1. Introduction
Multimorbidity is a frequently observed phenomenon among geriatric populations [
1]. Frailty, a condition commonly observed in individuals aged is distinguished by the progressive accumulation of health deficits and impairments in bodily functioning [
2,
3]. These factors are hypothesised to render individuals more susceptible to the deleterious effects of physical stressors. The aforementioned condition is a consequence of the depletion of the physiological reserves within the human body [
2].
Frailty, a condition commonly associated with advanced age, encompasses a range of cognitive and psychological aberrations that have been found to be interconnected with diverse pathological states [
2,
4]. Frailty, in accordance with a recent consensus in the medical field, is a syndrome of medical nature that emerges from a multitude of causes and contributors [
2].
The condition under discussion is distinguished by a gradual reduction in muscular power, stamina, and physiological capacity, consequently heightening an individual's vulnerability to the onset of heightened reliance and/or mortality [
2].
Frailty, a recognised clinical syndrome, has been associated with heightened susceptibility to adverse effects of pharmacotherapy and accelerated symptom progression. Consequently, it has the potential to disrupt the delicate equilibrium between the advantages and disadvantages of various medical interventions [
2]. The necessity for careful consideration of interventions in frail patients is paramount, as such actions may potentially be associated with heightened rates of hospitalisation and institutionalisation. In the context of heightened hospitalisation, there exists a potential peril of escalated patient immobilisation, which may consequently result in the reduction of skeletal muscle mass and subsequent development of various frailty-related complications [
5].
Frailty, a condition encompassing the aspect of chronological age within its definition, emerges as a significantly more accurate gauge of an individual's biological age [
2].
Frailty, a prevalent condition among the elderly population, is frequently distinguished by a combination of muscular weakness and reduced physical speed. In certain cases, frailty may also manifest alongside the presence of lower urinary tract symptoms (LUTS) in elderly women [
6].
The prevalence of frailty, a condition characterised by decreased physiological reserve and increased vulnerability to adverse health outcomes, exhibits considerable variation ranging from 36% to 88% across different assessment methods utilised in research studies [
7].
The assessment of frailty encompasses the utilisation of a wide array of instruments and indicators [
7]. The development of a commonly employed instrument was pioneered by Fried et al. [
7]. The present assessment focuses on the frailty phenotype, which has been derived from the Cardiovascular Health Study [
7]. The present study aims to assess the decline in skeletal muscle mass, alongside various indicators of muscular strength, endurance, balance, ambulatory capacity, and sedentary behaviour [
7]. Frailty, a condition characterised by decreased physiological reserve and increased vulnerability to stressors, can be assessed using various measures. These measures aim to capture different aspects of frailty and provide valuable insights into an individual's health status. Some commonly used measures include the Frailty Index of Accumulative Deficits (FI-CD), the Geriatric 8 score (G8 score), the simplified Five-item Index (sFI), the American Society of Anesthesiologists (ASA) physical status classification, the Mini-Cognitive test (mini-COG), the Clinical Frailty Scale (CFS), the Eastern Cooperative Oncology Group (ECOG) performance status, the Cumulative Illness Score Rating-Geriatrics (CISR-G), the Charlson Comorbidity Index (CCI), the Study of Osteoporotic Fractures (SOF) index, the "Fatigue, Resistance, Ambulation, Illness, Loss of Weight" (FRAIL) index, the Comprehensive Geriatric Assessment (CGA), and the Multidimensional Prognostic Index (MPI). These measures serve as valuable tools in the assessment and management of frailty, aiding healthcare professionals in providing appropriate care and interventions for frail individuals [
8,
9,
10,
11].
Prostate specific antigen, also known as PSA, is a protease that is widely used as a screening tool for the purpose of identifying and monitoring patients who have been diagnosed with prostate adenocarcinoma. The current consensus within the majority of healthcare systems is that the deployment of routine prostate-specific antigen (PSA) testing is not useful in the context of older male populations whose estimated lifespan is less than 15 years. This is the agreement that has been reached. Through the utilisation of gait speed, it is possible to ascertain the estimation of the potential lifespan of an individual. It is important to note that the 10-year survival rate in the male population that is 75 years old or older displays a significant amount of variation. To be more specific, those who have a walking pace of less than 0.4 metres per second (m/s) have a survival percentage of roughly 19% after a period of ten years. In contrast, those who have a walking speed that is greater than 1.4 metres per second have a much better survival percentage of roughly 87% after a period of ten years. In addition, the guidelines established by the European Association of Urology recommend the utilisation of the Geriatric 8 (G8) frailty score for the purpose of assessing the physical condition of persons and determining whether or not conventional treatment methods are appropriate for patients who are frail. The clinical illness known as frailty is characterised by a lower capacity to successfully adapt to and cope with a variety of stressors experienced by the individual. Patients who appear with a G8 score of 14 or lower require more inspection; this can be accomplished through the utilisation of Comprehensive Geriatric Assessment (CGA). The CGA is a thorough evaluation tool that spans various domains and was specifically intended to examine the elderly population that is affected by impairments that cannot be reversed. This fraction of patients is at an increased risk of experiencing mortality as well as problems that are connected with the treatment of cancer [
12].
