Submitted:
06 September 2023
Posted:
08 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Methods
2.1. Study Design and Setting
2.2. Sample Size and Participants
2.3. Study Tools
2.4. Study Variables
2.5. Ethical Consideration
2.6. Data Analysis
3. Results
3.1. Baseline Characteristics and Demographic Data
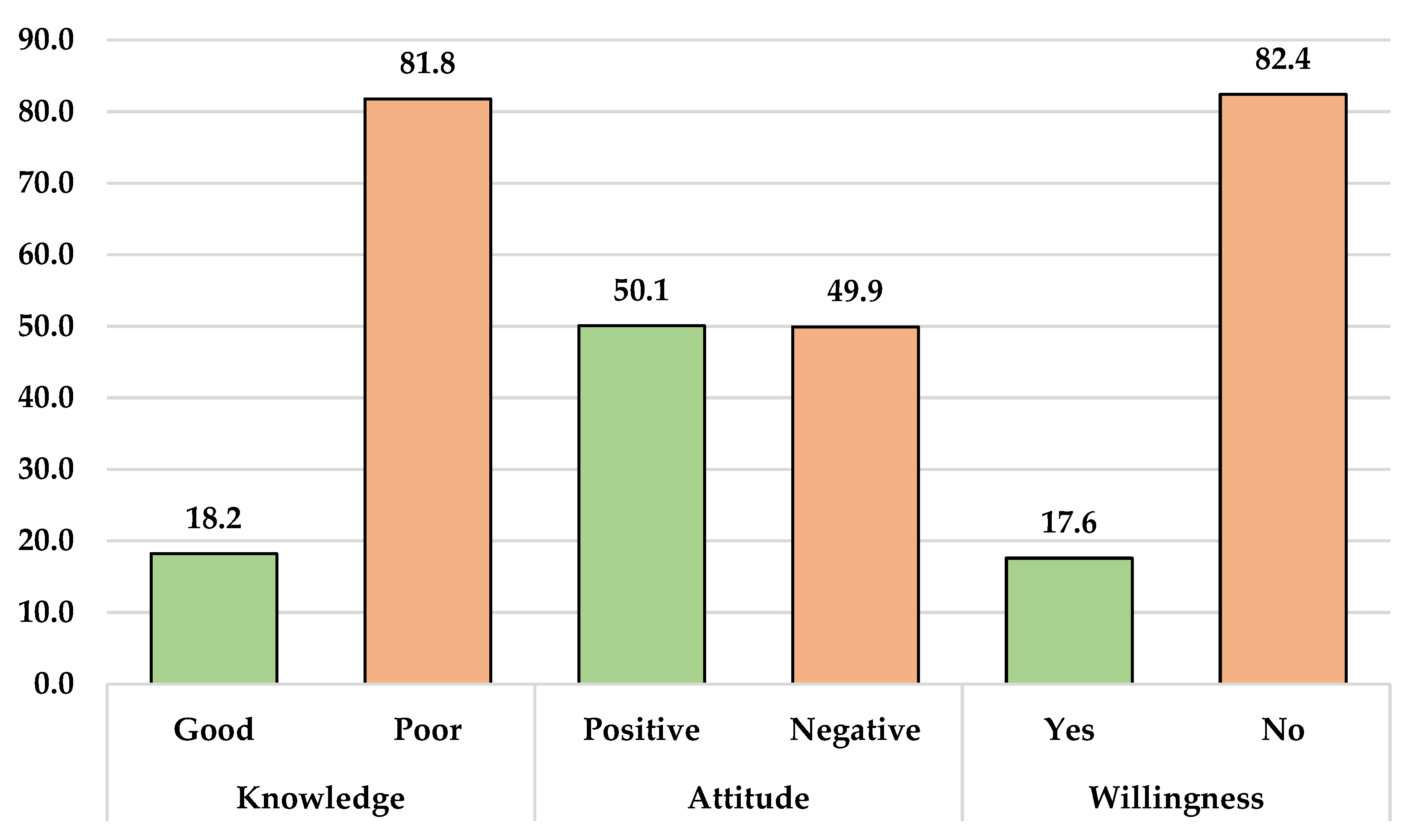
3.2. Knowledge, Attitude and Willingness to Mpox Vaccinate among HCWs
3.3. Relationships between Baseline Sociodemographic Characteristics and Knowledge, Attitude and Willingness Scores Toward Mpox
3.4. Univariate Binary Logistic Regression Analysis of Knowledge, Attitude and Willingness to Mpox Vaccination
3.5:. Multivariate Binary Logistic Regression Analysis of Knowledge, Attitude and Willingness to Mpox Vaccination
4. Discussion
5. Strengths and Limitations
6. Conclusion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Parker, S.; Buller, R.M. A Review of Experimental and Natural Infections of Animals with Monkeypox Virus between 1958 and 2012. Future Virol 2013, 8, 129–157. [CrossRef]
- Thornhill, J.P.; Barkati, S.; Walmsley, S.; Rockstroh, J.; Antinori, A.; Harrison, L.B.; Palich, R.; Nori, A.; Reeves, I.; Habibi, M.S. Monkeypox Virus Infection in Humans across 16 Countries—April–June 2022. N Engl J Med 2022, 387, 679–691. [CrossRef]
- Parker, S.; Nuara, A.; Buller, R.M.L.; Schultz, D.A. Human Monkeypox: An Emerging Zoonotic Disease. Future Microbiol 2007, 2, 17–34. [CrossRef]
- Yinka-Ogunleye, A.; Aruna, O.; Dalhat, M.; Ogoina, D.; McCollum, A.; Disu, Y.; Mamadu, I.; Akinpelu, A.; Ahmad, A.; Burga, J. Outbreak of Human Monkeypox in Nigeria in 2017–18: A Clinical and Epidemiological Report. Lancet Infect Dis 2019, 19, 872–879. [CrossRef]
- Damon, I.K.; Roth, C.E.; Chowdhary, V. Discovery of Monkeypox in Sudan. N Engl J Med 2006, 355, 962–963. [CrossRef]
- Centres for Disease Control and Prevention (CDC). Monkeypox- Past U.S. Cases and Outbreaks Available online: https:%0A//www.cdc.gov/poxvirus/monkeypox/outbreak/us-outbreaks.html (accessed on 20 January 2023).
- Damon, I.K. Status of Human Monkeypox: Clinical Disease, Epidemiology and Research. Vaccine 2011, 29, D54–D59. [CrossRef]
- Vaughan, A.; Aarons, E.; Astbury, J.; Balasegaram, S.; Beadsworth, M.; Beck, C.R.; Chand, M.; O’connor, C.; Dunning, J.; Ghebrehewet, S. Two Cases of Monkeypox Imported to the United Kingdom, September 2018. Eurosurveillance 2018, 23, 1800509. [CrossRef]
- Erez, N.; Achdout, H.; Milrot, E.; Schwartz, Y.; Wiener-Well, Y.; Paran, N.; Politi, B.; Tamir, H.; Israely, T.; Weiss, S. Diagnosis of Imported Monkeypox, Israel, 2018. Emerg Infect Dis 2019, 25, 980. [CrossRef]
- Yong, S.E.F.; Ng, O.T.; Ho, Z.J.M.; Mak, T.M.; Marimuthu, K.; Vasoo, S.; Yeo, T.W.; Ng, Y.K.; Cui, L.; Ferdous, Z. Imported Monkeypox, Singapore. Emerg Infect Dis 2020, 26, 1826. [CrossRef]
- Bunge, E.M.; Hoet, B.; Chen, L.; Lienert, F.; Weidenthaler, H.; Baer, L.R.; Steffen, R. The Changing Epidemiology of Human Monkeypox—A Potential Threat? A Systematic Review. PLoS Negl Trop Dis 2022, 16, e0010141. [CrossRef]
- Nuzzo, J.B.; Borio, L.L.; Gostin, L.O. The WHO Declaration of Monkeypox as a Global Public Health Emergency. Jama 2022, 328, 615–617. [CrossRef]
- Centres for Disease Control and Prevention (CDC). 2022 Mpox Outbreak Global Map Available online: https://www.cdc.gov/poxvirus/monkeypox/response/2022/world-map.html (accessed on 20 January 2023).
