Submitted:
31 August 2023
Posted:
01 September 2023
You are already at the latest version
Abstract
Keywords:
1. Introduction
2. Our Ancestral Hologenome
3. Molding and Managing the Next Generation
4. Our Microbes as Puppet Masters?
5. Our Conscious, Problem-Solving, Quatum-Operating Bacteria
6. Embodied Cognition and Meditation in the Holobiont
7. Connecting To and Through the IOM via Meditation, Embodied Cognition and Other Comtemplative Practices
8. Embodied Personality and Behavior
9. Conclusions
Author Contributions
Funding
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Twain, M. Three Thousand Years Among the Microbes. In Which Was the Dream? And Other Symbolic Writings of the Later Years; Tuckey, J.S., Ed.; University of California Press: Berkely and Los Angeles, CA USA; pp. 433–553.
- Dietert, R.; Dietert, J. The completed self: An immunological view of the human-microbiome superorganism and risk of chronic diseases. Entropy 2012, 14, 2036–2065. [Google Scholar] [CrossRef]
- Dietert, R.R.; Dietert, J. 2013. Science Sifting: Tools for Innovation in Science and Technology; World Scientific: Singapore: Singapore, 2013. [Google Scholar]
- Dietert, R.R. Integrating contemplative tools into biomedical science education and research training programs. J. Biomed. Educ. 2014, 2014, 239348. [Google Scholar] [CrossRef]
- Miller, W.B.; Baluška, F.; Reber, A.S. A revised central dogma for the 21st century: All biology is cognitive information processing. Prog. Biophys. Mol. Biol. 2023, 182, 34–48. [Google Scholar] [CrossRef] [PubMed]
- Dietert, R.R. The microbiome-immune-host defense barrier complex (microimmunosome) and developmental programming of noncommunicable diseases. Reprod. Toxicol. 2017, 68, 49–58. [Google Scholar] [CrossRef] [PubMed]
- Lee, C.K.; De Anda, J.; Baker, A.E.; Bennett, R.R.; Luo, Y.; Lee, E.Y.; Keefe, J.A.; Helali, J.S.; Ma, J.; Zhao, K.; Golestanian, R. Multigenerational memory and adaptive adhesion in early bacterial biofilm communities. Proc. Nat. Acad. Sci. USA 2018, 115, 4471–4476. [Google Scholar] [CrossRef] [PubMed]
- Wong, A.C.; Levy, M. Microbial memories. Immunity 2021, 54, 201–204. [Google Scholar] [CrossRef]
- Cross, K.L.; Leigh, B.A.; Hatmaker, E.A.; Mikaelyan, A.; Miller, A.K.; Bordenstein, S.R. Genomes of gut bacteria from Nasonia wasps shed light on phylosymbiosis and microbe-assisted hybrid breakdown. Msystems 2021, 6, e01342-20. [Google Scholar] [CrossRef]
- Brucker, R.M.; Bordenstein, S.R. The hologenomic basis of speciation: Gut bacteria cause hybrid lethality in the genus Nasonia. Science 2013, 341, 667–669. [Google Scholar] [CrossRef]
- Bell, K.; Bordenstein, S.R. A margulian view of symbiosis and speciation: The Nasonia wasp system. Symbiosis 2022, 87, 3–10. [Google Scholar] [CrossRef]
- Long, T.J. Home-Field Advantage: Why Host-Specificity is Important for Therapeutic Microbial Engraftment. Microbiol. Biotechnol. Lett. 2023, 51, 124–127. [Google Scholar] [CrossRef]
- Dietert, R.R. Microbiome First Medicine in Health and Safety. Biomedicines 2021, 9, 1099. [Google Scholar] [CrossRef]
- Barker, D.J. The fetal and infant origins of adult disease. BMJ 1990, 301, 1111. [Google Scholar] [CrossRef] [PubMed]
- Gluckman, P.D.; Hanson, M.A. The developmental origins of health and disease. In: Early life origins of health and disease, Adv. Exp. Med. Biol. 573, Wintour G.M.; Owens, J.A. Eds. Springer Science+Business Media Landes Bioscience / Eurekah.com, Georgetown, TX USA 2006, pp.1-7.
- Dietert, R.R.; Etzel, R.A.; Chen, D.; Halonen, M.; Holladay, S.D.; Jarabek, A.M.; Landreth, K.; Peden, D.B.; Pinkerton, K.; Smialowicz, R.J.; Zoetis, T. Workshop to identify critical windows of exposure for children's health: Immune and respiratory systems work group summary. Environ. Health Perspect. 2000, 108, 483–490. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, E.E.; Maamar, M.B.; Skinner, M.K. Environmentally Induced Epigenetic Transgenerational Inheritance and the Weismann Barrier: The Dawn of Neo-Lamarckian Theory. J. Dev. Biol. 2020, 8, 28. [Google Scholar] [CrossRef]
- Nilsson, E.E.; Ben Maamar, M.; Skinner, M.K. Role of epigenetic transgenerational inheritance in generational toxicology. Environ. Epigenet. 2022, 8, p.dvac001. [Google Scholar] [CrossRef] [PubMed]
- Nohesara, S.; Abdolmaleky, H.M.; Thiagalingam, S. Epigenetic Aberrations in Major Psychiatric Diseases Related to Diet and Gut Microbiome Alterations. Genes 2023, 14, 1506. [Google Scholar] [CrossRef]
- Marín-Tello, C.; Jintaridth, P.; Sanchez, F.; González, C.; Zelada-Castillo, L.; Vásquez-Arqueros, A.; Guevara-Vásquez, A.; Vieira, A. Epigenetic regulation by metabolites from the gut microbiome. Benef. Microbes 2022, 13, 437–443. [Google Scholar] [CrossRef]
- Banerjee, S.; Suter, M.A.; Aagaard, K.M. Interactions between environmental exposures and the microbiome: Implications for fetal programming. Curr. Opin. Endocr. Metab. Res. 2020, 13, 39–48. [Google Scholar] [CrossRef]
- Dreisbach, C.; Prescott, S.; Siega-Riz, A.M.; McCulloch, J.; Habermeyer, L.; Dudley, D.; Trinchieri, G.; Kelsey, C.; Alhusen, J. Composition of the maternal gastrointestinal microbiome as a predictor of neonatal birth weight. Pediatr. Res. 2023, 94, 1158–1165. [Google Scholar] [CrossRef]
- Gao, Y.; O’Hely, M.; Quinn, T.P.; Ponsonby, A.L.; Harrison, L.C.; Frøkiær, H.; Tang, M.L.; Brix, S.; Kristiansen, K.; Burgner, D.; Saffery, R. Maternal gut microbiota during pregnancy and the composition of immune cells in infancy. Front. Immunol. 2022, 13, 986340. [Google Scholar] [CrossRef]
- Nyangahu, D.D.; Jaspan, H.B. Influence of maternal microbiota during pregnancy on infant immunity. Clin. Exp. Immunol. 2019, 198, 47–56. [Google Scholar] [CrossRef] [PubMed]
- Tarrant, I.; Finlay, B.B. Like mother, like child: The maternal microbiome impacts offspring asthma. Cell Rep. Med. 2022, 3, 100722. [Google Scholar] [CrossRef] [PubMed]
- Di Gesù, C.M.; Matz, L.M.; Buffington, S.A. Diet-induced dysbiosis of the maternal gut microbiome in early life programming of neurodevelopmental disorders. Neurosci. Res. 2021, 168, 3–19. [Google Scholar] [CrossRef] [PubMed]
- Meckel, K.R.; Kiraly, D.D. Maternal microbes support fetal brain wiring. Nature 2020, 586, 203–205. [Google Scholar] [CrossRef]
- Vuong, H.E. Intersections of the microbiome and early neurodevelopment. Int. Rev. of Neurobiol. 2022, 167, 1–23. [Google Scholar] [CrossRef]
- Hsu, C.-N.; Yu, H.-R.; Chan, J.Y.H.; Wu, K.L.H.; Lee, W.-C.; Tain, Y.-L. The Impact of Gut Microbiome on Maternal Fructose Intake-Induced Developmental Programming of Adult Disease. Nutrients 2022, 14, 1031. [Google Scholar] [CrossRef]
