1. Introduction
Cardiovascular diseases continue to hold the unenviable position as the leading cause of death worldwide(WHO, 2020) Within this group of diseases, prominent exhibitors include ischemic heart disease, stroke, and heart failure, all of which contribute significantly to the global burden of morbidity and mortality(Gaziano et al., n.d.). Among them, ischemic heart disease stands out as one of the most severe because of its rapid onset, particularly when presenting as acute myocardial infarction, claiming over a million lives each year in the United States alone (Mechanic et al., 2022). The sudden interruption of blood flow to the cardiac muscle triggers hypoxia, and if blood supply is not promptly restored, it culminates in tissue necrosis with irreversible loss of cardiomyocytes. From this moment on, there is a series of pathophysiological response, from which the myocardial tissue undergoes structural remodeling (pathological hypertrophy) to maintain cardiac contraction and prevent progression towards heart failure. This process involves the release of proinflammatory mediators, an increase in the secretion of extracellular matrix, and compensatory hypertrophy of the remaining cardiomyocytes (Ferrini et al., 2019).
The Krüppel-like factors (KLFs) are a family of transcription factors known to be associated with many biological processes, including the regulation of cardiac hypertrophy. These belong to a group of DNA-binding proteins that are part of the zinc-fingers transcription factors family. Each one of them is composed of three zinc fingers of the Cys2His2 type, which are capable of binding to three pairs of bases, respectively, in GC-rich regions, such as the consensus sequences CACCC-, GC-, and GT-box (Oishi and Manabe, 2018). Since their discovery in 1993 up to the current date, a total of 18 KLFs have been reported, each with unique expression patterns and the ability to regulate gene transcription, either activating or repressing, numerous targets involved in physiological and pathological processes at the subcellular level (McConnell and Yang, 2010). These processes encompass growth, differentiation, and cellular apoptosis, as well as the maintenance of specialized tissues (Tetreault et al., 2013).
Moreover, KLFs are key players in the regulation of cardiac hypertrophy, and their activity can have both pro-hypertrophic and anti-hypertrophic effects, depending on the context and interactions with other regulatory factors. Several aspects, including changes in gene expression, modifications to cellular signaling pathways, and alterations to cellular processes within cardiomyocytes, can influence the development of cardiac hypertrophy. For instance, Klf2, which is highly expressed in endothelial cells, has been identified as a negative regulator of cardiac hypertrophy (Boon et al., 2007; Li et al., 2021). Previous research has shown Klf2´s ability to inhibit TGFβ signaling in endothelial cells by promoting the expression of Smad7 and blocking the activator protein 1 (AP-1) activity [9]. Moreover, Klf2 induction by Simvastatin, achieved a significant reduction in the expression of hypertrophic genes, such as atrial natriuretic peptide (ANP), brain natriuretic peptide (BNP), and α-myosin heavy chain (α-MHC), in a Transverse Aortic Constriction (TAC) model (Li et al., 2021). In contrast, Klf5 has been found to be increased in models of cardiac damage, namely end-stage heart failure or diabetic cardiomyopathy(Hoffman et al., 2021; Kyriazis et al., 2021). Additionally, its role as a mediator of hypertrophy has been demonstrated in heterozygous Klf5 mice, in which a reduced response to Angiotensin II infusion was observed, resulting in less cardiomyocyte growth and fibrosis development, emphasizing the importance of its presence for the onset of hypertrophy (Shindo et al., 2002). The significance of Klf5 in hypertrophy development lies in its capacity to transactivate targets such as Platelet-Derived Growth Factor (PDGF)-A/B, Egr-1, Plasminogen Activator Inhibitor-1 (PAI-1), inducible Nitric Oxide Synthase (iNOS), and Vascular Endothelial Growth Fac-tor (VEGF) receptors, amongst others, all of which play a pivotal role during cardiovascular remodeling (NAGAI et al., 2005)
In this study, we aimed to investigate the gene expression of specific KLFs following myocardial infarction induction and the development of hypertrophy. Our research group's primary goal is to contribute to the elucidation of the intricate mechanisms underlying KLFs gene regulation during cardiac hypertrophy, as well as their potential links to inflammatory genes and cardiac conduction. By examining the gene expression patterns of KLFs and their interactions with key mediators, we aim to shed light on the regulatory processes governing cardiac hypertrophy.
2. Materials and Methods
2.1. Animal Study Approval
All experiments were carried out using 150g ± 20g female Wistar rats. These were housed in polymethylmethacrylate boxes and kept at 20 – 24 °C in a room with 12-hour light/dark cycle. Food and water were available ad libitum in the cage. Research with animals carried out for this study was performed according to approved protocols (BI21-00006) and animal welfare regulations of Nuevo León Autonomous University´s Institutional Bioethics Committee.
2.2. Rat model and cardiotomy
For myocardial damage induction, 65 mg/kg of the beta-adrenergic drug, isoproterenol hydrochloride (SKU: I5627 Sigma-Aldrich, St. Louis, MO, USA) was administered intraperitoneally, dissolved in 0.5 mL of physiological solution (0.9% Sodium Chloride) at room temperature, in a single dose. The control group was administered with 0.5 mL of physiological solution intraperitoneally in a single dose. The experimental animals were euthanized under anesthesia by cervical dislocation. To collect the hearts, the thorax was accessed through an inverted T incision and longitudinal sternotomy. The heart was freed by clamping and cutting the great vessels of the corona cordis, allowing the removal of the organ from the rat's body. Myocardial damage was confirmed by H&E staining. This procedure was performed at different time lapses after chemical induction of cardiac insult with isoproterenol.
2.3. Cardiac morphometry and heart volume calculation
Heart´s length, width and height were measured with a digital vernier. Using the ellipsoid volume formula (V=3/4𝜋×𝐷1×𝐷2×𝐿), heart volumes were calculated and normalized to body weight of each experimental animal.
2.3. RNA Isolation and Quantitative Real-Time RT-PCR
Total RNA from the left ventricle area was extracted with TRIzol® (Invitrogen; Thermo Fisher Scientific, Inc., Waltham, MA, USA), according to the manufacturer's protocol. Complementary DNA (cDNA) was synthesized by reverse transcription reaction with 250 μg of total RNA using SuperScript™ VILO™ cDNA Synthesis Kit (Invitrogen; Thermo Fisher Scientific, Inc.). Real time PCR reactions were amplified and analyzed in triplicate using an Applied Biosystems 7500 Fast Real time PCR thermal cycler and following the SYBR-Green® FAST protocol (Thermo Fisher Scientific, Inc.) under the next reaction conditions: Step 1: 95°C for 20 seconds, Step 2: 40 cycles of 95°C for 3 seconds, Step 3: 40 cycles of 60°C for 30 seconds. Glyceraldehyde-3-phosphate de-hydrogenase (GAPDH) levels were used to normalize the expression of target genes. The relative expression levels of the genes were calculated using the 2–∆∆Ct method. The list of primers sequences for target genes can be found in supplementary material.
2.4. Statistical analysis
The collected data was analyzed using SPSS software version 17.0 (SPSS, Inc. Chicago, IL, USA), data are expressed as mean ± SEM. Statistical significance was determined using one-way ANOVA with Dunnett correction. A P value <0.05 was considered statistically significant. Graphs and visual aids were made using GraphPad Prism Version 5 and the Biorender app, respectively.
2.5. STRING
STRING integrates information from multiple sources, including high-quality experiments, curated databases, and computational predictions, to construct large-scale protein interaction networks. We utilized STRING (version 11.5) with the multiple protein search option to explore their interactions. The resulting interactome was downloaded in TSV format and visualized using Excel. Our investigation primarily focused on the direct interactions involving KLFs; priority was given to those with the highest correlation or weight, and we compared them with relevant literature. To facilitate a more intuitive comparison, we constructed a Venn diagram that depicted the distinct interactions of our genes of interest with diverse KLFs.
