1. Introduction
In an intensive care unit (ICU), situation awareness and prompt response to patient status changes are crucial, particularly when looking after multiple, potentially deteriorating, patients [
1,
2]. With higher patient loads and an aging population, the patient-to-care provider ratio, particularly for nursing staff, has significantly increased [
3]. In such circumstances, the risk of not promptly perceiving a potential problem and taking appropriate action raises the chances of medical errors and, consequently, patient morbidity and mortality [
1,
3,
4,
5]. Situation awareness plays a crucial role in medical settings. It is described as the cognitive process of perceiving, comprehending, and projecting the clinical situation, enabling healthcare professionals to make informed decisions and take timely actions to ensure patient safety and optimal outcomes [
2,
6,
7]. The concept of situation awareness provides a framework for developing user-centered design systems [
8]. Instead of simply presenting raw information, user-centered design integrates data in a way that aligns with users' abilities and needs. This approach is motivated by the goal of achieving optimal functioning of the human-machine interaction as a whole and ensuring safety [
8,
9].
An example of user-centered visualization technology is Philips Visual Patient Avatar [
10,
11,
12]. It is an innovative approach to patient monitoring that is designed to enhance user`s situation awareness [
10,
11]. This technique transforms alphanumeric monitoring data into a visual format represented by the avatar. Philips Visual Patient Avatar dynamically displays the patient's current vital signs through modifications in color, shape, and animations. This technology is guided by a user-centered design philosophy inspired by Endsley [
9], logical principles from Wittgenstein's Tractatus Logico-Philosophicus [
13], and insights from human-computer interaction as described in NASA's publication "On Organization of Information: Approach and Early Work" by Degani et al [
14]. Since March 2023, this technique has been integrated into Philips® IntelliVue MX patient monitors [
15]. This approach enables a more efficient perception of vital signs [
10,
16] and increases the likelihood of verbalizing the cause of the emergencies [
17] compared to conventional monitoring. Furthermore, computer-based studies showed that Phillips Visual Patient Avatar significantly improves diagnostic confidence among anesthetists and reduces workload compared to standard monitoring [
10,
16,
17,
18,
19].
An extended version of Visual Patient Avatar, called Visual Patient Avatar ICU, is currently being developed and investigated. Visual Patient Avatar ICU can additionally display patient-inserted devices such as arterial, central lines and urinary catheters along with their respective insertion locations (
Figure 1) [
19]. A previous computer-based study has demonstrated that the Visual Patient Avatar ICU improves information transfer, enhances diagnostic confidence, and reduces the perceived workload of ICU staff compared to conventional monitor modalities [
19].
This study aimed to evaluate user perception and acceptance of Visual Patient Avatar ICU among physicians and nurses in multiple intensive care units across various international hospitals. The feedback gathered from critical care staff helps identify the strengths and potential for improvement of this newly developed technology and contributes to its further improvement before clinical implementation.
2. Materials and Methods
The Materials and Methods should be described with sufficient details to allow
2.1. Approval and Consent
Based on the local regulations in Switzerland, Germany, and Spain, ethical approval was not required, as this study did not fall within the scope of the Human Research Act. The leading ethics committee in Zurich, Switzerland provided a declaration of non-jurisdiction. However, all participants provided written consent for recording, statistical analysis, and data publication.
2.2. Study design
This was an international, multi-center, researcher-initiated study utilizing an exploratory sequential mixed-methods design. The study was conducted across five tertiary care hospitals, namely the University Hospital of Zurich and Hirslanden Clinic of Zurich in Switzerland, the University Hospital of Frankfurt and University Hospital of Wuerzburg in Germany, and the Hospital Clinic de Barcelona in Spain. We interviewed the participants between June and August 2021. The online survey was conducted between July and October 2021. In this study, we included the same 50 participants who were part of a previous computer-based study that compared two different patient monitoring modalities (Visual Patient Avatar ICU versus conventional monitor) [
19].
2.3. Previous Study
In this the previous computer-based study, a total of 50 participants, consisting of five ICU nurses and five physicians at each of the five study sites, engaged with five distinct patient scenarios [
19]. These scenarios were presented twice, once as Visual Patient Avatar ICU and once as the conventional modality, resulting in a total of ten cases per participant. This study aimed to examine the impact of Visual Patient Avatar ICU on information transfer, which was assessed by accuracy in evaluating vital signs and installations [
19]. Subsequent to the completion of all cases, structured interviews were conducted as an integral component of this mixed-methods study.
