumes the role of the hero and enjoys an immersive experience in which a 3D world is explored and a magician is encountered.
Twice in the immersive experience the magician touches the left arm of the hero. The doctor touches the left arm of the child at the same times, blurring the boundaries between the virtual and the physical world; hence the characterisation of our solution as extended rather than virtual reality.
The first time the doctor touches the arm of the child, it is to clean the vaccination area with cotton and alcohol. The second touch is with the needle in order to deliver the vaccine. Thus, the vaccination is completed seamlessly with the VR content and the child remains unaware, calm and free of pain.
Following the completion of the vaccination, the VR story is soon concluded, the doctor removes the headset and the child is free to go, vaccinated and entertained!
3.2. System architecture
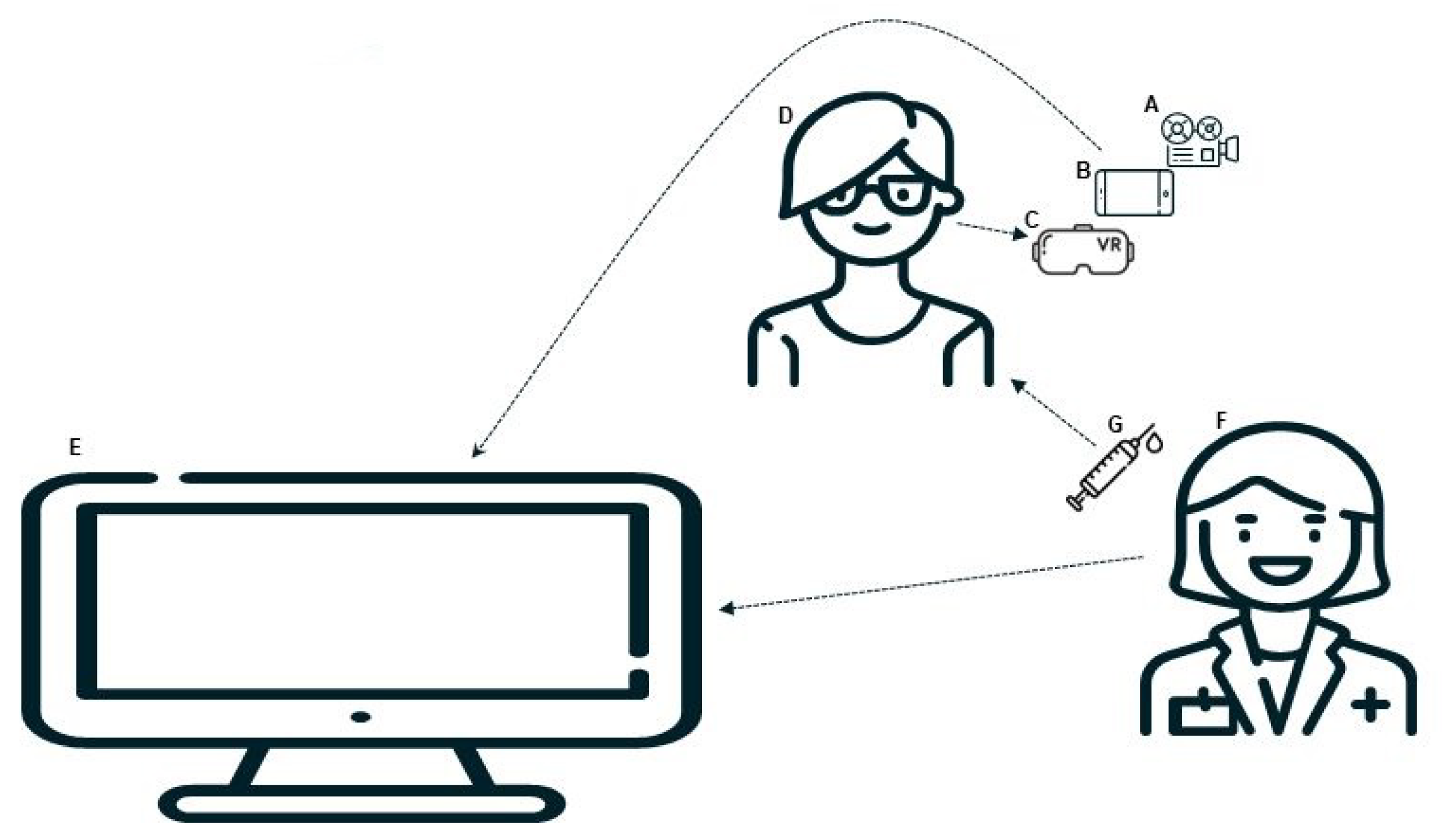
The architecture of the proposed approach is summarised in
Figure 2. The core of the VaccineHero solution is a 90-second immersive three dimensional experience (A in the figure), including a complete 3D world as seen from the point of view of an inanimate hero sitting in the centre of the scene, a magician avatar that interacts with the hero and the accompanying stereophonic sound that completes and enhances the immersion.