In the context of elderly individuals aged 75 years and above, the utilisation of prostate-specific antigen (PSA) as a diagnostic tool for prostate cancer is not recommended. Prostate cancer is a prevalent malignancy affecting the prostate gland. However, diagnosing prostate cancer can be challenging, especially in the absence of evident symptoms and a strong suspicion of the disease. In such cases, healthcare professionals face difficulties in accurately identifying and confirming the presence of prostate cancer. In the realm of medical practice, the utilisation of prostate-specific antigen (PSA) holds significant prominence. This particular antigen is extensively employed in the careful monitoring and observation of individuals with disabilities who are undergoing androgen replacement therapy for hypogonadism, a condition characterised by insufficient production of sex hormones. Additionally, PSA is also employed in the context of androgen restriction therapy for individuals with locally progressed and metastatic prostate cancer [
12,
13,
14].
In the realm of utilising prostate-specific antigen (PSA) as a screening tool among the population of frail individuals, as well as investigating the association between PSA levels and the general health status of frail men, this particular review article stands as a pioneering endeavour, to the utmost extent of our current comprehension.
2. Methods
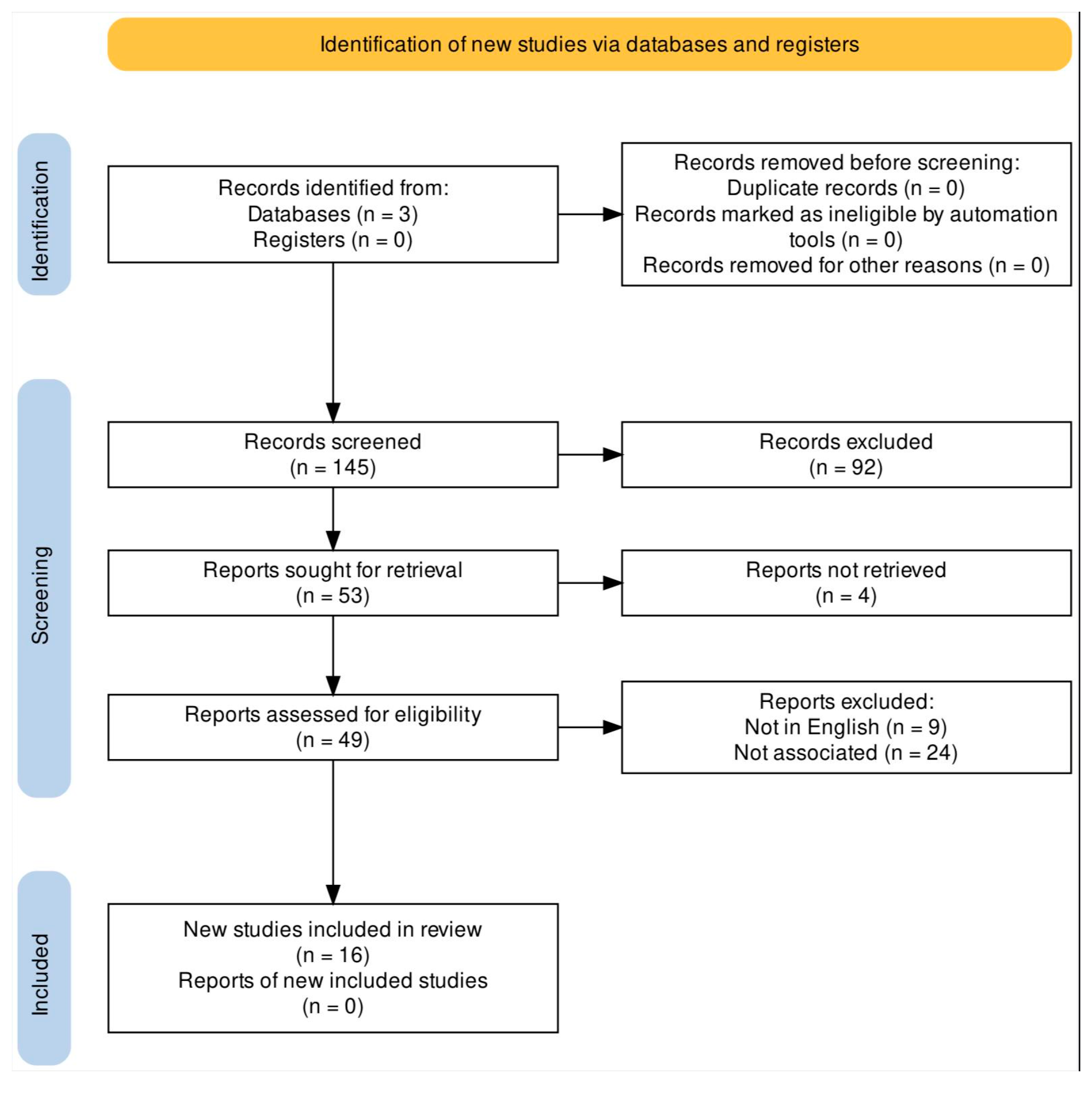
A comprehensive review of the existing literature was conducted, utilising the PubMed, Google Scholar, and Cochrane databases. The objective was to investigate the significance of prostate-specific antigen (PSA) as both a screening and prognostic tool in the context of prostatic ailments, including prostate cancer and benign prostatic obstruction, specifically in the population of frail men. The present study focused on the investigation of various medical aspects, including the prostate-specific antigen (PSA), frailty, prostate cancer screening, hypogonadism, and benign prostatic obstruction. These keywords were utilised to guide the research and analysis conducted in this study. By incorporating these specific terms, we aimed to explore the intricate relationship between these medical factors and their potential implications in the context of human health. The utilisation of these keywords allowed for a comprehensive examination of the subject matter, enabling a more thorough understanding of the various medical phenomena under investigation. The present investigation adhered to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines, which are widely recognised in the medical research community for ensuring transparent and comprehensive reporting of systematic reviews and meta-analyses. This diagram is depicted in
Figure 1. The present study employed a rigorous selection process, wherein studies pertaining to individuals who were not classified as frail or elderly were deliberately excluded. Additionally, studies that did not align with the specific outcomes under investigation in our review were also omitted. Furthermore, studies that were not documented in the English language were not considered for inclusion. Following a meticulous screening process of the studies initially identified, a total of 16 studies have been deemed suitable for inclusion in this comprehensive review. The objectives of this comprehensive analysis were to assess the significance of prostate-specific antigen (PSA) screening in individuals with frailty and the corresponding financial implications for the healthcare sector. Additionally, this study aimed to elucidate the utility of PSA tests in monitoring frail men undergoing treatment for frailty-related hypogonadism, tracking the clinical advancement of benign prostatic obstruction, and managing cases of localised, locally advanced, and metastatic prostate cancer.
