1. Introduction
According to the World Health Organization, a preterm birth (PTB) is defined as a live birth occurring between 20+o and 36+6 gestational weeks. An estimated 15 million babies are born prematurely each year worldwide, more than 60% of which occur in Africa and South Asia. Of every 10 babies born, 1 is preterm—and every 40 seconds, 1 of those babies dies. The average preterm birth rate is 12% in low-income countries compared with 9% in high-income countries. Although research efforts on preterm birth have been ongoing, preterm birth rates have remained unchanged over the past decade in every region of the world [
1]. The PTB rate in Vietnam was 9%, ranking Vietnam 21
st in the world in 2014 (UNICEF, 2014). Spontaneous preterm birth accounts for two-thirds of all preterm births, which is still a challenge in obstetric care. This is a major cause of neonatal morbidity and mortality, mostly due to immature respiratory organs, cerebral hemorrhage, and infection, which can lead to long-term neurological deficits such as intellectual impairment, cerebral palsy, chronic lung disease, deafness, and blindness [
2]. The supportive care for these premature babies necessitates a significant cost to families and the healthcare system. Therefore, the effective and safe application of PTB preventive measures are clinically of extreme importance.
Until now, the cervical length (CL) measurement via transvaginal ultrasound in the second trimester has been consistently shown to be a recommended strategy in the prediction of PTB, with the recommendations for the prevention of PTB being the use of micronized progesterone in patients with a short cervix [
3]. Prophylaxis of PTB with micronized progesterone was associated with an approximately 40% reduction in the risk of PTB in singleton pregnancies in mothers with a short cervix [
4]. Another non-invasive method of preventing PTB is using a cervical pessary, with the hypothesis that it narrows the uterocervical angle (UCA), which disperses the impact force from the uterus and the fetus down to the cervix. However, the results of these studies are controversial. A meta-analysis of eight studies in singleton pregnancies with short cervix found that a cervical pessary was not effective in reducing the risk of PTB at <34 weeks (RR = 0.73), <37 weeks (RR = 0.69), and <28 weeks (RR = 0.79) [
5]. Studies published during 2018-2022 about the combination of a cervical pessary with progesterone confirmed the effects of this therapy on pregnancy and neonatal outcomes [
6,
7,
8,
9]. Some studies have shown that combined therapy reduces the rate of PTB compared with progesterone alone [
10,
11], while other studies have reported no effect [
12,
13]. Due to the discrepancy in the results of the aforementioned studies and the hypothesis that a mechanical treatment (cervical pessary) in combination with biochemical treatment (progesterone) would be additionally effective in reducing the incidence of PTB in the group of women with an obtuse uterocervical angle, this study aimed to evaluate the role of the cervical pessary in preventing preterm birth in singleton pregnant women with a short cervical length and an obtuse uterocervical angle measured in the second trimester of pregnancy.
2. Materials and Methods
2.1. Study Design
A quasi-experimental study was conducted from September 2020 to September 2022 at the Haiphong Hospital of Obstetrics and Gynecology, Vietnam.
2.2. Sample Size Calculation
The sample size of this study was estimated using the following formula:
n: number of subjects for each group.
α: significance level.
1 – β: the power of the test.
f (α, ß): reliability. If α = 0.05 and ß = 0.1 then f (α, ß) = 10.5.
Ps (P standard): The success rate of the old method, taking Ps=85.4% based on the PTB rate in the group of pregnant women with a CL ≤25 mm without cervical pessary insertion, is 14.6%, according to a study by Saccone in 2017 [
12].
P
N (P new): The intended success rate of the new method is based on a certain study or pilot study, taking P
N=89.4% based on the rate of PTB in the group of pregnant women with a CL ≤25 mm and inserted pessary being 10.6%, according to the research by Saccone in 2017 [
12].
The minimum calculated sample size for each group is 62 patients.
We scheduled the recruitment of at least 87 patients to each group, with an estimated 40% of patients lost to follow-up.
2.3. Study Population
All singleton pregnant women aged 18-40 years old with a live fetus at the age from 16+o to 23+6 weeks with transvaginal ultrasound CL measurements ≤25 mm managed at the Haiphong Hospital of Obstetrics and Gynecology, Vietnam, from September 2020 to September 2022.
