Introduction and Objective:
Circumcision involves exposing the tip of the penis by surgically cutting away the foreskin, called the prepuce, which covers the glans (1). Circumcision is the most commonly performed surgery in the world, and considering its historical development, it is also the oldest surgery in the world (2). Pain during surgical procedures in children causes many adverse effects in the physiological local, and/or systemic body (3). These effects may lead to delays in recovery, increased consumption of narcotic analgesics and associated complications, prolongation of hospital stay, and chronic pain. In addition to the physiological effects, pain, with its psychological consequences, may go beyond the process and negatively affect the child’s motor and mental development. Therefore, it is quite important to assess pain and treat postoperative pain properly (4). Opioids used for postoperative analgesia in children have side effects such as superficial respiration and decreased intestinal motility, nausea, vomiting, pruritus, and addictive behaviour. These effects lead to complications, prolong hospital stays, increase costs, and affect patient comfort (5). Caudal block has been used in children for many years and is considered the gold standard for multimodal analgesia in the pediatric age group (6). Caudal block is an effective method for postoperative analgesia in anorectal surgery, intraluminal surgery, and perineal surgery (e.g., circumcision). Caudal block also reduces the use of systemic opioids and non-opioid analgesics without causing a motor block. This allows rapid mobilization of patients and reduces the incidence of postoperative side effects (7,8). Caudal block belongs to the category of central neuraxial blocks, which can provide both visceral and somatic analgesia. As a result of the development of peripheral nerve blocks, a transversus abdominis plane (TAP) block or quadratus lumborum block (QLB) may be performed during infra umbilical surgery in children. As it provides visceral analgesia, a caudal block is still the preferred method of analgesia in the pediatric age group (9-11).