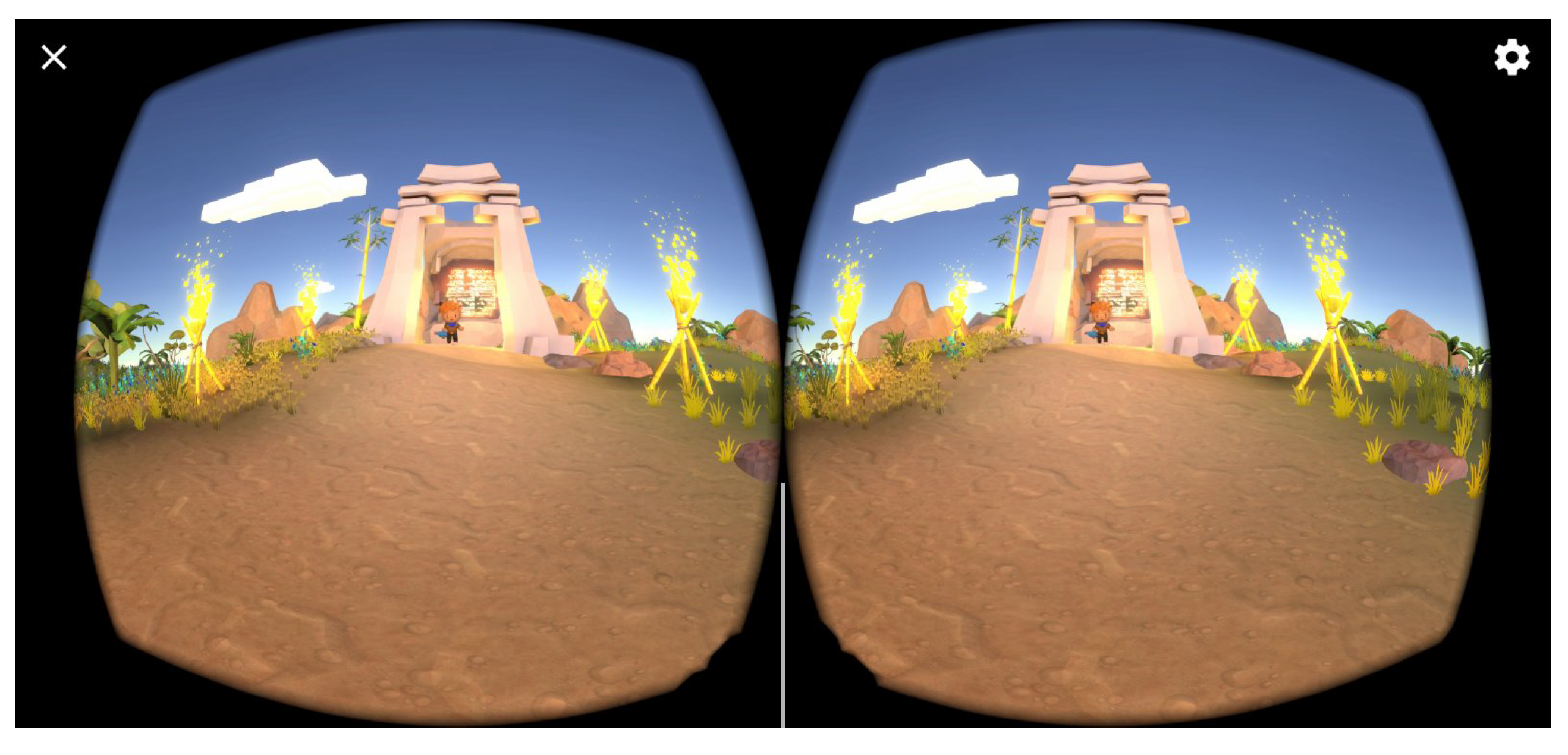
The VR application is loaded on an Android phone (B) and is set up to project to a headset. In this set up, as shown in
Figure 3, the phone’s monitor is split in two parts, each one displaying the scene as would be seen from the left or right eye, respectively. The minor differences between the two displays, when each one is seen by the left and the right eye, trick the brain into sensing depth where there is none, thus creating the 3D experience.
The phone is placed in a headset device (C) that can be fitted on the child patient (D). The headset aligns the two displays with the eyes and force the viewing of the content in the proper way for the three dimensional feeling to be stimulated. The child is also fitted with earbuds through which the content’s audio is delivered.
The 3D content that is displayed on the screen on the phone is simultaneously displayed on an external monitor (E) as well, using Miracast [
41]. This allows the doctor (F) to observe the progression of the VR story and perfectly time the delivery of the vaccination (G) so that it coincides with the moments in the video when the magician touches the hero’s arm.
3.3. Implementation considerations
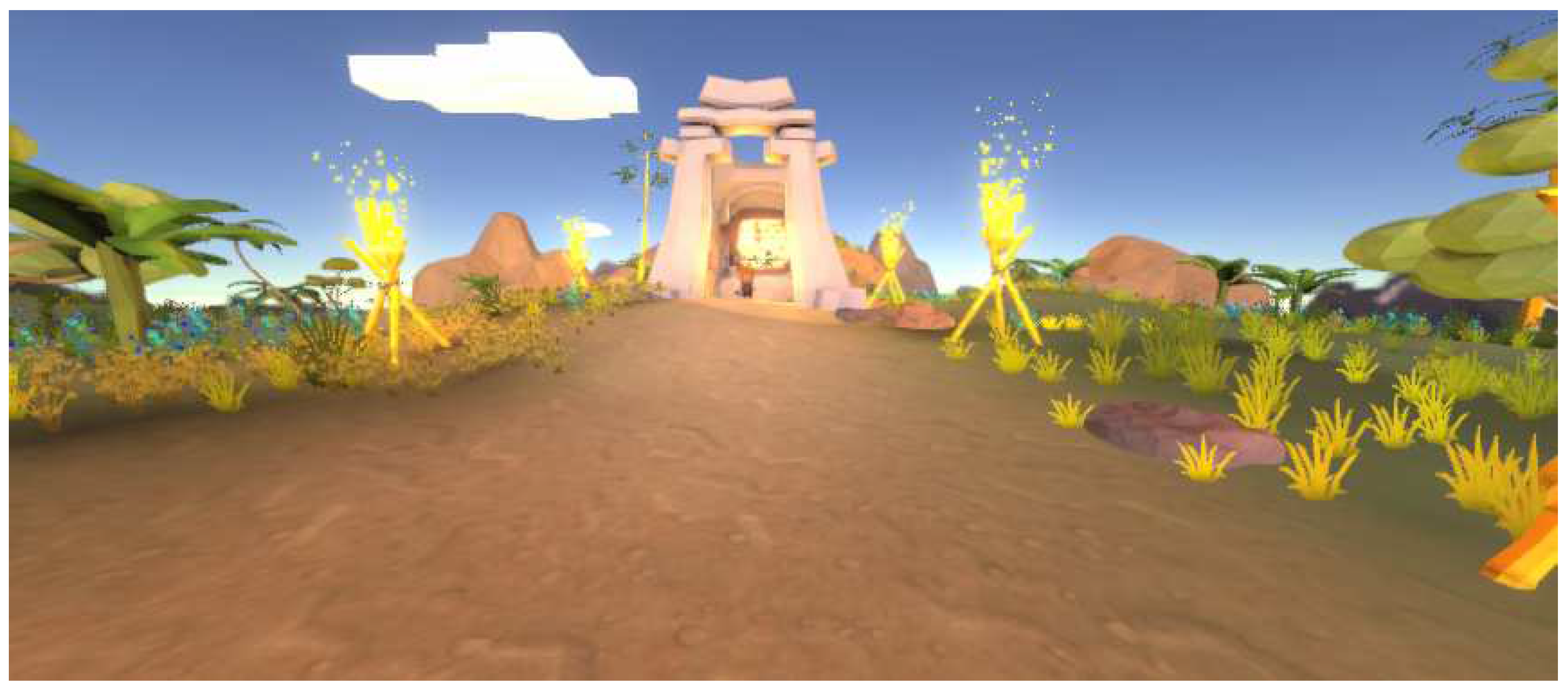
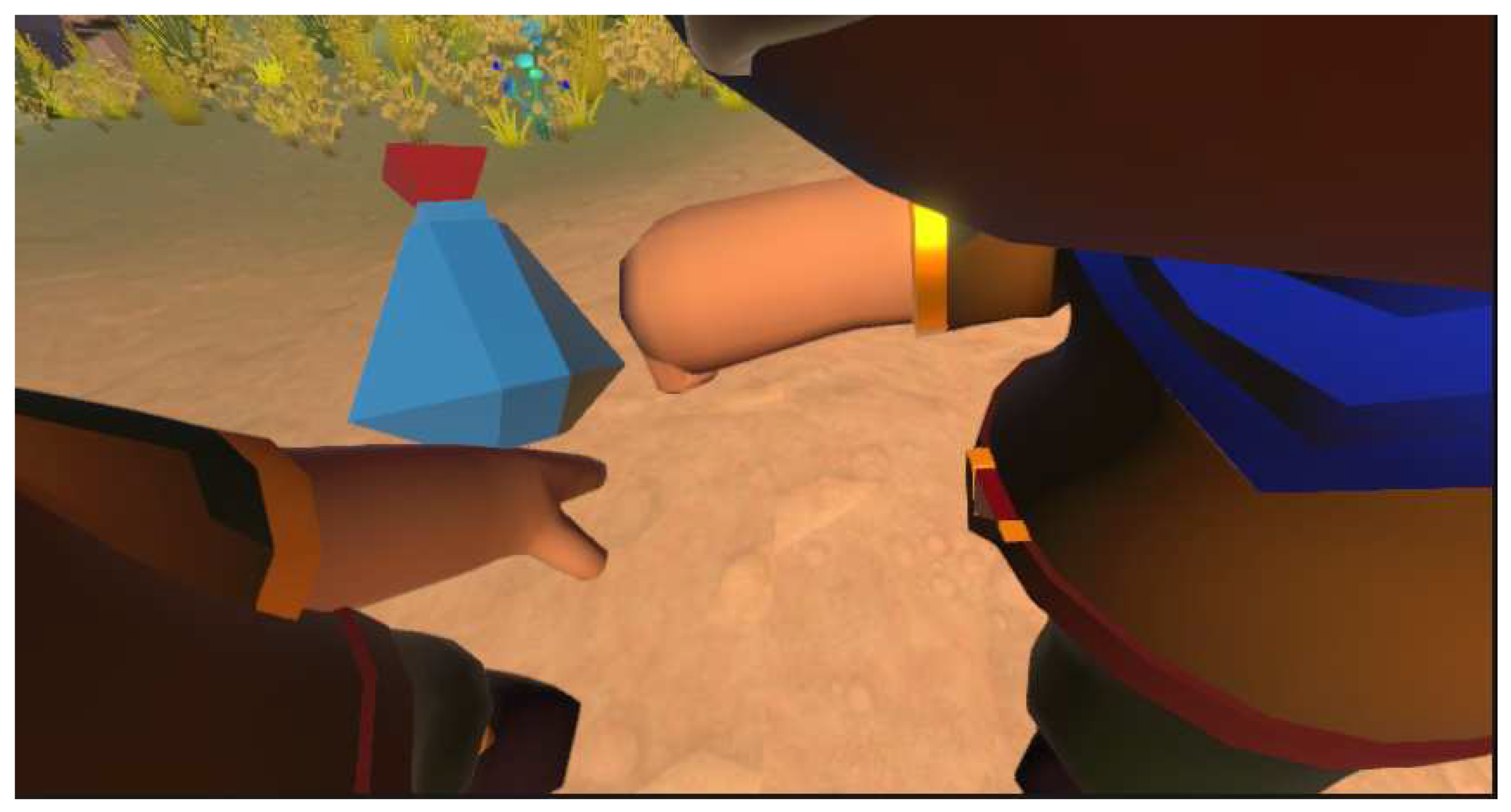
For the implementation of the VaccineHero application, the Unity game engine was utilized in combination with the C# programming language. The main scene of the 3D world (
Figure 4) was populated with models from the Unity Asset Store which were processed as needed through the Unity application, in order to adapt to the needs of the game. The processing included the improvement of the textures and analysis of the models, as well as the correction of compatibility problems between some of the models and the Unity app.
The models have been enriched with the addition of new functions, such as movements and special effects, which enhance the overall user experience.