2.4. Participant Interviews and Online Survey
2.4.1. Part I: Participant interviews
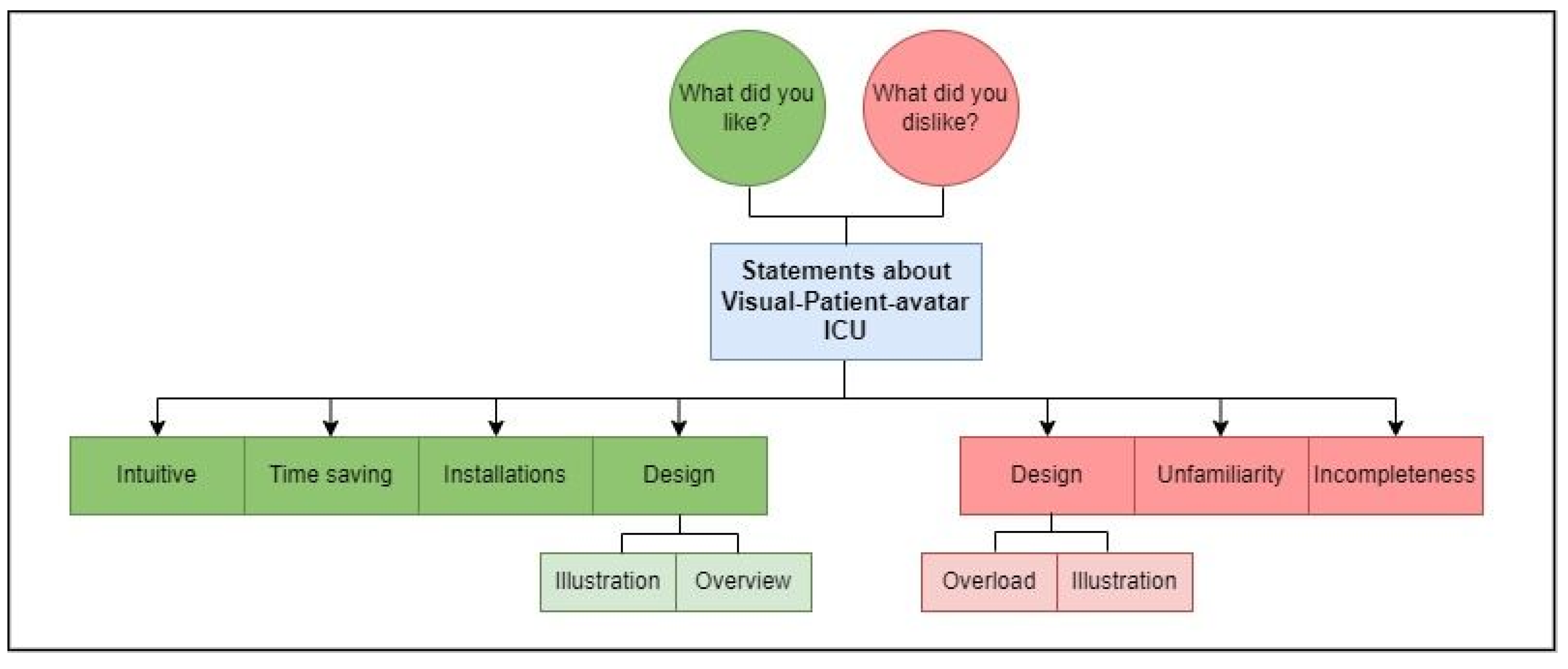
In the interview phase of our study, we requested input from all participants regarding two questions: "What did you like about Visual Patient Avatar ICU?" and "What did you dislike about Visual Patient Avatar ICU?" directly after they participated in the computer-based study. We aimed to investigate the positive and negative perceptions of Visual Patient Avatar ICU immediately after its use. Participants were instructed to record their thoughts as field notes using an iPad (Apple Inc., Cupertino, USA), utilizing two separate text boxes. There was no specified time constraint, and we accommodated responses in German, Spanish, or English.
In addition, a brief demographic survey was conducted to collect participant characteristics. To commence the systematic analysis, the field notes provided by participants in German and Spanish were translated into English using the online translation service DeepL (DeepL GmbH, Cologne, Germany) (supplementary material). The translated results underwent individual assessment to ensure plausibility and accuracy. Subsequently, the two authors, EAB and LB, organized the translated field notes into separate statements based on content topics. The authors (EAB, SA, LB) identified recurring patterns in responses and developed a coding tree that encompassed the major topics and subthemes addressed by the participants (
Figure 2) [
20]. EAB and LB independently assigned all statements to the coding tree. To validate this process, percentage agreement and inter-rater reliability calculations were conducted. In divergent allocations, the two raters engaged in discussions and reached mutual agreement to determine the appropriate coding.