- Patel, A.; Bilinska, J.; Tam, J.C.H.; Fontoura, D.D.S.; Mason, C.Y.; Daunt, A.; Snell, L.B.; Murphy, J.; Potter, J.; Tuudah, C. Clinical Features and Novel Presentations of Human Monkeypox in a Central London Centre during the 2022 Outbreak: Descriptive Case Series. bmj 2022, 378. [CrossRef]
- Mileto, D.; Riva, A.; Cutrera, M.; Moschese, D.; Mancon, A.; Meroni, L.; Giacomelli, A.; Bestetti, G.; Rizzardini, G.; Gismondo, M.R. New Challenges in Human Monkeypox Outside Africa: A Review and Case Report from Italy. Travel Med Infect Dis 2022, 102386. [CrossRef]
- Miura, F.; van Ewijk, C.E.; Backer, J.A.; Xiridou, M.; Franz, E.; de Coul, E.O.; Brandwagt, D.; van Cleef, B.; van Rijckevorsel, G.; Swaan, C. Estimated Incubation Period for Monkeypox Cases Confirmed in the Netherlands, May 2022. Eurosurveillance 2022, 27, 2200448. [CrossRef]
- Adler, H.; Gould, S.; Hine, P.; Snell, L.B.; Wong, W.; Houlihan, C.F.; Osborne, J.C.; Rampling, T.; Beadsworth, M.B.J.; Duncan, C.J.A. Clinical Features and Management of Human Monkeypox: A Retrospective Observational Study in the UK. Lancet Infect Dis 2022, 22, P1153-1162. [CrossRef]
- Tarín-Vicente, E.J.; Alemany, A.; Agud-Dios, M.; Ubals, M.; Suñer, C.; Antón, A.; Arando, M.; Arroyo-Andrés, J.; Calderón-Lozano, L.; Casañ, C. Clinical Presentation and Virological Assessment of Confirmed Human Monkeypox Virus Cases in Spain: A Prospective Observational Cohort Study. Lancet 2022, 400, 661–669. [CrossRef]
- Girometti, N.; Byrne, R.; Bracchi, M.; Heskin, J.; McOwan, A.; Tittle, V.; Gedela, K.; Scott, C.; Patel, S.; Gohil, J. Demographic and Clinical Characteristics of Confirmed Human Monkeypox Virus Cases in Individuals Attending a Sexual Health Centre in London, UK: An Observational Analysis. Lancet Infect Dis 2022, 22, 1321–1328. [CrossRef]
- Thornhill, J.P.; Palich, R.; Ghosn, J.; Walmsley, S.; Moschese, D.; Cortes, C.P.; Galliez, R.M.; Garlin, A.B.; Nozza, S.; Mitja, O. Human Monkeypox Virus Infection in Women and Non-Binary Individuals during the 2022 Outbreaks: A Global Case Series. Lancet 2022. [CrossRef]
- Heskin, J.; Belfield, A.; Milne, C.; Brown, N.; Walters, Y.; Scott, C.; Bracchi, M.; Moore, L.S.; Mughal, N.; Rampling, T. Transmission of Monkeypox Virus through Sexual Contact-A Novel Route of Infection. J Infect 2022, 83, 334–363. [CrossRef]
- Parvin, R.; Ali, A. Monkeypox Virus: A Comprehensive Review of Taxonomy, Evolution, Epidemiology, Diagnosis, Prevention, and Control Regiments so Far. Ger. [CrossRef]
- Reynolds, M.G.; Damon, I.K. Outbreaks of Human Monkeypox after Cessation of Smallpox Vaccination. Trends Microbiol 2012, 20, 80–87. [CrossRef]
- Le Pluart, D.; Ruyer-Thompson, M.; Ferré, V.M.; Mailhe, M.; Descamps, D.; Bouscarat, F.; Lescure, F.-X.; Lucet, J.-C.; Yazdanpanah, Y.; Ghosn, J. A Healthcare-Associated Infection with Monkeypox Virus of a Healthcare Worker during the 2022 Outbreak. In Proceedings of the Open Forum Infectious Diseases; Oxford University Press US, 2022; Vol. 9, p. ofac520. [CrossRef]
- Tiecco, G.; Degli Antoni, M.; Storti, S.; Tomasoni, L.R.; Castelli, F.; Quiros-Roldan, E. Monkeypox, a Literature Review: What Is New and Where Does This Concerning Virus Come From? Viruses 2022, 14, 1894. [CrossRef]
- Sah, R.; Hada, V.; Mohanty, A.; Alshahrani, N.Z.N.; Chakraborty, S.; Bhattacharya, M.; Chakraborty, C.; Dhama, K. Recent First Report of Human-to-Dog Transmission of Monkeypox Virus Emphasizes an Urgent Need of Enhancing Surveillance and Strengthen Further Explorative Research to Reveal Its Real Magnitude of Reverse Zoonosis from Other Animals Including Pets as Like. Int J Surg 2022, 106, 106949. [CrossRef]
- Seang, S.; Burrel, S.; Todesco, E.; Leducq, V.; Monsel, G.; Le Pluart, D.; Cordevant, C.; Pourcher, V.; Palich, R. Evidence of Human-to-Dog Transmission of Monkeypox Virus. Lancet 2022, 400, 658–659. [CrossRef]
- Martínez, J.I.; Montalbán, E.G.; Bueno, S.J.; Martínez, F.M.; Juliá, A.N.; Díaz, J.S.; Marín, N.G.; Deorador, E.C.; Forte, A.N.; García, M.A. Monkeypox Outbreak Predominantly Affecting Men Who Have Sex with Men, Madrid, Spain, 26 April to 16 June 2022. Eurosurveillance 2022, 27, 2200471. [CrossRef]
- Bragazzi, N.L.; Woldegerima, W.A.; Iyaniwura, S.A.; Han, Q.; Wang, X.; Shausan, A.; Badu, K.; Okwen, P.; Prescod, C.; Westin, M.; et al. Knowing the Unknown: The Underestimation of Monkeypox Cases. Insights and Implications from an Integrative Review of the Literature. Front Microbiol 2022, 13, 1011049. [CrossRef]
- Vivancos, R.; Anderson, C.; Blomquist, P.; Balasegaram, S.; Bell, A.; Bishop, L.; Brown, C.S.; Chow, Y.; Edeghere, O.; Florence, I. Community Transmission of Monkeypox in the United Kingdom, April to May 2022. Eurosurveillance 2022, 27, 2200422. [CrossRef]
- Vusirikala, A.; Charles, H.; Balasegaram, S.; Macdonald, N.; Kumar, D.; Barker-Burnside, C.; Cumiskey, K.; Dickinson, M.; Watson, M.; Olufon, O. Epidemiology of Early Monkeypox Virus Transmission in Sexual Networks of Gay and Bisexual Men, England, 2022. Emerg Infect Dis 2022, 28, 2082–2086. [CrossRef]
- van Furth, A.M.T.; van der Kuip, M.; van Els, A.L.; Fievez, L.C.R.; van Rijckevorsel, G.G.C.; van den Ouden, A.; Jonges, M.; Welkers, M.R.A. Paediatric Monkeypox Patient with Unknown Source of Infection, the Netherlands, June 2022. Eurosurveillance 2022, 27, 2200552. [CrossRef]
- Ahmed, S.K.; Abdulqadir, S.O.; Hussein, S.H.; Omar, R.M.; Ahmed, N.A.; Essa, R.A.; Dhama, K.; Lorenzo, J.M.; Abdulla, A.Q. The Impact of Monkeypox Outbreak on Mental Health and Counteracting Strategies: A Call to Action. Int J Surg 2022, 106, 106943. [CrossRef]
- Bragazzi, N.L.; Khamisy-Farah, R.; Tsigalou, C.; Mahroum, N.; Converti, M. Attaching a Stigma to the LGBTQI+ Community Should Be Avoided during the Monkeypox Epidemic. J Med Virol 2023, 95, e27913. [CrossRef]
- Peterson, B.W.; Damon, I.K. Orthopoxviruses: Vaccinia (Smallpox Vaccine), Variola (Smallpox), Monkeypox, and Cowpox. In Mandell, Douglas, and Bennett’s principles and practice of infectious diseases. 8th ed. Philadelphia: Elsevier; 2019.