When it comes to sound, there is music in the background throughout the story, which helps create a pleasant atmosphere. Additionally, scripts are used to add sounds to different events in the VR world, which combine to create an interesting, pleasant, seamless and immersive experience for the child. The addition of the sounds was performed by using Audio Source and adding an audio clip to each relevant component.
In order to achieve the connection between the virtual and physical world, the story that is presented to the child includes two key moments. In the first one, the magician touches the hero with an elixir (see
Figure 5) and in the second one the magician touches the hero again in order to bestow magical powers upon them.
Regarding the duration and important key moments of the overall story, one needs to keep in mind that the main goal of the application is to support the vaccination of toddlers. The story is not developed with the intention to optimise its artistic value or even the stimulation of the children but rather to facilitate the work of the medical professional. Therefore, our team observed and timed a number of real life conventional vaccinations; average times were logged and were then presented to doctors and confirmed by them. That is how the overall duration of 90 seconds was determined, as well as the exact time and duration of each contact between the magician and the hero, so that it will be convenient for the medical professionals to clean the area of vaccination with alcohol, leave enough time for the area to dry and then return to perform the vaccination at a normal pace.
The decision was made to target the Android operating system in the development of the application. As Android devices are often at the lower end of cost and processing capabilities, graphics have been adjusted to render correctly on devices with limited processing power. But this has been done in a way that any reduced detail will not affect the scene in a way that it might appear less descriptive, vivid or believable.
