1. Introduction
Verrucous carcinoma (VC) is an uncommon subtype of low-grade, well-differentiated squamous cell carcinoma (SCC) that develops mostly in the skin, genitalia, esophagus, and oral cavity. Oral verrucous carcinoma (OVC) accounts for 2–12% of all oral cavity carcinomas and mostly affects the buccal mucosa, followed by the hard palate, the floor of the mouth, and the gingiva [
1,
2,
3,
4].
Clinically, OVC appears as a painless, white-grey, warty, exophytic mass that resembles cauliflower [
5]. It presents a strong predisposition for local invasion and a low predisposition for diffusion in neighboring structures, which varies depending on the lesion size and the evolution period. Metastasis from OVC is uncommon [
3,
6,
7].
Histologically, OVC exhibits a well-differentiated squamous proliferation with a papillary or verrucous epithelial surface and clear hyperkeratosis, invading the subjacent stroma with well-defined, pushing margins. Minor cellular atypical is usually seen [
8].
This report describes a case of VC of the hard palate in a 75-year-old female patient.
2. Case Presentation
A 75-year-old female was referred to our Department of Oral Medicine and Maxillofacial Radiology for evaluation of a lesion on the left side of the palate dating back more than a year. Her medical record revealed controlled diabetes with no other specific health conditions; she didn’t report taking any systemic medications. She has had a history of smoking a minimum of 10 cigarettes per day for at least 40 years. Her physical examination disclosed no extra-oral abnormalities.
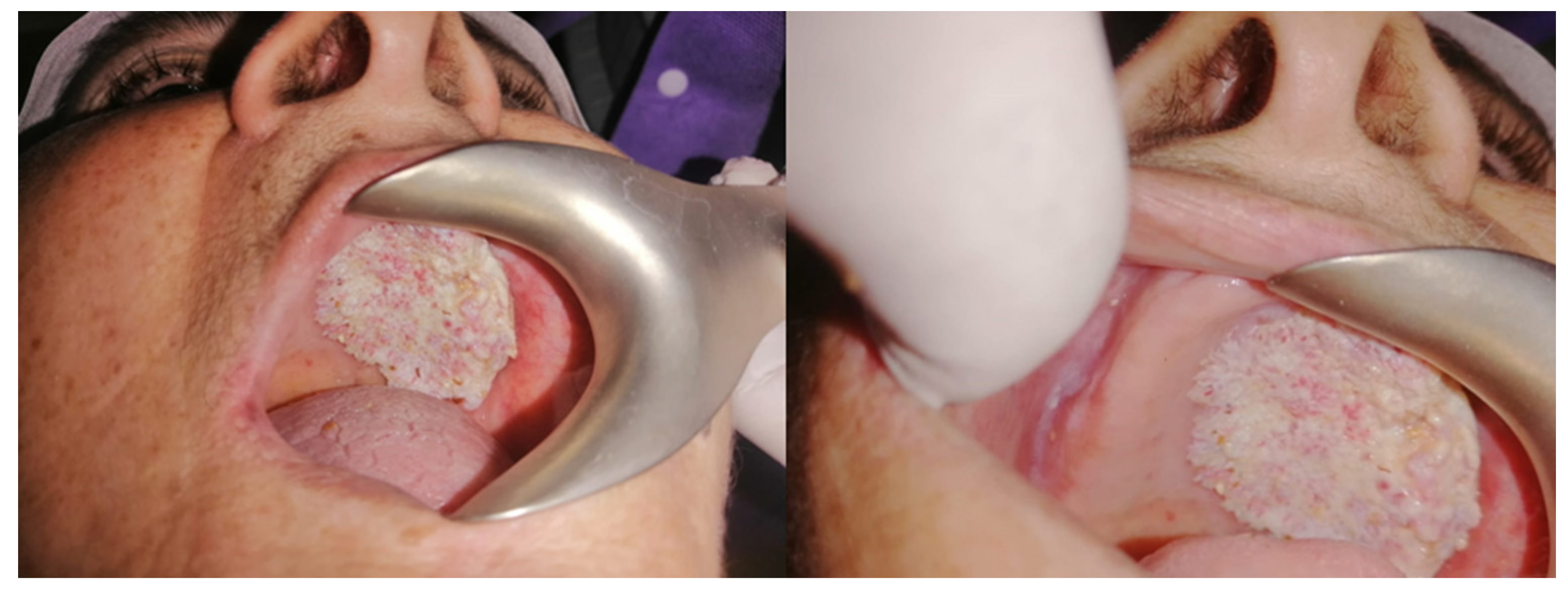
Intraorally, the patient presented a painless verrucous exophytic white lesion that covered the whole left maxillary alveolar ridge and reached the palate beyond the midline (
Figure 1).