3. Results
Female Wistar rats of 150g ± 20g were initially injected with a single interperitoneally dose of isoproterenol (65mg/kg) to induce myocardial damage(Grimm, 1998; Hosseini et al., 2022; Liu et al., 2013). At 24-hour intervals, animals were sedated, euthanized, and subjected to cardiac removal.
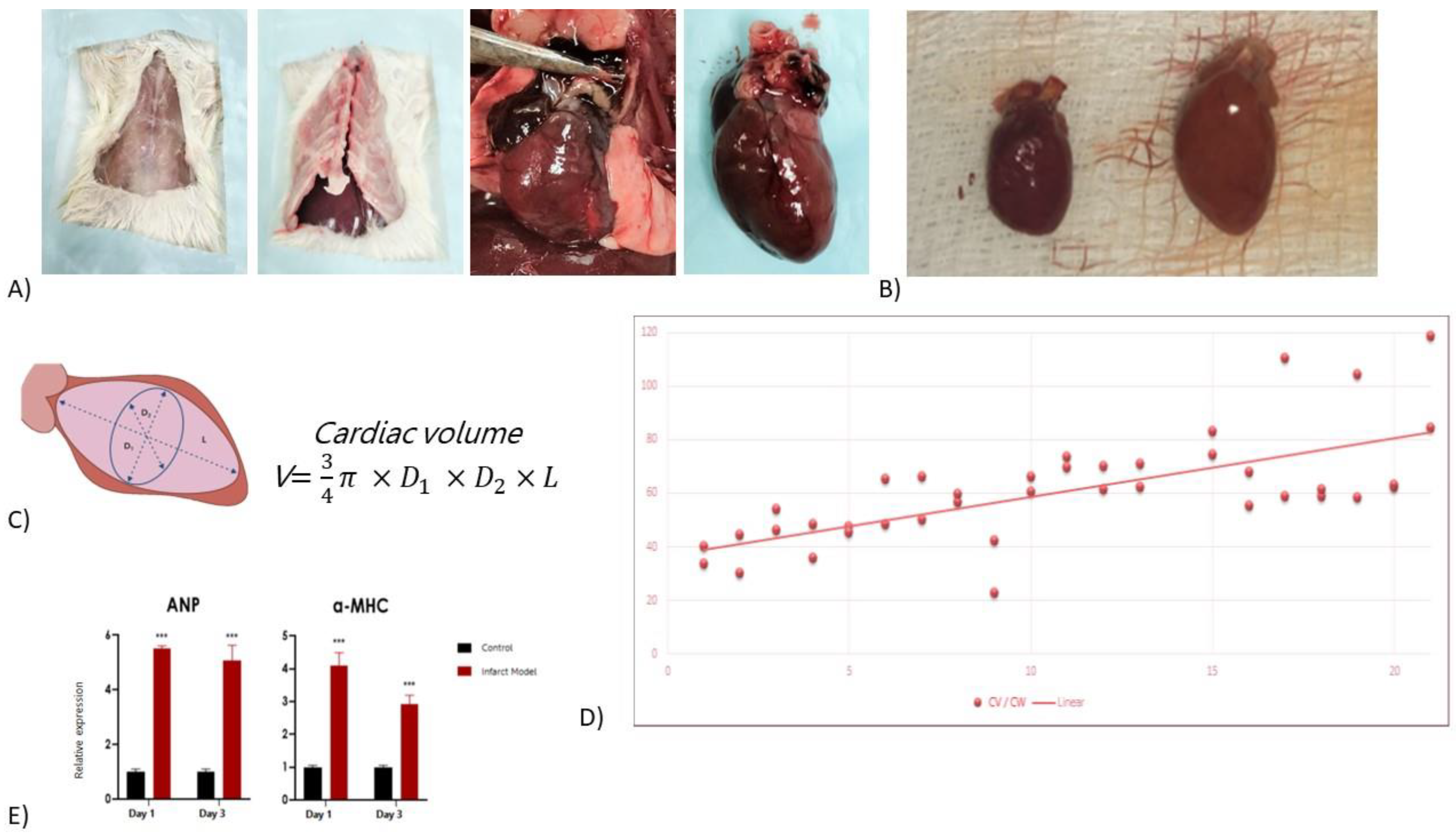
Figure 1A shows the representative surgical removal process. Cardiac hypertrophy was expected to occur in a period of approximately 21 days (Ferrini et al., 2019).
Figure 1B shows the comparative of the control heart size, versus heart size at 21 days post-induction.
Before surgery, animals were weighted, and after surgical removal of the organ, the heart was measured for length and width, as well as weighted (weights and measurements can be found in Supplemental
Table S1). With the measured variables, cardiac volume was calculated and normalized to the weight of each experimental animal (CV/BW). (
Figure 1C) and a graph of the time lapse versus CV/BW was developed (
Figure 1D), showing a continuous increase overtime. As a final control of isoproterenol-induced cardiac damage, both ANP and α-MHC, known markers of stress and cardiac hypertrophy, respectively, were shown to increase in expression over time, as seen in
Figure 1E.
Since our main goal centered on better understanding the regulation of the Krüppel-like family of transcription factors, and their post-infarction role, we sought to measure their expression levels in combination to the cardiac commitment triad of Gata4, Mef2c, and Tbx5 (GMT), which have been shown to reactivate under pathological conditions in the adult heart. As an insult to the heart promotes a state of inflammation, we further measured levels of known inflammatory cytokines Il-1, Il-6, Tnf-α, Nf-κb, amongst others.