A peculiarity of the implementation is that the story is designed to be experienced in first-person, with the camera placed where the eyes of the hero would be. As the camera is allowed to rotate freely to follow the movement of the head of the child, the head had to be removed from the hero avatar. This way we avoid the danger of it interfering with the camera and appearing in the display, making it seem as if the child were looking inside their own head.
It is worth noting that although any headset can be supported, the design and implementation was done with two solutions in mind, in order to best support the real life application of vaccination. The first solution is that of the (now discontinued, but still available in various store for purchase) Google Cardboard. The advantage of the Cardboard is that it is made of cheap materials (see
Figure 6a) and when purchased in bulk it can cost just a few cents per item. Thus, it can be treated as a single use expendable item, that is thrown away after the vaccination, similarly to the cotton and needle.
The other solution is that of a more robust headset, such as the one presented in
Figure 6b, that after each use can be sprayed with disinfectant and then wiped clean. In both cases, given the medical nature of the application, the fundamental requirement is that no tools are reused by different patients if they have not first been properly disenfected.
4. Clinical trials and evaluation
4.1. Ground truth
We have not been able to locate any similar study that used VR to facilitate vaccination and published quantified data regarding the discomfort levels of the children, so that we compare our approach against it. Therefore, in order to assess the efficacy of our approach, we can only compare it against the conventional approach of immunisation.
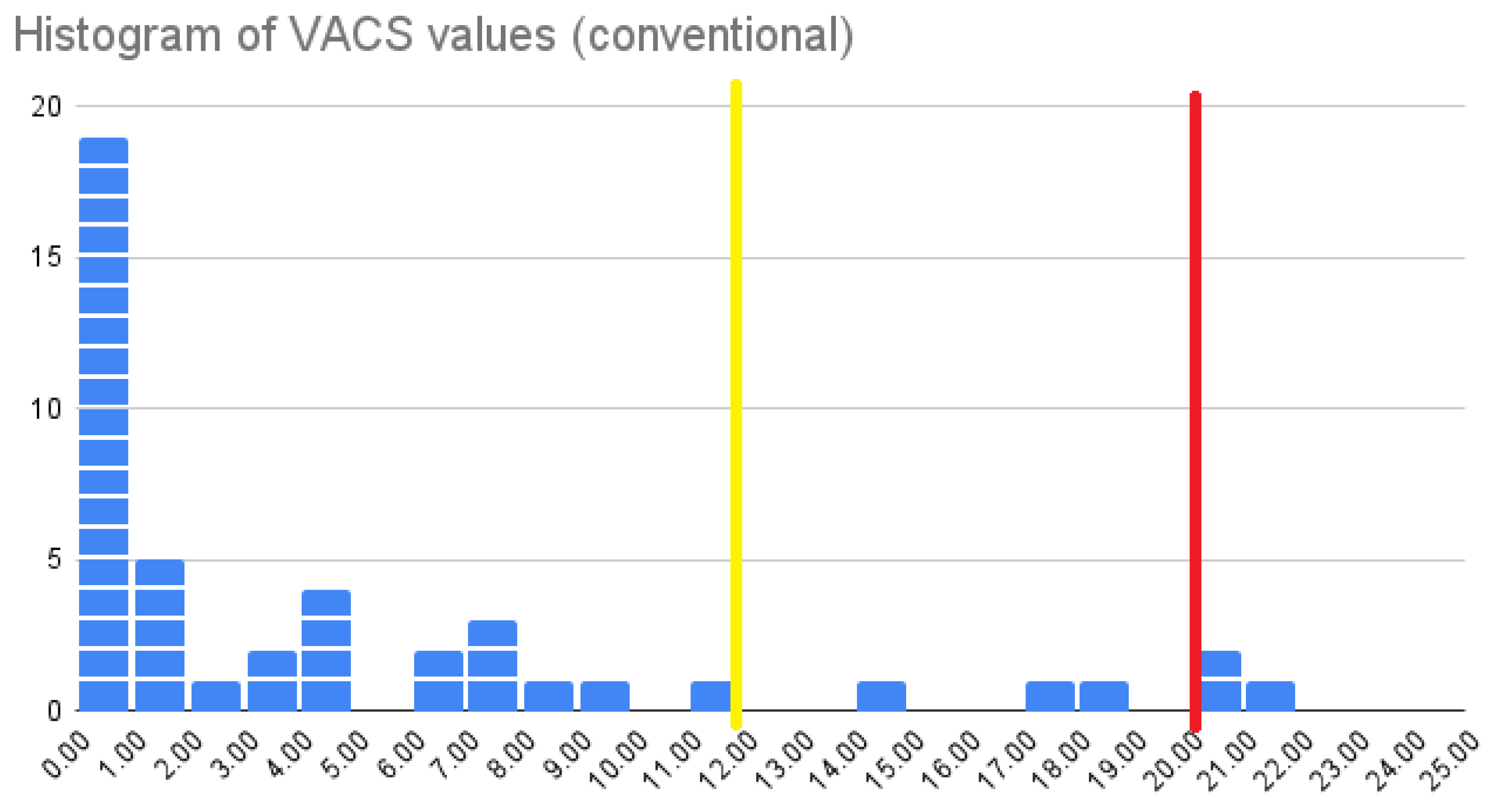
In previous work we have applied the conventional immunisation approach to a cohort of 40 children and recorded the VACS values [
6]; VACS, the VAccination diComfort Scale, is a methodological tool that quantifies children’s discomfort during vaccination on a scale from 0 to 25, with 0 indicating no discomfort at all and 25 corresponding to maximum distress.
In
Figure 7 we present the histogram of VACS values for the cohort of 40 children aged 2-12 years old that were vaccinated conventionally. In our previous work we found that doctors considered vaccination procedures to have been smooth with acceptable levels of children’s discomfort when VACS values had not surpassed 19, whilst children considered the experience acceptable when VACS values where bellow 11. These two thresholds are indicated in the figure with red and yellow colours, respectively.
In that cohort we observed that the average VACS value for children’s vaccinations is 4.752, 40% of children do not experience any discomfort at all (they have a VACS value of 0) and that for the remaining children that do experience some discomfort the average VACS value is 7.92.
These are the values against which we will compare the performance of VaccineHero.