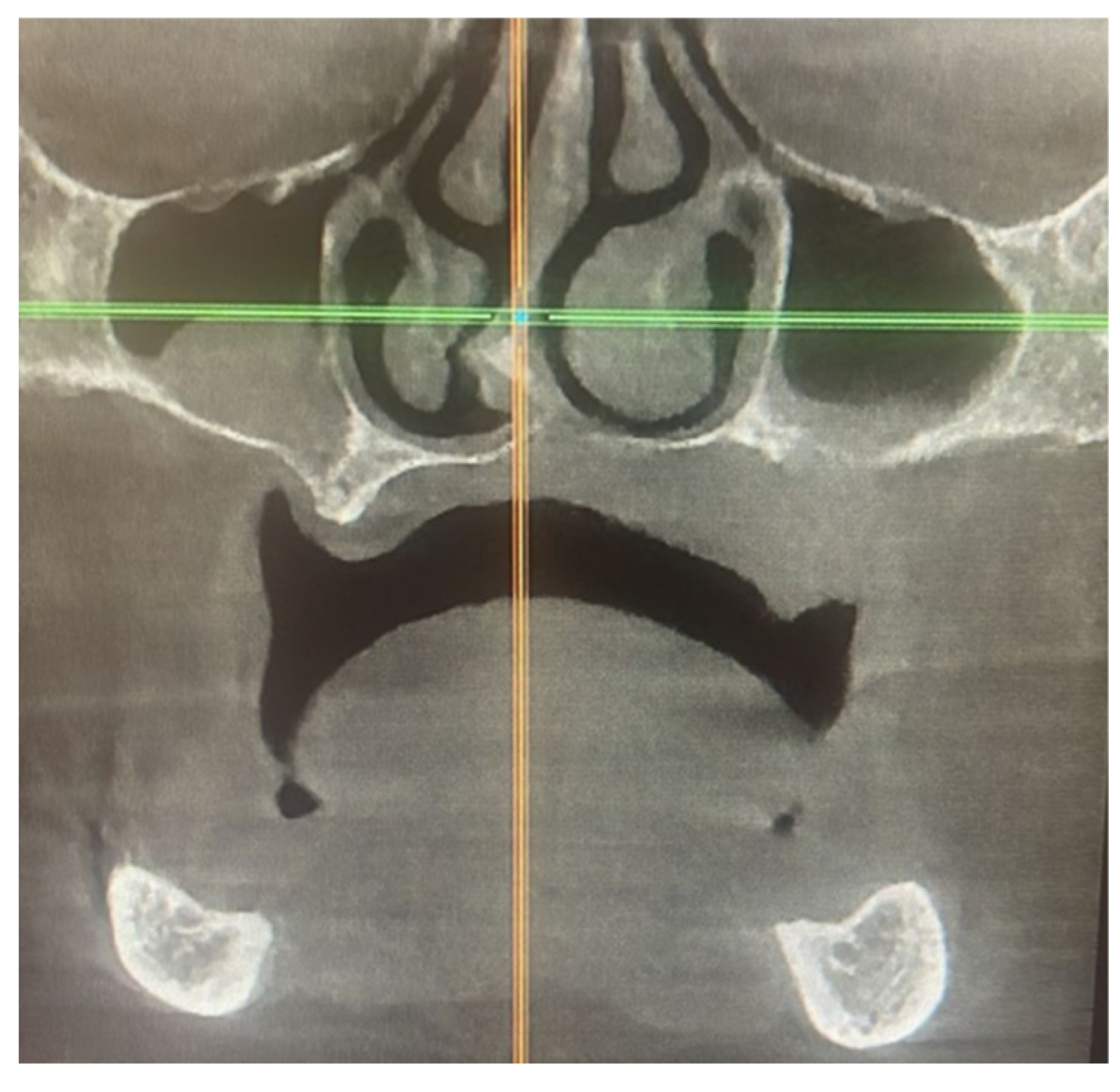
The computed tomography (CT) scan of the facial bones, with a focus on the hard palate, showed an increase in the left palatal mucosa thickness, cortical irregularity, and osteolysis of the inferior border of the maxillary sinus (
Figure 2).