2.4.2. Part II: Online survey
For the second phase of the study, we formulated five statements based on the major topics identified through our qualitative assessment. An online questionnaire was created using SurveyMonkey (SVMK Inc., San Mateo, USA), and the corresponding link was emailed to all previous participants, inviting them to evaluate the statements on a 5-point Likert Scale ranging from strongly disagree to strongly agree. Additionally, we collected anonymous demographic data. Participation in the online survey required less than five minutes. A single reminder to complete the questionnaire was sent after ten days. After an additional week, the survey portal was closed, concluding the data collection process. To ensure consistent timing, we contacted the different study centers staggered, maintaining approximately 40-day intervals between the qualitative and quantitative phases of the study.
2.5. Statistical analysis
Data management and creation of figures were performed with Microsoft Word, Excel and PowerPoint (Microsoft Corporation, Redmond, Washington, USA). In the qualitative study section, we present the number of statements and their respective percentages in relation to the total number of statements and major topics. To address the consistency of EAB and LB ratings, we calculated the percent agreement and inter-rater reliability using Cohen's kappa in R version 4.0.5 (R Foundation for Statistical Computing, Vienna, Austria). The results of the quantitative study section are reported as medians with interquartile ranges. We used the one-sample Wilcoxon signed-rank test (IBM SPSS Statistics 26, International Business Machines Corporation, Armonk, New York, USA) to evaluate the symmetry of the answer distribution to the given statements around the median (representing the neutral response) and to determine any tendency towards agreement or disagreement. Statistical significance was defined as P<0.05.
3. Results
3.1. Study and Participant Characteristics
We recruited 25 nurses and 25 physicians from ICUs to participate in structured interviews. Of these, 40 participants (80%) later responded to the email invitation and completed the online survey. The characteristics of the participants are provided in
Table 1.
3.2. Part I: Participant interviews
3.2.1. Coding template
By analyzing the field notes obtained, we derived a total of 148 statements. Using an inductive free coding approach we identified four major positive themes and three major negative themes [
20], (
Figure 2). Using the coding template, the percentage agreement between EAB and LB in assigning the 148 statements was 82.4%. The calculated inter-rater reliability, indicated by Cohen's kappa of 0.802, demonstrated substantial agreement [
21,
22].
Despite several discussions, 9 out of the 148 statements (6%) remained unclear in terms of their meaning or intention and were classified as "not codable". After this process was completed, the percentage agreement reached 100%, and the remaining 139 statements were used as a reference for further calculations.
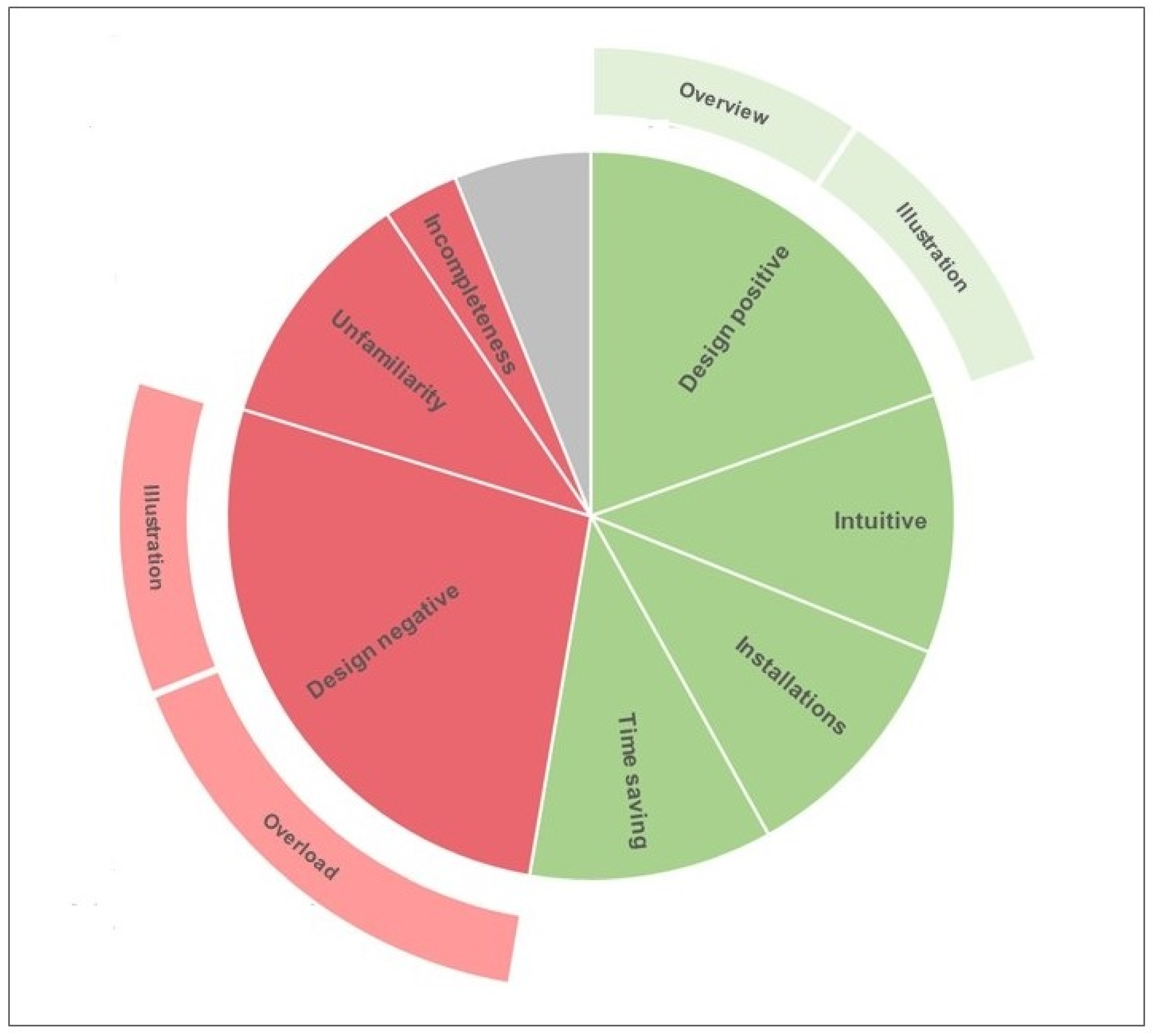
Overall, participants expressed moderately more positive statements (78/139, 56%) than statements regarding their dislikes of the Visual Patient Avatar ICU (61/139, 44%).
