Submitted:
15 August 2023
Posted:
17 August 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Background
2.1. Stress
2.2. Physiological Signals
2.3. Wearable Technology for Autism
3. Objectives
- 1-
- What intelligent wearable solutions are most acceptable for people with ASD?
- 2-
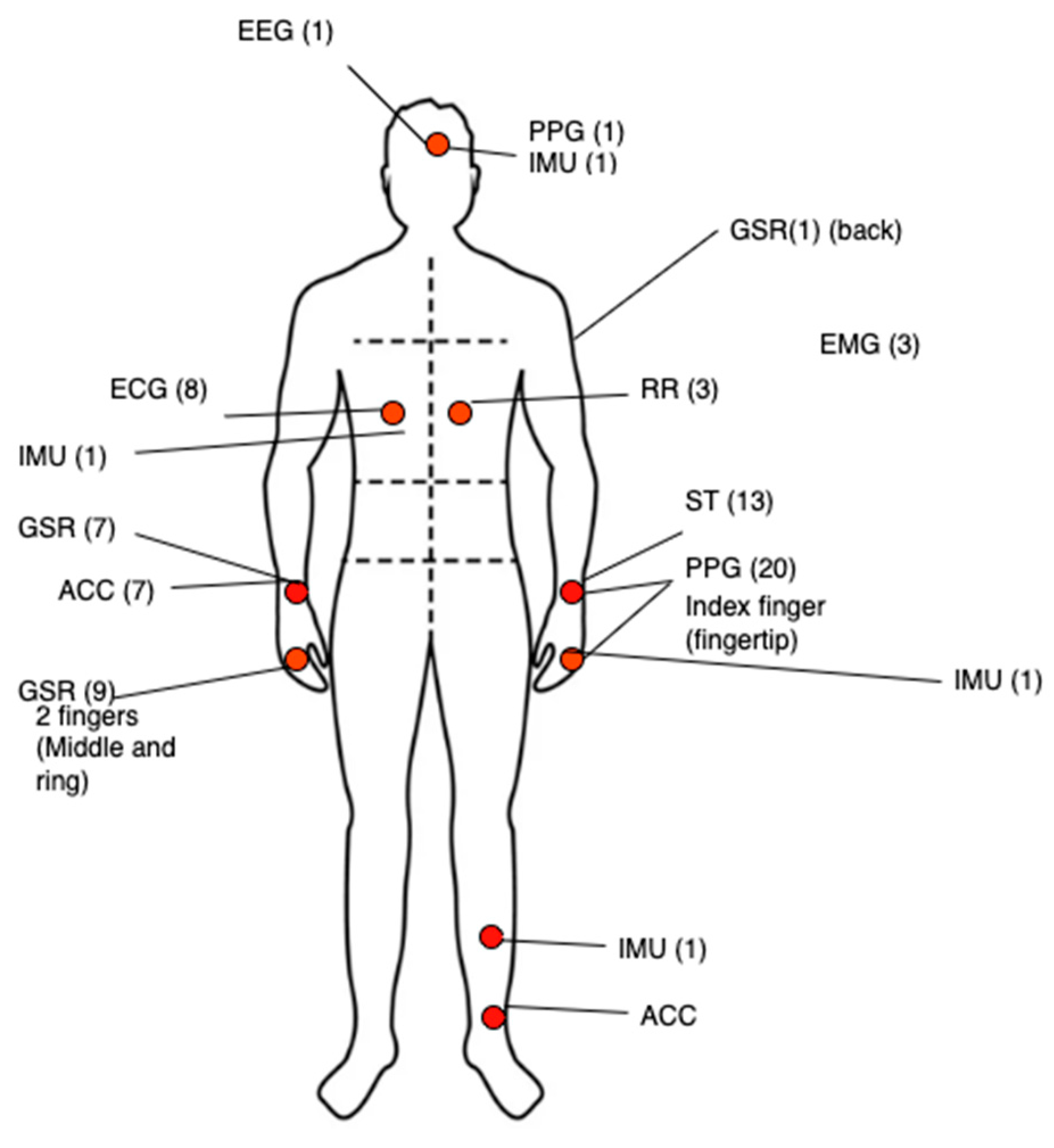
- Which physiological signals are used for monitoring stress?
- 3-
- Which Artificial Intelligent algorithms have been used to detect stress?
- 4-
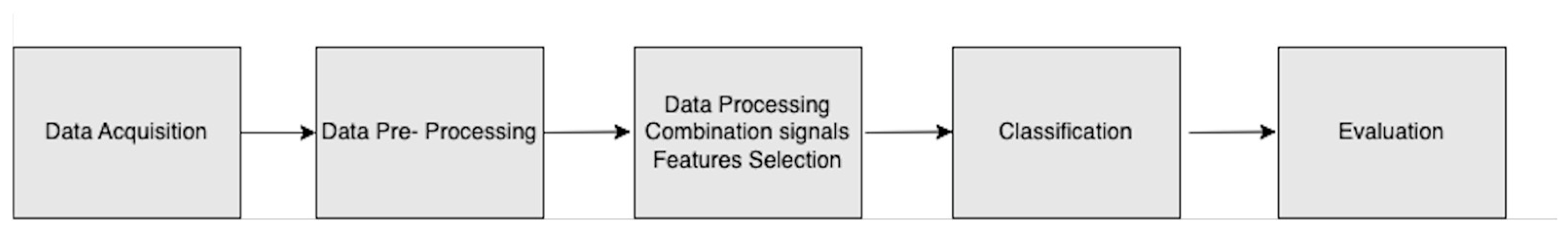
- What is the process for detecting stress using wearable technology?
