1. Introduction
Tooth extractions may be an unpleasant and painful experience for a child [
1]. Pain felt during dental treatments, especially tooth extraction; is the most common complication. It is known that dental fear and anxiety occur in pediatric patients whose pain control cannot be achieved during and after tooth extraction [
2]. Post-extraction wound healing and pain perception; are related to host-related factors such as the patient's immune system, the use of painkillers and antibiotics, the presence of infection in the region, and the atraumatic nature of the procedure. Trauma to the area whose numbness continues after local anesthesia by biting can also cause inflammation and pain in that area after extraction. Pain management during and after tooth extraction is part of behavioral guidance, especially in pediatric patients [
3,
4].
Low-level laser therapy (LLLT) is a widely used adjuvant medical treatment for wound healing [
5]. It is based on the idea that exposure to a specific wavelength can alter cellular behavior, resulting in both an increase in cell number and an increase in cell me-
metabolism [
6]. Aside from not having any negative effects, LLLT is an athermic, photobiological, and non-destructive therapy approach. Low-level working lasers typically operate at a wavelength of 630-980 nm and in the 50-550 mW range. They are also smaller and more cost-effective. These therapeutic lasers are used in a process known as "low-level laser therapy," "biostimulation," or "biomodulation." Herpes simplex, mucositis, post-surgical pain and inflammation prevention delay, and dysfunction of the temporomandibular joint are a few conditions where therapeutic lasers are used [
7,
8].
Another consequence of LLLT reported in vivo is that it boosts macrophage phagocytic activity in the early phases of tissue formation after damage. This indicates that wound debridement is facilitated, creating the circumstances for the proliferative phase of healing to begin [
9]. Histologically, a blood clot forms and turns into granulation tissue in the first 6-8 weeks after extraction, which is eventually replaced by mineralized and immature bone. During this time, applying LLLT to the extraction socket has no side effects, instead stimulating an inflammatory response that promotes tissue repair. It is defined as a biostimulation method that speeds up wound healing and thereby eliminates post-extraction discomfort [
10].