4.2. Trial settings
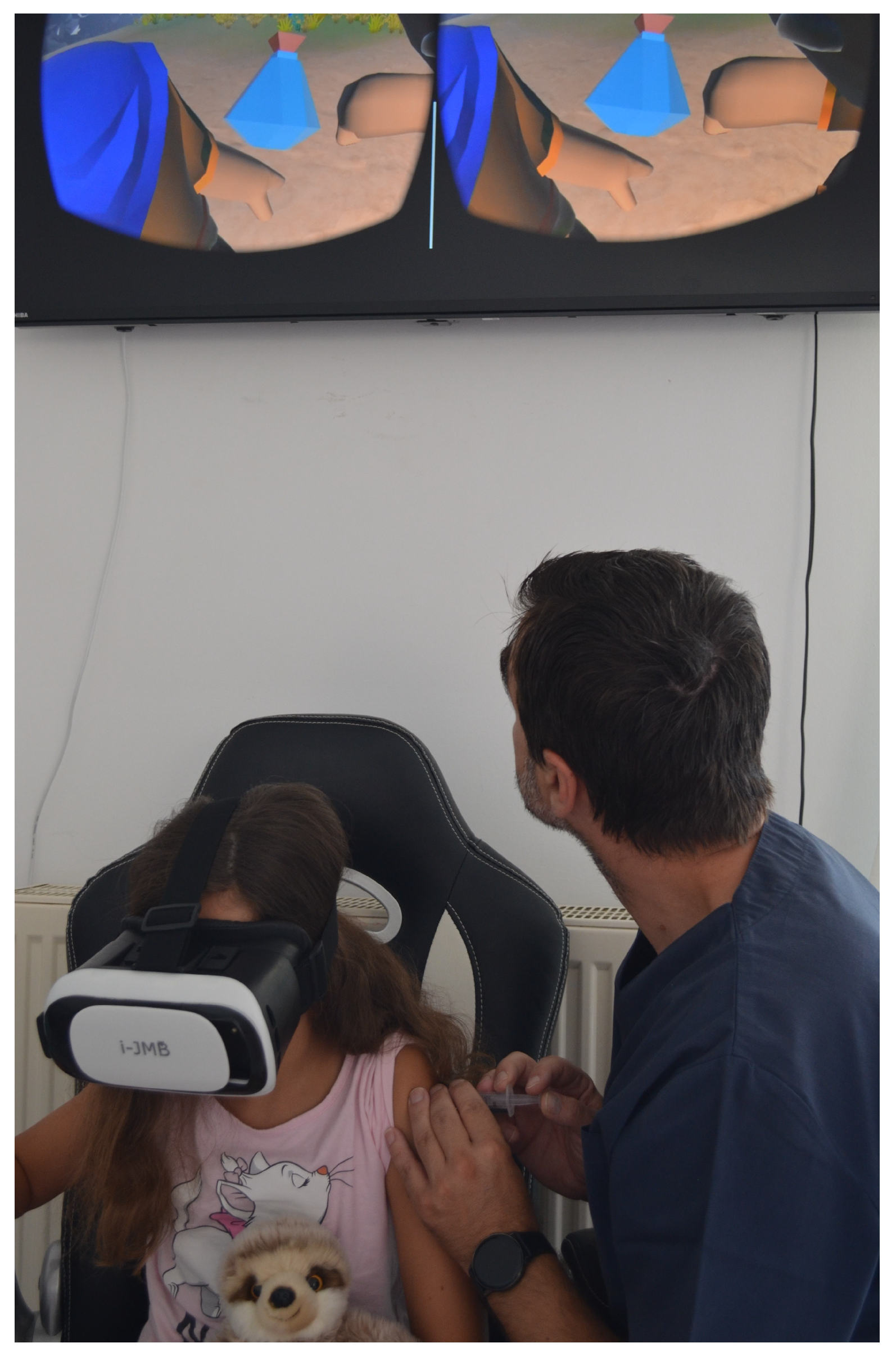
In order to assess the efficacy of the VaccineHero system and validate the proposed approach, a clinical trial was set up, involving two doctors with their independent clinical practices. The doctors were trained by our team on the use of the VaccineHero system, VaccineHero was deployed on their phones and Miracast was activated to connect to the TV monitors in their offices. The doctors were also trained on the use of the VAccination Discimfort Scale in order to assess children’s discomfort in a uniform and objective manner.
In
Figure 8 we see one of the doctors using the VaccineHero system in order to complete the immunisation of a young girl. In the figure we see the doctor observing the external monitor in order to perfectly time the delivery of the vaccination. For each such immunisation the VACS scale data were recorded and forwarded to our team in an anonymised manner, in order to be further processed as needed for our research.