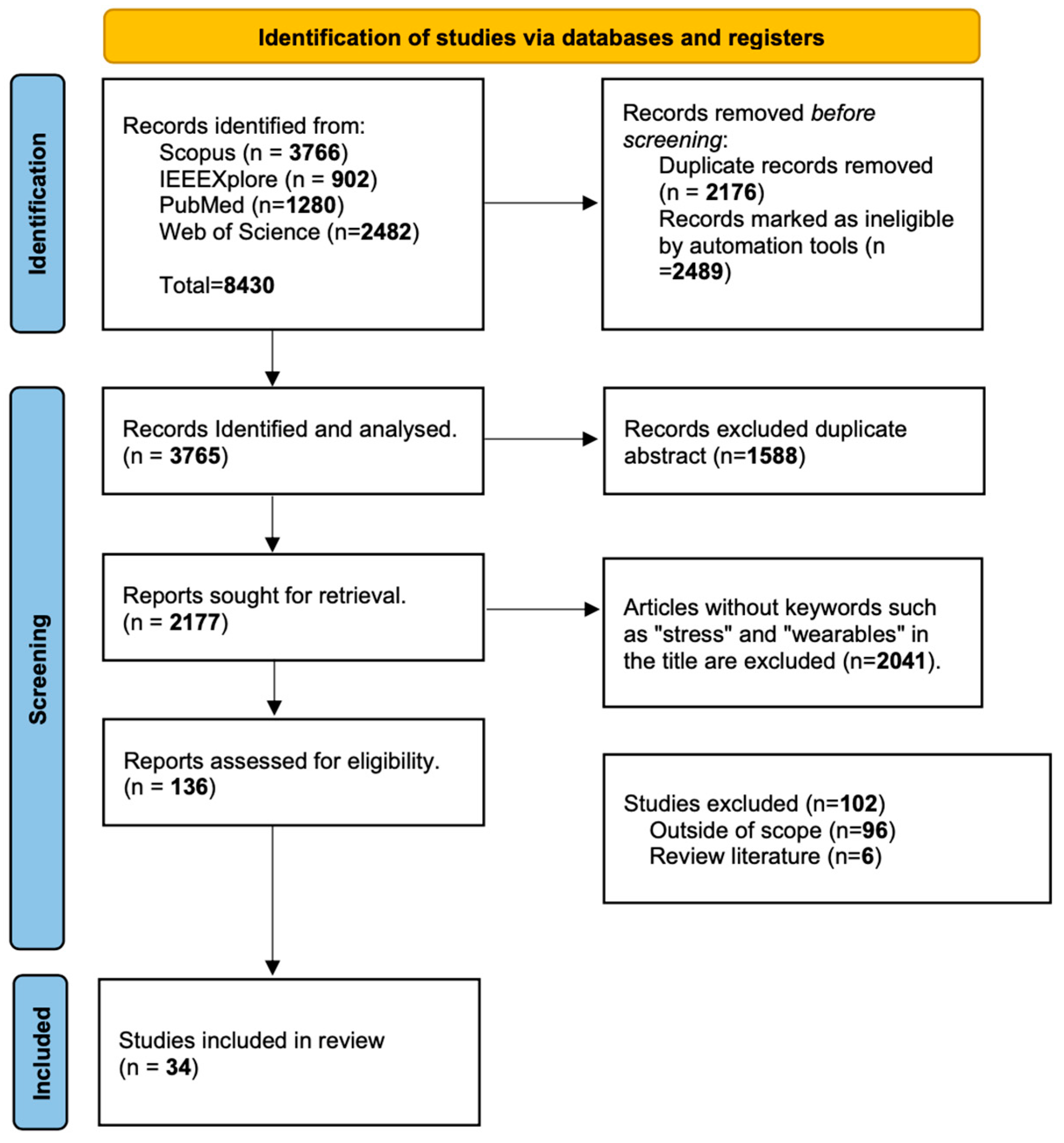
4. Methodology
3.1. Selection Keywords
3.2. Inclusion/ Exclusion criteria selection of studies
5. Results
Data Extraction
6. Discussion
7. Conclusions
Author Contributions
Funding
Data Availability Statement
Conflicts of Interest
References
- American Psychiatric Association, 2013. Diagnostic and Statistical Manual of Mental Disorders. 5th ed., Washington, DC.
- Salazar, F. , Baird, G., Chandler, S., Tseng, E., O'Sullivan, T., Howlin, P., Pickles, A., & Simonoff, E. (2015). Co-occurring psychiatric disorders in preschool and elementary school-aged children with autism spectrum disorder. Journal of autism and developmental disorders, 2294. [Google Scholar] [CrossRef]
- White, S. W. , Oswald, D., Ollendick, T., & Scahill, L. (2009). Anxiety in children and adolescents with autism spectrum disorders. ( 29(3), 216–229. [CrossRef] [PubMed]
- Fuld, S. Autism spectrum disorder: The impact of stressful and traumatic life events and implications for clinical practice. Clin Soc Work J, 2018. [Google Scholar] [CrossRef]
- Case-Smith, J. , Weaver L. L., and Fristad M. A. A systematic review of sensory processing interventions for children with autism spectrum disorders. Autism. [CrossRef]
- Available online:. Available online: https://www.apa.org/topics/stress (accessed on 15 July, 2023).