- Dinan, T.G.; Stanton, C.; Cryan, J.F. Psychobiotics: A novel class of psychotropic. Biol. Psychiatry 2013, 74, 720–726. [Google Scholar] [CrossRef]
- Stilling, R.M.; Dinan, T.G.; Cryan, J.F. The brain’s Geppetto—Microbes as puppeteers of neural function and behaviour? J. Neurovirol. 2016, 22, 14–21. [Google Scholar] [CrossRef]
- Johnson, K.V.A.; Foster, K.R. Why does the microbiome affect behaviour? Nat. Rev. Microbiol. 2018, 16, 647–655. [Google Scholar] [CrossRef]
- Dietert, R.R.; Dietert, J.M. The Human Superorganism: Using Microbes for Freedom vs. Fear. Applied Microbiol. 2023, 3, 883–905. [Google Scholar] [CrossRef]
- Wang, P.; Wang, S.C.; Liu, X.; Jia, S.; Wang, X.; Li, T.; Yu, J.; Parpura, V.; Wang, Y.F. Neural functions of hypothalamic oxytocin and its regulation. ASN Neuro. 2022, 14, 17590914221100706. [Google Scholar] [CrossRef] [PubMed]
- Tolomeo, S.; Chiao, B.; Lei, Z.; Chew, S.H.; Ebstein, R.P. A novel role of CD38 and oxytocin as tandem molecular moderators of human social behavior. Neurosci. Biobehav. Rev. 2020, 115, 251–272. [Google Scholar] [CrossRef]
- Walter, M.H.; Abele, H.; Plappert, C.F. The role of oxytocin and the effect of stress during childbirth: Neurobiological basics and implications for mother and child. Front. Endocrinol. 2021, 12, 1409. [Google Scholar] [CrossRef] [PubMed]
- Pekarek, B.T.; Hunt, P.J.; Arenkiel, B.R. Oxytocin and sensory network plasticity. Front. Neurosci. 2020, 14, 30. [Google Scholar] [CrossRef] [PubMed]
- Lee, H.J.; Macbeth, A.H.; Pagani, J.H.; Young 3rd, W.S. Oxytocin: The great facilitator of life. Prog. Neurobiol. 2009, 88, 127–151. [Google Scholar] [CrossRef] [PubMed]
- Carter, C.S.; Kenkel, W.M.; MacLean, E.L.; Wilson, S.R.; Perkeybile, A.M.; Yee, J.R.; Ferris, C.F.; Nazarloo, H.P.; Porges, S.W.; Davis, J.M.; Connelly, J.J. Is oxytocin “nature’s medicine”? Pharmacol. Rev. 2020, 72, 829–861. [Google Scholar] [CrossRef]
- Nunes, A.R.; Gliksberg, M.; Varela, S.A.; Teles, M.; Wircer, E.; Blechman, J.; Petri, G.; Levkowitz, G.; Oliveira, R.F. Developmental effects of oxytocin neurons on social affiliation and processing of social information. J. Neurosci. 2021, 41, 8742–8760. [Google Scholar] [CrossRef]
- Froemke, R.C.; Young, L.J. Oxytocin, neural plasticity, and social behavior. Annu. Rev. Neurosci. 2021, 44, 359–381. [Google Scholar] [CrossRef]
- Nagpal, J.; Cryan, J.F. Host genetics, the microbiome & behaviour—A ‘Holobiont’perspective. Cell Res. 2021, 31, 832–833. [Google Scholar] [CrossRef]
- Natochin, Y.V.; Orlova, O.G.; Rybalchenko, O.V.; Shakhmatova, E.I. Vasopressin and Oxytocin Secretion by Microorganisms. Microbiology 2022, 91, 104–106. [Google Scholar] [CrossRef]
- Lyon, L. ‘All disease begins in the gut’: Was Hippocrates right? Brain 2018, 141, e20. [Google Scholar] [CrossRef] [PubMed]
- Varian, B.J.; Poutahidis, T.; DiBenedictis, B.T.; Levkovich, T.; Ibrahim, Y.; Didyk, E.; Shikhman, L.; Cheung, H.K.; Hardas, A.; Ricciardi, C.E.; and Kolandaivelu, K. Microbial lysate upregulates host oxytocin. Brain Behave. Immune. 2017, 61, 36–49. [Google Scholar] [CrossRef] [PubMed]
- Lakshmi, G.B.V.S.; Yadav, A.K.; Mehlawat, N.; Jalandra, R.; Solanki, P.R.; Kumar, A. Gut microbiota derived trimethylamine N-oxide (TMAO) detection through molecularly imprinted polymer based sensor. Sci. Rep. 2021, 11, 1338. [Google Scholar] [CrossRef] [PubMed]
- Luo, Y.; Zhao, P.; Dou, M.; Mao, J.; Zhang, G.; Su, Y.; Wang, Q.; Wang, Q.; Wang, Y.; Sun, R.; Liu, T. Exogenous microbiota-derived metabolite trimethylamine N-oxide treatment alters social behaviors: Involvement of hippocampal metabolic adaptation. Neuropharmacology 2021, 191, 108563. [Google Scholar] [CrossRef]
- Lee, Y.; Kang, J.S.; Ham, O.J.; Son, M.Y.; Lee, M.O. Gut metabolite trimethylamine N-oxide induces aging-associated phenotype of midbrain organoids for the induced pluripotent stem cell-based modeling of late-onset disease. Front. Aging Neurosci. 2022, 14, 925227. [Google Scholar] [CrossRef]
- Legan, T.B.; Lavoie, B.; and Mawe, G.M. Direct and indirect mechanisms by which the gut microbiota influence host serotonin systems. Neurogastroenterol. Motil. 2022, 34, e14346. [Google Scholar] [CrossRef]
- Margolis, K.G.; Cryan, J.F.; Mayer, E.A. The microbiota-gut-brain axis: From motility to mood. Gastroenterology 2021, 160, 1486–1501. [Google Scholar] [CrossRef]
- Hamamah, S.; Aghazarian, A.; Nazaryan, A.; Hajnal, A.; Covasa, M. Role of Microbiota-Gut-Brain Axis in Regulating Dopaminergic Signaling. Biomedicines 2022, 10, 436. [Google Scholar] [CrossRef]
- Miller, A.K.; Westlake, C.S.; Cross, K.L.; Leigh, B.A.; Bordenstein, S.R. The microbiome impacts host hybridization and speciation. PLoS Biol. 2021, 19, e3001417. [Google Scholar] [CrossRef]
- Alberdi, A.; Andersen, S.B.; Limborg, M.T.; Dunn, R.R.; Gilbert, M.T.P. Disentangling host–microbiota complexity through hologenomics. Nature Rev. Genet. 2022, 23, 281–297. [Google Scholar] [CrossRef]
- Rosenberg, E. and Zilber-Rosenberg, I., 2019. The hologenome concept of evolution: Medical implications. Rambam Maimonides Med. J. 2019, 10, e0005. [Google Scholar] [CrossRef] [PubMed]
- Lin, C.; Lin, Y.; Zhang, H.; Wang, G.; Zhao, J.; Zhang, H.; Chen, W. Intestinal ‘Infant-Type’ Bifidobacteria Mediate Immune System Development in the First 1000 Days of Life. Nutrients 2022, 14, 1498. [Google Scholar] [CrossRef]
- Hunter, S.; Flaten, E.; Petersen, C.; Gervain, J.; Werker, J.F.; Trainor, L.J.; Finlay, B.B. Babies, bugs and brains: How the early microbiome associates with infant brain and behavior development. PLoS ONE 2023, 18, e0288689. [Google Scholar] [CrossRef] [PubMed]
- Schamarek, I.; Anders, L.; Chakaroun, R.M.; Kovacs, P.; Rohde-Zimmermann, K. The role of the oral microbiome in obesity and metabolic disease: Potential systemic implications and effects on taste perception. Nutr. J. 2023, 22, 1–13. [Google Scholar] [CrossRef] [PubMed]
- de Wouters d’Oplinter, A.; Verce, M.; Huwart, S.J.; Lessard-Lord, J.; Depommier, C.; Van Hul, M.; Desjardins, Y.; Cani, P.D.; Everard, A. Obese-associated gut microbes and derived phenolic metabolite as mediators of excessive motivation for food reward. Microbiome 2023, 11, 94. [Google Scholar] [CrossRef]
- Butler, M.I.; Cryan, J.F.; Dinan, T.G. Man and the microbiome: A new theory of everything? Annu. Rev. of Clin. Psychol. 2019, 15, 371–398. [Google Scholar] [CrossRef]