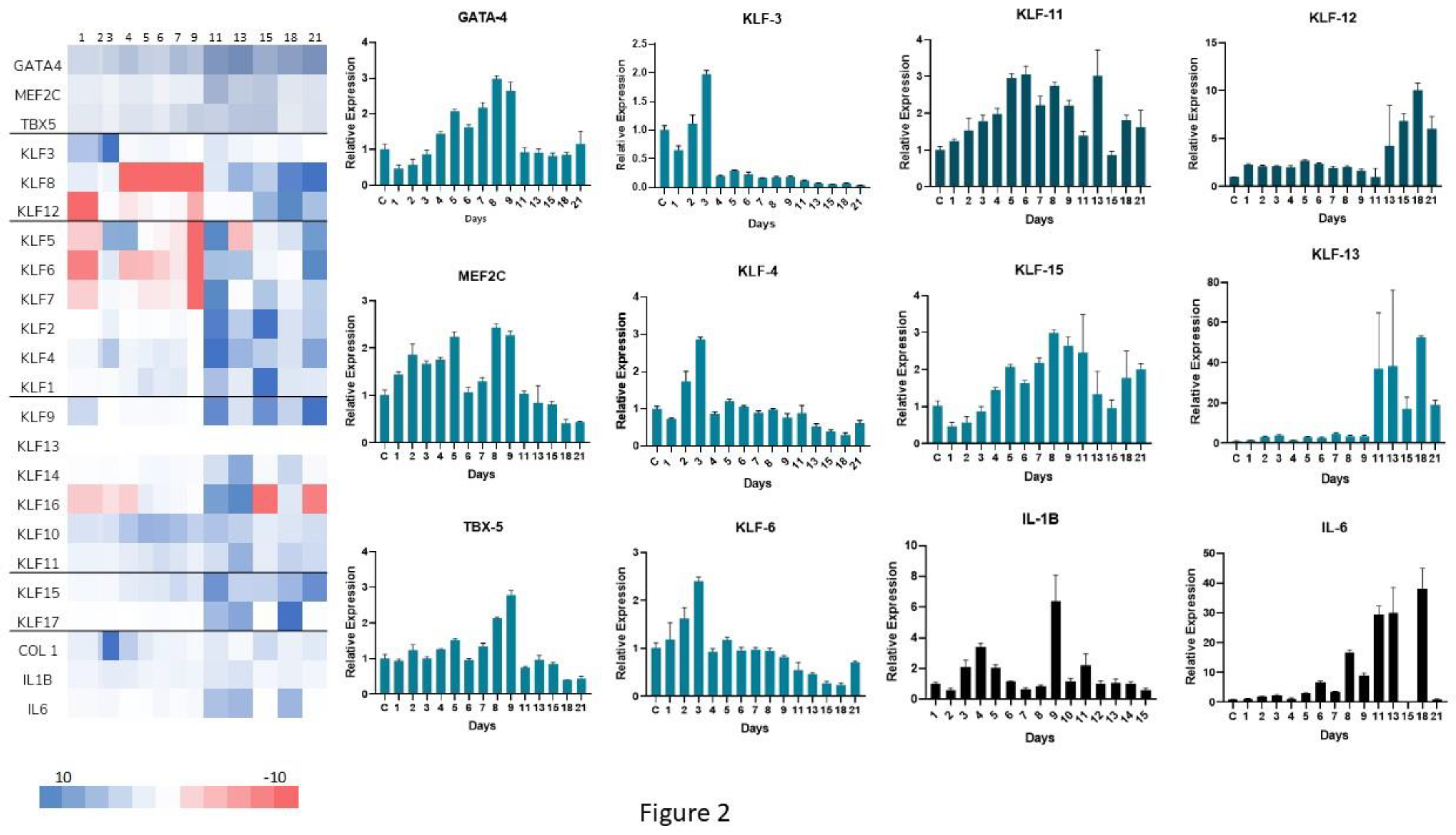
Figure 2A shows a complete overview (RT-PCR heat map) of the entire KLFs network of transcription factors, in addition to GMT and the inflammatory cytokines. Post-infarction cardiac hypertrophy is segmented into three primary phases: an early inflammatory phase consisting of the first 4 days, followed by a proliferative stage (day 5 – 14) and a final onset of scar tissue maturation up to three weeks from the initial state (Venugopal et al., 2022). Regarding this categorization, we conducted daily assessments of RNA expression from the initial 24 hours following the infarction event and extending up to day seven, which corresponds to the mid-inflammatory phase. Subsequently, samples were evaluated every alternate day for the duration of three weeks, encompassing the entire observation period.
Regulatory effects were deemed close to the projected hypertrophic stages (
Figure 2B). Several known KLFs related to cardiac function and growth exhibited significant alterations. First, our results showed an early up-regulation of
Klf4, particularly at days 2 and 3, similarly
Klf3 and
Klf6 also have their highest peaks around day 3. These members of the KLFs are noticeable as they are involved in pro-fibrotic and antiapoptotic signaling. Which could help explain the initial growth effects and fibrosis of the heart. Moreover, through the hypertrophic evolution related to the damage, in the proliferative stage, there is a remarkable upregulation of both
Klf11 at days 5 and 6, and
Klf15 at day 8. It is important to state that
Klf11 is related to TGF-β signaling which can lead to SMAD related cell growth (Pardali et al., 2017; Zhang et al., 2013). Meanwhile,
Klf15 is known directly as a hypertrophy modulator, known to inhibit both
Gata4 and
Mef2c (Fisch et al., 2007). Consistent with this observation we see a drastic drop in all 3 components of GMT:
Gata4 on day 8 and both
Mef2c and
Tbx5 on day 9. In the final mature stage, there is an up regulatory effect in
Klf12 and
Klf13, both pro-apoptotic regulators, which could indicate final patterning. Additionally, a quick look at
Il6 showed a continuous increase in inflammation through the entire remodeling process (
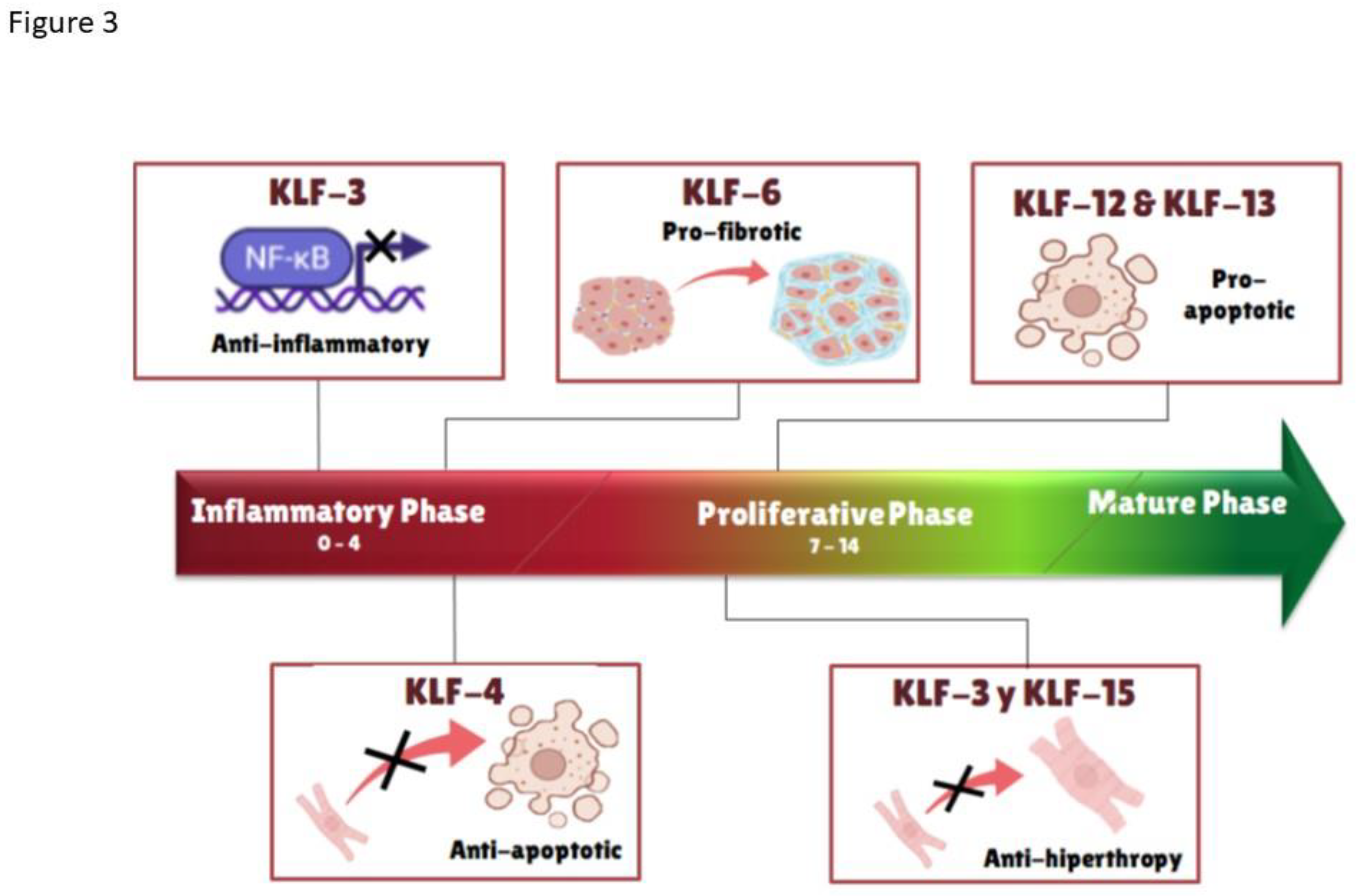
Figure 3 and
Table 1).