- Lazarus RS, Folkman S (1984). Coping and Adaptation. The Handbook of Behavioral Medicine, pp. 282-325.
- Fuld, S. Autism Spectrum Disorder: The Impact of Stressful and Traumatic Life Events and Implications for Clinical Practice. Clin Soc Work J. 2018;46(3):210-219. [CrossRef]
- Won E, Kim YK. Stress, the Autonomic Nervous System, and the Immune-kynurenine Pathway in the Etiology of Depression. Curr Neuropharmacol. 2016;14(7):665-73. [CrossRef]
- J. A. Healey and R. W. Picard, "Detecting stress during real-world driving tasks using physiological sensors," in IEEE Transactions on Intelligent Transportation Systems, vol. 6, no. 2, pp. 156-166, 05. 20 June. [CrossRef]
- Taj-Eldin, M.; Ryan, C.; O’Flynn, B.; Galvin, P. A Review of Wearable Solutions for Physiological and Emotional Monitoring for Use by People with Autism Spectrum Disorder and Their Caregivers. Sensors 2018, 18, 4271. [Google Scholar] [CrossRef] [PubMed]
- E4- Wristband. Available online: https://store.empatica.com/products/e4-wristband?variant=39588207747 (accessed on 9 June 2023).
- Sumin Helen Koo, Kim Gaul, Susan Rivera, Tingrui Pan and Dan Fong. ( 31(1), 37–55.
- Will Simm, Maria Angela Ferrario, Adrian Gradinar, Marcia Tavares Smith, Stephen Forshaw, Ian Smith, and Jon Whittle. 2016. Anxiety and Autism: Towards Personalized Digital Health. In Proceedings of the 2016 CHI Conference on Human Factors in Computing Systems (CHI '16). Association for Computing Machinery, New York, NY, USA, 1270–1281. [CrossRef]
- Black, M. H. , Milbourn, B., Chen, N. T. M., McGarry, S., Wali, F., Ho, A. S. V., et al. (2020). The use of wearable technology to measure and support abilities, disabilities and functional skills in autistic youth: a scoping review. Scand. J. Child Adolesc. Psychiatr. Psychol. 8, 48–69. [CrossRef]
- Kientz, J.A. , Hayes, G.R., Goodwin, M.S., Gelsomini, M., Abowd, G.D. (2020). Sensor-Based and Wearable. In: Interactive Technologies and Autism, Second Edition. Synthesis Lectures on Assistive, Rehabilitative, and Health-Preserving Technologies. Springer, Cham. [CrossRef]
- C. McCarthy, N. C. McCarthy, N. Pradhan, C. Redpath, and A. Adler. Validation of the empatica e4 wristband, in Proc. IEEE EMBS Int. Student Conf. (ISC), Ottawa, ON, Canada, 16, pp. 1–4. 20 May.
- Francese, R. , and Yang, X. (2021). Supporting autism spectrum disorder screening and intervention with machine learning and wearables: a systematic literature review. Complex Intel. Syst. 8, 3659–3674. [CrossRef]
- Samson C and Koh A (2020) Stress Monitoring and Recent Advancements in Wearable Biosensors. Front. Bioeng. Biotechnol. 8:1037. [CrossRef]
- Sivaratnam, C.S. , Newman, L.K., Tonge, B.J. et al. Attachment and Emotion Processing in Children with Autism Spectrum Disorders: Neurobiological, Neuroendocrine, and Neurocognitive Considerations. Rev J Autism Dev Disord 2, 222–242 (2015). [CrossRef]
- Goodwin MS, Mazefsky CA, Ioannidis S, Erdogmus D, Siegel M. Predicting aggression to others in youth with autism using a wearable biosensor. Autism Res. 2019 Aug;12(8):1286-1296. [CrossRef]
- S. H. Koo1, K. S. H. Koo1, K. Gaul, S. Rivera, T. Pan, D. Fong. Wearable Technology Design for Autism Spectrum Disorders. Archives of Design Research, vol. 31, no. 1, pp. 37-55, 2018.
- Rochette, L. , and Vergely, C. (2017). Hans Selye and the Stress Response: 80 Years after His ‘Letter’ to the Editor of Nature. Annal. de Cardiol. et d’Angeiol. 66, 181–183. [CrossRef]
- Lindau M, Almkvist O, Mohammed AH. (2016) Effects of stress on learning and memory. In: Fink G. (ed.) Concept, Cognition, Emotion and Behavior. San Diego, CA: Elsevier Academic Press, pp.
- White, S.W.; Oswald, D.; Ollendick, T.; Scahill, L. Anxiety in children and adolescents with autism spectrum disorders. Clin. Psychol. Rev. 2009, 29, 216–229. [Google Scholar] [CrossRef] [PubMed]
- Pop-Jordanova N, Pop-Jordanov J. Electrodermal Activity and Stress Assessment. Pril (Makedon Akad Nauk Umet Odd Med Nauki). 2020 Sep 1;41(2):5-15. [CrossRef]
- Karthikeyan P, Murugappan M, Yaacob S. Detection of human stress using short-term ECG and HRV signals. J Mech Med Biol. 2013.