Figure 3 provides an overview of the distribution of all statements derived from the field notes commenting on Visual Patient Avatar ICU.
Table 2 outlines the major themes with their hierarchical subthemes and the corresponding percentages and examples. In the subsequent section, we provide a detailed description of the categories and participants' perceptions.
3.2.2. Positive statements about Visual Patient Avatar ICU
3.2.2.1. Design
Of the 139 statements analyzed, 29 (21%) were related to positive design features of Visual Patient Avatar ICU. We further categorized this major topic into two subthemes: "Overview," comprising 14 of the 139 statements (10%), and "Illustration," comprising 15 of the 139 statements (11%). Participants appreciated the presentation of information in a simple overview format, as it allowed them to grasp everything at a glance (participant #8). Regarding the Visual Patient Avatar ICU illustration, the use of colored markings (participant #6) was frequently mentioned as a positive design feature. Additionally, participants, such as participant #12, expressed their liking for the visualization of organ systems.
3.2.2.2. Intuitiveness
Within the analyzed statements, 17 out of 139 (12%) highlighted characteristics such as simple handling and easy understanding (participant #26) associated with Visual Patient Avatar ICU. These findings were consolidated under the major topic "Intuitive" with agreement between the raters. Participant #7 mentioned that the system facilitated better retention of information, while participant #3 emphasized a quick learning curve in interpreting the Visual Patient Avatar ICU.
3.2.2.3. Time Saving
We identified "Time saving" as another major topic, comprising 16 out of 139 (12%) statements. Participant #9 stated that serious problems were clearly presented immediately, enabling quick problem identification (participant #50).
3.2.2.4. Patient inserted devices
Among the positive statements, the feature of displaying patients' installations was frequently highlighted, leading us to define it as another major topic, with 16 out of 139 (12%) statements. Participant #10 mentioned that the installations were immediately clear, making it easier for some participants to memorize the catheters (participant #5)
3.2.3. Negative statements about Visual Patient Avatar ICU
3.2.3.1. Design
The design of the Visual Patient Avatar ICU received critical feedback in 40 out of 139 statements (29%), which we identified as a major topic. Two distinct subthemes emerged, namely "Overload" and "Illustration," accounting for 24 out of 139 statements (17%) and 16 out of 139 statements (12%), respectively. Several participants raised concerns about overlapping information (participant #18) and a crowded visual representation (participant #21), resulting in sensory overload during initial exposure (participant #27). Moreover, specific aspects of the illustration were brought up in various statements. For instance, Participant #17 expressed the opinion that the graphics could benefit from a more professional appearance. Participant #12 commented on the lack of visual impact in the representation of the tidal volume, while Participant #16 criticized the central venous pressure visualization.
