1. Introduction
Over the last few years, there has been an increased interest in the development of new materials that restore the morphology and functionality of lost tooth structure and replace missing teeth, with various chemical and mechanical properties [
1]. These would meet the growing demand for the aesthetics, biocompatibility and long-term endurance of prosthetic restoration [
2]. Conventional techniques are being replaced with computer aided design/ computer aided manufacturing (CAD/CAM) technology, as it provides a series of advantages, such as the decrease interval for prosthetic treatment, removal of classic impression and the fact that it opens up new possibilities in the choice of prosthetic materials [
2,
3,
4]. At present, several such materials are available to be processed through CAD/CAM technology, like zirconia, glass ceramics, composite resins [
5,
6,
7] and polymer reinforced with grapheme [
8].
CAD/CAM systems represent a versatile computer technology with applications in dentistry. There are three main components that are combined in a CAD/CAM system: CAI - Computer Aided Inspection - spatial data digitization or scanning to record data about the oral environment of interest (tooth and adjacent environment); CAD - Computer Aided Design - to configure the restoration to fit the production according to dental requirements; and CAM - Computer Aided Manufacturing - a numerically controlled device which produces dental restoration from a basic shape [
6,
7,
9,
10].
Apart from the clinical parameters, the mechanical properties of the restorative materials depend on the chemical composition and play an important role in the long-term performance of prosthetic restorations. The latter, when applied into the oral cavity, interacts with the oral environment, and is subjected to the action of masticatory and parafunctional forces, sometimes excessive, leading to fissures that can extend, and even to fractures, thus to a reduction in its performance.
Leucite-reinforced glass ceramic (IPS Empress) is composed of SiO
2 (60-65%wt), AL
2O
3 (16-20%wt), K
20 (10-14% wt), Na
2O (3.5-6.5%) [
5,
11]. IPS Empress CAD (IvoclarVivadent), released in 2006, is a feldspathic glass made up of 35-45% leucite crystals with a particle size between 1 and 5 microns, embedded in a glassy matrix [
12]. This material appears in the shape of blocks for lab- or chairside-fabricated ceramic restorations. Given the increased density and homogeneity of the crystals in the glassy matrix, the blocks have a flexural strength of 160 MPa, which is still deemed insufficient when faced with high masticatory forces in the posterior region [
11,
12].
There is a certain amount of literature on the clinical performance of IPS-Empress restorations. A study conducted by Brochu showed a survival rate of IPS Empress crowns after 3 to 3.5 years of about 92%-99%, while crown fracture was found to be the most common reason for failure [
13]. A systematic review concluded that adhesively luted IPS Empress crowns tend to lead to a lower fracture rate on incisors and premolars and to a slightly higher one in the case of molars and canines [
14].
Cerasmart (GC, Tokyo, Japan) is a resin matrix CAD/CAD ceramic made up of organic portion polymers (29wt%): bis-MEPP, UDMA, DMA, and inorganic components (71wt%): silica SiO
2 (20 nm) and barium glass (300 nm) nanoparticles [
5,
11]. It combines the properties of ceramics with those of composite resins [
5] and was created in order to be in place between ceramics (exhibiting high aesthetics but poor mechanical properties), and composite resins (known for their poor aesthetics despite mechanical properties closer to dentin) [
15]. A study conducted by Sorrentino compare resistance to fracture and failure mode of monolithic hybrid composite-nanoceramic Cerasmart (GC, Tokyo, Japan) crowns prepared by CAD/CAM technology with different occlusal thickness, showed that the strength of the samples increased with occlusal thickness. The thickness highly affected the mode of failure but did not influence the fracture resistance of the restoration [
16]. A current study analyzed two different cements for the cementation of Cerasmart crowns, concluded that crowns fixed with self-adhesive resin cement showed increased fracture resistance compared to those cemented with resin-modified glass ionomer cement [
17].
G-CAM (Graphenano Dental, Spain) is a material recently launched on the dental market in 2019, composed of polymethyl-methacrylate (PMMA), one of the most common denture base materials, first introduced 84 years ago [
18] and graphene, first characterized in 2004 [
19]. PMMA is a light, aesthetic, and inexpensive polymer, chemically stable but with reduced mechanical resistance that needs reinforcement. The resistance can be increased by using a variety of reinforcing agents such as fibers, fillers, nanofillers and rubberlike substances [
20,
21] such as graphene. Graphene-based materials can have different applications in dental fields, such as therapeutic delivery systems to increase bone formation and osseointegration of implants, as nanofiller in the composition of adhesives and cements, and for the fabrication of CAD/CAM restorations [
8,
22]. In a recent study, the elastic modulus and flexural strength of PMMA and PMMA reinforced with graphene were analyzed and the presence of graphene in the composition exhibited higher values of the mechanical properties analyzed. Furthermore, inhomogeneous fracture morphology, peak load and bending stiffness were deemed satisfactory [
8]. Another study assessed the stress, deflection, strain, and deformation in the pontic and connector area of the dental bridge (3 and 4 unit) using zirconia and enhanced graphene-based polymer materials at 600 N loads by virtual biomechanical analysis, i.e. 3D Finite Element Analysis. Higher values were found in graphene-based bridges than in zirconia-based bridges, and in the three-unit bridge compared to the corresponding four-unit bridge, while stress concentration was at the point of loading and at the connector areas [
23].
A systematic review evaluated the long-term clinical survival rates on single-tooth restorations made by CAD/CAM technology, the frequency of failures depending on the CAD/CAM system, the type of restoration, the selected material, and the luting agent. It becomes apparent that fractures of the restoration or tooth were the majority of technical failures, in addition to biological failures like secondary caries and endodontic problems. Regarding CAD/CAM systems, the 5-year survival rate was 93.8% for Cerec 1, 82.1% for Celay, and 90.2% for Cerec 2 restorations. One-piece endocrowns with extension into the pulp chamber had a significantly higher failure rate of all the studied restorations. Similar 5-year survival rates were noticed in the case of core crowns (92.9%), full crowns (92.3%), and inlays/onlays (92.9%). Clinically, inlays/onlays can have similar results to full-coverage crowns. By analyzing the type of material used, glass-ceramics showed the the most significant failure rates and feldspathic restorations had the highest 5-year survival rates [
24].
The aim of the study was to investigate comparatively the compressive strength of a conventional ceramic, IPS Empress (IvoclarVivadent, Lichtenstein), a hybrid nanoceramic, Cerasmart (GC, Tokyo, Japan), and a newly marketed graphene-based polymer, G-CAM (Graphenano Dental, Spain), as well as to compare the compressive strength of each material at different occlusal thicknesses. The first null hypothesis establishes that there is no statistical difference in maximum compressive strength between the CAD/CAM materials at the same occlusal thickness. The second null hypothesis states that for a given material, there is no statistical difference in maximum compressive strength, regardless of the occlusal thickness of the crowns.
