1. Introduction
Climate change in the 21
st century is a recognised anthropogenic phenomenon and has resulted in unprecedented levels of atmospheric carbon dioxide (CO
2) – not surpassed for the past 400,000 years [
1]. Rising global temperatures poses far-reaching threats to public health through associated extreme weather, famine, air pollution, rising sea levels and change in spread of vector, water, and food-borne diseases [
2]. As such, all industries must take responsibility, and the healthcare sector is no exception.
A carbon footprint refers to the total direct/indirect greenhouse gas (GHG) emissions caused by an individual, organisation or product conveyed as ‘carbon dioxide equivalent’ (CO
2e) [
3]. This metric accounts for the seven main GHGs: CO
2, Methane (CH
4), Nitrous oxide (N
2O), Hydrofluorocarbons (HFC), Nitrogen trifluoride (NF
3), Sulphur hexafluoride (SF
6) and Perfluorocarbons (PFC) [
4]. In 2019, The National Health Service (NHS) of the UK produced 25 million tonnes of CO
2e, representing just over 7% of the UK’s net CO2e [
5,
6]. This has led to the NHS to be the first healthcare system globally to pledge a ‘net zero’ healthcare system by 2045 [
7]. Over half of NHS emissions are attributable to supply chain (62%), with the remaining shared between delivery of care (24%), travel to and from NHS sites (10%), and commissioned private health and care services (4%) [
5]. Operating theatres (OTs) have been found to be three to six times more energy-intense than the hospital, primarily due to continuous air conditioning, heating, and ventilation requirements [
8]. The overall footprint of surgery extends beyond this to include consumables, equipment, energy and water use, patient and staff travel and treatment of waste [
9].
Life cycle assessment (LCA) denotes an approach to evaluating the environmental burden associated with all stages of the life cycle of process, products, or services [
10]. There are two broad methods of conducting an LCA. Economic input-output LCAs operate under the premise that expensive items generate higher GHG emissions. An emission factor is applied to the monetary cost of a process/product. This method is useful for analysing entire supply-chains and identifying hotspots for more detailed foot-printing analysis but shouldn’t be used for comparing products within the same sector (e.g., Neurosurgery within the healthcare sector) [
11]. Conversely, process based LCAs assess the environmental impact of a unit from initial material extraction (‘cradle’) to final disposal (‘grave’) as defined by the ISO 14040 set of standards [
12]. It accounts for all material input, emissions, and waste outputs necessary to produce the end unit. A handful of prior studies have conducted such analyses with the intent to offer sustainable solutions. For instance, Tan and Lim (2020) found that an estimated 8641 tonnes of CO2e are produced by dermatologic surgery annually in Queensland, Australia. They identify several targets for sustainable change including switching to reusable surgical instruments and PPE, and recycling consumables where possible [
13]. A systematic review by Rizan et al. (2020) echoes these findings and establishes that electricity use, and the procurement of consumables were the main carbon hotspots. They advise using reusable or reprocessed surgical devices and improving the energy-efficiency of theatres [
14].
The literature highlights inefficiencies of Neurosurgical procedures including disposal of opened unused surgical items [
15], prolonged hospital stays beyond medical readiness [
16], and improper staffing resulting in perioperative delay [
17]. Despite this, there is a paucity of research investigating the carbon footprint of Neurosurgical operations. As such, this paper aims to outline the footprint of a lumbar microdiscectomy – a common elective Neurosurgical operation to treat spinal nerve root compression secondary to vertebral disc prolapse. In doing so, we hope to propose a framework for sustainable change for units nationally and internationally.
2. Methods
Data Collection and Analysis:
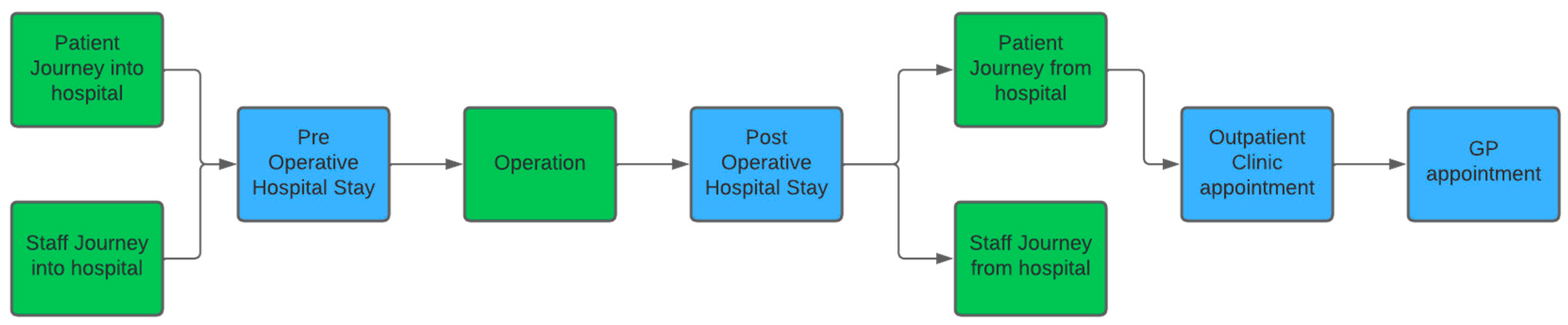
The first step in the process was to map out the patient journey to understand the phases required for study (
Figure 1). Step two involved a review of the literature to ascertain areas that had already been mapped in prior studies. Appropriate secondary sources were used to fill gaps in the footprinting analysis. For instance, a recent article by Tennison et al. (2021) provided a valuable source of foot printing data for elements of analysis including the acute inpatient stay, outpatient clinic appointment, and outpatient GP appointment [
5]. The third step involved collecting and collating the relevant sources of primary and secondary data to reach the final CO
2e figure for each stage of the footprinting analysis.