An incisional biopsy was performed under local anesthesia and sent for histological assessment.
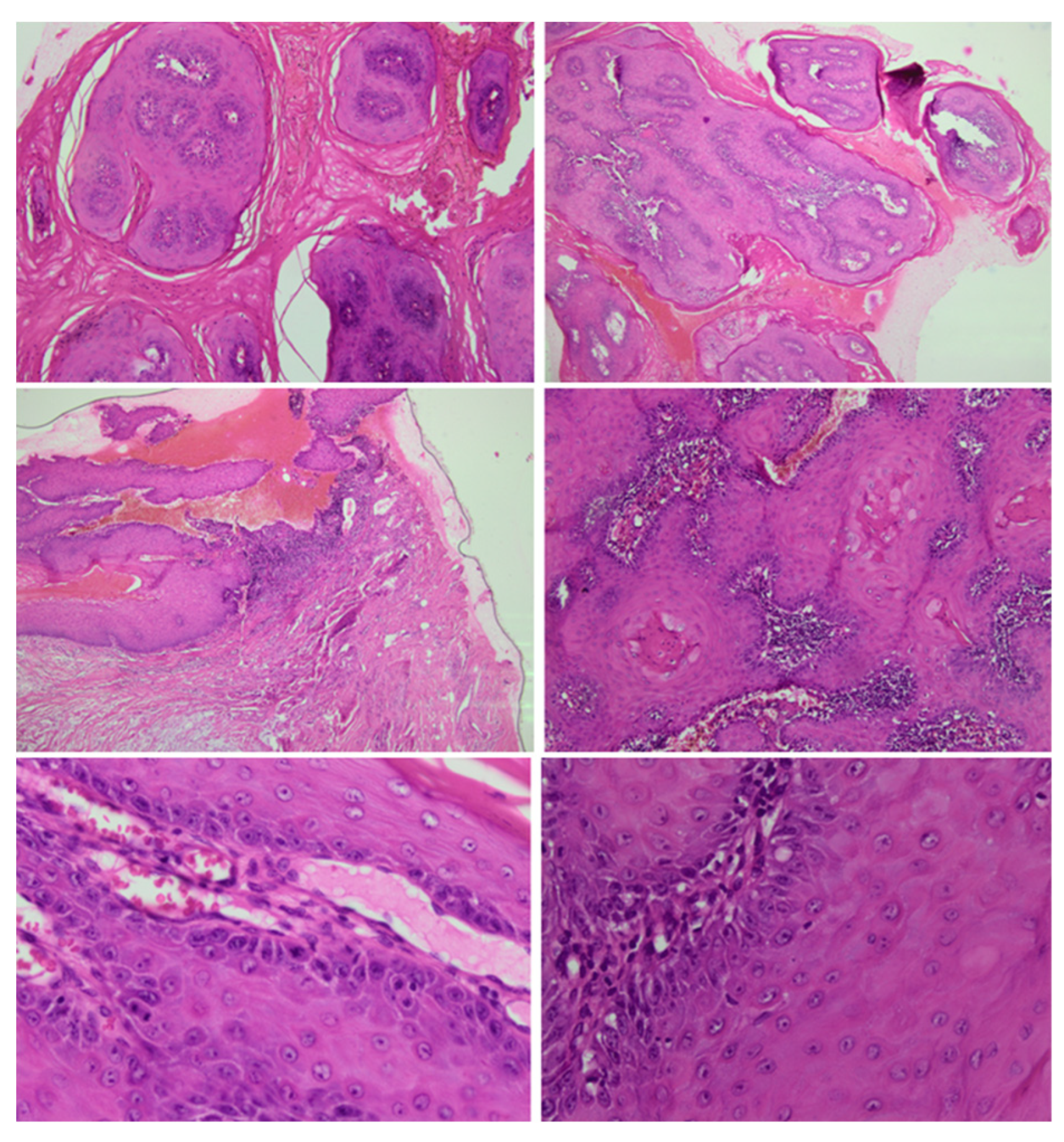
The anatomopathological examination showed papillary tumor proliferation covered by an acanthotic and keratinized stratified squamous epithelium. The interpapillary buds are enlarged and grow in depth. Minimal cellular atypia and lymphocyte infiltration were noted (
Figure 3).