- Brown, K.; Leggat, P.A. Human Monkeypox: Current State of Knowledge and Implications for the Future. Trop Med Infect Dis 2016, 1, 8. [CrossRef]
- Ahmed, S.K.; Rashad, E.A.A.; Mohamed, M.G.; Ravi, R.K.; Essa, R.A.; Abdulqadir, S.O.; Khdir, A.A. The Global Human Monkeypox Outbreak in 2022: An Overview. Int J Surg 2022, 104, 106794. [CrossRef]
- Nath, S.D.; Majumder, K.; Rimti, F.H.; Das, J.; Tabassum, M.N.; Oishee, A.N.; Mahmood, T.; Paul, M.; Akhter, M.; Bhadra, A.B. Assessment of Knowledge on Human Monkeypox Virus among General Population in Bangladesh: A Nationwide Cross-Sectional Study. medRxiv 2022. [CrossRef]
- Vaughan, A.; Aarons, E.; Astbury, J.; Brooks, T.; Chand, M.; Flegg, P.; Hardman, A.; Harper, N.; Jarvis, R.; Mawdsley, S. Human-to-Human Transmission of Monkeypox Virus, United Kingdom, October 2018. Emerg Infect Dis 2020, 26, 782. [CrossRef]
- Gong, Q.; Wang, C.; Chuai, X.; Chiu, S. Monkeypox Virus: A Re-Emergent Threat to Humans. Virol Sin 2022, 37, 477–482. [CrossRef]
- Philpott, D. Epidemiologic and Clinical Characteristics of Monkeypox Cases—United States, May 17–July 22, 2022. MMWR Morb Mortal Wkly Rep 2022, 71, 1018–1022.
- Ly-Yang, F.; Miranda-Sánchez, A.; Burgos-Blasco, B.; Fernández-Vigo, J.I.; Gegúndez-Fernández, J.A.; Díaz-Valle, D. Conjunctivitis in an Individual with Monkeypox. JAMA Ophthalmol 2022, 140, 1022–1024. [CrossRef]
- Tan, D.H.S.; Jaeranny, S.; Li, M.; Sukhdeo, S.S.; Monge, J.C.; Callejas, M.F.; Hasso, M.; Fattouh, R.; Lalonde, S.D.; Lam, J. Atypical Clinical Presentation of Monkeypox Complicated by Myopericarditis. In Proceedings of the Open Forum Infectious Diseases; 2022; Vol. 9, p. ofac394. [CrossRef]
- Kaler, J.; Hussain, A.; Flores, G.; Kheiri, S.; Desrosiers, D. Monkeypox: A Comprehensive Review of Transmission, Pathogenesis, and Manifestation. Cureus 2022, 14. [CrossRef]
- De Sousa, D.; Frade, J.; Patrocínio, J.; Borges-Costa, J.; Filipe, P. Monkeypox Infection and Bacterial Cellulitis: A Complication to Look For. Int J Infect Dis 2022, 123, 180–182. [CrossRef]
- Milano, E.; Belati, A.; De Santis, L.; Tanese, F.; Vavallo, A.; Dachille, G.; Loconsole, D.; Bavaro, D.F.; Di Gennaro, F.; Chironna, M. First Case of Paraphimosis as a Severe Complication of Monkeypox. Vaccines 2023, 11, 63. [CrossRef]
- Billioux, B.J.; Mbaya, O.T.; Sejvar, J.; Nath, A. Potential Complications of Monkeypox. Lancet Neurol 2022, 21, 872. [CrossRef]
- Ahmed, S.K.; Dabou, E.A.; Abdelsamad, S.; Mohamed, M.G.; Chandran, D.; Chakraborty, S.; Emran, T.B.; Dhama, K. Monkeypox Virus Infection and Myocarditis: A Review of Current Evidence and Possible Pathogenesis. Narra J 2023, 3, e104. [CrossRef]
- Vouga, M.; Nielsen-Saines, K.; Dashraath, P.; Baud, D. The Monkeypox Outbreak: Risks to Children and Pregnant Women. Lancet Child Adolesc Heal 2022, 6, 751–753. [CrossRef]
- Boesecke, C.; Monin, M.B.; van Bremen, K.; Schlabe, S.; Hoffmann, C. Severe Monkeypox-Virus Infection in Undiagnosed Advanced HIV Infection. Infection 2022, 50, 1633–1634. [CrossRef]
- Menezes, Y.R.; Miranda, A.B. de Severe Disseminated Clinical Presentation of Monkeypox Virus Infection in an Immunosuppressed Patient: First Death Report in Brazil. Rev Soc Bras Med Trop 2022, 55, e0392. [CrossRef]
- Ahmed, S.K.; Mohamed, M.G.; Dabou, E.A.A.R.; Abuijlan, I.; Chandran, D.; Nahed, A.; Chopra, H.; Dhama, K. Monkeypox (Mpox) in Immunosuppressed Patients. F1000Research 2023, 12, 127. [CrossRef]
- Ogoina, D.; Iroezindu, M.; James, H.I.; Oladokun, R.; Yinka-Ogunleye, A.; Wakama, P.; Otike-Odibi, B.; Usman, L.M.; Obazee, E.; Aruna, O. Clinical Course and Outcome of Human Monkeypox in Nigeria. Clin Infect Dis 2020, 71, e210–e214. [CrossRef]
- Chakraborty, S.; Chandran, D.; Mohapatra, R.K.; Alagawany, M.; El-Shall, N.A.; Sharma, A.K.; Chakraborty, C.; Dhama, K. Clinical Management, Antiviral Drugs and Immunotherapeutics for Treating Monkeypox. An Update on Current Knowledge and Futuristic Prospects. Int J Surg 2022, 105, 106847. [CrossRef]
- De Clercq, E.; Jiang, Y.; Li, G. Therapeutic Strategies for Human Poxvirus Infections: Monkeypox (Mpox), Smallpox, Molluscipox, and Orf. Travel Med Infect Dis 2022, 52, 102528. [CrossRef]
- Ahmed, S.K.; El-Kader, R.G.A.; Abdulqadir, S.O.; Abdullah, A.J.; Nahed, A.; Chandran, D.; Dey, A.; Emran, T.B.; Dhama, K. Monkeypox Clinical Symptoms, Pathology, and Advances in Management and Treatment Options: An Update. Int J Surg 2023, 109. [CrossRef]
- Walsh, S.R.; Dolin, R. Vaccinia Viruses: Vaccines against Smallpox and Vectors against Infectious Diseases and Tumors. Expert Rev Vaccines 2011, 10, 1221–1240. [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Knowledge of Human Monkeypox Viral Infection among General Practitioners: A Cross-Sectional Study in Indonesia. Pathog Glob Health 2020, 114, 68–75. [CrossRef]
- Meo, S.A.; Al-Khlaiwi, T.; Aljofan, Z.F.; Alanazi, A.I.; Meo, A.S. Public Perceptions of the Emerging Human Monkeypox Disease and Vaccination in Riyadh, Saudi Arabia: A Cross-Sectional Study. Vaccines 2022, 10, 1534. [CrossRef]
- Ilchmann, H.; Samy, N.; Reichhardt, D.; Schmidt, D.; Powell, J.D.; Meyer, T.P.H.; Silbernagl, G.; Nichols, R.; Weidenthaler, H.; De Moerlooze, L. Single and 2-Dose Vaccinations with Modified Vaccinia Ankara-Bavarian Nordic® Induce Durable B Cell Memory Responses Comparable to Replicating Smallpox Vaccines. J Infect Dis 2022, jiac455.