4.3. Clinical data and findings
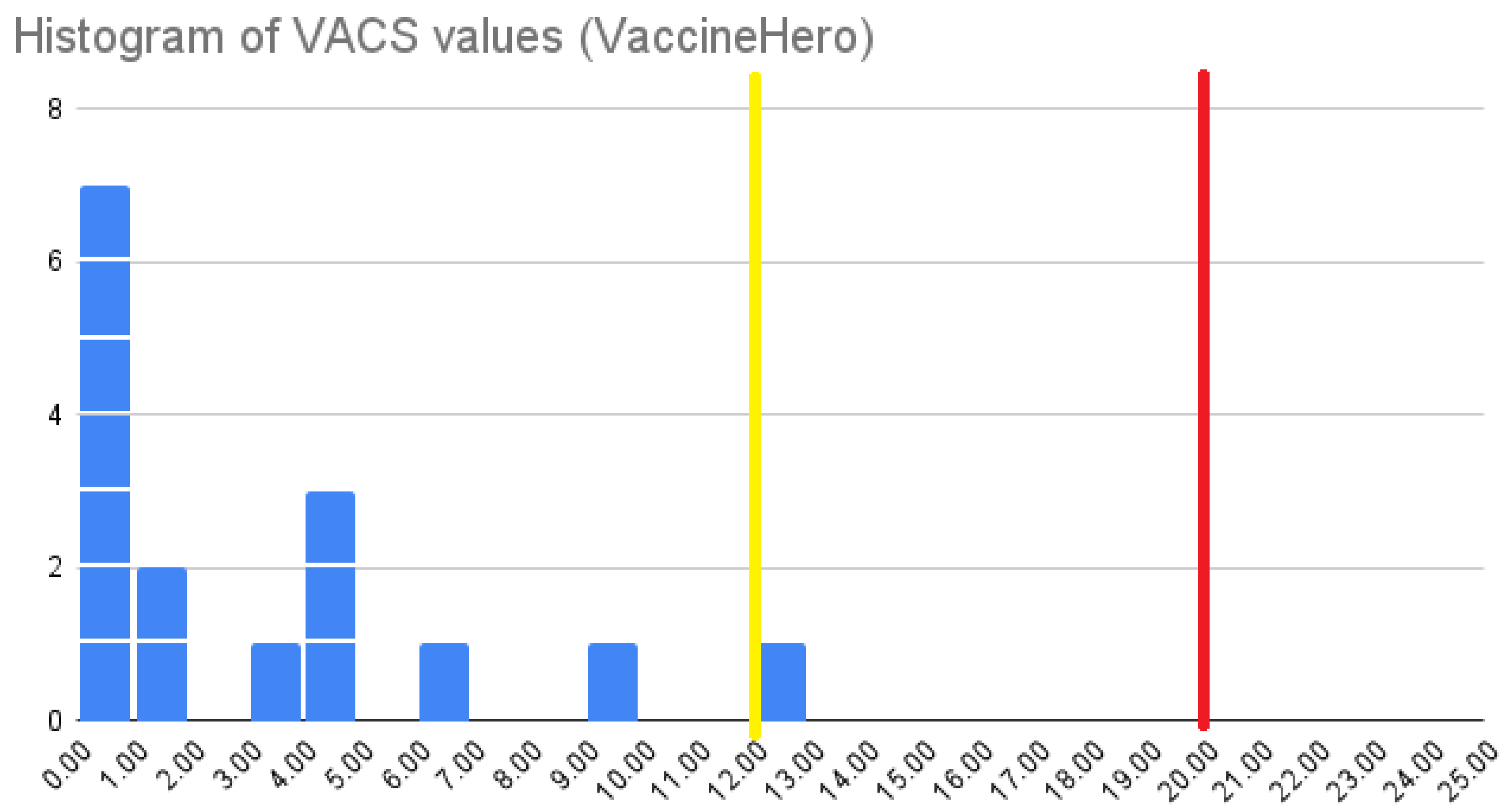
In total, 16 young patients aged 4-12 years old were vaccinated using the VaccineHero application in the period between June 6 and July 4, 2023. VACS values were recorded for the children’s experiences and the histogram of these values is presented in
Figure 9.
Comparing the two histograms (of
Figure 7 and
Figure 9) we observe that the percentage of children that experience no discomfort whatsoever when vaccinated conventionally is 40% and that is elevated to 44% when using the VaccineHero system. Taking into account the relatively small cohort of 16 children in the VaccineHero trial, we consider this raise of 10% to be marginal. Therefore it is inconclusive whether VaccineHero indeed helps more children experience a discomfort-free immunisation, but it is clear that it does not augment the percentage of children that are troubled by the experience. We conclude that, when considering only the percentage of the children that experience any level discomfort, VaccineHero is at least as good as the conventional approach. Therefore it fulfils the principle of “First, do no harm”, which is central in the ethics of healthcare.
Let us now examine the observed VACS values in more detail. When examining the whole cohort of children we acquire an average VACS value of 2.75. This constitutes a reduction of 42%, compared to the 4.752 average VACS value observed when using the conventional vaccination approach. Similarly, when focusing only on the children for whom the VACS value is greater than zero, i.e. the children that do feel some level of discomfort, the average VACS value when using VaccineHero is 4.89. We have a reduction of 38%, compared to the 7.92 average VACS value observed when following the conventional immunisation method.
Another point to consider is how bad can things get for the children. The maximum observed value of VACS when using VaccineHero is 12. That is considerably lower than the value of 19 that doctors consider acceptable discomfort and very close to the value of 11 that was found to be considered acceptable by children. For comparison, in the conventional vaccination approach the maximum observed VACS value was 21, above the acceptable thresholds for both doctors and children.
Overall, we conclude that VaccineHero does not necessarily alter the percentage of children that feel some discomfort. But for those children that do feel discomfort, it makes a huge difference, reducing their discomfort levels by approximately 40% and making the overall experience acceptable to both children and doctors.
5. Conclusions
In this work we presented VaccineHero, an eXtended Reality system that aims to reduce toddler’s discomfort during the immunisation medical procedure. After discussing the relevant literature, we presented the main concept of our proposal and illustrated the implementation of the VaccineHero system. A clinical trial involving two different clinics and doctors was implemented and the efficacy of the system was compared against the conventional immunisation method.
An impressive - in our subjective opinion - reduction of 40% in children’s measured discomfort was observed and extreme discomfort was eliminated altogether, which validated our approach and established the efficacy of our implementation. With young children making up a quarter of the world’s population, any intervention that affects the quality of their experience in a procedure as frequent as children’s vaccination, and by extension the quality of the experience of their parents as well, is an intervention that has the potential to make a huge difference in a lot of people’s quality of life.
The fact that VaccineHero requires only a simple headset that is cheap, easy to acquire and reusable, a simple android phone, and a TV monitor that most doctors’ offices already have, makes it a very affordable solution. That, combined with the fact that no special prior knowledge is required from the doctors who can be trained to use the system within a few minutes, makes VaccineHero easy to be widely adopted, thus having the potential to reach and help thousands of children. In fact, we are currently in the process of deploying VaccineHero and training physicians in a number of locations in Athens but also in other cities in Greece, further away from the capital.
We are of course pleased with the reduction we have observed in children’s discomfort when using VaccineHero as well as with its potential to reach even more children. Still, much more can be done to further extend both the current work and the system in general. Regarding the evaluation of the work, we intend to keep gathering data, in order to perform an assessment with a data set comprising several hundreds of patients. That will allow us to calculate the average VACS values with greater reliability and smaller error margins. It will also be interesting to examine not just the overall value of VACS, which describes the total discomfort experience by the child in the whole procedure, but also the independent components in order to assess in which stages of the vaccination procedure VaccineHero has the biggest impact and in which stages more could be achieved.