3. Results and Discussion- PSA association with frailty
3.1. PSA Screening in Frail Men
Several studies have demonstrated a notable disparity in the utilisation of prostate-specific antigen (PSA) tests among frail individuals residing in European nations, such as Ireland and France. These investigations have revealed a lower likelihood of frail patients undergoing PSA testing compared to their non-frail counterparts. Patients presenting with impaired cognitive function, pre-frailty, diminished grip strength, reduced gait speed, and inadequate levels of physical activity exhibited a decreased likelihood of being recommended routine prostate-specific antigen (PSA) screening. Nevertheless, it has been observed in various studies that individuals presenting with less severe concurrent medical conditions, such as angina, high cholesterol, and hypertension, exhibit a higher propensity towards undergoing prostate-specific antigen (PSA) tests. This inclination may be attributed to their increased frequency of visits to healthcare establishments [
15,
16].
One plausible hypothesis posits that medical practitioners may exhibit a tendency to refrain from conducting prostate-specific antigen (PSA) tests in individuals with exceedingly compromised health statuses. However, it is postulated that these same healthcare professionals may still opt to screen patients with less severe ailments, who do not exhibit signs of frailty. In addition, it has been observed that individuals in the middle age bracket who exhibit pronounced frailty and suffer from chronic ailments are comparatively less inclined to undergo prostate-specific antigen (PSA) testing for the detection of prostate cancer [
15,
16].
Contrary to prevailing notions, a comprehensive cohort study encompassing a substantial population of over five hundred thousand veterans aged 70 years or older residing in the United States of America has yielded intriguing findings. Notably, it has been observed that individuals of the male gender exhibiting suboptimal health status and frailty were subjected to medical evaluations with comparable frequency, and in certain age brackets, even more so than their younger counterparts within the v In the geriatric population of veterans aged 85 years and above, the utilisation of prostate-specific antigen (PSA) screening, a diagnostic tool for prostate cancer, exhibited varying rates based on the individuals' health status. Among men with good health, the prevalence of PSA screening was recorded at 34%, whereas for those with poorer health conditions, the rate escalated to 36% [
17].
A recent study conducted among male individuals aged 75 years and above has shed light on the utilisation of prostate-specific antigen (PSA) tests in the context of frailty. Surprisingly, the findings indicate that frail patients exhibited a significantly lower likelihood of undergoing PSA tests compared to their healthy counterparts within the same age group. In a recent study, it was observed that among individuals with a projected lifespan exceeding ten years, approximately 65% of men underwent prostate-specific antigen (PSA) tests. Conversely, their counterparts who exhibited frailty were found to have a lower rate of recent screening, with only 42% undergoing such tests. The research findings indicate that there remains a notable prevalence of PSA testing among individuals classified as highly frail, thereby contributing to the economic strain on the healthcare system [
14].
A recent investigation employed a frailty model to substantiate the notion that prostate-specific antigen (PSA) testing has resulted in the identification of prostate cancer at a younger age and a greater proportion among vulnerable individuals, particularly those with a familial predisposition to this malignancy [
18].
The consensus among various studies generally aligns with the recommended threshold proposed by the European Association of Urology guidelines pertaining to the screening of prostate cancer. Therefore, the utilisation of prostate-specific antigen (PSA) tests for screening purposes should be contingent upon not solely the chronological age of male individuals, but predominantly on their projected lifespan and functional capacity. Frail individuals with a projected lifespan of fewer than 15 years exhibit limited potential for reaping advantages from routine prostate-specific antigen (PSA) screenings [
12].