- Islam, M.R.; Hossain, M.J.; Roy, A.; Hasan, A.H.M.N.; Rahman, M.A.; Shahriar, M.; Bhuiyan, M.A. Repositioning Potentials of Smallpox Vaccines and Antiviral Agents in Monkeypox Outbreak: A Rapid Review on Comparative Benefits and Risks. Heal Sci Reports 2022, 5, e798. [CrossRef]
- Russo, A.T.; Berhanu, A.; Bigger, C.B.; Prigge, J.; Silvera, P.M.; Grosenbach, D.W.; Hruby, D. Co-Administration of Tecovirimat and ACAM2000TM in Non-Human Primates: Effect of Tecovirimat Treatment on ACAM2000 Immunogenicity and Efficacy versus Lethal Monkeypox Virus Challenge. Vaccine 2020, 38, 644–654. [CrossRef]
- Harapan, H.; Wagner, A.L.; Yufika, A.; Setiawan, A.M.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P. Acceptance and Willingness to Pay for a Hypothetical Vaccine against Monkeypox Viral Infection among Frontline Physicians: A Cross-Sectional Study in Indonesia. Vaccine 2020, 38, 6800–6806. [CrossRef]
- Aljamaan, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Alhaboob, A.; Altawil, E.S.; Alshahrani, F.; Alrabiaah, A.; Alaraj, A.; Alkriadees, K. Healthcare Workers’ Worries and Monkeypox Vaccine Advocacy during the First Month of the WHO Monkeypox Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines 2022, 10, 1408. [CrossRef]
- Alshahrani, N.Z.; Alzahrani, F.; Alarifi, A.M.; Algethami, M.R.; Alhumam, M.N.; Ayied, H.A.M.; Awan, A.Z.; Almutairi, A.F.; Bamakhrama, S.A.; Almushari, B.S. Assessment of Knowledge of Monkeypox Viral Infection among the General Population in Saudi Arabia. Pathogens 2022, 11, 904. [CrossRef]
- Riad, A.; Drobov, A.; Rozmarinová, J.; Drapáčová, P.; Klugarová, J.; Dušek, L.; Pokorná, A.; Klugar, M. Monkeypox Knowledge and Vaccine Hesitancy of Czech Healthcare Workers: A Health Belief Model (HBM)-Based Study. Vaccines 2022, 10. [CrossRef]
- Zucman, D.; Fourn, E.; Touche, P.; Majerholc, C.; Vallée, A. Monkeypox Vaccine Hesitancy in French Men Having Sex with Men with PrEP or Living with HIV in France. Vaccines 2022, 10, 1629. [CrossRef]
- Gagneux-Brunon, A.; Dauby, N.; Launay, O.; Botelho-Nevers, E. Attitudes towards Monkeypox Vaccination among Healthcare Workers in France and Belgium: An Element of Complacency? J Hosp Infect 2022, 130, 144–145. [CrossRef]
- Wang, B.; Peng, X.; Li, Y.; Fu, L.; Tian, T.; Liang, B.; Sun, Y.; Chen, Y.; Wu, X.; Liu, Q. Perceptions, Precautions, and Vaccine Acceptance Related to Monkeypox in the Public in China: A Cross-Sectional Survey. J Infect Public Health 2022, 16, 163–170. [CrossRef]
- Sahin, T.K.; Erul, E.; Aksun, M.S.; Sonmezer, M.C.; Unal, S.; Akova, M. Knowledge and Attitudes of Turkish Physicians towards Human Monkeypox Disease and Related Vaccination: A Cross-Sectional Study. Vaccines 2023, 11, 19. [CrossRef]
- Ahmed, S.K.; Abdulqadir, S.O.; Omar, R.M.; Abdullah, A.J.; Rahman, H.A.; Hussein, S.H.; Mohammed Amin, H.I.; Chandran, D.; Sharma, A.K.; Dhama, K. Knowledge, Attitude and Worry in the Kurdistan Region of Iraq during the Mpox (Monkeypox) Outbreak in 2022: An Online Cross-Sectional Study. Vaccines 2023, 11, 610. [CrossRef]
- Bendezu-Quispe, G.; Benites-Meza, J.K.; Urrunaga-Pastor, D.; Herrera-Añazco, P.; Uyen-Cateriano, A.; Rodriguez-Morales, A.J.; Toro-Huamanchumo, C.J.; Hernandez, A. V; Benites-Zapata, V.A. Mass Media Use to Learn About COVID-19 and the Non-Intention to Be Vaccinated Against COVID-19 in Latin America and Caribbean Countries. Front Med 2022, 9, 877764. [CrossRef]
- Rodriguez-Morales, A.J.; Franco, O.H. Public Trust, Misinformation and COVID-19 Vaccination Willingness in Latin America and the Caribbean: Today’s Key Challenges. Lancet Reg Heal 2021, 3, 100073. [CrossRef]
- Omrani, A.S.; Shalhoub, S. Middle East Respiratory Syndrome Coronavirus (MERS-CoV): What Lessons Can We Learn? J Hosp Infect 2015, 91, 188–196. [CrossRef]
- McEachan, R.; Taylor, N.; Harrison, R.; Lawton, R.; Gardner, P.; Conner, M. Meta-Analysis of the Reasoned Action Approach (RAA) to Understanding Health Behaviors. Ann Behav Med 2016, 50, 592–612. [CrossRef]
- Sallam, M.; Dababseh, D.; Yaseen, A.; Al-Haidar, A.; Ababneh, N.A.; Bakri, F.G.; Mahafzah, A. Conspiracy Beliefs Are Associated with Lower Knowledge and Higher Anxiety Levels Regarding COVID-19 among Students at the University of Jordan. Int J Environ Res Public Health 2020, 17, 4915. [CrossRef]
- Kluge, H.; Ammon, A. Monkeypox in Europe and beyond–Tackling a Neglected Disease Together. Eurosurveillance 2022, 27, 2200482. [CrossRef]
- Bates, B.R.; Grijalva, M.J. Knowledge, Attitudes, and Practices towards Monkeypox during the 2022 Outbreak: An Online Cross-Sectional Survey among Clinicians in Ohio, USA. J Infect Public Health 2022, 15, 1459–1465. [CrossRef]
- Jairoun, A.A.; Al-Hemyari, S.S.; Abdulla, N.M.; El-Dahiyat, F.; Shahwan, M.; Hassan, N.; Alyousef, N.G.; Sharif, S.; Jaber, A.A.S. Awareness and Preparedness of Human Monkeypox Outbreak among University Student: Time to Worry or One to Ignore? J Infect Public Health 2022, 15, 1065–1071. [CrossRef]
- Lin, G.S.S.; Tan, W.W.; Chan, D.Z.K.; Ooi, K.S.; Hashim, H. Monkeypox Awareness, Knowledge, and Attitude among Undergraduate Preclinical and Clinical Students at a Malaysian Dental School: An Emerging Outbreak during the COVID-19 Era. Asian Pac J Trop Med 2022, 15, 461. [CrossRef]