In our study, we aimed to compare the efficacy of a single caudal block in postoperative acute pain management, the need for additional analgesics, the frequency of side effects, the timing of the first analgesic administration, and the need for administration of a rescue analgesic (acetaminophen 10 mg/kg). Our primary hypothesis in this study is to demonstrate that caudal block reduces the need for rescue analgesics. Our primary outcome in the study is the pain score (FLACC, Wong-Baker ), and our secondary outcomes are the need for additional analgesics (acetaminophen), the initial need for additional analgesics, the presence of intraoperative and postoperative side effects (bradycardia, tachycardia, desaturation, nausea/vomiting).
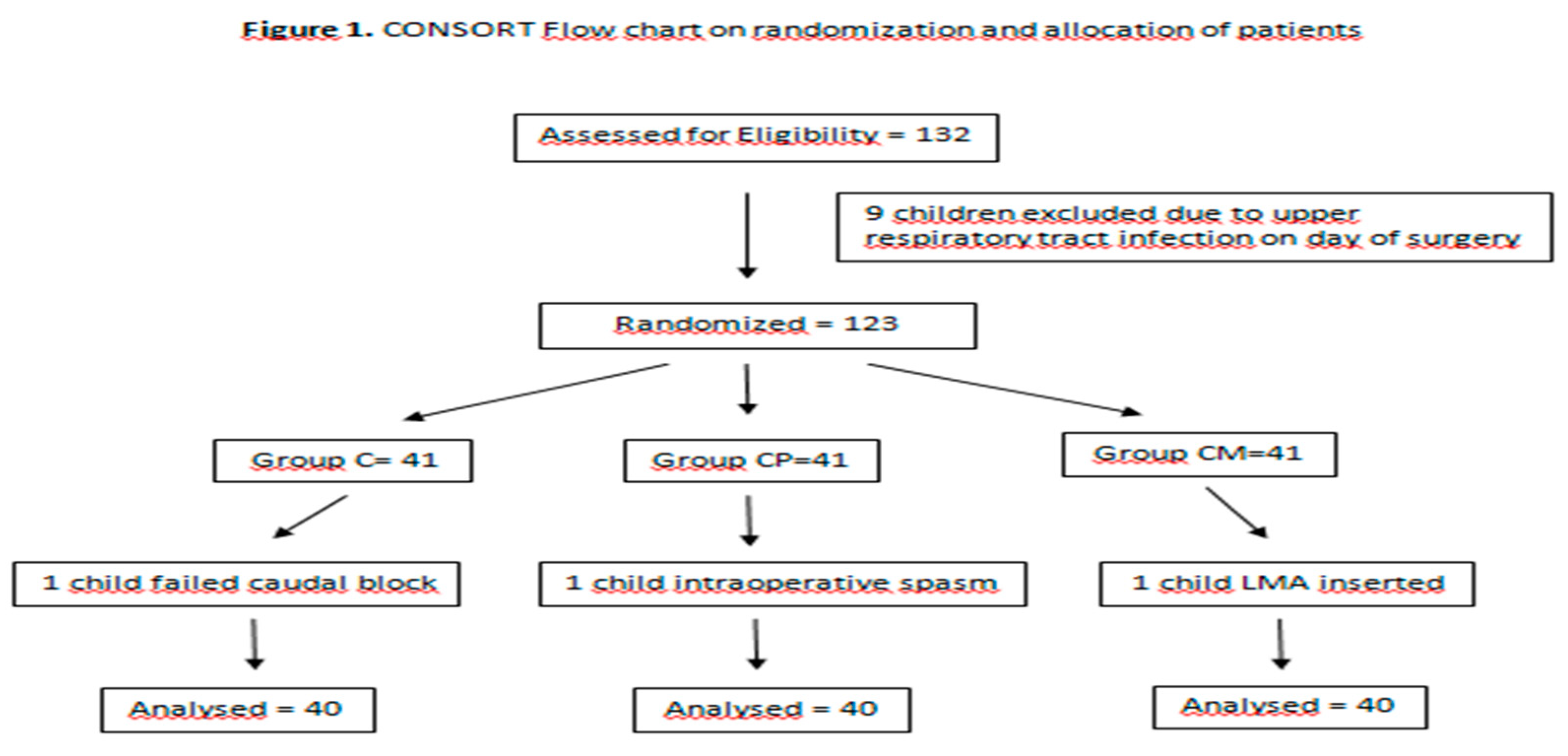
Materials and Methods: Ethical approval for our study was obtained from the Clinical Research Ethics Committee of Ordu College (Date: 04/11/2022 Decision No: 289). American Society of Anesthesiologists (ASA) I- II, 120 patients aged 1-12 years who will undergo circumcision surgery were enrolled in the study with the consent of their families. Our study was conducted between 01.12.2022 and 01.07.2023. The cases were enrolled in the annexe of Ordu College Training and Research Hospital, in the Department of Obstetrics and Pediatrics operating room. Patients without family consent, patients in whom regional anaesthesia is contraindicated, patients with local infection at the injection site, degenerative neuropathy, coagulopathy, brain tumours, increased intracranial pressure, anatomical difficulties, mental retardation, and patients with a history of allergy to local anaesthetics, chronic pain complaints, severe pulmonary, renal, and hepatic dysfunction were excluded from the study. Randomization was done by the closed envelope method, and children were divided into 3 groups (Caudal group, Caudal + i.v. paracetamol group, CP group, Caudal + i.v. meperidine group, CM). Patients and postoperative pain monitors were blinded to the study groups. Our study was designed as a prospective, randomized, single-blinded trial. Our CONSORT flow diagram is shown in
Figure 1.
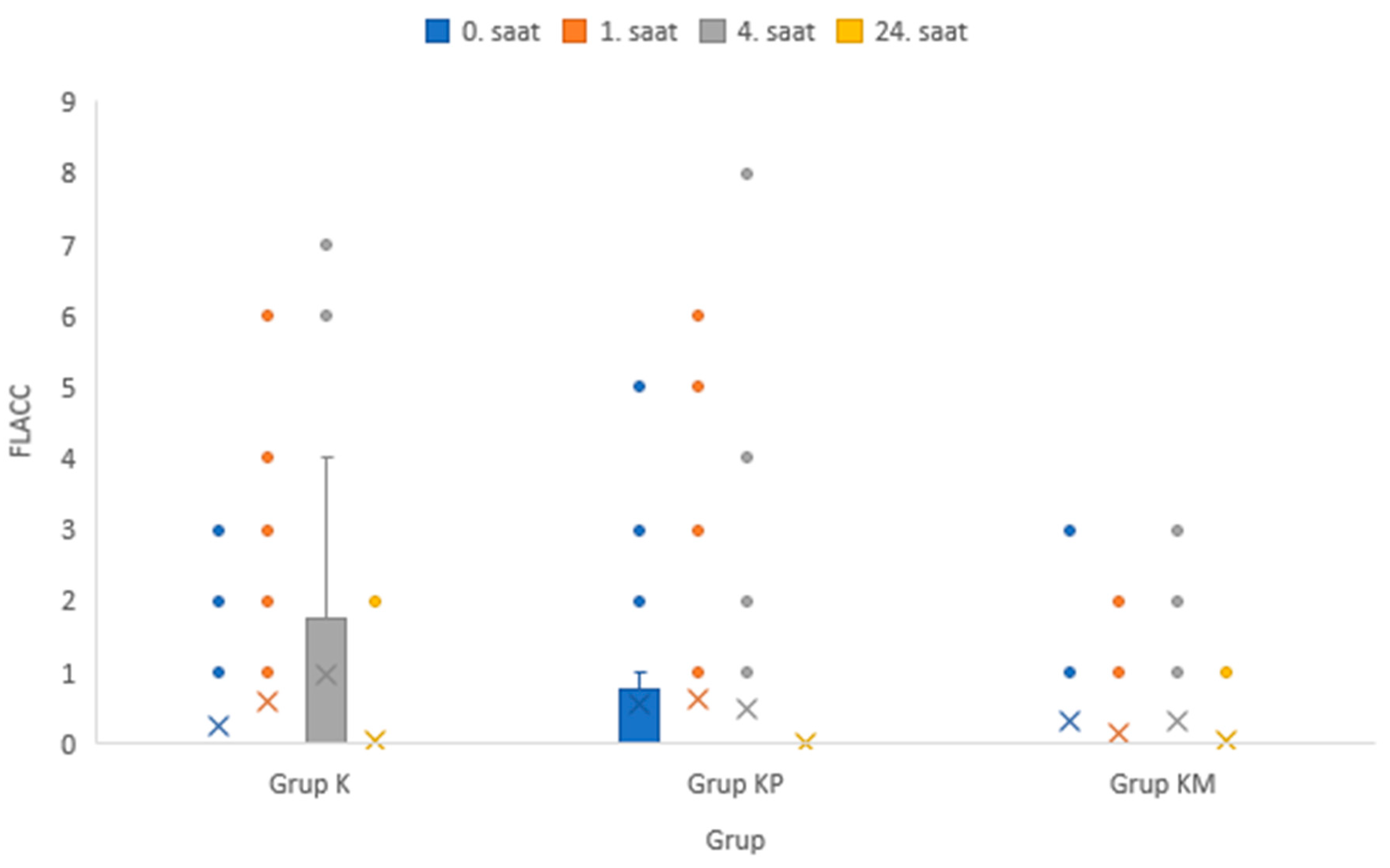