These findings support the diagnosis of an OVC.
The patient was referred to an oncologist, and a whole-body evaluation was performed using positron emission tomography (PET) scans after intravenous injection of 6.8 mCi of 18F-FDG and a high-resolution CT scan with an appropriate PET scanner. Diffuse hypermetabolic thickening at the left maxillary aspect with no evidence of active distant metastasis was detected.
An MRI-1.5T examination showed an expansile lesion of the hard palate on the left side measuring 3.7x3.6x1cm and extending to the bony floor of the left maxillary sinus. The lesion had intermediate signal intensity and showed enhancement after intravenous gadolinium administration. No neck lymphadenopathy or evidence of extension into the sinus or the nasal cavity was noticed.
These investigations confirmed the VC of the hard palate.
Considering the patient’s age and the lesion’s size, treatment by radiotherapy and chemotherapy will be adopted rather a surgical one.
3. Discussion
OVC is a rare tumor affecting the oral cavity; it is more frequent in patients between 40 and 60 years old with a male preponderance [
2,
9,
10]. The etiology of OVC is unknown; however, tobacco smoking, alcohol drinking, and chewing betel nuts are established major risk factors [
11,
12]. Additionally, other conditions, including chronic inflammation, ulcers, poorly fitting removable dentures, poor oral hygiene, and immunosuppression, have been reported as causal factors in the literature [
1]. In comparison to SCC oncogenesis, the human papillomavirus has a much smaller impact on OVC oncogenesis [
3,
11]. Moreover, it is suggested that OVC may arise in potentially malignant lesions, dysplasia, and carcinoma in situ [
3].
While OVC is not generally considered to have a racial predilection, many studies conducted on Asian patients reported a higher occurrence in men, with incidences as high as 77.4% [
10] and 94.9% [
12]; this seems to be related to the consumption culture of betel nut and tobacco chewing [
3].
The diagnosis of OVC is challenging. In fact, it is very difficult to distinguish OVC from other lesions, such as OSCC, oral verrucous keratosis (OVK), and oral verrucous hyperplasia (OVH) [
13,
14,
15]. OVH has been referred to as an early stage or precursor to OVC and is believed to have similar biological potential [
15]. Additionally, many authors raise the problem of the differentiation between “pure” OVC and “hybrid” OVC which has foci of SCC [
3]. Therefore, it is essential to differentiate OVC from all these lesions through meticulous histopathological assessment. Recent researches have recommended using biomarkers to identify OVC. Since it might be difficult to distinguish OVC from other lesions such as OSCC and OVH based on the histopathological findings, Hosseinpour et al. highlighted via a comprehensive review the value of using biomarkers like Ki67 and P53 to help with the final OVC diagnosis [
16].
OVC has a better prognosis than other types of cancerous tumors that might be fatal [
15]. The most common treatment for OVC is surgery [
3,
15]. In cases of extensive lesions, surgery combined with radiotherapy may be helpful [
15,
17]. Other treatment techniques, such as chemotherapy, may be performed when surgery is not indicated. In fact, a variety of cytostatic drugs have shown favorable effects on reducing tumor size [
15].
4. Conclusion
OVC is a rare tumor with an uncertain etiology and a difficult differential diagnosis. A thorough assessment, especially a histological one, is needed to establish a correct diagnosis.
Consent for Publication: Written informed consent was obtained from the patient for the publication of this case report and all accompanying images.