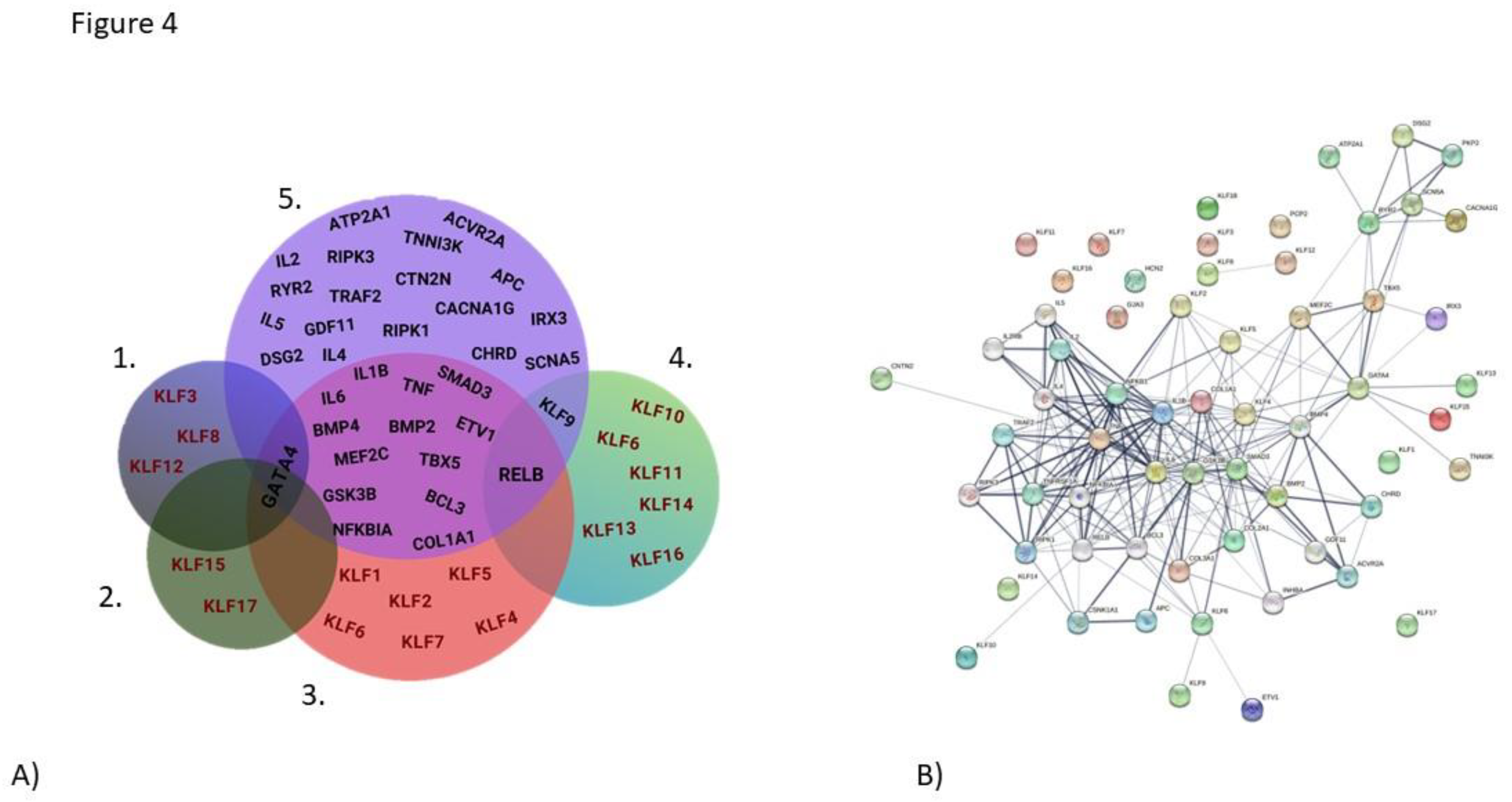
Cardiac function is critically related to its electrical functions. As a first bioinformatic approach, we sought to identify genes interacting with KLFs. Using the STRING database, we constructed rudimentary networks, aimed to initiate the identification of direct correlations between electrical genes. Our initial screening yielded the presence of components related to cardiac electrical function (Na/K pumps, calcium exchangers), Wnt, BMP, SMAD signaling elements, and inflammatory mediators (
Irx3, Acrv2a, Cntn2, Dsg1, Cx40, Cx43, Hcn, Kcna2, Pcp4, Atp2a2, Scl8a1, Scn5a, Tnni3k, Apc, Ryr2, Cacna1g, Bmp2, Bmp4, Gsk3B, Inhba, NfkB1, Ripk1, Smad2, Smad3, Tnfrsf1,Tnf-a)
Figure 4. Next, we proceeded to cluster these results based on the interacting KLFs subtypes. A detailed protein-protein interaction table is presented in
Supplementary Table S3. Briefly, each row in the table represents an interaction between two genes, specifically, reciprocal interactions between gene pairs, with the first column indicating protein 1 and the second column indicating protein 2. These interactions were determined through experimental methods or predicted based on various lines of evidence, including chromosomal proximity, gene fusion, phylogenetic co-occurrence, homology, co-expression, experimentally reported interactions, database annotations, and text-mining. Subsequent columns contain scores assigned to each type of interaction evidence, and the last column provides a combined score. This table serves as a resource for exploring and prioritizing interactions between genes of interest, leveraging the integration of multiple data sources performed by the STRING database.