Regarding the features of the system, it is now configured to suit vaccination in the left arm, which works best for right handed children. With right handed individuals constituting 90-95% of the population [
42,
43], there is an additional 5-10% that is not served equally well by this version of VaccineHero. In our future work we intend to make the application configurable, so that the arm of immunisation can be selected by the doctor.
Finally regarding the scope of application, vaccination is not the only possibility. Distractions have been shown to have a positive impact on the blood draw experience [
44,
45] and fear of needles has been found to be a deterrent for blood donation [
46]. New versions of the application can be adapted to support both of these medical operations, helping not only children but also grown ups who may experience discomfort with procedures that involve needles.
Author Contributions
Conceptualization, S.A., V.R., M.W. and V.P; methodology, M.W. and V.P.; Software, V.R.; validation, S.A; resources, S.A., M.W. and V.P.; data curation, M.W.; writing—original draft preparation, S.A, V.R. and M.W.; writing—review and editing, V.P., G.L.; visualization, V.R. and M.W; supervision, M.W. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Institutional Review Board Statement
The research described herein has been approved by the Research Ethics Committee of the University of Peloponnese (approval number 15884/2023).
Data Availability Statement
The data presented in this study are available upon reasonable request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Cassimos, D.C.; Effraimidou, E.; Medic, S.; Konstantinidis, T.; Theodoridou, M.; Maltezou, H.C. Vaccination Programs for Adults in Europe, 2019. Vaccines 2020, 8, 34. [Google Scholar] [CrossRef]
- Orenstein, W.A.; Ahmet, R. Simply put: Vaccination saves lives. Proc. Natl. Acad. Sci. USA 2017, 114, 4031–4033. [Google Scholar] [CrossRef]
- World Health Organization. Ten threats to global health in 2019. Available online: https://www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed on 4 August 2023).
- Hornsey, M. J., Harris, E. A., & Fielding, K. S. (2018). The psychological roots of anti-vaccination attitudes: A 24-nation investigation. Health Psychology, 37(4), 307–315. [CrossRef]
- Orenius T, LicPsych, Säilä H, Mikola K, Ristolainen L. Fear of Injections and Needle Phobia Among Children and Adolescents: An Overview of Psychological, Behavioral, and Contextual Factors. SAGE Open Nursing. 2018;4. [CrossRef]
- Wallace, M.; Antonopoulos, S.; Poulopoulos, V. VACS: VAccination disComfort Scale. Clin. Pract. 2022, 12, 1078–1091. [Google Scholar] [CrossRef]
- Hough-Telford C, Kimberlin DW, Aban I, Hitchcock WP, Almquist J, Kratz R, et al. Vaccine delays, refusals, and patient dismissals: a survey of pediatricians. Pediatrics. (2016) 138:e20162127. [CrossRef]
- Jacobson RM, Swan A, Adegbenro A, Ludington SL, Wollan PC, Poland GA. Making vaccines more acceptable — methods to prevent and minimize pain and other common adverse events associated with vaccines. Vaccine. (2001) 19:2418–27. [CrossRef]
- Taddio A, Appleton M, Bortolussi R, et al. Reducing the pain of childhood vaccination: an evidence-based clinical practice guideline. CMAJ. 2010;182(18):E843-E855. [CrossRef]
- Badovinac, S.; Gennis, H.; Riddell, R.P.; Garfield, H.; Greenberg, S. Understanding the Relative Contributions of Sensitive and Insensitive Parent Behaviors on Infant Vaccination Pain. Children 2018, 5, 80. [Google Scholar] [CrossRef]
- Blount, R.L.; Devine, K.A.; Cheng, P.S.; Simons, L.E.; Hayutin, L. The impact of adult behaviors and vocalizations on infant distress during immunizations. J. Pediatr. Psychol. 2008, 33, 1163–1174. [Google Scholar] [CrossRef]
- Esfahani MS, Sheykhi S, Abdeyazdan Z, Jodakee M, Boroumandfar K. A comparative study on vaccination pain in the methods of massage therapy and mothers’ breast feeding during injection of infants referring to Navabsafavi Health Care Center in Isfahan. Iran J Nurs Midwifery Res. 2013;18(6):494-498.
- Osinaike BB, Oyedeji AO, Adeoye OT, Dairo MD, Aderinto DA. Effect of breastfeeding during venepuncture in neonates. Ann Trop Paediatr. 2007;27:201–5. [CrossRef]
- Gray L, Miller LW, Phillipp BL, Blass EM. Breastfeeding is analgesic in healthy newborns. Pediatrics. 2002;109:590–3. [CrossRef]
- Cohen, L.L., MacLaren, J.E., Fortson, B.L., Friedman, A., DeMore, M., Lim, C.S., Shelton, E. and Gangaram, B., 2006. Randomized clinical trial of distraction for infant immunization pain. Pain, 125(1-2), pp.165-171. [CrossRef]
- Golinau B, Krane E, Seybold J, Almgren C, Anand KJ. Non-pharmacological techniques for pain management in neonates. Semin Perinatol. 2007;31:318–22. [CrossRef]
- Lacey, Colleen M., Marsha Finkelstein, and Megan V. Thygeson. "The impact of positioning on fear during immunizations: supine versus sitting up." Journal of pediatric nursing 23, no. 3 (2008): 195-200. [CrossRef]
- Thyr, M., Sundholm, A., Teeland, L. and Rahm, V.A., 2007. Oral glucose as an analgesic to reduce infant distress following immunization at the age of 3, 5 and 12 months. Acta Paediatrica, 96(2), pp.233-236. [CrossRef]
- Golestan M, Sadrebafghi M, Akhavan Karbasi S, Eslami Z, Hashemi A, Mirnaseri F, et al. Comparison Pain relieving effects of glucose and water in neonates. Iran J Pediatr. 2006;16:441–6.
- Thomas, Lewis. “On the Science and Technology of Medicine.” Daedalus, vol. 117, no. 3, 1988, pp. 299–316. JSTOR, http://www.jstor.org/stable/20025180. Accessed 4 Aug. 2023.
- Bradley WG. History of medical imaging. Proceedings of the American Philosophical Society. 2008 Sep 1;152(3):349-61.