- Zhu, R.; Fang, Y.; Li, H.; Liu, Y.; Wei, J.; Zhang, S.; Wang, L.; Fan, R.; Wang, L.; Li, S.; Chen, T. Psychobiotic Lactobacillus plantarum JYLP-326 relieves anxiety, depression, and insomnia symptoms in test anxious college via modulating the gut microbiota and its metabolism. Front. Immunol. 2023, 14, 1158137. [Google Scholar] [CrossRef]
- Chu, C.; Murdock, M.H.; Jing, D.; Won, T.H.; Chung, H.; Kressel, A.M.; Tsaava, T.; Addorisio, M.E.; Putzel, G.G.; Zhou, L.; Bessman, N.J. The microbiota regulate neuronal function and fear extinction learning. Nature 2019, 574, 543–548. [Google Scholar] [CrossRef]
- Maeng, L.Y.; Beumer, A. Never fear, the gut bacteria are here: Estrogen and gut microbiome-brain axis interactions in fear extinction. Int. J. Psychophysiol. 2023, 189, 66–75. [Google Scholar] [CrossRef]
- Sherwin, E.; Bordenstein, S.R.; Quinn, J.L.; Dinan, T.G.; Cryan, J.F. Microbiota and the social brain. Science 2019, 366, eaar2016. [Google Scholar] [CrossRef]
- Butler, M.I.; Bastiaanssen, T.F.; Long-Smith, C.; Morkl, S.; Berding, K.; Ritz, N.L.; Strain, C.; Patangia, D.; Patel, S.; Stanton, C.; O’Mahony, S.M. The gut microbiome in social anxiety disorder: Evidence of altered composition and function. Transl. Psychiatry 2023, 13, 95. [Google Scholar] [CrossRef] [PubMed]
- Cuesta-Marti, C.; Uhlig, F.; Muguerza, B.; Hyland, N.; Clarke, G.; Schellekens, H. Microbes, oxytocin and stress: Converging players regulating eating behavior. J. Neuroendocrinol. 2023, 15, e13243. [Google Scholar] [CrossRef] [PubMed]
- Vijay, A.; Valdes, A.M. Role of the gut microbiome in chronic diseases: A narrative review. Eur.J. Clin Nutr. 2022, 76, 489–501. [Google Scholar] [CrossRef] [PubMed]
- Davies, M.; Galazzo, G.; van Hattem, J.M.; Arcilla, M.S.; Melles, D.C.; de Jong, M.D.; Schultsz, C.; Wolffs, P.; McNally, A.; Schaik, W.V.; Penders, J. Enterobacteriaceae and Bacteroidaceae provide resistance to travel-associated intestinal colonization by multi-drug resistant Escherichia coli. Gut Microbes 2022, 14, 2060676. [Google Scholar] [CrossRef]
- Duar, R.M.; Kyle, D.; Casaburi, G. Colonization resistance in the infant gut: The role of B. infantis in reducing pH and preventing pathogen growth. High Throughput 2020, 9, 7. [Google Scholar] [CrossRef]
- Rowe, M.; Veerus, L.; Trosvik, P.; Buckling, A.; Pizzari, T. The reproductive microbiome: An emerging driver of sexual selection, sexual conflict, mating systems, and reproductive isolation. Trends Ecol. Evol. 2020, 35, 220–234. [Google Scholar] [CrossRef]
- Toson, B.; Simon, C.; Moreno, I. The endometrial microbiome and its impact on human conception. Int. J. Mol. Sci. 2022, 23, 485. [Google Scholar] [CrossRef]
- Wang, H.; Xu, A.; Gong, L.; Chen, Z.; Zhang, B.; Li, X. The microbiome, an important factor that is easily overlooked in male infertility. Front. Microbiol. 2022, 13, 831272. [Google Scholar] [CrossRef]
- Günther, V.; Allahqoli, L.; Watrowski, R.; Maass, N.; Ackermann, J.; von Otte, S.; Alkatout, I. Vaginal microbiome in reproductive medicine. Diagnostics 2022, 12, 1948. [Google Scholar] [CrossRef]
- Assis, V.; de Sousa Neto, I.V.; Ribeiro, F.M.; de Cassia Marqueti, R.; Franco, O.L.; da Silva Aguiar, S.; Petriz, B. The Emerging Role of the Aging Process and Exercise Training on the Crosstalk between Gut Microbiota and Telomere Length. Int. J. Environ. Res. Public Health 2022, 19, 7810. [Google Scholar] [CrossRef]
- Boopathi, S.; Kumar, R.S.; Priya, P.S.; Haridevamuthu, B.; Nayak, S.R.R.; Laura, C. Kushugulova, A.; Arockiaraj, J. Gut Enterobacteriaceae and uraemic toxins-Perpetrators for ageing. Exp. Gerontol. 2023, 173, 112088. [Google Scholar] [CrossRef] [PubMed]
- Ragonnaud, E.; Biragyn, A. Gut microbiota as the key controllers of “healthy” aging of elderly people. Immun. Ageing 2021, 18, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Dietert, R.R.; Dietert, J.M. Using Microbiome-Based Approaches to Deprogram Chronic Disorders and Extend the Healthspan following Adverse Childhood Experiences. Microorganisms 2022, 10, 229. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Wang, M.; Qi, X.; Shi, L.; Zhang, J.; Zhang, X.; Yang, T.; Ren, J.; Liu, F.; Zhang, G.; Yan, J. Predicting the postmortem interval of burial cadavers based on microbial community succession. Forensic Science Int. Genetics 2021, 52, 102488. [Google Scholar] [CrossRef]
- Zapico, S.C.; Adserias-Garriga, J. Postmortem Interval Estimation: New Approaches by the Analysis of Human Tissues and Microbial Communities’ Changes. Forensic Sci. 2022, 2, 163–174. [Google Scholar] [CrossRef]
- Buckeridge, K.M.; Mason, K.E.; McNamara, N.P.; Ostle, N.; Puissant, J.; Goodall, T.; Griffiths, R.I.; Stott, A.W.; Whitaker, J. Environmental and microbial controls on microbial necromass recycling, an important precursor for soil carbon stabilization. Commun. Earth Environ. 2020, 1, 1–9. [Google Scholar] [CrossRef]
- Wang, B.; An, S.; Liang, C.; Liu, Y.; Kuzyakov, Y. Microbial necromass as the source of soil organic carbon in global ecosystems. Soil Biology and Biochemistry 2021, 162, 108422. [Google Scholar] [CrossRef]
- Sagan, L. On the origin of mitosing cells. J. Theor. Biol. 1967, 14, 225–274. [Google Scholar] [CrossRef]
- Miller, W.B. Cognition, Information Fields and Hologenomic Entanglement: Evolution in Light and Shadow. Biology 2016, 5, 21. [Google Scholar] [CrossRef]
- Miller, W.B., Jr.; Enguita, F.J.; Leitão, A.L. Non-Random Genome Editing and Natural Cellular Engineering in Cognition-Based Evolution. Cells 2021, 10, 1125. [Google Scholar] [CrossRef]
- Podolsky, S.H. Metchnikoff and the microbiome. Lancet 2012, 380, 1810–1811. [Google Scholar] [CrossRef]
- Sato, N. Mereschkowsky, Founder of Endosymbiotic Hypothesis. In Endosymbiotic Theories of Organelles Revisited; Springer: Singapore; pp. 23–31. [CrossRef]
- Kowallik, K.V.; Martin, W.F. The origin of symbiogenesis: An annotated English translation of Mereschkowsky's 1910 paper on the theory of two plasma lineages. Biosystems 2021, 199, 104281. [Google Scholar] [CrossRef] [PubMed]
- Meyer-Abich, A. Hauptgedanken des holismus. Acta Biotheor. 1940, 5, 85–116. [Google Scholar] [CrossRef]
- Meyer-Abich, A. Hauptgedanken des holismus. Acta Biotheor. 1955, 11, 85–106. [Google Scholar] [CrossRef]
- Amidon, K.S. Adolf Meyer-Abich, holism, and the negotiation of theoretical biology. Biol. Theory 2008, 3, 357–370. [Google Scholar] [CrossRef]
- Obert, M.; Pfeifer, P.; Sernetz, M. Microbial growth patterns described by fractal geometry. J. Bacteriol. 1990, 172, 1180–1185. [Google Scholar] [CrossRef]
- Margulis, L. The conscious cell. Ann. N Y Acad. Sci. 2001, 929, 55–70. [Google Scholar] [CrossRef]