2. Materials and Methods
2.1. Sample Fabrication
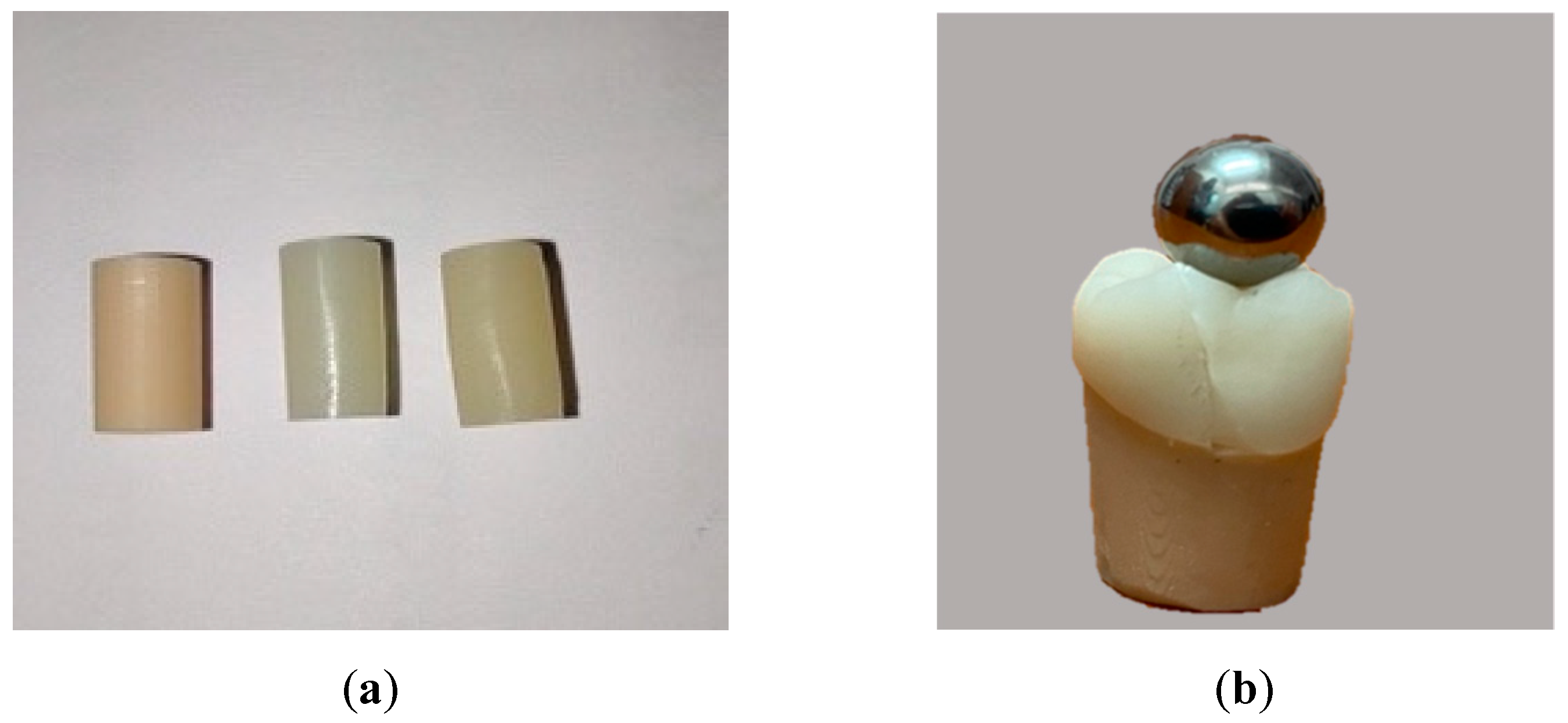
Forty-five samples representing the first mandibular molar (abutments and crowns) were designed and fabricated digitally. The abutments were milled out of Asiga Denta Model (Asiga, Australia) 3D printable resin material. The crowns were made from three different CAD/CAM materials: leucite-reinforced glass ceramic IPS Empress CAD (IvoclarVivadent, Lichtenstein), hybrid nanoceramic Cerasmart (GC, Tokyo, Japan), and graphene-reinforced polymer G-CAM (Graphenano Dental, Spain). The Empress crowns were wet-milled, the Cerasmart and G-CAM crowns were dry-milled, using the Coritec 150i Pro (Imes-Icore, Germany) 5-axis milling machine. The samples were divided into three groups based on the thickness of the material crowns ().
Table 1.
Crown thickness according to the groups.
Table 1.
Crown thickness according to the groups.
| Dimensions |
Group 1 |
Group 2 |
Group 3 |
| Under the cusps |
0.6 mm |
1 mm |
1.5 mm |
| Cervical margins |
0.4 mm |
0.7 mm |
1 mm |
2.2. Cementation Procedure
The adhesive technique was used for the cementation of the crowns to the corresponding abutments. The internal surfaces of the Empress crowns were treated with 4.6% hydrofluoric acid (IPS Ceramic Etching gel - IvoclarVivadent, Schaan, Lichtenstein) for 60 s. For the Cerasmart and G-CAM crowns, the internal surfaces were lightly sandblasted with aluminium-oxide 20 µm particles at 0.2 MPa pressure for 10 s. Then, the primer G-Multi Primer (GC Australasia Dental, Australia) was applied according to the recommendations of manufacturers. For the abutment substrates, the bonding agent G-Premio Bond (GC Australasia Dental, Australia) was applied and cured, using a light-emitting diode curing unit (Zenolite LED Curing Light, President Dental, Germany) with a mean light intensity of 1200 mW/cm2. Dual-cure resin cement G-CEM LinkForceTM (GC Australasia Dental, Australia) was added into all crowns and immediately seated onto the abutments. The cement was light cured with 1200 mW LED light-curing unit. After a light prepolymerization of 1-2 s, the excess of cement was removed and the final polymerization was applied for 40 s on each surfaces. After cementation, all samples and specimens were stored in distilled water for one week at room temperature before testing, in order to ensure the water uptake by the organic phase is completed, mimicking the working conditions from the oral environment.
2.3. Specimen Fabrication
A total of twenty cylindrical specimens were prepared from each crowns group and Asiga resin abutment materials with circular cross-section of 4 mm diameter and an anvil height of 8 mm (n=5 per material) used for manufacturing of above-described abutments and crowns. They were polished and finished.
2.4. Mechanical Testing
Firstly, the cylindrical specimens made of the studied materials were tested under compression, and the mechanical properties evaluated were compressive stress and strain at maximum load, and the value of the modulus of elasticity (Young’s modulus). Secondly, the molar crowns were tested for the same parameters in the static conditions (Error! Reference source not found.). They were each positioned perpendicularly onto the metallic support of the universal testing machine (Instron 3366 – 10kN, Instron, USA) and a uniaxial force was applied vertically from the occlusal surface with a crosshead speed of 1 mm /min along the longitudinal axis of the crowns until fracture. An 8 mm stainless-steel bearing ball was used for the molar crowns in order to simulate the ideal tripodal contact point of the opposing cusp in the central fossa of the first mandibular molar. The maximum compressive load (N) and compressive extension at maximum load (mm) were recorded by the machine software (Blue Hill, Instron, USA) during each mechanical test.
Figure 1.
Prepared specimens (a) and samples (b) for compressive strength testing.
Figure 1.
Prepared specimens (a) and samples (b) for compressive strength testing.