Inventory Analysis of Operation:
An inventory analysis of a lumbar microdiscectomy operation was performed on 11
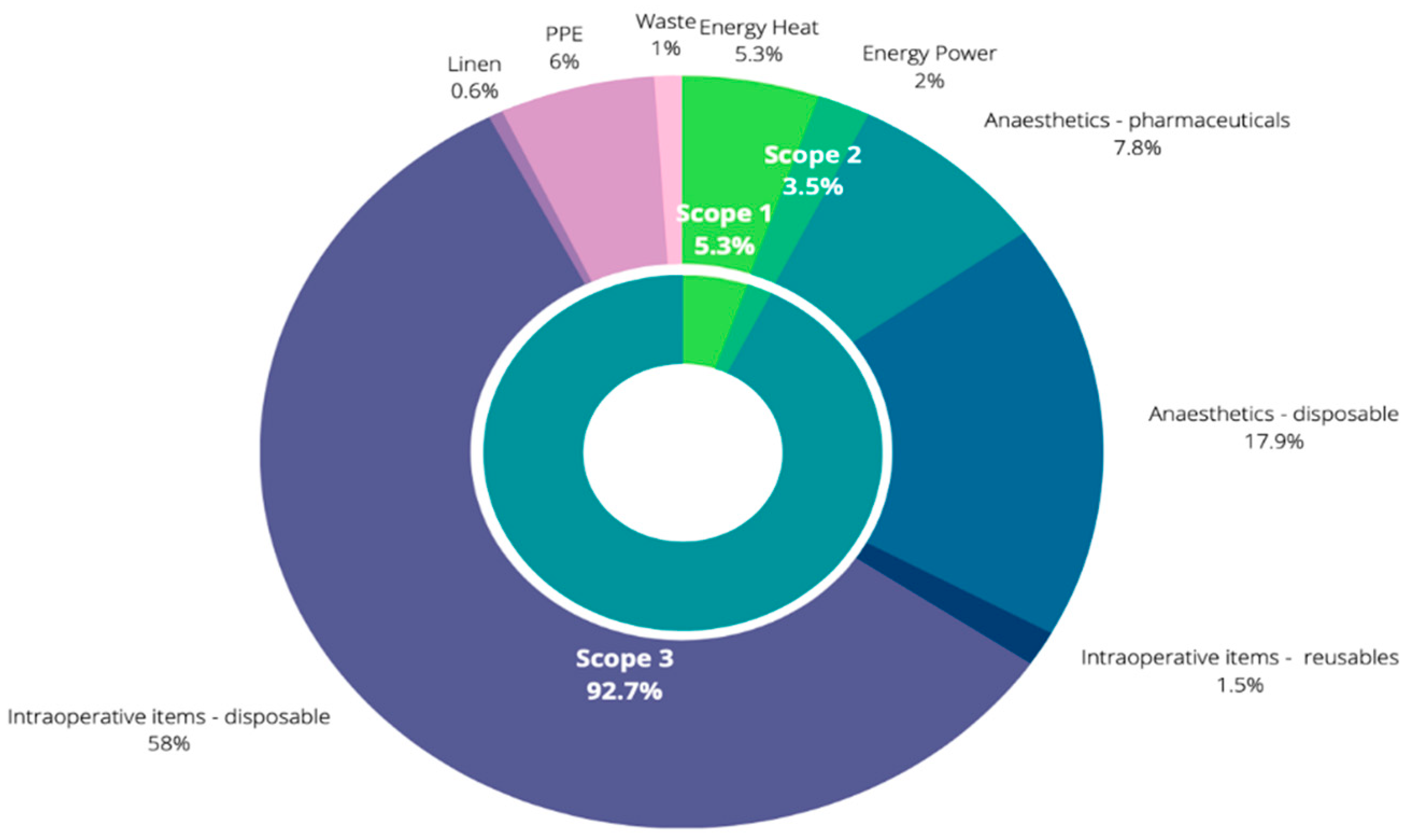
th April 2022 at Salford Royal Hospital, which is a part of the Northern Care Alliance (NCA) NHS Foundation Trust. All relevant permissions and consent were sought. Two lists were attended by two researchers to verify overall similarities in practices for lumbar microdiscectomies at our trust. All emission-generating elements of the operation were documented and grouped as per the Greenhouse Gas Protocol Scoping categories [
19]. Scope 1 covers direct emissions from owned sourced (i.e., heating the operating theatre). Scope 2 encompasses indirect emissions from purchased electricity, steam, and cooling (i.e., powering electrical equipment and lighting in the OT). Finally, Scope 3 incorporates all indirect upstream and downstream emissions derived from all the other variables (e.g., all emissions from the production and disposal of single-use equipment) (
Figure 2).