The purpose of this study is to evaluate clinically and radiologically the effect of LLLT on the healing sockets in pediatric patients who are scheduled to have bilateral primary molar teeth extracted, as well as to determine whether it influences pain management. Our H1 hypothesis was confirmed in our study: LLLT promotes faster healing in pediatric extraction sockets compared to the control group, and H2 less pain is reported at the extraction site.
2. Materials and Methods
2.1. Study Design
This double-blind, split-mouth, randomized clinical trial study was designed to evaluate the effectiveness of LLLT on the postoperative results of primary molar tooth extractions in patients who applied to Necmettin Erbakan University Faculty of Dentistry, Department of Pedodontics between November 2017 and April 2018. Our study was carried out with the approval of the Ethics Committee of Necmettin Erbakan University Faculty of Dentistry, numbered 2017-07.
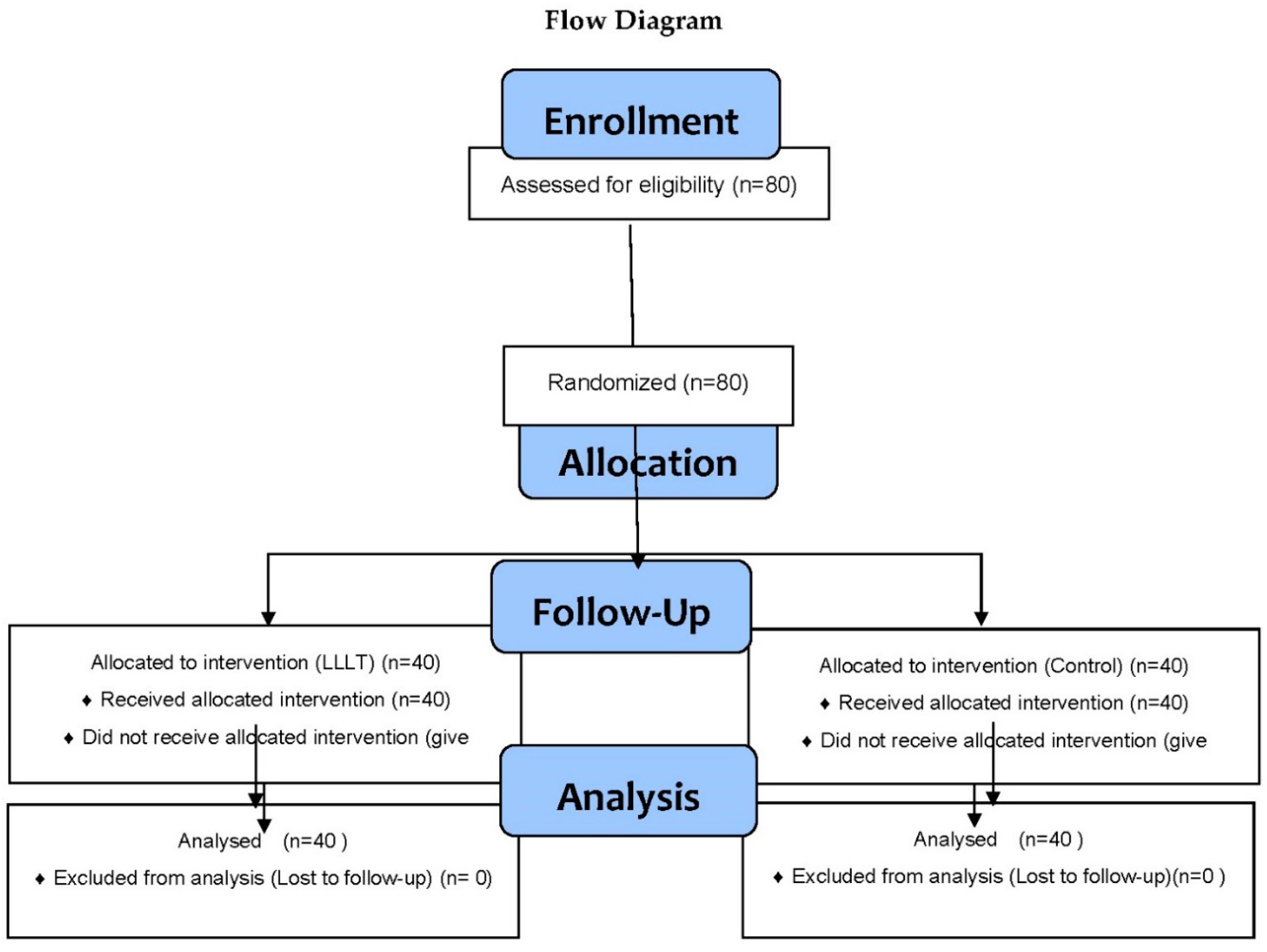
The minimum number of teeth to be evaluated in the study was found to be 35 according to the G Power test applied considering the data obtained in the sample studies, but n=40 was taken to avoid loss of patient-related data (α=0.05).
Our study included children aged 6 to 10 years old who did not have any systemic disease and had a Frankl behavioral scale score of 3 or 4 [
11]. The procedures and their adverse effects were thoroughly described to the parents of the pediatric patients, and the informed consent form was reviewed and signed by the parents, who also received a copy.
2.2. Inclusion Criteria of Teeth
As a result of clinical and radiographic evaluations of pediatric patients, it was taken into account that there was an indication for tooth extraction in bilateral primary molars, that they did not have any systemic disease, and that the use of antibiotics and painkillers was stopped at least 12 hours ago. During the radiographic evaluation, attention was paid to the fact that bilateral primary molars do not require complicated tooth extractions, do not show signs of infection, and have almost the same level of atraumatic extraction indications.
2.3. Determination of Working Groups
Teeth were randomly grouped as a control group or LLLT group (
Table 1). Which group of teeth would be extracted in the first session was determined randomly with the software R 2.11.1 (R Foundation for Statistical Computing, Vienna, Austria). Randomization is performed by a non-practicing physician. By performing the same treatments on both teeth but without turning on the laser in the control tooth, patients and their parents were rendered blind to the groups.