The gestational age is calculated according to the first day of the last menstrual period with a regular cycle (28-30 days) or according to the estimated date of delivery measured via ultrasound in the first trimester if the menstrual period is irregular or the first day of the last period is not known.
The exclusion criteria were as follows: (1) history of preterm birth or miscarriage in the 2nd trimester; (2) history of cervical intervention (LEEP), (3) pregnant women with signs of threatened miscarriage, miscarriage, IUGR, threatened preterm birth, or preterm birth; (4) preterm birth by medical indication; (5) pregnant women with preterm birth prevention by cervical cerclage; (6) non-adherence to progesterone treatment; (7) congenital malformations; and (8) loss to follow-up.
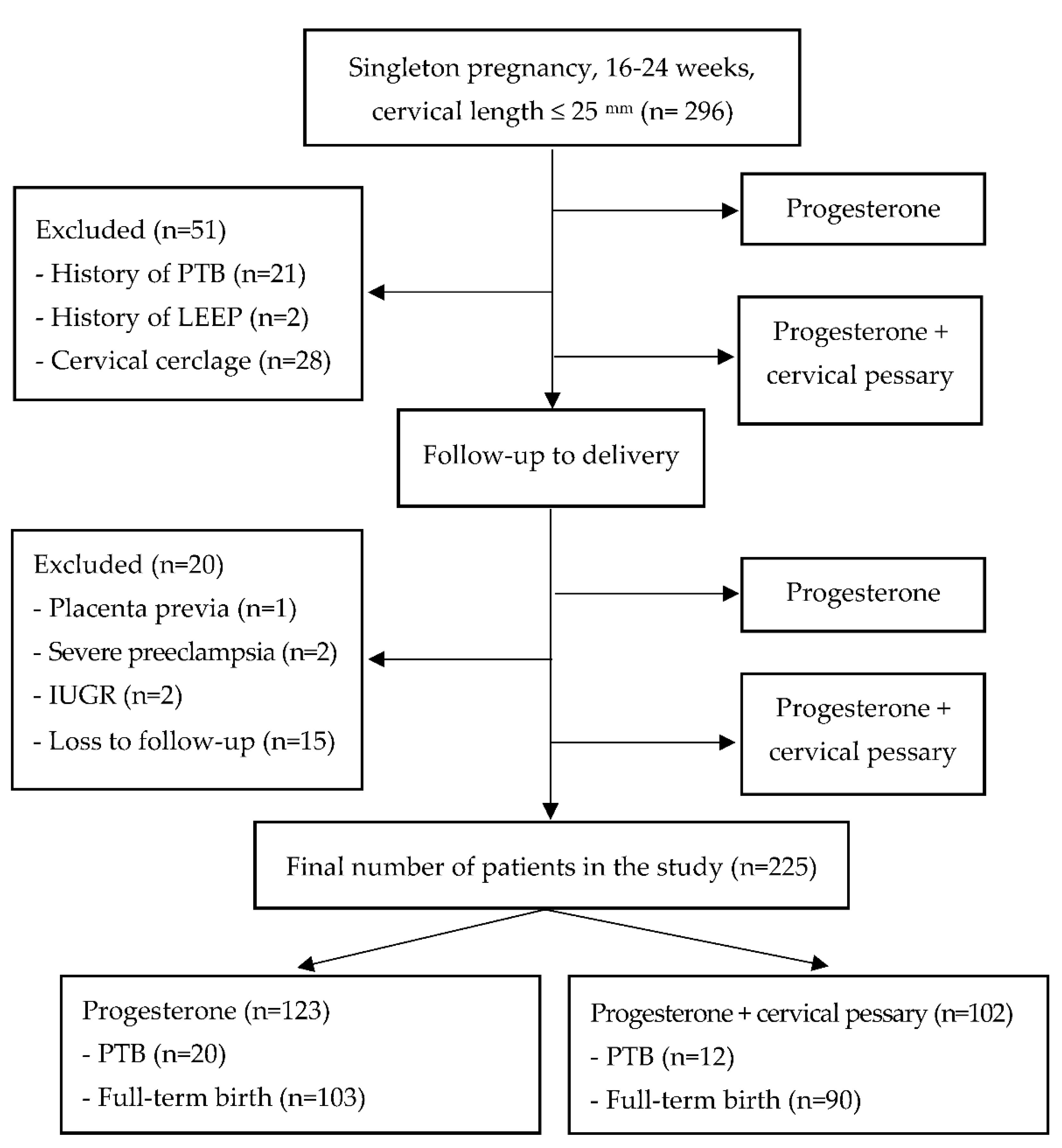
A total of 296 singleton pregnant women with a gestational age from 16
+0 to 23
+6 weeks with transvaginal ultrasound CL measurements ≤25 mm volunteered to participate in the study. Each patient had their CL and UCA measured once at enrollment and intervention and was followed to delivery. After excluding 71 cases with other high-risk factors for preterm birth or loss to follow-up, 225 pregnant women were divided into two groups: prophylaxis treatment with progesterone (123 women) and combined with a cervical pessary (102 pregnant women) (
Figure 1).
