10. Results
10.1. Addressing the Issue
The first aim of our study was to isolate the participants’ personal strategies and warning signs when it came to addressing the question of GIPV for the first time. Many participants were able to provide a go-to phrasing for their initial questioning regarding the potential presence of violence. Some of them expressed their habit of formulating their enquiry in a very direct manner, a tendency that proved to be nonspecific in regards to profession.
A: I don’t beat around the bush, I ask clear questions. Have you ever suffered physical or psychological acts of violence? Oftentimes, when I say psychological they ask me to explain what I mean by that, which is when I bring up the children if they have any, like have they ever saw anything… in any case, I make it really clear.
I: I always have if they’ve ever experienced any type of violence at any point in their life. I think I ask the question calmly, looking the patient in the eyes, I take my time.
Others reported choosing a looser approach by initially investigating the patient’s relationship, entourage and feeling of security in the wake of the upcoming childbirth.
B: Usually I start with a much broader question, I ask the patient if she has a support system to rely on during the pregnancy and after birth
D. It’s like dropping a stone into a deep well and looking for the echo, simple things such as “how are things with your partner”, getting them to open up about the relationship history which makes sense when discussing pregnancy.
In both cases, over half of the participants reported engaging in a “double strategy” where they would initially ask a direct question either focused on experienced hardships, or a broader enquiry into their living situations, then later in the consultation circling back to the potential notion of violence through pregnancy-based questions, asking about their spouse’s demeanor, support, and what the patient imagines or expects from their living situation after leaving the maternity with the newborn.
E: So I enquire about both past and present abuse. But I have a double-edged strategy, that starts with these mostly generic questions and then at some point goes into how secure the patient feels when thinking about going back home with the baby, is the father going to be supportive, if there are highs and lows, how far do the lows go…
The interview also took into account the possibility of patient reluctance or hostility towards such a question: some professionals reported a generalized trust into the patients answers, or perceivable tell-tale signs of inauthenticity:
I: Sometimes the answer lies in how people answer the question. Patients who answer yes to being victims of abuse usually take time to reflect on the question, whereas patients who say no can sometimes be a bit too quick, too abrupt, it’s like a “no” of convenience.
but patients questioning the relevance of this topic within their journey of care seemed to be more frequent. In those cases, most participants shared phrases they tend to use in order to explain or justify the pertinence of asking about IPV or opened into the potential benefits of sharing this information with a professional. In most cases, patient reassurance seemed key to the success of those consultations, and clearly expressing to the patient the dynamic of respect and service of the healthcare provider was often shared as being beneficial to the patients.
B: What I say is, “I’m asking all those questions because it’s important for me to get to know you so that I can better support you in your administrative endeavours, you don’t have to answer if you don’t want to and in no way am I trying to nag or pry, nor to make you uneasy in any way, really my purpose is to be as efficient as possible while assisting you
E “Through my eyes, it seems like you’re going through something that can have many negative consequences on your health, and I believe the best thing to do to maintain your health would be (…), but I can’t put myself in your shoes, these choices are yours to make and whenever you feel good to go, if ever, we would help you through it, but it would be your own decision.
10.2. Warning Signs
Regarding the presence of warning signs or elements of past history that stressed the importance of screening for IPV, most of the participants shared their own internal “red flags” but those appeared to be more profession-specific, i.e. linked to each person’s professional role towards the patients and what topics or symptoms are more likely to be addressed in each specific consultation.
I: Sometimes the answer lies in how people answer the question. Patients who answer yes to being victims of abuse usually take time to reflect on the question, whereas patients who say no can sometimes be a bit too quick, too abrupt, it’s like a “no” of convenience.
F: The pain in the a** patient, the one everyone calls insufferable, who’s always asking for something, in the emergency room every five minutes, with demands that don’t make sense… or the one who’s always late.
E: patient with a history of preterm labor, frequent bleeding, small babies at birth, or pregnancies that weren’t followed up on well enough or the classic late term pregnancy discovery. Patients with plenty of chronic illnesses that aren’t properly monitored, or patients labeled as “psychiatric” even though nobody was able to figure out an actual diagnosis.