2.5. Statistical Analysis
The data was exported in CSV files and was then aggregated in an Excel worksheet. For the compressive samples and specimens a mean value and standard deviations were calculated. The results obtained for molar samples were subjected to a more complex statistical analysis using the SPSS v26 software package. To test the difference between material groups, an analysis of variance would be appropriate. Considering the small sample and some violations of the assumptions of the ANOVA test, a non-parametric alternative was used. The Kruskal-Wallis test is a non-parametric alternative which does not assume that the data comes from a distribution that can be described through parameters such as mean and standard deviation, like in the case of the normal distribution [
29]. Like ANOVA it is used when there are three or more groups and the independent variable is continuous. Before applying the Kruskal-Wallis test, the normality of the data was tested with the Shapiro-Wilk test, the data was checked for outliers using the quartile method and the homogeneity of variance was tested using Levene’s test.
3. Results
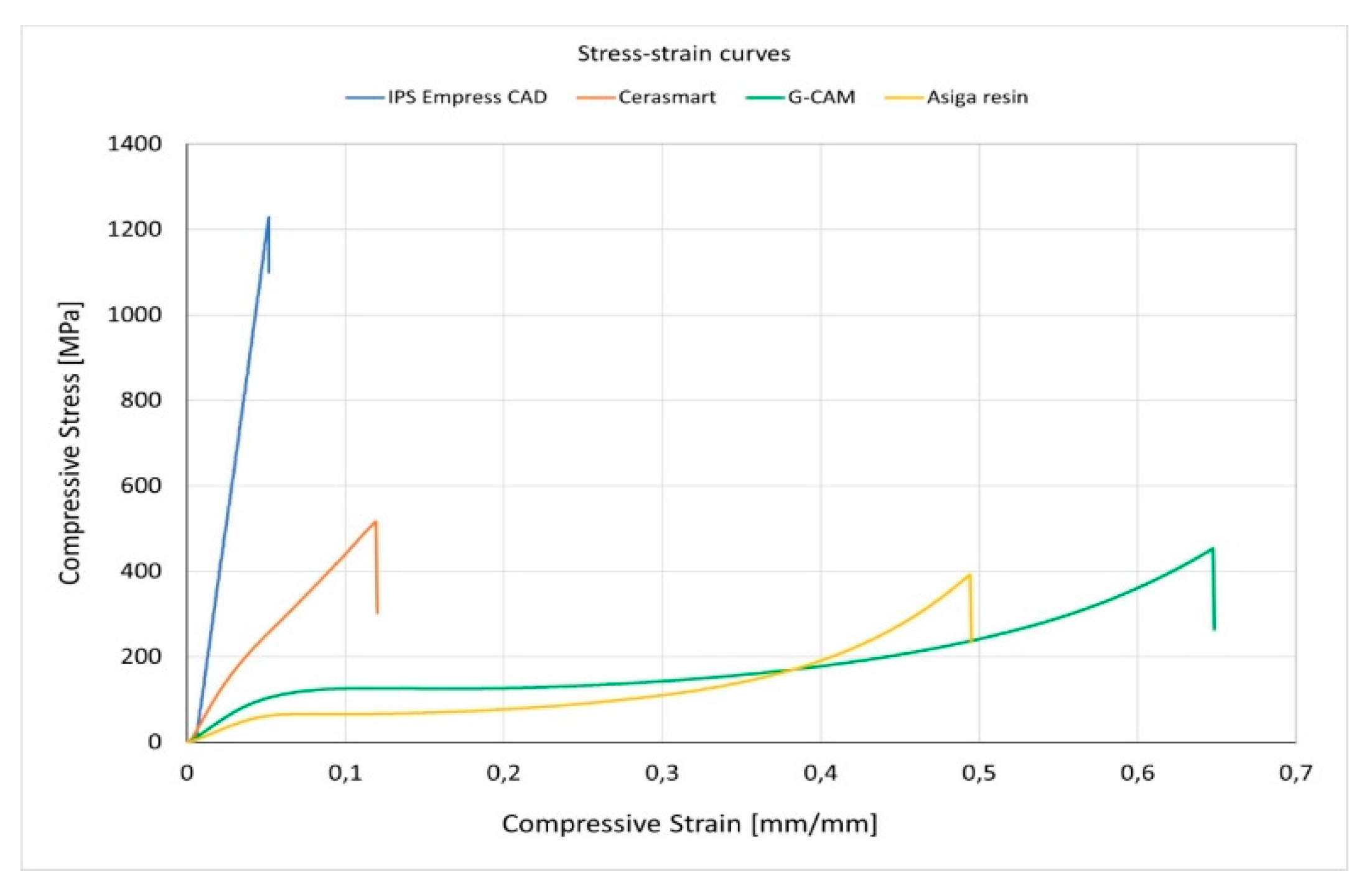
The mechanical properties of the cylindrical specimens made from the materials used for manufacturing the abutments and crowns and tested under the load were evaluated initially. In Figure 1 are shown the stress-strain curves of the investigated materials used to manufacture the abutments and crowns. Their mechanical behavior is essential in understanding the results obtained when two different materials are combined.
Figure 1.
Stress-strain curves of the investigated materials.
Figure 1.
Stress-strain curves of the investigated materials.
It was found the differences between the mechanical behavior of IPS Empress and Cerasmart materials on the one hand and the G-CAM and Asiga resin, on the other hand. If the former two exhibits reduced toughness, the others experience large deformations until fracture. The values of compressive stress, compressive strain and Young’s modulus for cylindrical specimens are presented in Table 1.
Table 1.
Descriptive statistics of the cylindrical specimens.
Table 1.
Descriptive statistics of the cylindrical specimens.