- Munhee Lee, Junhyung Moon, Dongmi Cheon, Juneil Lee, and Kyoungwoo Lee. 2020. Respiration signal based two layer stress recognition across non-verbal and verbal situations. In Proceedings of the 35th Annual ACM Symposium on Applied Computing (SAC '20). Association for Computing Machinery, New York, NY, USA, 638–645. [CrossRef]
- R. Riaz, N. R. Riaz, N. Naz, M. Javed, F. naz and H. Toor, "Effect of Mental Workload Related Stress on Physiological Signals," 2020 IEEE-EMBS Conference on Biomedical Engineering and Sciences (IECBES), Langkawi Island, Malaysia, 2021, pp. 339-344. [CrossRef]
- M. T. Tomczak et al., "Stress Monitoring System for Individuals with Autism Spectrum Disorders," in IEEE Access, vol. 8, pp. 228236-228244, 2020. [CrossRef]
- Alberdi A, Aztiria A, Basarab A. Towards an automatic early stress recognition system for office environments based on multimodal measurements: A review. J Biomed Inform. 2016 Feb;59:49-75. [CrossRef]
- Jeyhani, V. , Mahdiani, S., Peltokangas, M., & Vehkaoja, A. (2015). Comparison of HRV parameters derived from photoplethysmography and electrocardiography signals. ( 2015, 5952–5955. [CrossRef] [PubMed]
- Kim HG, Cheon EJ, Bai DS, Lee YH, Koo BH. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018 Mar;15(3):235-245. [CrossRef]
- Calkins, S. D. & Keane, S. P. Cardiac vagal regulation across the preschool period: Stability, continuity, and implications for childhood adjustment. Dev. Psychobiol. [CrossRef]
- Villarejo, M. V. , Zapirain, B. G., & Zorrilla, A. M. (2012). A stress sensor based on galvanic skin response (GSR) controlled by ZigBee. M. ( 12(5), 6075–6101. [CrossRef]
- Christiaan, H. Vinkers, Renske Penning, Juliane Hellhammer, Joris C. Verster, John H. G. M. Klaessens, Berend Olivier & Cor J. 5: Kalkman (2013) The effect of stress on core and peripheral body temperature in humans, Stress, 16, 2013; :5. [Google Scholar] [CrossRef]
- Masaoka Y, Homma I. Anxiety and respiratory patterns: their relationship during mental stress and physical load. Int. J. Psychophysiol. 1997, 27, 153–159. [Google Scholar] [CrossRef] [PubMed]
- Cho, D.; Ham, J.; Oh, J.; Park, J.; Kim, S.; Lee, N.-K.; Lee, B. Detection of stress levels from biosignals measured in virtual reality environments using a kernel-based extreme learning machine. Sensors 2017, 17, 2435. [Google Scholar] [CrossRef] [PubMed]
- Yiannis Koumpouros, Theodoros Kafazis. Wearables and mobile technologies in Autism Spectrum Disorder interventions: A systematic literature review. Research in Autism Spectrum Disorders,Volume 66, 2019, 101405, ISSN 1750-9467. [CrossRef]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G. The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. PLoS Med. 2009, 6, e1000097. [Google Scholar] [CrossRef] [PubMed]
- Zwilling M, Romano A, Hoffman H, Lotan M and Tesler R (2022) Development and validation of a system for the prediction of challenging behaviors of people with autism spectrum disorder based on a smart wearable shirt: A mixed-methods design. Front. Behav. Neurosci. 16:948184. [CrossRef]
- Hexos Skin. Available online: https://www.hexoskin.com (accessed on 16 June 2023).
- Katharine, S. Willis, Elizabeth Cross. Investigating the potential of EDA data from biometric wearables to inform inclusive design of the built environment, Emotion, Space and Society, Volume 45, 2022, 100906, ISSN 1755-4586. [CrossRef]
- Nguyen, J. , Cardy, R.E., Anagnostou, E. et al. Examining the effect of a wearable, anxiety detection technology on improving the awareness of anxiety signs in autism spectrum disorder: a pilot randomized controlled trial. Molecular Autism 12, 72 (2021). [CrossRef]
- L. D’Alvia et al., "Heart rate monitoring under stress condition during behavioral analysis in children with neurodevelopmental disorders," 2020 IEEE International Symposium on Medical Measurements and Applications (MeMeA), Bari, Italy, 2020, pp. 1-6. [CrossRef]
- J. Masino et al., "m-Health and Autism: Recognizing Stress and Anxiety with Machine Learning and Wearables Data," 2019 IEEE 32nd International Symposium on Computer-Based Medical Systems (CBMS), Cordoba, Spain, 2019, pp. 714-719. [CrossRef]
- Goldsmith HH, Reilly HH, Lemery KL, Longley S, Prescott A. The laboratory temperament assessment battery: Middle childhood version. Unpubl manuscript, Univ Wisconsin-Madison. 2001.
- Empatica E4. Available online: https://www.empatica.com/research/e4/ (accessed on 16 June 2023).