3.2. PSA Levels and Health Status of Frail Patients
The association between levels of prostate-specific antigen (PSA) and increasing age has been unequivocally established within the medical field. The observed phenomenon can be primarily ascribed to the physiological phenomenon of benign prostatic hyperplasia (BPH), which is characterised by the natural enlargement of the prostate gland that occurs as males advance in age. Diverse ethnic backgrounds have been associated with observed variations in levels of prostate-specific antigen (PSA) among men. The potential influence of comorbidities, including benign prostatic hyperplasia and urinary tract infections, on the results of prostate-specific antigen (PSA) screening in frail patients is a matter of concern. Elevated concentrations of prostate-specific antigen (PSA) in the male population may serve as a potential indicator of more pronounced benign prostatic enlargement (BPE) and heightened lower urinary tract symptoms (LUTS), consequently posing a potential threat to their overall quality of life [
12,
19,
20].
The assessment of prostate-specific antigen (PSA) levels has emerged as a significant diagnostic measure in the evaluation of Benign Prostatic Obstruction (BPO). This method has demonstrated its efficacy in predicting the clinical advancement of BPO, as well as determining the likelihood of acute urinary retention and the subsequent requirement for BPO-related surgical interventions. Patients presenting with more pronounced clinical manifestations related to benign prostatic obstruction (BPO) frequently demonstrate heightened levels of prostate-specific antigen (PSA) and augmented prostate volumes [
19]. Frail males presenting with benign prostatic obstruction (BPO) and heightened residual urine volumes are predisposed to recurrent urinary tract infections (UTIs). Urinary tract infections (UTIs) have the potential to cause an elevation in prostate-specific antigen (PSA) levels. Therefore, it is crucial to ensure proper management of any existing infections before performing a prostate-specific antigen (PSA) test in order to obtain precise and reliable outcomes [
19].
The association between age and prostate-specific antigen (PSA) concentrations has been extensively documented in the medical literature. Nevertheless, the potential influence of frailty on prostate-specific antigen (PSA) levels remains largely unexplored, with a dearth of empirical data supporting a definitive correlation between frailty and PSA levels. Hypogonadism, a commonly observed medical condition in the geriatric male population, exerts a substantial influence on the overall health and welfare of affected individuals. The administration of Testosterone therapy has demonstrated promising results in the improvement of the overall quality of life among individuals who are frail. Recent studies have extensively documented the well-established efficacy of testosterone in augmenting grip strength and elevating haemoglobin levels [
21]. Nevertheless, it is crucial to exercise prudence when employing this therapeutic intervention owing to its association with elevated cardiovascular risks and abnormal hematocrit values. Moreover, it is imperative to acknowledge that this particular intervention is contraindicated in male individuals manifesting indications of progressive prostate cancer.
Henceforth, it becomes crucial to meticulously observe the levels of prostate-specific antigen (PSA) in debilitated males who are undergoing testosterone therapy for the condition of hypogonadism [
22]. In contrast to initial expectations, it has been determined that prostate-specific antigen (PSA) lacks the necessary level of reliability as a clinical indicator for male hypogonadism [
23]. The significance of recognising the utilisation of testosterone as a therapeutic measure for hypogonadism in individuals with frailty lies in the lack of substantial evidence indicating its effect on prostate-specific antigen (PSA) levels. Moreover, it has been observed that the beneficial outcomes associated with testosterone intervention, such as enhancements in muscular strength, lean body mass, and overall well-being among debilitated males, exhibit a transient nature and cease to exist beyond a duration of six months subsequent to the termination of testosterone treatment [
21,
24].
The application of testosterone replacement therapy has demonstrated potential benefits for individuals suffering from hypogonadism and frailty, particularly those with obesity, when used in conjunction with lifestyle intervention. The aforementioned therapeutic modality has exhibited efficacy in augmenting sexual well-being and optimising cardiovascular endurance. Furthermore, it has been noted that this intervention exhibits the ability to attenuate muscle atrophy while maintaining prostate-specific antigen (PSA) levels within acceptable ranges [
25].
Human chorionic gonadotropin (hCG) has emerged as a promising therapeutic intervention for the management of androgen deficiency in elderly males. The utilisation of hCG has shown potential in addressing this condition, which is characterised by a decrease in androgen levels in ageing men. By exploring the application of hCG, researchers aim to develop effective strategies for addressing androgen deficiency in this specific population. The hormone in question has been discovered to possess the capacity to enhance the concentrations of testosterone, estradiol, and diverse testicular steroids in the human body. In a recent study, it was found that a three-month treatment regimen did not have any effect on prostate-specific antigen (PSA) levels. However, the results regarding muscle strength and physical functioning did not show any significant improvements [
26].
The measurement of prostate-specific antigen (PSA) levels is widely utilised within the medical community as a means to evaluate the effectiveness of Androgen Deprivation treatment (ADT) in the management of metastatic prostate cancer among elderly patients [
13]. PSA surveillance has been utilised in multiple research endeavours to assess the effectiveness of emerging hormonal treatments, such as Abiraterone acetate, in cohorts of elderly males who exhibit frailty. The clinical effectiveness of abiraterone acetate has been established through an observational study conducted on a group of elderly individuals in their eighties who exhibit frailty and have previously received docetaxel therapy for the management of metastatic castration-resistant prostate cancer. The clinical study findings have unveiled encouraging clinical outcomes, demonstrating an observed prostate-specific antigen (PSA) response rate of approximately 50% within this specific patient cohort. The present study conducted a comparative analysis to assess the levels of toxicity across various age groups, with a specific focus on the elderly population. The findings of this investigation indicated that there was no statistically significant increase in toxicity among older individuals when compared to younger age groups [
27].