Statistical power analysis was performed based on data from similar studies. With an effect size of d=1.02 and an alpha error of 5%, the number of patients expected to provide the universe with a power of 95% was calculated to be 90. The power analysis calculation was based on the study by Şahin et al.(12), considering the parameter for the time in which the first rescue analgesic is needed. Considering that there would be patients who could not be included in the study due to the analysis or other reasons, 120 patients were included, with 40 cases in each group. The individuals who collected the data were the anesthesiologist who performed the caudal block in the operating room and the postoperative bedside visit. The anesthesiologist who collected the data in the operating room, who performed the caudal block, knew which group he belonged to. However, the researcher who collected the data during the bedside visit and the postoperative data did not know which patient group he belonged to. Whether each case had a preoperative fast of at least 6 hours was questioned. Children who were brought to the preoperative room accompanied by their parents received premedication with 0.07 mg/kg midazolam (Zolamid®, VEM İlaç, Sarıyer, Türkiye ) , 1 mcg/kg fentanyl (Talinat 0,5 mg/10 ml Vem İlaç San. ve Tic. A.Ş. Şişli, İstanbul, Türkiye). After ECG, pulse oximetry (SPO2) and noninvasive blood pressure measurement were performed on the patients brought to the operating room, and sedation was performed by mask anaesthesia with sevoflurane (Sevorane AbbVie Medical İlaçlar San. ve Tic. Ltd. Şti. Ümraniye, İstanbul, Türkiye). Anesthesia was maintained with sevoflurane and medical air. The caudal block was performed in children under mask anaesthesia. Following the patient was placed in the lateral decubitus position and the knees were pulled toward the abdomen, antisepsis was performed with povidone-iodine 10% (Isosol antiseptic solution Merkez İlaç, Çekmeköy, Istanbul, Türkiye). A linear USG probe (GE Logiq-e Nextgen model, General Electric Medical Systems, Phoenix, AZ, United States) (7-12 mHz) was placed transversely on the sacral horns, and a hyperechoic formation extending between two hypoechoic sacral horns was detected. The superficial one is the sacrococcygeal ligament, the profundal one is the dorsal bone region of the sacrum, and the caudal canal lies between these two hyperechoic transverse formations. To create a "pop" sensation, the sacrococcygeal ligament was pierced with a 35-mm 22-gage block needle (Epican Paed B-Braun Melsungen AG, Germany) between the two sacral tuberosities. After entering this area and verifying that no cerebrospinal fluid (CSF) was aspirated, 0.5 ml/kg 0.15% bupivacaine hydrochloride (Bustesin %0,5 Vem İlaç San. ve Tic. A.