It appeared that in many cases, the first warning sign was obtained not by initial patient observation, but by information sharing within a team. This allowed many participants to underline the importance of adequate information sharing within each patient’s team in order to facilitate care and spare the patient from repeated questioning on the same, potentially triggering topics.
B It’s very precious that the resident sounded the alarm as early as she did, I think she was accurate picking up on signs of vulnerability
E: sometimes workers are obligated to start over and tackle the question with a patient when they’ve already been briefed on the situation by previous colleagues, which is not that easy
10.3. Finding Support and Betterment through Teamwork
Teamwork was also reported as being essential in cases where notions of IPV had to be handled, namely because division of labor according to each caregiver’s field of expertise provided each team member with a clearer frame for their own mission regarding the patient, allowing for more personal confidence in the quality of their work as well as trust that every aspect of the question would be tackled by the best possible interlocutor in terms of helpfulness.
C I didn’t go into too much detail because the social worker had just been there and I know she had formally investigated the spousal violence aspect, all of that.
I/ I had asked around beforehand, I had gone to see the psychologist and social worker to learn about what to and not to say, so her care protocol could be as homogenous as possible and also so that we could somehow officialise what she was saying to us
The crucial importance of teamwork wasn’t limited to the necessity of adequate and timely transmissions, but was almost ubiquitously cited as a primordial resource for field-based peer learning through shared experiences.
C: we had lawyers come to the maternity ward, explaining proper protocols, giving us insight on how certain situations should be handled, so we would be more at ease
D I was lucky enough to work with highly trained midwives, who were solid pillars to stand on (…) they had also shared ways to formulate basic questions
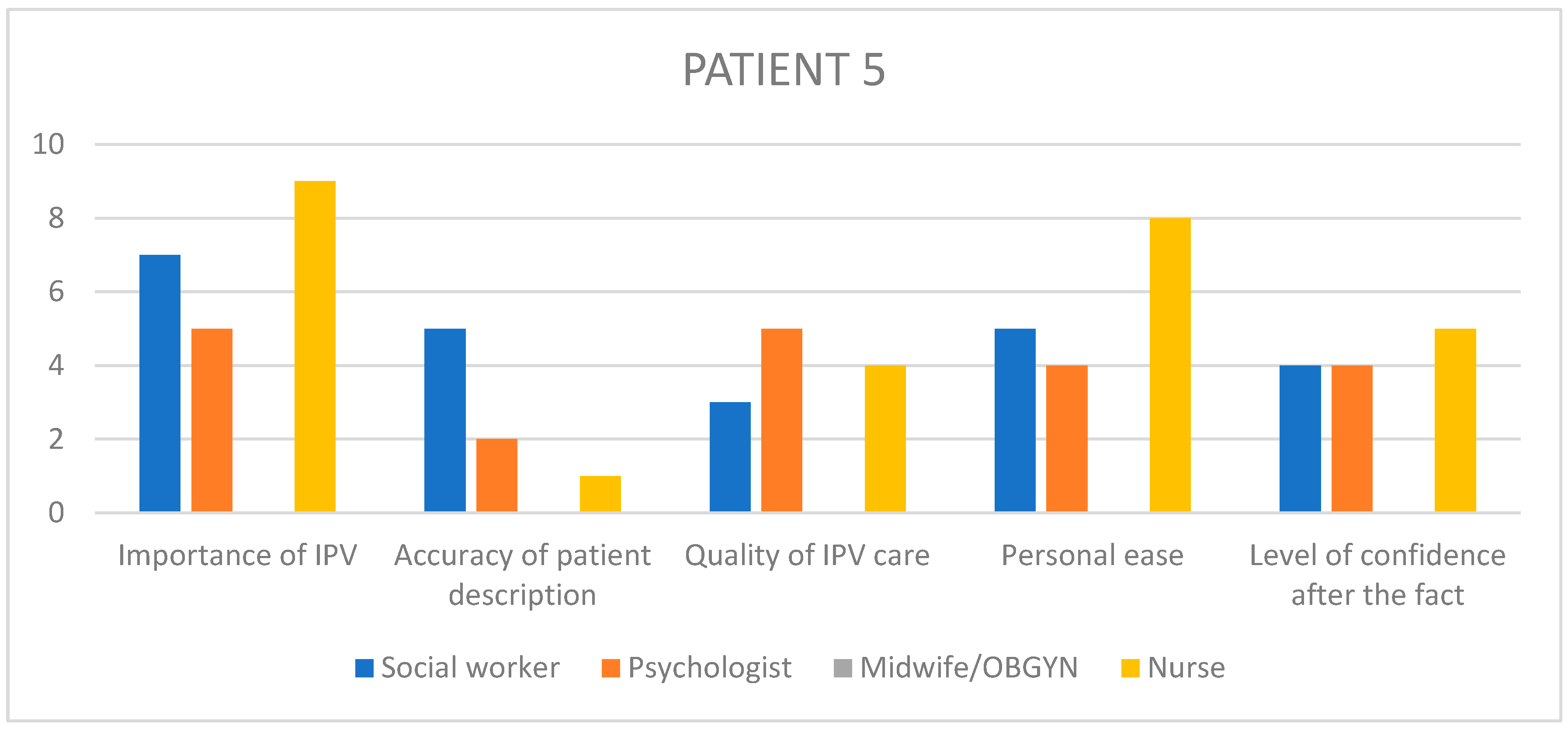
It was also cited by many as an essential support system in cases of complex, potentially overwhelming situations calling for team support or trust in systemic authority when outstanding measures of institutional involvement had to be called upon. This last notion was mostly contained in the case of patient 5, where an event of verbal violence, physical intimidation and threats from the patient’s perpetrator directed at a junior doctor came as a wave of shock throughout the entire team, and was described a posteriori as having been extremely well handled on a collective level.