3.3. Cost-Effectiveness of PSA Tests in Frail Individuals
The absence of apparent advantageous outcomes associated with prostate-specific antigen (PSA) screening among males with a predicted lifespan of less than 15 years has been definitively ascertained [
12]. The establishment of this threshold is primarily dictated by the performance status and frailty of individuals, with age being just one factor among many. The utilisation of prostate-specific antigen (PSA) tests in frail individuals has not shown any discernible survival benefit. Furthermore, studies have revealed that the adoption of screening protocols for males aged 70 and older significantly amplifies the economic strain on the healthcare system. In accordance with recent research findings, it has been observed that a significant surge of 5 percentage points in screening rates corresponds to a noteworthy 13.8% escalation in the financial burden imposed on the healthcare system [
28].
In a recent study conducted to assess cost-utility, it has been observed that the utilisation of routine prostate-specific antigen (PSA) tests imposes a considerable economic burden on healthcare systems. Consequently, it is strongly advised that a paradigmatic alteration takes place, whereby an inaugural prostate-specific antigen (PSA) examination is performed upon reaching the age of 50. Subsequent diagnostic evaluations ought to be exclusively allocated to individuals who manifest clinical manifestations suggestive of prostate cancer [
29]. In the population of geriatric males aged 70 years or older, the utilisation of prostate-specific antigen (PSA) tests has been observed to demonstrate a significant association with excessive financial expenditures. The financial burdens associated with these expenditures primarily arise from the necessity of expensive follow-up procedures, such as various imaging modalities, along with therapeutic interventions aimed at attaining curative results [
30]. Henceforth, the execution of a tactical approach aimed at diminishing the utilisation of prostate-specific antigen (PSA) examinations in frail individuals, who are unlikely to experience any therapeutic advantages from curative measures for prostate cancer, exhibits the capacity to curtail healthcare costs while simultaneously augmenting the general welfare of elderly and frail cohorts.
3.4. Prostate- specific antigen and Sarcopenia
Androgen deprivation therapy (ADT) is a well-established treatment option for men with metastatic prostate cancer. However, ADT causes excessive muscle loss and Sarcopenia, because of the decrease of testosterone. Ten times more lean body mass is lost from ADT in comparison to normal aging every year of treatment. [
31] A randomized controlled trial involved men with prostate cancer receiving ADT who were either given 40mg of crystalline oral testosterone or placebo. Low dose liver-targeted testosterone therapy (LTTT) was found to increase the whole body protein anabolism without increasing peripheral testosterone. PSA was regularly measured in these patients and they were withdrawn from receiving LTTT if the PSA concentration rose by more than 50% or to more than 4 ng/mL at any time during the follow-up. Thus close monitoring of PSA can be utilized for safely treating muscle and bone loss in men with prostate cancer on treatment with ADT.
The potential benefits of LTTT as an intervention to counteract the negative impacts of androgen deprivation therapy (ADT) on muscle and bone mass have been recognized. LTTT has exhibited the capacity to significantly impede the deterioration of muscle and bone mass, while not concurrently inducing an increase in testosterone levels in the peripheral blood. The aforementioned discovery indicates that LTTT may present a favorable pathway for the maintenance of musculoskeletal well-being in individuals undergoing Androgen Deprivation Therapy (ADT). The average levels of prostate-specific antigen (PSA) exhibited a consistent and stable pattern during the entire duration of this therapeutic intervention, without any notable observed effects. The discontinuation of treatment by a minority of participants is a noteworthy observation, albeit with the caveat that their prostate-specific antigen (PSA) levels returned to baseline values. Additional investigations are warranted to determine the optimal dosage of LTTT, as indicated in previous scholarly inquiry [
31].