- Maglogiannis, Ilias G., Kostas Karpouzis, and Manolis Wallace. "Image and signal processing for networked e-health applications." Synthesis Lectures On Biomedical Engineering 1, no. 1 (2005): 1-108. [CrossRef]
- Sutton, R.T., Pincock, D., Baumgart, D.C. et al. An overview of clinical decision support systems: benefits, risks, and strategies for success. npj Digit. Med. 3, 17 (2020). [CrossRef]
- Biswas, S.S., 2023. Role of chat gpt in public health. Annals of biomedical engineering, 51(5), pp.868-869. [CrossRef]
- Javaid, Mohd, and Abid Haleem. "Virtual reality applications toward medical field." Clinical Epidemiology and Global Health 8.2 (2020): 600-605. [CrossRef]
- LLi, Lan, Fei Yu, Dongquan Shi, Jianping Shi, Zongjun Tian, Jiquan Yang, Xingsong Wang, and Qing Jiang. "Application of virtual reality technology in clinical medicine." American journal of translational research 9, no. 9 (2017): 3867.
- Javaid, M. and Haleem, A., 2019. Industry 4.0 applications in medical field: A brief review. Current Medicine Research and Practice, 9(3), pp.102-109. [CrossRef]
- Coyne, Leanne, Thayer A. Merritt, Brittany L. Parmentier, Rachel A. Sharpton, and Jody K. Takemoto. "The past, present, and future of virtual reality in pharmacy education." American journal of pharmaceutical education 83, no. 3 (2019). [CrossRef]
- Lin, Mike Tz-Yauw, Jau-Shyong Wang, Hui-Ming Kuo, and Yuzhou Luo. "A study on the effect of virtual reality 3D exploratory education on students’ creativity and leadership." Eurasia Journal of Mathematics, Science and Technology Education 13, no. 7 (2017): 3151-3161. [CrossRef]
- Mazurek, Justyna & Kiper, Paweł & Cieślik, Błażej & Rutkowski, Sebastian & Mehlich, Krzysztof & Turolla, Andrea & Szczepańska-Gieracha, Joanna. (2019). Virtual reality in medicine: A brief overview and future research directions. Human Movement. 20. 16-22. [CrossRef]
- Khan, R., Plahouras, J., Johnston, B.C., Scaffidi, M.A., Grover, S.C. and Walsh, C.M., 2018. Virtual reality simulation training for health professions trainees in gastrointestinal endoscopy. Cochrane Database of Systematic Reviews, (8). [CrossRef]
- Bracq, Marie-Stéphanie; Michinov, Estelle; Jannin, Pierre. Virtual Reality Simulation in Nontechnical Skills Training for Healthcare Professionals: A Systematic Review. Simulation in Healthcare: The Journal of the Society for Simulation in Healthcare 14(3):p 188-194, June 2019. https://journals.lww.com/simulationinhealthcare/Fulltext/2019/06000/Virtual_Reality_Simulation_in_Nontechnical_Skills.9.aspx. [CrossRef]
- Ghai S, Ghai I. Virtual reality enhances gait in cerebral palsy: a training dose-response meta-analysis. Frontiers in neurology. 2019 Mar 26;10:236. [CrossRef]
- Subramanian, Sandeep K., Christiane B. Lourenço, Gevorg Chilingaryan, Heidi Sveistrup, and Mindy F. Levin. "Arm motor recovery using a virtual reality intervention in chronic stroke: randomized control trial." Neurorehabilitation and neural repair 27, no. 1 (2013): 13-23. [CrossRef]
- Optale, Gabriele, Cosimo Urgesi, Valentina Busato, Silvia Marin, Lamberto Piron, Konstantinos Priftis, Luciano Gamberini, Salvatore Capodieci, and Adalberto Bordin. "Controlling memory impairment in elderly adults using virtual reality memory training: a randomized controlled pilot study." Neurorehabilitation and neural repair 24, no. 4 (2010): 348-357. [CrossRef]
- Kipping, B., Rodger, S., Miller, K., & Kimble, R. M. (2012). Virtual reality for acute pain reduction in adolescents undergoing burn wound care: a prospective randomized controlled trial. Burns, 38(5), 650-657. [CrossRef]
- Ministry of Health. MOH Launches VR to Help Kids Overcome Fear of Immunization. 3 August 2018. https://www.moh.gov.sa/en/Ministry/MediaCenter/News/Pages/News-2018-08-03-0017.aspx Accessed 5 Aug. 2023.
- Ogilvy. VR Vaccine. https://www.ogilvy.com.br/hermes-1/ Accessed 5 Aug. 2023.
- Chang ZY, Kang GC, Koh EYL, Fong RJK, Tang J, Goh CK, Tan NC. Immersive Virtual Reality in Alleviating Pain and Anxiety in Children During Immunization in Primary Care: A Pilot Randomized Controlled Trial. Front Pediatr. 2022 Mar 25;10:847257. [CrossRef]
- Taddio, A., Ilersich, A., McMurtry, C.M., Bucci, L.M. and MacDonald, N.E., 2021. Foodborne and Animal Contact Disease Outbreaks: Managing pain and fear: Playing your CARDs to improve the vaccination experience. Canada Communicable Disease Report, 47(1), p.87. [CrossRef]
- Mushtaq Ahmed M, PremChander RaoT,Nagaraja G S, Extended Display Mode Using Android Miracast, Proceedings of the International Conference Computational Systems for Health & Sustainability”, pp 84-86, 17-18 April, 2015, Bangalore,Karnatak.
- Annett, M. (1967). The binomial distribution of right, mixed, and left handedness. Quarterly Journal of Experimental Psychology, 19, 327–333. [CrossRef]
- Porac, C., & Coren, S. (1978). Relationships among lateral preference behaviors in human beings. Behavioral and Brain Sciences, 2, 311–312. [CrossRef]
- Çelikol Ş, Tural Büyük E, Yıldızlar O. Children’s Pain, Fear, and Anxiety During Invasive Procedures. Nursing Science Quarterly. 2019;32(3):226-232. [CrossRef]
- Piazza JR, Merkel S, Rothberg B, Gargaro J, Kullgren K. Understanding both sides of the blood draw: The experience of the pediatric patient and the phlebotomist. Patient Experience Journal. 2022; 9(1):35-45. [CrossRef]
- Yuan, S., Hoffman, M., Lu, Q., Goldfinger, D. and Ziman, A. (2011), Motivating factors and deterrents for blood donation among donors at a university campus–based collection center. Transfusion, 51: 2438-2444. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).