G: I would always involve the social worker, they were the service designed to shed some light for us.
D: it’s not easy, when you’re so young a doctor – I think she was well supported by the entire team, and the chief really stepping up into her position of authority.
10.4. Obstacles
As well as inspiring strategies and experience based resources, several limitations were formulated by participants, on different levels. Some shared their experience of facing mental barriers of a moral nature, mostly stemming from their frustration when they felt the baby’s wellbeing was being either overlooked or mishandled.
E we’re all familiar with this but its still frustrating, feeling like we would want to go way faster than the patient does
D. It’s like I identify with the baby and beg for protection before it can.
Others implied that their own difficulties most often arose from their own emotional sensitivity, citing empathy or emotional burdening as main targets for adverse feelings coming from these situations.
I: sometimes, I don’t know why, we just forget about it. Sometimes you feel up to asking the questions, other times we sort of brush over it when we probably linger on the question for longer.
it’s a super difficult situation to deal with for a doctor. It’s hard to witness the violence people live, it’s always… well it’s empathy. Maybe it’s got to do with identifying with the patient.
F These are painful situations, so I think I have a tendency to put them aside in my head as soon as I can, because of how psychologically burdening they are.
C We all know the hardest patients situations are also the hardest to handle for professionals
Collective limitations were of three different natures. Firstly, several caregivers cited a detrimental aspect of workload division within a team, either for fear of information being lost
-
A.
I cant believe this wasn’t common knowledge amongst everyone on the case, I am shocked.
-
I.
Since I only focus on the medical side, I might have false information.
which could result in repeatedly asking the same questions to the patient if the colleagues’ reported answers were insufficient or unclear, or if opportunities for questioning were limited.
F. Sometimes there are so many people working the same case that I feel like if everyone brings up spousal violence over and over again, the patient might feel like they’re not anything more than the abuse, and that’s counter productive
and finally a negative side of a multi-professional setting was expressed by two participants, stating that when facing difficult or triggering situations, it could sometimes be tempting to do as little as possible counting on the next consultant to fill in the blanks, always relying on the rest of the team to avoid facing hard truths they felt in no position to handle.