Sarcopenia has also been discovered to be a negative prognostic factor for PSA progression in men with metastatic hormone sensitive prostate cancer (mHSPC), who receive early docetaxel or abiraterone acetate treatment. [
32] In a retrospective study, in which sarcopenia was defined as a skeletal muscle index of ≤52.4 cm
2/m
2, patients with mHSPC and sarcopenia had shorter time to PSA progression (median, 20.7 months vs. not reached; log-rank
p < 0.001) than those without sarcopenia. [
32]
Similarly sarcopenia was significantly associated with earlier PSA progression in patients with metastatic castrate-resistant prostate cancer (mCRPC). This was shown in a secondary analysis of a prospective observational study of men with mCRPC and sarcopenia. Patients were considered sarcopenic if they met the following two criteria: a) muscle weakness (<35.5kg) through grip strength and slowness (<0.8m/s) through gait speed per the Sarcopenia Definitions and Outcomes Consortium (SDOC) and b) low muscle mass or low muscle quality at the level of the 3rd lumbar vertebra in CT scans. [
33]
The median time to PSA progression was significantly shorter for sarcopenic men in comparison to non-sarcopenic participants (4 months and 17 months, respectively (p<0.001)). Sarcopenia was significantly associated with PSA progression in the univariate analysis (HR = 2.77, 95%CI = 1.54–4.98, p<0.001) and although this association was also evident in the multivariable analysis (HR = 1.77, 95%CI = 0.91–3.48, p = 0.095), it was no longer significant which was hypothesized to be caused by the small number of participants. [
33]
4. Conclusion
The utilisation of Prostate Specific Antigen (PSA) has become increasingly recognised as a valuable tool in both screening and prognostic evaluation of male frailty. PSA is a protein produced by the cells of the prostate gland, and its levels in the blood can provide important insights into the health status of the prostate. The screening aspect of PSA involves measuring its concentration in the blood to detect any abnormalities that may indicate the presence of prostate conditions, such as prostate cancer or benign prostatic hyperplasia (BPH). By monitoring PSA levels, healthcare professionals can identify potential issues at an early stage, allowing for timely intervention and improved patient outcomes. In addition to screening, PSA also serves as a prognostic modality, providing valuable information about the severity and progression of prostate-related conditions. Elevated PSA levels can indicate a higher risk The utilisation of this particular method holds great promise in the realm of medical diagnostics, specifically in the timely detection of prostate cancer. This method is particularly beneficial for individuals who may be categorised as frail and have a life expectancy that surpasses a notable 15-year threshold. Prostate cancer, a prevalent malignancy affecting the male population, is a significant health concern worldwide. Early detection plays a crucial role in improving patient outcomes and The utilisation of this particular approach has the potential to provide valuable assistance in the initiation of optimal therapeutic interventions for males who are debilitated and suffering from metastatic prostate cancer. Metastatic prostate cancer refers to the spread of cancerous cells from the prostate gland to other parts of the body. This advanced stage of the disease often leads to significant physical and functional impairments in affected individuals. The approach being discussed here involves a comprehensive assessment of the patient's condition, taking into account various factors such as the extent of cancer spread, the overall health status of the individual, and the presence of any other underlying medical conditions. By considering these factors, healthcare professionals can gain a better understanding of the unique needs and challenges faced by debilitated males with metastatic prostate cancer. Once a thorough assessment has been conducted, the gathered information can be used to guide the selection and implementation of appropriate therapeutic interventions. These interventions may include a combination of treatments such as chemotherapy, radiation therapy, hormone therapy, and In addition, it is worth noting that testosterone therapy plays a crucial role in monitoring and managing the health of frail males who are suffering from hypogonadism, a condition characterised by low testosterone levels. This therapy is especially important for individuals with a history of prostate cancer, as their medical background requires careful consideration and monitoring. Testosterone therapy is a medical intervention that aims to restore and maintain optimal testosterone levels in individuals with hypogonadism. This condition can lead to a variety of symptoms, including decreased energy levels, reduced muscle mass, diminished libido, and mood disturbances. By administering testosterone, healthcare professionals can effectively address these symptoms and improve the overall well-being of patients. However, when it comes to frail males with a previous medical record of prostate cancer, additional caution must be exercised. Prostate cancer is a common malignancy in males, and its treatment often involves reducing testosterone levels to prevent cancer growth. Therefore, the use of testosterone therapy in individuals with a history of prostate cancer requires careful consideration and close monitoring to ensure that it does not exacerbate or promote. The assessment of frailty plays a pivotal role in the assessment of the suitability of prostate-specific antigen (PSA) tests for individuals who have concurrent medical conditions, with the ultimate objective of alleviating the financial burden on the healthcare system.