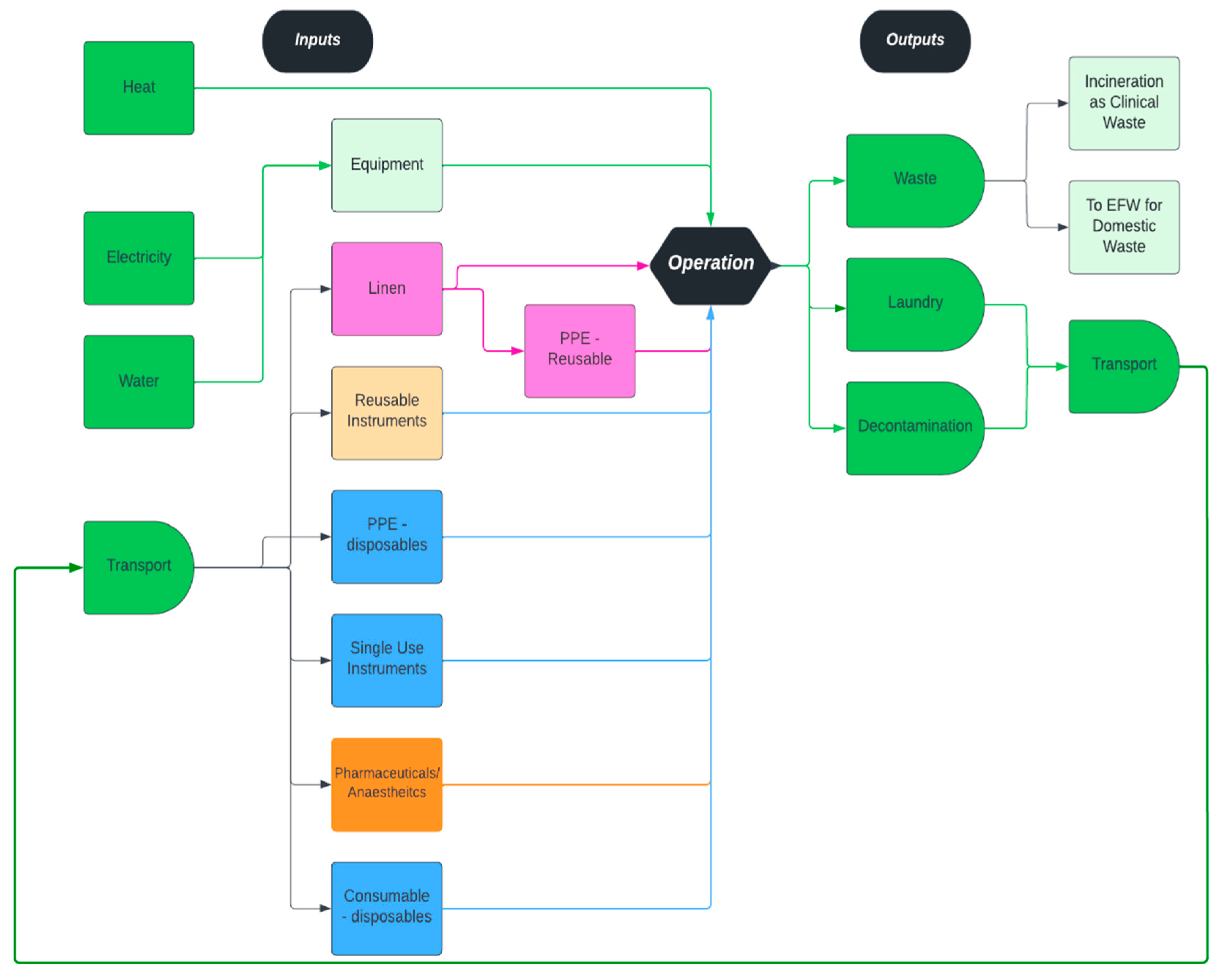
Inventory categories were defined within which all variables were catalogued (
Figure 2). For consumables including personal protective equipment (PPE), medications and disposable equipment, we recorded the number of items/volume/weights used (as appropriate), number of items per pack, manufacturer, and packaging material. Documentation of reusable equipment involved noting the number of items used and manufacture company. Given that all instruments within sterile packs would be resterilised, all items in these packs were documented regardless of whether the items were used. For lighting and electricals, we documented the number of items used, duration of use, manufacture company and serial number. The kilowatt-hour (kWh) rating facilitated reconciliation of the derived emission. Non-hazardous and hazardous waste (including sharps waste) was weighed separately. Hazardous waste is sent for incineration whilst non-hazardous waste is sent to an ‘energy for waste’ (EFW) facility. All laundered items were recorded. Following data collection, an average of the two operations were taken. A full input-output summary of the operation can be visualised in
Figure 3. These items were then reconciled using the trust’s ‘CO
2 analysis database’ and additional primary and secondary sources of footprinting data (
Figure 4).
CO2 Analysis Database:
In 2021, the trust undertook a carbon footprinting exercise, using a company called ‘CO2Analysis.’ The output of this work was a detailed breakdown of scope 3 carbon emissions against all items the trust had procured in the study year. The trust provided CO2 analysis with a complete record of purchase orders for the year 2020/21. CO2 analysis then analysed this using their ‘SpendInsight Knowledge’ base - a bespoke artificial intelligence (AI) powered carbon accounting system for products and services, which is owned by NHS England and facilitates accurate analysis of expenditure. The final step implemented by CO2 analysis involved mapping this to the Centre for Sustainability Accounting (CenSA) scope 3 GHG emission factors.