F In the end, nobody really dove into the situation because everyone was ill at ease and thought it was not their call to make because the next person would probably tackle it better.
F They get so tricky that in the end nobody has a clue how to actually care for them.
Some of these limitations were collective in nature, but institutional in essence: several participants evoked the difficulties arising from the magnitude of the hospital structure
-
A.
This is a problem, the structure itself is so big that there are indeed connections between us, but they’re hard to find, hard to hold on to.
which contradicts another adverse tendency that was described twice in interviews which is the scarce access to interpreters in cases of language barrier, even in a level 3 maternity ward where the migrant population is a notable part of the overall patient load.
C I found there was a lot of judgemental projections on this family, and I spent the week trying to add some perspective to the mix. I thought, would it be too hard to just hold a well-intentioned attitude towards them.
C. It was like a runway of professionals one after the other, just because the interpreter was here. Midwife, then pediatrician, then social worker, and I showed up in the middle of all of that.
Lastly, one participant questioned the institutional setting of sharing information about vulnerable patients through the MPS staff, expressing their feeling that too many people were involved in these collegial meetings, most of them not having met the patient or having little to no knowledge of the case facts, but being able to partake in important decisions that didn’t always seem either relevant or practically feasible.
The other aim of our study was to shed some light onto previously unnoticed points of convergence and divergence unearthed from a variety of healthcare workers’ experiences when faced with different types of IPV. Our qualitative phenomenological analysis allowed us to isolate three main topics emerging across cases and professions.
Understanding the initial request
Taken chronologically, most patients’ first contact with maternity services happens during the prenatal period. It is during this timespan of varying length depending on term of the pregnancy, that patients are likely to be oriented for assessment by their initial point of contact (mainly medical professionals, doctors and midwives) to paramedical professionals in order to provide the most wholesome care possible (social workers, psychologists) and take the necessary steps to allow the baby to be born in the best possible settings. Along these first consultations, it is likely that patients will be asked screening questions regarding the potential history of abuse they might carry: in all five of the selected cases, and reported by 7 out of 11 professionals, a shared trait of these potential abuse victims during the first consultation is their silence.
10.5. Decrypting the Silence
The silence described can take many forms. Some participants depicted their experience of this silence as a fatalistic, implicit part of speech.
C4: it was mostly… the silences that came after anything she would share. She had a sort of… silent pout, that I interpreted a being a sign of suffering but at the same time, acceptance of a fatality that she would have to learn to live with that suffering.
E4: consultations were very long because there were moments where she would share something and right after that be all withdrawn and silent, she’d look at me saying “I shouldn’t have told you”.
F2: these patients can be in absolute mutism.
In some cases, this silence was even perceived by participants as being corporally expressed, interpreted from the patient’s overall demeanour, movements and occupation of space within the consultation space or the hospitalization rooms.
F2: She hadn’t set foot outside in a week, even when we offered she went for a breath of fresh air. She said, word for word “I’ll try and make it to the hallway”, when time came for her to leave the ward. It was a way for her to express how difficult it was for her to move forward, to go outside. But it was really physical.
C3: it was surprising, given the surgery she’d just gone through, she was on her feet really fast, she didn’t look ill at all, she just wanted out.
In the majority of these cases, this silence was associated with a perceived absence of demand on the part of the patient, in settings where participants would have expected of them to actively seek some sort of help in any regard, be it relating to the actual ongoing abuse or any other sort of assistance, from social to medical, sometimes reaching dire extremes.
H5: As time went on, she wouldn’t realize her refusal was putting the baby in danger, she couldn’t be reasoned with.
I3: After all, delaying care for so long had gravely endangered her baby’s health, as well as her own.
This perception of patient mutism or restraint is where originates another remark shared by a majority of participants over 4 of the selected patients: how well the patient really understands the role of each professional. it is a common experience for psychologists for example to have patients referred to them in relation to a specific risk factor or vulnerability trait which might not have been transparently discussed with the patient, causing them to attend their psychologist appointment with little to no idea as to why the appointment makes sense in their case. In these situations, it is easily understandable that a patient unsure of the benefit a professional might provide them would remain discreet and scarcely informative, not knowing what they may gain from sharing intimate information.