| Material |
Compressive Stress
[MPa] |
Compressive Strain
[mm/mm] |
Young’s Modulus
[MPa] |
| |
Average |
Std. Dev. |
Average |
Std. Dev. |
Average |
Std. Dev. |
IPS Empress
CAD |
1257.8 |
69.46 |
0.04974 |
0.00205 |
27540.7 |
295.77 |
| Cerasmart |
501.3 |
35.51 |
0.11526 |
0.00955 |
6358.9 |
159.96 |
| G-CAM |
435.3 |
33.53 |
0.64993 |
0.00222 |
2598.7 |
12.02 |
| Asiga resin |
360.4 |
28.25 |
0.51604 |
0.03082 |
1458.4 |
84.54 |
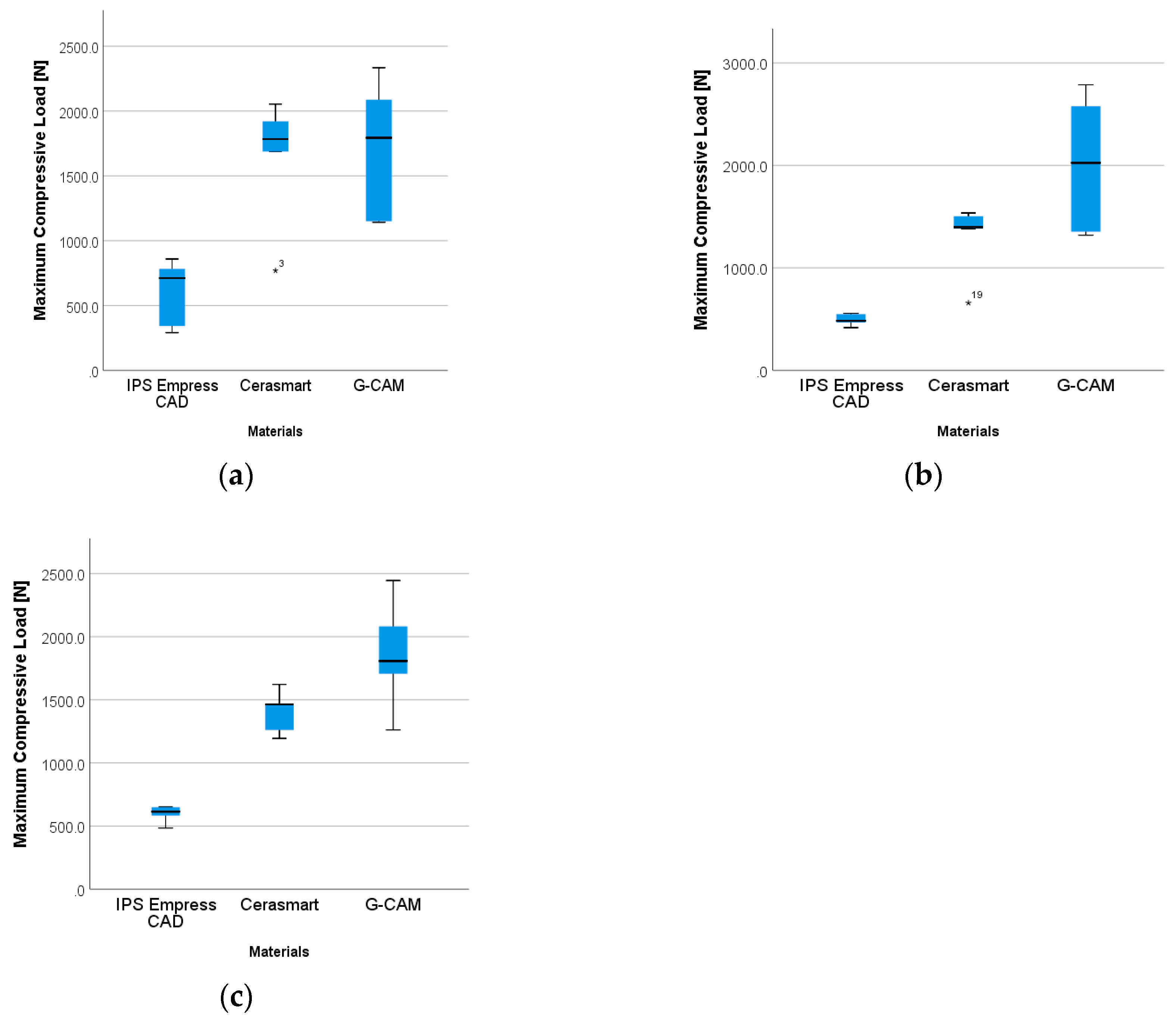
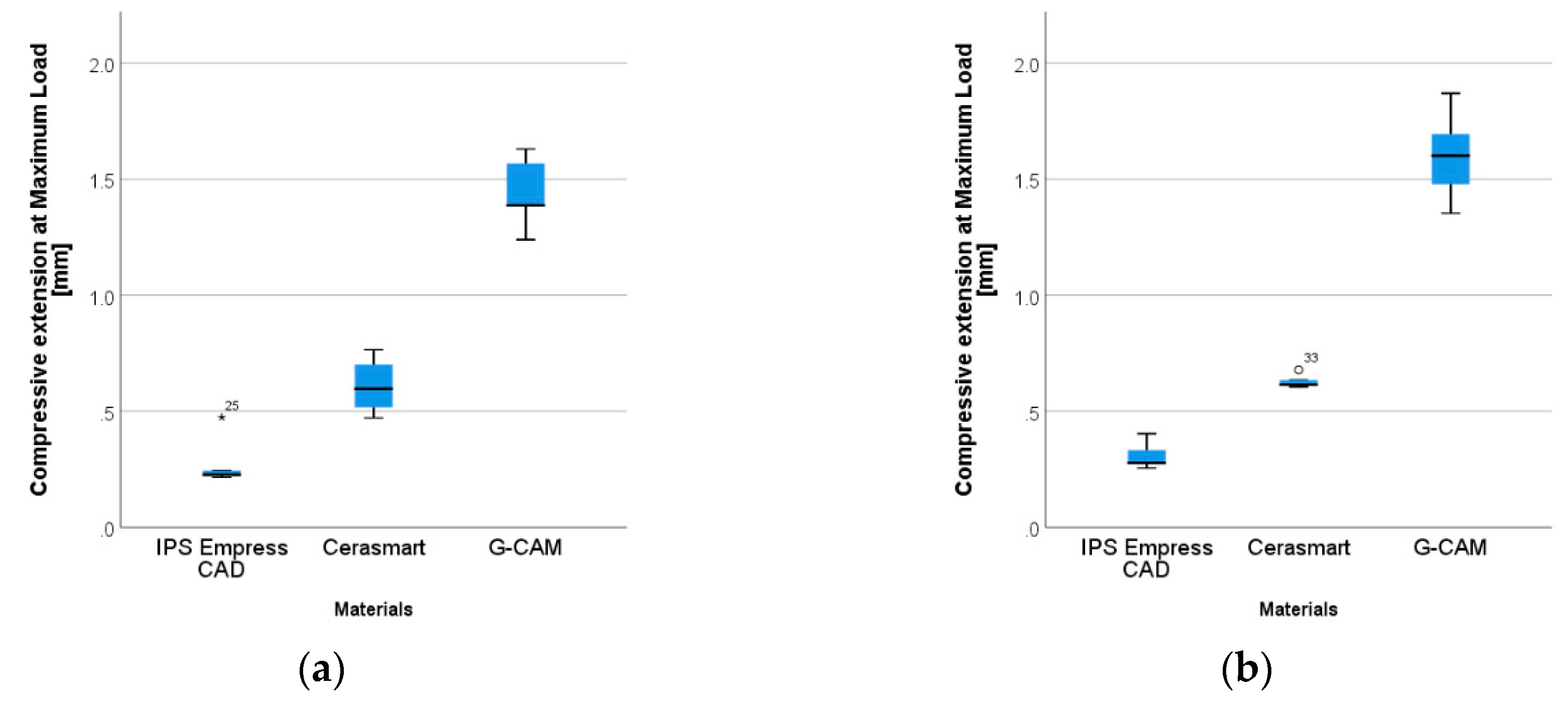
In case of the molar crowns samples, the descriptive statistics (average and standard deviation) regarding the maximum compressive load and compressive extension at maximum load for each material and thickness group are presented in
Table 2.