The final step of the reconciliation process involved determining the number of each item present in a box/shipment and dividing accordingly depending on how many of those items were used in the operation. For reusable instruments, information was gathered from our decontamination team on the lifetime of instruments, how many times they are likely to be reused and how long the process takes from being used in theatre, transport to decontamination, sterilisation and back out to the theatre to be reused. This gave a final CO2e figure for each item.
Additional Data Sources:
Where purchase order data was absent/inaccurately logged, secondary sources were used to footprint comparable items. Scope 1 and 2 footprinting involved primary data collection of local energy data. By accessing the trusts contracts and using the appropriate GHG conversion factors, we were able to calculate scope 1 and 2 emissions. All additional sources of inventory reconciliation including scope 1 and 2 data can be visualised in
Figure 4 [
20,
21,
22,
23].
Table 1.
Additional sourced of footprinting data.
Table 1.
Additional sourced of footprinting data.
| Data source |
Scope |
Type |
Operative data used |
Reference |
| Parvatker et al 201920 |
3 |
Secondary |
Carbon impact of the pharmaceuticals (except paracetamol) |
[20] |
| Myo et al 202121 |
3 |
Secondary |
Carbon impact of paracetamol |
[21] |
| Burguburu et al. 202222 |
3 |
Secondary |
Lifecycle Carbon impact of Scrubs |
[22] |
| Rizan & Lillywhite 202223 |
3 |
Secondary |
Carbon impact of sterilisation |
[23] |
| Greenhouse gas reporting: conversion factors 2021 |
|
Primary |
Gas, heat and power, and electricity carbon factors, Waste Carbon Factors |
[17] |
| Supplier Manufacturer Data |
|
Primary |
Case and Box quantities, to turn the CO2Analysis.com data into quantities used within the procedure |
N/A |
| Hospital sterilisation and decontamination unit (HSDU) |
|
Primary |
Tray turnaround times: Time taken from instrument use to cleaning at HSDU and back to theatre to be reusedEnergy consumption: Energy used to decontaminate and sterilise instruments per yearTrays per year: Total energy consumed divided by energy per tray |
N/A |
| Laundry |
|
Primary |
Carbon impact of linen (other than scrubs) |
N/A |
| Energy |
|
Primary |
Carbon impact of the theatre and the equipment used within it. The site has a mix of energy sources, using grid electricity, gas, and a large on-site CHP plant |
N/A |
3. Results
Summary of Results:
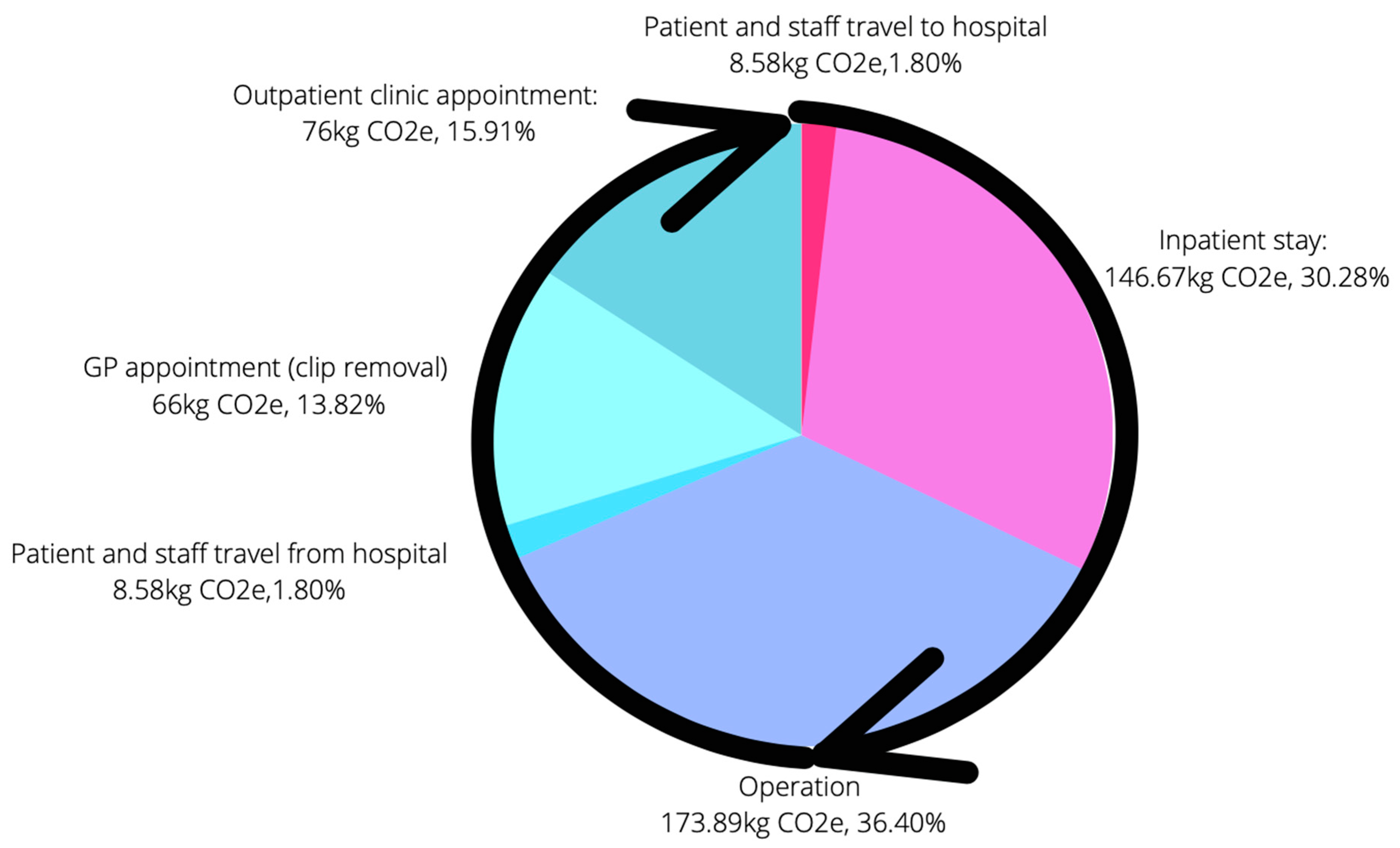
The total CO
2e of the analysed functional unit was calculated at 477.73kg CO
2e (Figure 5). The operation (173.89kg CO
2e, 36.40%) and the inpatient stay (144.67kg CO
2e, 30.28%) were the biggest contributors. Review of six years of local data revealed an average of 287 cases annually. The literature estimates 10,000 elective decompressions nationally per year [
24]. Thus, the estimated carbon impact of lumbar microdiscectomies is 137.11 tonnes CO
2e at the trust, and 4,777 tonnes CO
2e nationally.