A5: From the very first consultation she alleged not seeing any interest in meeting with me.
C: Sometimes I try and flip the question around, I say “do you know what you’re seeking by coming here”.
10.6. The Balance of Benefit and Trust
Following the same logic, the interviews brought forth that providing a patient with clear, timely benefits to their current situation or quality of life drastically increases bonding between patient and caregiver and therefore allows for more truthfulness and depth of shared information.
A: and providing social security rights creates some kind of trust, it directly benefits her day to day life, and that makes for more regularity in attending consultations, and over time, that’s how you feel able to tackle some questions.
B: the administrative side of things might not seem all that interesting, but it allows us to build a very solid patient rapport and move forward from there.
These benefits can be material or logistical in nature, but in several cases have proven to be immediate in a different manner, taking root in person-to-person spontaneous proximity regardless of the healthcare setting: as depicted in the following examples, several participants noted the impact of individual affinity as a turning point for confidence and freedom of expression.
F2: you can feel it, when patients sort of latch onto you, you become somewhat of a reassuring attachment figure, it was obvious we had a special kind of bond
A5: the patient was from the Caribbean, her mother was white so it’s weird, but she and I sort of looked alike.
I: sometimes patients feel comfortable when we ask about violence because it feels nice to them that we cared enough to ask…
10.7. Inauthenticity in the Patient’s Speech: Spreading Confusion or Expressing Ambivalence
The notion of truthfulness was also mentioned several times across all patient cases, citing the likelihood of discrepancies in patient discourse according to which professional they’re talking to, in relation with the feelings of gain or proximity cited above, but sometimes seemingly in the sole objective of blurring lines and raising a verbal smokescreen between the caregiving team and the abuse that has them in its grip.
A5: discourse can be sort of empty, bland, distant, on very important subjects. (…) she could have completely different standpoints questioning the entire care she had received and I started to get worried, having this discrepancy between the real reasons why she was hospitalized and the stance she was taking in her mother’s presence.
This discrepancy is often linked to patient ambivalence regarding the perpetrator of their abuse, understanding in part even superficially the demeanour of healthcare providers, more or less subtly nudging them towards self-preservation through separation and judicializing of the ordeal, and whatever social, cultural, traditional values or emotional ties at play in keeping them in such a vulnerable position.
C4: I think there were times where she regretted having told us some things. She actually said it clearly. “Yes, he’s very nice, forget everything i said before »
B4: at first she didn’t want to live with him, then she changed her mind, and I wasn’t too keen on that, which she ended up holding against me in the end
10.8. When Keeping a Secret Reaches the Extreme
In two cases, the previously mentioned discrepancy of speech and emotional ambivalence reached their peak in increased avoidance of care to the point of terminating follow-up against medical advice, with in one case an addition of open aggressiveness directed at a doctor by the perpetrator. This trait of hostility, though not as ubiquitous across cases as the other themes, has been reported by 4 participants in a variety of different forms, cited as follows.
C3: The entire conversation was centred on the fact that she felt imprisoned in the ward, that she hated it, that she wanted out at soon as possible.
D5: she had been given a mission not to get along with me.
D5: (about the altercation between the patient’s mother and the paediatrician) I know it escalated to insults, she said “bitch”, I know the poor paediatrician was so traumatized she wasn’t sure what she had heard.
The baby’s existence in space and time.
The second main topic to emerge from our research was the added value of investigating the maternal investment of their future child in the context of GIPV.
10.9. Pregnancy and Timing
Across cases and from personal experience reported by five participants, pregnancy appears to be a very specific moment in a woman’s life when questioning the brutality of their living conditions.
B: it’s true that pregnancy all the way to childbirth is not a banal time in a woman’s life, it’s kind of a turning point – I feel like it’s all or nothing. Sometimes that’s when a woman will decide to come clean about everything, we hear that quite often, like “it’s the first time I’ve ever said anything about this”.