2.4. Assessment of Cervical Length and Uterocervical Angle
The CL and UCA measurements were performed by a single sonographer who was certified and monitored by the Maternal Fetal Medicine Foundation.
The ultrasound machines used for measurements were the Samsung Medison WS80A (Korea) and GE Voluson E6 (GE Healthcare Korea) with a transvaginal probe (frequency 4.0-9.0 MHz).
CL measurements were performed following the standard method of The Fetal Medicine Foundation, tracing a single straight line from the internal to external os. Pregnant women with a CL ≤25 mm were considered at risk for spontaneous preterm birth, according to previous studies [
3].
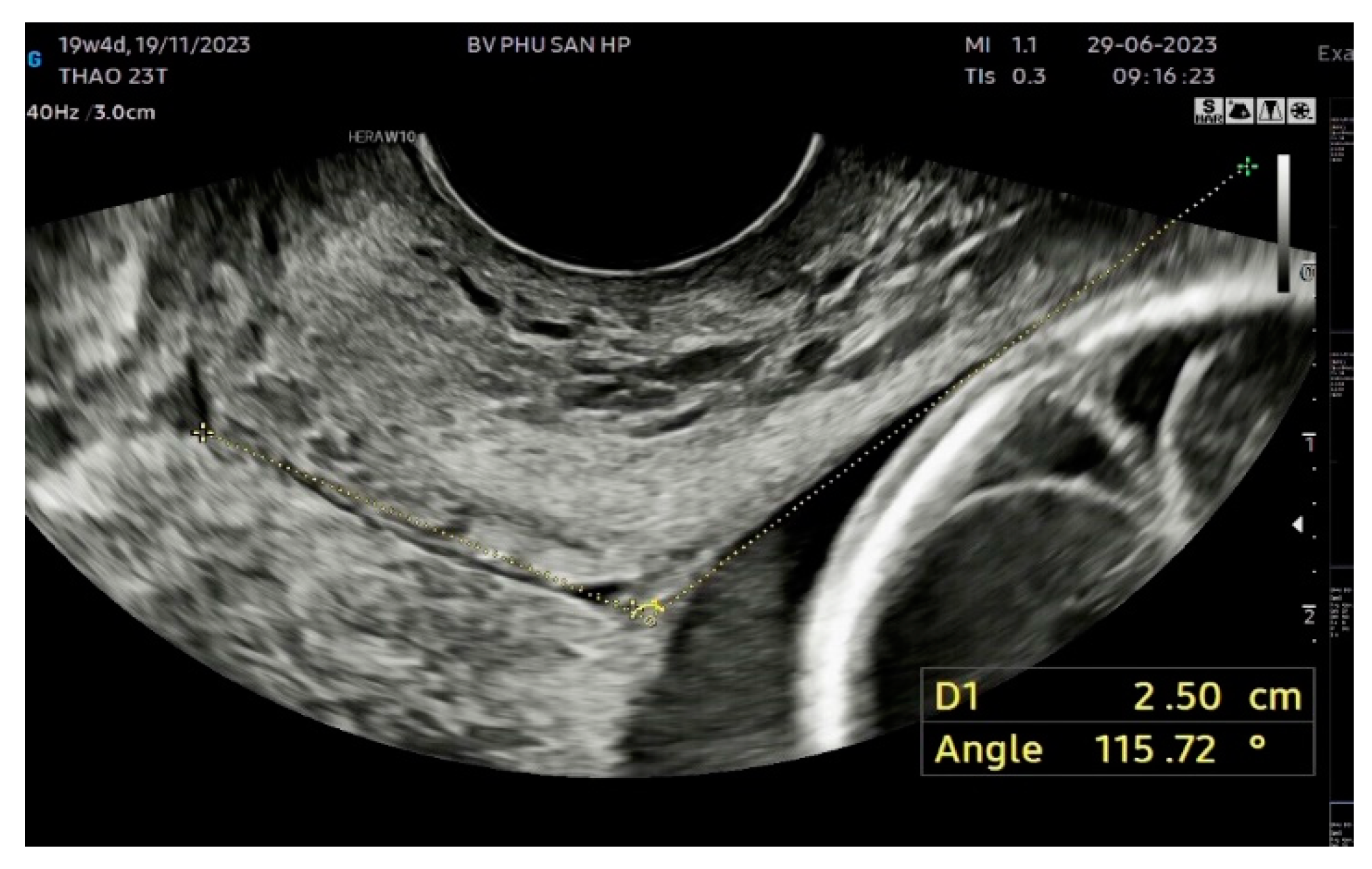
The UCA was measured according to the method described by Dziadosz et al. [