Patient and Staff Travel:
Patient and staff travel denoted the first stage of the footprinting analysis. Recent data from the Department of Transport (DoT), found that travel by car accounts for 75% of all car journeys in the North-West of England [
25]. As of 2020, 58.41% of all registered cars in the UK were petrol-run [
26]. The average car trip distance in the North-West of England is 7.5miles (12km) [
25]. As such, the CO
2e for the patient journey was based on a 7.5-mile trip in a petrol vehicle. In 2021, the CO
2e for the average petrol car in the UK is 174g/km [
27]. Thus, the calculated CO
2e for a single patient journey was 2.08kg CO
2e. This is multiplied by a factor of four when working on the assumption that the average patient will be dropped-off and picked-up by a family member, equating to four trips and 8.32kg CO
2e.
It was estimated that on an average day in the Neurosurgical department, 26 members of staff service 20 patients, equating to roughly 1.3 members of staff per patient. A recent trust-wide travel survey of 628 members revealed that 73% of NCA staff travel to work alone by car. The average staff journey was 12.16 miles (19.56 km). Operating with the same assumptions as above, the CO2e for a staff journey is 3.40kg CO2e per trip and 6.81kg CO2e for the return trip. This equates to 8.85kg CO2e for staff travel and 17.17kg CO2e for patient and staff travel as per the functional unit of the analysis.
Inpatient Stay (Pre- and Post-Operative):
Review of lumbar microdiscectomy cases conducted at Salford Royal Hospital over a 6-year period revealed a mean length of stay of 1.29 days. This equates to approximately 1 day and 7 hours. This finding is echoed in a study by Khechen et al., (2019) which found that 9.7% of patients stay in hospital longer than one day post-operatively following a lumbar microdiscectomy [
28]. As such, 1 day and 7 hours was modelled for the inpatient LOS. Multiple prior studies have modelled the emission factor per hospital bed-day. Notably, Tennison et al. (2021) found that the average acute inpatient hospital-stay in the UK generates 125kg CO2e per bed-day [
5]. This figure drops to 112kg CO2e per bed day when you deduct the environmental impact of patient, staff, and visitor travel [
5] – a stage of the LCA already accounted for in the analysis. This data was used to calculate the ecological impact of the patient stay itself. Taking the average hospital stay at Salford Royal for a lumbar microdiscectomy at 1 day and 7 hours, the modelled CO
2e for the inpatient stay equates to 144.67kg CO
2e.
The Operation:
Reconciliation of the inventory analysis against the ‘CO2 analysis’ database and several additional sources revealed a total CO2e of 173.89kg. Scope 3 emissions contributed to the majority of this with single-use intraoperative equipment accounting for over half of the total emissions (100.80/173.89kg, 57.97%). This rises to more than three-quarters of the total emissions when disposable anaesthetic equipment is considered (131.92/173.89kg CO2e, 75.86%).
GP Appointment (Clip Removal):
Method of skin closure for a lumbar microdiscectomy varies between sutures and clips and is generally dictated by surgeon preference. A visit to the general practitioner (GP) is required for removal in the case of clipping. Tennison et al., (2021) determines that the average GP visit to generate 66kg CO
2e per visit, a figure used in the analysis [
5].
Outpatient Follow-Up Appointment:
All patients are followed-up in the outpatient clinic at Salford Royal Hospital six weeks following a lumbar microdiscectomy. Tennison et al., (2021) modelled the environmental impact of the average outpatient appointment in acute care to be 76kg CO
2e, a figure used in the analysis [
5].
4. Discussion
The present study puts the ecological impact of a lumbar microdiscectomy at 477.73kg CO
2e, with single-use intraoperative items accounting for a significant source of this burden. Given that there are over 10,000 adult patients each year undergoing elective spinal surgery in the UK [
24], this represents a significant healthcare-associated ecological burden. The figure determined by the functional unit of analysis is ecologically comparable to a single flight from Manchester to Istanbul or a return flight from Manchester to Berlin [
29], and would take 19 trees one year to offset the emissions [
30].