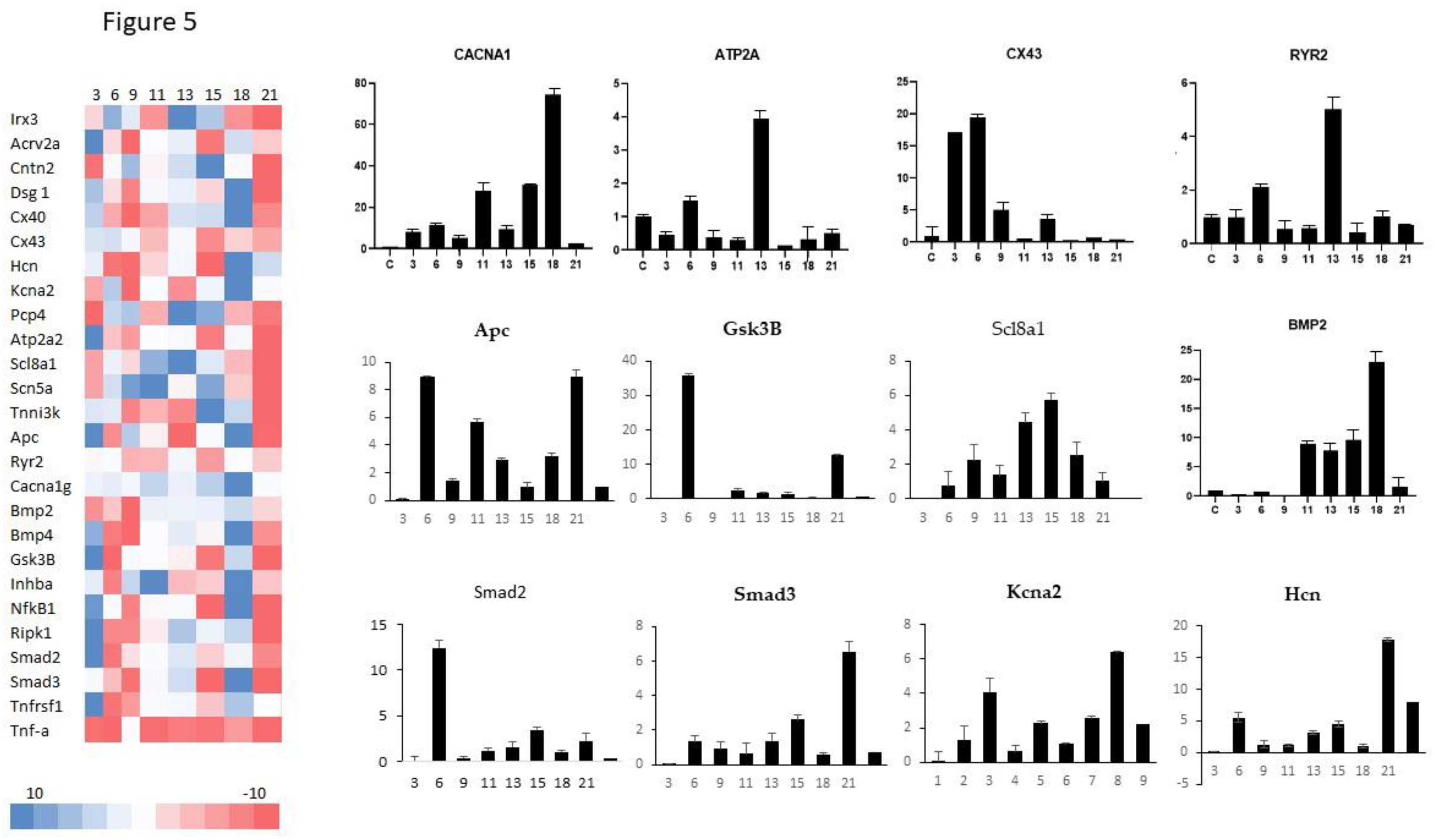
Finally,
Figure 5 presents an overview (RT-PCR heat map) of the expression profiles of key components of either cardiac electrical function, WNT, BMP, SMAD signaling and inflammatory mediators; these components as seen in
Figure 4 have a relation to the different KLFs. Taking a more particular guise,
Figure 4 (right) shows interesting regulatory effects which in part may be driven by the changes in expression of diverse KLFs. Earlier mention
Klf11, was shown to have its highest expression just around day 9 and was said to have potential regulatory effects over SMAD signaling, through inflammation(Boon et al., 2007; Pardali et al., 2017). In this respect,
Smad2 expression profile shows an important elevation of its expression early on, around day 6, but is quickly suppressed by day 9. Nonetheless, levels of
Smad2 re-activate similarly to those of
Smad3. Inflammatory cytokines such
Il-6 were shown to elevate at late stages of hypertrophic remodeling, coinciding with elevation of
Klf13 and
Klf12. Moreover,
Bmp2 expression further correlates with
TGF-b signaling, in direct relation to SMAD expression(Varga et al., 2021; Zou et al., 2021).
GATA4 is an important component of the cardiac commitment triad GMT(Christoforou et al., 2013). Its expression was shown at its highest just over a week post myocardial damage, as potential cardiac recovery from damage should take place. Expression of cardiac specific genes such as ion channels Hcn1 and Kcna2 showed their highest elevation around day 18. Surprisingly, the sodium calcium exchanger Scl8a1 was highly expressed earlier, around day 15 before steadily declining its expression.
4. Discussion
The heart is a critical organ in charge of distributing oxygen and nutrients to the entire body. Regrettably, this essential organ lacks the potential to self-regenerate, hence the heart is susceptible to the harsh effects of wear and tear, as well as environmental and genetic degeneration, which in turn leads to exacerbation of an inflammatory state, typically followed by loss of cardiomyocytes, fibrosis, and pathological remodeling (Goradel et al., 2018; Islas and Moreno-Cuevas, 2018; Santoyo-Suarez et al., 2023; Sarre-Álvarez and Cabrera-Jardines, R Rodríguez-Weber, 2018). Given its lack of natural capacity for renewal, it is critical to enhance our comprehension of the progression of these altered deteriorating stages. According to the American Heart Association, myocardial infarction, better known as a heart attack, kills just over 800,000 people in the U.S. alone every year and is considered the leading killer of CVD´s (Tsao et al., 2023). The Krüppel-like factors family has recently received extensive attention, as novel research has centered in their involvement in many processes including embryogenesis and development of diseases related to several organs(Choi et al., 2018; Dabravolski et al., 2022; Leenders et al., 2012; Pabona et al., 2010; Santoyo-Suarez et al., 2023; Shankman et al., 2015; Vinjamur et al., 2014; Yang et al., 2018; Zheng et al., 2009). Isoproterenol is a β-adrenergic stimulant known to induce infarction-like lesions in the myocardium, leading to loss of cardiomyocytes, fibrosis, and remodeling, potentially leading to heart failure (Grimm, 1998). Several studies have confirmed that β-adrenergic stimulation increases cardiac contractility developing maladaptive hypertrophy, led by several mechanisms including enhanced protein synthesis, proto-oncogene expression, elevated oxidative stress, and stimulation of mitogen activated protein kinases (Chowdhury et al., 2013). As earlier stated, post-infarction pathological remodeling typically takes 3 weeks (approximately 21 days). We tested a single intraperitoneal dose of isoproterenol (65 mg/kg), and over the course of 3 weeks, CV/BW more than doubled (
Figure 1D). The cardiac hypertrophy was further confirmed by the increase in fibrosis, as observed by H&E staining (supplemental
Figure 1). The observed pathological maladaptive hypertrophy, as seen in our animal models, is consistent with the earlier studies, wherein high dosages of isoproterenol induced significant irregularities in cardiac architecture, fibrotic infiltration, widening of the interstitium, and loss of cardiomyocytes (Grimm, 1998). Finally, Atrial Natriuretic Peptide (NPPA) is considered a marker for cardiac stress. In clinical settings, NPPA elevation has long been considered a staple of heart failure (Ilatovskaya et al., 2022), as it has been shown to elevate during high demanding workflows, stimulating vasodilation and alleviates hypertension (NISHIKIMI et al., 2006). During a stress-related event such as the one promoted by isoproterenol, myocyte damage induces remodeling and an expected elevation in NPPA (Ilatovskaya et al., 2022), as seen in our results,
Figure 1E shows a 5-fold surge in NPPA levels and an initial 4-fold increase in α-MHC expression, both indicative of cardiac damage and heart hypertrophy, respectively.
As we followed myocardial damage over time, GMT alterations were expected. Post infarction-like stimulus is known to induce a strong MAPK kinase signaling cascade. As a result, considerable GATA4 phosphorylation occurs, favoring pro-hypertrophic gene transcription [39].
GATA4 is a transcription factor that directly regulates the expression of several heart-specific genes, including the α-MHC, troponin C (Tnnc1), troponin I (Tnni3), NPPA, BNP, and ion transport genes, such as the cardiac sodium-calcium exchanger Slc8a1 (
Figure 5). Previously, murine research has shown that specific
Gata4 overexpression can cause cardiac hypertrophy, as demonstrated by Liang et al., (2001) who used transgenic animals capable of expressing
Gata4 2.5 times more than wild type. In
Figure 2 we observed this similar increase by day 8. Moreover,
Mef2c and
Tbx5, both essential players in
Gata4 regulation show similar trends of upregulation by day 9. Our interactome data (
Figure 4B and Supplemental
Table S3) further confirmed this interaction and showed a strong
Gata4 relation to
Klf2, 4, 5, 13 and 15. Moreover,
Klf6 showed involvement with Gata4
and SMAD3 which are related to SMAD signaling, in addition
Klf6 was further related to
Il-6, and
Nf-κb (Nf-κb1a, and
Relb), all related to inflammatory processes(Zhang et al., 2014). TGFβ, a driver of SMAD signaling, functions as an effector of tissue fibrosis, which can eventually lead to scaring and elevation of collagen related genes (Hu et al., 2018). Both
Klf4 and
6 exhibited early post myocardial damage elevations, potentially leading the way for hypertrophy. Under this perspective, hypertrophy could lead to high levels of fibrosis in the heart, reducing its function and increasing its size. Our data further confirms the activation of
Col1A1 and
Col3A1 (Supplemental
Table S3), as expression data show both the elevation of
Klf4 and
6, as well as elevation of
Bmp2, Il-6, and
Smad3 (Graphs of
Figure 2 and
Figure 5). In opposition, around 1 week post myocardial damage, upregulation of
Klf15 peaks, potentially blocking hypertrophy progression(Leenders et al., 2012, 2010; Wenying et al., 2021).