14]. The UCA was calculated as the angle between two lines. The first line was drawn between the internal (I) and external ostium (os) (E). The second line was drawn 3 cm parallel to the lower aspect of the anterior inner uterine wall passing through the end of the first line at the internal os (
Figure 2). Each participant had three images measured to reduce measurement bias, and the most obtuse UCA from the three images was used.
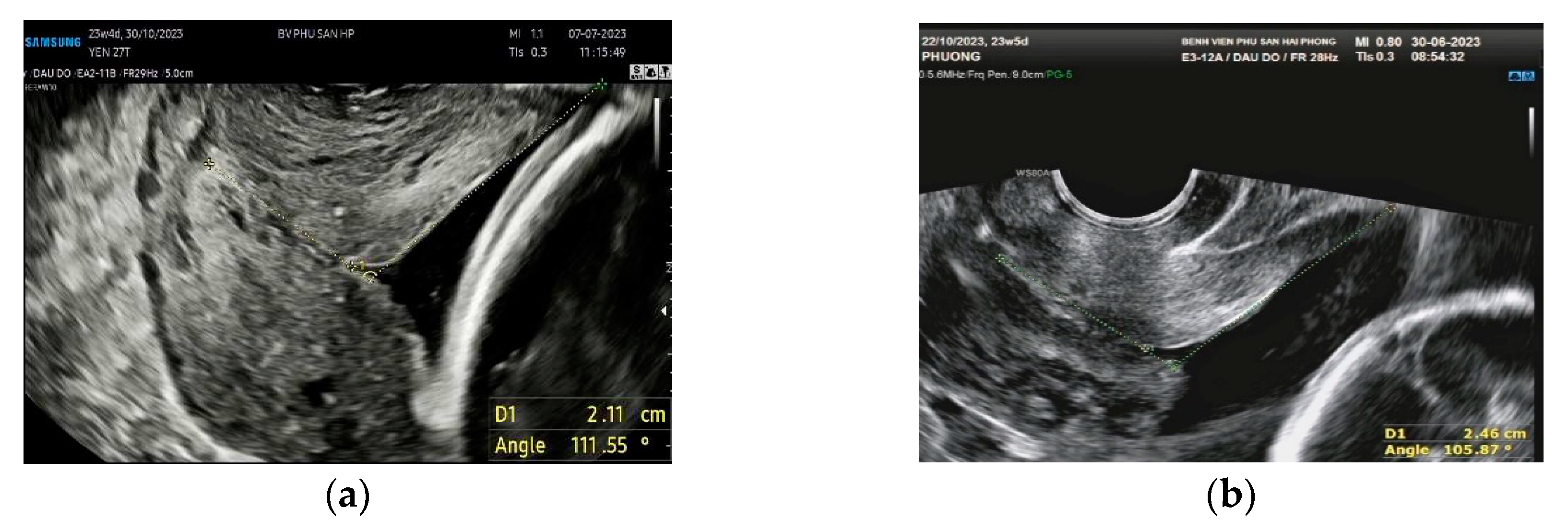
In the case of a funnel-shaped internal os, the first line of the UCA was placed to measure CL, and the second line was drawn from the innermost part of the cervix that can be measured and extended tangentially to the lower anterior inner uterine (
Figure 3).