Ş. Şişli, İstanbul, Türkiye) was administered. The caudal block was performed in this manner in all cases. No other i.v. analgesics were administered to the cases in the Caudal group (group K). Cases in group CP received 10 mg/kg acetaminophen iv after caudal block. Cases in group CM received 1 mg/kg meperidine administered i.v. after the caudal block. Paracetamol and meperidine, which we administered intravenously, were given for the following reason: to allow the patient to spend the time until the onset of the effect of the caudal block comfortably and painlessly. After the caudal block, the patient’s spontaneous breathing returned, mask induction anaesthesia was terminated, and free oxygen was started. Vital signs were recorded at 0, 5, 10, and 15 min intraoperatively (TA, pulse, SpO2, and ETCO2) immediately after patients were placed on the operating table and immediately after monitoring. Intraoperative adverse events were tachycardia, bradycardia, desaturation, and whether or not nausea/vomiting occurred was recorded. The postoperative findings were collected at the 0th hour when he was taken to the recovery room, and the postoperative service visited him at the 1st and 4th hours. At the 24th hour, the pediatric surgeon was called to the pediatric surgical outpatient clinic, and the pediatric surgeon surveyed the pain scores and the amount of analgesics consumed. In other words, the 24th-hour data were collected by the pediatric surgeon. The FLACC pain scores and Wong-Baker pain scores were recorded 4 times. The FLACC pain scores are shown in
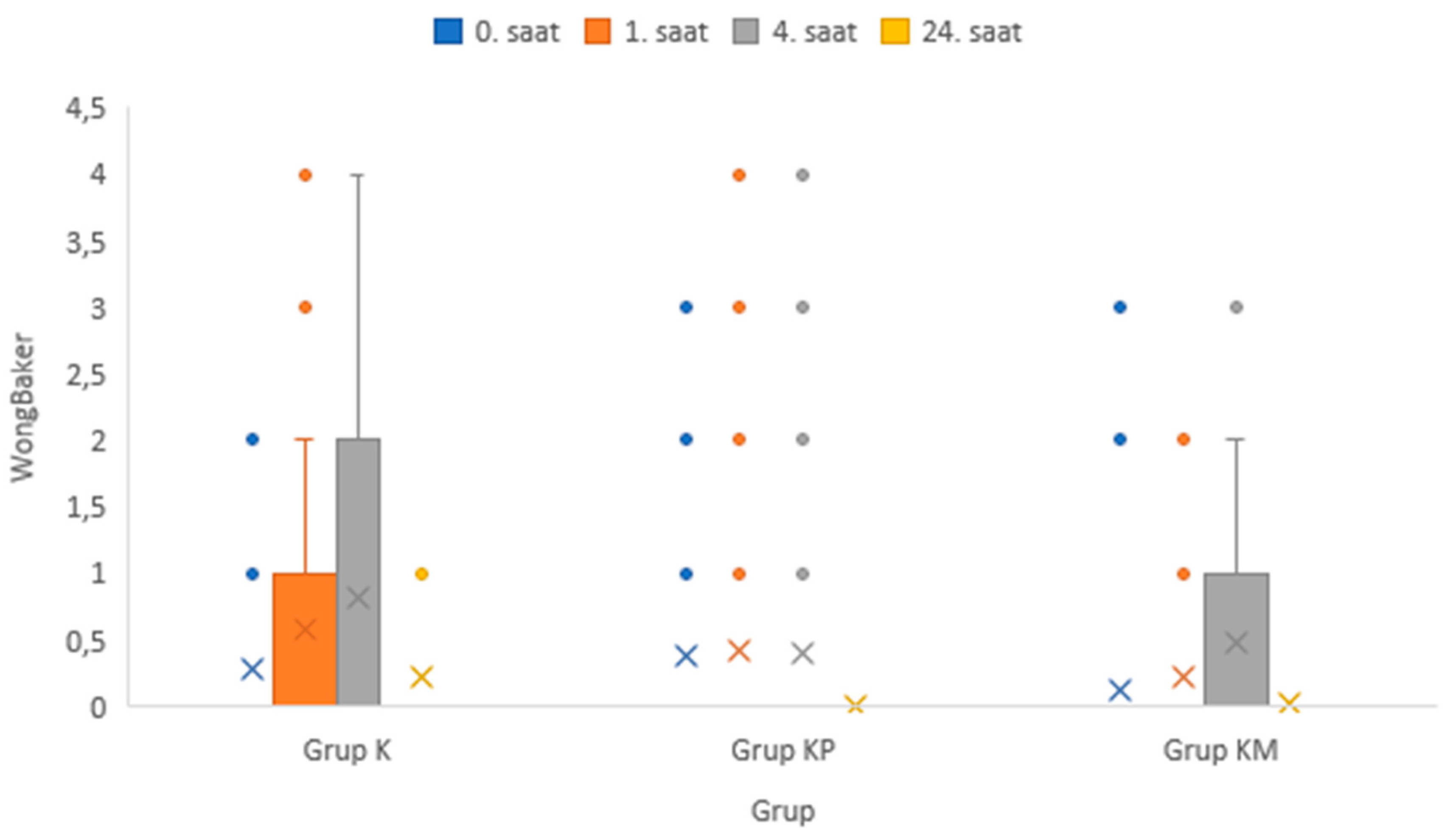
Table 1, and the Wong-Baker pain scores are shown in
Figure 2. Parents were instructed to administer 10 mg/kg acetaminophen as an oral syrup for pain. The onset of postoperative pain, the timing of the first analgesic administration, the total amount of acetaminophen administered (mg), and whether postoperative side effects (nausea/vomiting, pruritus, motor block) occurred were recorded. FLACC pain If the Wong-Baker pain score is 4 or higher, pain is assumed, and 10 mg/kg oral acetaminophen syrup is administered as an emergency analgesic.