Author contributions
A single author N.K. decided the article's topic. One other author independently T.B. checked and two others (S.K., E.M.) rechecked the articles. A fourth author (A.P.) resolved conflicts. All authors checked and corrected the final draught.
Funding
No funding sources.
Data availability
All available in searched databases.
Acknowledgements
No acknowledgements.
Conflicts of Interest
No conflict of interest to declare.
References
- Dartigues JF, Le Bourdonnec K, Tabue-Teguo M, Le Goff M, Helmer C, Avila-Funes JA, Coureau G, Feart C, Pérès K, Genuer R, Letenneur L, Amieva H, Proust-Lima C. Co-Occurrence of Geriatric Syndromes and Diseases in the General Population: Assessment of the Dimensions of Aging. J Nutr Health Aging. 2022;26(1):37-45. PMID: 35067701; PMCID: PMC8720645. [CrossRef]
- Bauer SR, Walter LC, Ensrud KE, Suskind AM, Newman JC, Ricke WA, Liu TT, McVary KT, Covinsky K. Assessment of Frailty and Association With Progression of Benign Prostatic Hyperplasia Symptoms and Serious Adverse Events Among Men Using Drug Therapy. JAMA Netw Open. 2021 Nov 1;4(11):e2134427. PMID: 34817584; PMCID: PMC8613596. [CrossRef]
- Bellos TC, Tzelves LI, Manolitsis IS, Katsimperis SN, Berdempes MV, Skolarikos A, Karakousis ND. Sarcopenia in Urinary Bladder Cancer: Definition, Prevalence and Prognostic Value in Survival. Maedica (Bucur). 2022 Jun;17(2):427-435. PMID: 36032591; PMCID: PMC9375863. [CrossRef]
- Bellos TC, Tzelves LI, Manolitsis IS, Katsimperis SN, Berdempes MV, Skolarikos A, Karakousis ND. Frailty and benign prostatic hyperplasia: The thrilling underlying impact. Arch Ital Urol Androl. 2022 Sep 27;94(3):345-349. PMID: 36165483. [CrossRef]
- Kostakopoulos NA, Karakousis ND. Frailty assessment and postoperative complications in urologic oncology operations. J Frailty Sarcopenia Falls. 2020 Sep 1;5(3):57-61. PMID: 32885102; PMCID: PMC7461351. [CrossRef]
- Bauer SR, Jin C, Kamal P, Suskind AM. Association Between Lower Urinary Tract Symptoms and Frailty in Older Men Presenting for Urologic Care. Urology. 2021 Feb;148:230-234. Epub 2020 Oct 10. PMID: 33049232; PMCID: PMC7870540. [CrossRef]
- Suskind AM. Frailty and Lower Urinary Tract Symptoms. Curr Urol Rep. 2017 Sep;18(9):67. PMID: 28718161; PMCID: PMC6677257. [CrossRef]
- Pyrgioti EE, Karakousis ND. B12 levels and frailty syndrome. J Frailty Sarcopenia Falls. 2022 Mar 1;7(1):32-37. PMID: 35291574; PMCID: PMC8886776. [CrossRef]
- Kostakopoulos NA, Karakousis ND. Frailty assessment and postoperative complications in urologic oncology operations. J Frailty Sarcopenia Falls. 2020 Sep 1;5(3):57-61. PMID: 32885102; PMCID: PMC7461351. [CrossRef]
- Pilotto A, Custodero C, Maggi S, Polidori MC, Veronese N, Ferrucci L. A multidimensional approach to frailty in older people. Ageing Res Rev. 2020 Jul;60:101047. Epub 2020 Mar 21. PMID: 32171786; PMCID: PMC7461697. [CrossRef]
- Dent E, Kowal P, Hoogendijk EO. Frailty measurement in research and clinical practice: A review. Eur J Intern Med. 2016 Jun;31:3-10. Epub 2016 Mar 31. PMID: 27039014. [CrossRef]
- Mottet N, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, Fanti S, Fossati N, Gandaglia G, Gillessen S, Grivas N, Grummet J, Henry AM, van der Kwast TH, Lam TB, Lardas M, Liew M, Mason MD, Moris L, Oprea-Lager DE, van der Poel HG, Rouvière O, Schoots IG, Tilki D, Wiegel T, Willemse PM, Cornford P. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer-2020 Update. Part 1: Screening, Diagnosis, and Local Treatment with Curative Intent. Eur Urol. 2021 Feb;79(2):243-262. Epub 2020 Nov 7. PMID: 33172724. [CrossRef]
- Cornford P, van den Bergh RCN, Briers E, Van den Broeck T, Cumberbatch MG, De Santis M, Fanti S, Fossati N, Gandaglia G, Gillessen S, Grivas N, Grummet J, Henry AM, der Kwast THV, Lam TB, Lardas M, Liew M, Mason MD, Moris L, Oprea-Lager DE, der Poel HGV, Rouvière O, Schoots IG, Tilki D, Wiegel T, Willemse PM, Mottet N. EAU-EANM-ESTRO-ESUR-SIOG Guidelines on Prostate Cancer. Part II-2020 Update: Treatment of Relapsing and Metastatic Prostate Cancer. Eur Urol. 2021 Feb;79(2):263-282. Epub 2020 Oct 7. PMID: 33039206. [CrossRef]
- Hoffman KE, Nguyen PL, Ng AK, D'Amico AV. Prostate cancer screening in men 75 years old or older: an assessment of self-reported health status and life expectancy. J Urol. 2010 May;183(5):1798-802. Epub 2010 Mar 17. PMID: 20299039. [CrossRef]
- Flahavan EM, Drummond FJ, Bennett K, Barron TI, Sharp L. Prostate specific antigen testing is associated with men's psychological and physical health and their healthcare utilisation in a nationally representative sample: a cross-sectional study. BMC Fam Pract. 2014 Jun 17;15:121. PMID: 24938184; PMCID: PMC4065544. [CrossRef]
- Rat C, Schmeltz H, Rocher S, Nanin F, Gaultier A, Nguyen JM. Factors Related to Prostate-Specific Antigen-Based Prostate Cancer Screening in Primary Care: Retrospective Cohort Study of 120,587 French Men Over the Age of 50 Years. JMIR Public Health Surveill. 2018 Oct 23;4(4):e10352. PMID: 30355559; PMCID: PMC6231884. [CrossRef]
- Walter LC, Bertenthal D, Lindquist K, Konety BR. PSA screening among elderly men with limited life expectancies. JAMA. 2006 Nov 15;296(19):2336-42. PMID: 17105796. [CrossRef]
- Valberg M, Grotmol T, Tretli S, Veierød MB, Moger TA, Devesa SS, Aalen OO. Prostate-specific antigen testing for prostate cancer: Depleting a limited pool of susceptible individuals? Eur J Epidemiol. 2017 Jun;32(6):511-520. Epub 2016 Jul 18. PMID: 27431530; PMCID: PMC5468491. [CrossRef]
- Gravas S., et al. EAU Guidelines on Management of Non-Neurogenic Male Lower Urinary Tract Symptoms (LUTS) in: EAU Guidelines, edition presented at the annual EAU Congress 2022 Amsterdam, 2022. ISBN 978-94-92671-16-5.