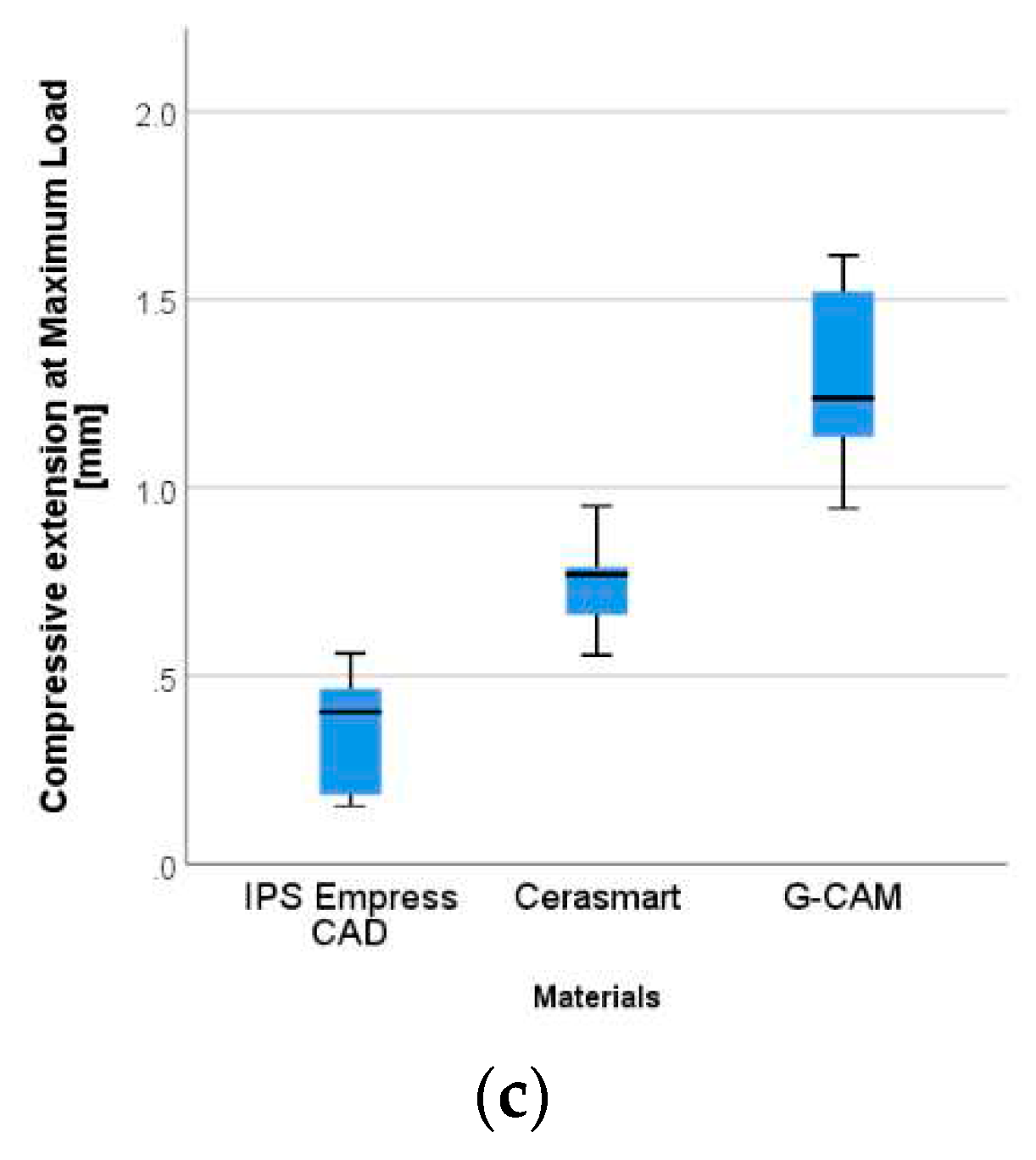
The distributions of values in each material category for the three thickness groups are depicted in
Figure 2 and
Figure 3. The values for G-CAM samples show a much wider distribution than the values in the other two material groups. This applies to all measured characteristics.
The molar samples fabricated from IPS Empress CAD seem to have lower load values than both Cerasmart and G-CAM. To test if this difference is statistically significant, an analysis of variance was performed.
The following hypotheses can be formulated:
H1. There is no significant difference in maximum compressive load between materials in each thickness group.
H2. There is no significant difference in compressive extension at maximum load between materials in each thickness group.
H3. There is no significant difference in maximum compressive load between materials regardless of thickness group.
H4. There is no significant difference in compressive extension at maximum load between materials regardless of thickness group.
As the variables are continuous and there are three material groups, an ANOVA would be appropriate. The ANOVA requires that the data be approximately normally distributed, there shouldn’t be any significant outliers, and there should be homogeneity of variance. The Shapiro-Wilk test was used to determine if the data is approximately normally distributed (
Table 3).
The quartile method was used to determine if there are any outliers. Values that are 1.5 times the interquartile range above the third quartile or below the first quartile were considered outliers. Some outliers were identified.
The homogeneity of variance was tested using Levene’s test of homogeneity of vari
Table 4.
The Levene’s test of homogeneity.
Table 4.
The Levene’s test of homogeneity.
| Characteristic |
Thickness |
Levene Statistic |
df1 |
df2 |
Sig. |
Maximum
compressive load |
0.6-0.4 |
1.157 |
2 |
12 |
0.347 |
| 1-0.7 |
6.448 |
2 |
12 |
0.013 |
| 1.5-1 |
4.061 |
2 |
12 |
0.045 |
Compressive extension
at maximum load |
0.6-0.4 |
1.902 |
2 |
12 |
0.192 |
| 1-0.7 |
0.687 |
2 |
12 |
0.522 |
| 1.5-1 |
4.861 |
2 |
12 |
0.028 |
Given the small sample size and the violation of some of the assumptions necessary for an ANOVA, the Kruskal-Wallis non-parametric test was used. It is the non-parametric alternative of ANOVA, does not have any assumption on the distribution of data and is more robust to outliers.
H1. The same type of test was used to determine if there is a significant difference in maximum compressive load between materials in different thickness groups. A significant difference between materials was found for all material thickness groups: 0.6-0.4 (H(2)=8.180, p=.017), 1-0.7 (H(2)=9.780, p=.008) and 1.5-1 (H(2)=11.180, p=.004). The distributions of the data were similar as observed from the box plot. A Dunn post-hoc test with a Bonferroni correction revealed that in all cases G-CAM (Me0.6-0.4= 1793.9N, Me1-0.7= 2024.85N, Me1.5-1=1807.39N) had a significantly higher maximum compressive load than Empress (Me0.6-0.4= 711.8N, Me1-0.7= 483.2N, Me1.5-1= 613.9N) (Table 6)
H2. The difference in compressive extension between materials in different thickness groups was also tested using the Kruskal-Wallis test. A significant difference between materials was found for all material thickness groups: 0.6-0.4 (H(2)=11.520, p=.003), 1-0.7 (H(2)=12.020, p=.002) and 1.5-1 (H(2)=12.500, p=.002). The distributions of the data were similar as observed from the box plot. A Dunn post-hoc test with a Bonferroni correction revealed that in all cases G-CAM (Me0.6-0.4= 1.238mm, Me1-0.7= 1.386mm, Me1.5-1= 1.601mm) had a significantly higher compressive extension than IPS Empress CAD (Me0.6-0.4= 0.405mm, Me1-0.7= 0.226mm, Me1.5-1= 0.277mm).
Table 5 shows the test statistics for the Kruskal-Wallis tests with their corresponding adjusted p-values for each thickness group for the tested hypotheses.
The Kruskal Wallis test was also applied to the three materials regardless of their thickness groups for the measured characteristics.