Statistical Method
Data were analyzed using IBM SPSS v23. Agreement with normal distribution was assessed using the Shapiro-Wilk test. The chi-square test was used to compare categorical variables by group. One-way analysis of variance was used to compare normally distributed data by groups of three or more, and multiple comparisons were examined with the Duncan test. The Kruskal-Wallis test was used to compare nonnormally distributed data by groups of three or more, and multiple comparisons were examined with Dunn’s test. Results of analysis Mean ± sd for quantitative data. Categorical data as variance and median minimum–maximum) were presented as frequency (percentage). The significance level was taken as p < 0.050.
Results:
The comparison of categorical variables between groups is shown in
Table 2.
When examining whether there was a relationship between the group and postoperative pain, it was found that there was a statistically significant relationship, and the rate without postoperative pain was 72.50% in Group K, 57.50% in group KP, and 87.50% in group KM (p=0.011). The rate of postoperative pain was 27.50% in Group K, 42.50% in Group KP and 12.50% in Group KM (p=0.011). When it was investigated whether there was a correlation between the group and the presence of postoperative side effects, there was no statistically significant correlation, and the rate of absence of postoperative side effects in Group K was 90.00%. In comparison, 77.50% in Group KP and 67.50% in Group KM were determined (p=0.050). The rate of occurrence of postoperative side effects was 10.00% in Group K, 22.50% in Group KP and 32.50% in Group KM (p=0.050).
Significant results were obtained when the group analyzed weight and age variables. The results are presented in
Table 3 (p-values p=0.011 and p=0.003, respectively)
The comparison of intraoperative vital signs between groups is shown in
Table 4. Significant differences were found between the input pulse values, 5-minute pulse values, 15-minute pulse values, and input SpO2 values (p values p < 0.001, p < 0.001, p=0.011, p=0.037, respectively)
Among the time periods measured according to the groups, only the 24th hour Wong-Baker pain scores were significantly different.
(p < 0.001). There was no significant difference between the FLACC and Wong-Baker pain scores in the other periods. Our results are shown in
Table 5 and
Figure 3 and
Figure 4.
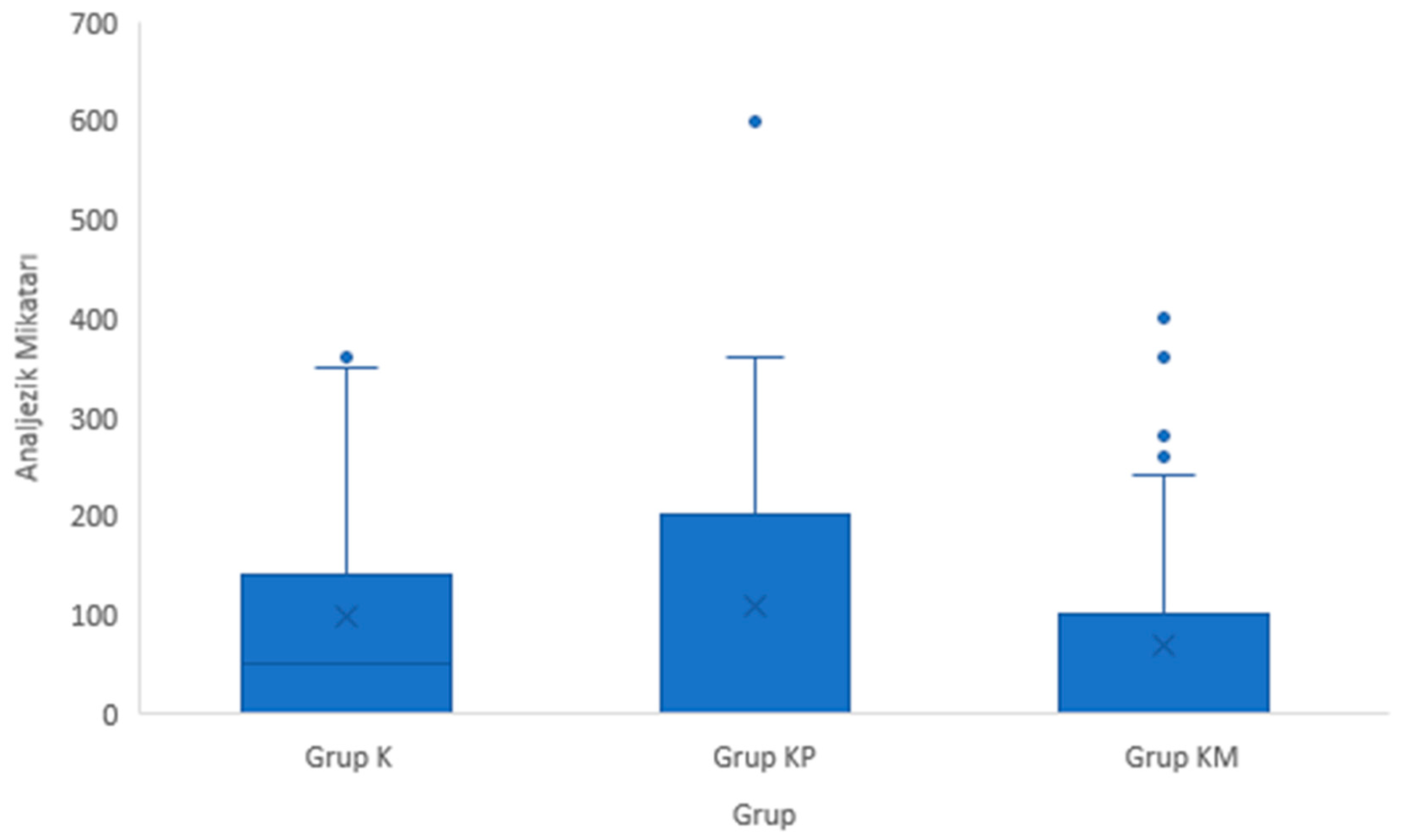
There was no difference between the postoperative hours in which analgesics were administered and the total amount of analgesics (rescue analgesic 10 mg/kg oral acetaminophen) by groups. (p=0.408, p=0.238). Our results are shown in
Table 6 and
Figure 5.