- Litchfield MJ, Cumming RG, Smith DP, Naganathan V, Le Couteur DG, Waite LM, Blyth FM, Handelsman DJ. Prostate-specific antigen levels in men aged 70 years and over: findings from the CHAMP study. Med J Aust. 2012 Apr 2;196(6):395-8. PMID: 22471541. [CrossRef]
- Sih R, Morley JE, Kaiser FE, Perry HM 3rd, Patrick P, Ross C. Testosterone replacement in older hypogonadal men: a 12-month randomized controlled trial. J Clin Endocrinol Metab. 1997 Jun;82(6):1661-7. PMID: 9177359. [CrossRef]
- Dohle, G.R. Et al. EAU Guidelines Panel on Male Hypogonadism, Edn. Presented at the EAU Annual Congress Paris 2012: Arnhem, the Netherlands.
- Glina S. Is serum PSA a predictor of male hypogonadism? Arch Endocrinol Metab. 2021 Apr 5;65(2):124-125. PMID: 33826838; PMCID: PMC10065319. [CrossRef]
- O'Connell MD, Roberts SA, Srinivas-Shankar U, Tajar A, Connolly MJ, Adams JE, Oldham JA, Wu FC. Do the effects of testosterone on muscle strength, physical function, body composition, and quality of life persist six months after treatment in intermediate-frail and frail elderly men? J Clin Endocrinol Metab. 2011 Feb;96(2):454-8. Epub 2010 Nov 17. PMID: 21084399. [CrossRef]
- Barnouin Y, Armamento-Villareal R, Celli A, Jiang B, Paudyal A, Nambi V, Bryant MS, Marcelli M, Garcia JM, Qualls C, Villareal DT. Testosterone Replacement Therapy Added to Intensive Lifestyle Intervention in Older Men With Obesity and Hypogonadism. J Clin Endocrinol Metab. 2021 Mar 8;106(3):e1096-e1110. PMID: 33351921. [CrossRef]
- Liu PY, Wishart SM, Handelsman DJ. A double-blind, placebo-controlled, randomized clinical trial of recombinant human chorionic gonadotropin on muscle strength and physical function and activity in older men with partial age-related androgen deficiency. J Clin Endocrinol Metab. 2002 Jul;87(7):3125-35. PMID: 12107212. [CrossRef]
- Maines F, Caffo O, De Giorgi U, Fratino L, Lo Re G, Zagonel V, D'Angelo A, Donini M, Verderame F, Ratta R, Procopio G, Campadelli E, Massari F, Gasparro D, Ermacora P, Messina C, Giordano M, Alesini D, Basso U, Fraccon AP, Vicario G, Conteduca V, Galligioni E. Safety and Clinical Outcomes of Abiraterone Acetate After Docetaxel in Octogenarians With Metastatic Castration-Resistant Prostate Cancer: Results of the Italian Compassionate Use Named Patient Programme. Clin Genitourin Cancer. 2016 Feb;14(1):48-55. Epub 2015 Aug 6. PMID: 26382222. [CrossRef]
- Rao K, Liang S, Cardamone M, Joshu CE, Marmen K, Bhavsar N, Nelson WG, Ballentine Carter H, Albert MC, Platz EA, Pollack CE. Cost implications of PSA screening differ by age. BMC Urol. 2018 May 9;18(1):38. PMID: 29743049; PMCID: PMC5944051. [CrossRef]
- Keeney E, Sanghera S, Martin RM, Gulati R, Wiklund F, Walsh EI, Donovan JL, Hamdy F, Neal DE, Lane JA, Turner EL, Thom H, Clements MS. Cost-Effectiveness Analysis of Prostate Cancer Screening in the UK: A Decision Model Analysis Based on the CAP Trial. Pharmacoeconomics. 2022 Dec;40(12):1207-1220. [CrossRef]
- Kim DD, Daly AT, Koethe BC, Fendrick AM, Ollendorf DA, Wong JB, Neumann PJ. Low-Value Prostate-Specific Antigen Test for Prostate Cancer Screening and Subsequent Health Care Utilization and Spending. JAMA Netw Open. 2022 Nov 1;5(11):e2243449. PMID: 36413364; PMCID: PMC9682424. [CrossRef]
- Rhee H, Navaratnam A, Oleinikova I, Gilroy D, Scuderi Y, Heathcote P, Nguyen T, Wood S, Ho KKY. A Novel Liver-targeted Testosterone Therapy for Sarcopenia in Androgen Deprived Men With Prostate Cancer. J Endocr Soc. 2021 Jun 19;5(9):bvab116. [CrossRef]
- Lee JH, Jee BA, Kim JH, Bae H, Chung JH, Song W, Sung HH, Jeon HG, Jeong BC, Seo SI, Jeon SS, Lee HM, Park SH, Kang M. Prognostic Impact of Sarcopenia in Patients with Metastatic Hormone-Sensitive Prostate Cancer. Cancers (Basel). 2021 Dec 17;13(24):6345. [CrossRef]
- Papadopoulos E, Wong AKO, Law SHC, Zhang LZJ, Breunis H, Emmenegger U, Alibhai SMH. The impact of sarcopenia on clinical outcomes in men with metastatic castrate-resistant prostate cancer. PLoS One. 2023 Jun 1;18(6):e0286381. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).