Ecological analysis is a novel area of enquiry in the surgical field. As such, the availability of comparable literature is limited. Rizan et al.’s (2020) review of eight studies found a range between 6-814kg CO
2e per functional unit of analysis with a cataract surgery in India at the bottom end, and a robotic hysterectomy in the US at the top end of this range [
14]. The present figure finds itself close to the median (410kg) of this range. However, six of the eight studies only consider the operation itself contrasting the present study, which maps the entire patient journey from attendance to hospital to the final outpatient visit. Considering the operation alone puts the present figure (173.89kg CO
2e) at the lower end of this range and lower than any of the operations studied in a Western healthcare setting. Aside from differences in operative procedure and footprinting methodology, there are elements in the present study that can account for this finding. Notably, total intravenous anaesthesia (TIVA) with Propofol was the anaesthetic agent of choice contrasting anaesthetic gas chosen by most of the studies analysed by Rizan et al. (2020), which contributed substantially to the overall carbon figure [
14]. The differential carbon impact of TIVA versus gas is well-established and has been found to be almost four orders of magnitude lower than its gaseous counterparts [
31]. The greater carbon impact of gaseous anaesthesia is attributable to the waste emissions from N
2O – a carrier gas with a global warming potential (GWP) 310 times that of CO
2 [
31]. TIVA has also been shown to confer additional clinical benefits over xenon-based alternatives including lower rates of post-operative nausea [
32] and a reduced risk of malignant hyperthermia [
33]. Notably, it has been found to reduce recovery times in lumbar decompression [
34]. Inhaled agents were previously thought to confer cardioprotective benefits over intravenous counterparts, based on experimental models [
35]. However, more robust studies have since dispelled this idea, with a recent RCT concluding no difference between the two class of agents [
36]. Neverthless, longer set-up times, greater risk of equipment failure and higher costs have all been cited as barriers to TIVA use [
37]. Despite this, there has been a steady increase in its adoption in the UK, particularly in the field of Neurosurgery [
38].
The local travel survey revealed that almost three quarters (73%) of 628 staff members travelled into work alone by car. By encouraging car-pooling initiatives and investing in local public transport infrastructure, the emissions derived from this stage can be minimised not only for elective surgery, but all healthcare-related activities.
Intraoperative single-use items accounted for over half of the carbon impact of the operation rising to over three-quarters (131.92kg CO
2e, 75.9%) when anaesthetic disposables are considered. Conversely, the carbon cost of sterilising reusable equipment accounted for a minute fraction of the overall emissions at 1.5% (2.60kg CO
2e), 50 times less than the overall impact derived from single-use items (
Figure 3). This finding is echoed by multiple prior studies[
39,
40] of similar healthcare systems and appears to be a significant inherent source of emission in surgery. Furthermore, we noted that most disposables were contained in several layers of packaging, most of which contained plastic. Sterilised instruments were also double wrapped in plastic. A potential strategy would be to urge manufacturers to seek alternative means of packaging without compromising sterility by using single-layer plastic wrapping for sterile instruments – a strategy that has been shown to be just as effective in preventing bacterial contamination [
41].
Clips were chosen as the method of choice for skin closure. This necessitates an additional outpatient primary care visit – an activity which contributed an additional 66kg CO
2e (13.82%). Given that skin closure is largely down to surgeon preference, this additional carbon (and financial) cost can be eliminated entirely by substituting with absorbable sutures. The limited evidence suggests that clips may increase the risk of post-operative wound infection [
42]. However, more robust randomised controls are required to verify this link.
5. Limitations
We must acknowledge the variability of surgical and anaesthetic practices for a lumbar microdiscectomy between trusts and regions. For instance, units will differ in the use of TIVA vs. xenon-based gases, manage waste differently and vary in energy sources used to power hospital facilities and operating theatres. Thus, the external validity of this single-centre trial is limited. Additionally, the purchase order data reconciled from the CO
2 analysis database is reliant on accurate logging of purchase orders. On several instances, we were unable to reconcile certain inventoried items and therefore had to use data for equivalent items to reach a final figure. Another limitation relates to the use of secondary sources to footprint certain aspects of the overall analysis. Tennison et al. (2021) [
5] provided a valuable data source and although they used national data, local factors in our hospital may differ considerably, resulting in discrepant emission data for important aspects of the analysis including the acute inpatient stay and outpatient clinic appointments.
6. Conclusions
Surgery is a significant source of healthcare derived emissions, and Neurosurgery is no exception, producing 477.73kg CO2e at our trust per patient. This analysis has allowed us to both appreciate the magnitude of emissions as well as identify sources for sustainable change. By substituting polluting elements for carbon-friendly alternatives (e.g., TIVA instead of gaseous anaesthesia, suture closure vs. staples) and challenging the single-use culture, we can all play a part in curbing the effect of global warming and pave the way to a ‘net zero’ healthcare system. Similar analyses of common surgical procedures will enable healthcare authorities to understand problem areas that require attention across numerous surgical disciplines. Ultimately, comprehension of the problem is prerequisite to attaining this ambitious ‘net zero’ target and catering to the increasingly astute and environmental conscious patient demographic.