3.2.3.2. Unfamiliarity
Concerning the negative aspects of the Visual Patient Avatar ICU, the participants' responses indicated a prevalent perception of "Unfamiliarity," with 16 out of 139 statements (12%) addressing this issue. It became evident that, similar to Participant #35 who mentioned that "It takes time to get used to it," other participants also asserted the need for "A period of habituation" (participant #39) or emphasized the necessity for "more practice" (participant #49).
3.2.3.3. Incompleteness
Among the 139 statements analyzed, 5 (4%) expressed concerns regarding "Incompleteness," which was identified as an additional major topic through inductive free coding. Participant #4 mentioned missing numbers as a specific example of this incompleteness. In another statement, Participant #20 critically questioned the level of saturation, asking, "Saturation low: how low is it? 90% or 70%?"
3.3. Part II: Online Survey
The results of the assessment of the five statements, based on the major topics identified during the qualitative analysis of the field notes, are graphically represented in
Figure 4.
4. Discussion
4.1. Principal Findings
Visual Patient Avatar ICU received positive feedback regarding its design features, intutiveness, time saving aspect, and the display of patient-inserted devices. Participants appreciated the simple overview format, color markings and visualization of organ systems. The system was perceived as easy to understand and facilitated information retention.
On the other hand, concerns were raised about crowded visual presentation and sensory overload. Unfamiliarity was a prevalent perception, emphasizing the need for time and practice to become accustomed to the system. Incompleteness was also mentioned, particularly regarding missing information and clarity of certain parameter.
Our data are consistent with previous studies investigating user perception of Visual Patient Avatar among anesthesiology personnel. One of the first studies researching Visual Patient Avatar monitoring in 2018 highlighted that over 80% of anesthesia providers found it intuitive and easy to learn [
11,
23]. Furthermore, study participants could correctly identify above 70% of all vital signs visualizations without any prior training [
15], confirming our results that users find Visual Patient Avatar intuitive. This further translates that Visual Patient Avatar can be easily thought in a classroom-based setting. Rössler et al. compared different teaching setting for Visual Patient Avatar instructions: on one-to-one basis or classroom-based instructions [
24]. Although one-to-one instructions were most effective, the class instructions showed also to be a highly effective teaching model. However, one needs to recognize the need of some critical care professionals to work over extended period with the new visualization technology to have the feeling of familiarity and routine in daily practice.
The extended version of Visual Patient Avatar, Visual Patient Avatar ICU, additionally displays patient-inserted devices such as arterial and central lines, providing critical care staff with a better overview of a patient. This can provide critical care staff with a better overview of a patient. The authors believe that it may also potentially facilitate hand over and prevent omission of a certain patient-inserted devices. The routine check of patient-inserted devices for signs of infection, change of dressing and recognizing the extended period of device in situ requiring removal is highly crucial and prevents nosocomial infections and subsequent complications [
25,
26,
27,
28,
29]. The first step in care for patient-inserted devices care is awareness that these are present.
On the other hand, extra visualizations providing us with valuable additional information may contribute to information overload. These have been described as “sensory overload during initial exposure” or “crowded” by less than 20% of study participants. There is a fine balance to find in providing medical staff with compact information and at the same time not overwhelming the clinical picture. Interestingly, Visual Patient Avatar ICU in its current form has been found to lower perceived workload in a computer.based settings [
19]. This implies that although to some participants it may appear crowded, it is still simplifying the process of comprehension of patient monitoring. Furthermore, Görges et al. demonstrated that enhanced patient monitoring with additional information resulted in shorter median decision-making times, improved nurse triaging, and reduced frustration by implementing a broader perspective on ICU monitoring[
1].
Another issue worth addressing is a sense of incompleteness that has been expressed in a qualitative part of our study. Missing numbers in Visual Patient Avatar ICU were for few study participants leading to uncertainty. This is consistent with data from other studies that investigated three different monitoring systems: Visual Patient Avatar, conventional monitor and split screen combining both modalities [
30]. The positive response to the split screen monitoring system was that it provides a symbiotic modality that helps to focus on vital parameter changes, first spotting it on Phillips Visual Patient Avatar, followed by quantification on conventional monitoring and thus increasing its safety [
30].
4.2. Strengths and Limitations
This study has its strengths and limitations. It was a multicenter, international study across three European countries including large university hospitals. This design should reduce selection bias and confounding factors for intercultural differences, diverse clinical settings and healthcare systems.