- Sallam, M.; Eid, H.; Awamleh, N.; Al-Tammemi, A.B.; Barakat, M.; Athamneh, R.Y.; Hallit, S.; Harapan, H.; Mahafzah, A. Conspiratorial Attitude of the General Public in Jordan towards Emerging Virus Infections: A Cross-Sectional Study Amid the 2022 Monkeypox Outbreak. Trop Med Infect Dis 2022, 7, 411. [CrossRef]
- Temsah, M.-H.; Aljamaan, F.; Alenezi, S.; Alhasan, K.; Saddik, B.; Al-Barag, A.; Alhaboob, A.; Bahabri, N.; Alshahrani, F.; Alrabiaah, A. Monkeypox Caused Less Worry than COVID-19 among the General Population during the First Month of the WHO Monkeypox Alert: Experience from Saudi Arabia. Travel Med Infect Dis 2022, 49, 102426. [CrossRef]
- Dong, C.; Yu, Z.; Zhao, Y.; Ma, X. Knowledge and Vaccination Intention of Monkeypox in China’s General Population: A Cross-Sectional Online Survey. Travel Med Infect Dis 2022, 102533. [CrossRef]
- Gonzales-Zamora, J.; Soriano-Moreno, D.R.; Soriano-Moreno, A.N.; Ponce-Rosas, L.; Sangster-Carrasco, L.; De-Los-Rios-Pinto, A.; Benito-Vargas, R.M.; Murrieta-Ruiz, V.; Morocho-Alburqueque, N.; Caira-Chuquineyra, B. Level of Knowledge Regarding Monkeypox among Peruvian Physicians during the 2022 Outbreak: A Cross-Sectional Study. 2022. [CrossRef]
- Salim, N.A.; Septadina, I.S.; Permata, M. Knowledge, Attitude, and Perception of Anticipating 2022 Global Human Monkeypox Infection among Internal Medicine Residents at Palembang Indonesia: An Online Survey. J Kedokt dan Kesehat Publ Ilm Fak Kedokt Univ Sriwij 2022, 9, 253–262. [CrossRef]
- Al-Mustapha, A.I.; Sikiru, N.A.; Kolawole, B.; Oyewo, M.; Ahmed, H.; Odukoya, A.; Ogundijo, O.A.; Asiegbu, E.C.; Nanven, M.B.; Lawal-Atolagbe, T. A Cross-Sectional Survey of Public Knowledge of the Monkeypox Disease in Nigeria. 2022. [CrossRef]
- Ghazy, R.M.; Okeh, D.U.; Sallam, M.; Hussein, M.; Ismail, H.M.; Yazbek, S.; Mahboob, A.; Abd ElHafeez, S. Psychological Antecedents of Healthcare Workers towards Monkeypox Vaccination in Nigeria. Vaccines 2022, 10, 2151. [CrossRef]
- Sallam, M.; Al-Mahzoum, K.; Al-Tammemi, A.B.; Alkurtas, M.; Mirzaei, F.; Kareem, N.; Al-Naimat, H.; Jardaneh, L.; Al-Majali, L.; AlHadidi, A. Assessing Healthcare Workers’ Knowledge and Their Confidence in the Diagnosis and Management of Human Monkeypox: A Cross-Sectional Study in a Middle Eastern Country. In Proceedings of the Healthcare; MDPI, 2022; Vol. 10, p. 1722. [CrossRef]
- Kumar, N.; Ahmed, F.; Raza, M.S.; Rajpoot, P.L.; Rehman, W.; Khatri, S.A.; Mohammed, M.; Muhammad, S.; Ahmad, R. Monkeypox Cross-Sectional Survey of Knowledge, Attitudes, Practices, and Willingness to Vaccinate among University Students in Pakistan. Vaccines 2023, 11, 97. [CrossRef]
- Alsanafi, M.; Al-Mahzoum, K.; Sallam, M. Monkeypox Knowledge and Confidence in Diagnosis and Management with Evaluation of Emerging Virus Infection Conspiracies among Health Professionals in Kuwait. Pathogens 2022, 11, 994. [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Physicians’ Willingness to Be Vaccinated with a Smallpox Vaccine to Prevent Monkeypox Viral Infection: A Cross-Sectional Study in Indonesia. Clin Epidemiol Glob Heal 2020, 8, 1259–1263. [CrossRef]
- Harapan, H.; Setiawan, A.M.; Yufika, A.; Anwar, S.; Wahyuni, S.; Asrizal, F.W.; Sufri, M.R.; Putra, R.P.; Wijayanti, N.P.; Salwiyadi, S. Confidence in Managing Human Monkeypox Cases in Asia: A Cross-Sectional Survey among General Practitioners in Indonesia. Acta Trop 2020, 206, 105450. [CrossRef]
- Alshahrani, N.Z.; Algethami, M.R.; Alarifi, A.M.; Alzahrani, F.; Sheerah, H.A.; Abdelaal, A.; Sah, R.; Rodriguez-Morales, A.J. Knowledge and Attitude Regarding Monkeypox Virus among Physicians in Saudi Arabia, a Cross-Sectional Study. 2022. [CrossRef]
- Alshahrani, N.Z.; Mitra, S.; Alkuwaiti, A.A.; Alhumam, M.N.; Altmimi, S.M.B.; Alamri, M.H.M.; Albalawi, Z.A.S.; Almorgi, M.W.; Alharbi, H.K.D.; Alshahrani, S.M. Medical Students’ Perception Regarding the Re-Emerging Monkeypox Virus: An Institution-Based Cross-Sectional Study From Saudi Arabia. Cureus 2022, 14. [CrossRef]
- Ogoina, D.; Izibewule, J.H.; Ogunleye, A.; Ederiane, E.; Anebonam, U.; Neni, A.; Oyeyemi, A.; Etebu, E.N.; Ihekweazu, C. The 2017 Human Monkeypox Outbreak in Nigeria—Report of Outbreak Experience and Response in the Niger Delta University Teaching Hospital, Bayelsa State, Nigeria. PLoS ONE 2019, 14, e0214229. [CrossRef]
- Ibrahim, P.K.; Abdulrahman, D.S.; Ali, H.M.; Haji, R.M.; Ahmed, S.K.; Ahmed, N.A.; Abdulqadir, S.O.; Kareem, S.A.; Kamali, A.S.M.A. The 2022 Monkeypox Outbreak—Special Attention to Nurses’ Protection Should Be a Top Priority. Ann Med Surg 2022, 82, 104615. [CrossRef]
- Ahmed, S.K. Prevention, Vaccination, Management and Infection Control of Monkeypox Outbreak: An Update Global Recommendation for the Next Year 2023. J Pure Appl Microbiol 2022, 16, 3189–3191. [CrossRef]
- Ahmed, S.K.; Omar, R.M.; Hussein, S.H.; Ahmed, N.A.; Abdulqadir, S.O.; Essa, R.A.; Dhama, K.; Abdulla, A.Q. Middle East Countries Preparedness for Monkeypox Outbreak: A Call to Action. Int J Surg 2022, 106, 106948. [CrossRef]
- Al-Mandhari, A.; Kodama, C.; Abubakar, A.; Hajjeh, R.; Brennan, R. Monkeypox Outbreak and Response Efforts in the Eastern Mediterranean Region. East Mediterr Heal J 2022, 28, 465–468. [CrossRef]
- Shariq, A.; Rasheed, Z.; Al Abdulmonem, W. Human Monkeypox: An Update on Knowledge and Future Implications. Int J Health Sci (Qassim) 2022, 16, 1–2.