2.4. Local Anesthesia and Tooth Extraction
Tooth extractions were performed by a single physician. Topical anesthesia (Xylocaine, Astra, Södertalje, Switzerland) was applied to the dried mucosa in the area to be localized with the help of an ear stick for 1 minute. Posterior-superior-alveolar nerve block anesthesia and palatal anesthesia were applied for the upper primary molars; Inferior-alveolar nerve block anesthesia and lingual anesthesia (Ultracain, Aventis Pharma, Istanbul, Turkey) were applied for the lower primary molars. After anesthesia control was achieved, a randomly selected tooth was extracted. Tooth extraction on the other side was performed two weeks later. During the shootings, attention was paid to the traumatic approach. After the control of bleeding was achieved, data were recorded for each group.
2.5. Approach After Tooth Extraction
In the control group, no application was made after the procedure. In the LLLT group, the diode laser device Doctor Smile Wiser (Wiser, Doctor Smile, Milan, Italy) (
Figure 1) with a wavelength of 980 nm and a power of 0.5 W was used for LLLT. During the procedure, the patient, physician, and assistant staff wore protective glasses (Wiser, Doctor Smile, Milan, Italy). With 300 mW of energy, a 400 m tip held 1 cm away from the extraction socket was applied to the extraction socket for 60 seconds from three points determined from the vestibule, lingual/palatal, and occlusal surfaces.
All pediatric patients and their parents were given information about post-extraction care, and appointments for control sessions were scheduled. The danger of damaging the soft tissue of the child's teeth, which is one of the complications of local anesthetic, was emphasized again, and the parent was instructed to notify us if this occurred.
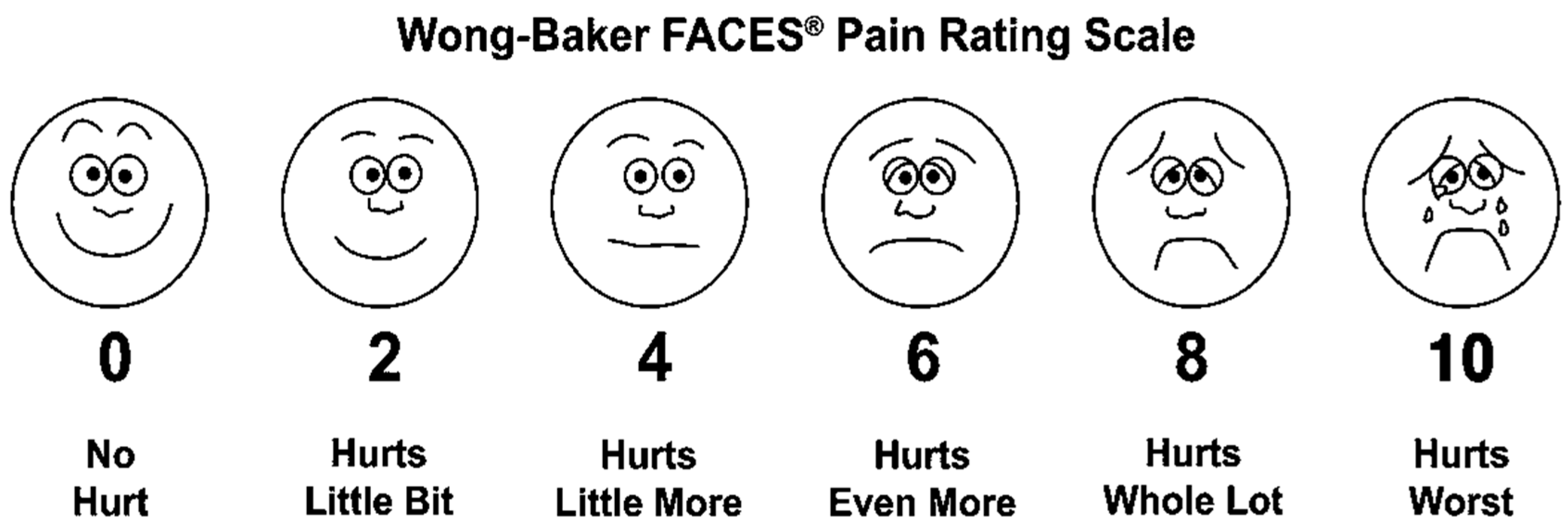
2.6. The Wong-Baker Faces Pain Rating Scale Assessments in Study Groups
Pain assessment in both groups was performed with the Wong-Baker Pain Rating Scale (Wong-Baker FACES Pain Rating Scale PRS) (
Figure 2). Patients were asked to choose a face or number from the scale, and the selected value was the practitioner dentist on the day of the procedure; other days were recorded by the parent. During the 7 days following the extraction session, the parents informed the doctors about the values chosen by the child patients from the scale given to them, the need for painkiller use, and the number of uses. Pain formation as a result of traumatizing the soft tissue by biting, which is one of the complications of local anesthesia, was not recorded.