E: some patients place a lot of hope into their current pregnancy, therefore even right at the beginning of the pregnancy it’ll be time for them to confide, I think
It also appears that specific timings during the pregnancy allow for different levels of understanding or decisiveness regarding the mother’s experience of IPV: a few participants did not recall witnessing any differences according to the term of pregnancy, although three of them evoked the second trimester of pregnancy as the timing of choice for coming to terms with the reality of IPV and the potential internal process towards making a change.
B : these are patients where in the beginning of the pregnancy they’ll be on their guards, they’ll still be stuck, and they’re at risk of dropping out of care completely so it’s complicated. And at the end they’ll be resigned, fatalistic, vulnerable with childbirth getting closer, and that’s even more complicated. So there’s sort of a period of light in the middle of pregnancy I believe.
D: I think the baby has to be present enough in the woman’s psyche, there needs to be transparency… I think there needs to be active foetal movement, basically.
Although this term-specific opinion wasn’t shared by all participants, six of them reached a point of convergence on the subject of micro-timing when it came to a patient’s decision to share their abuse situation with a professional of any sort. Micro-timing was defined by those participants as a phenomenon of split second decision often triggered by a certain event or thought process of spontaneous, rapid occurrence.
B: sometimes I think that all you need is something happening 2 seconds before the consultation for her to decide she doesn’t want to discuss it at all. Maybe the partner will have sent a text right then and there, so it’s like all is well, do you get it ? like, it could be the right time one second, and the wrong time the next.
E: there might be moments of crisis which might get them to the point of filing a complaint, like that will be the right moment just like that. I don’t feel like there’s a specific timeframe more comfortable than another, apart from those crisis events.
D: It can be just because of that one event pushing them over the limit.
Similarly, participants shared their experience of pregnancy as being prime change-making territory for various reasons, most having to do with a newfound protective state of mind at the dawn of future maternity. This protectiveness was reported by some as being mainly directed at the baby, as an extension of maternal preoccupation.
D: (referring to sharing risk ratios for adverse events in children after gestational
IPV) with women who have a tendency to over intellectualize, it can be really helpful to share these numbers because it sort of pulls them out of their day-to-day acceptance
D5: for her baby though, if she thinks her baby might be in danger, if she’s unhappy at home or meets that one professional with whom there’s a good rapport, I think she could try and find a way out
Or in some cases, this protectiveness appeared to be primarily directed towards the patient themselves, either through a process of breaking the acceptance and submission cycle of abuse linked to a different self-perception during pregnancy, as is the case with patient 1 who fled her husband across national borders when her pregnancy was discovered. But in one case, this self-protectiveness seemed to arise mainly from the new birth stressing the unacceptable nature of potential reproductive coercion, the newborn in that case being perceived as an adverse event the mother theorizes as major enough to implement a change of any matter.
C3; her speech was pretty transparent, that she hadn’t wanted this pregnancy, that she never wanted to be pregnant again, and that she was actually relieved that the hysterectomy had happened because that meant no more pregnancies.
On the other hand, it appeared to the same number of participants that in three of the selected cases the pregnancy and projection of the upcoming maternal responsibility towards the newborn-to-be was not experienced by the patient as an impulse for change but rather a dangerous opportunity for the perpetrator to further their dynamic of overpowering and submission of the mother, under pretences of codependency and idealized family values.
C: in the patient’s discourse, it’s often linked with a notion of not wanting to deprive their child of a fatherly presence. It has to do with these idealized representations of a mum, dad, baby nuclear family. And maybe it’s also rooted in the fact that at this time, imagining themselves raising a baby alone triggers too much anxiety for them.
C3: He had completely isolated her, she lived secluded from her family and just kept having his babies.