- Shapiro, J.A. Bacteria are small but not stupid: Cognition, natural genetic engineering and socio-bacteriology. Stud. Hist. Phil. Biol. Biomed. Sci. 2008, 38, 807–819. [Google Scholar] [CrossRef]
- Nijland, R.; Burgess, J.G. Bacterial olfaction. Biotech. J. 2010, 5, 974–977. [Google Scholar] [CrossRef]
- Blaser, M.J. Missing microbes: How the overuse of antibiotics is fueling our modern plagues; Henry Holt and Co: New York, NY USA, 2014; 288p. [Google Scholar]
- Lyon, P. The cognitive cell: Bacterial behavior reconsidered. Front. Microbiol. 2015, 6, 264. [Google Scholar] [CrossRef]
- Pinto, D.; Mascher, T. (Actino) Bacterial “intelligence”: Using comparative genomics to unravel the information processing capacities of microbes. Curr. Genet. 2016, 62, 487–498. [Google Scholar] [CrossRef] [PubMed]
- Baghbanzadeh, S.; Kassal, I. Geometry, supertransfer, and optimality in the light harvesting of purple bacteria. J. Phys. Chem. Lett. 2016, 7, 3804–3811. [Google Scholar] [CrossRef] [PubMed]
- Marletto, C.; Coles, D.M.; Farrow, T.; Vedral, V. Entanglement between living bacteria and quantized light witnessed by Rabi splitting. J. Physics Comm. 2018, 2, 101001. [Google Scholar] [CrossRef]
- Torday, J.S.; Miller Jr, W.B. The Cosmologic continuum from physics to consciousness. Prog. Biophys. Mol. Biol. 2018, 140, 41–48. [Google Scholar] [CrossRef] [PubMed]
- Miller Jr, W.B.; Baluška, F.; Torday, J.S. Cellular senomic measurements in cognition-based evolution. Prog. in Biophys. Mol. Biol. 2020, 156, 20–33. [Google Scholar] [CrossRef]
- Miller Jr, W.B.; Torday, J.S.; Baluška, F. The N-space Episenome unifies cellular information space-time within cognition-based evolution. Prog. Biophys. Mol. Biol. 2020, 150, 112–139. [Google Scholar] [CrossRef]
- Reber, A.S.; Baluška, F. Cognition in some surprising places. Biochem. Biophys. Res. Commun. 2021, 564, 150–157. [Google Scholar] [CrossRef]
- Palacios-García, I.; Parada, F.J. The holobiont mind: A bridge between 4E cognition and the microbiome. Adapt. Behav. 2021, 10597123211053071. [Google Scholar] [CrossRef]
- Higgins, J.S.; Lloyd, L.T.; Sohail, S.H.; Allodi, M.A.; Otto, J.P.; Saer, R.G.; Wood, R.E.; Massey, S.C.; Ting, P.C.; Blankenship, R.E.; Engel, G.S. Photosynthesis tunes quantum-mechanical mixing of electronic and vibrational states to steer exciton energy transfer. Proc. Natl. Acad. Sci. U S A 2021, 118, e2018240118. [Google Scholar] [CrossRef]
- Dani, R.; Kundu, S.; Makri, N. Coherence Maps and Flow of Excitation Energy in the Bacterial Light Harvesting Complex 2. J. Phys. Chem. Lett. 2023, 14, 3835–3843. [Google Scholar] [CrossRef]
- Schwartz, S.A.; 2023. Science slowly accepts the matrix of consciousness. Explore (NY) 2023, 19, 3–5. [Google Scholar] [CrossRef] [PubMed]
- Delgado, F.; Enríquez, M. Quantum Entanglement and State-Transference in Fenna–Matthews–Olson Complexes: A Post-Experimental Simulation Analysis in the Computational Biology Domain. Int. J. Mol. Sci. 2023, 24, 10862. [Google Scholar] [CrossRef] [PubMed]
- Cupellini, L.; Qian, P.; Nguyen-Phan, T.C.; Gardiner, A.T.; Cogdell, R.J. Quantum chemical elucidation of a sevenfold symmetric bacterial antenna complex. Photosynth. Res. 2023, 156, 75–87. [Google Scholar] [CrossRef] [PubMed]
- Scheil, V.; Holzinger, R.; Moreno-Cardoner, M.; Ritsch, H. Optical Properties of Concentric Nanorings of Quantum Emitters. Nanomaterials 2023, 13, 851. [Google Scholar] [CrossRef]
- Varela, F.J.; Thompson, E.; Rosch, E. The Embodied Mind: Cognitive Science and Human Experience, 1st ed.; The MIT Press: Cambridge, MA USA, 1991; 308p, https://archive.org/details/embodiedmindcogn0000vare/page/n5/mode/2up (accessed on 29 August 2023).
- Matko, K.; Sedlmeier, P. What is meditation? Proposing an empirically derived classification system. Front. Psychol. 2019, 10, 2276. [Google Scholar] [CrossRef]
- Euler, E.; Rådahl, E.; and Gregorcic, B. Embodiment in physics learning: A social-semiotic look. Physical Rev. Physics Educ. Res. 2019, 15, 010134. [Google Scholar] [CrossRef]
- Kersting, M.; Haglund, J.; Steier, R. A growing body of knowledge: On four different senses of embodiment in science education. Sci. & Educ. 2021, 30, 1183–1210. [Google Scholar] [CrossRef]
- Buono, A.; Burnidge, A. Dancing Our Microbiome at the Science Museum: A Dance/STEAM Collaboration. J. Dance Educ. 2022, 22, 98–107. [Google Scholar] [CrossRef]
- Perlovsky, L. Origin of music and embodied cognition. Front. Psychol. 2015, 6, 538. [Google Scholar] [CrossRef]
- Wang, Z.; Liu, S.; Xu, X.; Xiao, Y.; Yang, M.; Zhao, X.; Jin, C.; Hu, F.; Yang, S.; Tang, B.; Song, C. Gut microbiota associated with effectiveness and responsiveness to mindfulness-based cognitive therapy in improving trait anxiety. Front. Cell. Infect. Microbiol. 2022, 12, 719829. [Google Scholar] [CrossRef]
- Shatkin-Margolis, A.; White, J.; Jedlicka, A.E.; Tam, T.; Hill, A.; Yeung, J.; Crisp, C.C.; Pauls, R.N. The effect of mindfulness-based stress reduction on the urinary microbiome in interstitial cystitis. Int. Urogynecology Journal 2022, 33, 665–671. [Google Scholar] [CrossRef]
- Zhang, X.; Mao, F.; Li, Y.; Wang, J.; Wu, L.; Sun, J.; Cao, F. Effects of a maternal mindfulness intervention targeting prenatal psychological distress on infants’ meconium microbiota: A randomized controlled trial. Psychoneuroendocrinology 2022, 145, 105913. [Google Scholar] [CrossRef]
- Khine, W.W.T.; Voong, M.L.; Ng, T.K.S.; Feng, L.; Rane, G.A.; Kumar, A.P.; Kua, E.H.; Mahendran, R.; Mahendran, R.; Lee, Y.K. Mental awareness improved mild cognitive impairment and modulated gut microbiome. Aging (Albany NY) 2020, 12, 24371–24393. [Google Scholar] [CrossRef] [PubMed]
- Sun, Y.; Ju, P.; Xue, T.; Ali, U.; Cui, D.; Chen, J. Alteration of faecal microbiota balance related to long-term deep meditation. Gen. Psychiatr. 2023, 36, e100893. [Google Scholar] [CrossRef]
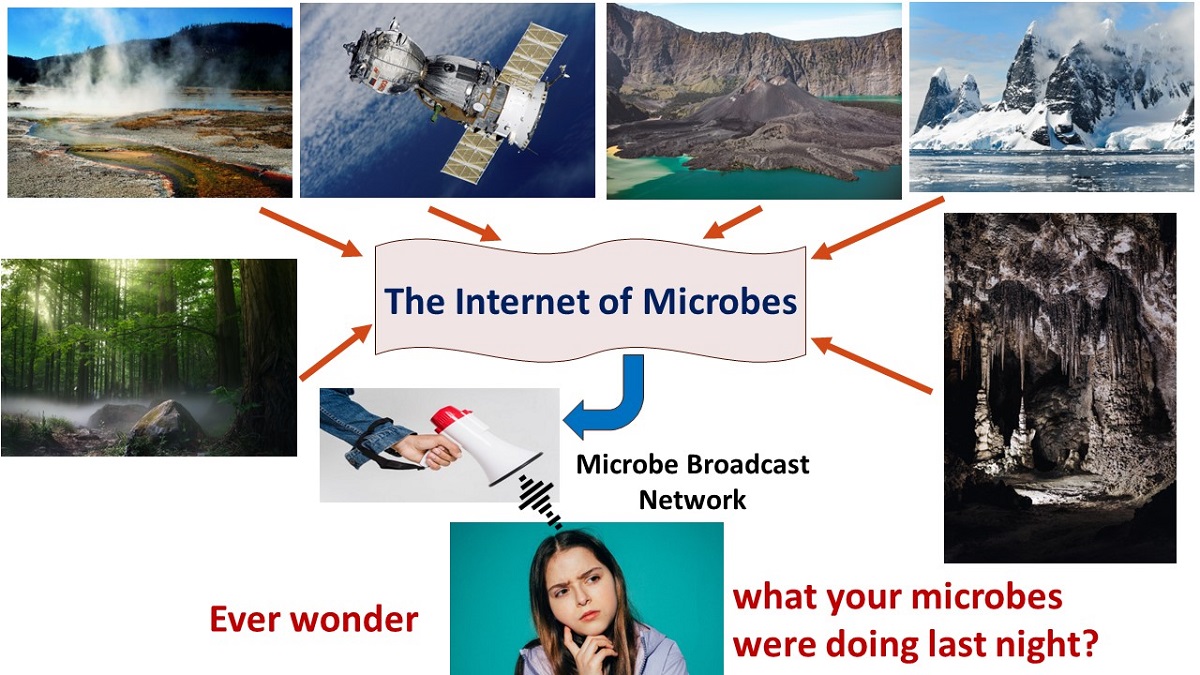
- Slijepcevic, P.; Wickramasinghe, N.C. An internet of microbes straddling the cosmos. Adv. Genet. 2020, 106, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Dietert, R.R.; Dietert, J.M. Using the Internet of Microbes to Survive the Assault on the Human Microbiome. Amer. J. Biomed. Sci. Res. 2023, 19, AJBSR.MS.ID.002552. [Google Scholar] [CrossRef]
- Weil, M.; Hoff, K.J.; Meißner, W.; Schäfer, F.; Söllinger, A.; Wang, H.; Hagenau, L.; Kuss, A.W.; Urich, T. Full genome sequence of a methanomassiliicoccales representative enriched from peat soil. Microb. Resour. Announc. 2021, 10, e00443-21. [Google Scholar] [CrossRef]