2.5. Cervical Pessary
The cervical pessary used in our study was Arabin (Dr Arabin GmbH & Co, Witten, Germany) which consists of flexible, comfortable silicone with an outer diameter of 65 mm (for nulliparous women) or 70 mm (for multiparous women), an inner diameter of 32 mm, and a height of 25 mm. Before inserting the Arabin pessary, participants had a gynecological examination and screening for vaginal infection. Bacterial swabs can be used to exclude bacterial colonization. The cervical pessary was placed by two senior physicians of the Department of Pregnancy Management and Prenatal Diagnosis of Haiphong Hospital of Obstetrics and Gynecology in the manner described by Arabin et al. [
15]. The Arabin is folded and inserted vertically into the vagina, applying pressure along the posterior vaginal wall to the posterior vaginal fornix; the inner diameter is directed upwards, and the participant does not feel pain. The pessary is released into the vagina, and the inner diameter is applied directly to the cervix. It is important to make sure the entire cervix is located within the inner diameter by moving the index and middle fingers around the cervix. Press the back edge of the pessary up to the back to help the cervix fold backward. Place the speculum to check again: the inner diameter of the pessary covers the entire cervix, and the participant does not feel pain or strain.
The Arabin pessary was removed at 37 weeks or more in asymptomatic patients or cases of (1) PTB (uterine contractions unresponsive to tocolytics), (2) labor, (3) heavy vaginal bleeding, (4) leaking amniotic fluid/rupture of membranes, (5) feeling of pain or discomfort, or (6) where it was required by the participants.
2.6. Micronized Progesterone
We used Cyclogest manufactured by Actavis UK Limited. Both groups of pregnant women were supported with rectal progesterone at a dose of 200 mg/day every night to the end of 36 gestational weeks or at the onset of labor. Medication adherence was recorded at each routine antenatal visit. In the case of pregnant women with symptoms of threatened preterm birth during pregnancy, they were managed according to the protocol.
2.7. Research Variables
Maternal characteristics; ultrasonographic characteristics; gestational age at birth; preterm birth rates <34 weeks and <37 weeks of gestation; neonatal characteristics and outcomes, including mean birth weight (grams); percentage of low birth weight (<2500 g); NICU admission; death; and adverse neonatal outcome (defined as having at least one of the following disease signs: necrotizing enterocolitis, cerebral hemorrhage, respiratory failure, bronchopulmonary dysplasia, neonatal retinopathy, sepsis, or neonatal mortality) were recorded. Pregnant women giving birth at other hospitals were contacted by phone to collect information about the birth and maternal and neonatal outcomes.
2.8. Study Outcome
The main outcome of this study was preterm birth before 37 and before 34 weeks gestation.
2.9. Statistical Analysis
Categorical variables were described as frequencies (n) and percentages (%), while continuous variables were expressed as mean and standard deviation. The Kolmogorov–Smirnow and Shapiro–Wilk tests were used to assess the normality of variables. The characteristic differences between the group of patients with progesterone treatment and the group of patients with combined treatment of progesterone and cervical pessary were assessed using the Chi-square test and Fisher’s exact test for categorical variables, and T-test and Mann–Whitney U test for continuous variables with normal distribution and non-normal distribution data, respectively. We determined the correlation between CL, UCA, and gestational age at birth and calculated the OR (95% CI) to determine the association between the output variable and the independent variables. A binary regression model was used to assess the association between CL, UCA, and PTB outcomes. They were divided into two groups according to UCA values ≥95
o and ≥105
o for analysis. The role of the cervical pessary on the PTB outcome with different UCA measurements was assessed according to the UCA group. Patients with a UCA ≥95
o and ≥105
o groups were considered at increased risk of PTB <37 weeks and <34 weeks according to the results of previous studies [
14,
16].
The significance level was set to 0.05.
All analyses were performed using SPSS version 26.0 (SPSS, Inc., Chicago, IL).
2.10. Ethical Consideration
The research protocol was approved by the Ethics Committee in Biomedical Research of Hue University of Medicine and Pharmacy, Vietnam (IDH 2020/035), dated 28 February 2020; and the Scientific Council of Hai Phong Obstetrics and Gynecology Hospital, Vietnam (IEC, 1186/QD-BVPSHP), dated 20 August 2020. All pregnant women voluntarily participated in the study and signed a written consent after listening to a full explanation of the research objectives.