- Planalp EM, Van Hulle C, Gagne JR and Goldsmith HH (2017) The Infant Version of the Laboratory Temperament Assessment Battery (Lab-TAB): Measurement Properties and Implications for Concepts of Temperament. Front. Psychol. 8:846. [CrossRef]
- Tamara Vanderwal, Clare Kelly, Jeffrey Eilbott, Linda C. Mayes, F. Xavier Castellanos, Inscapes: A movie paradigm to improve compliance in functional magnetic resonance imaging, NeuroImage, Volume 122, 2015, Pages 222-232, ISSN 1053-8119. [CrossRef]
- de Vries H, Kamphuis W, Oldenhuis H, van der Schans C, Sanderman R. Moderation of the Stressor-Strain Process in Interns by Heart Rate Variability Measured With a Wearable and Smartphone App: Within-Subject Design Using Continuous Monitoring. JMIR Cardio. 2021 Oct 4;5(2):e28731. [CrossRef]
- Hahrad Shakerian, Mahmoud Habibnezhad, Amit Ojha, Gaang Lee, Yizhi Liu, Houtan Jebelli, SangHyun Lee. A: Assessing occupational risk of heat stress at construction, 2021. [CrossRef]
- Whiston A, Igou ER, Fortune DG, Analog Devices Team, Semkovska M. Examining Stress and Residual Symptoms in Remitted and Partially Remitted Depression Using a Wearable Electrodermal Activity Device: A Pilot Study. IEEE J Transl Eng Health Med. 2022 Dec 12;11:96-106. [CrossRef]
- M. Umair, N. M. Umair, N. Chalabianloo, C. Sas and C. Ersoy, "HRV and Stress: A Mixed-Methods Approach for Comparison of Wearable Heart Rate Sensors for Biofeedback," in IEEE Access, vol. 9, pp. 14005-14024, 2021. [CrossRef]
- Arquilla K, Webb AK, Anderson AP. Textile Electrocardiogram (ECG) Electrodes for Wearable Health Monitoring. Sensors (Basel). 2020 Feb 13;20(4):1013. [CrossRef]
- D. S. Lee, T. W. D. S. Lee, T. W. Chong and B. G. Lee, "Stress Events Detection of Driver by Wearable Glove System," in IEEE Sensors Journal, vol. 17, no. 1, pp. 194-204, 1 Jan.1, 2017. [CrossRef]
- Golgouneh, A. , Tarvirdizadeh, B. Fabrication of a portable device for stress monitoring using wearable sensors and soft computing algorithms. Neural Comput & Applic, 2020. [Google Scholar] [CrossRef]
- Niaz Chalabianloo, Yekta Said Can, Muhammad Umair, Corina Sas, Cem Ersoy. 2022; 87. [CrossRef]
- Van-Tu Ninh and Sinéad Smyth and Minh-Triet Tran and Cathal Gurrin. Analysing the Performance of Stress Detection Models on Consumer-Grade Wearable Devices. arXiv, 2022.
- 4: Leiner, Andreas Fahr & Hannah Früh (2012) EDA Positive Change: A Simple Algorithm for Electrodermal Activity to Measure General Audience Arousal During Media Exposure, Communication Methods and Measures, 6, 2012; :4. [CrossRef]
- Nath, R.K. , Thapliyal, H. & Caban-Holt, A. Machine Learning Based Stress Monitoring in Older Adults Using Wearable Sensors and Cortisol as Stress Biomarker. J Sign Process Syst, 2022. [Google Scholar] [CrossRef]
- Iqbal T, Simpkin AJ, Roshan D, Glynn N, Killilea J, Walsh J, Molloy G, Ganly S, Ryman H, Coen E, Elahi A, Wijns W, Shahzad A. Stress Monitoring Using Wearable Sensors: A Pilot Study and Stress-Predict Dataset. Sensors (Basel). 2022 Oct 24;22(21):8135. [CrossRef]
- N. Z. Jia et al., "Design of a Wearable System to Capture Physiological Data to Monitor Surgeons’ Stress During Surgery," 2020 42nd Annual International Conference of the IEEE Engineering in Medicine & Biology Society (EMBC), Montreal, QC, Canada, 2020, pp. 4539-4542. [CrossRef]
- Herborn KA, Graves JL, Jerem P, Evans NP, Nager R, McCafferty DJ, McKeegan DE. Skin temperature reveals the intensity of acute stress. Physiol Behav. 2015 Dec 1;152(Pt A):225-30. [CrossRef]
- Sun, Gengxin, Xu, Huixiang, Zhang, Nan, Liu, Qiuju. Wearable Psychological Stress Monitoring Equipment and Data Analysis Based on a Wireless Sensor. Hindawi, 2022. [CrossRef]
- Dalmeida KM, Masala GL. HRV Features as Viable Physiological Markers for Stress Detection Using Wearable Devices. Sensors (Basel). 2021 Apr 19;21(8):2873. [CrossRef]
- J. Wijsman, B. J. Wijsman, B. Grundlehner, H. Liu, J. Penders and H. Hermens, "Wearable Physiological Sensors Reflect Mental Stress State in Office-Like Situations," 2013 Humaine Association Conference on Affective Computing and Intelligent Interaction, Geneva, Switzerland, 2013, pp. 600-605. [CrossRef]
- Hira ZM, Gillies DF. A Review of Feature Selection and Feature Extraction Methods Applied on Microarray Data. Adv Bioinformatics. 2015;2015:198363. [CrossRef]
- Li B, Sano A. Early versus Late Modality Fusion of Deep Wearable Sensor Features for Personalized Prediction of Tomorrow's Mood, Health, and Stress. Annu Int Conf IEEE Eng Med Biol Soc. 2020 Jul;2020:5896-5899. [CrossRef]
- Research Center for Development of Advanced Technologies. Available online: http://en.rcdat.ir. (accessed on 16 June 2023).