Author Contributions
SS: Conceptualization, methodology, validation, formal analysis, investigation, data curation, writing – original draft, project administration. KJG: Conceptualization, methodology, writing – review & editing, supervision. HB: Methodology, validation, formal analysis, data curation, writing – original draft.
Funding
This research did not receive any specific grant from funding agencies in the public, commercial, or not-for-profit sectors.
Institutional Review Board Statement
Given the nature of this study, obtaining ethics approval was not required.
Informed Consent Statement
Not applicable.
Data Availability Statement
The source data for this study will be made available as a supplementary material.
Conflicts of Interest
None.
Abbreviations
AI: Artificial Intelligence; CH4: Methane; CO2: Carbon dioxide; EFW: Energy for waste; GHG: Greenhouse gas; GP: General practitioner; GWP: Global warming potential; HFC: Hydrofluorocarbons; KgCO2e: Kilograms of carbon dioxide equivalent; kWH: Killowat-hour; LCA: Life-cycle assessment; LOS: Length of stay; NCA: Northern Care Alliance; NHS: National Health Service; N2O: Nitrous oxide; OT: Operating theatre; PFC: Perflourocarbons; PPE: Personal protective equipment; TIVA: Total intravenous anaesthesia.
References
- Wheeler N, Watts N. Climate Change: From Science to Practice. Curr Environ Health Rep. 2018;5(1):170-178. [CrossRef]
- Rossati A. Global Warming and Its Health Impact. Int J Occup Environ Med. 2017;8(1):7-20. [CrossRef]
- Pandey D, Agrawal M, Pandey JS. Carbon footprint: current methods of estimation. Environ Monit Assess. 2011;178(1-4):135-160. [CrossRef]
- Montzka SA, Dlugokencky EJ, Butler JH. Non-CO2 greenhouse gases and climate change. Nature. 2011;476(7358):43-50. [CrossRef]
- Tennison I, Roschnik S, Ashby B, et al. Health care's response to climate change: a carbon footprint assessment of the NHS in England. Lancet Planet Health. 2021;5(2):e84-e92. [CrossRef]
- Department for Business, Energy & Industrial Strategy (2020). 2019 UK greenhouse gas emissions. Available at: https://assets.publishing.service.gov.uk/government/uploads/system/uploads/attachment_data/file/875485/2019_UK_greenhouse_gas_emissions_provisional_figures_statistical_release.pdf. Accessed on 2 September 2022.
- NHS, NHS England 2020, Delivering a ‘Net Zero’ National Health Service. https://www.england.nhs.uk/greenernhs/wp-content/uploads/sites/51/2020/10/delivering-a-net-zero-national-health-service.pdf.Accessed on 2 September 2022.
- MacNeill AJ, Lillywhite R, Brown CJ. The impact of surgery on global climate: a carbon footprinting study of operating theatres in three health systems. Lancet Planet Health. 2017;1(9):e381-e388. [CrossRef]
- Whiting A., Tennison I., Roschnik S. Collins M, Surgery and the NHS carbon footprint. The Bulletin of the Royal College of Surgeons of England. 2020; 102(5): 182-185. [CrossRef]
- Klöpffer W. Life cycle assessment as part of sustainability assessment for chemicals. Environ Sci Pollut Res Int. 2005;12(3):173-177. [CrossRef]
- Berners-Lee M, Howard DC, Moss J, Kaivanto K, Scott WA. Greenhouse gas footprinting for small businesses--the use of input-output data. Sci Total Environ. 2011;409(5):883-891. [CrossRef]
- ISO, 14040: 2006 Environmental Management: Life Cycle Assessment: Principles and Framework International Organization for Standardization. https://www.iso.org/standard/37456.html. Accessed 2 September 2022.
- Tan E, Lim D. Carbon footprint of dermatologic surgery. Australas J Dermatol. 2021;62(2):e170-e177. [CrossRef]
- Rizan C, Steinbach I, Nicholson R, Lillywhite R, Reed M, Bhutta MF. The Carbon Footprint of Surgical Operations: A Systematic Review. Ann Surg. 2020;272(6):986-995. [CrossRef]
- Zygourakis CC, Yoon S, Valencia V, et al. Operating room waste: disposable supply utilization in neurosurgical procedures. J Neurosurg. 2017;126(2):620-625. [CrossRef]
- Linzey JR, Foshee R, Moriguchi F, et al. Length of Stay Beyond Medical Readiness in a Neurosurgical Patient Population and Associated Healthcare Costs. Neurosurgery. 2021;88(3):E259-E264. [CrossRef]
- Kamat AS, Parker A. Effect of perioperative inefficiency on neurosurgical theatre efficacy: A 15-year analysis. Br J Neurosurg. 2015;29(4):565-568. [CrossRef]
- Department of Business, Energy & Industrial Strategy, The United Kingdom Government. Greenhouse gas reporting - Conversion factors 2021. https://www.gov.uk/government/publications/greenhouse-gas-reporting-conversion-factors-2021. Accessed 2 September 2022.
- The Greenhouse Gas Protocol. Product Life Cycle Accounting and Reporting Standard, 2011. https://ghgprotocol.org/sites/default/files/standards/Product-Life-Cycle-Accounting-Reporting-Standard_041613.pdf. Accessed 2 September 2022.