H3. The maximum compressive load was also significantly different between material groups (H(2)=29.839, p<.001). The distributions of the data were similar as observed from the box plot. A Dunn post-hoc test with a Bonferroni correction revealed that G-CAM (Me= 1807.4N) and Cerasmart (Me= 1464.1N) had a significantly higher maximum compressive load than IPS Empress CAD (Me= 555.5N)(zG-CAM-IPSEmpressCAD=3.920, p<.001; zCerasmart-IPSEmpressCAD=-5.255, p<.001).
H4. A significant difference between material groups was found also for the compressive extension at maximum values (H(2)=38.271, p<.001). The distributions of the data were similar as observed from the box plot. A Dunn post-hoc test with a Bonferroni correction revealed that G-CAM (Me= 1.478mm) had a significantly higher compressive extension than both Cerasmart (Me=0.635mm) and IPS Empress CAD (Me= 0.273mm)(zG-CAM-Empress=-3.156, p=.005; zG-CAM-Cerasmart=-6.186, p<.001, zCerasmart-IPSEmpressCAD=3.030, p=.007).
4. Discussion
The experimental study aimed to investigate the mechanical behavior of three CAD/CAM restorative materials: IPS Empress CAD (IvoclarVivadent), Cerasmart (GC) and G-CAM (Grafenano Dental) used for the fabrication of the molar crowns and tested in terms of the resistance to axial compressive load. The samples formed from cemented crowns on the Asiga resin dies and the cylindrical specimens fabricated from each type of material were analysed and the correlations between the mechanical properties of the crowns and abutments’ materials were also made.
The results suggested that the mean values of maximum compressive load for G-CAM crowns were statistically significantly higher than those of IPS Empress CAD and Cerasmart for the same thickness group. The statistically significant differences regarding the compressive load were found between G-CAM and IPS Empress CAD crowns. Between G-CAM and Cerasmart materials there are differences in this regard, but not statistically significant. It can be stated that the null hypothesis has been rejected in both circumstances after assembling and assessing the data.
The physiological and normal mastication force varies from 70 to 150N, with a maximal biting force of 500 to 700N, according to Scully's Oxford Handbook of Dental Science [
30]. Several other studies have corroborated this, despite the fact that maximal biting forces of up to 1000N have been documented in the past among some Eskimo groups [
31,
32,
33,
34].
The mechanical properties of restorative materials have impact on the clinical performance and long-term longevity of CAD/CAM restorations. These properties differ from one type of material to another and mainly depend on the microstructure [
2,
22].
The compressive strength and Young’s modulus are the important properties of the materials to be considered when assessing the mechanical behavior of crown materials and abutment substrates by reason of the chewing forces. The values of the compressive strength and Young’s modulus for the tested materials were for IPS Empress CAD 1258 MPa and 27 GPa; for Cerasmart 501.3 MPa and 6.3 GPa and for G-CAM 435 MPa and 2.5 GPa. Based on the results of this experimental study, the compressive strength and Young’s modulus for the Asiga resin material were 360 MPa and 1.4 GPa, in comparison with the dentin as the tooth substrate values the compressive strength is 297 MPa and modulus of elasticity for compression is 17 GPa. [
35,
36]. These findings indicated the difference between modulus of elasticity of the Asiga resin used as an abutment material and the dentin.
Combining materials with different toughness will influence the mechanical behavior of CAD/CAM manufactured molar samples. The abutment has a more ductile behavior with large deformations until fracture and the crowns made of a brittle material will fracture at lower compressive forces with a glass-like fracture pattern. Due to the fragile behavior, the analyzed thickness of the IPS Empress CAD crowns does not have a significant influence on the compressive strength of the samples; almost all the samples presented the defects at the crowns, only in the form of chips. Our results showed that IPS Empress CAD has significantly lower force bearing values than the other two materials (Cerasmart and G-CAM), in spite of the fact that leucite-based ceramics have a crystalline phase that enhances the mechanical properties of the material, with quantity and homogeneity of the crystals being the essential factors preventing the crack propagation [
37].
Fradeani et al. clinically assessed 125 crowns made of leucite-reinforced glass ceramic over 11-year period, showing a high survival probability of 95.2% (98.9% for anterior teeth and 84.4% for posterior teeth). The authors concluded that these crowns exhibited low failure rate, excellent aesthetic and emphasized the importance of using adhesive cementation technique for ensuring the success rate [
38].
A study carried out by Murgueitio analysed the survival rate and failure mode of IPS leucite-reinforced ceramic onlays and partial crowns by measuring occlusal thickness and performing a 3-year follow-up and demonstrated that increased material thickness determines a lower chance of failure and vital teeth are less likely to fail compared to non-vital ones [
39]. A controlled clinical trial conducted by Frankenberger assessing 96 IPS Empress indirect restorations (inlays and onlays) over a 12-year period found satisfactory clinical results, with a low failure rate of 16% and with more bulk fractures when cementation was performed with a light-curing composite. The restorations with dual cure resin cement exhibited significantly fewer bulk fractures [
40].
An
in-vitro study conducted by Heintze evaluated mandibular molar crowns made of IPS Empress and IPS e.max Press adhesively cemented on CAD/CAM milled PMMA abutments during static and dynamic loading. All crowns were loaded by applying an eccentric force in a chewing simulator. Another four crowns of each material were subjected to force measurements with a 3D force sensor during dynamic loading using two different lateral movements (from fossa to cusp and vice versa). The fracture rate of IPS Empress molar crowns was higher compared to IPS e.max Press, 50% of the IPS Empress crowns failed (75% fractures and 25% chippings) during dynamic loading, while lithium disilicate ceramic molar crowns presented no fracture, even if the forces exerted on the crowns and abutments were 2-3 times higher than those during static loading [
20].
In our study, molar samples manufactured with Cerasmart crowns proved to have a higher load resistance compared to IPS Empress CAD crowns but a slightly lower one that G-CAM. The results can be explained by the fact that Cerasmart and Asiga resin have similar ultimate stress, but the crown material will be more brittle. In G1, the samples have more complete fractures because the low thicknesses of the crown contributes to a lesser extent to the overall strenght of the sample. As the crown thickness increases, the number of complete fractures decreases, the material contributing more to the strength of the sample; increased thickness leads to a higher strenght of molar samples. The results of this study are confirmed by other studies, which demonstrated a high compressive strength and good fracture performance for resin ceramic materials [
22].
Jassim
et al. performed a comparative assessment of fracture strength for crowns made of CAD/CAM materials (lithium disilicate, zirconia, reinforced composite, hybrid ceramic - Cerasmart and zirconia-reinforced lithium silicate) on first premolars prepared teeth, extracted for orthodontic purposes, which were subjected, post cementation, to an axial compressive force, and noticed the differences between these materials with regard to fracture strength owing to their different chemical composition and microstructure [
41].
A clinical study evaluated for a period from 1 to 9 years the clinical performance of 121 all ceramic crowns, fabricated by IPS Empress 2 system, placed on the vital teeth, except for 11 crowns fixed on endodontically treated teeth. It was found a survival rate of 95.24% after 5 years and 87.1% up to 9 years and all ceramic crowns applied on the endodontically treated teeth without post and core restorations showed a higher failure rate compared to all-ceramic crowns on vital teeth [
42].