Qualitative research involves analyzing non-numeric data to uncover overall trends and deeper meanings in individual responses without assigning frequencies to the issues identified in the data [
31]. This leads to equal attention to rare and frequently described points. Furthermore, the inability to test for statistical significance reduces the confidence in data generalizability compared to quantitative data [
31]. To compensate it, we performed a sequential mixed-methods study: the conclusions from the initial qualitative study served as the foundation for the second quantitative phase, which assessed the consistency and generalizability of the findings. Combining qualitative and quantitative approaches in a mixed-methods design allowed for the examination of complex phenomena and produced more robust results than using either method alone.
Furthermore, study participants’ recruitment was not purely random and was dependent on doctors and nurses availability and schedule of the initial simulation study [
19]. There is, however, little reason to believe that staffs availability would introduce significant bias for user-perception of Visual Patient Avatar ICU.
5. Conclusion
This study marks the initial attempt to assess the user perception of Visual Patient Avatar ICU among physicians and nurses in multiple intensive care units across various international hospitals directly after working with the technology in the computer-based study. The main objective of the research was to identify the strengths and potential for improvement of this innovative monitoring technology and contribute to its further improvement before its implementation in clinical settings. Overall, critical care professionals expressed a positive attitude towards Visual Patient Avatar ICU, describing it as an easy and intuitive tool that enhances information retention and facilitates problem identification. Participants appreciated the presentation of information in a simple overview format, as it allowed them to grasp everything at a glance. However, a subset of participants raised concerns about potential information overload, initial unfamiliarity with the technology, and a sense of incompleteness when patient monitoring numbers were not included. These findings offer valuable insights into the user perception of Visual Patient Avatar ICU and encourage further development before its clinical implementation.
6. Patents
Please see Conflicts of Interest section.
Supplementary Materials
The following supporting information can be downloaded at the website of this paper posted on Preprints.org, Translated field notes collected during interviews. Translated participants’ field notes. Translated field notes (in English) of 50 participants of this study. The brackets [ ] indicate which parts were each assessed as one statement.
Author Contributions
Conceptualization, L.B., E.A.B., T.R.R., S.A., M.T.G., P.M., S.H., K.Z., F.J.R., E.R., M.L., D.W.T.; Methodology, T.R.R., D.W.T., L.B.; Software, T.R.R., E.A.B.; Validation, T.R.R., Y.Y. and Z.Z.; Formal Analysis, E.A.B., D.W.T., L.B.; Investigation, L.B., P.M., T.R., S.A., E.A.B., M.T.G., S.H. K.Z., F.J.R., E.R., M.L., D.W.T.; Resources, D.W.T.; Data Curation, L.B., J.L.; Writing – Original Draft Preparation, J.L., G.G., E.A.B., L.B.; Writing – Review & Editing, J.L., T.R.R., G.G., C.B.N, L.B., P.M., S.H., K.Z., F.J.R., E.R., M.L.; Visualization, L.B., J.L., G.G.; Supervision, J.L, D.W.T.; Project Administration, J.L.; Funding Acquisition, D.W.T.
Funding
The Institute of Anesthesiology of the University Hospital of Zurich, Zurich, Switzerland and the University of Zurich, Zurich, Switzerland funded this project.
Institutional Review Board Statement
The study was conducted according to the guidelines of the Declaration of Helsinki. The Cantonal Ethics Committee of the Canton of Zurich in Switzerland, reviewed the study protocol and issued a declaration of no jurisdiction (Business Management System for Ethics Committees Number Req-2021-00102). We obtained written informed consent from all participants for the use of their data.
Informed Consent Statement
Informed written consent was obtained from all subjects involved in the study to publish this paper.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Acknowledgments
The authors are thankful to the study participants for their time and effort.