Discussion:
As a result of our study, it was found that postoperative pain was lowest in the group KM with 12.50% (p=0.011). Significant results were obtained in the weight and age variables analysis by groups (p-values p=0.011 and p=0.003, respectively). Significant differences were found between the input pulse values, 5-minute pulse values, 15-minute pulse values, and input SpO2 values (p values p < 0.001, p < 0.001, p=0.011, p=0.037, respectively). Only Wong-Baker pain scores at the 24th Wong-Baker pain scores significantly differed from the periods measured after the groups (p<0.001) .There was no significant difference between the FLACC and Wong-Baker pain scores in other periods. There was no difference between the groups regarding the time when postoperative analgesics were administered and the total amount of analgesics administered (rescue analgesic 10 mg/kg oral paracetamol) (p=0.408, p=0.238).
In a clinical prospective study by Varsha R. et al. (13), 46 children scheduled for inguinal hernia surgery were divided into 2 groups. They performed a 0.25% bupivacaine concentration, caudal block at 0.75 ml/kg volume and ilioinguinal iliohypogastric block with 0.25% bupivacaine at 0.25 ml/kg volume in 23 patients under USG guidance. They added 1 mcg/kg dexmedetomidine as an adjuvant to the block fluids in both groups. Postoperative pain scores for 24 hours were assessed using the FLACC pain scale. If the FLACC pain score was 4 or more, 1 mcg/kg i.v. fentanyl was administered as a rescue analgesic, and 10 mg/kg oral ibuprofen was administered after the 2nd postoperative hour (in 2-24 hours). The authors found that the ilioinguinal iliohypogastric group was more beneficial in blocking time. However, they found no difference in all other parameters, whether in terms of postoperative side effects, total amount of analgesic consumed, timing of first rescue analgesic administration, or duration of postoperative analgesia. They reported that ilioinguinal block was performed in a shorter time, but only at the level of statistical significance in terms of block time. Our study is not a study comparing two different blocks but a study performed within groups of caudal blocks. Nevertheless, it is similar to Varsha R. et al. (12) study in some aspects. In our study, the adjuvants administered were i.v. paracetamol and meperidine. In our study, all groups were similar regarding intraoperative/postoperative side effects, with additional adjuvants and the caudal-only group. Furthermore, our study’s total amount of analgesics consumed over 24 hours was similar. Our results partially agree with the work of Varsha R. et al.
Li et al. (7) compared caudal block concentration in adult anorectal surgery. They compared a group receiving a low volume of low-concentration ropivacaine with a group receiving a high volume of high-concentration ropivacaine. They found that the caudal block group receiving a low volume and concentration achieved similar effective analgesia to the other group, that the total amount of analgesic consumed was similar between the groups, and that a high volume and concentration provided no additional benefit. Li et al. (7) conducted a study on perineal surgery, even though it was an adult population. Our results are similar in some ways. Although our study was a pediatric population, we used bupivacaine at a low concentration (0.125%) in all 3 groups. In our case, the total amount of analgesics consumed was similar in our 3 caudal groups. Our results are in partial agreement with the work of Li et al.
Kollipara et al. (14) and Ahiskalıoglu et al. (15) compared the caudal block performed with the conventional method in pediatric infra umbilical surgery with the caudal block performed with USG. They found that the caudal block performed with USG increased initial entry success and significantly reduced the risk of multiple procedures compared with the conventional method. The authors also found that ultrasound significantly reduced the time to perform the caudal block. Although there was no difference between groups in FLACC pain scores during the measurement periods, there was a statistically significant result in favour of the group in which USG was used at the 30th minute of transition from the postanesthesia care unit to the postoperative service in the Wong-Baker pain scale. We used USG caudally in all cases, and FLACC pain scores were similar in all groups at all periods measured in our study. Similar to the study by Kollipara et al., a significant difference was found between our postoperative 24-hour Wong-Baker pain scores. Our results are partially consistent with the literature.