References
- Mafi, S.; Navabi, N.; Kalantari, M. An aggressive verrucous carcinoma of the palate with rare presentations and recurrence: a case report and literature review. J. Oral. Health Oral. Epidemiol. 2020, 9, 156–161. [Google Scholar]
- Rekha, KP.; Angadi, PV. Verrucous carcinoma of the oral cavity: a clinico-pathologic appraisal of 133 cases in Indians. Oral Maxillofac. Surg. 2010, 14, 211–218. [Google Scholar] [PubMed]
- Candau-Alvarez, A.; Dean-Ferrer, A.; Alamillos-Granados, F.J.; Heredero-Jung, S.; García-García, B.; Ruiz-Masera, J.J.; Arévalo-Arévalo, R.; Zafra-Camacho, F.; Valenzuela-Salas, B. Verrucous carcinoma of the oral mucosa: an epidemiological and follow-up study of patients treated with surgery in 5 last years. Med. Oral Patol. Oral Cir. Bucal. 2014, 19, e506–511. [Google Scholar] [CrossRef] [PubMed]
- Ferlito, A.; Rinaldo, A.; Mannarà, GM. Is primary radiotherapy an appropriate option for the treatment of verrucous carcinoma of the head and neck? J. Laryngol. Otol. 1998, 112, 132–139. [Google Scholar] [CrossRef] [PubMed]
- Keerthi Narayan, V. Verrucous carcinoma of buccal mucosa in female: a rare case report of traumatic tooth origin. Case Rep. Dent. 2021, 2021, 6673038. [Google Scholar] [CrossRef] [PubMed]
- Liu, W.; Shen, X.M.; Liu, Y.; Li, J.; Zhou, Z.T.; Wang, L.Z. Malignant transformation of oral verrucous leukoplakia: a clinicopathologic study of 53 cases. J. Oral Pathol. Med. 2011, 40, 312–316. [Google Scholar] [CrossRef]
- Ogawa, A.; Fukuta, Y.; Nakajima, T.; Kanno, S.M.; Obara, A.; Nakamura, K.; Mizuki, H.; Takeda, Y.; Satoh, M. Treatment results of oral verrucous carcinoma and its biological behavior. Oral Oncol. 2004, 40, 793–797, Erratum in: Oral Oncol. 2005, 41, 436-438. [Google Scholar] [CrossRef]
- Zidar, N.; Gale, N. Larynx cancer: pathology and genetics. In Encyclopedia of cancer, 3rd ed.; Academic Press, 2019; pp. 346–355. [Google Scholar]
- Koch, B.B.; Trask, D.K.; Hoffman, H.T.; Karnell, L.H.; Robinson, R.A.; Zhen, W.; Menck, H.R. Commission on cancer, American College of Surgeons; American Cancer Society. National survey of head and neck verrucous carcinoma: patterns of presentation, care, and outcome. Cancer 2001, 92, 110–120. [Google Scholar] [CrossRef] [PubMed]
- Walvekar, R.R.; Chaukar, D.A.; Deshpande, M.S.; Pai, P.S.; Chaturvedi, P.; Kakade, A.; Kane, S.V.; D’Cruz, A.K. Verrucous carcinoma of the oral cavity: A clinical and pathological study of 101 cases. Oral Oncol. 2009, 45, 47–51. [Google Scholar] [CrossRef] [PubMed]
- Saghravanian, N.; Ghazvini, K.; Babakoohi, S.; Firooz, A.; Mohtasham, N. Low prevalence of high risk genotypes of human papilloma virus in normal oral mucosa, oral leukoplakia and verrucous carcinoma. Acta Odontol. Scand. 2011, 69, 406–409. [Google Scholar] [CrossRef] [PubMed]
- Huang, T.T.; Hsu, L.P.; Hsu, Y.H.; Chen, P.R. Surgical outcome in patients with oral verrucous carcinoma: long-term follow-up in an endemic betel quid chewing area. O.R.L J. Otorhinolaryngol. Relat. Spec. 2009, 71, 323–328. [Google Scholar] [CrossRef] [PubMed]
- Grover, S.; Jha, M.; Sharma, B.; Kapoor, S.; Mittal, K.; Parakkat, N.K.; Shivappa, A.B.; Kaur, R. Verrucous hyperplasia: case report and differential diagnosis. Sultan Qaboos Univ. Med. J. 2017, 17, e98–e102. [Google Scholar] [CrossRef] [PubMed]
- Thomas, G.J.; Barrett, A.W. Papillary and verrucous lesions of the oral mucosa. Diagn Histopathol. 2009, 15, 279–285. [Google Scholar] [CrossRef]
- Alkan, A.; Bulut, E.; Gunhan, O.; Ozden, B. Oral verrucous carcinoma: a study of 12 cases. Eur. J. Dent. 2010, 4, 202–207. [Google Scholar] [CrossRef] [PubMed]
- Hosseinpour, S.; Mashhadiabbas, F.; Ahsaie, M.G. Diagnostic biomarkers in oral verrucous carcinoma: a systematic review. Pathol Oncol Res. 2017, 23, 19–32. [Google Scholar] [CrossRef] [PubMed]
- McClure, D.L.; Gullane, P.J.; Slinger, R.P.; Wysocki, G.P. Verrucous carcinoma--changing concepts in management. J Otolaryngol. 1984, 13, 7–12. [Google Scholar] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).