Conflicts of Interest
TRR is an inventor of Visual Patient Predictive technology, for which the University of Zurich and Koninklijke Philips N.V. hold patent applications and design protections. Joint-development and licensing agreements exist with Philips Medizin Systeme Böblingen GmbH, Böblingen, Germany; Koninklijke Philips N.V., Amsterdam, The Netherlands; Philips Research/Philips Electronics Nederland BV, Eindhoven, The Netherlands; and Philips USA, Cambridge, MA, USA. Within the framework of these agreements, TRR receives travel support, lecturing and consulting honoraria, and may potentially receive royalties in the event of successful commercialization. TRR is an inventor of Visual Blood technology, for which the University of Zurich holds patent applications and design protections; potential royalties may follow successful commercialization. CBN is an inventor of Visual Patient and Visual Patient Predictive technologies, for which the University of Zurich and Koninklijke Philips N.V. hold patents, patent applications, design protections, and trademarks. Joint-development and licensing agreements exist with Philips Medizin Systeme Böblingen GmbH, Böblingen, Germany; Koninklijke Philips N.V., Amsterdam, The Netherlands; Philips Research/Philips Electronics Nederland BV, Eindhoven, The Netherlands; and Philips USA, Cambridge, MA, USA. Within the framework of these agreements, CBN receives travel support, lecturing and consulting honoraria, and may potentially receive royalties in the event of successful commercialization. CBN is an inventor of Visual Clot technology, with patent applications, design protections, and trademarks held by the University of Zurich. In case of successful commercialization, CBN may receive royalties. CBN is an inventor of Visual Blood technology, for which the University of Zurich holds patent applications and design protections; potential royalties may follow successful commercialization. CBN received travel support, lecturing, and consulting honoraria from Instrumentation Laboratory – Werfen, Bedford, MA, USA. DWT is the first named inventor of Visual Patient and Visual Patient Predictive technologies, for which the University of Zurich and Koninklijke Philips N.V. hold patents, patent applications, design protections, and trademarks. Joint-development and licensing agreements exist with Philips Medizin Systeme Böblingen GmbH, Böblingen, Germany; Koninklijke Philips N.V., Amsterdam, The Netherlands; Philips Research/Philips Electronics Nederland BV, Eindhoven, The Netherlands; and Philips USA, Cambridge, MA, USA. Within the framework of these agreements, DWT receives research funding, travel support, lecturing and consulting honoraria, and may potentially receive royalties in the event of successful commercialization. DWT also holds a position on the Philips Patient Safety Advisory Board. DWT is the first named inventor of Visual Clot technology, with patent applications, design protections, and trademarks held by the University of Zurich. In case of successful commercialization, DWT may receive royalties. DWT is the first named inventor of Visual Blood technology, for which the University of Zurich holds patent applications and design protections; potential royalties may follow successful commercialization. Additionally, DWT received travel support, lecturing, and consulting honoraria from Instrumentation Laboratory – Werfen, Bedford, MA, USA, the Swiss Foundation for Anaesthesia Research in Zurich, Switzerland, and the International Symposium on Intensive Care and Emergency Medicine in Brussels, Belgium. KZ has received honoraria for participation in advisory board meetings for Haemonetics and Vifor and received speaker fees from CSL Behring, Masimo, Pharmacosmos, Boston Scientific, Salus, iSEP, Edwards and GE Healthcare. He is the Principal Investigator of the EU-Horizon 2020 project ENVISION (Intelligent plug-and-play digital tool for real-time surveillance of COVID-19 patients and smart decision-making in Intensive Care Units) and Horizon Europe 2021 project COVend (Biomarker and AI-supported FX06 therapy to prevent progression from mild and moderate to severe stages of COVID-19). KZ leads as CEO the Christoph Lohfert Foundation as as well as the Health, Patient Safety & PBM Foundation. The other authors report no conflicts of interest regarding this paper.
References
- Görges, M., et al., A far-view intensive care unit monitoring display enables faster triage. Dimens Crit Care Nurs, 2011. 30(4): p. 206-17. [CrossRef]
- Wright, M.C., J.M. Taekman, and M.R. Endsley, Objective measures of situation awareness in a simulated medical environment. Qual Saf Health Care, 2004. 13 Suppl 1(Suppl 1): p. i65-71. [CrossRef]
- Neuraz, A., et al., Patient Mortality Is Associated With Staff Resources and Workload in the ICU: A Multicenter Observational Study. Crit Care Med, 2015. 43(8): p. 1587-94. [CrossRef]
- Knight, L.D., Staffing Ratios and Patient Outcomes: Looking Beyond Nurses, Doctors, and Survival at ICU Discharge. Crit Care Med, 2016. 44(2): p. e107-8. [CrossRef]
- Pastores, S.M., Staffing Ratios and Workload in Critically Ill Patients: Do They Impact Outcomes? Crit Care Med, 2015. 43(8): p. 1775-6. [CrossRef]
- Endsley, M.R., A Systematic Review and Meta-Analysis of Direct Objective Measures of Situation Awareness: A Comparison of SAGAT and SPAM. Hum Factors, 2021. 63(1): p. 124-150. [CrossRef]
- Schulz, C.M., et al., Situation awareness in anesthesia: concept and research. Anesthesiology, 2013. 118(3): p. 729-42. [CrossRef]
- JDOFE., R., How user-centered design supports situation awareness for complex interfaces. Human–Computer Interaction Series: Jean Vanderdonckt. 2021: Q. Vera Liao. [CrossRef]
- Endsley, M.R., Designing for Situation Awareness An Approach to User-Centered Design. 2nd ed. 2011: CRC Press Inc. Boca Raton, FL, USA.