- Koenig, K.L.; Beÿ, C.K.; Marty, A.M. Monkeypox 2022: A Primer and Identify-Isolate-Inform (3I) Tool for Emergency Medical Services Professionals. Prehosp Disaster Med 2022, 1–6. [CrossRef]
- Health, M. of Health Indicators in the Kurdistan Region Available online: https://gov.krd/moh-en/publications/ (accessed on 20 January 2023).
- Riccò, M.; Ferraro, P.; Camisa, V.; Satta, E.; Zaniboni, A.; Ranzieri, S.; Baldassarre, A.; Zaffina, S.; Marchesi, F. When a Neglected Tropical Disease Goes Global: Knowledge, Attitudes and Practices of Italian Physicians towards Monkeypox, Preliminary Results. Trop Med Infect Dis 2022, 7, 135. [CrossRef]
- Taber, K.S. The Use of Cronbach’s Alpha When Developing and Reporting Research Instruments in Science Education. Res Sci Educ 2018, 48, 1273–1296. [CrossRef]
- Malaeb, D.; Sallam, M.; Salim, N.A.; Dabbous, M.; Younes, S.; Nasrallah, Y.; Iskandar, K.; Matta, M.; Obeid, S.; Hallit, S. Knowledge, Attitude and Conspiracy Beliefs of Healthcare Workers in Lebanon towards Monkeypox. Trop Med Infect Dis 2023, 8, 81. [CrossRef]
- Haldane, V.; De Foo, C.; Abdalla, S.M.; Jung, A.-S.; Tan, M.; Wu, S.; Chua, A.; Verma, M.; Shrestha, P.; Singh, S. Health Systems Resilience in Managing the COVID-19 Pandemic: Lessons from 28 Countries. Nat Med 2021, 27, 964–980. [CrossRef]
- Lai, C.-C.; Hsu, C.-K.; Yen, M.-Y.; Lee, P.-I.; Ko, W.-C.; Hsueh, P.-R. Monkeypox: An Emerging Global Threat during the COVID-19 Pandemic. J Microbiol Immunol Infect 2022, 55, 787–794. [CrossRef]
- Miraglia del Giudice, G.; Della Polla, G.; Folcarelli, L.; Napoli, A.; Angelillo, I.F.; Longanella, W.; Mensorio, M.M.; Cantore, F.; Group, C.W. Knowledge and Attitudes of Health Care Workers about Monkeypox Virus Infection in Southern Italy. Front Public Heal 2023, 11, 1091267. [CrossRef]
- Temsah, M.-H.; Aljamaan, F.; Alenezi, S.; Abouammoh, N.; Alhasan, K.; Dasuqi, S.A.; Alhaboob, A.; Hamad, M.A.; Halwani, R.; Alrabiaah, A. Monkeypox Disease (MPOX) Perceptions among Healthcare Workers versus General Population during the First Month of the WHO Alert: Cross-Sectional Survey in Saudi Arabia. Vaccines 2022, 10, 2071. [CrossRef]
- Ulloque-Badaracco, J.R.; Alarcón-Braga, E.A.; Hernandez-Bustamante, E.A.; Al-kassab-Córdova, A.; Benites-Zapata, V.A.; Bonilla-Aldana, D.K.; Rodriguez-Morales, A.J. Acceptance towards Monkeypox Vaccination: A Systematic Review and Meta-Analysis. Pathogens 2022, 11, 1248. [CrossRef]
- Lounis, M.; Riad, A. Monkeypox (MPOX)-Related Knowledge and Vaccination Hesitancy in Non-Endemic Countries: Concise Literature Review. Vaccines 2023, 11, 229. [CrossRef]
- Mahameed, H.; Al-Mahzoum, K.; AlRaie, L.A.; Aburumman, R.; Al-Naimat, H.; Alhiary, S.; Barakat, M.; Al-Tammemi, A.B.; Salim, N.A.; Sallam, M. Previous Vaccination History and Psychological Factors as Significant Predictors of Willingness to Receive Mpox Vaccination and a Favorable Attitude towards Compulsory Vaccination. Vaccines 2023, 11, 897. [CrossRef]
- Winters, M.; Malik, A.A.; Omer, S.B. Attitudes towards Monkeypox Vaccination and Predictors of Vaccination Intentions among the US General Public. PLoS ONE 2022, 17, e0278622. [CrossRef]
- Kumar, N.; Ahmed, F.; Raza, M.S.; Rajpoot, P.L.; Rehman, W.; Khatri, S.A.; Mohammed, M.; Muhammad, S.; Ahmad, R. Monkeypox Cross-Sectional Survey of Knowledge, Attitudes, Practices, and Willingness to Vaccinate among University Students in Pakistan. Vaccines 2022, 11, 97. [CrossRef]
- Sahin, T.K.; Erul, E.; Aksun, M.S.; Sonmezer, M.C.; Unal, S.; Akova, M. Knowledge and Attitudes of Turkish Physicians towards Human Monkeypox Disease and Related Vaccination: A Cross-Sectional Study. Vaccines 2022, 11, 19. [CrossRef]
- Neufeind, J.; Schmid-Küpke, N.; Rehfuess, E.; Betsch, C.; Wichmann, O. How a Generally Well-Accepted Measles Vaccine Mandate May Lead to Inequities and Decreased Vaccine Uptake: A Preregistered Survey Study in Germany. BMC Public Health 2022, 22, 1–14. [CrossRef]
- Bardosh, K.; De Figueiredo, A.; Gur-Arie, R.; Jamrozik, E.; Doidge, J.; Lemmens, T.; Keshavjee, S.; Graham, J.E.; Baral, S. The Unintended Consequences of COVID-19 Vaccine Policy: Why Mandates, Passports and Restrictions May Cause More Harm than Good. BMJ Glob Heal 2022, 7, e008684. [CrossRef]
| Variables | Items | Frequency | Percentage |
|---|---|---|---|
| Age | 21-30 | 401 | 63.0 |
| 31-40 | 173 | 27.2 | |
| 41+ | 63 | 9.8 | |
| Gender | Male | 318 | 49.9 |
| Female | 319 | 50.1 | |
| Marital status | Single | 314 | 49.3 |
| Married | 304 | 47.7 | |
| Widow/er | 19 | 3 | |
| Level of education | Undergraduate (diploma or BSc degree) | 616 | 96.7 |
| Postgraduate (MSc, PhD or its equivalent) | 21 | 3.3 | |
| Work experience | Less than 1 year | 168 | 26.4 |
| 1-5 years | 271 | 42.5 | |
| More than 5 years | 198 | 31.1 | |
| Occupational category | Medical technicians | 130 | 20.4 |
| Nurse | 227 | 35.6 | |
| Pharmacist | 121 | 19.0 | |