- Mafra, D.; Ribeiro, M.; Fonseca, L.; Regis, B.; Cardozo, L.F.; Dos Santos, H.F.; de Jesus, H.E.; Schultz, J.; Shiels, P.G.; Stenvinkel, P.; Rosado, A. Archaea from the gut microbiota of humans: Could be linked to chronic diseases? Anaerobe 2022, 77, 102629. [Google Scholar] [CrossRef]
- Cozannet, M.; Borrel, G.; Roussel, E.; Moalic, Y.; Allioux, M.; Sanvoisin, A.; Toffin, L.; Alain, K. New insights into the ecology and physiology of Methanomassiliicoccales from terrestrial and aquatic environments. Microorganisms 2020, 9, 30. [Google Scholar] [CrossRef]
- Umbach, A.K.; Stegelmeier, A.A.; Neufeld, J.D. Archaea are rare and uncommon members of the mammalian skin microbiome. Msystems 2021, 6, e00642-21. [Google Scholar] [CrossRef]
- DasSarma, S.; DasSarma, P.; Laye, V.J.; Schwieterman, E.W. Extremophilic models for astrobiology: Haloarchaeal survival strategies and pigments for remote sensing. Extremophiles 2020, 24, 31–41. [Google Scholar] [CrossRef]
- Krawczyk, K.T.; Locht, C.; Kowalewicz-Kulbat, M. Halophilic archaea Halorhabdus rudnickae and Natrinema salaciae activate human dendritic cells and orient T helper cell responses. Front. Immunol. 2022, 13, 833635. [Google Scholar] [CrossRef]
- Gupta, A.; Saha, A.; Sar, P. Thermoplasmata and Nitrososphaeria as dominant archaeal members in acid mine drainage sediment of Malanjkhand Copper Project, India. Arch. Microbiol. 2021, 203, 1833–1841. [Google Scholar] [CrossRef] [PubMed]
- St. John, E.; Flores, G.E.; Meneghin, J.; Reysenbach, A.L. Deep-sea hydrothermal vent metagenome-assembled genomes provide insight into the phylum Nanoarchaeota. Environ. Microbiol. Rep. 2019, 11, 262–270. [Google Scholar] [CrossRef] [PubMed]
- Munson-McGee, J.H.; Rooney, C.; Young, M.J. An uncultivated virus infecting a nanoarchaeal parasite in the hot springs of Yellowstone National Park. J. Virol. 2020, 94, e01213-01219. [Google Scholar] [CrossRef] [PubMed]
- Natan, E.; Fitak, R.R.; Werber, Y.; Vortman, Y. Symbiotic magnetic sensing: Raising evidence and beyond. Philos. Trans. R. Soc. Lond. B Biol. Sci. 2020, 375, 20190595. [Google Scholar] [CrossRef]
- Lin, W.; Wu, L.F. Magnetotactic bacteria and magnetoreception. J. Oceanol. Limnol. 2021, 39, 2001–2004. [Google Scholar] [CrossRef]
- Li, J.; Liu, P.; Menguy, N.; Zhang, X.; Wang, J.; Benzerara, K.; Feng, L.; Sun, L.; Zheng, Y.; Meng, F.; Gu, L. Intracellular silicification by early-branching magnetotactic bacteria. Sci. Adv. 2022, 8, eabn6045. [Google Scholar] [CrossRef]
- Simon, R.A.; Ranasinghe, P.D.; Barazanji, N.; Jungeström, M.B.; Xu, J.; Bednarska, O.; Serrander, L.; Engström, M.; Bazylinski, D.A.; Keita, Å.V.; Walter, S. Magnetotactic bacteria from the human gut microbiome associated with orientation and navigation regions of the brain. J. Oceanol. Limnol. 2021, 39, 2044–2052. [Google Scholar] [CrossRef]
- Icer, M.A.; Özbay, S.; Ağagündüz, D.; Kelle, B.; Bartkiene, E.; Rocha, J.M.F.; Ozogul, F. The Impacts of Acidophilic Lactic Acid Bacteria on Food and Human Health: A Review of the Current Knowledge. Foods 2023, 12, 2965. [Google Scholar] [CrossRef]
- Saha, U.B.; Saroj, S.D. Lactic acid bacteria: Prominent player in the fight against human pathogens. Expert Rev.of Anti Infect Ther. 2022, 20, 1435–1453. [Google Scholar] [CrossRef]
- Al-Balawi, M.; Morsy, F.M. Enterococcus faecalis is a better competitor than other lactic acid bacteria in the initial colonization of colon of healthy newborn babies at first week of their life. Front. Microbiol. 2020, 11, 2017. [Google Scholar] [CrossRef]
- Zhang, D.; Zhang, J.; Kalimuthu, S.; Liu, J.; Song, Z.M.; He, B.B.; Cai, P.; Zhong, Z.; Feng, C.; Neelakantan, P.; Li, Y.X. A systematically biosynthetic investigation of lactic acid bacteria reveals diverse antagonistic bacteriocins that potentially shape the human microbiome. Microbiome 2023, 11, 91. [Google Scholar] [CrossRef]
- Santer, M. Joseph Lister: First use of a bacterium as a 'model organism' to illustrate the cause of infectious disease of humans. Notes Rec. R Soc. Lond. 2010, 20, 59–65. [Google Scholar] [CrossRef]
- Selway, C.A.; Mills, J.G.; Weinstein, P.; Skelly, C.; Yadav, S.; Lowe, A.; Breed, M.F.; Weyrich, L.S. Transfer of environmental microbes to the skin and respiratory tract of humans after urban green space exposure. Environ. Int. 2020, 145, 106084. [Google Scholar] [CrossRef]
- Mhuireach, G.Á.; Van Den Wymelenberg, K.G.; Langellotto, G.A. Garden soil bacteria transiently colonize gardeners' skin after direct soil contact. Urban Agric. Region. Food Syst. 2023, 8, 1–22. [Google Scholar] [CrossRef]
- Gruber, C.; Legat, A.; Pfaffenhuemer, M.; Radax, C.; Weidler, G.; Busse, H.J.; Stan-Lotter, H. Halobacterium noricense sp. nov., an archaeal isolate from a bore core of an alpine Permian salt deposit, classification of Halobacterium sp. NRC-1 as a strain of H. salinarum and emended description of H. salinarum. Extremophiles 2004, 8, 431–439. [Google Scholar] [CrossRef] [PubMed]
- Wu, J.H.; McGenity, T.J.; Rettberg, P.; Simões, M.F.; Li, W.J.; Antunes, A. The archaeal class Halobacteria and astrobiology: Knowledge gaps and research opportunities. Front. Microbiol. 2022, 13, 1023625. [Google Scholar] [CrossRef] [PubMed]
- Agioutantis, P.; Koumandou, V.L. Bioenergetic diversity of the human gut microbiome. Meta Gene 2018, 16, 10, 14. [Google Scholar] [CrossRef]
- Barker, C.F.; and Markmann, J.F. Historical overview of transplantation. Cold Spring Harb. Perspect. Med. 2013, 3, a014977. [Google Scholar] [CrossRef]
- Stolf, N.A. History of heart transplantation: A hard and glorious journey. Braz.J. Cardiovasc. Surg. 2017, 32, 423–427. [Google Scholar] [CrossRef] [PubMed]
- Bunzel, B.; Schmidl-Mohl, B.; Grundböck, A.; Wollenek, G. Does changing the heart mean changing personality? A retrospective inquiry on 47 heart transplant patients. Qual.Life Res. 1992, 1, 251–256. [Google Scholar] [CrossRef] [PubMed]
- Pearsall, P.; Schwartz, G.E.; Russek, L.G. Changes in heart transplant recipients that parallel the personalities of their donors. Integr. Med 2000, 2, 65–72. [Google Scholar] [CrossRef] [PubMed]
- Liester, M.B. Personality changes following heart transplantation: The role of cellular memory. Med. Hypotheses 2020, 135, 109468. [Google Scholar] [CrossRef]
- Joshi, S. Memory transference in organ transplant recipients. J. New Approaches Med. Health 2011, 19. https://www.namahjournal.com/doc/Actual/Memory-transference-in-organ-transplant-recipients-vol-19-iss-1.html (accessed on 29 August 2023).