Klf15 has been shown to block
Mef2c and
Gata4 specific DNA-binding sites, preventing the binding of its coactivator, Myocardin, which works as a hypertrophy antagonist (Prosdocimo et al., 2015). Hence, marking the start of the maturation phase, wherein we can observe an elevation of
Klf12 and
13. While information regarding KLF12 is limited in its involvement in the downregulation of Survivin, -an antiapoptotic factor- has been demonstrated (Mak et al., 2017). In addition, KLF13, a pro-apoptotic factor, seems to favor homeostatis, as it is potentially inhibiting BCL-XL and consequently triggering cell death. Left Anterior Descending Coronary Artery Ligation (LAD) murine models have shown an increase in
Klf13 expression related to early phase cardiomyocyte death, a contrasting effect to that of
Klf4 (Bayoumi et al., 2018; Zhou and Herring, 2005).
GMT genes contribute to cardiac maintenance, contraction, and growth of the heart (Christoforou et al., 2013; Dirkx et al., 2013; Liu, 2017; Liu et al., 2016). Unsurprisingly, electrical function is also related to these genes. Tbx5 has been related to SRF and CX43 (early activation post myocardial damage), which are directly related to myocardial stress, which, when exacerbated, leads to pathological hypertrophy (Christoforou et al., 2013; Liang et al., 2001). Cardiac muscle contraction (RYR, ATP2A, αMHC) and electrical activity are intrinsically related. Interestingly our findings reveal a sharp decrease in several of these genes, particularly by day 10 (
Figure 5), strongly suggesting a decline in function, along with the preceding drop of CX43 expression (Zhang et al., 2022). Notably, our initial bioinformatic screening did directly link KLFs to these genes, implying indirect inter-actions. These interactions could further explain both up- and down- regulatory effects, making further exploration imperative to better elucidate these mechanisms.
5. Conclusion
The heart is a vital organ that can be damaged by various factors, including stress, genetic defects, and environmental factors. At high dosage, isoproterenol can induce myocardial damage, leading to inflammation, loss of heart muscle cells, scarring, and remodeling or hypertrophy.
KLFs are involved in a variety of cellular processes, including gene transcription, cell growth, and differentiation. Our study showed that KLFs are dysregulated by myocardial damage, promoting the progression of abnormal hypertrophy. We showed that expression profiles of different KLFs change during different stages of cardiac damage, suggesting that KLFs may play a role in modulating the hypertrophic response and influencing downstream signaling pathways. The findings of this study provide new insights into the molecular mechanisms underlying cardiac damage and abnormal hypertrophy. A better understanding of their targets and interacting partners could help us lead to the development of new therapeutic interventions to treat heart diseases.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org. Supplemental Figure S1. Infarct Model. H&E staining A, B) 21d post infarct high fibroblast in-filtration, C) Loss of muscle fibers, D) Control no infarct. Supplemental Table S1. Primer list. Supplemental Table S2. Weights and lengths. Supplemental Table S3. Table of protein-protein interaction pairs from the STRING database.
Author Contributions
Conceptualization: JFI, GRP-R, JLD-G; methodology MGS-S, JAG-L, JDM-M, JLD-G; software JAG-L, PZ-M; validation GPR-R; formal analysis GRP-R, JAG-L, PZ-M; investigation JDM-M, AE-R; resources: LG-O, AS-D, AE-R, AC-M; writing and editing: JFI, DFB-C, ENG-T; supervision JFI, project administration JFI, GRP-R, ENG-T, funding acquisition JFI, AE-R. All authors have read and agreed to the published version of the manuscript.
Funding
“This research was funded by CONAHCYT, grant Ciencia de Fronteras No. CF-MG-20191004101335125-51208”
Institutional Review Board Statement
“The animal study protocol was approved by the Institu-tional Review Board of Facultad de Medicina, Universidad Autonoma de Nuevo Leon, protocol number BI21-00006.
Conflicts of Interest
“The authors declare no conflict of interest.”
References
- Bayoumi, A.S., Park, K., Wang, Y., Teoh, J., Aonuma, T., Tang, Y., Su, H., Weintraub, N.L., Kim, I., 2018. A carvedilol-responsive microRNA, miR-125b-5p protects the heart from acute myocardial infarction by repressing pro-apoptotic bak1 and klf13 in cardiomyocytes. J Mol Cell Cardiol 114, 72–82. [CrossRef]
- Boon, R.A., Fledderus, J.O., Volger, O.L., van Wanrooij, E.J.A., Pardali, E., Weesie, F., Kuiper, J., Pannekoek, H., ten Dijke, P., Horrevoets, A.J.G., 2007. KLF2 Suppresses TGF-β Signaling in Endothelium Through Induction of Smad7 and Inhibition of AP-1. Arterioscler Thromb Vasc Biol 27, 532–539. [CrossRef]
- Choi, J.P., Wang, R., Yang, X., Wang, X., Wang, L., Ting, K.K., Foley, M., Cogger, V., Yang, Z., Liu, F., Han, Z., Liu, R., Baell, J., Zheng, X., 2018. Ponatinib (AP24534) inhibits MEKK3-KLF signaling and prevents formation and progression of cerebral cavernous malformations. Sci Adv 4. [CrossRef]
- Chowdhury, D., Tangutur, A.D., Khatua, T.N., Saxena, P., Banerjee, S.K., Bhadra, M.P., 2013. A proteomic view of isoproterenol induced cardiac hypertrophy: Prohibitin identified as a potential biomarker in rats. J Transl Med 11, 130. [CrossRef]
- Christoforou, N., Chellappan, M., Adler, A.F., Kirkton, R.D., Wu, T., Addis, R.C., Bursac, N., Leong, K.W., 2013. Transcription Factors MYOCD, SRF, Mesp1 and SMARCD3 Enhance the Cardio-Inducing Effect of GATA4, TBX5, and MEF2C during Direct Cellular Reprogramming. PLoS One 8. [CrossRef]
- Dabravolski, S.A., Sukhorukov, V.N., Kalmykov, V.A., Grechko, A. V., Shakhpazyan, N.K., Orekhov, A.N., 2022. The Role of KLF2 in the Regulation of Atherosclerosis Development and Potential Use of KLF2-Targeted Therapy. Biomedicines 10, 254. [CrossRef]
- Dirkx, E., Da Costa Martins, P.A., De Windt, L.J., 2013. Regulation of fetal gene expression in heart failure ☆. [CrossRef]
- Ferrini, A., Stevens, M.M., Sattler, S., Rosenthal, N., 2019. Toward Regeneration of the Heart: Bioengineering Strategies for Immunomodulation. Front Cardiovasc Med 6. [CrossRef]
- Fisch, S., Gray, S., Heymans, S., Haldar, S.M., Wang, B., Pfister, O., Cui, L., Kumar, A., Lin, Z., Sen-Banerjee, S., Das, H., Petersen, C.A., Mende, U., Burleigh, B.A., Zhu, Y., Pinto, Y., Liao, R., Jain, M.K., 2007. Kruppel-like factor 15 is a regulator of cardiomyocyte hypertrophy. Proc Natl Acad Sci U S A 104, 7074–7079. [CrossRef]
- Gaziano, T., Reddy, S., Paccaud, F., Horton, S., n.d. Disease Control Priorities in Developing Countries., in: Jamison, D., Berman, J., Measham, A. (Eds.),. Oxford University Press, Washington.