| Dentist | 65 | 10.2 | |
| Physician | 94 | 14.8 | |
| Residence area | The capital (Erbil) | 166 | 26.1 |
| Outside the capital | 471 | 73.9 | |
| Heard about human Monkeypox before 2022 | Yes | No | |
| 382 (60%) | 255 (40%) | ||
| Knowledge items | Correct answers n (%) |
Incorrect answers n (%) |
|---|---|---|
| Q1. Mpox is a new infection that appeared this year 2022. | 324 (50.9) | 313 (49.1) |
| Q2. Mpox is a viral disease infection. | 476 (74.7) | 161 (25.3) |
| Q3. Mpox is a bacterial disease infection. | 443 (69.5) | 193 (30.3) |
| Q4. Mpox is prevalent in middle eastern countries. | 283 (44.4) | 354 (55.6) |
| Q5. Mpox is prevalent in Western and Central Africa. | 334 (52.4) | 303 (47.6) |
| Q6. There are many human Mpox cases in Iraq. | 328 (51.5) | 309 (48.5) |
| Q7. Mpox is transmitted from one person to another. | 435 (68.3) | 202 (31.7) |
| Q8. Mpox is transmitted to humans through direct contact from infected animals. | 442 (69.4) | 195 (30.6) |
| Q9. Mpox is spread by droplets (coughing and sneezing). | 320 (50.2) | 317 (49.8) |
| Q10. Mpox and smallpox have similar signs and symptoms. | 176 (27.6) | 461 (72.4) |
| Q11. Mpox infection is associated with typical skin lesions. | 377 (59.2) | 260 (40.8) |
| Q12. Lymphadenopathy (swollen lymph nodes) is one clinical sign or symptom that could be used to differentiate Mpox and smallpox cases. | 275 (43.2) | 362 (56.8) |
| Q13. There is a specific vaccine for Mpox. | 195 (30.6) | 442 (69.4) |
| Q14. There is a smallpox vaccine that can be used for Mpox. | 197 (30.9) | 440 (69.1) |
| Q15. There is a specific treatment for Mpox. | 224 (35.2) | 413 (64.8) |
| Q16. Antivirals are required in the management of human Mpox patients. | 385 (60.4) | 252 (39.6) |
| Questions No. | Questions |
Agree No. (%) |
Disagree & Undecided No. (%) |
|
| Attitude toward of mpox | ||||
| A1 | I am confident that the world's population can control the Mpox worldwide | 404 (63.4) | 233 (36.6) | |
| A2 | I am interested in learning more about Mpox | 484 (76) | 153 (24.0) | |
| A3 | I think that Mpox can add new burden on healthcare system of the affected countries | 422 (66.2) | 215 (33.8) | |
| A4 | I think that mass media coverage about Mpox may have influence on its worldwide prevention | 400 (62.8) | 237 (37.2) | |
| A5 | I think that it is dangerous to travel to the countries epidemic with Mpox | 460 (72.2) | 177 (27.8) | |
| Willingness of HCWs to mpox vaccination | ||||
| W1 | I'm considering getting the smallpox vaccine to prevent Mpox viral infection | 395 (62) | 242 (38.0) | |
| W2 | The monkeypox infection has been alleviated, and there is no need to be vaccinated against Mpox infection. | 177 (27.8) | 460 (72.2) | |
| W3 | I am worried about the possible side effects of vaccination against Mpox infection | 307 (48.2) | 330 (58.1) | |
| W4 | The recommendation for the vaccination against Mpox infection by doctors, the community and other professionals has a great influence on me. | 333 (52.3) | 188 (29.5) | |
| W5 | If the country provides the vaccination against Mpox infection for free, I am willing to be vaccinated. | 327 (51.3) | 304 (47.7) |
|
Variables |
Knowledge | Attitude | Willingness | ||||||||||
| Good |
Poor |
X2 | p-value |
Positive |
Negative |
X2 | p-value |
Yes |
No |
X2 | p-value | ||
| Age (years) | 21-30 | 73 (18.2) | 328 (81.8) | 0.03 | 0.98 | 183 (45.6) | 218 (54.4) | 9.17 | 0.01 | 63 (15.7) | 338 (84.3) | 2.61 | 0.27 |
| 31-40 | 32 (18.5) | 141 (81.5) | 97 (56.1) | 76 (43.9) | 36 (20.8) | 137 (79.2) | |||||||
| 41+ | 11 (17.5) | 52 (82.5) | 39 (61.9) | 24 (38.1) | 13 (20.6) | 50 (79.4) | |||||||
| Gender | Male | 54 (16.9) | 265 (83.1) | 0.70 | 0.40 | 162 (74.0) | 157 (26.0) | 0.12 | 0.72 | 50 (15.7) | 269 (84.3) | 1.60 | 0.20 |
| Female | 62 (19.5) | 256 (80.5) | 157 (49.4) | 161 (50.6) | 62 (19.5) | 256 (80.5) | |||||||
| Marital status | Single | 55 (17.5) | 259 (82.5) | 2.71 | 0.25 | 128 (40.8) | 186 (59.2) | 21.6 | <0.01 | 57 (18.2) | 257 (81.8) | 0.16 | 0.92 |
| Married | 60 (19.7) | 244 (80.3) | 179 (58.9) | 125 (41.1) | 52 (17.1) | 252 (82.9) | |||||||
| Widow\er | 1 (5.3) | 18 (94.7) | 12 (63.2) | 7 (36.8) | 3 (15.8) | 16 (84.2) | |||||||
| Level of education | Under graduated | 115 (18.7) | 501 (81.3) | 2.63 | 0.10 | 308 (50.0) | 308 (50.0) | 0.04 | 0.83 | 109 (17.7) | 507 (82.3) | 0.16 | 0.68 |
| Graduated | 1 (4.8) | 20 (95.2) | 11 (52.4) | 10 (47.6) | 3 (14.3) | 18 (85.7) | |||||||
| Duration of practice | Less than 1 year | 31 (18.5) | 137 (81.5) | 1.54 | 0.46 | 52 (31.0) | 116 (69.0) | 37.0 | <0.01 | 31 (18.5) | 137 (81.5) | 0.31 | 0.85 |
| 1-5 years | 44 (16.2) | 227 (83.8) | 144 (53.1) | 127 (46.9) | 45 (16.6) | 226 (83.4) | |||||||
| More than 5 years | 41 (20.7) | 157 (79.3) | 123 (62.1) | 75 (37.9) | 36 (18.2) | 162 (81.8) | |||||||