When we examine the literature, the number of studies grouping caudal blocks within itself is vanishingly small due to the trend toward peripheral nerve blocks in recent years. The literature compares peripheral nerve blocks and caudal blocks. For this reason, the discussion section of our article is based on the articles in the literature.
Abdullayev R. et al. (16) compared general anaesthesia with laryngeal mask anaesthesia for sumumbilical procedures in their study; they performed a caudal block using the conventional method. The authors found that caudal block significantly reduced the length of stay in the recovery room. They stated that this situation reduces recovery room costs and contributes to the country’s economy, and that caudal block is a cost-effective procedure. In our study, each patient stays in the recovery room for the same amount of time as required by hospital guidelines. Nevertheless, our study found that caudal block increased patient comfort. We observed that patients who underwent caudal block in both the recovery room and the ward had high patient comfort.
Kumar et al. (17) compared a USG-guided transversus abdominis plane (TAP) block with a conventional caudal block in pediatric inguinal hernia surgery. CHEOPS (Children’s Hospital of Eastern Ontario Pain Scale) assessed postoperative pain scores. In terms of postoperative pain scores at hours 6,7,8,12,24 and total amount of rescue analgesic consumed, the outcomes were in favor of TAP block. Pain scores were high in the caudal block, and the amount of emergency analgesics consumed was high in the caudal block group. The caudal block performed with the blind technique was behind the TAP block performed with USG. This situation can be considered a successful advantage of ultrasound. In our study, the caudal block was performed with USG in all cases. Our study observed no difference between total emergency analgesics consumed and our FLACC pain scores. The results obtained in our study might be related to the fact that we performed a caudal block with USG in all cases.
Ipek et al. (18) performed USG-gated caudal block, USG-gated quadratus lumborum block (QLB), and transversus abdominis plane block (TAP) in their clinical prospective study of pediatric patients undergoing lower abdominal surgery. The authors found that time to first pain application, total amount of analgesic consumed, and amount of fentanyl consumed intraoperatively were lower in the caudal block group. The authors assessed postoperative pain scores using the Pediatric Objective Pain Scale (POAS), different from our study. They found that the time to discharge was longer only in the caudal block group. The results of our study are in full agreement with the results of the study by Ipek et al.
Canakci et al. (19) performed a caudal block in a group of children using the conventional method of circumcision surgery. Another group was administered subcutaneous morphine (0.1 mg/kg). In the third group, the dorsal penile block was performed by urologists. Pain scores were assessed with CHEOPS at the 1st, 6th, 12th, and 24th postoperative hours. Except for the sixth hour, CHEOPS pain scores were low in the caudal block group at all measurement periods. They also found that the Ramsay sedation scale was similar in all periods in which the same measurement was performed and that intraoperative/postoperative adverse events were similar between groups. The authors stated that the caudal block performed by the conventional method can be safely used in circumcisions, and the incidence of side effects is very low. Our side effect profile is quite low. The results of our study are consistent with the literature.
Our study has some limitations. First, the cases could be categorized in terms of age group. The second limiting factor is that we evaluated pain scores only in the first 24 hours postoperatively. The third limiting factor may be that due to sociocultural habits, parents administer analgesics at home without the doctor’s recommendation for fear of "he will be in pain" even though the child is not in pain. We could not break this behaviour even though we explained it very well.
In conclusion, the caudal block can be safely used in circumcision surgery. Ultrasound guidance increases the chances of success and reduces the complication rate. Caudal block can be safely used in pediatric surgery since it does not cause serious complications, has low postoperative pain scores, and reduces the number of postoperative analgesics.
References
- Koo HP, Duckett JW. Circumcision-QuoVadis. Journal of Pediatric Surgery 1995; 9: 149-54.
- Ellis DG, Mann CM. Abnormalities of the Urethra, Penis and Scrotum. In: O?NeillJA, Rowe MI, Grosfeld JL, Fonkalsrud EW, Coran AG, (eds). Pediatric Surgery. 5th ed. United States: St Louis MosbyYear Book Inc; 1998, 1783-95.
- Macres, S. M.; Moore, P. G.; Fishman, S. M., Acute pain management. In Clinical Anesthesia: Seventh Edition, Wolters Kluwer Health: 2013.
- Wen, S. Q.; Taylor, B. J.; Lixia, Z.; Hong-Gu, H., Children’s experiences of their postoperative pain management: a qualitative systematic review. JBI Evidence Synthesis 2013, 11 (4), 1-66.
- Hurley, R. W.; Wu, C. L., Acute postoperative pain. Miller’s Anesthesia 2010, 7, 2757-87.