- Goradel, N.H., Hour, F.G., Negahdari, B., Malekshahi, Z.V., Hashemzehi, M., Masoudifar, A., Mirzaei, H., 2018. Stem Cell Therapy: A New Therapeutic Option for Cardiovascular Diseases. J Cell Biochem 119, 95–104. [CrossRef]
- Grimm, D., 1998. Development of heart failure following isoproterenol administration in the rat: role of the renin–angiotensin system. Cardiovasc Res 37, 91–100. [CrossRef]
- Hoffman, M., Palioura, D., Kyriazis, I.D., Cimini, M., Badolia, R., Rajan, S., Gao, E., Nikolaidis, N., Schulze, P.C., Goldberg, I.J., Kishore, R., Yang, V.W., Bannister, T.D., Bialkowska, A.B., Selzman, C.H., Drakos, S.G., Drosatos, K., 2021. Cardiomyocyte Krüppel-Like Factor 5 Promotes De Novo Ceramide Biosynthesis and Contributes to Eccentric Remodeling in Ischemic Cardiomyopathy. Circulation 143, 1139–1156. [CrossRef]
- Hosseini, A., Rajabian, A., Sobhanifar, M.-A., Alavi, M.S., Taghipour, Z., Hasanpour, M., Iranshahi, M., Boroumand-Noughabi, S., Banach, M., Sahebkar, A., 2022. Attenuation of isoprenaline-induced myocardial infarction by Rheum turkestanicum. Biomedicine & Pharmacotherapy 148, 112775. [CrossRef]
- Hu, H.-H., Chen, D.-Q., Wang, Y.-N., Feng, Y.-L., Cao, G., Vaziri, N.D., Zhao, Y.-Y., 2018. New insights into TGF-β/Smad signaling in tissue fibrosis. Chem Biol Interact 292, 76–83. [CrossRef]
- Ilatovskaya, D. V., Levchenko, V., Winsor, K., Blass, G.R., Spires, D.R., Sarsenova, E., Polina, I., Zietara, A., Paterson, M., Kriegel, A.J., Staruschenko, A., 2022. Effects of elevation of ANP and its deficiency on cardiorenal function. JCI Insight 7. [CrossRef]
- Islas, J., Moreno-Cuevas, J., 2018. A MicroRNA Perspective on Cardiovascular Development and Diseases: An Update. Int J Mol Sci 19, 2075. [CrossRef]
- Kyriazis, I.D., Hoffman, M., Gaignebet, L., Lucchese, A.M., Markopoulou, E., Palioura, D., Wang, C., Bannister, T.D., Christofidou-Solomidou, M., Oka, S.I., Sadoshima, J., Koch, W.J., Goldberg, I.J., Yang, V.W., Bialkowska, A.B., Kararigas, G., Drosatos, K., 2021. KLF5 Is Induced by FOXO1 and Causes Oxidative Stress and Diabetic Cardiomyopathy, Circulation Research. [CrossRef]
- Leenders, J.J., Wijnen, W.J., Hiller, M., Van Der Made, I., Lentink, V., Van Leeuwen, R.E.W., Herias, V., Pokharel, S., Heymans, S., De Windt, L.J., Høydal, M.A., Pinto, Y.M., Creemers, E.E., 2010. Regulation of cardiac gene expression by KLF15, a repressor of myocardin activity. Journal of Biological Chemistry 285, 27449–27456. [CrossRef]
- Leenders, J.J., Wijnen, W.J., van der Made, I., Hiller, M., Swinnen, M., Vandendriessche, T., Chuah, M., Pinto, Y.M., Creemers, E.E., 2012. Repression of cardiac hypertrophy by KLF15: Underlying mechanisms and therapeutic implications. PLoS One 7, 1–10. [CrossRef]
- Li, H., Wang, Y., Liu, Jiwen, Chen, X., Duan, Y., Wang, X., Shen, Y., Kuang, Y., Zhuang, T., Tomlinson, B., Chan, P., Yu, Z., Cheng, Y., Zhang, L., Liu, Z., Zhang, Y., Zhao, Z., Zhang, Q., Liu, Jie, 2021. Endothelial Klf2-Foxp1-TGFβ signal mediates the inhibitory effects of simvastatin on maladaptive cardiac remodeling. Theranostics 11, 1609–1625. [CrossRef]
- Liang, Q., De Windt, L.J., Witt, S.A., Kimball, T.R., Markham, B.E., Molkentin, J.D., 2001. The Transcription Factors GATA4 and GATA6 Regulate Cardiomyocyte Hypertrophy in Vitro and in Vivo. Journal of Biological Chemistry 276, 30245–30253. [CrossRef]
- Liu, Y., 2017. Earlier and broader roles of Mesp1 in cardiovascular development. Cellular and Molecular Life Sciences 74, 1969–1983. [CrossRef]
- Liu, Y., Chen, L., Diaz, A.D., Benham, A., Xu, X., Wijaya, C.S., Fa’Ak, F., Luo, W., Soibam, B., Azares, A., Yu, W., Lyu, Q., Stewart, M.D., Gunaratne, P., Cooney, A., McConnell, B.K., Schwartz, R.J., 2016. Mesp1 Marked Cardiac Progenitor Cells Repair Infarcted Mouse Hearts. Sci Rep 6, 1–14. [CrossRef]
- Liu, Y., Jia, H., Chang, X., Ding, G., Zhang, H., Zou, Z.-M., 2013. The metabolic disturbances of isoproterenol induced myocardial infarction in rats based on a tissue targeted metabonomics. Mol Biosyst 9, 2823. [CrossRef]
- Mak, C.S.L., Yung, M.M.H., Hui, L.M.N., Leung, L.L., Liang, R., Chen, K., Liu, S.S., Qin, Y., Leung, T.H.Y., Lee, K.-F., Chan, K.K.L., Ngan, H.Y.S., Chan, D.W., 2017. MicroRNA-141 enhances anoikis resistance in metastatic progression of ovarian cancer through targeting KLF12/Sp1/survivin axis. Mol Cancer 16, 11. [CrossRef]
- McConnell, B.B., Yang, V.W., 2010. Mammalian Krüppel-Like factors in health and diseases, Physiological Reviews. [CrossRef]
- Mechanic, O.J., Gavin, M., Grossman, S.A., Ziegler, K., 2022. Acute Myocardial Infarction (Nursing).
- NAGAI, R., SUZUKI, T., AIZAWA, K., SHINDO, T., MANABE, I., 2005. Significance of the transcription factor KLF5 in cardiovascular remodeling. Journal of Thrombosis and Haemostasis 3, 1569–1576. [CrossRef]
- NISHIKIMI, T., MAEDA, N., MATSUOKA, H., 2006. The role of natriuretic peptides in cardioprotection. Cardiovasc Res 69, 318–328. [CrossRef]
- Oishi, Y., Manabe, I., 2018. Krüppel-Like Factors in Metabolic Homeostasis and Cardiometabolic Disease. Front Cardiovasc Med 5, 1–14. [CrossRef]
- Pabona, J.M.P., Zeng, Z., Simmen, F.A., Simmen, R.C.M., 2010. Functional differentiation of uterine stromal cells involves cross-regulation between bone morphogenetic protein 2 and Krüppel-like factor (KLF) family members KLF9 and KLF13. Endocrinology 151, 3396–3406. [CrossRef]
- Pardali, E., Sanchez-Duffhues, G., Gomez-Puerto, M.C., Dijke, P., 2017. TGF- β -Induced Endothelial-Mesenchymal Transition in Fibrotic Diseases. Int J Mol Sci 18. [CrossRef]
- Prosdocimo, D.A., Sabeh, M.K., Jain, M.K., 2015. Kruppel-like factors in muscle health and disease. Trends Cardiovasc Med 25, 278–287.