| Occupation | Medical technician | 18 (13.8) | 112 (86.2) | 5.77 | 0.21 | 57 (43.8) | 73 (56.2) | 3.48 | 0.48 | 14 (10.8) | 116 (89.2) | 7.63 | 0.10 |
| Nurse | 44 (19.4) | 183 (80.6) | 120 (52.9) | 107 (47.1) | 42 (18.5) | 185 (81.5) | |||||||
| Pharmacist | 29 (24.0) | 92 (76.0) | 59 (48.8) | 62 (51.2) | 22 (18.2) | 99 (81.8) | |||||||
| Dentist | 12 (18.5) | 53 (81.5) | 32 (49.2) | 33 (50.8) | 17 (26.2) | 48 (73.8) | |||||||
| Physician | 13 (13.8) | 81 (86.2) | 51 (54.3) | 43 (45.7) | 17 (18.1) | 77 (81.9) | |||||||
| Place of residence | Outside the capital | 91 (19.3) | 380 (80.7) | 1.49 | 0.21 | 224 (47.6) | 247 (52.4) | 4.59 | 0.03 | 86 (18.3) | 385 (81.7) | 0.57 | 0.45 |
| The Capital (Erbil) | 25 (15.1) | 141 (84.9) | 95 (57.2) | 71 (42.8) | 26 (15.7) | 140 (84.3) | |||||||
| Heard about human Monkeypox before 2022 | Yes | 98 (25.7) | 284 (74.3) | 35.5 | <0.01 | 196 (51.3) | 186 (48.7) | 0.57 | 0.44 | 65 (17.0) | 317 (83.0) | 0.21 | 0.64 |
| No | 18 (7.1) | 237 (92.9) | 123 (48.2) | 132 (51.8) | 47 (18.4) | 208 (81.6) | |||||||
|
Items |
Knowledge | Attitude | Willingness | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| OR | 95% CI | P | OR | 95% CI | P | OR | 95% CI | P | ||||
| Age (41+ as ref.) | ||||||||||||
| 21-30 years | 1.05 | 0.52 | 2.11 | 0.887 | 0.51 | 0.29 | 0.89 | 0.018 | 0.71 | 0.36 | 1.39 | 0.328 |
| 31-40 years | 1.07 | 0.50 | 2.28 | 0.855 | 0.78 | 0.43 | 1.41 | 0.423 | 1.01 | 0.49 | 2.06 | 0.977 |
| Gender (Female as ref.) | ||||||||||||
| Male | 0.84 | 0.56 | 1.25 | 0.401 | 1.05 | 0.77 | 1.44 | 0.721 | 0.76 | 0.50 | 1.15 | 0.206 |
| Marital status (Widow\er as ref.) | ||||||||||||
| Single | 3.82 | 0.50 | 29.23 | 0.196 | 0.40 | 0.15 | 1.04 | 0.062 | 1.18 | 0.33 | 4.19 | 0.795 |
| Married | 4.42 | 0.57 | 33.81 | 0.152 | 0.83 | 0.32 | 2.18 | 0.713 | 1.10 | 0.30 | 3.91 | 0.882 |
| Educational level (Post graduate as ref.) | ||||||||||||
| Undergraduate | 0.21 | 0.02 | 1.64 | 0.139 | 0.90 | 0.38 | 2.17 | 0.830 | 1.29 | 0.37 | 4.45 | 0.687 |
| Duration of practice (More than 5 years as ref.) | ||||||||||||
| Less than 1 year | 0.86 | 0.51 | 1.45 | 0.589 | 0.27 | 0.17 | 0.42 | < 0.01 | 1.01 | 0.59 | 1.73 | 0.947 |
| Between 1-5 years | 0.74 | 0.46 | 1.18 | 0.215 | 0.69 | 0.47 | 1.00 | 0.053 | 0.89 | 0.55 | 1.45 | 0.656 |
| Occupation (Physician as ref.) | ||||||||||||
| Medical technical | 1.00 | 0.46 | 2.16 | 0.997 | 0.65 | 0.38 | 1.12 | 0.125 | 0.54 | 0.25 | 1.17 | 0.121 |
| Nurse | 1.49 | 0.76 | 2.93 | 0.238 | 0.94 | 0.58 | 1.53 | 0.820 | 1.02 | 0.55 | 1.91 | 0.930 |
| Pharmacist | 1.96 | 0.95 | 4.03 | 0.066 | 0.80 | 0.46 | 1.37 | 0.424 | 1.00 | 0.50 | 2.02 | 0.985 |
| Dentist | 1.41 | 0.59 | 3.32 | 0.432 | 0.81 | 0.43 | 1.54 | 0.533 | 1.60 | 0.74 | 3.44 | 0.225 |
| Residence (The Capital “Erbil” as ref.) | ||||||||||||
| Outside the capital | 1.35 | 0.83 | 2.18 | 0.223 | 0.67 | 0.47 | 0.96 | 0.033 | 1.20 | 0.74 | 1.94 | 0.450 |
| Heard about mpox before 2022 (No as ref.) | ||||||||||||
| Yes | 4.54 | 2.67 | 7.73 | < 0.01 | 1.13 | 0.82 | 1.55 | 0.447 | 0.90 | 0.60 | 1.37 | 0.64 |
|
Items |
Knowledge | Attitude | Willingness | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| AOR | 95% CI | P | AOR | 95% CI | P | AOR | 95% CI | P | ||||
| Age (41+ as ref.) | ||||||||||||
| 21-30 years | - | - | - | - | 0.95 | 0.51 | 1.77 | 0.887 | - | - | - | - |
| 31-40 years | - | - | - | - | 0.91 | 0.49 | 1.68 | 0.778 | - | - | - | - |
| Gender (Female as ref.) | ||||||||||||
| Male | - | - | - | - | - | - | - | - | 0.78 | 0.51 | 1.20 | 0.268 |
| Marital status (Widow\er as ref.) | ||||||||||||
| Single | 2.99 | 0.37 | 23.90 | 0.302 | 0.48 | 0.17 | 1.32 | 0.158 | - | - | - | - |
| Married | 3.42 | 0.42 | 27.37 | 0.246 | 0.70 | 0.26 | 1.88 | 0.481 | - | - | - | - |
| Educational level (Post graduate as ref.) | ||||||||||||
| Undergraduate | 4.45 | 0.56 | 35.15 | 0.156 | - | - | - | - | - | - | - | - |
| Duration of practice (More than 5 years as ref.) | ||||||||||||
| Less than 1 year | 0.95 | 0.50 | 1.79 | 0.875 | 0.35 | 0.20 | 0.59 | < 0.01 | - | - | - | - |
| Between 1-5 years | 0.75 | 0.44 | 1.28 | 0.299 | 0.79 | 0.51 | 1.22 | 0.294 | - | - | - | - |
| Occupation (Physician as ref.) | ||||||||||||
| Medical technical | 1.19 | 0.53 | 2.68 | 0.664 | 0.74 | 0.42 | 1.31 | 0.314 | 0.56 | 0.26 | 1.20 | 0.139 |
| Nurse | 1.82 | 0.89 | 3.72 | 0.099 | 1.07 | 0.64 | 1.79 | 0.787 | 1.03 | 0.55 | 1.93 | 0.916 |
| Pharmacist | 1.81 | 0.85 | 3.86 | 0.122 | 0.83 | 0.47 | 1.46 | 0.529 | 0.96 | 0.47 | 1.94 | 0.918 |
| Dentist | 1.51 | 0.62 | 3.70 | 0.360 | 0.83 | 0.42 | 1.61 | 0.586 | 1.62 | 0.75 | 3.47 | 0.215 |
| Residence (The Capital “Erbil” as ref.) | ||||||||||||
| Outside the capital | 1.38 | 0.82 | 2.31 | 0.215 | 0.81 | 0.55 | 1.19 | 0.294 | - | - | - | - |
| Heard about mpox before 2022 (No as ref.) | ||||||||||||
| Yes | 4.85 | 2.81 | 8.36 | <0.001 | - | - | - | - | - | - | - | - |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).