Fages and collaborators carried out a study at three levels: in vitro (compressive mechanical tests), in silico (finite elements simulations) and in vivo (clinical survival rate) by analyzing glass ceramic CAD/CAM crowns made of Vita Mark II applied on the premolars and molars teeth. The in vitro and
in silico studies showed that an adequate geometric design of the preparations permit to increase up to 80% the mechanical strength of ceramic crowns. The in vivo clinical study of CAD/CAM full-ceramic crowns was realized based on the results obtained in vitro and in silico studies and exhibited a 98.97% success rate over a 6-year period [
43]. Resin matrix-ceramic Enamic exhibited a survival rate of 92.9% and 96.8% at 2 years when analyzed 45 full coverage single-unit crowns [
44].
Mechanical compatibility in terms of maximum compressive stresses and strains between the material of abutments (Asiga resin) and crowns made of G-CAM will lead to higher compressive loads that can be applied onto the molar samples. For G-CAM, as the thickness of the crowns increases and the material have the same properties, the samples presented complete fracture (abutment and crown). The thicker the crowns in G3, the more the numbers of complete fractures (abutment and crown) increase. At present, there are relatively few studies focusing on the G-CAM material, which is why it was not possible to correlate the results of the present study with others.
Regarding the restoration’ cementation, G-CEM Link Force is adhesive resin cement with the capacity to adhere to the restorative materials due to the functional monomers in the composition and the adhesive protocol increase the fracture strength of the crowns [
45]. The bond strength of the resin cement is influenced by the surface treatments; the shear bond strength for the sand blast pretreatment surfaces was higher compared to the acid-etch alone [
46].
There are several limitations of this study: the small sample size, the testing conditions do not reflect the complexity of the oral cavity and used a simplified model that considers only the axial compressive load on the dental crown and 3D resin printed abutment as a substrate, obtained in the standardized way. Further studies are required to evaluate the CAD/CAM materials in similar conditions to those in the oral environment and to simulate the action of the chewing forces. The aspects investigated in this study could be taken into consideration when clinicians choose the appropriate material for the prosthetic rehabilitation in various clinical situations.
5. Conclusions
1. IPS Empress CAD and Cerasmart materials have a fragile behavior, with a high compressive strength and Young’s modulus and compared to G-CAM and Asiga resins.
2. The mechanical behaviour of the CAD/CAM materials influences the values of the compressive strength on the molar samples; the abutments have a more ductile behavior, with large deformations under compressive load, whereas Cerasmart crowns present higher load resistance compared to IPS Empress CAD crowns, but slightly lower that G-CAM.
3. The mechanical compatibility between abutments and G-CAM crowns regarding the maximum compressive stresses and strains enables higher compressive loads to be applied on the molar samples.
4. For IPS Empress CAD, crown thickness does not have a significant influence on compressive strength. For Cerasmart, the thickness increases as the number of complete fractures decreases. For G-CAM, if the thickness increases and the materials have the same properties, the number of complete fractures increases also.
Author Contributions
Conceptualization, S.D.B, M.C.; methodology, S.D.B., M.C.D.; software: V.B.; A.M.B.; validation, S.D.B.; A.M.B.; V.B.; formal analysis, S.D.B.; A.M.B.; investigation, S.D.B.; A.M.B. ; resources, A.M.B.; data curation, M.C.; writing-original draft preparation, A.M.B.; M.C.; writing-review and editing, A.M.B..; M.C.; visualization, S.D.B; M.C.D.; supervision, S.D.B.; M.C.D.; project administration, S.D.B.; A.M.B.; M.C.D.; funding acquisition, S.D.B; M.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
This study did not require ethical approval because human subjects were not used.
Data Availability Statement
The data presented in this study are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Goujat, A.; Abouelleil, H.; Colon, P.; Jeannin, C.; Pradelle, N.; Seux, D.; Grosgogeat, B. Mechanical properties and internal fit of 4 CAD-CAM block materials. J Prosthet Dent. 2018, 119, 384–389. [Google Scholar] [CrossRef] [PubMed]
- Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on polymer, ceramic and composite materials for CAD/CAM indirect restorations in dentistry - application, mechanical characteristics and comparison. Materials 2021, 14, 1592. [Google Scholar] [CrossRef]
- Renne, W.; Ludlow, M.; Fryml, J.; Schurch, Z.; Mennito, A.; Kessler, R.; Lauer, A. Evaluation of the accuracy of 7 digital scanners: An in vitro analysis based on 3-dimensional comparisons. J Prosthet Dent. 2017, 118, 36–42. [Google Scholar] [CrossRef]
- Schmidt, A.; Klussmann, L.; Wöstmann, B.; Schlenz, M.A. Accuracy of digital and conventional full-arch impressions in patients: An update. J Clin Med. 2020, 9, 688. [Google Scholar] [CrossRef]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J Prosthodont Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Furtado de Mendonca, A.; Shahmoradi, M.; Gouvêa, C.V.D.; de Souza, G.M.; Ellakwa, A. Microstructural and mechanical characterization of CAD/CAM materials for monolithic dental restorations: Characterization of CAD/CAM materials. J Prosthodont. 2019, 28, e587–e594. [Google Scholar] [CrossRef] [PubMed]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials. J Prosthet Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br Dent, J. 2008, 204, 505–511. [Google Scholar] [CrossRef]
- Miyazaki, T.; Hotta, Y. CAD/CAM systems available for the fabrication of crown and bridge restorations: CAD/CAM systems. Aust Dent, J. 2011, 56, 97–106. [Google Scholar] [CrossRef]
- Di Carlo, S.; De Angelis, F.; Brauner, E.; Pranno, N.; Tassi, G.; Senatore, M.; Bossù, M. Flexural strength and elastic modulus evaluation of structures made by conventional PMMA and PMMA reinforced with graphene. Eur Rev Med Pharmacol Sci 2020, 24, 5201–5208. [Google Scholar]
- Rekow, D. Computer-aided design and manufacturing in dentistry: A review of the state of the art. J. Prosthet Dent. 1987, 58, 512–516. [Google Scholar] [CrossRef] [PubMed]
- Uzun, G. An overview of dental CAD/CAM systems. Biotechnol Biotechnol Equip. 2008, 22, 530–535. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J Mech Behav Biomed Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef] [PubMed]