- Philip Schmidt, Attila Reiss, Robert Duerichen, Claus Marberger, and Kristof Van Laerhoven. 2018. Introducing WESAD, a Multimodal Dataset for Wearable Stress and Affect Detection. In Proceedings of the 20th ACM International Conference on Multimodal Interaction (ICMI '18). Association for Computing Machinery, New York, NY, USA, 400–408. [CrossRef]
- Goldberger, A.; Amaral, L.; Glass, L.; Hausdorff, J.; Ivanov, P.C.; Mark, R.; Mietus, J.E.; Moody, G.B.; Peng, C.K.; Stanley, H.E. PhysioBank, PhysioToolkit, and PhysioNet: Components of a new research resource for complex physiologic signals. Circulation 2000, 101, e215–e220. [Google Scholar] [CrossRef] [PubMed]
- Haouij NE, Poggi JM, Sevestre-Ghalila S, Ghozi R, Ja ̈ıdane M. AffectiveROAD System and Database to Assess Driver’s Attention. In: Proceedings of the 33rd Annual ACM Symposium on Applied Computing. SAC ’18. New York, NY, USA: Association for Computing Machinery; 2018. p. 800–803.
- SWELL Dataset. Available online: https://www.kaggle.com/datasets/qiriro/swell-heart-rate-variability-hrv (accessed on 2 August 2023).
- S. Prashant Bhanushali, S. S. Prashant Bhanushali, S. Sadasivuni, I. Banerjee and A. Sanyal, "Digital Machine Learning Circuit for Real-Time Stress Detection from Wearable ECG Sensor," 2020 IEEE 63rd International Midwest Symposium on Circuits and Systems (MWSCAS), Springfield, MA, USA, 2020, pp. 978-981. [CrossRef]
- Prerna Garg, Jayasankar Santhosh, Andreas Dengel, and Shoya Ishimaru. 2021. Stress Detection by Machine Learning and Wearable Sensors. In 26th International Conference on Intelligent User Interfaces - Companion (IUI '21 Companion). Association for Computing Machinery, New York, NY, USA, 43–45. [CrossRef]
- Bin Heyat MB, Akhtar F, Abbas SJ, Al-Sarem M, Alqarafi A, Stalin A, Abbasi R, Muaad AY, Lai D, Wu K. Wearable Flexible Electronics Based Cardiac Electrode for Researcher Mental Stress Detection System Using Machine Learning Models on Single Lead Electrocardiogram Signal. Biosensors (Basel). 2022 Jun 17;12(6):427. [CrossRef]
- S. Aristizabal et al., "The Feasibility of Wearable and Self-Report Stress Detection Measures in a Semi-Controlled Lab Environment," in IEEE Access, vol. 9, pp. 102053-102068, 2021. [CrossRef]
- Ghosh S, Kim S, Ijaz MF, Singh PK, Mahmud M. Classification of Mental Stress from Wearable Physiological Sensors Using Image-Encoding-Based Deep Neural Network. Biosensors (Basel). 2022 Dec 9;12(12):1153. [CrossRef]
- Talaat, F.M. , El-Balka, R.M. Stress monitoring using wearable sensors: IoT techniques in medical field. Neural Comput & Applic. [CrossRef]
- R. Gupta, A. R. Gupta, A. Bhongade and T. K. Gandhi, "Multimodal Wearable Sensors-based Stress and Affective States Prediction Model," 2023 9th International Conference on Advanced Computing and Communication Systems (ICACCS), Coimbatore, India, 2023, pp. 30-35. [CrossRef]
- Barki, H.; Chung, W.-Y. Mental Stress Detection Using a Wearable In-Ear Plethysmography. Biosensors 2023, 13, 397. [Google Scholar] [CrossRef] [PubMed]
- Bari R, Rahman MM, Saleheen N, Parsons MB, Buder EH, Kumar S. Automated Detection of Stressful Conversations Using Wearable Physiological and Inertial Sensors. Proc ACM Interact Mob Wearable Ubiquitous Technol. 2020 Dec;4(4):117. [CrossRef]
- L. G. A. Raymondi, F. E. A. L. G. A. Raymondi, F. E. A. Guzmán, J. Armas-Aguirre and P. A.González, "Technological solution for the identification and reduction of stress level using wearables," 2020 15th Iberian Conference on Information Systems and Technologies (CISTI), Seville, Spain, 2020, pp. 1-7. [CrossRef]
- Ramírez-Valenzuela, R.A. , Monroy, R., Loyola-González, O. et al. A one-class-classification approach to create a stresslevel curve plotter through wearable measurements and behavioral patterns. Int J Interact Des Manuf 15, 159–171 (2021). [CrossRef]
- Issei Imura, Yusuke Gotoh, Koji Sakai, Yu Ohara, Jun Tazoe, Hiroshi Miura, Tatsuya Hirota, Akira Uchiyama, and Yoshinari Nomura, A Method for Estimating Physician Stress Using Wearable Sensor Devices, Sens. Mater., Vol. 34, No. 8, 2022, p. 2955-2971.