3. Results
There were no statistically significant differences in maternal age, maternal BMI, CL, and cervical internal os shape before intervention between the two study groups. However, the mean UCA at intervention was statistically significantly larger in the group with combined treatment of progesterone and cervical pessary (113.02 ± 17.14 mm) than in the group treated with progesterone (89.12 ± 19.25 mm) (p<0.001).
The rate of PTB <37 weeks in the groups with prophylactic treatment via progesterone alone and combined with a cervical pessary were, respectively, 16.3% and 11.8%, and the rate of PTB <34 weeks were 6.5% and 4.9%. There was no statistically significant difference in preterm birth rates <37 weeks and <34 weeks between the two groups (p>0.05).
There was no statistically significant difference in neonatal outcomes in the group treated with progesterone and the group with the combination of progesterone therapy and a cervical pessary (p>0.05).
In the group of patients treated with progesterone, there was a statistically significant relationship between the UCA at intervention and PTB <37 weeks, with an OR (95%CI) of 1.107 (1.047-1.171); as each measure of the UCA increased 1.02 degrees, the probability of PTB <37 weeks increased to 10.7%. Meanwhile, in the group of patients treated with progesterone combined with a cervical pessary, no statistically significant relationship was found between CL, UCA, and outcomes of PTB <37 weeks (p>0.05).
There was a statistically significant relationship between the prophylaxis treatments and PTB <37 weeks in the subgroup of pregnant women with UCA ≥ 95o. The probability of PTB <37 weeks in the group of progesterone treatment combined with cervical pessary decreased by 60.6%, with an OR (95% CI) of 0.394 (0.165-0.941), p<0.05. However, no statistically significant association was found between PTB prophylaxis treatments and outcomes of PTB <34 weeks (p>0.05).
There was a significant association between the group of progesterone treatment combined with a cervical pessary, with the lower rate of PTB <37 weeks with OR (95% CI) of 0.028 (0.005-0.146), p<0.001. Besides that, the patients with combined therapy of progesterone and cervical pessary were associated significantly with a decrease in PTB <34 weeks, with an OR (95% CI) of 0.141 (0.030-0.664), p<0.05.
4. Discussion
Our results on 225 singleton pregnant women at 16
+0 to 23
+6 weeks gestation with a short cervical length showed that the combination of progesterone and cervical pessary did not reduce the risk of PTB <34 weeks (OR = 0.741, 95% CI: 0.235-2.339, p = 0.608) and <37 weeks (OR = 0.687, 95% CI: 0.318-1.482, p=0.337) compared with treatment with progesterone (
Table 2). There was also no statistically significant difference in neonatal outcomes with regard to adverse neonatal outcomes, NICU admission, Apgar scores, and average birth weight (gram) in the two groups (p>0.05,
Table 3).
Table 1.
General characteristics of pregnant women in two study groups (n = 225).
Table 1.
General characteristics of pregnant women in two study groups (n = 225).
| Maternal characteristics |
Progesterone (n = 123) |
Progesterone + cervical pessary (n = 102) |
p |
| Maternal age (X ± SD) (years) |
27.63 ± 5.47 |
27.9 ± 5.54 |
0.717 |
| 27.76 ± 5.49 |
- |
| BMI (X ± SD) (kg/m2) |
23.47 ± 2.68 |
23.33 ± 2.35 |
0.687 |
| 23.41 ± 2.53 |
- |
| Obstetric history |
Nulliparous |
99 (80.5) |
81 (79.4) |
0.841 |
| Multiparous |
24 (19.5) |
21 (20.6) |
| Gestational age at intervention (X ± SD) (weeks) |
20.18 ± 2.46 |
21.03 ± 2.42 |
0.010 |
| 20.56 ± 2.47 |
| Cervical internal os shape at intervention |
Closed |
74 (60.2) |
74 (72.5) |
0.248 |
| T-shaped |
- |
- |
| Y-shaped |
16 (13.0) |
11 (10.8) |
| V-shaped |
17 (13.8) |
9 (8.8) |
| U-shaped |
16 (13.0) |
8 (7.8) |
| Cervical length at intervention (X ± SD) (mm) |
23.75 ± 3.37 |
23.06 ± 3.08 |
0.117 |
| Uterocervical angle at intervention (X ± SD) (mm) |
89.12 ± 19.25 |
113.02 ± 17.14 |
<0.001 |
As shown in
Table 1, there were no statistically significant differences in the general characteristics between the two study groups (p>0.05). However, the UCA measurement at intervention in the group treated with progesterone plus a cervical pessary was 113.02
0 ± 17.14
0, statistically significantly larger than in the group treated with progesterone (p<0.001). This can be explained by the non-randomized sampling method in the study. Pregnant women had the right to choose the method of prevention of PTB with progesterone or progesterone combined with a cervical pessary. Pregnant women with a large UCA were more likely to want to use combination therapy with the aim of reducing the risk of PTB.