2.7. Wound Healing Assessment
For the evaluation of soft tissue healing in extraction sockets, intraoral photographs were taken at an angle of 60° to the occlusal surface on the 3rd and 7th days following the extraction session. Non-epithelialized surface measurements were made by two observing physicians using the ImageJ (NIH, Rockville, USA) program.
2.8. Statistical Assessment
Statistical evaluations of the obtained data were made using SPSS software (SPSS 21.00; IBM, Chicago, USA). The χ² and Wilcoxon signed-rank tests were used to analyze the data. The parental ratings and the children's ratings were compared pairwise using Spearman's rank correlation coefficient.
4. Discussion
Lasers have become an indispensable tool in dentistry, serving a wide range of purposes. From surgical procedures involving the gingiva and jawbone to managing tooth decay, gingival reshaping, maxillary sinusitis, and aesthetic dental treatments, lasers have proven effective in addressing a variety of oral health issues. Additionally, they help treat conditions such as periodontitis, sensitivity, gingival discoloration, aphthae and herpes, recurrent aphthae, jaw joint disorders, and oral mucosal diseases. Lasers also play a crucial role in sterilizing root canals, treating peri-implantitis, promoting post-extraction wound healing, and facilitating implant surgery. With their precision and versatility, lasers are revolutionizing the field of dentistry and improving patient outcomes [
12,
13].
Due to their numerous advantages, soft tissue applications have seen a significant rise in the use of Nd: YAG, Er: YAG, CO2, and Diode lasers. These lasers require no or minimal anesthesia, eliminate vibration, cause minimal scarring, and shorten application times. Additionally, thanks to their hemostasis feature, they offer an expanded field of view, particularly in children. The risk of postoperative edema, pain, and infection is low, and the method does not require any stitches. This makes it a highly tolerable procedure, especially for children. The use of these lasers in soft tissue applications has greatly enhanced the safety and efficacy of the procedure, making it a preferred choice among healthcare professionals [
14,
15,
16].
Reports suggest that low-level laser therapy can potentially reduce inflammation and provide relief from post-surgery pain. This therapy can alter the pain threshold, decrease the release of bradykinin and histamine, stimulate the production of natural endorphins, and influence the production of prostaglandins [
17].
According to a recent study, patients who received orthodontic arch wire placement reported less pain when undergoing low-level laser therapy (LLLT) compared to those who received a placebo treatment. However, these results were not statistically significant (p>0.05) [
18].
According to the study conducted by Ismail et al. on post-op pain after root canal treatment, the groups were divided into LLLT, laser-activated irrigation, and control. It was observed that the control group reported the highest level of pain in 24-hour pain values, followed by LAI and LLLT (p<0.001). However, there was no significant difference found between the three groups in 72-hour measurements (p=0.179). These findings suggest that while LLLT and LAI may be effective in reducing post-op pain, further research is required to determine their long-term efficacy and potential benefits [
19].
A study conducted in 2018 found a statistically significant difference on the 7th day when the groups with and without LLLT were evaluated in cases of oral mucositis diagnosed in 101 pediatric patients receiving chemotherapy. When pain perception and analgesic use were assessed on the 4th and 7th days, the decrease on the 7th day was found to be statistically significant (p<0.007) [
20]. The research results demonstrate a clear parallelism with the presented findings.
According to a clinical study involving 60 pediatric patients diagnosed with minor recurrent oral aphthous stomatitis, it was found that LLLT administered for four consecutive days post-diagnosis led to a significant decrease in lesion size. The size reduction was measured using a periodontal probe, and it was observed that the lesion size decreased statistically significantly between the fourth and seventh days (p<0.05). Additionally, the study reported a statistically significant decrease in pain perception values on the fourth day (p=0.0001) [
21].