- Chalmers T, Hickey BA, Newton P, Lin CT, Sibbritt D, McLachlan CS, Clifton-Bligh R, Morley J, Lal S. Stress Watch: The Use of Heart Rate and Heart Rate Variability to Detect Stress: A Pilot Study Using Smart Watch Wearables. Sensors (Basel). 2021 Dec 27;22(1):151. [CrossRef]
- M. Stojchevska et al., “Assessing the added value of context during stress detection from wearable data,” BMC MEDICAL INFORMATICS AND DECISION MAKING, vol. 22, no. 1, 2022.
- Ninh, VT. et al. (2022). An Improved Subject-Independent Stress Detection Model Applied to Consumer-grade Wearable Devices. In: Fujita, H., Fournier-Viger, P., Ali, M., Wang, Y. (eds) Advances and Trends in Artificial Intelligence. Theory and Practices in Artificial Intelligence. IEA/AIE 2022. Lecture Notes in Computer Science(), vol 13343. Springer, Cham. [CrossRef]
- Valenti, S.; Volpes, G.; Parisi, A.; Peri, D.; Lee, J.; Faes, L.; Busacca, A.; Pernice, R. Wearable Multisensor Ring-Shaped Probe for Assessing Stress and Blood Oxygenation: Design and Preliminary Measurements. Biosensors 2023, 13, 460. [Google Scholar] [CrossRef] [PubMed]
- Shajari S, Salahandish R, Zare A, Hassani M, Moossavi S, Munro E, Rashid R, Rosenegger D, Bains JS, Sanati Nezhad A. MicroSweat: A Wearable Microfluidic Patch for Noninvasive and Reliable Sweat Collection Enables Human Stress Monitoring. Adv Sci (Weinh). 2023 Mar;10(7):e2204171. [CrossRef]
- Jansen, L.M.C. , Gispen-de Wied, C.C., Wiegant, V.M. et al. Autonomic and Neuroendocrine Responses to a Psychosocial Stressor in Adults with Autistic Spectrum Disorder. J Autism Dev Disord 36, 891–899 (2006). [CrossRef]
- Russell, JA. A circumplex model of affect. Journal of Personality and Social Psychology. 1161. [Google Scholar]
- Milstein N, Gordon I. Validating Measures of Electrodermal Activity and Heart Rate Variability Derived from the Empatica E4 Utilized in Research Settings That Involve Interactive Dyadic States. Frontiers in Behavioral Neuroscience. 2020;14:148.
- Hassenzahl, M.; Tractinsky, N. User experience—A research agenda. Behav. Inf. Technol. 2006, 25, 91–97. [Google Scholar] [CrossRef]
- Morville, P. Semantic Studios. Available online: http://semanticstudios.com/user_experience_design/ (accessed on 13 January 2023).
- Francés-Morcillo, L.; Morer-Camo, P.; Rodríguez-Ferradas, M.I.; Cazón-Martín, A. Wearable Design Requirements Identification and Evaluation. Sensors 2020, 20, 2599. [Google Scholar] [CrossRef] [PubMed]
- Valencia, K.; Rusu, C.; Botella, F. User Experience Factors for People with Autism Spectrum Disorder. Appl. Sci. 2021, 11, 10469. [Google Scholar] [CrossRef]
- Koo, S.H.; Gaul, K.; Rivera, S.; Pan, T.; Fong, D. Wearable Technology Design for Autism Spectrum Disorders. Arch. Des. Res. 2018, 31, 37–55. [Google Scholar] [CrossRef]
| Nomenclature | Referred to | Nomenclature | Referred to |
|---|---|---|---|
| ACC | Accelerometer | LR | Lineal Regression |
| ANN | Artificial Neural Network | LSTM | Long Short-Term Memory |
| ANS | Autonomic Nervous System | LF | Low Frequency |
| BP | Blood Pressure | ML | Machine Learning |
| BVP | Blood Volume Pulse | MLP | Multilayer Perceptron |
| CNN | Convolutional Neural Network | NB | Naïve Bayes |
| DT | Decision Tree | PCA | Principal Component Analysis |
| DASS | Depression Anxiety Stress Scale | pNN50 | Percentage of successive RR intervals that differ by more than 50 ms. |
| ECG | Electrocardiography | PPG | Photoplethysmography |
| EDA | Electrodermal Activity | PRV | Pulse Rate Variability |
| EEG | Electroencephalogram | PSS | Perceived Stress Scale |
| EMG | Electromyography | PSD | Power Spectrum Density |
| GSR | Galvanic Skin Response | RBF | Radial Base Function |
| GB | Gradient Boosting | RR | Respiration Rate |
| GSM | Gramian Angular Field | RF | Random Forest |
| HF | High Frequency | RSP | Respiration |
| HR | Heart Rate | RMSSD | Root mean Square of successive differences between normal heartbeats |
| HRV | Heart Rate Variability | SC | Skin Conductance |
| IBI | Interbeat Interval | SCL | Skin Conductance Level |
| IMU | Inertial Measurement Unit | SCR | Skin Conductance Response |