- Lakota, J.; Jagla, F.; Pecháňová, O. Heart memory or can transplanted heart manipulate recipients brain control over mind body interactions? Act Nerv Super Rediviva 2021, 63, 49–51. [Google Scholar]
- Kang, D.W.; Adams, J.B.; Gregory, A.C.; Borody, T.; Chittick, L.; Fasano, A.; Khoruts, A.; Geis, E.; Maldonado, J.; McDonough-Means, S.; Pollard, E.L. Microbiota transfer therapy alters gut ecosystem and improves gastrointestinal and autism symptoms: An open-label study. Microbiome 2017, 5, 1–16. [Google Scholar] [CrossRef]
- Kang, D.W.; Adams, J.B.; Coleman, D.M.; Pollard, E.L.; Maldonado, J.; McDonough-Means, S.; Caporaso, J.G.; Krajmalnik-Brown, R. Long-term benefit of Microbiota Transfer Therapy on autism symptoms and gut microbiota. Sci. Rep. 2019, 9, 5821. [Google Scholar] [CrossRef]
- Dossaji, Z.; Khattak, A.; Tun, K.M.; Hsu, M.; Batra, K.; Hong, A.S. Efficacy of Fecal Microbiota Transplant on Behavioral and Gastrointestinal Symptoms in Pediatric Autism: A Systematic Review. Microorganisms 2023, 11, 806. [Google Scholar] [CrossRef]
- Li, N.; Chen, H.; Cheng, Y.; Xu, F.; Ruan, G.; Ying, S.; Tang, W.; Chen, L.; Chen, M.; Lv, L.; Ping, Y. Fecal microbiota transplantation relieves gastrointestinal and autism symptoms by improving the gut microbiota in an open-label study. Front. Cellular Infect. Microbiol. 2021, 11, 759435. [Google Scholar] [CrossRef]
- Avolio, E.; Olivito, I.; Rosina, E.; Romano, L.; Angelone, T.; De Bartolo, A.; Scimeca, M.; Bellizzi, D.; D'Aquila, P.; Passarino, G.; Alò, R. Modifications of Behavior and Inflammation in Mice Following Transplant with Fecal Microbiota from Children with Autism. Neuroscience 2022, 498, 174–189. [Google Scholar] [CrossRef] [PubMed]
- Nassar, S.T.; Tasha, T.; Desai, A.; Bajgain, A.; Ali, A.; Dutta, C.; Pasha, K.; Paul, S.; Abbas, M.S.; Venugopal, S.; ABBAS, M.S. Fecal Microbiota Transplantation Role in the Treatment of Alzheimer's Disease: A Systematic Review. Cureus 2022, 14. [Google Scholar] [CrossRef] [PubMed]
- Park, S.H.; Lee, J.H.; Shin, J.; Kim, J.S.; Cha, B.; Lee, S.; Kwon, K.S.; Shin, Y.W.; Choi, S.H. Cognitive function improvement after fecal microbiota transplantation in Alzheimer’s dementia patient: A case report. Curr. Med. Res. Opin. 2021, 37, 1739–1744. [Google Scholar] [CrossRef]
- Park, S.H.; Lee, J.H.; Kim, J.S.; Kim, T.J.; Shin, J.; Im, J.H.; Cha, B.; Lee, S.; Kwon, K.S.; Shin, Y.W.; Ko, S.B. Fecal microbiota transplantation can improve cognition in patients with cognitive decline and Clostridioides difficile infection. Aging (Albany NY) 2022, 14, 6449. [Google Scholar] [CrossRef] [PubMed]
- Segal, A.; Zlotnik, Y.; Moyal-Atias, K.; Abuhasira, R.; Ifergane, G. Fecal microbiota transplant as a potential treatment for Parkinson's disease–A case series. Clinical Neurology and Neurosurgery 2021, 207, 106791. [Google Scholar] [CrossRef]
- Zhao, Z.; Ning, J.; Bao, X.Q.; Shang, M.; Ma, J.; Li, G.; Zhang, D. Fecal microbiota transplantation protects rotenone-induced Parkinson’s disease mice via suppressing inflammation mediated by the lipopolysaccharide-TLR4 signaling pathway through the microbiota-gut-brain axis. Microbiome 2021, 9, 1–27. [Google Scholar] [CrossRef]
- Chen, H.; Chen, Z.; Shen, L.; Wu, X.; Ma, X.; Lin, D.; Zhang, M.; Ma, X.; Liu, Y.; Wang, Z.; Zhang, Y. Fecal microbiota transplantation from patients with autoimmune encephalitis modulates Th17 response and relevant behaviors in mice. Cell Death Discov 2020, 6, 75. [Google Scholar] [CrossRef]
- Collyer, R.; Clancy, A.; Borody, T. Faecal microbiota transplantation alleviates symptoms of depression in individuals with irritable bowel syndrome: A case series. Medicine in Microecology 2020, 6, 100029. [Google Scholar] [CrossRef]
- Doll, J.P.; Vázquez-Castellanos, J.F.; Schaub, A.C.; Schweinfurth, N.; Kettelhack, C.; Schneider, E.; Yamanbaeva, G.; Mählmann, L.; Brand, S.; Beglinger, C.; Borgwardt, S. Fecal microbiota transplantation (FMT) as an adjunctive therapy for depression—Case report. Front. Psychiatry 2022, 13, 815422. [Google Scholar] [CrossRef]
- Rao, J.; Qiao, Y.; Xie, R.; Lin, L.; Jiang, J.; Wang, C.; Li, G. Fecal microbiota transplantation ameliorates stress-induced depression-like behaviors associated with the inhibition of glial and NLRP3 inflammasome in rat brain. J. Psychiatr. Res. 2021, 137, 147–157. [Google Scholar] [CrossRef]
- Pu, Y.; Zhang, Q.; Tang, Z.; Lu, C.; Wu, L.; Zhong, Y.; Chen, Y.; Hashimoto, K.; Luo, Y.; Liu, Y. Fecal microbiota transplantation from patients with rheumatoid arthritis causes depression-like behaviors in mice through abnormal T cells activation. Translational Psychiatry 2022, 12, 223. [Google Scholar] [CrossRef]
- Zhu, F.; Guo, R.; Wang, W.; Ju, Y.; Wang, Q.; Ma, Q.; Sun, Q.; Fan, Y.; Xie, Y.; Yang, Z.; Jie, Z. Transplantation of microbiota from drug-free patients with schizophrenia causes schizophrenia-like abnormal behaviors and dysregulated kynurenine metabolism in mice. Mol. Psychiatry 2020, 25, 2905–2918. [Google Scholar] [CrossRef] [PubMed]
- Bajaj, J.S.; Gavis, E.A.; Fagan, A.; Wade, J.B.; Thacker, L.R.; Fuchs, M.; Patel, S.; Davis, B.; Meador, J.; Puri, P.; Sikaroodi, M. A randomized clinical trial of fecal microbiota transplant for alcohol use disorder. Hepatology 2021, 73, 1688–1700. [Google Scholar] [CrossRef] [PubMed]
- D’Amato, A.; Di Cesare Mannelli, L.; Lucarini, E.; Man, A.L.; Le Gall, G.; Branca, J.J.; Ghelardini, C.; Amedei, A.; Bertelli, E.; Regoli, M.; Pacini, A. Faecal microbiota transplant from aged donor mice affects spatial learning and memory via modulating hippocampal synaptic plasticity-and neurotransmission-related proteins in young recipients. Microbiome 2020, 8, 1–19. [Google Scholar] [CrossRef] [PubMed]
- Dietert, R.R. Microbiome First Approaches to Rescue Public Health and Reduce Human Suffering. Biomedicines 2021, 9, 1581. [Google Scholar] [CrossRef] [PubMed]
| Critical Aspects of Human Life [Reference(s)] |
Processes/Functions Under Microbiome Regulation |
|---|---|
| Control of offspring maladies [52,53,54] |
The specific hologenome, particularly at the level of the microimmunosome, can determine offspring fitness and inflammation-driven risk to the offspring |
| Preparation of the next generation in utero [22,29] |
The maternal microbiome affects not only the course of the pregnancy but also the fetal and eventually postnatal development of the offspring |
| Infant maturation [55,56] |
The newborn-infant microbiome determines whether systems like the immune and neurological systems can fully mature (for normal function). |
| Food preferences/choices [57,58] |
Oral and gut microbiome composition can drive food choices and cravings. |
| Emotional balance [59,60] |
Specific gut microbiota including psychobiotic bacteria make neuroactive chemicals that can help to alleviate anxiety and depression. |
| Fear regulation [33,61,62] |
The microbiome regulates fear extinction, which is necessary for healthy, balanced fear responses. |
| Sociability [42,63,64,65] |
Gut microbiota are involved in the regulation of oxytocin- signaling, and microbiome composition can affect social behavior. |
| Health risks [66,67,68] |
Microbiome composition is known to affect the risk of both chronic and infectious diseases. |
| Sexual selection and reproductive success [69,70,71,72] |
Sexual performance issues, infertility, conception problems and problems carrying to term have all been linked with dysbiotic reproductive microbiomes. |
| Aging [73,74,75,76] |
Microbiome status affects disease burden, sleep quality, inflammation and oxidative damage level, telomere length, and circadian clock regulation |
| Postmortum [77,78,79,80] |
Microbes are the ultimate recyclers of physical life on Earth |
| Category of Contribution (Date) | Researcher(s) | Contribution [Reference(s)] |
|---|---|---|
| Probiotics/Fermented Foods (1903 and 1907 papers) |
Elie Metchnikoff | The Nobel Laureate developed the concept of orthobiosis in advocating for the consumption of friendly florae laden fermented milk to aid longevity (1903 and 1907 papers. [see 84] |
| Endosymbiosis (1905 and 1910 papers) |
Konstantin Sergejewitch Mereschkowsky | Published an early model including endosymbiosis of chloroplasts in 1905 including a larger paper in 1910. [see 85,86] |
| A form of Endosymbiosis (written contributions during the 1940s) |
Adolf Meyer-Abich | Developed Holism/Holobiosis concepts [87,88,89]. |
| Endosymbiosis (1967 paper) |
Lynn Margulis as Sagan |
Endosymbiosis (ancient bacteria as the origins of mitochondria) [81] |
| Fractal nature of microbes (1990 paper) |
Martin Obert and colleagues |
Experimental evidence that microbial growth patterns follow fractal geometry [90] |
| Conscious microbes (2001 paper) |
Lynn Margulis | Published her article “The Conscious Cell” in the New York Academy of Sciences [91] |