10.10. The Baby Fadeout Phenomenon
The most prominent element when exploring the baby’s psychic representation throughout cases and interviews was, independently from the change-inducing potential of pregnancy and childbirth, the recurrence of “baby fade-out” in the patient discourse. This was mentioned in all cases by 9 out of 11 participants. Baby fade-out would be defined, in those cases, by the professional’s noticing the absence of the baby in the mother’s discourse or demeanor. This can come to the attention of professionals on a very literal standpoint, through the absence or scarcity of mentioning the baby in the mother’s discourse, be it pre- or postnatal. In one postnatal case, this was expressed through the mother never mentioning the newborn by name, giving the impression of disinterest or even rebuttal.
G5: it was something growing inside her belly. It wasn’t a being.
C3: I was startled by the interactions I witnessed in the mother-infant unit. She barely had any discourse about her baby, didn’t show any sign of concern about her, in a sort of denial of the needs of a premature baby who needed intention, a specific kind of care… she mostly called her “that one” instead of her name.
In other cases, baby fadeout was also described as the tendency not to include the baby’s wellbeing in potentially life-altering decisions on the part of the mother, even in cases where professionals explicitly recalled the importance of taking the baby into account to the mother’s attention, on different occasions and for different reasons, ranging from maternal or pediatric health concerns to more social questionings like the new dyad’s living situation.
B4: her daughter’s wellbeing... no, it came and went, wasn’t very present in her mind. Actually, we told her many times with the midwife, « come on, think of “baby’s name”
D5: Parents who don’t feel guilty when something alerts the care system is always worrisome in a way, at least in the sense of negligence which still is a form of violence albeit a relatively passive form
In most cases, neonatal pediatric assessments revealed evidence of the selected babies being premature, underweight, requiring increased stimulation to fully thrive outside the womb: even in the first instants of a child’s life, some signs of decreased vitality and withdrawal also testify to the baby’s contextual sensory response of making itself less noticeable. This was very evident in the case of patient 3, where the mother had clearly stated her disinterest in the newborn.
C3: she was a very tiny baby, who barely put on any weight, she was very sleepy. I don’t know if we can call it withdrawal at this point, but she didn’t feel very present in the moment, she wasn’t making any progress in her ability to feed etc.
10.11. Noticing Maternal Override
Following that same logic, 6 participants over the full range of selected mentioned the notable frequency of this baby fadeout being linked to maternal override or overpowering. We chose the term of maternal override as a sufficiently accurate umbrella term for all phenomena where the patient’s motherhood authority is challenged by a third party, oftentimes the perpetrator of the abuse. In those cases, mothers are found to be undermined in their capability to make decisions, or even legitimacy to do so.
I5: the grandmother doing skin to skin contact with the newborn, that’s not usual
C3: She kept referring to a higher power that had complete authority over her (…) it was like something didn’t belong to her anymore, that could be due to her husband, there was an obvious dynamic of domination. Like being depossessed of her own life.
D5: She gave birth to her mother’s baby.
Empowerment
The final metatheme to emerge from the interview analysis isn’t of the same investigative nature as the two previous one, but rather appears as an experience-based essential component of a caregiver’s course of action when taking on patients struggling with IPV, namely patient empowerment. Patient empowerment is the constant prerogative of both showing respect and thorough consideration for everything a patient shares or doesn’t, in order to restore a balance where the patient is the first decision-maker within their care system. This sentiment has been described by many participants as a way to avoid unwanted reproduction of the violence dynamic already at play in their life, where one intentionally or not, allows themselves to influence or impose their own cognitions on the patient who is already prone to submitting to another’s authority.
10.12. Cultural Awareness
The first step in this dynamic of giving back control to the patient is to provide the most secure environment for them to share their opinions in a morally neutral manner, backed up with a comprehensive attitude of cultural integration which includes the caregiver’s self-awareness that they may not always be able to understand or reflect within a patient’s specific educational or traditional value-system and in these cases, having the ability to self-analyse and withhold judgment.