- Gasciauskaite, G., et al., Human-centered visualization technologies for patient monitoring are the future: a narrative review. Crit Care, 2023. 27(1): p. 254. [CrossRef]
- Tscholl, D.W., et al., Situation Awareness-Oriented Patient Monitoring with Visual Patient Technology: A Qualitative Review of the Primary Research. Sensors (Basel), 2020. 20(7). [CrossRef]
- Philips. A new way to see your patient's vitals takes shape https://www.philips.co.uk/healthcare/technology/visual-patient-avatar.
- Wittgenstein, L., Tractatus Logico-Philosophicus. 1922, London, UK: Routledge & Kegan Paul.
- Degani A. JD, I.D.L., Shafto M., Olson L., On Organization of Information: Approach and Early Work. NASA Ames Research Center. 2009.
- Wetli, D.J., et al., Improving Visual-Patient-Avatar Design Prior to Its Clinical Release: A Mixed Qualitative and Quantitative Study. Diagnostics (Basel), 2022. 12(2). [CrossRef]
- Tscholl, D.W., et al., Using an animated patient avatar to improve perception of vital sign information by anaesthesia professionals. Br J Anaesth, 2018. 121(3): p. 662-671. [CrossRef]
- Roche, T.R., et al., Avatar-based patient monitoring in critical anaesthesia events: a randomised high-fidelity simulation study. Br J Anaesth, 2021. 126(5): p. 1046-1054. [CrossRef]
- Garot, O., et al., Avatar-based versus conventional vital sign display in a central monitor for monitoring multiple patients: a multicenter computer-based laboratory study. BMC Med Inform Decis Mak, 2020. 20(1): p. 26. [CrossRef]
- Bergauer, L., et al., Avatar-based patient monitoring improves information transfer, diagnostic confidence and reduces perceived workload in intensive care units: computer-based, multicentre comparison study. Sci Rep, 2023. 13(1): p. 5908. [CrossRef]
- Guetterman, T.C., M.D. Fetters, and J.W. Creswell, Integrating Quantitative and Qualitative Results in Health Science Mixed Methods Research Through Joint Displays. Ann Fam Med, 2015. 13(6): p. 554-61. [CrossRef]
- Viera, A.J. and J.M. Garrett, Understanding interobserver agreement: the kappa statistic. Fam Med, 2005. 37(5): p. 360-3.
- Koch, G.G., et al., A general methodology for the analysis of experiments with repeated measurement of categorical data. Biometrics, 1977. 33(1): p. 133-58. [CrossRef]
- Tscholl, D.W., et al., User perceptions of avatar-based patient monitoring: a mixed qualitative and quantitative study. BMC Anesthesiol, 2018. 18(1): p. 188. [CrossRef]
- Rössler, J., et al., Correction: Comparing Classroom Instruction to Individual Instruction as an Approach to Teach Avatar-Based Patient Monitoring With Visual Patient: Simulation Study. JMIR Med Educ, 2020. 6(2): p. e24459. [CrossRef]
- Pitiriga, V., et al., Lower risk of bloodstream infections for peripherally inserted central catheters compared to central venous catheters in critically ill patients. Antimicrob Resist Infect Control, 2022. 11(1): p. 137. [CrossRef]
- Mimoz, O., et al., [Practice assessment of central venous lines care in surgical ICU of French university hospitals]. Ann Fr Anesth Reanim, 2010. 29(2): p. 104-12. [CrossRef]
- Carrer, S., et al., Effect of different sterile barrier precautions and central venous catheter dressing on the skin colonization around the insertion site. Minerva Anestesiol, 2005. 71(5): p. 197-206.
- Bacuzzi, A., et al., Recommendations and reports about central venous catheter-related infection. Surg Infect (Larchmt), 2006. 7 Suppl 2: p. S65-7. [CrossRef]
- Alanazi, F.K., et al., Healthcare-associated infections in adult intensive care units: A multisource study examining nurses' safety attitudes, quality of care, missed care, and nurse staffing. Intensive Crit Care Nurs, 2023. 78: p. 103480. [CrossRef]
- Akbas, S., et al., User Perceptions of Different Vital Signs Monitor Modalities During High-Fidelity Simulation: Semiquantitative Analysis. JMIR Hum Factors, 2022. 9(1): p. e34677. [CrossRef]
- P, O., An Analysis of the Strengths and Limitation of Qualitative and Quantitative Research Paradigms. Probl. Educ. 21st Century., 2009. 13:13–38.
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).