- Santoyo-Suarez, M.G., Mares-Montemayor, J.D., Padilla-Rivas, G.R., Delgado-Gallegos, J.L., Quiroz-Reyes, A.G., Roacho-Perez, J.A., Benitez-Chao, D.F., Garza-Ocañas, L., Arevalo-Martinez, G., Garza-Treviño, E.N., Islas, J.F., 2023. The Involvement of Krüppel-like Factors in Cardiovascular Diseases. Life 13, 420. [CrossRef]
- Sarre-Álvarez, D., Cabrera-Jardines, R Rodríguez-Weber, F., 2018. Enfermedad cardiovascular aterosclerótica. Revisión de las escalas de riesgo y edad cardiovascular. Med Int Mex 6, 910–923.
- Shankman, L.S., Gomez, D., Cherepanova, O.A., Salmon, M., Alencar, G.F., Haskins, R.M., Swiatlowska, P., Newman, A.A.C., Greene, E.S., Straub, A.C., Isakson, B., Randolph, G.J., Owens, G.K., 2015. KLF4-dependent phenotypic modulation of smooth muscle cells has a key role in atherosclerotic plaque pathogenesis. Nat Med 21, 628–637. [CrossRef]
- Shindo, T., Manabe, I., Fukushima, Y., Tobe, K., Aizawa, K., Miyamoto, S., Kawai-Kowase, K., Moriyama, N., Imai, Y., Kawakami, H., Nishimatsu, H., Ishikawa, T., Suzuki, T., Morita, H., Maemura, K., Sata, M., Hirata, Y., Komukai, M., Kagechika, H., Kadowaki, T., Kurabayashi, M., Nagai, R., 2002. Krüppel-like zinc-finger transcription factor KLF5/BTEB2 is a target for angiotensin II signaling and an essential regulator of cardiovascular remodeling. Nat Med 8, 856–863. [CrossRef]
- Tetreault, M.-P.M.P., Yang, Y., Katz, JP.J.P., 2013. Krüppel-like factors in cancer. Nat Rev Cancer 13, 701–713. [CrossRef]
- Tsao, C.W., Aday, A.W., Almarzooq, Z.I., Anderson, C.A.M., Arora, P., Avery, C.L., Baker-Smith, C.M., Beaton, A.Z., Boehme, A.K., Buxton, A.E., Commodore-Mensah, Y., Elkind, M.S.V., Evenson, K.R., Eze-Nliam, C., Fugar, S., Generoso, G., Heard, D.G., Hiremath, S., Ho, J.E., Kalani, R., Kazi, D.S., Ko, D., Levine, D.A., Liu, J., Ma, J., Magnani, J.W., Michos, E.D., Mussolino, M.E., Navaneethan, S.D., Parikh, N.I., Poudel, R., Rezk-Hanna, M., Roth, G.A., Shah, N.S., St-Onge, M.-P., Thacker, E.L., Virani, S.S., Voeks, J.H., Wang, N.-Y., Wong, N.D., Wong, S.S., Yaffe, K., Martin, S.S., 2023. Heart Disease and Stroke Statistics—2023 Update: A Report From the American Heart Association. Circulation 147. [CrossRef]
- Varga, E., Pap, R., Jánosa, G., Sipos, K., Pandur, E., 2021. IL-6 Regulates Hepcidin Expression Via the BMP/SMAD Pathway by Altering BMP6, TMPRSS6 and TfR2 Expressions at Normal and Inflammatory Conditions in BV2 Microglia. Neurochem Res 46, 1224–1238. [CrossRef]
- Venugopal, H., Hanna, A., Humeres, C., Frangogiannis, N.G., 2022. Properties and Functions of Fibroblasts and Myofibroblasts in Myocardial Infarction. Cells 11, 1386. [CrossRef]
- Vinjamur, D.S., Wade, K.J., Mohamad, S.F., Haar, J.L., Sawyer, S.T., Lloyd, J.A., 2014. Krüppel-like transcription factors KLF1 and KLF2 have unique and coordinate roles in regulating embryonic erythroid precursor maturation. Haematologica 99, 1565–1573. [CrossRef]
- Wenying, L., Lu, H., Sun, J., Zhao, G., Wang, H., Guo, Y., Eitzman, D., Chen, E., Fan, Y., Zhang, J., 2021. KLF11 Protects against Venous Thrombosis via Suppressing Tissue Factor Expression. Thromb Haemost 122, 777–788. [CrossRef]
- WHO, 2020. The top 10 causes of death [WWW Document]. The top 10 causes of death. URL https://www.who.int/news-room/fact-sheets/detail/the-top-10-causes-of-death (accessed 8.2.23).
- Yang, H., Xi, X., Zhao, B., Su, Z., Wang, Z., 2018. KLF4 protects brain microvascular endothelial cells from ischemic stroke induced apoptosis by transcriptionally activating MALAT1. Biochem Biophys Res Commun 495, 2376–2382. [CrossRef]
- Zhang, Y., Lei, C.-Q., Hu, Y.-H., Xia, T., Li, M., Zhong, B., Shu, H.-B., 2014. Krüppel-like Factor 6 Is a Co-activator of NF-κB That Mediates p65-dependent Transcription of Selected Downstream Genes. Journal of Biological Chemistry 289, 12876–12885. [CrossRef]
- Zhang, Y., Wang, Y., Liu, Y., Wang, N., Qi, Y., Du, J., 2013. Krüppel-Like Factor 4 Transcriptionally Regulates TGF-β1 and Contributes to Cardiac Myofibroblast Differentiation. PLoS One 8, 0–9. [CrossRef]
- Zhang, Y., Zheng, Y., Wang, S., Fan, Y., Ye, Y., Jing, Y., Liu, Z., Yang, S., Xiong, M., Yang, K., Hu, J., Che, S., Chu, Q., Song, M., Liu, G.-H., Zhang, W., Ma, S., Qu, J., 2022. Single-nucleus transcriptomics reveals a gatekeeper role for FOXP1 in primate cardiac aging. Protein Cell. [CrossRef]
- Zheng, H., Pritchard, D.M., Yang, X., Bennett, E., Liu, G., Liu, C., Ai, W., 2009. KLF4 gene expression is inhibited by the notch signaling pathway that controls goblet cell differentiation in mouse gastrointestinal tract. AJP: Gastrointestinal and Liver Physiology 296, G490–G498. [CrossRef]
- Zhou, J., Herring, B.P., 2005. Mechanisms responsible for the promoter-specific effects of myocardin. J Biol Chem 280, 10861–9. [CrossRef]
- Zou, M.-L., Chen, Z.-H., Teng, Y.-Y., Liu, S.-Y., Jia, Y., Zhang, K.-W., Sun, Z.-L., Wu, J.-J., Yuan, Z.-D., Feng, Y., Li, X., Xu, R.-S., Yuan, F.-L., 2021. The Smad Dependent TGF-β and BMP Signaling Pathway in Bone Remodeling and Therapies. Front Mol Biosci 8. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).