| Conscious life including microbes (2007 paper) |
Shapiro | Supported the conclusions that life required cognition at all levels. [92] |
| Informational sensing systems among bacteria (2010 paper) |
Reindert Nijland and J. Grant Burgess |
Demonstrated that as part of an exquisite sensing system, bacteria detect and analyze volatile organic compounds (VOC) using a form of olfaction. [93] |
| Pharma-based degradation of the human microbiome (2014 book) |
Martin Blaser | Illustrated the extensive degradation of the human microbiome though overuse of antibiotics and other factors [94] |
| Bacteria as fully functioning cognitive organisms. (2015 paper) |
Pamela Lyon | Lyon presented evidence that bacteria, as cognitive cells, feature intelligence, sensing and perception, behavioral adaptation, memory, learning, anticipation, future prediction, complex decision making, and inter-kingdom communication all in the name of survival and reproduction. [95] |
| A keystone paper linking the quantum properties, states entanglement and operation of fully cognitive bacteria (2016 paper) |
William B. Miller, Jr. | Miller demonstrated that the holobiont and its collection of complex collaborators are cognitively entangled in a Pervasive Informational Field (PIF) operating within a quantum framework. He argues that microbes can hold multiple ambiguity states until they take action to purposely resolve it. They can also exist in a duality of function operating within a larger community (such as a biofilm) while simultaneously demonstrating specialized individual behaviors. Miller argues that the PIF is robust including noise and that bacteria must use discernment for valued decision making. [82] |
| Extending bacteria cognition to a model of the Microbial Mind (2016 paper) |
Daniela Pinto and Thorsten Mascher |
Introduced the concept of bacterial nanobrains [96] |
| Specialized properties of bacteria (2016 paper) |
Sima Baghbanzadeh and Ivan Kassal |
This is an early demonstration of the novel properties of light harvesting by purple bacteria [97] |
| Clear evidence of quantum entanglement among bacteria (2018 paper) |
Chiana Marletto and colleagues |
The researchers used light -based stimulation in one of the early uses of green sulfur bacteria to demonstrate clear quantum entanglement [98] |
| Further development of bacteria as inherently quantum. (2018 paper) |
John S. Torday and William B. Miller Jr. |
The researchers argued that resolution of ambiguity (e.g., informational problem solving in microbes) |
| is the basis of life and is inherently quantum in nature [Torday and Miller, Jr., 2018 99]. | ||
| A reformulation of evolution based of cognition (2020 paper) |
William B. Miller, Frantisek Baluška and John S. Torday |
The researchers described a model of cognition-based evolution [100] |
| A quantum explanation of microbes operating at a distance. (2020 and 2021 papers) |
William B. Miller, Jr. Arthur S. Reber, Frantisek Baluška and John S. Torday |
The researchers introduced the concept that prokaryotic bioelectric fields and senomic fields can interact together to form supracellular N-space fields that can couple cells in coherence at a distance. They also argue for prolonged memory in bacteria. [101,102] |
| Consideration of the holobiont mind and its implications (2021 paper) |
Ismael Palacios-Garcıa and Francisco J Parada |
The researchers discussed the concept of “the holobiont mind,” which pertains to the current paper’s consideration of embodied cognition [103] |
| Important discovery of how bacteria use vibrational coupling as part of their quantum processing (2021 paper) |
Jacob S. Higgins and colleagues |
The researchers showed that green sulfur bacteria (via their protein complexes) can mix electronic and vibrational states (vibronic coupling) via quantum mechanics allowing them to steer excess photosynthetic energy excitation toward a quenching site. [104] |
| Coherence map creation (2022 paper) |
Reshmi Dani and colleagues |
The researchers studied the light harvesting antennae of purple bacteria to construct quantum coherence maps [105]. |
| An important perspective of changing scientific dogma regarding quantum-based bacteria operating across a matrix of consciousness. (2023 paper) |
Stephan A. Schwartz | The researcher argued that science is embracing a new view of reality where all beings of Earth are conscious and are living in a matrix of consciousness in which all beings are both interconnected and independent [106]. |
| This is a clear proof-of concept of the quantum nature of bacteria. (2023 paper) |
Francisco Delgado and Marco Enríquez | Both quantum entanglement and state transference are clearly demonstrated using information-gathering Fenna–Matthews–Olson protein complexes derived green sulfur bacteria. [107]. |
| Evidence of quantum processing in purple bacteria (2023 paper) |
Lorenzo Cupellini and colleagues |
Research on the light harvesting antennae of purple bacteria produced clear evidence of quantum chemical processing [Cupellini et al., 2023 108]. |
| The concentric nanorings of bacteria quantum emitters (2023 paper) |
Verena Scheil and colleagues |
This study on the light-harvesting antennae of purple bacteria enabled a comparison of multiple stacked nanoring geometry vs. single rings in terms of quantum properties. [109] |
| Type of Meditation Protocol [Reference] |
Results |
|---|---|
| Mindfulness | Pre-intervention, fecal B diversity significantly differed between test and control groups. The higher anxiety group had a lower abundance of Streptococcus, Blautia,Romboutsia, Escherichia_Shigella, Eubacterium_hallii_group,Eggerthella, and Allorhizobium_Neorhizobium_Pararhizobium_ Rhizobium; and a higher abundance of Lachnoanaerobaculum, Lachnoclostridium, Rothia, Leptotrichia, Lachnospraceae_UCG_010, Faecalibacterium, Coprococcus_3, Eubacteriumeligens_group, Atopobium, GCA_900066575, and Pseudopropionibacterium vs. the controls. Mindfulness intervention significantly reduced trait anxiety and depression scores and increased resiliency in the test group. Relative abundance of 18 bacteria significantly changed during the intervention with the profile of the test group becoming more similar to that of the healthy controls. Prevalance of Subdoligranulum was negatively correlated with mindfulness responsiveness and tryptophan metabolism. Tryptophan metabolic genes were enriched among high responders to the intervention. |
| Experimental group of 21 young adults with high anxiety trait scores and 29 young adult controls. Protocol of 8 weeks of once a week (2-2.5 hours) group meditation session with daily personal (45 minute) meditation sessions. A 4-week post-intervention follow-up was used. A mindfulness attention awareness scale and a depression scale were used for the evaluation as well as fecal microbiota analysis. Pre and post treatment analyses were performed. [116] | |
| Mindfulness (including yoga) | All 12 patients showed a marked improvement in symptom scores post meditation sessions. Additionally, the urinary tract microbiome diversity increased significantly with major changes in some taxa. |
| A total of twelve patients undergoing treatment for interstitial cystitis (IC), or bladder pain syndrome (BPS) underwent an 8 week mindfulness meditation course. Urinary samples were collected for micobiome analysis both pre and post meditation therapy. [117] | |
|
Mindfulness Beginning with 160 total participants, (two randomized groups of 80 pregnant women each) , maternal mindfulness intervention was applied to prenatal care of 80 pregnant women with symptoms of depression or anxiety while another 80 pregnant women with the same symptoms received the usual prenatal care. For infant merconium microbiome analysis a total of 130 infant samples were able to be collected. Fecal samples from 66 of the intervention newborns and 64 of the controls were analyzed and the results compared. |
No change in alpha diversity was noted but there was a significant group change in beta diversity. Bifidobacterium and Blautia were abundant in the intervention group while Staphylococcus was abundant in the control group. |
| [118] | |
|
Mindfulness The participants were among an elderly population residing in a community facility in China. They had been separated by the criteria of those diagnosed with mild cognitive impairment (MPI) and those aging normally. A mindfulness awareness program was insituted for nine months among 28 MCI subjects and 40 normally functioning participants. Neuropsychological evaluation was performed at each evaluation interval. Blood and stool samples were collected and analyzed at 0, 3, and 9 months. The stool samples were analyzed for cytokine and microbiota profiles. |