Micronized progesterone applications have been shown to effectively reduce the risk of PTB and improve neonatal outcomes in singleton pregnancies with short cervical lengths measured via transvaginal ultrasound in the second trimester [
17] [
18]. Micronized progesterone is also the best PTB prophylactic intervention in singleton pregnancies with a high risk of PTB (previous history of PTB or short cervical length) [
19]. Progesterone is known for its immunomodulatory plus anti-inflammatory effects, which inhibit uterine contractions and prostaglandin production, which are potent uterotonics and promoters of cervical ripening [
20]. Micronized progesterone administration acts on the immune system by increasing the CD4+ ratio, which determines T-cell regulation [
21].
In some pregnancies, micronized progesterone administration alone has likely been shown to effectively reduce the risk of PTB, so that any additional benefits of other preventive interventions, such as a pessary, are barely noticeable. Recent studies comparing the use of progesterone alone versus the combination of progesterone plus a cervical pessary in preventing PTB in singleton pregnancies in women with a short cervical length showed opposite results. A meta-analysis of five RCTs showed that the combination of progesterone and a cervical pessary did not reduce the risk of PTB <28 weeks (RR = 1.54, 95% CI: 0.87-2.74, p = 0.14), <32 weeks (RR = 1.32, 95% CI: 0.89-1.97, p=0.16), <34 weeks (RR = 0.78, 95% CI: 0.46-1.34, p = 0.37), and <37 weeks (RR = 1.09, 95% CI: 0.52-2.27, p = 0.82) in comparison with treatment with progesterone alone. There was also no difference in neonatal outcomes between the two groups (p>0.05) [
22].
In contrast, a meta-analysis of three non-RCT studies found that the combined treatment of progesterone and a cervical pessary was effective in significantly reducing the incidence of PTB <34 weeks (RR = 0.41, 95% CI: 0.24-0.70, p = 0001). However, the CI ranged from 0.14 to 1.18, indicating that no conclusions could be drawn about the results of the above meta-analyses [
22].
A meta-analysis of total RCTs and non-RCTs showed that marginal significance was achieved in reducing the risk of PTB <34 weeks of gestation (RR=0.63, 95% CI: 0.39-101, p=0.05) in the group treated with combined therapy compared with progesterone alone. The CI ranged from 0.31 to 1.30, indicating insufficient evidence to confirm this conclusion [
22].
The binary regression model assessing the association between CL, UCA at invention, and outcomes of PTB <37 weeks illustrated that there was a statistically significant relationship between the UCA at intervention and outcomes of PTB <37 weeks in the group treated with progesterone alone, with OR (95% CI) of 1.107 (1.047-1,171) (p<0.001) for each measure of the UCA increasing 1.02 degrees, and the probability of PTB <37 weeks increased to 10.7%. We did not find a statistically significant relationship between CL, UCA, and outcomes of PTB <37 weeks in the group of patients treated with progesterone combined with a cervical pessary (p>0.05) (
Table 4). The difference in results between the two groups may be that the cervical pessary has partly played a role in narrowing the cervical angle, thereby reducing the rate of PTB in this group of patients.