- Hynková, K.; Özcan, M.; Voborná, I. Composition and mechanical properties of contemporary CAD/CAM glass ceramics. Ital J Dent Med. 2020, 5, 63–69. [Google Scholar]
- Sakaguchi, R.L.; Ferracane, J.L.; Powers, J.M. Craig’s Restorative Dental Materials, 4th ed.; Elsevier: St. Louis, Missouri, 2019. [Google Scholar]
- Ritzberger, C.; Apel, E.; Höland, W.; Peschke, A.; Rheinberger, V. Properties and clinical application of three types of dental glass-ceramics and ceramics for CAD-CAM technologies. Materials 2010, 3, 3700–3713. [Google Scholar] [CrossRef]
- Brochu, J.F.; El-Mowafy, O. Longevity and clinical performance of IPS-Empress ceramic restorations - A literature review. J Can Dent Assoc 2002, 68, 233–237. [Google Scholar]
- Fasbinder, D.J. Clinical performance of chairside CAD/CAM restorations. J Am Dent Assoc. 2006, 137, 22S–31S. [Google Scholar] [CrossRef]
- Dhima, M.; Paulusova, V.; Carr, A.B.; Rieck, K.L.; Lohse, C.; Salinas, T.J. Practice-based clinical evaluation of ceramic single crowns after at least five years. J Prosthet Dent. 2014, 111, 124–130. [Google Scholar] [CrossRef]
- Heintze, S.; Rousson, V. Fracture rates of IPS Empress all-ceramic crowns-A systematic review. Int, J. Prosthodont. 2010, 23, 129–133. [Google Scholar]
- Lauvahutanon, S.; Takahashi, H.; Shiozawa, M.; Iwasaki, N.; Asakawa, Y.; Oki, M.; Finger, W.J.; Arksornnukit, M. Mechanical properties of composite resin blocks for CAD/CAM. Dent Mater, J. 2014, 33, 705–710. [Google Scholar] [CrossRef] [PubMed]
- Alamoush, R.A.; Silikas, N.; Salim, N.A.; Al-Nasrawi, S.; Satterthwaite, J.D. Effect of the composition of CAD/CAM composite blocks on mechanical properties. BioMed Res Int. 2018, 4893143. [Google Scholar] [CrossRef] [PubMed]
- Sorrentino, R. In vitro analysis of the fracture resistance of CAD-CAM Cerasmart molar crowns with different occlusal thickness. Biomed. J Sci Tech Res. 2018, 3. [Google Scholar] [CrossRef]
- Peyton, F.A. History of resins in dentistry. Dent Clin North Am. 1975, 19, 211–222. [Google Scholar] [CrossRef]
- Novoselov, K.S.; Geim, A.K.; Morozov, S.V.; Jiang, D.E.; Zhang, Y.; Dubonos, S.V.; Grigorieva, I.V.; Firsov, A. Electric field effect in atomically thin carbon films. Science 2004, 306, 666–669. [Google Scholar] [CrossRef]
- Gad, M.M.; Fouda, S.M.; Al-Harbi, F.A.; Näpänkangas, R.; Raustia, A. PMMA denture base material enhancement: A review of fiber, filler, and nanofiller addition. Int J Nanomedicine 2017, 12, 3801–3812. [Google Scholar] [CrossRef]
- Abdulrazzaq Naji, S.; Jafarzadeh Kashi, T.S.; Behroozibakhsh, M.; Hajizamani, H.; Habibzadeh, S. Recent advances and future perspectives for reinforcement of poly (methyl methacrylate) denture base materials: A literature review. J Dent Biomater. 2018, 5, 490–502. [Google Scholar]
- Agarwalla, S.V.; Malhotra, R.; Rosa, V. Translucency, hardness and strength parameters of PMMA resin containing graphene-like material for CAD/CAM restorations. J Mech Behav Biomed Mater. 2019, 100, 103388. [Google Scholar] [CrossRef] [PubMed]
- McDonald, J.H. Handb. Biol. Stat. 2014.
- Scully, C. Physiological biting force. In Oxford Handbook of Applied Dental Science; Oxford University Press inc.: United States, 2002. [Google Scholar]
- Al-Zarea, B.K. Maximum bite force following unilateral fixed prosthetic treatment: A within-subject comparison to the dentate side. Med Princ Pract. 2015, 24, 142–146. [Google Scholar] [CrossRef]
- Takaki, P.; Vieira, M.; Bommarito, S. Maximum bite force analysis in different age groups. Int Arch Otorhinolaryngol. 2014, 18, 272–276. [Google Scholar]
- Varga, S.; Spalj, S.; Lapter Varga, M.; Anic Milosevic, S.; Mestrovic, S.; Slaj, M. Maximum voluntary molar bite force in subjects with normal occlusion. Eur J Orthod. 2011, 33, 427–433. [Google Scholar] [CrossRef]
- Waugh, L.M. Dental Observations Among Eskimo. J Dent Res 1937, 16, 355–356. [Google Scholar]
- Milewski, G. Numerical and experimental analysis of effort of human tooth hard tissues in terms of proper occlusal loadings. Acta Bioeng Biomech. 2005, 7, 47–59. [Google Scholar]
- Angker, L.; Swain, M.V.; Kilpatrick, N. Micro-mechanical characterisation of the properties of primary tooth dentine. J Dent. 2003, 31, 261–267. [Google Scholar] [CrossRef]
- Byeon, S.M.; Song, J.J. Mechanical properties and microstructure of the leucite-reinforced glass-ceramics for dental CAD/CAM. J Dent Hyg Sci. 2018, 18, 42–49. [Google Scholar] [CrossRef]
- Fradeani, M.; Redemagni, M. An 11-year clinical evaluation of leucite-reinforced glass-ceramic crowns: A retrospective study. Quintessence Int 2002, 33, 503–510. [Google Scholar]
- Murgueitio, R.; Bernal, G. Three-year clinical follow-up of posterior teeth restored with leucite-reinforced IPS Empress onlays and partial veneer crowns: Three-year clinical follow-up of ceramic onlays and partial crowns. J Prosthodont. 2012, 21, 340–345. [Google Scholar] [CrossRef]
- Frankenberger, R.; Taschner, M.; Garcia-Godoy, F.; Petschelt, A.; Krämer, N. Leucite-reinforced glass ceramic inlays and onlays after 12 years. J Adhes Dent 2008, 10, 393–398. [Google Scholar]
- Jassim, Z.M.; Majeed, M.A. Comparative evaluation of the fracture strength of monolithic crowns fabricated from different all-ceramic CAD/CAM materials (an in vitro study). Biomed Pharmacol, J. 2018, 11, 1689–1697. [Google Scholar] [CrossRef]
- Toman, M.; Toksavul, S. Clinical Evaluation of 121 lithium disilicate all-ceramic crowns up to 9 years. Quintess Int. 2015, 46, 189–197. [Google Scholar]
- Fages, M.; Corn, S.; Slangen, P.; Raynal, J.; Ienny, P.; Turzo, K.; Cuisinier, F.; Durand, J.C. Glass ceramic CAD/CAM crowns and severely altered posterior teeth: A three levels study. J Mater Sci Mater Med. 2017, 28, 145. [Google Scholar] [CrossRef]
- Chirumamilla, G.; Goldstein, C.E.; Lawson, N.C. A 2-year retrospective clinical study of Enamic crowns performed in a private practice setting: Clinical study of Enamic crowns performed in a private practice setting. J Esthet Restor Dent. 2016, 28, 231–237. [Google Scholar] [CrossRef] [PubMed]
- Guerreiro, J.; Dias, R.; Carracho, J. Influence of cement type on the fracture resistance of resin nanoceramic crowns over knife-edge margins: A pilot study. Rev Port Estomatol Med Dent Cir Maxilofac 2021, 62, 150–156. [Google Scholar] [CrossRef]
- Alkhurays, M. Influence of different luting cements on the shear bond strength of pretreated lithium disilicate materials. J Contemp Dent Pract. 2019, 20, 1056–1060. [Google Scholar] [CrossRef] [PubMed]
|
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions, or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).