| KNN | K-Nearest Neighbors | SCWT | Stroop Color-Word Test |
| LDA | Linear Discriminant Analysis | TSST | Trier Social Stress Test |
| Study | Year | Device Type | Signals /Sensors | Parameters/ Features | Communication | Methods | Algorithms | People |
|---|---|---|---|---|---|---|---|---|
| [67] | 2013 | - | ECG, respiration, sking conductance, EMG | HR, SDNN, SCL | Perceived Stress Scale Questionnaire, Visual Analogue Scales (VAS) | - | Subjects between 19 to 53 | |
| [56] | 2017 | Glove | PPG, IMU | STD, variance, PSD, RMS. | Bluetooth | SVM, RBF | - | |
| [46] | 2019 | Wrist-band | PPG | HR, RR | Bluetooth | Stress tasks | SVM, LR | Subjects with ASD |
| [83] | 2020 | - | ECG, Respiration, IMU | HRV, 3-axis accelerometer, 3-axis gyroscope. mean, median, 80th percentile, and quartile deviation | - | - | SVM | Subjects between 24 and 33 |
| [30] | 2020 | Wrist-band | PPG, ST, GSR | Bluetooth | - | - | Subjects with ASD between 5 and 24 | |
| [57] | 2020 | Wrist-band | PPG, GSR | 90 features | Bluetooth | SVR, ANN, ANFIS, kNN, SVM, NB | Subjects between 24 and 27 | |
| [63] | 2020 | Chest band attached to underwear | ECG, EMG, EDA and IMU | - | - | - | - | - |
| [69] | 2020 | SC, ST, AC | - | - | Big give Personality. | MLP, LSTM | - | |
| [75] | 2020 | - | ECG | 5 time-domain features | - | - | kNN, LDA, SVM, RF | - |
| [84] | 2020 | Wrist-band | PPG | - | Bluetooth | - | ML | Suejects between 25 and 35 |
| [51] | 2021 | Wrist-band | PPG | HRV | Bluetooth | - | - | Subjects between 19 and 33 |
| [66] | 2021 | ECG | HRV subdivided: 11 features time domain. | - | - | SVM, KNN, GB, RF, MLP | - | |
| [59] | 2022 | - | EDA, HR | - | - | - | LR, RF, SVM, MLP, KNN | - |
| [76] | 2021 | Wrist-band chest-worn | ECG, RSP, EMG, EDA, ST | - | - | - | KNN, AdaBoost, SVM,LDA RF Random Forest, LDA | - |
| Study | Year | Device type | Signals /Sensors | Parameters/ Features | Communication | Methods | Algorithms | People |
| [85] | 2021 | Wrist-band | GSR, PPG, IMU, ST | - | - | SWS | Baggin-TPMiner | - |
| [52] | 2021 | Wrist-band | EDA, PPG, ST | Bluetooth | ANN, k-NN, SVM, RF | |||
| [54] | 2021 | Wrist-worn, chest strap | PPG, EEG | 12 features HRV | Bluetooth | TSST | - | Subjects between 23 and 33 |
| [86] | 2021 | Wrist-band | ECG /PPG | HRV | SDNN, NN50, pNN50, LF and HF | - | - | - |
| [62] | 2022 | Wrist-band | PPG, ACC, ST | BVP, IBI, HRV | Bluetooth | TSST, STAI, Stroop-CW | - | Subjects between 24 and 40 |
| [78] | 2021 | Wrist-band | EDA,PPG, IMU, ST | - | Bluetooth | TSST, STAI, PSS-10 | Deep learning | Subjects between 22 and 30 |
| [87] | 2021 | Wrist-band | ECG | HRV: FLV, LF, AF, TP | TSST, DASS | Subjects between 20 and 37 | ||
| [79] | 2022 | - | RESP, ST, ECG, ACC | - | - | - | CNN | - |
| [77] | 2022 | T-Shirt | ECG | HRV,MRR, RMS, TPR,NN50, SDRR | Bluetooth | DASS, SFS, CFS | DT ,NB, RF, LR | Subject between 23 and 35 |
| [65] | 2022 | - | EEG, ECG, TMP | - | Bluetooth | - | - | - |
| [58] | 2022* | Wrist-band | ECG, EDA, ST, PPG | STD, RR, RMSSD, TINN, FC-max- FC-min, LF/HF | Bluetooth | SCWT, TSST | SVM, RBF | Subjects between 23 and 33 |
| [88] | 2022 | Writs-band | GSR, ST, ACC | Bluetooth | PSQ | GBT | ||
| [61] | 2022 | GSR, PPG | Median, SD, amplitude, peaks per minute, mean, RMS | Bluetooth | TSST | DT, k-NN RF, SVM, LR, LSTM | Subject between 67 and 79 | |
| [89] | 2022 | - | EDA, PPG, ST, ACC | - | - | - | SVM, RF, NN | - |
| [82] | 2023 | Ear portable | PPG. IMU | - | - | - | CNN | - |
| [90] | 2023 | Ring | PPG, GSR | Mean, SDNN, PPI, HRV, SpO2, SCL, SCR, SNS | - | Video | - | Subjects between 23 and 27 |
| [91] | 2023 | Microsweat | Cortisol | - | - | - | - | - |
| [53] | 2022 | Wrist-band | EDA | - | - | - | DASS. DBI | Subjects between18 and 47 |
| Study | Year | Device type | Signals /Sensors | Parameters/ Features | Communication | Methods | Algorithms | People |
| [80] | 2023 | Wrist-band | GSR, PPG, ACC | DSP Algorithm | Bluetooth | - | RF, XGBoost, DT, OSM | |
| [81] | 2023 | Wrist-band | GSR, PPG, ACC. ST, ECG, RESP | Mean, mean, SD, Mean RR, amplitude, SCL/SRC min, max | - | - | RF | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).