- Parvatker AG, Tunceroglu H, Sherman JD et al. Cradle-to-Gate Greenhouse Gas Emissions for Twenty Anesthetic Active Pharmaceutical Ingredients Based on Process Scale-Up and Process Design Calculations, ACS Sustainable Chemistry & Engineering 2019;7(7):6580-6591. [CrossRef]
- Myo J, Pooley S, Brennan F. Oral, in place of intravenous, paracetamol as the new normal for elective cases. Anaesthesia. 2021;76(8):1143-1144. [CrossRef]
- Burguburu A, Tanné C, Bosc K et al. Comparative life cycle assessment of reusable and disposable scrub suits used in hospital operating rooms, Cleaner Environmental Systems. Elsevier BV. 2022;4:100068. [CrossRef]
- Rizan C, Lillywhite R, Reed M, Bhutta MF. Minimising carbon and financial costs of steam sterilisation and packaging of reusable surgical instruments. Br J Surg. 2022;109(2):200-210. [CrossRef]
- Weir S, Samnaliev M, Kuo TC, et al. The incidence and healthcare costs of persistent postoperative pain following lumbar spine surgery in the UK: a cohort study using the Clinical Practice Research Datalink (CPRD) and Hospital Episode Statistics (HES). BMJ Open. 2017;7(9):e017585. Published 2017 Sep 11. [CrossRef]
- Department of Transport. Transport Statistics Great Britain, 2021. https://www.gov.uk/government/statistics/transport-statistics-great-britain-2021/transport-statistics-great-britain-2021. Accessed 2 September 2022.
- Department for Transport. Licensed cars by propulsion or fuel type: Great Britain and United Kingdom, 2020. https://www.gov.uk/government/statistical-data-sets/veh02-licensed-cars#licensed-vehicles. Accessed 2 September 2022.
- Department for Transport. National Travel Survey, 2022. https://www.gov.uk/government/statistics/national-travel-survey-2020/national-travel-survey-2020 Accessed 2 September 2022.
- Khechen B, Haws BE, Patel DV et al. Risk Factors for a Long Hospital Stay Following Minimally Invasive Lumbar Discectomy. Clin Spine Surg. 2019;32(1):56-59. [CrossRef]
- Flight carbon calculator: https://co2.myclimate.org/en/portfolios?calculation_id=4962556. Accessed 2 September 2022.
- How much CO2 does a tree absorb? : https://ecotree.green/en/how-much-co2-does-a-tree-absorb. Accessed 2 September 2022.
- Sherman J, Le C, Lamers V, Eckelman M. Life cycle greenhouse gas emissions of anesthetic drugs. Anesth Analg. 2012;114(5):1086-1090. [CrossRef]
- Coburn M, Kunitz O, Apfel CC, Hein M, Fries M, Rossaint R. Incidence of postoperative nausea and emetic episodes after xenon anaesthesia compared with propofol-based anaesthesia. Br J Anaesth. 2008;100(6):787-791. [CrossRef]
- Rosenberg H, Pollock N, Schiemann A, Bulger T, Stowell K. Malignant hyperthermia: a review. Orphanet J Rare Dis. 2015;10:93. Published 2015 Aug 4. [CrossRef]
- Ozkose Z, Ercan B, Unal Y, et al. Inhalation versus total intravenous anesthesia for lumbar disc herniation: comparison of hemodynamic effects, recovery characteristics, and cost. J Neurosurg Anesthesiol. 2001;13(4):296-302. [CrossRef]
- Van Allen NR, Krafft PR, Leitzke AS,, et al. The role of Volatile Anesthetics in Cardioprotection: a systematic review. Med Gas Res. 2012 Aug 28;2(1):22. PMID: 22929111; PMCID: PMC3598931. [CrossRef]
- Zangrillo A, Testa V, Aldrovandi V et al. Volatile agents for cardiac protection in noncardiac surgery: a randomized controlled study. J Cardiothorac Vasc Anesth. 2011 Dec;25(6):902-7. Epub 2011 Aug 27. PMID: 21872490. [CrossRef]
- Lim A, Braat S, Hiller J, Riedel B. Inhalational versus propofol-based total intravenous anaesthesia: practice patterns and perspectives among Australasian anaesthetists. Anaesth Intensive Care. 2018;46(5):480-487. [CrossRef]
- Pandit JJ, Andrade J, Bogod DG, et al. 5th National Audit Project (NAP5) on accidental awareness during general anaesthesia: summary of main findings and risk factors. Br J Anaesth. 2014;113(4):549-559. [CrossRef]
- Thiel CL, Eckelman M, Guido R, et al. Environmental impacts of surgical procedures: life cycle assessment of hysterectomy in the United States. Environ Sci Technol. 2015;49(3):1779-1786. [CrossRef]
- Latta M, Shaw C, Gale J. The carbon footprint of cataract surgery in Wellington. N Z Med J. 2021;134(1541):13-21. Published 2021 Sep 3.
- Webster J, Radke E, George N, Faoagali J, Harris M. Barrier properties and cost implications of a single versus a double wrap for storing sterile instrument packs. Am J Infect Control. 2005;33(6):348-352. [CrossRef]
- Smith TO, Sexton D, Mann C, Donell S. Sutures versus staples for skin closure in orthopaedic surgery: meta-analysis. BMJ. 2010;340:c1199. Published 2010 Mar 16. [CrossRef]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).