Herascu et al. investigated the effect of LLLT on postoperative wounds. In conclusion, they reported that LLLT at a wavelength of 904 nm stimulates postoperative aseptic wound healing [
22]. Recent studies have observed a notable effect of low-level laser therapy (LLLT) in vivo, specifically in increasing the phagocytic activities of macrophages during the initial stages of tissue formation following trauma. These findings have significant implications for the potential use of LLLT as a therapeutic intervention in the treatment of various injuries and post-operative recovery [
23,
24,
25].
It is crucial to emphasize the critical nature of these clinical advantages, particularly for children with weakened immune systems. This encompasses individuals who have insulin-dependent diabetes, previously experienced endocarditis or heart complications, have undergone heart surgery, have artificial valves, and oncology patients undergoing chemotherapy or radiation therapy.
Following a tooth extraction, rapid ridge resorption is a common occurrence that can impede the recovery of lost alveolar bone. Consequently, ridge augmentation procedures can be quite arduous and necessitate the assistance of a proficient dental professional to guarantee optimal results. A recent study conducted by Akhil et al. analyzed the changes in bone density for the test (LLLT) and control groups in terms of alveolar ridge augmentation techniques. The results revealed that the test group had a change in bone density of -136 ± 236.08 HU, while the control group had a value of -44.30 ± 180.89 HU. Interestingly, there was no statistically significant difference between the two groups in these parameters [
26]. Maintaining the three-dimensional dimensions of the alveolar bone is of utmost importance and can be achieved by accelerating the healing process of wounds. Our study has provided confirmation of this perspective, as supported by our findings.
According to a study conducted by Mandic in 2015, evidence suggests that LLLT can effectively promote bone healing around immediate implants. The study's findings indicate that LLLT may be a promising approach to improving the success rates of implant procedures. This is certainly a noteworthy development in the field of implant dentistry and one that could have far-reaching implications for both practitioners and patients alike [
27]. Overall, it is encouraging to see that research in this area continues to advance our understanding of how we can best support optimal outcomes for those undergoing pertaining alveolar bone procedures.
Mester and Tota [
28] discovered that LLLT accelerates wound healing in rats. This is because LLLT can trigger the release of growth factors, including vascular endothelial growth factor [
29]. A review of various in vivo and clinical studies, along with a meta-analysis by Woodruff et al. [
30], showed that LLLT is an efficient method for enhancing wound tensile strength and reducing the size of wounds, resulting in faster healing times. Another study by Noda et al. found that laser-treated sites had faster epithelialization compared to un-irradiated controls [
8].
According to Elbay et al.'s study, there were no statistically significant differences in pain perception between the LLLT and control groups following primary molar tooth extraction. However, mean VAS scores were slightly higher for the control group on the first and second evenings, and PRS scores were higher for the control group on the first evening. More analgesics were given to children in the control group on the first evening, but both groups received equal amounts on the next two evenings [
2].
In a recent study conducted by Paschoal and Santos-Pinto, it was found that there was parallel wound healing in both the control and laser groups after premolar tooth extraction in adolescents. Although the pain perception values were lower in the laser group, there was no significant statistical difference observed between the two groups [
31]. It's interesting to note that this clinical study produced findings that are quite similar to the results that we obtained from our research. Our findings are supported by the findings of other experts in the field.
5. Conclusions
The efficacy of LLL treatment in enhancing the healing of soft tissue, stimulating osteoclasts, and promoting osteoblast proliferation, vascularization, and collagen fiber organization has been established. Its positive effects on the inflammatory mechanism are noteworthy, as it reduces the exudative phase and promotes the healing process. Moreover, multiple cell systems, including fibroblasts, macrophages, lymphocytes, epithelial cells, and endothelium, have been shown to be influenced by LLLT, with a decrease in bradykinin levels and an increase in acetylcholine levels. The release of β-endorphins and nitric oxide further amplifies the healing process. Although the complete impact of LLLT on secondary wound healing in the extraction socket is yet to be fully understood, its benefits are undeniably apparent.