In recent years, many studies have suggested UCA as a potential ultrasound parameter predicting PTB [
23]. Although there are many complex mechanisms leading to PTB, cervical histological and anatomical variations play a key role in the pathogenesis of preterm birth labor [
24]. The pressure from nearby organs and, more importantly, the growing pregnant uterus can impact the cervical internal os and alter cervical function [
25]. The anatomical integrity of the cervix can be visualized by measuring the CL and UCA. It can be said that an obtuse UCA is associated with a direct force from the pregnant uterus to the cervical internal os, while it is hypothesized that an acute uterocervical angle is associated with less direct force action on this os, which plays a supportive role in maintaining integrity as well as preventing the expansion of the internal os [
15,
26]. In other words, it is hypothesized that the acute cervical angle acts as a barrier to the progression of labor [
27]. Thus, many studies in recent years have evaluated UCA as a potential predictor of PTB. It is measured mainly in the second trimester of pregnancy while measuring cervical length via transvaginal ultrasound.
The results of a systematic review and meta-analysis by Hessami et al. (2021) [
28] included 11 studies involving 5.061 pregnant women (4.511 singleton pregnancies and 550 twins) to understand the relationship between UCA and PTB showed that the value of UCA in pregnancies with PTB was significantly higher than in those with full-term labor (WMD=15.25, 95% CI: 11.78-18.72, p<0.001, I
2=75.9%, p<0.001). Notable results were observed in singleton pregnancy (WMD = 14.43, 95% CI: 8.79- 20.06, p<0.001, I
2 = 82.4%, p<0.001) and twins (WMD = 15.14), 95% CI: 13.42-16.87, p<0.001, I
2 = 0.0%, p=0.464).
In 225 singleton pregnant women with GA from 16
+0 to 23
+6 weeks having CL ≤25 mm, the effectiveness of the cervical pessary in PTB reduction rate was clearly shown in the group of pregnant women with a UCA ≥95
0 and ≥105
0 (
Table 5 and
Table 6).
Dziadosz et al. (2016) [
14] studied 972 singleton pregnant women with a gestational age from 16 to 24 weeks and found that UCA thresholds ≥ 95º and ≥ 105º have a prognostic value of PTB <37 weeks and <34 weeks, with a sensitivity of 80% and 81%, respectively, compared to a sensitivity of 62% and 60% in predicting PTB <37 weeks and <34 weeks with a CTC length ≤25 mm. A recent study by Singh et al. (2022) [
16] on 159 singleton pregnancies with the same weeks gestational showed a higher risk of PTB in pregnant women with a UCA ≥95° and CL ≤25 mm, with a sensitivity and specificity of 86.7%, 93% (p<0.001) and 31.1%, 95.6% (p<0.001), respectively. A UCA is considered a better predictor of PTB ultrasound, with a higher coefficient of variation (56.4%) than CL (16.9%).
It can be explained that if the UCA is obtuse, the gravity of the uterus and the fetus acting on the internal os tend to be along the direction of the cervix, which can lead to shortening of the cervix, and this is one of the factors causing preterm birth. Therefore, the function of a cervical pessary based on this mechanism is not only to support the cervix to evenly distribute the force from the uterus but also to change the UCA from obtuse to acute, changing the force of the uterus to the posterior vaginal fornix to avoid shortening the cervix. This has been proven in the study by Cannie et al. [
29]. They analyzed CL and UCA measurements in two groups of pregnant women: 198 women with no high risk of preterm birth and 73 women with a high risk of preterm birth who had an Arabin pessary at 14 to 33 weeks gestation. The authors performed cervical magnetic resonance imaging before inserting the Arabin pessary and monthly follow-up until the pessary was removed. The results showed that in the group of pregnant women with a low risk of PTB, the UCA measurement did not change, but the CL values decreased significantly with GA (r = -0.15, p<0.05). In the high-risk preterm birth group, 63 patients who delivered after 34 weeks had a mean UCA value that was significantly reduced compared to that before the Arabin pessary was inserted (132° vs. 146°, p<0.01), but it did not change in the 8 patients who delivered before 34 weeks (143° vs. 152°, p>0.05).
This study had two major strengths. First, the quasi-experimental study has a sample size for each analytical group that is specifically calculated, ensuring the representativeness and validity of the research results. Second, the measurement of all uterocervical angles was performed by a single obstetrician to optimize the interobserver variability.
However, the present study had several limitations. First, in the quasi-experimental study with a non-randomized sampling method, the decision to use a cervical pessary was influenced by patient selection, which may lead to classification bias. Second, the present study has not evaluated covariates such as maternal age and gestational age in the association of CL and UCA with PTB; therefore, we cannot rule out the independent role of CL, especially UCA with PTB.