Six taxa of bacteria were associated with improved cognitive function among the MCI -MAP group. Ruminococcus emerged as the bacteria positively associated with improvement in multiple cognitive test parameters. |
| [119] | |
|
Deep Tibetan Meditation Fecal microbiota samples were collected, analyzed, and compared among a group of Tibetan Chinese Buddist monks from Qiongke, Jiaqu and Ezhi Temples who praticed long term deep meditation vs. a group of neighboring residents. A total of 37 samples from the monks and 18 from local residents were of a quality to permit microbiota analysis. All participants lived at high elevation. |
Compared to the control group, the meditation group had an increased prevalence of Bacteroidales, Sutterellaceae, Burkholderiales and Betaproteobacteria. After cut-off analysis, two bacterial genera (Megamonas and Faecalibacterium) were enriched in the meditation group. Based on the literature, the first of two bacteria genera are associated with a higher quality of life and the second genera is often reduced among anxiety disorder patients. |
| [120] | |
| Microbes in humans [Reference(s] |
Phyla/Genus location in environment | Feature(s) |
|---|---|---|
| Archaea Methanomassiliicoccus luminyensis gut) [123,124,125] |
Geothermal hot spring (Indian ocean island), Mud volcano (Barents sea), Peat land soil (France), Deep sea hypersaline anoxic (Kyros) basin | Methanogenesis is the hallmark of these archaea. |
| Archaea Halobacteriota (skin) [126,127,128] |
Alpine Permian-era bore core of a salt deposit, hypersaline-deep lake Antarctica, Solar salterns, Survives space launches, space conditions above the ozone layer as well as Mars-like conditions |
Polyextremophilic with tolerance of saturating salinity, anaerobic conditions, high levels of ultraviolet and ionizing radiation, subzero temperatures, desiccation, and toxic ions. |
| Analysis of skin microbiota samples showed that computer key archaeal deposits from humans were primarily Nitrososphaeria Nitrososphaeria (54.3% of archaeal reads) and Nanoarchaeota. [126,129,130,131] |
Nitrososphaeria are a prominent archaea in acid mine drainage sediments. While Nanoarchaeota are obligate ectobionts that are mainly found in deep-sea hydrothermal vents and geothermal springs (e.g., Yellowstone National Park) across the globe. | Both types of archaea seem to metabolize best under harsh conditions and are relatively resistant to metal toxicity. |
| Magnetotatic bacteria can be detected in several human tissues. Seven species were recently identified from the human gut (Magnetococcus marinus , Magnetospira sp. QH-2, Magnetospirillum magneticum , Magnetospirillum sp. ME-1, Magnetospirillum sp. XM-1, Magnetospirillum gryphiswaldense , and Desulfovibrio magneticus ). [132,133,134,135] |
They have wide global distribution including in extreme niches and are important in the global distribution of iron. Magnetotatic bacteria are potential symbiotes for deep-sea marine bivalves, detected in bats, whales, birds, and humans. |
Important in both biomineralization, magnetite crystal formation, and navigation. These bacteria also have a high level of horizontal gene transfer for magnetite production capabilities. |
| Acidophillic and aciduric lactic acid bacteria are mild-moderate extremophiles in that they are acid resistant. They are also extremely important in fermented foods as well as in the human mouth, gut and female genital tract microbiomes and in initial colonization of the newborn’s colon. [136,137,138,139,140] |
Beyond humans these bacteria are widespread in fermented foods, sileage, and plant and animal species. The first isolate of what eventually became known as Lactococcus lactis was first used by Joseph Lister [140] |
Lactic acid bacteria producing acidic niches (lactic acid) as a result of carbohydrate fermentation and also produce bacteriocins. These functions play a protective role in humans particularly in the vaginal microbiome. |
| Microbiome rewilding studies indicate that visiting green spaces can lead to increased acquisition of environmental microbes (e.g., skin and respiratory microbiota). Persistent gardening results in shared, prolonged skin acquisition of soil microbiota. [141,142]. |
Soil microbes (Sphingomonas, Blastococcus (skin and nose), Solirubrobacter (skin), and Massilia (nasal) were consistently detected after green space visits. For gardeners, the most frequently transferred taxa were: Sphingomonadaceae, Nocardioidaceae, Xanthobacteraceae, Burkholderiaceae, and Pseudomonadaceae. |
We are constantly exchanging microbes with our surroundings. We can choose where and how we spend our time with this in mind. |
| Condition or Disorder [Reference(s)] |
Nature of FMT or Microbiota Transfer Therapy |
Effect |
|---|---|---|
| Autism Spectrum Disorder (ASD) [153] |
Human-Human Microbiota Transfer Therapy |
Microbiota Transfer Therapy resulted in improvement of both behavioral and gastrointestinal symptoms among the autistic children for at least eight weeks after treatment (the duration of this study). |
| Autism Spectrum Disorder [154] |
Human-Human Microbiota Transfer Therapy |
A two-year follow-up for participants in the Kang et. al., 2017 study showed that composition changes in gut microbiota persisted and the behavioral improvements continued to increase even years after the initial study. |
| Autism Spectrum Disorder [155] |
Human-Human | A systematic review of FMT as a treatment for pediatric ASD concluded that it is a promising intervention for reversing both behavioral as well as gastrointestinal symptoms. |
| Autism Spectrum Disorder [156] |
Human-Human | FMT treatment of autistic children with standardized human gut microbiota resulted in improvement of both behavioral and gastrointestinal symptoms. |
| Autism Spectrum Disorder [157] |
Human-Mouse | FMT transfer of microbiota from autistic children to mice produced autistic related behavioral changes in the mice (e.g., sociability, social cage test, novel object test, novel cage test) along with increased pro-inflammatory factors in the gut and brain. |
| Alzheimer's Disease Systematic Review [158] |
Human-Human, Human-Mouse in review |
Overall FMT transferring healthy microbiota improved the symptoms of Alzheimer's Disease |
| Alzheimer's Disease [Park et al., 2021 159] |
Human-Human | FMT treatment for Clostridioides difficile infection in an Alzheimer's Disease (AD) patient noticeably improved the symptoms of AD. |
| Dementia [160] |
Human-Human | Five cases are described of dementia patients treated for Clostridioides difficile infection with FMT. They experienced improved cognition following the treatment. |
| Parkinson’s Disease [161] |
Human-Human | In a case series of Parkinson’s Disease (PD) patients using FMT, there was improvement of both PD motor and non-motor symptoms. |
| Parkinson’s Disease [162] |
Mouse-Mouse | Using a rotenone-induced model of PD in mice, FMT with normal gut microbiota suppressed PD symptoms via suppression of inflammation-mediated cell signaling. |
| Autoimmune Encephalomyelitis [163] |
Human-Mouse | Behavioral characteristics associated with the human condition were transferred to the mice with the microbiota transfer. |
| Depression [164] |
Human-Human | A case study series is reported where irritable bowel plus depression patients received transplantation of healthy donor fecal microbiota, symptoms of depression improved in all three cases examined. |
| Depression [165] |
Human-Human | Two case studies showed beneficial outcome after a four-week interval with significant continuing benefits in one patient after eight weeks. |
| Depression [166] |
Human-Rat | FMT transfer of normal human microbiota reduced depressive symptoms in unpredictably mildly-stressed rats and also suppressed activation of glial cells and NLRP3 inflammasomes in the rat brain. |
| Depression [167] |
Human-Mouse | FMT from human rheumatoid arthritis patients into antibiotic treated mice produced immune-inflammatory-based depression behavior in the mice. |
| Schizophrenia [168] |
Human-Mouse | FMT transfer from drug-free schizophrenia patients produced metabolic alterations and schizophrenia-like behaviors (e.g., impaired spatial learning and memory) in the recipient mice. |
| Alcohol Use Disorder [169] |
Human-Human | Phase 1 clinical trial found that in the short-term there were favorable gut microbiome changes as well as reduced cravings and misuse of alcohol among transplant recipients vs. placebo controls. |
| Restricted learning and memory linked to aging [170] |
Mouse-Mouse | Transfer of aged donor mouse fecal microbiota into young mice reduced synaptic plasticity in the hippocampus and neurochemical production resulting in loss of spatial learning and memory capacity. |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).