A1: really, this is something frequent with African mothers, having the family’s support, welcoming the newborn as a family with the aunt, the grandmother present
E4: she said, “because now we’re a family” meaning that the traditional wedding implied a common living situation
As a prolongation of this cultural awareness, supporting endeavors of culturally inclusive caregiving within a maternity ward, allowing patients to openly share their feelings towards the care they’re provided and how it fits into their personal habits, values or belief systems, seems to be a very precious tool.
G: Sometimes during group sessions we heard mothers finally allowing themselves to say, “midwives are telling me I should bathe my baby a certain way and I don’t dare to tell them that I’ve already had four kids in my country and I always did it differently, but I’m afraid they’ll decide that I’m not capable, that I don’t do things properly just because I do things our way”.
E4: it was obvious it meant a lot to her, to her there were principles to uphold, an order to abide by.
10.13. Respecting Boundaries
Working from the outside in, once a climate of mutual respect related to cultural differences has been established, respecting the patient’s right to intimacy is an essential tenant of respectful care. This may seem like a given in most contexts, but when dealing with cases of IPV where potentially unmistakable warning signs are spotted, being able to keep oneself in check and not cross the line of what a patient feels comfortable saying is essential for maintaining patient rapport, no matter how well-intentioned one’s insistence might be thought as justified.
D: I’ll always tread lightly. These are situations where if you kind of bust in, doors close and that’s very counter productive.
F2 they’re perfectly allowed not to share anything about themselves with us
10.14. Personal Experience over Factual Evidence
In addition to respecting a patient’s decision to share or not share certain information, respecting the patient’s viewpoint on the elements they share, or the way they choose to handle them psychologically is another crucial part of respect in an empowerment mindframe.
F: if it’s a patient who’s done the work, who has no issue talking about it etc, I think we have to de-taboo the situation and collect it as we would with any other past history event
Similarly, there is some added therapeutic value to be found in the ability to prioritize a patient’s emotional experience of their current or past situation rather than the factual evidence professionals might be able to gather one way or another.
A1: my intern really wanted to see what had been cited in the complaint. I thought to myself, right now with this patient, I really didn’t need to see that. I needed the patient herself to tell me what she’d gone through, how she’s experiencing things at this moment.
C:Sometimes I realize that if I get stuck in factual facts, that can bring up a lot of resistance on the part of the patient, or in any case a sort of “cancellation” of the events. I’d say it’s better to go forward angling your questions on what the patient’s experiencing from the relationship, offering an ear to their feelings rather than asking them to unravel facts.
10.15. Giving Back Control
The final endpoint of an empowering process in the question of caring for abuse victims is to actively valorize their legitimacy in decisionmaking on different levels. The first would be to express deference and respect to past or current choices they might already have made, in order to release them of a potential sentiment of weakness, guilt or impotency that might resemble what they might be made to feel in an abusive situation.
E4: these are people who’ve always been brought down, whose choices were never taken into account, or their desires either, and it’s not our place to put them through that again.
F2: (about deciding to give the baby up for adoption) I try and remind them that the decision they took is a mother’s decision, that it’s a brave decision and that they should feel proud of themselves in their motherly role: like, being a mother doesn’t have to be the imagined scenario of giving birth and going home with a baby, sometimes it’s making tough calls in order to really protect the baby. That’s acting like a proper mother.
The other, and in most participants’ opinions’ most frequent and valuable attitude, is the respect of a patient’s use of time. That is, formulating and highlighting the fact that none of the opinions or advice given at the current time is meant to force the patient into an immediate course of action. Rather, expressing that any thought process that might have been triggered by the current care environment has all rights to carry on over all the time it needs to reach a conclusion, and reassuring the patient that whenever this conclusion is attained, the healthcare system will always be reachable and available to support and reinforce the patient in any way possible. Working at the same pace as the patient thus seems to be the best way to maintain present-time rapport during the course of the pregnancy, but also seems helpful in cementing the possibility of future change with no expiration date, a promise that the healthcare system is due to uphold.
E4: we gave her all the time and space to do whatever she wanted, we said that in any case we’d always support her no matter what choice she makes.
F2 we gave her freedom to take all the time she needed, no matter how frustrating it was for us