- Shah UJ, Karuppiah N, Karapetyan H, Martin J, Sehmbi H. Analgesic Efficacy of Adjuvant Medications in the Pediatric Caudal Block for Infraumbilical Surgery: A Network Meta-Analysis of Randomized Controlled Trials. Cureus. 2022;14(8):e28582. PMID: 36185831; PMCID: PMC9521396. [CrossRef]
- Li X, Li J, Zhang P, Deng H, Yang M, He H, Wang R. The minimum effective concentration (MEC90) of ropivacaine for ultrasound-guided caudal block in anorectal surgery. A dose finding study. PLoS One. 2021 Sep 17;16(9):e0257283. PMID: 34534232; PMCID: PMC8448308. [CrossRef]
- Brasher C, Gafsous B, Dugue S, Thiollier A, Kinderf J, Nivoche Y, Grace R, Dahmani S. Postoperative pain Management in Children and Infants: an update. Pediatr Drugs. 2014;16:129–40. [CrossRef]
- Kao S-C, Lin C-S. Caudal epidural block: an updated review of anatomy and techniques. Biomed Res Int. 2017;2017:1–5. [CrossRef]
- Faasse MA, Lindgren BW, Frainey BT, Marcus CR, Szczodry DM, Glaser AP, Suresh S, Gong EM. Perioperative effects of caudal and transversus abdominis plane (TAP) blocks for children undergoing urologic robotassisted laparoscopic surgery. J Pediatr Urol. 2015;11:121.e1–7. [CrossRef]
- Sethi N, Pant D, Dutta A, Koul A, Sood J, Chugh PT. Comparison of caudal epidural block and ultrasonography-guided transversus abdominis plane block for pain relief in children undergoing lower abdominal surgery. J Clin Anesth. 2016;33:322–9. [CrossRef]
- Sahin L, Soydinc MH, Sen E, Cavus O, Sahin M. Comparison of 3 different regional block techniques in pediatric patients. A prospective randomized single-blinded study. Saudi Med J. 2017 Sep;38(9):952-959. PMID: 28889155; PMCID: PMC5654031. [CrossRef]
- Varsha R, Desai SN, Mudakanagoudar MS, Annigeri VM. Comparison between caudal epidural and ultrasound-guided ilioinguinal-iliohypogastric block with bupivacaine and dexmedetomidine for postoperative analgesia following pediatric inguinal hernia surgeries: A prospective randomized, double-blind study. J Anaesthesiol Clin Pharmacol. 2021 Jul-Sep;37(3):389-394. Epub 2021 Oct 12. PMID: 34759549; PMCID: PMC8562458. [CrossRef]
- Kollipara N, Kodali VRK, Parameswari A. A randomized double-blinded controlled trial comparing ultrasound-guided versus conventional injection for caudal block in children undergoing infra-umbilical surgeries. J Anaesthesiol Clin Pharmacol. 2021 Apr-Jun;37(2):249-254. Epub 2021 Jul 15. PMID: 34349375; PMCID: PMC8289659. [CrossRef]
- Ahiskalioglu A, Yayik AM, Ahiskalioglu Oral E, Ekinci M, Golboyu, BE, Celik, EC et al Ultrasound-guided versus conventional injection for caudal block in children: a prospective randomized clinical study. J Clin Anesth 2018; 44 (1): 91-96. [CrossRef]
- Abdullayev R, Sabuncu U, Uludağ Ö, Selcuk Kusderci H, Oterkus M, Buyrukcan A, Duran M, Bulbul M, Apaydin HO, Aksoy N, Abes M. Caudal Anesthesia for Pediatric Subumbilical Surgery, Less Load on the Postoperative Recovery Unit. Cureus. 2019 Mar 30;11(3):e4348. PMID: 31187013; PMCID: PMC6541153. [CrossRef]
- Kumar A, Dogra N, Gupta A, Aggarwal S. Ultrasound-guided transversus abdominis plane block versus caudal block for postoperative analgesia in children undergoing inguinal hernia surgery: A comparative study. J Anaesthesiol Clin Pharmacol. 2020 Apr-Jun;36(2):172-176. Epub 2020 Jun 15. PMID: 33013030; PMCID: PMC7480308. [CrossRef]
- İpek CB, Kara D, Yılmaz S, Yeşiltaş S, Esen A, Dooply SSSL, Karaaslan K, Türköz A. Comparison of ultrasound-guided transversus abdominis plane block, quadratus lumborum block, and caudal epidural block for perioperative analgesia in pediatric lower abdominal surgery. Turk J Med Sci. 2019 Oct 24;49(5):1395-1402. PMID: 31648515; PMCID: PMC7018333. [CrossRef]
- Canakci E, Yagan O,Tas N,Mutlu T,Cirakoglu A,Benli E. Comparison of preventive analgesia techniques in circumcision cases: Dorsal penile nerve block, caudal block, or subcutaneous morphine?JPMA 2017;67(2):159-65.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).